Abstract
Environmental factors can act as facilitators of chronic non-communicable diseases. Ambient noise and air pollution collectively outrank all other environmental risk factors in importance, contributing to over 75% of the disease and disability burden associated with known environmental risk factors. In the first part of this review, we discussed the global burden and epidemiologic evidence supporting the importance of these novel risk factors as facilitators of cardiometabolic disease. In this part, we will discuss pathophysiological mechanisms responsible for noise and air pollution-mediated effects. Akin to traditional cardiovascular risk factors, a considerable body of evidence suggests that these environmental agents induce low-grade inflammation, oxidative stress, vascular dysfunction, and autonomic nervous system imbalance, thereby facilitating the development of diseases such as hypertension and diabetes. Through their impact on traditional risk factors and via additional novel mechanisms, environmental risk factors may have much larger impact on cardiovascular events than currently appreciated. In the second part of this review, we discuss deficiencies and gaps in knowledge and opportunities for new research.
Keywords: Noise, Air pollution, Oxidative stress, Inflammation, Atherosclerosis, Cardiovascular risk factor, Environment, Cardiometabolic disease
Introduction
Air and noise pollution are pervasive health problems that have co-existed in civilization for centuries, and together they are the most common environmental risk factors in the physical environment that people may encounter in modern society, particularly in urban areas. Empirical and epidemiologic evidence supports the concept that both air pollution and noise independently may induce stereotypic activation of pathways such as oxidative stress, vascular dysfunction, and autonomic imbalance, and amplify the impact of traditional risk factors on cardiovascular disease (CVD). Air pollution and noise in urban environments contribute disproportionately to cardiovascular and metabolic risk and disability, and account substantially to the burden of disease globally attributable to environmental factors.1 In this review, we present the mechanistic evidence linking these factors with cardiovascular and metabolic disease, address unmet research needs and technology-aided solutions to further understand disease mechanisms and to mitigate their risk.
Pathophysiology of noise and air pollution-induced cardiovascular disease
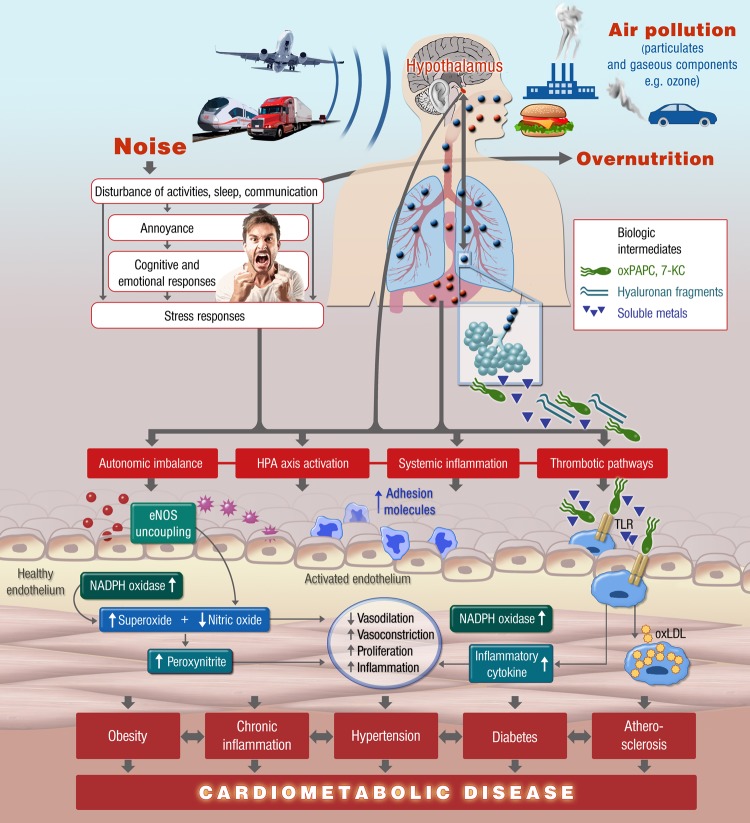
Analogous to traditional risk factors, a growing body of evidence has substantiated the concept that air pollution and noise leads to vascular (endothelial) dysfunction, hypertension, atherosclerosis, and complications including myocardial infarction, stroke, and congestive heart failure. Four generalized pathways have been postulated to help explain the systemic effects of air pollution and noise (Figure 1): (a) perturbation of autonomic nervous system and/or sympathoadrenal activation; (b) release of pro-inflammatory mediators, modified lipids, or phospholipids and activation of leukocyte populations; (c) endothelial dysfunction caused by oxidative stress; and (d) activation of prothrombotic pathways.2–10 These pathophysiologic pathways are not mutually exclusive, and may be principally active at differing time points following exposure to either noise or air pollution, and likely vary in importance, in relation to chronicity of exposure and in causation of CV sequelae.
Figure 1.
Proposed pathophysiological mechanisms of cardiovascular disease induced by environmental air pollution and noise. ox-PAPC, oxidatively modified 1-palmitoyl-2-arachidonoyl-sn-phosphatidylcholine; 7-KC, 7-ketocholesterol.
