Abstract
Objective
To determine if focal increased uptake at the rotator interval (RI) and/or inferior capsule (IC) on 18F-FDG PET/CT (“positive PET”) predicts the presence of adhesive capsulitis (AC).
Materials and Methods
Three populations were retrospectively examined. Group 1 included 1,137 consecutive 18F-FDG PET/CT studies and was used to determine the prevalence of focal uptake at the RI or IC. Group 2 included 361 cases from a 10-year period with 18F-FDG PET/CT and MRI of shoulder performed within 45 days of each other and was used to enrich the study group. Group 3 included 109 randomly selected patients from the same time frame as groups 1 and 2 and was used to generate the control group. The study group consisted of 15 cases from the 3 groups, which had positive PET findings. PET/CT images were assessed in consensus by two musculoskeletal radiologists. The reference standard for a diagnosis of AC was clinical and was made by review of the medical record by a pain medicine physician.
Results
The prevalence of focal activity at either the RI or IC (“positive PET”) was 0.53%. Nine patients had a clinical diagnosis of AC and 15 patients had a positive PET. The sensitivity and specificity of PET for detection of AC was 56% and 87%, respectively. PET/CT had a positive likelihood ratio for AC of 6.3 (95% CI: 2.8–14.6).
Conclusion
Increased uptake at the RI or IC on PET/CT confers a moderate increase in the likelihood of AC.
Keywords: FDG PET/CT, adhesive capsulitis, rotator interval, inferior capsule
Introduction
18F-FDG PET/CT is a powerful diagnostic tool in oncology due to its ability to localize metabolically active neoplastic tissues. However, degenerative and inflammatory processes can have increased uptake and sometimes present a diagnostic. In the course of interpretation of 18F-FDG PET/CTs in a busy oncological practice, we have encountered cases of focal increased uptake in the region of the rotator interval (RI) and inferior capsule (IC) that were found to be unrelated to neoplasm (Fig. 1) [1]. Because signal abnormality at the RI and IC has been associated with adhesive capsulitis (AC) on MRI [2, 3], increased uptake at these locations has been anecdotally linked to AC [1, 4, 5]. However, this association has not been systematically studied.
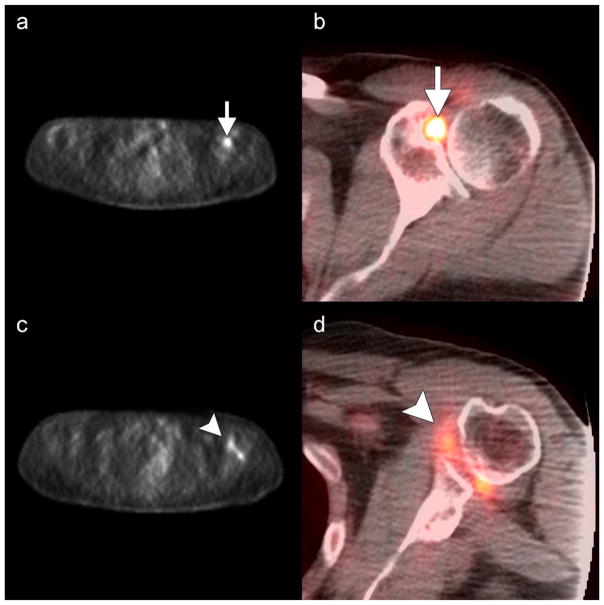
Fig. 1.
Focal uptake at the rotator interval and axillary pouch. Axial unfused (a and c) and fused (b and d) 18F-FDG PET/CT images in a 64-year-old man with mantle cell lymphoma reveals focal increased uptake at the a–b) rotator interval (arrows, SUV=5.8) and c–d) inferior capsule (arrowheads, SUV=3.5).
