Abstract
Background. Pregnancy occurs among 1–7% of women on chronic dialysis. Experience regarding pregnancy and dialysis originates from anecdotal reports, case series and surveys. This survey updates the US nephrologists’ experience with pregnancy on hemodialysis (HD) over the past 5 years. We evaluated maternal and fetal outcomes, certain practice patterns such as dialysis regimens utilized and nephrologist knowledge and comfort level when caring for a pregnant patient on HD.
Methods. An anonymous Internet-based 23-question survey was e-mailed to end-stage renal disease Networks of America program directors for forwarding to practicing nephrologists.
Results. A total of 196 nephrologists responded to the survey, reporting >187 pregnancies. Of the respondents, 45% had cared for pregnant females on HD and 78% of pregnancies resulted in live births. In 44% of the pregnancies a diagnosis of preeclampsia was made. There were no maternal deaths. Nephrologists most commonly prescribe 4–4.5 h of HD 6 days/week for pregnant women on dialysis. Women dialyzed cumulatively for >20 h/week were 2.2 times more likely to develop preeclampsia than those who received ≤20 h of HD per week.
Conclusion. Providing intensive HD is a common treatment approach when dialyzing pregnant women. Maternal and fetal outcomes can be improved. There is a trend toward better live birthrates with more intense HD. Whether more cumulative hours of dialysis per week increases the risk of preeclampsia needs to be further investigated.
Keywords: hemodialysis, national survey, nephrology, outcomes, pregnancy
Introduction
Experience regarding pregnancy and dialysis comes from anecdotal reports, case series and surveys. The first cases of pregnant woman on hemodialysis (HD) ever published were by Herwig et al. [1] in 1965 and Orme et al. [2] in 1968. The first international case of a pregnant woman on HD was reported in 1971, by an Italian group [3]. This was followed by several European and US case reports describing successful pregnancies in women on dialysis [4–6].
In 1980, the European Dialysis and Transplant Association (EDTA) reported the first case series of successful pregnancies. They reported 16 successful pregnancies in women on HD. These women had an average dialysis time of 18 h/week and the average frequency of dialysis was 3 days/week [7]. In 1985, Roxe and Parker [8] published survey results based on 45 pregnancies in the USA. In 1986, Hou [9] surveyed American dialysis centers and reported 16 pregnancies, and in 1988, Redrow et al. [10] conducted a US survey and reported 14 pregnancies on peritoneal dialysis and HD.
In 1992, the Saudi Arabian experience of 27 pregnancies was reported [11]. The authors found that the pregnancies that continued for >28 weeks were associated with longer dialysis hours, averaging 12.0 ± 2.6 h/week [11]. In 1994, survey results based on 60 pregnancies were reported [12]. In 1998, Bagon et al. [13] published their experience with pregnancy and dialysis based on 15 cases from a national survey and 5 cases from a single center. They found that more successful pregnancies occurred in those who conceived before starting dialysis and that the dose of dialysis had an impact on birthweight. In 1998, experience in the USA was updated based on 344 pregnancies reported through a survey between 1992 and 1995 [14]. The authors found that the outcome of pregnancy was better in women who conceived before starting dialysis than in women who conceived after starting dialysis. In addition, they found a trend toward better survival and less prematurity in women who were dialyzed ≥20 h/week. The number of days on dialysis per week did not make a difference in infant survival or mean gestational age [14].
In 2010, the Brazilian experience with 52 pregnancies was published [15]. In 2013, the Australian/New Zealand Registry reported 49 pregnancies [16]. Finally, in 2014, the results comparing 22 pregnancies from the Toronto Registry from 2000 to 2013 and 70 pregnancies from a 1990–2011 cohort of women were reported [17]. This study suggested that intensive HD (>36 h/week) had positive effects with respect to live births, gestational age and birthweight [17].
Taken together, the number of cases reported during each era is quite small. This study was conducted to update the US experience over the past 5 years, to evaluate maternal and fetal outcomes associated with dialyzing a pregnant woman, to examine certain practice patterns such as dialysis regimens utilized and to evaluate nephrologists' knowledge and comfort level when caring for a pregnant patient on HD.
Materials and Methods
We designed an anonymous national online survey using SurveyMonkey consisting of 23 questions. The survey was deemed exempt by the institutional review board of the Northwell Health System. A link to the survey was e-mailed to end-stage renal disease (ESRD) Networks of America program directors with instructions to forward to their practicing nephrologists. The total number of practicing nephrologists who received the survey is not known. Only practicing adult US nephrologists were eligible to participate, and this was reflected in the cover letter for the survey. The survey was voluntary. Although some nephrologists may have taken care of more than one pregnant woman on dialysis in the past 5 years, data regarding only the most recent pregnancy was collected. The initial correspondence was sent in May 2014. Survey reminders were subsequently sent in March 2015 and October 2015. Results were tabulated by SurveyMonkey. Further statistical analysis was completed using the Microsoft Excel (version 2007) data analysis tool pack. Goodness of fit test and analysis of variance were used to complete the statistical analysis.
The questions were designed based on a literature review as well as the experience of the authors (Table 1). The first two questions were to assess pregnancy encounters among practicing nephrologists. The third question inquired about the timing of conception. The next four questions were to assess outcomes such as live births, preeclampsia and maternal deaths. Questions 8 and 9 inquired about practice patterns, questions 10–14 inquired about dialysis regimens utilized and question 15 inquired about the comfort level of the practicing nephrologist. The remainder of the questions were demographic in nature.
Table 1.
Survey questions
| 1. Have any of your chronic HD patients become pregnant in the past 5 years? |
| 2. If yes, how many? |
| 3. How many years of dialysis did each of your patients receive prior to pregnancy? |
| 4. The number of pregnancies in my dialysis center that have resulted in live births is? |
| 5. Pick the best choice for this statement: in my facility, the number of viable pregnancies is: increasing, decreasing, staying the same or there have been no pregnant dialysis patients in my unit. |
| 6. Were any of the pregnancies associated with the development of preeclampsia? |
| 7. Have you had any maternal deaths? |
| 8. Do you or a member of your staff counsel your female dialysis patients about contraception? |
| 9. Would you or a member of your staff ever recommend termination of pregnancy in a dialysis patient? |
| 10. How many hours per HD session do you prescribe for the pregnant patient? |
| 11. How many days per week do you provide dialysis for the pregnant patient? |
| 12. Place a check next to any of the following changes you make in your dialysis orders for a pregnant patient: blood flow/dialyzer/access/medications/others |
| 13. What do you believe the target predialysis BUN should be for a pregnant dialysis patient? |
| 14. Do you have access to fetal monitoring during dialysis? |
| 15. How comfortable do you feel about caring for a pregnant dialysis patient? |
| 16. What is your gender? |
| 17. How many years have you been in practice? |
| 18. Where did you complete your medical school training? |
| 19. What best describes your age group? |
| 20. What best describes your dialysis unit geographic region in the USA? |
| 21. What best describes you? |
| 22. Are you a medical director of a dialysis unit? |
| 23. Please add any additional comments regarding pregnancy and dialysis |
Results
To date, 196 nephrologists have responded to the survey. The number of years in practice and the age groups of the responding nephrologists are equally distributed. Of the 196 nephrologists who responded, 88 (45%) have cared for pregnant women on HD. Because some nephrologists took care of more than one pregnant woman on dialysis, they cumulatively report caring for >187 chronic HD patients over the past 5 years.
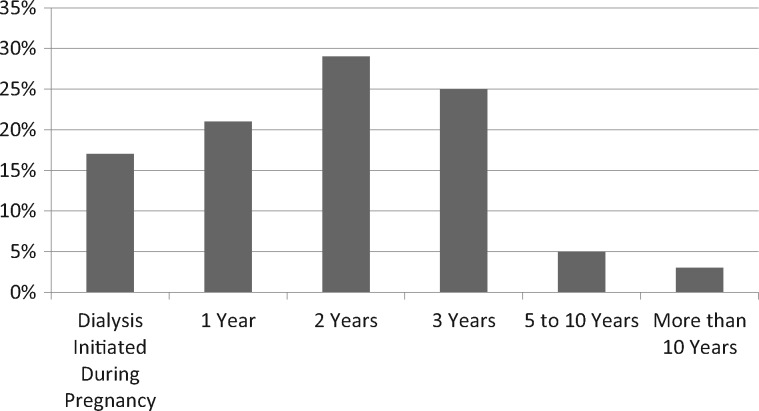
Regarding the timing of conception, of 106 pregnancies, 18 women were started on HD during their pregnancy (17%), 80 pregnancies occurred within the first 5 years of being on dialysis (75%), 5 occurred after being on dialysis for 5–10 years (5%), 3 occurred after being on dialysis for >10 years (3%) (Figure 1). Of 86 pregnancies reported, 67 resulted in live births (78%). Further analysis showed there was a statistically significant trend toward more live births in those women who were dialyzed for ≥4 days/week compared with those who were dialyzed <4 days/week (P < 0.005). Although not statistically significant, there was a trend toward more live births for those being dialyzed >20 h/week compared with those who were dialyzed <20 h/week. In addition, there was a trend toward more live births in those who were dialyzed ≥4 h/session.
Fig. 1.
How many years of dialysis did each of your patients receive prior to pregnancy?
Of 86 pregnancies, 38 were complicated by a diagnosis of preeclampsia, resulting in a 44% preeclampsia rate. We found that women were less likely to develop preeclampsia if they were dialyzed ≤20 h/week (P < 0.05). Further analysis showed that women who were receiving >20 h/week of HD were 2.2 times more likely to develop preeclampsia than those who received ≤20 h of HD per week. The number of days on dialysis per week or the number of hours per session had no significant impact on preeclampsia. There were no maternal deaths reported in this survey.
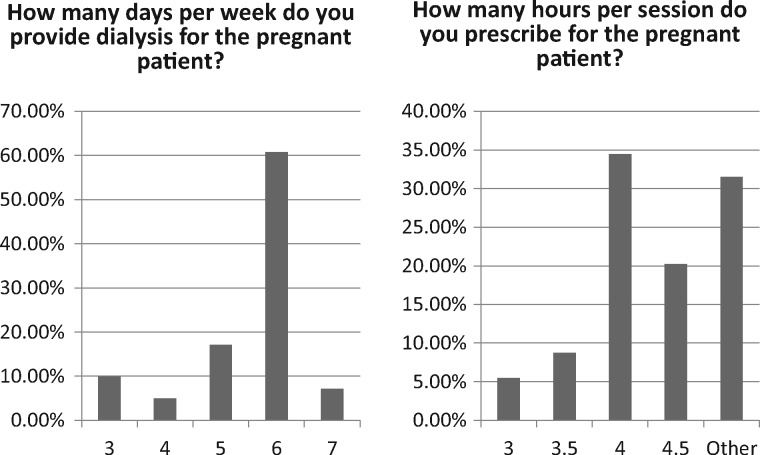
Most nephrologists prescribe 4–4.5 h of HD per session (average 4.2 ± 0.9). Of respondents, 61% provide dialysis 6 days/week (average 5.5 ± 1.1) (Figure 2). Regarding the dialysis prescription, 80% made changes in medications. Twenty-one percent aimed for a target predialysis blood urea nitrogen (BUN) of <20 mg/dL, while 66% targeted a BUN of <50 mg/dL. Seventy-five percent of respondents do not have access to fetal monitoring during dialysis for their pregnant patient.
Fig. 2.
Dialysis prescription provided to pregnant HD patients.
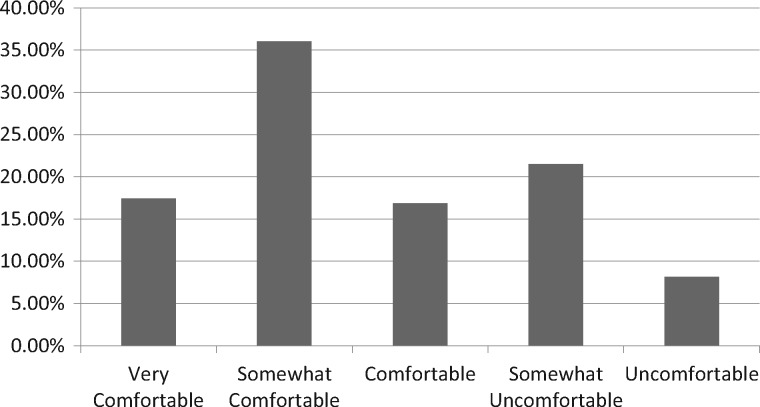
Of the respondents, 46% stated they or a member of their staff counsel their female dialysis patients about contraception; 37% stated they would recommend termination of pregnancy in a dialysis patient. Thirty percent stated they are somewhat uncomfortable to uncomfortable caring for a pregnant woman on HD, while 36% stated that they are somewhat comfortable. This leaves only 34% stating they are comfortable and very comfortable (Figure 3).
Fig. 3.
Comfort level of nephrologists when caring for a pregnant dialysis patient.
Discussion
This survey updates the US experience on pregnancy in women on HD. In the past, the chance of a dialysis patient conceiving was low. In the 1980s, the incidence of conception on dialysis was ∼0.9% [18]. From 1992 to 2003, the incidence ranged from 1 to 7% [18]. Data from our survey show that US nephrologists are encountering pregnant women on HD more often, with nearly half of responding nephrologists caring for a pregnant woman on HD.
In women on dialysis, infertility is thought to be common. Reasons for infertility are multifactorial. ESRD alters a woman’s hormonal milieu. Females on dialysis may lack the estradiol-stimulated luteinizing hormone surge. In addition, prolactin levels may be increased, causing changes that may facilitate anovulatory cycles [18–20]. Additional factors such as decreased libido, body image factors, depression, effect of uremic toxins and pharmacologic side effects from antihypertensive agents or cyclophosphamide may play a role in infertility. Our survey suggests that infertility and anovulation may be less commonly encountered in the present-day dialysis female of childbearing age than in the past, a trend that needs to be further examined. Reasons for this could include improved dialysis techniques and dialysis prescription, as well as better anemia, blood pressure and volume management [20].
In 1994, Hou [21] showed that although the majority of pregnancies occurred within 1 year of being on dialysis, pregnancy was possible even after 10 years of being on dialysis, accounting for 21% of the reported pregnancies. In our survey, the majority of patients conceived within the first 5 years of being on HD (75%), however, there were several pregnancies reported after being on dialysis for >5 or even 10 years. For this reason, it is important to counsel all women of childbearing age on dialysis on contraception and pregnancy risks. In fact, in 1994 Hou [21] stressed the importance of receiving contraceptive counseling in this group of women. However, our survey shows that only 46% of nephrologists or a member of their staff actually counseled their female dialysis patients about contraception.
Pregnancy is more commonly encountered in the HD population than the peritoneal dialysis (PD) population. The exact reasons are still unclear. Two potential explanations include the use of hypertonic dialysate in the peritoneum, which may interfere with transport of the ovum to the fallopian tube, or even prior episodes of peritonitis that may result in the formation of adhesions and subsequent failure of implantation [12, 21]. Furthermore, increasing abdominal girth during pregnancy may factor in a patient switching from PD to HD [21, 22]. The US registry reported 2.4% of pregnancies in HD patients and 1.1% in PD patients between 1992 and 1995 [14]. Although our survey did not specifically inquire about PD and pregnancy, there was mention of one woman conceiving while on PD. She was switched to HD due to abdominal discomfort.
The dialysis prescription used to dialyze a pregnant woman now supports more intense dialysis. Based on the 1998 US survey, there was a trend toward better infant survival and less prematurity in women who received ≥20 h of dialysis per week [14]. More recently, Hladunewich et al. [17] noted better live birthrates in those dialyzed >36 h/week as opposed to those dialyzed for ≤20 h/week. Our survey shows that US nephrologists are now providing intensive HD for their pregnant dialysis patients. Between 1990 and 2011 the average time on dialysis was 17 ± 5 h/week [17]. Based on our survey results, US nephrologists are now prescribing on average 4–4.5 h for 6 days/week or an average of 23±7 h/week.
Regarding the dialysis prescription, the number of days per week on dialysis, whether 3, 4, 5 or 6 does not impact infant survival or mean gestational age [14]. Instead, it is the cumulative total hours per week of dialysis that may make the difference. Several studies have now shown that there is a trend toward better survival and decreased prematurity with increasing the total hours per week of dialysis [14, 17]. Our survey supported a trend toward more live births with more cumulative hours on dialysis (≥20 h). However, we also found that dialyzing more often (≥4 days/week) or for more time (≥4 h/session) may improve infant survival. In all prior studies that have shown a trend toward improved live birthrates with more hours on dialysis, as well as this survey, it is uncertain if there were other variables that confounded this finding, such as other maternal comorbidities, maternal residual renal function, other variables of the dialysis prescription or changes in the dialysis prescription made during the course of the pregnancy.
More dialysis time is associated with better volume and electrolyte control. The frequency of preterm delivery and intrauterine growth restriction tends to correlate with BUN levels [23]. There is an inverse association between BUN level and birthweight and adverse fetal outcome, with more favorable outcomes when the serum urea level is <75 mg/dL [15]. Polyhydramnios is common in the dialysis population and is a risk for preterm labor. There are suggestions that high placental BUN may result in excessive amniotic fluid accumulation. Intensifying the dialysis prescription helps in lowering the predialysis BUN level, thus decreasing the risk of polyhydramnios and preterm labor [18, 24, 25]. The literature suggests decreasing BUN to 44–50 mg/dL (16–18 mmol/L) [26, 27]. Our survey shows that most US nephrologists target a BUN of <50 mg/dL (66%) and 21% aim for a target predialysis BUN of <20 mg/dL.
Globally, the live birthrate seems to be increasing in pregnant dialysis women. In the 1970s, the EDTA reported a live birthrate of 23% [7]. In 1992 and 1994, Saudi Arabia and the USA reported live birthrates of 30 and 27%, respectively [11, 12]. Between 1992 and 1995, 42% of pregnancies led to a surviving infant in the USA [14]. In the late 1990s, Belgium reported a live birthrate of 50% and Japan reported a live birthrate of 49% [13]. There was a 61.4% live birthrate reported from 1990 to 2011 in the USA and 86.4% from 2000 to 2013 in Canada [17]. Our survey showed a 78% live birthrate from 2010 to 2015. The increase in live births could be due to the change in practice patterns toward more intensive dialysis prescriptions.
Maternal prognosis on dialysis is quite good. There was no maternal mortality reported in our survey. In 1998 there were reports of two maternal deaths [14]. Again perhaps, dialysis prescription changes and more intense monitoring are contributing to the improved prognosis.
Preeclampsia remains a major complication occurring in nearly half of the pregnancies in our survey. Since the diagnosis of preeclampsia involves blood pressure and urine protein excretion measurements, the diagnosis may be a difficult one to make in a woman on dialysis who may already have fluctuating blood pressures. Because the diagnosis of preeclampsia is usually made conjunctively by the obstetrician and nephrologist, we assume that standard criteria were used.
Preeclampsia does affect the outcome of pregnancy and can result in intrauterine growth restriction and even fetal death [15]. The pathophysiology of preeclampsia is complex. Inhibition of maternal nitric oxide synthesis adversely effects implantation and increasing uterine arterial resistance is also thought to play a role. Furthermore, placental underperfusion, hypoxia and even ischemia can lead to release of circulating antiangiogenic factors such as soluble fms-like tyrosine kinase (sFlt-1), soluble endoglin and other substances that can cause widespread maternal systemic endothelial dysfunction and increased vascular permeability [28]. We found that women were less likely to develop preeclampsia if dialyzed ≤20 h/week (P < 0.05). It may be possible that there is an association between total cumulative hours on HD and preeclampsia risk due to increased vasoconstriction associated with tighter volume control. However, we recognize that this needs to be studied further, as we relied on the diagnosis of preeclampsia made by the responding physicians and we recognize that there may be other patient variables factored into this, as mentioned in the ‘Limitations’ section.
Maternal and fetal monitoring during a dialysis session can be important for outcomes. Intradialytic fetal monitoring assesses the fetal heart rate as well as monitors for uterine contractions to ensure that the fetus or placenta are not being affected by the altered maternal hemodynamics during dialysis. In our survey, we found that most US nephrologists do not have access to obstetric monitoring during HD (75%).
Finally, since pregnancy on dialysis is more frequently encountered, pregnancy care should be part of the health maintenance plan of women of childbearing age on dialysis. Nephrologists rarely discuss conception, termination and types of contraception with their female dialysis patients and greater attention to these issues is needed.
Limitations
We acknowledge that there may be limitations to our survey. Our sample size was small. Nephrologists who have cared for pregnant women on dialysis may have responded more frequently than those without such experiences, thus contributing to the overestimation of the frequency of encountering a pregnant woman on dialysis. In addition, there is the potential to report only the successful outcomes. Since preeclampsia has certain diagnostic criteria, it is important to stress that the diagnosis of preeclampsia in this survey was based on an already made diagnosis in the responding nephrologist’s patient, hence criteria may not have been standardized. We did not include women on PD in this survey. We did not differentiate between women who were dialyzed due to the progression of chronic kidney disease or those who were dialyzed in the setting of acute kidney injury. Most of the nephrologists surveyed were from academic institutions and were geographically from the northeast region. While a physician survey may not be the ideal method for ascertainment of patient outcomes, these data do represent the largest group of pregnant patients reported in more than a decade and provide an update on the US experience. For these reasons, we believe that the information collected in this survey may be very insightful to the nephrology and obstetric communities, providing a good sense of real-world experience, and may help stimulate further epidemiologic research.
Conclusion
Providing intensive HD is a common treatment approach when dialyzing a pregnant woman. Nephrologists are now providing 4–4.5 h of HD 6 days a week. Maternal and fetal outcomes can be improved. There is a trend toward better live birthrates with more intense HD. Whether more cumulative hours of dialysis per week is associated with a risk of preeclampsia needs to be further investigated. The nephrologists' comfort level and knowledge can be improved.
Acknowledgements
We acknowledge all the nephrologists throughout the USA who took part in the survey. Results of this study were presented at the National Kidney Foundation Spring Clinical Meeting in April 2016.
Conflict of interest statement
None declared.
References
- 1. Herwig KR, Merill JP, Jackson RL. et al. Chronic renal disease and pregnancy. Am J Obstet Gyn 1965; 92: 1117–1121 [DOI] [PubMed] [Google Scholar]
- 2. Orme BM, Ueland K, Simpson DP. et al. The effect of hemodialysis on fetal survival and renal function in pregnancy. Trans Am Soc Artif Intern Organs 1968; 14: 402–404 [PubMed] [Google Scholar]
- 3. Confortini P, Galanti G, Ancona G. et al. Full term pregnancy and successful delivery in a patient on chronic hemodialysis. Proc Eur Dial Transplant Assoc 1971; 8: 74–80 [Google Scholar]
- 4. Unzelman RF, Alderfer GR, Chojnacki RE.. Pregnancy and chronic hemodialysis. Trans Am Soc Artif Intern Organs 1973; 19: 144–149 [DOI] [PubMed] [Google Scholar]
- 5. Rigenbach M, Renger B, Beavais P. et al. Grossesse et accouchement d’un enfant vivant chez une patiente traitee par hemodialyse iterative. J Urol Nephrol 1978; 84: 360–366 [PubMed] [Google Scholar]
- 6. Ackrill P, Goodwin FJ, Marsh FP. et al. Successful pregnancy in patient on regular dialysis. Br Med J 1975; 2:172–174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Successful pregnancies in women treated by dialysis and kidney transplantation. Report from the Registration Committee of the European Dialysis and Transplant Association. Br J Obstet Gynaecol 1980; 87: 839–845 [DOI] [PubMed] [Google Scholar]
- 8. Roxe DM, Parker J. Report of a survey of reproductive function in female hemodialysis patients. Proceedings of the American Nephrology Nursing Association, National Meeting, New Orleans, 1985.
- 9. Hou S. Pregnancy in women requiring dialysis for renal failure. Am J Kidney Dis 1987; 9: 368–373 [DOI] [PubMed] [Google Scholar]
- 10. Redrow M, Cherem L, Elliott J. et al. Dialysis in the management of pregnant patients with renal insufficiency. Medicine 1988; 67: 199–208 [DOI] [PubMed] [Google Scholar]
- 11. Souqiyyeh MZ, Huraib SO, Saleh AGM. et al. Pregnancy in chronic hemodialysis patients in the Kingdom of Saudi Arabia. Am J Kidney Dis 1992; 19: 235–238 [DOI] [PubMed] [Google Scholar]
- 12. Hou S. Frequency and outcome of pregnancy in women on dialysis. Am J Kidney Dis 1994; 23: 60–63 [DOI] [PubMed] [Google Scholar]
- 13. Bagon JA, Vernaeve H, Muylder XD. et al. Pregnancy and dialysis. Am J Kidney Dis 1998; 31: 756–765 [DOI] [PubMed] [Google Scholar]
- 14. Okundaye I, Abrinko P, Hou S.. Registry of pregnancy in dialysis patients. Am J Kidney Dis 1998; 31: 766–773 [DOI] [PubMed] [Google Scholar]
- 15. Luders C, Castro MCM, Titan SM. et al. Obstetric outcome in pregnant women on long term dialysis: a case series. Am J Kidney Dis 2010; 56: 77–85 [DOI] [PubMed] [Google Scholar]
- 16. Shahir AK, Briggs N, Katsoulis J. et al. An observational outcome study from 1966–2008, examining pregnancy and neonatal outcomes from dialyzed women using data from ANZDATA Registry. Nephrology 2013; 18: 276–284 [DOI] [PubMed] [Google Scholar]
- 17. Hladunewich MA, Hou S, Odutayo A. et al. Intensive hemodialysis associates with improved outcomes: a Canadian and United States cohort comparison. J Am Soc Nephrol 2014; 25: 1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Holley JL, Reddy SS.. Pregnancy in dialysis patients: a review of outcomes, complications, and management. Semin Dial 2003; 16: 384–388 [DOI] [PubMed] [Google Scholar]
- 19. Schmidt RJ, Holley JL.. Fertility and contraception in end-stage renal disease. Adv Ren Replace Ther 1998; 5: 38–44 [DOI] [PubMed] [Google Scholar]
- 20. Holley JL, Schmidt RJ, Bender FH. et al. Gynecologic and reproductive issues in women on dialysis. Am J Kidney Dis 1997; 29: 685–690 [DOI] [PubMed] [Google Scholar]
- 21. Hou SH. Pregnancy in women on hemodialysis and peritoneal dialysis. Baillieres Clin Obstet Gynecol 1994; 8: 481–500 [DOI] [PubMed] [Google Scholar]
- 22. Chang H, Miller MA, Bruns FJ.. Tidal peritoneal dialysis during pregnancy improves clearance and abdominal symptoms. Perit Dial Int 2002; 22: 272–274 [PubMed] [Google Scholar]
- 23. Jones DC, Hayslett JP. Outcome of pregnancy in women with moderate or severe renal insufficiency. N Engl J Med 1996; 335: 226–232 [DOI] [PubMed] [Google Scholar]
- 24. Nageotte MP, Grundy HO.. Pregnancy outcome in women requiring chronic hemodialysis. Obstet Gynecol 1998; 72: 456–459 [PubMed] [Google Scholar]
- 25. Giatras I, Levy DP, Malone FD. et al. Pregnancy during dialysis: case report and management guidelines. Nephrol Dial Transplant 1988; 13: 3266–3272 [DOI] [PubMed] [Google Scholar]
- 26. Groothoff J. Pregnancy during dialysis: still a challenge to get there, but worth the effort. Nephrol Dial Transplant 2015; 30: 1053–1055 [DOI] [PubMed] [Google Scholar]
- 27. Manisco G, Poti M, Maggiulli G. et al. Pregnancy in end stage renal disease patients on dialysis: how to achieve a successful delivery. Clin Kidney J 2015; 8: 293–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Maynard SE, Karumanchi SA.. Angiogenic factors and preeclampsia. Semin Nephrol 2011; 31: 33–46 [DOI] [PMC free article] [PubMed] [Google Scholar]