The acute responses occurring within seconds/minutes/hours after noise exposure or PM inhalation are likely mediated principally via changes in autonomic tone and/or sympathoadrenal activation, alterations in endothelial function, direct effects on pro-coagulant pathways and thrombosis mediated by the release of pro-coagulant proteins.11 The acute effects of both air pollution and noise pollution may often occur in the context of chronic exposure in a susceptible patient, typified by the individual with pre-existing ‘vulnerable plaque’, ‘vulnerable myocardium’ (arrhythmias), or ‘vulnerable circulation’ (in a heart failure patient at risk for circulatory overload). The effects of chronic repetitive environmental exposure are more complex, with a number of issues that one needs to consider, including, that the cumulative impact (exposure over time) occurs within the framework of other more dominant risk factors. In this regard, the effects of noise and air pollution may be either additive or synergistic. When chronically exposed, attenuation in response may occur; a phenomenon known as habituation. As example, the probability that noise causes physiologic effects is generally higher during the first days of exposure compared with the subsequent days, and exposure–response relationships derived in the field (where subjects have often been exposed to the noise for many years) are usually much shallower than those derived in laboratory settings, which often include exposure to unfamiliar noise events in an unfamiliar environment.3,12,13 Attenuation of response to air pollution with repeated exposure has good biologic plausibility, but has never been conclusively shown in an experimental context. In certain contexts, however, the opposite may happen, i.e. the second exposure may cause larger effects than the first one, a phenomenon known as priming.14
Noise pollution: mechanisms leading to cardiovascular events
According to the noise reaction model introduced by Babisch, two principal pathways have been theorized as being responsible for the adverse health effects of noise, a direct and indirect pathway.15 The direct pathway is activated by an instantaneous interaction of the acoustic nerve with structures of the central nervous system. The indirect pathway in turn represents the cognitive perception of the sound, and its subsequent cortical activation and is related to emotional responses (Figure 1).16 It is important to note, however, that recent studies have demonstrated adverse effects on vascular function were completely independent from sleep quality and self-reported noise sensitivity.17
Both reaction chains can initiate physiological stress responses, involving the hypothalamus, the limbic system, and the autonomous nervous system with activation of the hypothalamus–pituitary–adrenal (HPA) axis and the sympathetic–adrenal–medulla axis. This leads to a cascade of effects, including a rise in heart rate and in levels of stress hormones (cortisol, adrenalin, and noradrenaline).18 This general stress model is a physiologic acute adaptation to stress, which may ultimately lead to pathophysiologic alterations in the intermediate or chronic time frame, resulting in manifest adverse health effects. While the conscious experience with noise might be the primary source of stress reactions during day time in awake subjects, the non-conscious biological response during nighttime in sleeping subjects, at much lower noise levels, is thought to play an important role in pathophysiology, particularly through disruption of sleep-wake cycle, diurnal variation and perturbation of time periods critical for physiological and mental restoration.15
Recently, a study addressed whether there are combined effects of objectively estimated noise levels (aircraft or road) and noise annoyance on the prevalence of arterial hypertension (in HYENA).19 The study indicated that for aircraft noise, noise annoyance acted as an effect modifier of the relationship between noise and arterial hypertension, with stronger associations among the annoyed.19 In contrast, the study found no effect modification by annoyance on the road traffic noise and hypertension association. More studies are needed to elucidate the influence of annoyance to noise on the relationship between noise exposure and CVD.
Experimental animal models designed to address the vascular consequences of noise are scarce. A Pubmed search identified just two publications studying the effects of noise on function in animal models. In a murine model, noise stress (100 dB, 1 kHz, 4 h/day, 6 days/week) selectively impaired responses to endothelium-dependent vasodilators (A23187 and acetylcholine) and increased those to vasoconstrictors20,21 In these studies, no mechanistic insight to the underlying mechanisms were provided, stressing the urgent need for animal models in order to study the vascular consequences of noise. In light of the importance of the HPA axis and the autonomic nervous system as the systems most likely to be involved with acute stressors, it is reasonable to speculate on their involvement in response to noise-induced stress. Given the involvement of the autonomic nervous system in response to triggers such as smoking, air pollution, and acute mental stress, it is likely that acute cardiovascular responses including changes in vascular tone, in response to noise alone, or more importantly in the context of co-exposure to noise and air pollution, may involve enhanced sympathetic activity in association with neurohormonal changes.
The results of older experimental studies were recently confirmed in humans.20,21 Two studies showed that nighttime noise dose-dependently leads to endothelial dysfunction, increased blood pressure, and impaired sleeping quality in healthy subjects and patients with coronary artery disease.14,17 Importantly, this effect was caused by oxidative stress, since nighttime noise-induced endothelial dysfunction was significantly improved by the acute administration of vitamin C.14 As expected, noise-induced endothelial dysfunction was more pronounced in CAD patients, who had pre-existent dysfunction, compared with healthy volunteers.17 Interestingly, the deterioration of vascular function in response to noise was independent on the degree of annoyance of the study participants, suggesting that noise may trigger vascular dysfunction independent of emotional responses through direct effects on the autonomic system.17 These findings go along with the observations of the HYENA study showing that noise-induced increases in systolic and diastolic blood pressure were not always linked to an awakening reaction.22 We could also demonstrate that the adverse effects of nighttime aircraft noise on the vasculature are getting accentuated rather than desensitized in response to repetitive noise exposures pointing to a priming effect.14 In line with animal data, nighttime noise led to a 4-mmHg increase in systolic blood pressure in patients and in healthy subjects, equivalent to a 4% increase in the risk of new-onset heart failure.23
There is currently limited data on other noise-induced pathways, such as involvement of inflammation or thrombosis pathways. In one study, noise has been shown to induce a reduction in the level of coagulation factor XII (Hageman-factor)17 which has been associated with increased coronary risk.24,25 Also, exposure to nighttime traffic noise may affect the immune system through disturbance of sleep, thereby increasing risk for CVD.26 Sleep is known to have a strong regulatory influence on the immune system, with disturbances in sleep being associated with reduced immune function and a pro-inflammatory state.27 Furthermore, cortisol, which has been found increased after exposure to traffic noise, is known to play an important role in regulating the immune system, and acute and chronic stress has been associated with suppression of the immune system.28,29 The importance of noise, both day- and nighttime exposure, in perturbation of inflammatory and haemostatic factors needs to be investigated.
The role of exposure to noise in the genesis of perturbations in glucose metabolism and lipid abnormalities has only been scarcely touch upon30 and clearly needs to be evaluated in a rigorous manner. This of course may aggravate or even accelerate the atherosclerotic process and predispose to future cardiovascular events.
Based on the results to date, noise pollution may indeed accentuate conventional risk factors such as hypertension. Taken together, noise, particularly at nighttime has been demonstrated to cause sympathovagal imbalance, vascular dysfunction, and increased blood pressure. These changes are consistent with changes in multiple large-scale studies, where noise exposure increases blood pressure in subjects exposed to road or railway noise.22,31–33 Alterations in sleep seen with noise may result in nocturnal autonomic arousals, which is well demonstrated to prevent blood pressure dipping and contribute to the risk for developing hypertension, a concept that is confirmed by the observation that the risk of developing hypertension is higher in subjects exposed to noise during night hours.22,34,35
Air pollution: mechanisms leading to cardiovascular events
A variety of different approaches have been adopted to study the effects of air pollution in the experimental context. These approaches include exposure to concentrated ambient particles, diesel exhaust from engines to mimic road traffic exposure, air pollution mixtures in exposure chambers and finally direct exposure to ambient atmospheres, in both animals and humans. Published studies vary greatly with regards to route/duration of exposure, pre-existing disease/risk in humans, strain/susceptibility of animals, location of exposure (influenced by source of pollutants, climate/wind patterns), and compositional characteristics of particles.
Oxidative stress pathways are integral to the mechanism of the vascular damage induced by air pollution, and increases in oxidative stress and inflammatory markers or activation of genes have been shown to result from diesel exhaust, wood smoke, PM2.5, or UFP.36–38,39 Increase in oxidant stress appears to be a broadly applicable mechanism, regardless of the type of pollutants that contributes to the adverse effects of air pollution. Inflammatory responses have been consistently observed in experimental animal models and may relate to the activation of innate and adaptive immune responses, leading to the release of cytokines/chemokines.40–42 Activation of central nerve system reflex arcs may also facilitate systemic inflammation, and is thought to be a relevant mechanism that may link pulmonary exposures to systemic inflammatory activation.43–45 Penetration to the systemic circulation of diffusible components such as soluble metals and intermediates such as oxidized phospholipids, quinines, semiquinones, and aldehydes generated in the lung, may also lead to potentiation of inflammatory responses.41,46,47 These results have been less consistently observed in controlled acute human exposure studies, and increases in peripheral markers of inflammation, observed in some studies have not been replicable in other ones, possibly due to differences in the sensitivity of the measurements, in the study protocols or vulnerability of the subjects due to individual-level factors or unmeasured prior exposures.48 Data from multiple groups demonstrate an effect of PM2.5, UFP, and diesel exhaust in systemic endothelial dysfunction and diminished nitric oxide availability due to activation of reactive oxygen species pathways including endothelial nitric oxide synthase uncoupling. Changes in blood pressure in animal models are also associated with activation of central sympathetic mechanisms.49 The findings in animal models are mirrored in humans with exposure to both PM2.5 and traffic-related pollutants such as diesel exhaust, having been shown to cause acute peripheral conduit vasoconstriction within a few hours. In animals, exposure to PM2.5 results in endothelial dysfunction and activation of Rho/ROCK signaling and heightened calcium sensitivity.50,51 Controlled exposure studies show that diesel exhaust, which appears to have larger effects than other pollutants, acutely (within minutes to hours) impairs resistance vessel responses to acetylcholine, bradykinin, and nitroprusside with evidence to suggest elevation in ET-1 as an additional mechanism of vasoconstriction.52–55 As a result, short-term exposure to diesel potentiates exercise-induced ST-segment depression and ischaemic burden.56 The effects on vascular function with PM2.5 are more variable with no observable effects with acute exposure in some studies and delayed effects in others, which sometimes may persist for as long as 24 h in healthy adults.37,57,58 Increased peripheral vasoconstriction due to short-term exposure to PM2.5 may result in elevation in systemic blood pressure and increased cardiac afterload and over the longer-term result in left ventricular hypertrophy, myocardial fibrosis and alteration in coronary flow reserve.59 This may in turn lead to impaired diastolic relaxation and eventual impairment contractile reserve. At a molecular level, increased β-myosin heavy chain and down regulation of SERCA2a, indicative of abnormal calcium cycling, have been demonstrated.
Exposure to air pollution has been shown to result in facilitation of a number of pathways that are pro-atherogenic. The formation of highly oxidized forms of phospholipids (oxidatively modified 1-palmitoyl-2-arachidonoyl-sn-phosphatidylcholine or oxPAPC) and cholesterol (e.g. 7-ketocholesterol) has been previously shown to potentiate inflammation and may play an important role in acceleration of atherosclerosis.60,61 The generation of reactive biologic mediators such as oxPAPC in response to PM2.5 exposure may promote the migration of bone-marrow-derived CD11b+Ly6Chi+ cells to the atherosclerotic plaque via gradients in chemokines such as CCL-2 that could be synthesized in response to such derivatives.62 Both fine and ultrafine ambient PM lead to the development of dysfunctional HDL that loses its anti-inflammatory properties, antioxidant capacity, reduced ability to protect against LDL-induced monocyte migration and decreased paraoxonase activity.63 Exposure to ultrafine particles such as from diesel may result in 5-lipoxygenase-mediated formation of 12-HETE and 13-HODE, peroxidation products in the plasma and liver but, interestingly, not lung.64 Multiple studies have demonstrated increased progression of atherosclerosis and plaque inflammation after exposure to PM2.5, diesel exhaust, gaseous co-pollutants, and UFP.65–67 Experimental studies in murine models of arterial thrombosis have shown an IL-6-dependent activation of platelets within 30 min of intratracheal instillation of diesel exhaust particles.68 A significant effect of diesel exhaust on fibrinolytic function has also been seen both in healthy men and in men with coronary heart disease in response to intermittent exercise.52,56 Bradykinin-induced release of t-PA decreased with diesel exhaust when compared with filtered air at 6 h following exposure to diesel exhaust but did not persist 24 h following exposure.37Ex vivo studies in a flow chamber have shown heightened thrombosis under different shear rates and increased platelet-leukocyte aggregates.69
The evidence of an association between long-term exposure to PM2.5 and the burden of atherosclerosis in humans in cross-sectional studies using a variety of surrogates including carotid intima media thickness, coronary artery and aortic calcium, and ankle brachial indices is very consistent. Although the cross-sectional nature of these data warrants caution, the similarity of findings, and the bias towards the null inherent with the estimations of long-term exposure, support a biological relationship between air pollution exposure and atherosclerosis. Importantly, a reduction in PM2.5 levels is associated with a decrease in carotid intima media thickness progression reinforcing the biologic plausibility of this association.70
Prior reviews have covered the experimental evidence and mechanisms by which air pollution can independently increase risk for T2DM.43–45 Exposure to PM2.5 induces inflammation, impairs insulin response pathways in the liver, skeletal muscle and adipose, worsens hyperglycaemia at concentrations relevant to human exposure and affects pathways such as innate immune activation, endoplasmic reticulum stress, brown adipose function, and central nervous system pathways involved in glucose control, appetite satiety regulation, inflammation, and energy metabolism.
Gaps in current knowledge of air and noise pollution-mediated disease
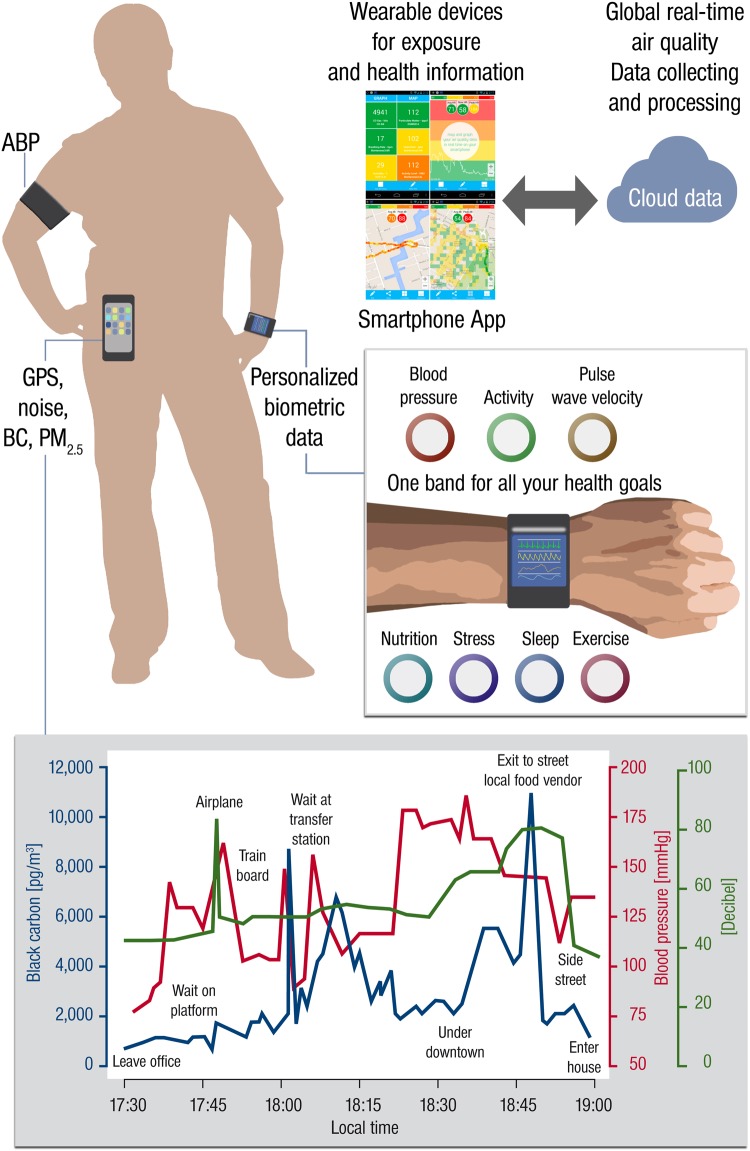
There are currently no studies that simultaneously have examined the effects of noise and air pollution exposure in experimental models or humans. A number of important questions at the mechanistic level in animals may help provide direction for future human studies. The questions that need to be addressed are many and include the magnitude and time course of response of co-exposure, interactive effects of both factors on surrogate measures such as blood pressure and metabolic risk, duration of effect/time course of reversal, impact of low-grade background noise on air pollution exposure effects and vice versa, impact on circadian rhythm and finally the effect of prevention and lifestyle (e.g. diet, stress, and exercise). The impact of traffic-related air pollutant co-exposure with noise is most worthy of initial study. Finally, the development of technologies that provide personal measures of health in conjunction with data on environmental exposure provide an unprecedented opportunity for research and may allow an extraordinary understanding of the interactions between environmental and non-environmental risk factors (Figure 2). However, the extent of these advances in knowledge are tempered by the need to manage subject burden and costs and less accurate or precise data due to the inexpensive nature of the devices available for use or reliance on individuals for their proper use.
Figure 2.
Hypothetical framework of investigations that combine technological innovation in biometric data with personalized exposure information in real time to study interactive effects of environmental risk factors on cardiovascular end-points. ABP, ambulant blood pressure monitoring; BC, black carbon; PM, particulate matter.
Conclusion
In summary, the present review summarizes mechanisms of importance in mediating cardiometabolic risk in response to noise and particulate matter as important and novel cardiovascular risk factors. Noise and PM may cause oxidative stress, vascular dysfunction, autonomic imbalance and metabolic abnormalities, potentiating not only risk factors such as hypertension and diabetes but culminating in progression of atherosclerosis and susceptibility to cardiovascular events. There is increasing rationale for studying the interaction between these novel risk factors and their collective impact on cardiometabolic disease.
Author's contributions
T.M., S.R. handled funding and supervision, drafted the manuscript. M.S., T.G., F.P.S., X.R., F.R.B., L.C.C., and R.D.B. made critical revision of the manuscript for key intellectual content.
Funding
This study was supported by the Center for Translational Vascular Biology (CTVB) and funded by the ‘Stiftung Mainzer Herz,’ T.M. is PI of the DZHK (German Center for Cardiovascular Research), partner site Rhein-Main, Mainz, Germany.
Conflict of interest: none declared.
Acknowledgement
The authors thank Margot Neuser for graphical support and Saumya Kanakanala for formulation of tables.
References
- 1. Stansfeld SA. Noise effects on health in the context of air pollution exposure. Int J Environ Res Public Health 2015;12:12735–12760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Griefahn B, Marks A, Robens S. Noise emitted from road, rail and air traffic and their effects on sleep. J Sound Vib 2006;295:129–140. [Google Scholar]
- 3. Basner M, Isermann U, Samel A. Aircraft noise effects on sleep: application of the results of a large polysomnographic field study. J Acoust Soc Am 2006;119:2772–2784. [DOI] [PubMed] [Google Scholar]
- 4. Griefahn B, Brode P, Marks A, Basner M. Autonomic arousals related to traffic noise during sleep. Sleep 2008;31:569–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Marks A, Griefahn B, Basner M. Event-related awakenings caused by nocturnal transportation noise. Noise Contrib Eng J 2008;56:52–62. [Google Scholar]
- 6. Horne JA, Pankhurst FL, Reyner LA, Hume K, Diamond ID. A field study of sleep disturbance: effects of aircraft noise and other factors on 5,742 nights of actimetrically monitored sleep in a large subject sample. Sleep 1994;17:146–159. [DOI] [PubMed] [Google Scholar]
- 7. Ohrstrom E, Hadzibajramovic E, Holmes M, Svensson H. Effects of road traffic noise on sleep: studies on children and adults. J Environ Psychol 2006;26:116–126. [Google Scholar]
- 8. Basner M, Glatz C, Griefahn B, Penzel T, Samel A. Aircraft noise: effects on macro- and micro-structure of sleep. Sleep Med 2008;9:382–387. [DOI] [PubMed] [Google Scholar]
- 9. Basner M. Nocturnal aircraft noise increases objectively assessed daytime sleepiness. Somnologie 2008;12:110–117. [Google Scholar]
- 10. Elmenhorst EM, Elmenhorst D, Wenzel J, Quehl J, Mueller U, Maass H, Vejvoda M, Basner M. Effects of nocturnal aircraft noise on cognitive performance in the following morning: dose-response relationships in laboratory and field. Int Arch Occup Environ Health 2010;83:743–751. [DOI] [PubMed] [Google Scholar]
- 11. Munzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J 2014;35:829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Basner M, Müller U, Elmenhorst E-M. Single and combined effects of air, road, and rail traffic noise on sleep and recuperation. Sleep 2011;34:11–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pearsons K, Barber D, Tabachnick BG, Fidell S. Predicting noise-induced sleep disturbance. J Acoust Soc Am 1995;97:331–338. [Google Scholar]
- 14. Schmidt FP, Basner M, Kroger G, Weck S, Schnorbus B, Muttray A, Sariyar M, Binder H, Gori T, Warnholtz A, Munzel T. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J 2013;34:3508–3514a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Babisch W. Cardiovascular effects of noise. Noise Health 2011;13:201–204. [DOI] [PubMed] [Google Scholar]
- 16. Babisch W. The noise/stress concept, risk assessment and research needs. Noise Health 2002;4:1–11. [PubMed] [Google Scholar]
- 17. Schmidt F, Kolle K, Kreuder K, Schnorbus B, Wild P, Hechtner M, Binder H, Gori T, Munzel T. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol 2015;104:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Golbidi S, Frisbee JC, Laher I. Chronic stress impacts the cardiovascular system: animal models and clinical outcomes. Am J Physiol Heart Circ Physiol 2015;308:H1476–H1498. [DOI] [PubMed] [Google Scholar]