Adhesive capsulitis is a relatively common inflammatory disorder of the shoulder joint associated with pain and limited range of motion [6]. Early conservative management (e.g., passive exercises) and minimally invasive intervention (e.g., manipulation under anesthesia and intra-articular steroid injection) have been shown to result in improved outcomes [7–10] and can prevent the “downward spiral of learned disuse” associated with adhesive capsulitis [8]. Incidentally detected increased uptake at the RI and IC on PET/CT may allow patients with AC to receive an early diagnosis and timely treatment. However, current data are lacking, and it is unknown if increased uptake at these locations reliably predicts the presence of AC in unselected patients undergoing 18F-FDG PET/CT.
This study aims to provide preliminary data towards that goal, and determine the ability of 18F-FDG PET/CT to detect AC based on increased uptake at the RI and/or IC. The central hypothesis is that increased uptake at these locations is associated with the presence of AC. A secondary aim was to determine the agreement of uptake on 18F-FDG PET/CT with signal abnormality on MRI.
Methods
Institutional review board approval was obtained as required for this retrospective cohort study. Inclusion criteria was patients with 1) 18F-FDG PET/CTs performed at our institution and 2) no history of surgical intervention at the shoulders.
Patient Groups
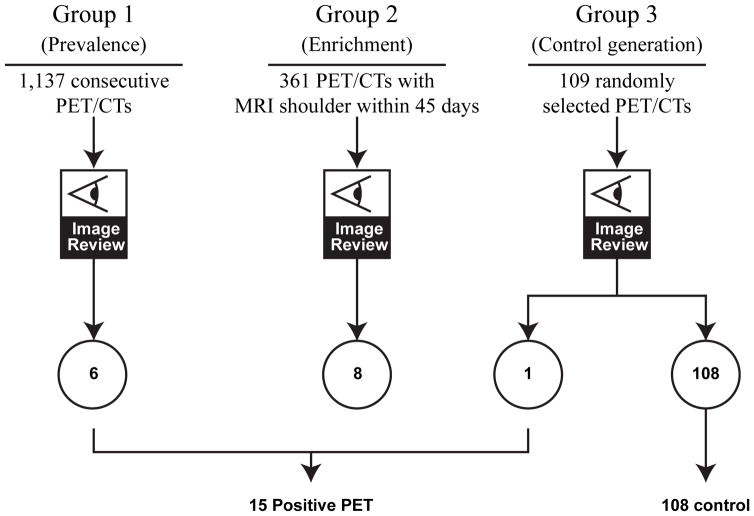
Three different patient populations were examined for different analysis purposes (Fig. 2). Group 1 included 1,137 consecutive 18F-FDG PET/CT studies performed in January 2009. This group was used to determine the prevalence of abnormalities at the RI or IC (defined below). The year was chosen to allow for sufficient follow-up to allow confident determination of whether uptake was related to malignancy. Group 2 included 361 cases from 04/09/2003 to 07/04/2014 with 18F-FDG PET/CT and MRIs performed within 45 days of each other. This group was used to enrich the study population (the MRIs were not reviewed as part of this study). Group 3 included 109 randomly selected patients from the same time frame as the above groups and was used to generate a control group for clinical symptoms. Patients from groups 1 and 2 were excluded from the pre-randomization selection pool. Positive PET cases from the 3 groups were used to form the study group (please refer to Imaging and Image Analysis below for definition of “positive PET”). Cases from the study group were mixed with negative cases from group 3 and presented to a pain management physician (MPE) for chart review (see Chart Review below).
Fig. 2.
Patient groups.
Imaging and Image Analysis
All 18F-FDG PET/CTs were performed at our institution according to standard guidelines and uniform image acquisition and processing protocols. Patients were instructed to fast for at least 6 hours prior to imaging and had a measured blood glucose level of less than 150 mg/dL at the time of radiopharmaceutical administration. Patients received 370 – 740 MBq of 18F-FDG, and were asked to rest quietly in a darkened room for about 60 minutes before images were acquired on a PET/CT scanner (Discovery, GE Healthcare, Milwaukee, WI). CT images were acquired without oral or intravenous contrast, and used for attenuation correction of PET data.
18F-FDG PET/CTs from patients in all 3 groups were reviewed by 2 radiologists with fellowship training in musculoskeletal radiology (RS and BA), one of whom also had special expertise in oncological imaging and PET/CT (BA). The readers were blinded to the clinical data. Specifically, the readers did not know if the patient had symptoms related to the shoulders. A positive PET was defined as one with focal 18F-FDG uptake confined to the RI or IC, which was subjectively greater than that of the adjacent synovium and muscles (Fig. 1). Progression to malignancy of focal uptake at the RI and IC was assessed on follow-up imaging on all modalities. Cases where increased uptake at the RI and IC was part of diffuse synovitis (i.e., the uptake was not focal) were not considered positive.
Chart Review
In the positive and control cases, data were collected on patient demographics (age, gender, and race), presence of common comorbidities (diabetes and thyroid dysfunction), underlying cancer diagnosis and disease status, and the presence of symptoms related to the shoulders. A fellowship-trained pain medicine physician (MPE) was blinded to the images and reports and reviewed the electronic medical record for clinic notes at or within 30 days of the MRI or 18F-FDG PET/CT for documentation of shoulder pain. The clinic notes were from a variety of clinical services, including orthopedics, rheumatology, cancer pain service, and a variety of oncological subspecialties. The presence of AC was subjectively classified as positive for AC, negative for AC, or unclear (not enough evidence for or against a diagnosis).
Statistical Analysis
Summary statistics of patient characteristics were provided in the form of mean, SD, and range for continuous outcomes (age) and in the form of frequency and percentages for categorical outcomes (race, gender, presence of diabetes, and presence of symptoms related to the shoulder joints). The prevalence of focal uptake at the RI and IC along with their exact binomial confidence intervals was estimated. All tests were two-sided, and p-values of 0.05 or less were considered statistically significant. Statistical analysis was carried out using SAS version 9 (SAS Institute, Cary, NC).
Results
A total of 6 positive PETs (focal increased uptake at the RI or IC) was identified from the 1,137 consecutive 18F-FDG PET/CTs in Group 1, for a prevalence of 0.53% (95% CI: 0.22–1.12%).
The study group was generated from these 6 cases plus positive cases found in Groups 2 and 3. Group 2 consisted of 361 patients with PET/CT and MRI shoulder performed within 45 days of each other. Among these patients, 8 were found with positive PETs and included in the study group. Group 3 consisted of 109 randomly selected cases and was used to generate the control group. A single positive PET was found in this group, which could not be used as a control, and was moved to the study group. A total of 15 cases were thus included in the study group (6 + 8 + 1) and 108 cases were included in the study group (109-1).
The 108 patients from the control group were combined with the 15 patients from the study group. A pain medicine physician, blinded to the imaging findings, reviewed the patient record to determine if symptoms consistent with AC were present at the time of PET/CT. Of these 123 patients, 9 classified as positive for AC, 47 as negative for AC, and 67 as unclear (not enough evidence for or against a diagnosis).
This clinical assessment of AC was used as the reference standard for comparison with 18F-FDG PET-CT findings. The correlation between PET-positivity and AC was significant (Fisher’s exact, p = 0.001). Five of the 15 PET-positive patients had AC (33%), while 4 of the 108 control patients had AC (4%). All of the 5 PET-positive patients with AC were from the MRI group (Group 2).
The sensitivity of PET for detection of AC was 56% (95% CI: 23% – 85%), and the specificity was 91% (95% CI: 84%–95%). The positive likelihood ratio was 6.3 (95% CI: 2.8 – 14.6). The negative likelihood ratio was 0.49 (95% CI: 0.2 – 1.01).
Discussion
Increased FDG uptake can occur in neoplastic and inflammatory cells, due to increased expression of glucose transporters. The high sensitivity of 18F-FDG PET/CT is therefore accompanied by low specificity. At the glenohumeral joint, non-neoplastic uptake can be seen in patients diagnosed with AC [1, 4, 5], osteoarthritis [11], rheumatoid arthritis [12], subacromial impingement [5], and rotator cuff enthesopathy [5]. While patients with a known diagnosis of AC have been shown to have increased focal uptake at the RI and IC [4, 5], the association in the inverse direction had not been studied. This association is of practical importance to imaging specialists who encounter this phenomenon on PET/CT and their patients.
Our study showed that focal uptake at these locations was not a rare occurrence, and has a prevalence of 0.53% (95% CI: 0.22–1.12%). We also showed that incidentally detected focal uptake at the RI or IC was indeed associated with a diagnosis of AC (Fisher’s exact, p = 0.001). In addition, the presence of focal uptake at these locations had a high specificity of 91% (95% CI: 84 – 95%) for the presence of AC, and conferred a moderate increase in the probability that the patient would have this diagnosis, with a positive likelihood ratio of 6.3 (95% CI: 2.8–14.6). Sensitivity for detection of AC was low (56% with 95% CI: 23% – 85%). This compares unfavorably with the high reported sensitivity of MRI and MRA in this regard, which is reported in the range of 59–98%, depending on technique, imaging features and cutoffs [2, 13–16]. We suspect that this low sensitivity is at least partially explained by the lower spatial resolution of PET compared to that of MRI [17].
The results from our retrospective study provide preliminary data on the significance of incidentally detected focal uptake at the RI and IC on 18F-FDG PET/CT. However, prospective studies will be needed to determine if these findings can allow confident diagnosis of AC.
Our findings also contribute to the sometimes contradictory evidence on the correlation between musculoskeletal uptake of 18F-FDG PET/CT and symptoms. On the one hand, there are reports suggesting an absence of association between symptoms and foci of increased uptake at the acetabular fossa [18], the knees and lumbar interspinous ligaments in patients with polymyalgia rheumatica [19, 20] atlantoaxial joints of patients with rheumatoid arthritis [12], and knees in patients with osteoarthritis [21]. However, the data is far from clear on this point, and other investigators have found significant differences in FDG avidity of symptomatic knees and shoulders when compared to that of asymptomatic joints [22, 23], and association of increased uptake at painful joints in patients with rheumatoid arthritis [24, 25]. Further study is needed to better define the role of 18F-FDG PET in detection of common musculoskeletal conditions.
The main limitation of our study is the reliability of clinical documentation for diagnosis of AC, which was used as the reference standard for this study. This limitation is inherent to the study design; however, we believe that our findings can serve as a starting point for future prospective studies on shoulder pain in oncological patients. Another limitation relates to absence of formal review of MRIs in group 2. We did not include a formal review of these MRIs. As a cancer center, our MRIs of the shoulder, especially those performed in older patients, are performed with a wide field of view in order to assess the scapula, shoulder, and proximal humerus for the presence of metastases. We did not feel confident in using this small number of suboptimal scans in diagnosing AC, in drawing conclusions on the utility of MRI in the setting of focal uptake at the RI or IC, nor in assessing the association between findings on PET and MRI.
Conclusion
Increased uptake at the RI, IC, or both on FDG PET/CT confers a moderate increase in the likelihood of AC.
Acknowledgments
The work was partially supported by the NIH/NCI under award number P30CA016672 and used the biostatistics research group.
Footnotes
Conflict of Interest
The authors declare that they have no conflict of interest
Contributor Information
Radhika Sridharan, Department of Diagnostic Imaging, Universiti Kebangsaan Malaysia Medical Centre, JalanYaacob Latif, 56000 Cheras, Kuala Lumpur, Malaysia., +60 3-7145-5555.
Mitchell Philip Engle, Department of Pain Medicine, The University of Texas M.D. Anderson Cancer Center, 1400 Pressler, Unit 0409, Houston, TX 77030.
Naveen Garg, Department of Diagnostic Imaging, The University of Texas M.D. Anderson Cancer Center, 1400 Pressler, Unit 1475, Houston, TX 77030.
Wei Wei, Department of Biostatistics, The University of Texas M.D. Anderson Cancer Center, 1400 Pressler, Unit 1411, Houston, TX 77030
Behrang Amini, Department of Diagnostic Imaging, The University of Texas M.D. Anderson Cancer Center, 1400 Pressler, Unit 1475, Houston, TX 77030.
References
- 1.Salem U, Zhang L, Jorgensen JL, Kumar R, Amini B. Adhesive Capsulitis Mimicking Metastasis on 18F-FDG-PET/CT. Clin Nucl Med. 2014 doi: 10.1097/RLU.0000000000000524. [DOI] [PubMed] [Google Scholar]
- 2.Gondim Teixeira PA, Balaj C, Chanson A, Lecocq S, Louis M, Blum A. Adhesive capsulitis of the shoulder: value of inferior glenohumeral ligament signal changes on T2-weighted fat-saturated images. AJR Am J Roentgenol. 2012;198(6):W589–596. doi: 10.2214/AJR.11.7453. [DOI] [PubMed] [Google Scholar]
- 3.Ahn KS, Kang CH, Oh YW, Jeong WK. Correlation between magnetic resonance imaging and clinical impairment in patients with adhesive capsulitis. Skeletal Radiol. 2012;41(10):1301–1308. doi: 10.1007/s00256-012-1391-8. [DOI] [PubMed] [Google Scholar]
- 4.Kim du H, Sung DH, Ga HY, Choi JY. Metabolic patterns of the shoulder joint on (18)F-fluorodeoxyglucose positron emission tomography/computed tomography in adhesive capsulitis. Ann Nucl Med. 2014;28(2):136–144. doi: 10.1007/s12149-013-0794-5. [DOI] [PubMed] [Google Scholar]
- 5.Sopov V, Bernstine H, Stern D, Yefremov N, Sosna J, Groshar D. Spectrum of focal benign musculoskeletal 18F-FDG uptake at PET/CT of the shoulder and pelvis. AJR Am J Roentgenol. 2009;192(4):1029–1035. doi: 10.2214/AJR.08.1686. [DOI] [PubMed] [Google Scholar]
- 6.Hsu JE, Anakwenze OA, Warrender WJ, Abboud JA. Current review of adhesive capsulitis. J Shoulder Elbow Surg. 2011;20(3):502–514. doi: 10.1016/j.jse.2010.08.023. [DOI] [PubMed] [Google Scholar]
- 7.Flannery O, Mullett H, Colville J. Adhesive shoulder capsulitis: does the timing of manipulation influence outcome? Acta Orthop Belg. 2007;73(1):21–25. [PubMed] [Google Scholar]
- 8.Earley D, Shannon M. The use of occupation-based treatment with a person who has shoulder adhesive capsulitis: a case report. Am J Occup Ther. 2006;60(4):397–403. doi: 10.5014/ajot.60.4.397. [DOI] [PubMed] [Google Scholar]
- 9.Griggs SM, Ahn A, Green A. Idiopathic adhesive capsulitis. A prospective functional outcome study of nonoperative treatment. J Bone Joint Surg Am. 2000;82-A(10):1398–1407. [PubMed] [Google Scholar]
- 10.Gaspar PD, Willis FB. Adhesive capsulitis and dynamic splinting: a controlled, cohort study. BMC Musculoskelet Disord. 2009;10:111. doi: 10.1186/1471-2474-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wandler E, Kramer EL, Sherman O, Babb J, Scarola J, Rafii M. Diffuse FDG shoulder uptake on PET is associated with clinical findings of osteoarthritis. AJR Am J Roentgenol. 2005;185(3):797–803. doi: 10.2214/ajr.185.3.01850797. [DOI] [PubMed] [Google Scholar]
- 12.Kubota K, Ito K, Morooka M, Mitsumoto T, Kurihara K, Yamashita H, et al. Whole-body FDG-PET/CT on rheumatoid arthritis of large joints. Ann Nucl Med. 2009;23(9):783–791. doi: 10.1007/s12149-009-0305-x. [DOI] [PubMed] [Google Scholar]
- 13.Ahn KS, Kang CH, Kim Y, Jeong WK. Diagnosis of adhesive capsulitis: comparison of contrast-enhanced MRI with noncontrast-enhanced MRI. Clin Imaging. 2015;39(6):1061–1067. doi: 10.1016/j.clinimag.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Jung JY, Jee WH, Chun HJ, Kim YS, Chung YG, Kim JM. Adhesive capsulitis of the shoulder: evaluation with MR arthrography. Eur Radiol. 2006;16(4):791–796. doi: 10.1007/s00330-005-0020-5. [DOI] [PubMed] [Google Scholar]
- 15.Emig EW, Schweitzer ME, Karasick D, Lubowitz J. Adhesive capsulitis of the shoulder: MR diagnosis. AJR Am J Roentgenol. 1995;164(6):1457–1459. doi: 10.2214/ajr.164.6.7754892. [DOI] [PubMed] [Google Scholar]
- 16.Mengiardi B, Pfirrmann CW, Gerber C, Hodler J, Zanetti M. Frozen shoulder: MR arthrographic findings. Radiology. 2004;233(2):486–492. doi: 10.1148/radiol.2332031219. [DOI] [PubMed] [Google Scholar]
- 17.Saha GB. Performance Characteristics of PET Scanners. In: Saha GB, editor. Basics of PET Imaging: Physics, Chemistry, and Regulations. New York, NY: Springer-Verlag; 2010. [Google Scholar]
- 18.Kubicki SL, Richardson ML, Martin T, Rohren E, Wei W, Amini B. The acetabular fossa hot spot on 18F-FDG PET/CT: epidemiology, natural history, and proposed etiology. Skeletal Radiol. 2015;44(1):107–114. doi: 10.1007/s00256-014-2011-6. [DOI] [PubMed] [Google Scholar]
- 19.Camellino D, Paparo F, Morbelli S, Cutolo M, Sambuceti G, Cimmino MA. Interspinous bursitis is common in polymyalgia rheumatica, but is not associated with spinal pain. Arthritis Res Ther. 2014;16(6):492. doi: 10.1186/s13075-014-0492-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cimmino MA, Camellino D, Paparo F, Morbelli S, Massollo M, Cutolo M, et al. High frequency of capsular knee involvement in polymyalgia rheumatica/giant cell arteritis patients studied by positron emission tomography. Rheumatology (Oxford) 2013;52(10):1865–1872. doi: 10.1093/rheumatology/ket229. [DOI] [PubMed] [Google Scholar]
- 21.Nakamura H, Masuko K, Yudoh K, Kato T, Nishioka K, Sugihara T, et al. Positron emission tomography with 18F-FDG in osteoarthritic knee. Osteoarthritis Cartilage. 2007;15(6):673–681. doi: 10.1016/j.joca.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 22.Kamasaki T, Hayashida N, Miyamoto I, Usui T, Chiba K, Kudo T, et al. PET/CT shows subjective pain in shoulder joints to be associated with uptake of (18)F-FDG. Nucl Med Commun. 2014;35(1):44–50. doi: 10.1097/MNM.0000000000000029. [DOI] [PubMed] [Google Scholar]
- 23.Hong YH, Kong EJ. (18F)Fluoro-deoxy-D-glucose uptake of knee joints in the aspect of age-related osteoarthritis: a case-control study. BMC Musculoskelet Disord. 2013;14:141. doi: 10.1186/1471-2474-14-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vijayant V, Sarma M, Aurangabadkar H, Bichile L, Basu S. Potential of (18)F-FDG-PET as a valuable adjunct to clinical and response assessment in rheumatoid arthritis and seronegative spondyloarthropathies. World J Radiol. 2012;4(12):462–468. doi: 10.4329/wjr.v4.i12.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elzinga EH, van der Laken CJ, Comans EF, Boellaard R, Hoekstra OS, Dijkmans BA, et al. 18F-FDG PET as a tool to predict the clinical outcome of infliximab treatment of rheumatoid arthritis: an explorative study. J Nucl Med. 2011;52(1):77–80. doi: 10.2967/jnumed.110.076711. [DOI] [PubMed] [Google Scholar]