Abstract
This cross-sectional study tested social anxiety symptoms, trait mindfulness, and drinking to cope with social anxiety as potential predictors and/or serial mediators of drinking problems. A community-based sample of individuals with co-occurring social anxiety symptoms and alcohol dependence were recruited. Participants (N = 105) completed measures of social anxiety, drinking to cope with social anxiety, and alcohol use and problems. As well, participants completed the Five Facet Mindfulness Questionnaire, which assesses mindfulness facets of accepting without judgment, acting with awareness, not reacting to one’s internal experiences, observing and attending to experiences, and labeling and describing. As predicted, the relationship between social anxiety symptoms and drinking problems was mediated by social anxiety coping motives across each of the models. Further, the relationship between specific mindfulness facets (acting with awareness, accepting without judgment, and describe) and drinking problems was serially mediated by social anxiety symptoms and drinking to cope with social anxiety. This research builds upon existing studies that have largely been conducted with college students to evaluate potential mediators driving drinking problems. Specifically, individuals who are less able to act with awareness, accept without judgment, and describe their internal experiences may experience heightened social anxiety and drinking to cope with that anxiety, which could ultimately result in greater alcohol-related problems.
Keywords: social anxiety, drinking problems, mindfulness facets, alcohol dependence
Introduction
Research suggests that coping motives may be a critical mechanism linking social anxiety symptoms and correlates of alcohol use disorders. For example, among college students, coping motives have been shown to partially mediate the relationship between social anxiety and alcohol dependence symptoms (Ham, Zamboanga, Bacon, & Garcia, 2009). Further, research has found that drinking to reduce negative affect prospectively predicts the development of alcohol dependence among community participants (Carpenter & Hasin, 1998). Supporting these findings, a review of adolescent and young adult drinking motives and outcomes found that coping motives were significantly and positively associated with drinking problems (Kuntsche, Knibbe, Gmel, & Engels, 2005). Taken together, drinking to cope with negative affect may be a meaningful factor in understanding the development of alcohol dependence, particularly for individuals with social anxiety symptoms.
Indeed, there is considerable empirical support for the “tension-reduction hypothesis” or “self-medication” etiological model of alcohol use disorders, by which people develop alcohol use disorders because alcohol temporarily reduces negative affect (see discussion in Sher, Grekin, & Williams, 2005). Research implicating negative affect in the development and maintenance of substance use lends merit to the self-medication model (Cheetham, Allen, Yucel, & Lubman, 2010). At the same time, negative affective states, when considered in isolation, are not always strongly associated with drinking problems or consumption (Sher et al., 2005). Thus, it is necessary to consider what other factors may precipitate internally motivated drinking.
Theoretically, there is good reason to suspect that internally motivated drinking and correlates of alcohol dependence, such as alcohol-related problems, may be negatively associated with certain facets of trait mindfulness. Whereas mindfulness involves the ability to bring one’s full attention to the present moment without judgment (Kabat-Zinn, 1994), addiction can be conceptualized as an inability to accept the present moment coupled with a habitual drive to achieve the temporary relief or pleasure provided by indulging in substance use (Baer, 2003; Kavanagh, Andrade, & May, 2005; Marlatt, 1994). Further, there is evidence that alcohol-related problems may be differentially related to distinct facets of trait mindfulness, including: (a) accepting and not judging one’s experiences (Accepting without Judgment); (b) acting with awareness in the present moment (Acting with Awareness); (c) not reacting to one’s internal experiences (Nonreactivity); (d) observing and attending to experiences (Observe); and (e) labeling and describing (Describe; Baer, Smith, Krietemeyer, & Toney, 2006).
Testing the connection between mindfulness facets and correlates of alcohol use, Karyadi and Cyders (2015) exposed high risk, undergraduate social drinkers to pictures of alcohol to elicit alcohol cravings. Study findings indicated that accepting without judgment and acting with awareness were associated with less problematic alcohol use, and that describe was associated with lower cued alcohol cravings. The mindfulness facets of nonreactivity and observe were not significantly associated with factors related to drinking. Similarly, in a sample of college-aged students, the mindfulness facets of accepting without judgment, acting with awareness, and describing one’s internal states were significantly associated with drinking correlates, whereas nonreactivity and observe were not (Fernandez, Wood, Stein, & Rossi, 2010). Finally, in a clinical sample of individuals who had recently completed an outpatient program for substance use, severity of dependence was significantly, negatively associated with accepting without judgment, acting with awareness, and describing (Bowen & Enkema, 2014).
Building on this research, mindfulness-based therapeutic interventions have been successfully used for treating substance use disorders (Chiesa & Serretti, 2014). One example is Mindfulness Based Relapse Prevention (MBRP), which integrates components of cognitive behavioral relapse prevention with mindfulness practices (Bowen et al., 2014). MBRP has been associated with lower probability of heavy drinking and lower risk of relapse (Bowen et al., 2014), as well as lower rates of substance use and craving beyond 12-step based programs and psychoeducation-based treatment as usual (Bowen et al., 2009; Witkiewitz & Bowen, 2010). As another example, a 10-session mindfulness training adapted from Mindfulness-Based Cognitive Therapy was associated with decreased alcohol attention bias and physiological recovery from alcohol cues (Garland, Gaylord, Boettiger, & Howard, 2010). In fact, a recent review found that mindfulness based treatments were largely associated with reduced alcohol consumption (Chiesa & Serretii, 2014). The success of these interventions underscores the importance of testing why specific trait mindfulness facets may exert a positive therapeutic effect.
One factor that might help drive the positive therapeutic effect of specific mindfulness facets is a reduction in drinking to cope with negative affect. Indeed, Reynolds, Keough, and O’Connor (2015, p. 223) noted, “the antithesis of drinking to change one’s internal emotional state is to accept that state… Accepting without judgment leads to tolerance of unwanted internal experiences.” In other words, individuals who are less judgmental of their internal experiences may be better able to accept thoughts, emotions, and physiological sensations as impermanent, and consequently, may be better equipped to “ride the wave” of human experience. In fact, Reynolds et al. (2015) found that undergraduate students who were less judgmental of internal states and experiences reported less motivation to drink to reduce negative affect. This study also suggested that when individuals were better able to describe and label their internal experiences (i.e., the describe facet of mindfulness), they reported less coping motives to drink. Relatedly, in a study examining adults who reported at least one traumatic life event and alcohol use in the previous month, lower nonjudgmental acceptance significantly predicted higher coping motives (Vujanovic, Bonn-Miller, & Marlatt, 2011). Finally, in a recent cross-sectional study with college students, drinking to cope was negatively related to the mindfulness facets of accepting without judgment, acting with awareness, and describing (Roos, Brown, & Pearson, 2015). Importantly, drinking to cope mediated the relationships between each of these facets and drinking problems. Similarly, recent research suggests that the relationship between heightened negative affect and greater drinking to cope may indirectly flow through problems with emotional clarity (Veilleux, Skinner, Reese, & Shaver, 2014). Together, these findings suggest that lower levels of mindfulness facets—particularly the facets of accepting without judgment, acting with awareness, and describing—may contribute to individuals’ drinking to cope.
Mindfulness has also been associated with social anxiety symptoms both theoretically and empirically. Acceptance-based perspectives of social anxiety hold that in social anxiety-inducing contexts (e.g., social environments), socially anxious individuals will experience negative thoughts regarding social evaluation (Herbert & Cardaciotto, 2005). Subsequently, their attention toward internal experiences will increase, decreasing awareness of external cues. At this point, socially anxious individuals, who are less able to accept thoughts and experiences without judgment, will theoretically experience heightened social anxiety regarding their internal anxious state and social performance, increasing the likelihood of engaging in maladaptive coping mechanisms, such as substance abuse (Herbert & Cardaciotto, 2005). In contrast, individuals who are better able to accept their internal states without judgment will engage in less use of maladaptive coping strategies and experience reduced distress. Other facets of mindfulness may function in similar ways. For example, individuals who have difficulty acting with awareness in the present moment may become distracted by negative, self-focused attention, ultimately leading to greater social anxiety.
Supporting these theoretical links, mindfulness (measured as a unitary construct) has been negatively correlated with social anxiety symptoms among cross-sectional samples of undergraduate students (Rasmussen & Pidgeon, 2011) and individuals with clinical levels of social anxiety disorder (Schmertz, Masuda, & Anderson, 2012). Furthermore, Mindfulness Based Stress Reduction, which focuses on mindfulness training, or increasing flexible and nonjudgmental attention, has been shown to successfully reduce social anxiety symptoms (e.g., Goldin, Ramel, & Gross, 2009; Jazaieri, Goldin, Werner, Ziv, & Gross, 2012; Kabat-Zinn, 1990; Kocovski, Fleming, & Rector, 2009).
There has been very little research investigating the relationship between social anxiety symptoms and specific facets of trait mindfulness. Notwithstanding, Parsons et al. (2015) recently found that specific mindfulness facets, as measured by the Five Facet Mindfulness Questionnaire (Baer et al., 2006), were significantly correlated with measures of social anxiety symptoms and responses to a social anxiety stressor among a sample of undergraduate students. Specifically, remaining nonjudgmental and nonreactive toward internal experiences, acting with awareness in the present moment, and having the ability to label and describe one’s internal experiences were negatively related to both trait and state aspects of social anxiety symptoms (see also Desrosiers, Klemanski, & Nolen-Hoeksema, 2013).
Finally, there is compelling evidence that anxiety disorders, including social anxiety disorder, predates the development of alcohol use disorders (for reviews, see: Buckner, Heimberg, Ecker, & Vinci, 2013; Kushner, Krueger, Frye, & Peterson, 2008; Smith & Randall, 2012). Further, prior work suggests that drinking to cope with social anxiety mediates the relationship between symptoms of social anxiety and drinking problems (Buckner & Heimberg, 2010), and that coping motives mediate the relationship between trait mindfulness facets and drinking problems (Roos et al., 2015). However, there is not strong empirical precedent to guide whether social anxiety symptoms predate trait mindfulness facets, or whether trait mindfulness facets predate symptoms of social anxiety.
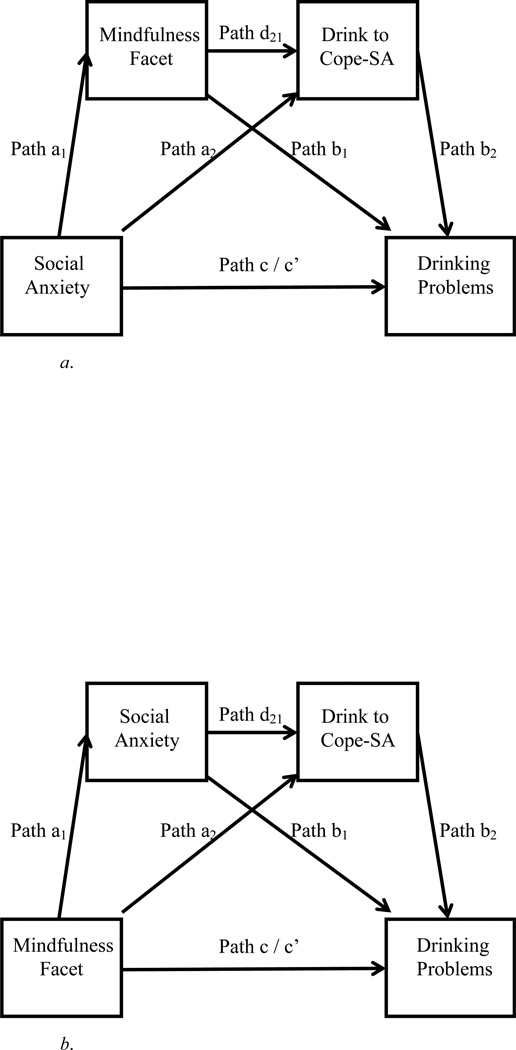
The goal of the present study was to test social anxiety symptoms, trait mindfulness facets, and drinking to cope with social anxiety as potential predictors and mediators driving alcohol-related problems. First, we tested whether the relationship between social anxiety symptoms and drinking problems indirectly flowed through trait mindfulness facets and drinking to cope with social anxiety acting in serial (Figure 1a). In other words, we tested whether the association between social anxiety and drinking problems flowed first through specific mindfulness facets, and then through drinking to cope with social anxiety. We expected that greater social anxiety symptoms would predict a diminished ability to accept without judgment, which in turn was expected to predict greater coping motives to drink. Ultimately, less acceptance without judgment and greater drinking to cope, acting in serial, were hypothesized to result in greater drinking problems. We expected a similar pattern of relationships for the acting with awareness and describe facets. Second, we tested whether the relationship between trait mindfulness facets and drinking problems indirectly flowed through social anxiety symptoms and drinking to cope with social anxiety acting in serial (Figure 1b). Similar to the previous model, we predicted that greater nonjudgmental acceptance would predict less social anxiety symptoms, which in turn would predict less drinking to cope, and less drinking problems. We expected a similar pattern of relationships for the acting with awareness and describe facets.
Figure 1.
a. Hypothesized Serial Multiple Mediation Model with Social Anxiety as the Predictor Variable.
b. Hypothesized Serial Multiple Mediation Model with Trait Mindfulness as Predictor Variable.
Method
Participants
This study was a secondary data analysis of participants drawn from a broader attention bias modification intervention trial (Clerkin, Magee, Wells, Beard, & Barnett, 2016). See Table 1 for detailed sample characteristics. Individuals were eligible to participate in the trial if during an initial phone screen they 1) were ≥ 18 years old; 2) met diagnostic criteria for current alcohol dependence as assessed by the Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., 1998); 3) reported elevated social anxiety symptoms (i.e., scores of ≥ 30 on the experimenter-administered Liebowitz Social Anxiety Scale; Mennin et al., 2002); 4) reported willingness to decrease their drinking; and 5) spoke English and indicated that they could read. Participants were excluded from participation if during an initial phone screen they 1) screened positive for current psychotic or manic symptoms; 2) demonstrated significant cognitive impairment; 3) reported drug use other than nicotine or marijuana within the past month; 4) were currently receiving cognitive-behavioral therapy for social anxiety or an alcohol use disorder; and 5) had been taking a psychotropic medication for less than six weeks. At the time of written informed consent, participants’ Breath Alcohol Content (BrAC) needed to be < .02.
Table 1.
Descriptive Statistics and Sample Characteristics
| Sample Characteristics | Raw M (SD) range or % N = 105 |
|
|---|---|---|
| Age (years) | 43.14 (11.59) | |
| Sex | ||
| Male | 57.1% | |
| Female | 42.9% | |
| Education | ||
| Some High School or Less | 7.6% | |
| High School Graduate | 32.4% | |
| Some College | 31.4% | |
| Associates/Bachelors Degree | 23.8% | |
| Masters Degree | 2.9% | |
| Doctorate/Professional Degree | 1.9% | |
| Race | ||
| American Indian/Alaska Native | 1.9% | |
| Asian | 1.0% | |
| Black/African American | 51.4% | |
| White | 39.0% | |
| Multiracial | 5.7% | |
| Other | 1.0% | |
| Social Anxiety Symptoms | ||
| Social Anxiety Composite | 35.95 (14.24) | |
| Liebowitz Social Anxiety Scale | 73.42 (25.48) | |
| Social Interaction Anxiety Scale – 17 item | 31.34 (14.09) | |
| Social Phobia Scale | 30.20 (16.35) | |
| Alcohol Related Measures | ||
| Drinker Inventory of Consequences | 41.47 (26.59) | |
| Daily Drinking Questionnaire | 30.13 (25.44) | |
| Alcohol Withdrawal Symptom Checklist | 16.40 (10.14) | |
| Social Anxiety Coping Motives | ||
| Drink to Cope with Social Anxiety (DTC-SA) | 5.96 (2.08) | |
| Depression Symptoms | ||
| Center for Epidemiologic Studies Depression | 28.09 (11.09) | |
| Scale | ||
| Raw M (SD) N = 77 |
||
| Mindfulness Facets | ||
| Accepting without Judgment | 24.44 (6.08) | |
| Acting with Awareness | 25.65 (6.94) | |
| Nonreactivity | 19.79 (4.19) | |
| Observe | 26.43 (5.92) | |
| Describe | 25.82 (6.08) | |
Note. Raw values of the Daily Drinking Questionnaire are included in the table for descriptive purposes. All questionnaire measures reflect scores reported during the baseline assessment.
The current study used data from the baseline assessment of the trial, which was collected prior to the intervention. To ensure current drinking problems, participants were excluded from analyses if they reported that they had consumed alcohol during the preceding month either “never” or “less than once per month” (n = 6). To ensure current social anxiety symptoms, participants were also excluded from analyses in the present study if at baseline, they scored more than 2 SD below the mean of a sample diagnosed with social phobia on the LSAS (Heimberg et al., 1999; LSAS range in current study: 24 – 133), or if they did not report any symptoms of social anxiety on either of the other two trait measures of social anxiety (n = 4). This resulted in a final sample of 105 participants.
Procedure
A community-based sample of individuals with co-occurring social anxiety symptoms and alcohol dependence were recruited. Only measures relevant to the current study are included here. See Clerkin et al. (2016) for more information.
Measures
The Mini-International Neuropsychiatric Interview English Version 5.0 for DSM-IV (MINI; Sheehan et al., 1998) was used to evaluate inclusion and exclusion criteria. Participants in the present study all screened positive for alcohol dependence on the MINI, which assesses symptoms of alcohol dependence during the preceding 12 months.
Drinking problems
The Drinker Inventory of Consequences measure (DrInC; Miller, Tonigan, & Longabaugh, 1995) assesses drinking problems in five domains during the previous month: physical, intrapersonal, social responsibility, interpersonal, and impulse control. In the present study, we evaluated how often participants experienced drinking problems in the past month (on a 4-point scale from “never” to “daily or almost daily”). The DrInC has been found to be a reliable and valid assessment of drinking problems (Forcehimes, Tonigan, Miller, Kenna, & Baer, 2007). Participants were also asked to indicate whether they had “ever” experienced each problem. Those who indicated “No” for these items received a score of “0” for the past month items. In the current sample, the measure demonstrated excellent reliability (α = .96).
Alcohol consumption
The calendar-based Daily Drinking Questionnaire (Collins, Parks, & Marlatt, 1985) was used to evaluate weekly alcohol consumption. To minimize error, participants were provided with a definition of a standard drink (e.g., 12 ounces, or one can or bottle of beer; 5 ounce glass of wine, etc.), and a calendar was used to help orient participants to the previous week. Then, participants were asked to report verbally how much alcohol (measured in number of standard drinks) they drank each day during the previous week, as well as during an “average” day during the previous month. The research assistant recorded each daily standard drink number reported by the participant, checking for each answer that the participant was reporting standard drinks and converting the number to standard drink units if necessary. Consumption (i.e., total drinks per week) was analyzed in the current study.
Social anxiety
Our key measures of social anxiety symptoms were: 1) the experimenter rated Liebowitz Social Anxiety Scale (LSAS; Liebowitz, 1987; α = .96); 2) the self-reported 17-item Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998; Rodebaugh, Woods, & Heimberg, 2007; α = .93); and 3) the self-reported 20-item Social Phobia Scale (SPS; Mattick & Clarke, 1998; α = .94). The three measures of social anxiety were significantly inter-correlated (N = 105; r range: .67 - .79). The LSAS and SIAS-17 were transformed to be on the same scale as the SPS (i.e., each LSAS score was multiplied by a constant of 5/9, and each SIAS-17 score was multiplied by a constant of 20/17, resulting in a total score of 80 for all three measures). Then an average of the measures was taken to compute our key measure of social anxiety symptoms, referred to as Social Anxiety Composite.
Mindfulness
Mindfulness facets were measured using the Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006). This measure uses a 5-point scale to assess five facets of mindfulness: (a) Accepting without Judgment, or accepting one’s experiences without judgment (e.g., “I tell myself I shouldn’t be feeling the way I’m feeling” – reverse scored); (b) Acting with Awareness, or giving one’s full attention to the present moment while redirecting one’s attention from distractions (e.g., “I find it difficult to stay focused on what’s happening in the present moment” – reverse scored); (c) Nonreactivity, or not reacting to one’s internal experiences (e.g., “I perceive my feelings and emotions without having to react to them”); (d) Observe, or observing and attending to experiences (e.g., “When I’m walking, I deliberately notice the sensations of my body moving”); and (e) Describe, or labeling and describing (e.g., “I’m good at finding words to describe my feelings”). Reliability for each facet was good to excellent in the current sample (Accepting without Judgment: α = .84; Acting with Awareness: α = .89; Nonreactivity: α = .70; Observe: α = .77; Describe: α = .84).
Drinking to cope with social anxiety
An adaptation of the Drink to Cope (referred to here as “drinking to cope with social anxiety” or DTC-SA; Thomas, Randall, & Carrigan, 2003) was used to assess participants’ use of alcohol as a means of coping with their social anxiety. The following items were used to create a composite DTC-SA score: 1) What percentage of the time would you use alcohol to feel more comfortable or less anxious in social situations where alcohol is available? (0% to 100%; recoded 0 to 10); 2) What percentage of the time do you drink before engaging in a social situation (0% to 100%; recoded 0 to 10); 3) What percentage of the time do you drink after engaging in a social situation (0% to 100%; recoded 0 to 10); and 4) How much does alcohol relieve your anxiety or discomfort in social situations (0, “not at all”, to 10, “completely”). Participants were also asked to indicate whether they ever drank during, before, or after social situations. Those who indicated “No” for these items received a score of “0” on items 1–3 of the DTC-SA, respectively. The reliability of the DTC-SA in the current sample was good (α = .73).
Additional Measures
The Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977), which assesses symptoms of depression, and the Alcohol Withdrawal Symptom Checklist (AWSC; Pittman et al., 2007), which assesses the severity of a variety of alcohol symptoms within the last 24 hours, were included to better characterize the sample. Reliability for these measures was good to excellent in the current sample (CES-D: α = .89; AWSC: α = .88).
Data Analyses
Serial mediation models were tested following contemporary guidelines for conducting mediation analyses, which emphasize testing hypothesized indirect effects, as opposed to individual pathways (Hayes, 2013). See Figures 1a and 1b. For each set of models, each mindfulness facet was tested in a separate model, but models were otherwise identical. Drinking Consumption was initially considered as a covariate in primary mediation models, but was dropped because the pattern of findings for key indirect effects were the same whether consumption was included or not (a minor deviation from this pattern is noted in Table 3b).
Table 3.
Mindfulness Facet as Predictor: Unstandardized Regression Coefficients, Standard Errors, Standardized Regression Coefficients, and Indirect Effects
| A. Accepting Without Judgment → Social Anxiety → Drinking to Cope → Drinking Problems Model | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (Social Anxiety) |
M2 (DTC-SA) |
Y (Drinking Problems) |
|||||||||||||
| b | SE | p | β | b | SE | p | β | b | SE | p | β | ||||
| X (Accepting Without Judgment) |
a1 | −1.07 | .23 | <.01 | −.45 | a2 | .02 | .04 | .68 | .05 | c’ | −.35 | .40 | .39 | −.08 |
| M1 (Social Anxiety) | -- | -- | -- | -- | d21 | .06 | .02 | <.01 | .43 | b1 | .53 | .19 | <.01 | .29 | |
| M2 (DTC-SA) | -- | -- | -- | -- | -- | -- | -- | -- | b2 | 3.34 | 1.44 | .02 | .26 | ||
| Total Effect (c) | |||||||||||||||
| b = −1.08, SE = .40, p =.007, β= −.25 | |||||||||||||||
| Specific Indirect Effects | |||||||||||||||
| 1. Accepting without judgment → Social anxiety symptoms → Drinking problems Estimate = −.57, SE = .22, 95% CI (−1.07, −.21), PM = .52 | |||||||||||||||
| 2. Accepting without judgment → Drinking to cope with social anxiety → Drinking problems Estimate = .05, SE = .15, 95% CI (−.21, .43), PM = −.05 | |||||||||||||||
| 3. Accepting without judgment → Social anxiety symptoms → Drinking to Cope with social anxiety → Drinking problems Estimate = −.22, SE = .11, 95% CI (−.52, −.05), PM = .20 | |||||||||||||||
| B. Acting with Awareness → Social Anxiety → Drinking to Cope → Drinking Problems Model | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (Social Anxiety) |
M2 (DTC-SA) |
Y (Drinking Problems) |
|||||||||||||
| b | SE | p | β | B | SE | p | β | B | SE | p | β | ||||
| X (Acting with Awareness) |
a1 | −1.15 | .20 | <.01 | −.55 | a2 | −.04 | .04 | .33 | −.13 | c’ | −.35 | .43 | .41 | −.09 |
| M1 (Social Anxiety) | -- | -- | -- | -- | d21 | .05 | .02 | <.01 | .34 | b1 | .51 | .20 | .01 | .28 | |
| M2 (DTC-SA) | -- | -- | -- | -- | -- | -- | -- | -- | b2 | 3.17 | 1.46 | .03 | .25 | ||
| Total Effect (c) | |||||||||||||||
| b = −1.23, SE = .38, p =.001, β= −.32 | |||||||||||||||
| Specific Indirect Effects | |||||||||||||||
| 1. Acting with awareness → Social anxiety symptoms → Drinking problems Estimate -.59, SE = .25, 95% CI (−1.13, −.17), PM = .47 | |||||||||||||||
| 2. Acting with awareness → Drinking to cope with social anxiety → Drinking problems Estimate = −.12, SE = .15, 95% CI (−.53, .08), PM = .10 | |||||||||||||||
| 3. Acting with awareness → Social anxiety symptoms → Drinking to Cope with social anxiety → Drinking problems Estimate = −.18, SE = .12, 95% CI (−.53, −.03), PM = .14 | |||||||||||||||
| C. Describe → Social Anxiety → Drinking to Cope → Drinking Problems Model | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (Social Anxiety) |
M2 (DTC-SA) |
Y (Drinking Problems) |
|||||||||||||
| b | SE | p | β | b | SE | p | β | b | SE | p | β | ||||
| X (Describe) | a1 | −.78 | .30 | <.01 | −.33 | a2 | −.02 | .04 | .63 | −.05 | c’ | −.63 | .49 | .20 | −.14 |
| M1 (Social Anxiety) | -- | -- | -- | -- | d21 | .06 | .02 | <.01 | .40 | b1 | .52 | .19 | <.01 | .28 | |
| M2 (DTC-SA) | -- | -- | -- | -- | -- | -- | -- | -- | b2 | 3.20 | 1.46 | .03 | .25 | ||
| Total Effect (c) | |||||||||||||||
| b = −1.22, SE = .56, p = . 03, β =-.28 | |||||||||||||||
| Specific Indirect Effects | |||||||||||||||
| 1. Describe → Social anxiety symptoms → Drinking problems Estimate -.40, SE = .19, 95% CI (−.89, −.12), PM = .33 | |||||||||||||||
| 2. Describe → Drinking to cope with social anxiety → Drinking problems Estimate = −.05, SE = .12, 95% CI (−.36, .15), PM = .04 | |||||||||||||||
| 3. Describe → Social anxiety symptoms → Drinking to Cope with social anxiety → Drinking problems Estimate = −.14, SE = .09, 95% CI (−.44, −.02), PM = .11 | |||||||||||||||
Note. The pattern of findings for the specific indirect effects were the same when consumption was included as a covariate. However, for the third indirect effect (Acting with awareness → Social anxiety symptoms → Drinking to cope with social anxiety → Drinking problems), the 95% bias-corrected confidence interval crossed zero (Estimate = −.10, SE = .08, 95% CI [−.37, .001], 90% CI [−.31, −.01], PM = .10).
Individual pathways and indirect effects were evaluated using Mplus version 7 (Muthén & Muthén, 1998–2015). Ten thousand bootstrap samples were used in each test of the indirect effect. Each model contained bias-corrected bootstrap confidence intervals for three specific indirect effects: 1) Paths a1 → b1; 2) Paths a2 → b2; 3) Paths a1 → d21 → b2 (the serial mediation indirect effect; see Figures 1a and 1b). Statistical significance was determined by 95% bias-corrected bootstrap unstandardized confidence intervals that did not overlap with zero. Finally, the ratio of the indirect effect to the total effect (PM) was reported as an effect size measure.
Results
See Table 1 for descriptive statistics and sample characteristics. A square root transformation was conducted on Drinking Consumption. This helped to maximize the normality of the distribution, minimize the influence of potential outliers, and minimize violations of OLS regression assumptions.
Of the 105 participants, 28 (26.7%) did not receive the FFMQ because this measure was added to the study protocol after data collection was underway. There were no significant group differences between individuals who were administered the FFMQ (vs. not) on any variables included in the serial mediation model (Social Anxiety Composite, DTC-SA, or Drinking Problems; all p > .10), on drinking Consumption and alcohol withdrawal symptoms (both p > .10), or on most demographic variables (Age, Sex, Race, Ethnicity, Marital Status; all p > .05). There was a significant group difference between those who received the FFMQ (vs. not) on Educational Status (assessed with a Linear-by-Linear Association = 4.71, p = .03), as well as on depressive symptoms (CESD; p = .05). When compared to those who were not administered the FFMQ, those administered the FFMQ had lower CESD scores and higher levels of education.
Listwise deletion of missing data has been found to bias results and reduce statistical power (Jelicic, Phelps, & Lerner, 2009; Widaman, 2006). Further, according to Graham (2009, pp. 559–560), multiple imputation and maximum likelihood methods are “always at least as good as the old procedures (e.g., listwise deletion, except in artificial, unrealistic circumstances), and MI/ML methods are typically better than old methods, and often very much better.” This is true even when the missing at random assumption has been violated, and with significant amounts of missing data (Graham, 2009; Graham & Schafer, 1999). Thus, following modern recommendations to handle missing data, missing data in the first set of mediation models, with social anxiety as the predictor, were addressed using full information maximum likelihood (FIML) estimation. Because full information maximum likelihood cannot be used to estimate missing values on the predictor variable, the sample size for analyses when the mindfulness facet was the predictor was 77.
Social Anxiety as Predictor
As reflected in Table 2, across each model, neither of the hypothesized mediation pathways involving the mindfulness facets were significant (social anxiety symptoms → mindfulness facet → drinking problems; social anxiety symptoms → mindfulness facet → drinking to cope → drinking problems). However, consistent with prior research, across each model, individuals with greater social anxiety symptoms were more likely to drink to cope with social anxiety (pathway a2), and individuals who were more likely to drink to cope with social anxiety were more likely to experience greater drinking problems (pathway b2). Critically, there was a significant indirect effect of social anxiety symptoms on drinking problems via coping motives for each model, indicating that drinking to cope with social anxiety functioned as a mediator of the relationship between social anxiety symptoms and drinking problems.
Table 2.
Social Anxiety as Predictor: Unstandardized Regression Coefficients, Standard Errors, Standardized Regression Coefficients, and Indirect Effects
| A. Social Anxiety → Accepting Without Judgment → Drinking to Cope → Drinking Problems Model | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (Accepting Without Judgment) |
M2 (DTC-SA) |
Y (Drinking Problems) |
|||||||||||||
| b | SE | p | β | b | SE | p | β | b | SE | p | β | ||||
| X (Social Anxiety) | a1 | −.19 | .04 | <.01 | −.44 | a2 | .07 | .01 | <.01 | .49 | c’ | .35 | .18 | .06 | .19 |
| M1 (Accepting without Judgment) |
-- | -- | -- | -- | d21 | .02 | .04 | .71 | .04 | b1 | −.38 | .43 | .38 | −.09 | |
| M2 (DTC-SA) | -- | -- | -- | -- | -- | -- | -- | -- | b2 | 3.73 | 1.23 | <.01 | .29 | ||
| Total Effect (c) | |||||||||||||||
| b = .67, SE = .17,p < .001, β =.36 | |||||||||||||||
| Specific Indirect Effects | |||||||||||||||
| 1. Social anxiety symptoms → Accepting Without Judgment → Drinking problems Estimate = .07, SE = .08, 95% CI (−.08, .25), PM = .10 | |||||||||||||||
| 2. Social anxiety symptoms → Drinking to cope with social anxiety → Drinking problems Estimate = .27, SE = .10, 95% CI (.11, .49), PM = .40 | |||||||||||||||
| 3. Social anxiety symptoms → Accepting Without Judgment → Drinking to Cope with social anxiety → Drinking problems Estimate = −.01, SE = .03, 95% CI (−.07, .05), PM = −.01 | |||||||||||||||
| B. Social Anxiety → Acting with Awareness → Drinking to Cope → Drinking Problems Model | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (Acting with Awareness) |
M2 (DTC-SA) |
Y (Drinking Problems) |
|||||||||||||
| b | SE | p | β | b | SE | p | β | b | SE | p | β | ||||
| X (Social Anxiety) | a1 | −.26 | .04 | <.01 | −.54 | a2 | .06 | .02 | <.01 | .40 | c’ | .33 | .20 | .09 | .18 |
| M1 (Acting with Awareness) |
-- | -- | -- | -- | d21 | −.04 | .04 | .33 | −.12 | b1 | −.38 | .45 | .40 | −.10 | |
| M2 (DTC-SA) | -- | -- | -- | -- | -- | -- | -- | -- | b2 | 3.54 | 1.25 | <.01 | .28 | ||
| Total Effect (c) | |||||||||||||||
| b = .67, SE = .17, p <.001, β =.36 | |||||||||||||||
| Specific Indirect Effects | |||||||||||||||
| 1. Social anxiety symptoms → Acting with awareness → Drinking problems Estimate = .10, SE = .12, 95% CI (−.14, .34), PM = .15 | |||||||||||||||
| 2. