Abstract
Trabeculectomy surgery is the current standard of care in glaucoma for achieving a low target intraocular pressure if medical therapy is not adequate. Augmentation of trabeculectomy with antimetabolites brought a revolutionary change in the long-term success rates of trabeculectomy, but along with it came a plethora of complications. There still is a big window for therapeutic innovations on this subject. The foremost target for these innovations is to modulate the wound healing response after glaucoma drainage surgery. Achieving the desired balance between long-term success of filtering blebs versus early failure due to scarring of blebs and hypotony due to dysfunctional filtering blebs poses a unique challenge to the ophthalmologists. Alternatives to trabeculectomy such as glaucoma drainage devices and minimally invasive glaucoma surgeries cannot solve the problem of glaucoma blindness in our country, mainly due to their unpredictable results and unfavorable cost-benefit ratio. In this article, we present a summary of our innovations in glaucoma surgery to advance patient care by making it more effective, safer, and economical.
Key words: Bleb needling, bleb revision, cyclodialysis, innovations in trabeculectomy, mitomycin-C, Ologen
Trabeculectomy, the traditional guarded filtering surgery first introduced by Cairns in 1968[1] still remains the most commonly performed incisional glaucoma surgery when target intraocular pressure (IOP) is not achieved with ocular hypotensive medical therapy. It involves creating an ostium between anterior chamber (AC) and subconjunctival space, thus bypassing the diseased natural outflow pathway. The success of trabeculectomy depends on a delicate balance between the flow of aqueous through the functioning fistula and wound healing mechanisms causing scarring and counteracting this flow at the level of conjunctiva-Tenon-episcleral interface, the scleral flap or the internal ostium. The reported long-term success rates of primary trabeculectomy ranges from 57% to 90%, and it is currently the most effective long-term surgical method for lowering the IOP.[2]
The Need for Innovation
Although the use of antimetabolites such as mitomycin-C (MMC) and 5-fluorouracil (5-FU) have increased the success rates of trabeculectomy, their use has been associated with an increased risk of bleb-related complications such as bleb-related infections[3] and hypotony[4] maculopathy with irreversible visual loss.[5] In addition, the success rate remains poor in various secondary glaucomas such as neovascular, uveitic and aphakic glaucomas and also in eyes which have undergone previous vitreoretinal surgery. Innovations are required to modify the fibroblastic response following surgical trauma, achieve a lower IOP and minimize complications while maintaining long-term outflow. This can be achieved by techniques to augment aqueous outflow through both subconjunctival and suprachoroidal routes, use of biodegradable spacers to maintain the subconjunctival space and creation of a controlled cyclodialysis cleft in eyes with a high risk of conjunctival scarring. In eyes where scarring sets in and the bleb begins to fail, early recognition and intervention with new techniques for bleb remodulation are essential. In eyes which end up with a late bleb leak and hypotony specific surgical interventions are warranted to restore the integrity of the conjunctival epithelial barrier. In addition, in the recent years, many new microsurgical devices have been introduced as alternatives to trabeculectomy which are very expensive and largely out of reach of the majority of the population in our country due to economic restraints. In a developing country like ours, medical therapy of glaucoma poses a huge socioeconomic burden on the patients amounting to nearly 42% of their monthly income[6] and many patients have a poor compliance to life-long medical therapy. Hence, the goal is to achieve target IOP with a glaucoma surgery at an affordable cost with minimal complications, so that the patient can have a good quality of life. This brings in the need for us to develop low cost, efficacious, and safe surgical innovations which can benefit the glaucoma community at large. The following review outlines the surgical innovations developed at the glaucoma facility of Dr. Rajendra Prasad Centre for Ophthalmic Sciences, New Delhi, to facilitate glaucoma management, which have been published in peer-reviewed indexed journals [Table 1].
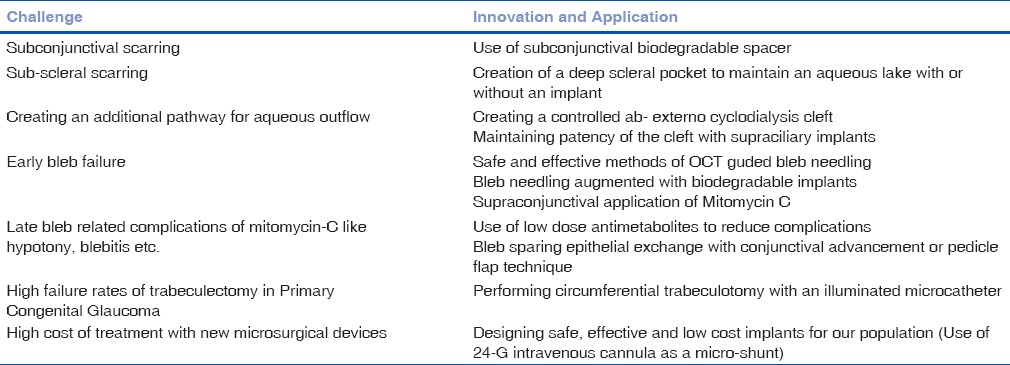
Table 1.
Challenges in glaucoma surgery
Lowering the Dose of Mitomycin-C
Since the introduction of MMC, the success rates of trabeculectomy have increased, however complications such as hypotony, hypotony maculopathy, suprachoroidal hemorrhage, choroidal effusions, bleb leak, blebitis, bleb encapsulation, failure, and endophthalmitis have exponentially increased.[3,4,5] Titrating the dose and duration of MMC is of prime importance to regulate the wound healing response after trabeculectomy.
Sihota et al.[7] reported a randomized controlled, noninferior, clinical trial consisting of fifty consecutive patients with primary glaucoma, uncontrolled on maximal hypotensive therapy. A 1-min subconjunctival application of low dose 0.1 mg/ml MMC was shown to be noninferior to 0.2 mg/ml and is a safer alternative, as thinning of the bleb is significantly less frequent in the long-term. Currently, we are using 0.01% MMC for all adult patients undergoing trabeculectomies for primary glaucoma. The dose is increased for eyes with a failed filter undergoing resurgery and all forms of secondary glaucoma or previous eye surgery with conjunctival involvement. A wide area of MMC application is a must, to avoid localized cystic blebs.
Trabeculectomy “EXTRA”
The success of trabeculectomy to maintain a low IOP declines over time, with about 10% eyes failing each year due to scarring. The outcomes are much worse for refractory glaucomas such as uveitic, neovascular, and traumatic and for subsequent surgeries after a failed trabeculectomy.[6] Other conditions associated with poor trabeculectomy outcomes include eyes with previous retinal buckling surgery, pars plana vitrectomy, penetrating keratoplasty and developmental glaucomas such as iridocorneal endothelial (ICE) syndrome innovation is required to prolong the functional period of the filtration by augmenting the trabeculectomy. New techniques have been developed by the authors, to add an “EXTRA” efficacy by modifying the traditional trabeculectomy techniques.
Trabeculectomy Augmented with Biodegradable Implants
Bioengineered, biodegradable, porous collagen-glycosaminoglycan matrix implant acts as a spacer in the subconjunctival and/or subscleral space. It also leads to random and relatively loose reorganization of regenerating myofibroblasts, fibroblasts and the extracellular collagen matrix laid by them, resulting in reduced scar formation.
Fornix-based trabeculectomy with subconjunctival Ologen implant (Ologen, Aeon Astron Europe, the Netherlands) and low-dose MMC (0.1 mg/ml × 1 min) was evaluated by Dada et al.[8] in 33 eyes with primary open angle glaucoma. Mean preoperative IOP 34.06 ± 6.56 mmHg decreased to 12.54 ± 1.67 mmHg at 12 months. The implant was visible for 6–9 months. Wound leak with shallow AC, implant extrusion requiring resuturing and Tenon's cyst were reported complications.
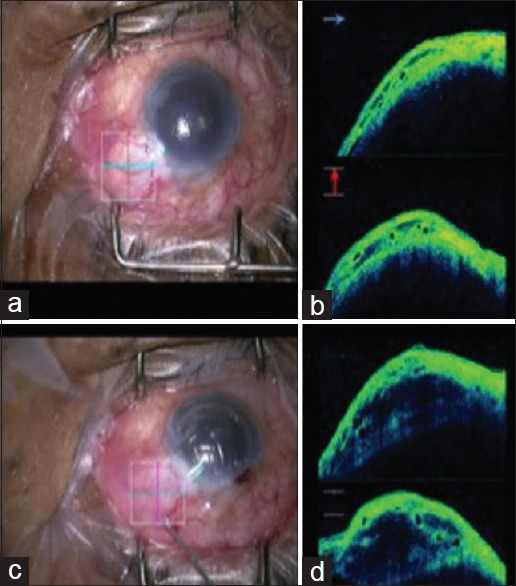
Angmo et al.[9] further evaluated the efficacy and safety of trabeculectomy with combined subconjunctival and subscleral Ologen implant in 27 eyes with advanced glaucomatous optic neuropathy with mean preoperative IOP of 38.3 ± 6.6 mmHg. The short-term results were encouraging with postoperative IOP of 12.5 ± 1.6 mmHg at 24 months. The use of an additional implant under the scleral flap, placed in a scleral pocket, helps to maintain an intrascleral aqueous lake and reduces adhesion between the lamellar scleral flap and scleral bed, thereby augmenting aqueous outflow [Fig. 1]. Caution is required while using this technique and additional sutures must be used to close the scleral flap as there is a risk of over-filtration of aqueous with swallowing of the AC and hypotony.
Figure 1.
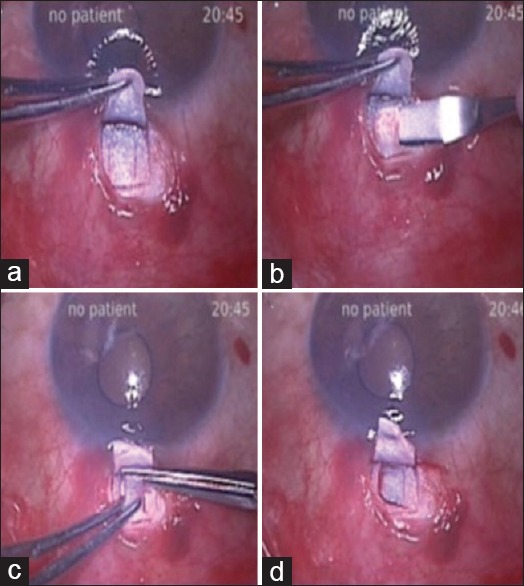
(a) Conventional partial thickness scleral flap is raised and two partial thickness vertical cuts are made at the scleral bed. (b) Smaller partial thickness flap is raised from the scleral bed. (c) Smaller flap is cut. (d) A deep scleral pocket is created to allow pooling of aqueous
In our experience, the use of Ologen implant alone under the conjunctiva is not sufficient to achieve a low target IOP as it covers only a small area under the conjunctiva (<6 mm diameter) and fibrosis occurs around the implant and within its porous structures, especially in eyes which already have a subclinical conjunctival inflammation due to multi-drug topical therapy. Hence, we always combine the Ologen implantation with the application of low-dose MMC over a broad area, in eyes requiring low target IOP. The subconjunctival Ologen implant must be placed posterior to the scleral flap, to permit visualization of the 10-0 monofilament nylon sutures for laser suturolysis if required. The implant under the scleral flap should fit within the scleral gutter as it its dimensions are larger than the scleral flap, over filtration will occur. Additionally with the use of Ologen, if bleb needling is required, it must be done through the implant itself, to permit adequate aqueous drainage [Fig. 2].
Figure 2.
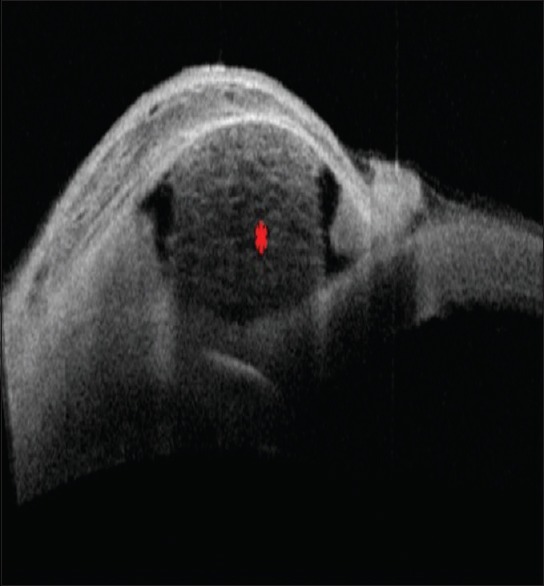
Postoperative anterior segment optical coherence tomography at 3 months follow-up showing a well-elevated bleb with subconjunctival Ologen (red asterisk) in situ
Trabeculectomy Enhanced with Cyclodialysis
Disinsertion of the ciliary body from its scleral attachment opens up the potential suprachoroidal space with an increase in aqueous absorption through uveoscleral pathway. Cyclodialysis, as practiced earlier, used a cyclodialysis spatula passed under the scleral lip to mechanically depress the ciliary body with side to side sweeping movements of spatula, thereby separating the ciliary body from the scleral spur was a blind and unpredictable procedure with the risks of hypotony and hemorrhage. The suprachoroidal drainage pathway is especially useful in eyes with preexisting conjunctival scarring (postvitreo-retinal or corneal grafting surgery or a failed trabeculectomy) or conditions with a high risk of failure such as the ICE syndrome.
Sihota et al.[10] evaluated a limited ab-externo cyclodialysis performed under direct vision as a part of trabeculectomy in 45 patients with postkeratoplasty glaucoma. The mean preoperative IOP was 38.9 ± 3.9 mmHg, and IOP was maintained below 15 mmHg in all but two patients, without any antiglaucoma medications. There was no decrease in graft clarity and no graft failure after the surgery in any eye for up to 2 years. Ultrasound biomicroscopy confirmed drainage from both the subconjunctival and suprachoroidal pathways.
Dada et al.[11] reported a novel technique of trabeculectomy combined with cyclodialysis with a 3-site (triple) implantation of Ologen-subconjunctival, subscleral, and supraciliary (within the cyclodialysis cleft) in eyes with advanced glaucoma. The placement of the biodegradable collagen implant (Ologen) helps to reduce fibrosis at these potential sites of scarring and with its space-occupying and antifibrotic properties. Cyclodialysis clefts often close spontaneously due to postoperative inflammation, and hence the placement of a small piece of the implant helps to prevent early closure of cyclodialysis cleft made during surgery.
Anterior Segment Optical Coherence Tomography Guided Trabeculectomy
In patients with opaque grafts with secondary glaucoma glaucoma following penetrating keratplasty anterior segment optical coherence tomography (ASOCT) was used to visualize the AC details.[12] This modality helps the surgeon in decision-making with the site and extent of peripheral anterior synechiae and the lenticular status, allowing better preoperative planning of the trabeculectomy or tube site. Being a noncontact procedure, it is also be useful method for assessing the AC depth in the postoperative period.
Circumferential Trabeculotomy for Primary Congenital Glaucoma
In primary congenital glaucoma (PCG) due to an abnormal development of the AC angle, the infant presents with an enlarged eyeball with a hazy cornea and raised IOP. Goniotomy or trabeculotomy is often performed as the first surgery in Caucasian eyes, however in our country trabeculectomy augmented with MMC combined with trabeculotomy is generally the accepted norm. However, this procedure is associated with a higher risk and late complications attributed to the use of MMC. Traditional ab-externo trabeculotomy can be performed in hazy corneas, however, it only allows access to 90–120° of the angle with limited success. A circumferential (360°) trabeculotomy is preferred as it can treat the entire angle. Initially, circumferential trabeculectomy was performed using a suture, however there was a risk of misdirection of the leading end of suture into the subretinal or suprachoroidal space. The use of illuminated microcatheter-assisted circumferential trabeculotomy by virtue of trans-scleral visualization, minimizes the risk of false passage.[13]
Temkar et al.[14] and Dada et al. performed the first prospective, randomized trial of thirty patients (sixty eyes) with bilateral PCG aged ≤2 years, with one eye of each patient being randomized to: illuminated microcatheter – assisted trabeculotomy (Group I) or combined trabeculotomy with trabeculectomy augmented with MMC (Group II). At 1 year, absolute success (IOP <15 mmHg without medication) was achieved in 86.7% (26/30) and 90.0% (27/30) in Groups I and II, respectively (P > 0.99) and qualified success (IOP <15 mmHg with medication) in 93.3% (28/30) in both groups. Thus illuminated microcatheter assisted circumferential trabeculotomy achieved comparable surgical outcomes to MMC-augmented combined trabeculotomy-trabeculectomy and can be advocated as the primary surgical procedure in eyes with PCG. Whenever trabeculotomy is performed alone; it should be done at the temporal limbus, such that superior conjunctiva is available for subsequent trabeculectomy if required [Fig. 3].
Figure 3.
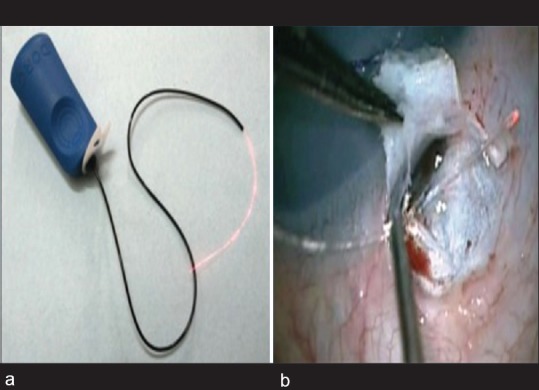
(a) 40 gauge illuminated microcatheter (DORC international). (b) Schlemm's canal exposed for inserting illuminated microcatheter
Bleb Revisions for Restoring Function of a Failing Filter (Trabeculectomy)
Pharmacological remodeling
Velpandian et al.[15] demonstrated transconjunctival penetration of MMC when applied over the intact conjunctiva in a dosage of 0.4 mg/ml for 3 min was applied before beginning the trabeculectomy in 41 eyes. Nearly 90% of eyes concentration above the required levels to inhibit human fibroblastic response was found in Tenon's capsule. They concluded from the study that in patients showing early signs of bleb failure like increased vascularity around the bleb and corkscrew vessels,[16] supra-conjunctical application of MMC may be performed to inhibit subconjunctival fibrosis. This technique is safer compared to MMC drops which are associated with corneal complications and can be performed as an outpatient procedure.
Slit lamp optical coherence tomography-guided bleb revision
Bleb needling with antifibrotic agent (5-FU) augmentation is an established technique to salvage a failing bleb. The slit-lamp (SL)-ASOCT allows for visualization of the internal bleb architecture and hence improves the accuracy of surgical intervention with minimal damage to the adjacent functional areas. Dada et al. reported the first optical coherence tomography (OCT) guided intervention in ophthalmology with the use of OCT-guided bleb revisions.[17] A 26-gauge needle was introduced under the conjunctival flap into the dysfunctional bleb and fibrotic tissue was disrupted under the direct visual control of the needle track as monitored with SL-OCT imaging in patients operated with MMC-augmented trabeculectomy with features of bleb failure at 6–8 weeks postoperatively.
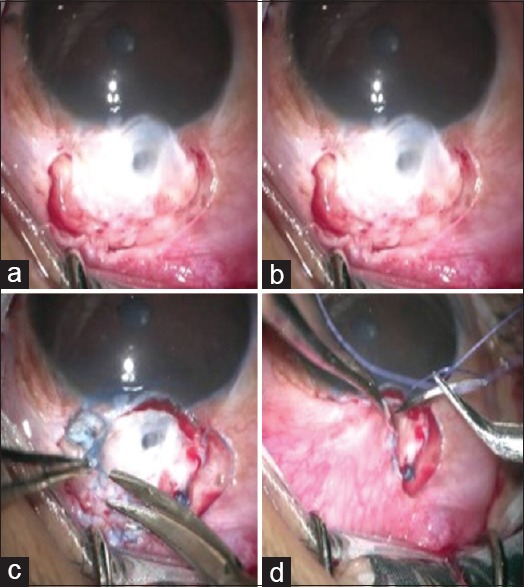
Intraoperative optical coherence tomography guided bleb needling
Dada et al. have described a new technique of intraoperative OCT-guided bleb needling to be performed in the operation theater.[18] This technique offers an opportunity to conduct the procedure in aseptic milieu, with the comfortable positioning of both patient and the surgeon and better management in the event of any complication. The passage of the needle through the bleb or under the scleral flap can be visualized simultaneously under the miscroscope with an overlay of the live OCT image [Fig. 4].
Figure 4.
(a) Flat bleb with increased vascularity. (b) Corresponding live intraoperative optical coherence tomography imaging-horizontal scan (blue horizontal line) and vertical scan (red vertical line) of the bleb area shows minimal hyporeflective spaces, indicating a fibrosed bleb. (c) Bleb begins to elevate after needling. (d) Intra-operative intraoperative optical coherence tomography imaging showing a relatively raised bleb with multiple hypo-reflective spaces
Bleb needling augmented with subconjunctival implant using an intraocular lens injector system
To increase the success rates of bleb needling, Dada and Angmo[19] described a technique of needling with subconjunctival Ologen implantation, to prevent re-adhesion. After standard needling procedure using a 26-gauge needle, the Ologen was inserting using an intraocular lens (IOL) delivery system through a 1.5 mm conjunctival incision, 10 mm from the limbus, i.e., away from the site of the bleb. The implant was then massaged close to the limbus, to maintain a slightly posterior bleb. This technique can be a useful tool in surgeon's armamentarium in cases with high risk of failure and a very vascular bleb and increases the long-term success of the needling procedure.
Surgical bleb revisions for dysfunctional filtering blebs with hypotony
Antimetabolites such as MMC and 5-FU associated with a higher incidence of complications such as hypotony, hypotony maculopathy, and endophthalmitis.[4] Traditional management of thin sweating bleb by excision or cautery of the bleb with the advancement of the conjunctiva and possibly sclera was associated with increased IOP and complications in a significant number of patients.[20,21]
Sihota et al.[22] reported a new technique for management of hypotonic maculopathy due to late bleb leakage. The bleb area was examined using anterior segment fluorescein angiography which showed generalized seepage of aqueous from the bleb. The bleb was excised and a conjunctival rotational pedicle flap was raised from the temporal conjunctiva to cover the defect superiorly. Mitomycin epithelial toxicity leads to such dysfunctional blebs and “sweating” conjunctiva over the bleb, which leads to chronic over filtration and hypotonic maculopathy. Excision of the diseased bleb conjunctiva alone with an overlay of the healthy conjunctiva is a safe and effective method of treating this potential complication of MMC-augmented trabeculectomy.
The authors also reported a prospective, observational case series of 34 consecutive eyes, having prior operated trabeculectomy with mitomycin and having a dysfunctional filtering bleb with evidence of hypotony or hypotony maculopathy, bleb sweating or leak, or previous episode of blebitis. These cases underwent bleb sparing epithelial exchange, i.e., the epithelium over a dysfunctional trabeculectomy bleb was peeled off and replaced with the conjunctiva advanced from the superior fornix, without disturbing the matrix of the bleb itself in any way [Figs. 5 and 6]. The average duration between trabeculectomy and bleb revision was 7.2 ± 3.9 years (median, 6 years). The mean preoperative IOP was 5.8 ± 4.2 mmHg. Postoperatively, absolute success at 12 months was 91.2% (31/34 eyes) and qualified success was 8.8% (3/34 eyes). There was a significant improvement in visual acuity. Postoperative complications were raised IOP (3/34) and mild ptosis (1/34). The ASOCT of the filtering blebs postoperatively showed a decrease in the bleb height, a thicker epithelium, and smaller hyporeflective spaces within the bleb tissue.[23]
Figure 5.
Bleb sparing epithelial exchange technique of bleb revision. (a) The conjunctiva around the bleb area is separated. (b) The dead epithelium over bleb is stained using trypan blue dye. (c) Stained epithelium is peeled off, leaving underlying bleb intact. (d) The surrounding conjunctiva is advanced over the bleb
Figure 6.
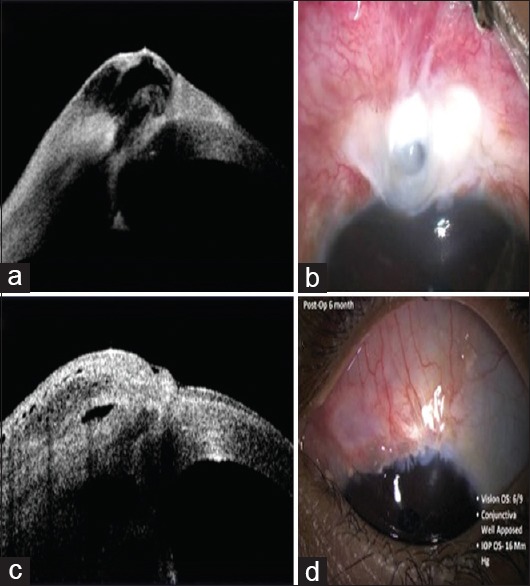
(a) Clinical photograph showing thin-walled avascular bleb. (b) Corresponding anterior segment optical coherence tomography showing a thin layer of conjunctiva over the bleb area. (c) Postoperative clinical photograph showing healthy conjunctiva advanced over the bleb. (d) Corresponding anterior segment optical coherence tomography showing well elevated bleb, covered with a healthy conjunctiva
Cataract Surgery and Trabeculectomy
In eyes undergoing cataract surgery with previously operated trabeculectomy, trypan blue dye can be used to assess the functional status of filtering bleb and grade the filtration.[24] This gives a good idea about the adequacy of subconjunctival filtration in eyes undergoing phacoemulsification and can be used to plan for intraoperative surgical interventions in the form of needling, repeat surgery, or other bleb modulations.
Dada et al. described the technique of inserting conventional foldable hydrophobic IOL in microincision cataract surgery (MICS) without enlarging the wound, in patients undergoing combined MICS with trabeculectomy.[25] After completion of bimanual phacoemulsification, a 3.2 mm incision was made using the keartome below previously outlined scleral flap. IOL was inserted through this incision. The scleral flap was then elevated, and an ostium made using a Kelly's punch. This technique can also be useful in younger patients where a simple bimanual irrigation-aspiration is used for lenticular surgery, and the IOL inserted through the superior trabeculectomy fistula.
Minimally Invasive Glaucoma Surgery
Replacing the Ex-PRESS mini shunt
The Ex-PRESS glaucoma filtration device is a nonvalved miniature stainless steel device developed as an alternative to trabeculectomy, which has significantly increased the cost of surgery without any significant clinical benefit. Although published literature suggests equal efficacy and safety of the Ex-PRESS shunt and standard trabeculectomy; our experience with the Ex-PRESS shunt has not been encouraging[26] and we have abandoned its use. However, we developed our own mini-shunt implant (The poor man's Ex-PRESS!).
We used a low-cost alternative which is universally available and can function as an alternative to classic trabeculectomy. Glaucoma filtering surgery using a 24-gauge intravenous cannula together with low dose subconjunctival MMC in pseudophakic patients with primary open angle glaucoma and advanced glaucomatous optic neuropathy. Postoperatively, IOPs ranged from 12 to 15 mmHg over 12-month follow-up.[27] Although this technique still requires further refinement and evaluation, we should try and innovate such microsurgical devices which can be affordable to our population.
Preventing corneal complications of glaucoma drainage devices
Tube- endothelial touch is a well-known complication of Ahmed glaucoma valve (AGV) implantation leading to corneal decompensation, with over 20% endothelial loss being reported after 2-year follow-up. Dada et al.[28] described a technique to reposition the AGV tube in the AC by passing two 10-0 prolene anchor sutures and pulling away the tube from the endothelium. Resolution of corneal edema was noted without affecting the tube drainage and IOP. This is a useful technique which can be adopted in any patient who has had a glaucoma drainage device which is adequately lowering IOP but leading to progressive corneal endothelial damage. This obviates the need to explant the glaucoma drainage device and can also reduce the need for subsequent endothelial keratoplasty.
Glaucoma surgery is a double edged sword with fibrotic bleb failure at one end of the spectrum and hypotony maculopathy with a visual loss at the other. There is no single surgical method to achieve optimal long-term outcomes for preserving the quality of life of the patient. Therefore, it is imperative that every glaucoma surgeon should innovate and modify his own surgical techniques and overcome the challenges posed by the treatment of this blinding disease. Even though there is an “economically driven” global shift towards minimally invasive glaucoma surgeries, trabeculectomy continues to be the current gold standard choice of glaucoma surgery in previously unoperated eyes with moderate to advanced glaucoma. We should continue our efforts to improvise our current surgical techniques to achieve better long-term IOP control with minimal complications and at the lowest cost to the patients. The quest for surgical innovations for the benefit of our patients is a critical need, and we conclude with this famous quote by Albert Einsten – “Imagination is more important than knowledge.”
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968;66:673–9. [PubMed] [Google Scholar]
- 2.Landers J, Martin K, Sarkies N, Bourne R, Watson P. A twenty-year follow-up study of trabeculectomy: Risk factors and outcomes. Ophthalmology. 2012;119:694–702. doi: 10.1016/j.ophtha.2011.09.043. [DOI] [PubMed] [Google Scholar]
- 3.Lehmann OJ, Bunce C, Matheson MM, Maurino V, Khaw PT, Wormald R, et al. Risk factors for development of post-trabeculectomy endophthalmitis. Br J Ophthalmol. 2000;84:1349–53. doi: 10.1136/bjo.84.12.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Higashide T, Ohkubo S, Sugimoto Y, Kiuchi Y, Sugiyama K. Persistent hypotony after trabeculectomy: Incidence and associated factors in the Collaborative Bleb-related Infection Incidence and Treatment Study. Jpn J Ophthalmol. 2016;60:309–18. doi: 10.1007/s10384-016-0450-4. [DOI] [PubMed] [Google Scholar]
- 5.Gedde SJ, Herndon LW, Brandt JD, Budenz DL, Feuer WJ, Schiffman JC. Tube Versus Trabeculectomy Study Group. Postoperative complications in the tube versus trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol. 2012;153:804–14.e1. doi: 10.1016/j.ajo.2011.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nayak B, Gupta S, Kumar G, Dada T, Gupta V, Sihota R. Socioeconomics of long-term glaucoma therapy in India. Indian J Ophthalmol. 2015;63:20–4. doi: 10.4103/0301-4738.151458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sihota R, Angmo D, Chandra A, Gupta V, Sharma A, Pandey RM. Evaluating the long-term efficacy of short-duration 0.1 mg/ml and 0.2 mg/ml MMC in primary trabeculectomy for primary adult glaucoma. Graefes Arch Clin Exp Ophthalmol. 2015;253:1153–9. doi: 10.1007/s00417-015-3028-9. [DOI] [PubMed] [Google Scholar]
- 8.Dada T, Kusumesh R, Bali SJ, Sharma S, Sobti A, Arora V, et al. Trabeculectomy with combined use of subconjunctival collagen implant and low-dose mitomycin C. J Glaucoma. 2013;22:659–62. doi: 10.1097/IJG.0b013e3182594f5b. [DOI] [PubMed] [Google Scholar]
- 9.Angmo D, Wadhwani M, Upadhyay AD, Temkar S, Dada T. Outcomes of trabeculectomy augmented with subconjunctival and subscleral ologen implantation in primary advanced glaucoma. J Glaucoma. 2017;26:8–14. doi: 10.1097/IJG.0000000000000537. [DOI] [PubMed] [Google Scholar]
- 10.Sihota R, Srinivasan G, Gupta V. Ab-externo cyclodialysis enhanced trabeculectomy for intractable post-penetrating keratoplasty glaucoma. Eye (Lond) 2010;24:976–9. doi: 10.1038/eye.2009.282. [DOI] [PubMed] [Google Scholar]
- 11.Dada T, Sharma R, Sinha G, Angmo D, Temkar S. Cyclodialysis-enhanced trabeculectomy with triple ologen implantation. Eur J Ophthalmol. 2016;26:95–7. doi: 10.5301/ejo.5000633. [DOI] [PubMed] [Google Scholar]
- 12.Dada T, Shah BM, Bali SJ, Bansal N, Panda A, Vanathi M. Anterior segment OCT imaging in opaque grafts with secondary glaucoma following tectonic penetrating keratoplasty for perforated corneal ulcers. Eye (Lond) 2011;25:1522–4. doi: 10.1038/eye.2011.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Girkin CA, Marchase N, Cogen MS. Circumferential trabeculotomy with an illuminated microcatheter in congenital glaucomas. J Glaucoma. 2012;21:160–3. doi: 10.1097/IJG.0b013e31822af350. [DOI] [PubMed] [Google Scholar]
- 14.Temkar S, Gupta S, Sihota R, Sharma R, Angmo D, Pujari A, et al. Illuminated microcatheter circumferential trabeculotomy versus combined trabeculotomy-trabeculectomy for primary congenital glaucoma: A randomized controlled trial. Am J Ophthalmol. 2015;159:490–7.e2. doi: 10.1016/j.ajo.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Velpandian T, Sihota R, Sinha A, Gupta V. Transconjunctival penetration of mitomycin C. Indian J Ophthalmol. 2008;56:197–201. doi: 10.4103/0301-4738.40357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shingleton BJ. Management of the failing glaucoma filter. Ophthalmic Surg Lasers. 1996;27:445–51. [PubMed] [Google Scholar]
- 17.Dada T, Vengayil S, Gadia R, Gupta V, Sihota R. Slitlamp-optical coherence tomography-guided needling of failing filtering blebs. Arch Ophthalmol. 2008;126:284–6. doi: 10.1001/archophthalmol.2007.55. [DOI] [PubMed] [Google Scholar]
- 18.Dada T, Angmo D, Midha N, Sidhu T. Intraoperative optical coherence tomography guided bleb needling. J Ophthalmic Vis Res. 2016;11:452–4. doi: 10.4103/2008-322X.194150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dada T, Angmo D. Bleb needling with subconjunctival ologen. Oman J Ophthalmol. doi: 10.4103/ojo.OJO_159_2015. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wadhwani RA, Bellows AR, Hutchinson BT. Surgical repair of leaking filtering blebs. Ophthalmology. 2000;107:1681–7. doi: 10.1016/s0161-6420(00)00282-7. [DOI] [PubMed] [Google Scholar]
- 21.Al-Shahwan S, Al-Torbak AA, Al-Jadaan I, Omran M, Edward DP. Long-term follow up of surgical repair of late bleb leaks after glaucoma filtering surgery. J Glaucoma. 2006;15:432–6. doi: 10.1097/01.ijg.0000212257.02702.e8. [DOI] [PubMed] [Google Scholar]
- 22.Sihota R, Dada T, Gupta SD, Sharma S, Arora R, Agarwal HC. Conjunctival dysfunction and mitomycin C-induced hypotony. J Glaucoma. 2000;9:392–7. doi: 10.1097/00061198-200010000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Sihota R, Angmo D, Sen S, Gupta V, Dada T, Pandey RM. The long-term outcome of primary “bleb-sparing, epithelial exchange” in dysfunctional filtering blebs. J Glaucoma. 2016;25:571–8. doi: 10.1097/IJG.0000000000000322. [DOI] [PubMed] [Google Scholar]
- 24.Dada T, Bali SJ, Mohan S, Bhartiya S, Sobti A, Panda A. Trypan blue staining of filtering bleb in eyes with operate trabeculectomy. Nepal J Ophthalmol. 2012;4:224–9. doi: 10.3126/nepjoph.v4i2.6536. [DOI] [PubMed] [Google Scholar]
- 25.Dada T, Muralidhar R, Sethi HS. Insertion of a foldable hydrophobic IOL through the trabeculectomy fistula in cases with microincision cataract surgery combined with trabeculectomy. BMC Ophthalmol. 2006;6:14. doi: 10.1186/1471-2415-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Angmo D, Sharma R, Temkar S, Dada T. Evaluation of ExPress glaucoma filtration device in Indian patients with advanced glaucoma. Indian J Ophthalmol. 2015;63:459–62. doi: 10.4103/0301-4738.159894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dada T, Angmo D, Temkar S, Sharma R. Use of a 24 gauge intravenous cannula for minimally invasive trabeculectomy. J Ophthalmic Vis Res. 2015;10:87–9. doi: 10.4103/2008-322X.156130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dada T, Gupta R, Tinwala SI, Sobti A, Panda A. Repositioning of Ahmed glaucoma valve tube in the anterior chamber with prolene sutures to manage tube-endothelial touch. Nepal J Ophthalmol. 2012;4:309–11. doi: 10.3126/nepjoph.v4i2.6549. [DOI] [PubMed] [Google Scholar]