- 19. Floud S, Blangiardo M, Clark C, de Hoogh K, Babisch W, Houthuijs D, Swart W, Pershagen G, Katsouyanni K, Velonakis M, Vigna-Taglianti F, Cadum E, Hansell AL. Exposure to aircraft and road traffic noise and associations with heart disease and stroke in six European countries: a cross-sectional study. Environ Health 2013;12:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wu CC, Chen SJ, Yen MH. Attenuation of endothelium-dependent relaxation in mesenteric artery during noise-induced hypertension. J Biomed Sci 1994;1:49–53. [DOI] [PubMed] [Google Scholar]
- 21. Wu CC, Chen SJ, Yen MH. Effects of noise on blood pressure and vascular reactivities. Clin Exp Pharmacol Physiol 1992;19:833–838. [DOI] [PubMed] [Google Scholar]
- 22. Haralabidis AS, Dimakopoulou K, Vigna-Taglianti F, Giampaolo M, Borgini A, Dudley ML, Pershagen G, Bluhm G, Houthuijs D, Babisch W, Velonakis M, Katsouyanni K, Jarup L, Consortium H. Acute effects of night-time noise exposure on blood pressure in populations living near airports. Eur Heart J 2008;29:658–664. [DOI] [PubMed] [Google Scholar]
- 23. Ekundayo OJ, Allman RM, Sanders PW, Aban I, Love TE, Arnett D, Ahmed A. Isolated systolic hypertension and incident heart failure in older adults: a propensity-matched study. Hypertension 2009;53:458–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bach J, Endler G, Winkelmann BR, Boehm BO, Maerz W, Mannhalter C, Hellstern P. Coagulation factor XII (FXII) activity, activated FXII, distribution of FXII C46T gene polymorphism and coronary risk. J Thromb Haemost 2008;6:291–296. [DOI] [PubMed] [Google Scholar]
- 25. Lessiani G, Falco A, Nicolucci E, Rolandi G, Davi G. Deep venous thrombosis and previous myocardial infarction in mild factor XII deficiency: a risk factor for both venous and arterial thrombosis. J Thromb Thrombolysis 2009;27:348–351. [DOI] [PubMed] [Google Scholar]
- 26. Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 2011;32:1484–1492. [DOI] [PubMed] [Google Scholar]
- 27. Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biological Psych 2016;80:40–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Selander J, Bluhm G, Theorell T, Pershagen G, Babisch W, Seiffert I, Houthuijs D, Breugelmans O, Vigna-Taglianti F, Antoniotti MC, Velonakis E, Davou E, Dudley ML, Jarup L, Consortium H. Saliva cortisol and exposure to aircraft noise in six European countries. Environ Health Perspect 2009;117:1713–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Khanfer R, Lord JM, Phillips AC. Neutrophil function and cortisol:DHEAS ratio in bereaved older adults. Brain Behav Immun 2011;25:1182–1186. [DOI] [PubMed] [Google Scholar]
- 30. Maschke C, Rupp T, Hecht K. The influence of stressors on biochemical reactions – a review of present scientific findings with noise. Int J Hyg Environ Health 2000;203:45–53. [DOI] [PubMed] [Google Scholar]
- 31. Jarup L, Babisch W, Houthuijs D, Pershagen G, Katsouyanni K, Cadum E, Dudley ML, Savigny P, Seiffert I, Swart W, Breugelmans O, Bluhm G, Selander J, Haralabidis A, Dimakopoulou K, Sourtzi P, Velonakis M, Vigna-Taglianti F. Hypertension and exposure to noise near airports: the HYENA study. Environ Health Perspect 2008;116:329–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Babisch W, Ising H, Gallacher JEJ, Sweetnam PM, Elwood PC. Traffic noise and cardiovascular risk: the caerphilly and speedwell studies, third phase-10-year follow up. Arch Environ Health 1999;54:210–216. [DOI] [PubMed] [Google Scholar]
- 33. Dratva J, Phuleria HC, Foraster M, Gaspoz J-M, Keidel D, Künzli N, Liu LJS, Pons M, Zemp E, Gerbase MW, Schindler C. Transportation noise and blood pressure in a population-based sample of adults. Environ Health Perspect 2012;120:50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Carrington MJ, Trinder J. Blood pressure and heart rate during continuous experimental sleep fragmentation in healthy adults. Sleep 2008;31:1701–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lercher P, Widmann U, Kofler W. Transportation noise and blood pressure: the importance of modifying factors. Internoise 2000;4:1–5. [Google Scholar]
- 36. Barregard L, Sallsten G, Gustafson P, Andersson L, Johansson L, Basu S, Stigendal L. Experimental exposure to wood-smoke particles in healthy humans: effects on markers of inflammation, coagulation, and lipid peroxidation. Inhal Toxicol 2006;18:845–853. [DOI] [PubMed] [Google Scholar]
- 37. Tornqvist H, Mills NL, Gonzalez M, Miller MR, Robinson SD, Megson IL, Macnee W, Donaldson K, Soderberg S, Newby DE, Sandstrom T, Blomberg A. Persistent endothelial dysfunction in humans after diesel exhaust inhalation. Am J Respir Crit Care Med 2007;176:395–400. [DOI] [PubMed] [Google Scholar]
- 38. Peretz A, Peck EC, Bammler TK, Beyer RP, Sullivan JH, Trenga CA, Srinouanprachnah S, Farin FM, Kaufman JD. Diesel exhaust inhalation and assessment of peripheral blood mononuclear cell gene transcription effects: an exploratory study of healthy human volunteers. Inhal Toxicol 2007;19:1107–1119. [DOI] [PubMed] [Google Scholar]
- 39. Hiraiwa K, van Eeden SF. Contribution of lung macrophages to the inflammatory responses induced by exposure to air pollutants. Mediators Inflamm 2013;2013:619523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Goto Y, Ishii H, Hogg JC, Shih CH, Yatera K, Vincent R, van Eeden SF. Particulate matter air pollution stimulates monocyte release from the bone marrow. Am J Respir Crit Care Med 2004;170:891–897. [DOI] [PubMed] [Google Scholar]
- 41. Kampfrath T, Maiseyeu A, Ying Z, Shah Z, Deiuliis JA, Xu X, Kherada N, Brook RD, Reddy KM, Padture NP, Parthasarathy S, Chen LC, Moffatt-Bruce S, Sun Q, Morawietz H, Rajagopalan S. Chronic fine particulate matter exposure induces systemic vascular dysfunction via NADPH oxidase and TLR4 pathways. Circ Res 2011;108:716–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Deiuliis JA, Kampfrath T, Zhong J, Oghumu S, Maiseyeu A, Chen LC, Sun Q, Satoskar AR, Rajagopalan S. Pulmonary T cell activation in response to chronic particulate air pollution. Am J Physiol Lung Cell Mol Physiol 2012;302:L399–L409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rajagopalan S, Brook RD. Air pollution and type 2 diabetes: mechanistic insights. Diabetes 2012;61:3037–3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Liu C, Ying Z, Harkema J, Sun Q, Rajagopalan S. Epidemiological and experimental links between air pollution and type 2 diabetes. Toxicol Pathol 2013;41:361–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Simon SA, Liedtke W. How irritating: the role of TRPA1 in sensing cigarette smoke and aerogenic oxidants in the airways. J Clin Invest 2008;118:2383–2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dominici F, Peng RD, Ebisu K, Zeger SL, Samet JM, Bell ML. Does the effect of PM10 on mortality depend on PM nickel and vanadium content? A reanalysis of the NMMAPS data. Environ Health Perspect 2007;115:1701–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Liberda EN, Cuevas AK, Gillespie PA, Grunig G, Qu Q, Chen LC. Exposure to inhaled nickel nanoparticles causes a reduction in number and function of bone marrow endothelial progenitor cells. Inhal Toxicol 2010;22(Suppl. 2):95–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC Jr, Whitsel L, Kaufman JD, on behalf of the American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 2010;121:2331–2378. [DOI] [PubMed] [Google Scholar]
- 49. Ying Z, Xu X, Bai Y, Zhong J, Chen M, Liang Y, Zhao J, Liu D, Morishita M, Sun Q, Spino C, Brook RD, Harkema JR, Rajagopalan S. Long-term exposure to concentrated ambient PM2.5 increases mouse blood pressure through abnormal activation of the sympathetic nervous system: a role for hypothalamic inflammation. Environ Health Perspect 2014;122:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ying Z, Yue P, Xu X, Zhong M, Sun Q, Mikolaj M, Wang A, Brook RD, Chen LC, Rajagopalan S. Air pollution and cardiac remodeling: a role for RhoA/Rho-kinase. Am J Physiol Heart Circ Physiol 2009;296:H1540–H1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sun Q, Yue P, Ying Z, Cardounel AJ, Brook RD, Devlin R, Hwang J-SS, Zweier JL, Chen LC, Rajagopalan S. Air pollution exposure potentiates hypertension through reactive oxygen species-mediated activation of Rho/ROCK. Arterioscler Thromb Vasc Biol 2008;28:1760–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Mills NL, Tornqvist H, Robinson SD, Gonzalez M, Darnley K, MacNee W, Boon NA, Donaldson K, Blomberg A, Sandstrom T, Newby DE. Diesel exhaust inhalation causes vascular dysfunction and impaired endogenous fibrinolysis. Circulation 2005;112:3930–3936. [DOI] [PubMed] [Google Scholar]
- 53. Shah AP, Pietropaoli AP, Frasier LM, Speers DM, Chalupa DC, Delehanty JM, Huang LS, Utell MJ, Frampton MW. Effect of inhaled carbon ultrafine particles on reactive hyperemia in healthy human subjects. Environ Health Perspect 2008;116:375–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lund AK, Lucero J, Lucas S, Madden MC, McDonald JD, Seagrave JC, Knuckles TL, Campen MJ. Vehicular emissions induce vascular MMP-9 expression and activity associated with endothelin-1-mediated pathways. Arterioscler Thromb Vasc Biol 2009;29:511–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Peretz A, Sullivan JH, Leotta DF, Trenga CA, Sands FN, Allen J, Carlsten C, Wilkinson CW, Gill EA, Kaufman JD. Diesel exhaust inhalation elicits acute vasoconstriction in vivo. Environ Health Perspect 2008;116:937–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Mills NL, Tornqvist H, Gonzalez MC, Vink E, Robinson SD, Soderberg S, Boon NA, Donaldson K, Sandstrom T, Blomberg A, Newby DE. Ischemic and thrombotic effects of dilute diesel-exhaust inhalation in men with coronary heart disease. N Engl J Med 2007;357:1075–1082. [DOI] [PubMed] [Google Scholar]
- 57. Brook RD, Urch B, Dvonch JT, Bard RL, Speck M, Keeler G, Morishita M, Marsik FJ, Kamal AS, Kaciroti N, Harkema J, Corey P, Silverman F, Gold DR, Wellenius G, Mittleman MA, Rajagopalan S, Brook JR. Insights into the mechanisms and mediators of the effects of air pollution exposure on blood pressure and vascular function in healthy humans . Hypertension 2009;54:659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Mills NL, Robinson SD, Fokkens PH, Leseman DL, Miller MR, Anderson D, Freney EJ, Heal MR, Donovan RJ, Blomberg A, Sandstrom T, MacNee W, Boon NA, Donaldson K, Newby DE, Cassee FR. Exposure to concentrated ambient particles does not affect vascular function in patients with coronary heart disease. Environ Health Perspect 2008;116:709–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wold LE, Ying Z, Hutchinson KR, Velten M, Gorr MW, Velten C, Youtz DJ, Wang A, Lucchesi PA, Sun Q, Rajagopalan S. Cardiovascular remodeling in response to long-term exposure to fine particulate matter air pollution. Circ Heart Fail 2012;5:452–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Campen MJ, Lund A, Rosenfeld M. Mechanisms linking traffic-related air pollution and atherosclerosis. Curr Opin Pulmonary Med 2012;18:155–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Rao X, Zhong J, Maiseyeu A, Gopalakrishnan B, Villamena FA, Chen LC, Harkema JR, Sun Q, Rajagopalan S. CD36-dependent 7-ketocholesterol accumulation in macrophages mediates progression of atherosclerosis in response to chronic air pollution exposure. Circ Res 2014;115:770–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Tsou CL, Peters W, Si Y, Slaymaker S, Aslanian AM, Weisberg SP, Mack M, Charo IF. Critical roles for CCR2 and MCP-3 in monocyte mobilization from bone marrow and recruitment to inflammatory sites. J Clin Invest 2007;117:902–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Yin F, Lawal A, Ricks J, Fox JR, Larson T, Navab M, Fogelman AM, Rosenfeld ME, Araujo JA. Diesel exhaust induces systemic lipid peroxidation and development of dysfunctional pro-oxidant and pro-inflammatory high-density lipoprotein. Arterioscler Thromb Vasc Biol 2013;33:1153–1161. [DOI] [PubMed] [Google Scholar]
- 64. Li R, Navab K, Hough G, Daher N, Zhang M, Mittelstein D, Lee K, Pakbin P, Saffari A, Bhetraratana M, Sulaiman D, Beebe T, Wu L, Jen N, Wine E, Tseng CH, Araujo JA, Fogelman A, Sioutas C, Navab M, Hsiai TK. Effect of exposure to atmospheric ultrafine particles on production of free fatty acids and lipid metabolites in the mouse small intestine. Environ Health Perspect 2015;123:34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Sun Q, Wang A, Jin X, Natanzon A, Duquaine D, Brook RD, Aguinaldo JG, Fayad ZA, Fuster V, Lippmann M, Chen LC, Rajagopalan S. Long-term air pollution exposure and acceleration of atherosclerosis and vascular inflammation in an animal model. J Am Med Assoc 2005;294:3003–3010. [DOI] [PubMed] [Google Scholar]
- 66. Campen MJ, Lund AK, Knuckles TL, Conklin DJ, Bishop B, Young D, Seilkop S, Seagrave J, Reed MD, McDonald JD. Inhaled diesel emissions alter atherosclerotic plaque composition in ApoE(-/-) mice. Toxicol Appl Pharmacol 2010;242:310–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lund AK, Lucero J, Harman M, Madden MC, McDonald JD, Seagrave JC, Campen MJ. The oxidized low-density lipoprotein receptor mediates vascular effects of inhaled vehicle emissions. Am J Respir Crit Care Med 2011;184:82–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Nemmar A, Hoet PH, Dinsdale D, Vermylen J, Hoylaerts MF, Nemery B. Diesel exhaust particles in lung acutely enhance experimental peripheral thrombosis. Circulation 2003;107:1202–1208. [DOI] [PubMed] [Google Scholar]
- 69. Lucking AJ, Lundback M, Mills NL, Faratian D, Barath SL, Pourazar J, Cassee FR, Donaldson K, Boon NA, Badimon JJ, Sandstrom T, Blomberg A, Newby DE. Diesel exhaust inhalation increases thrombus formation in man. Eur Heart J 2008;29:3043–3051. [DOI] [PubMed] [Google Scholar]
- 70. Newby DE, Mannucci PM, Tell GS, Baccarelli AA, Brook RD, Donaldson K, Forastiere F, Franchini M, Franco OH, Graham I, Hoek G, Hoffmann B, Hoylaerts MF, Kunzli N, Mills N, Pekkanen J, Peters A, Piepoli MF, Rajagopalan S, Storey RF, on behalf of Esc Working Group on Thrombosis EAfCP, Rehabilitation and Association ESCHF. Expert position paper on air pollution and cardiovascular disease. Eur Heart J 2015;36:83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]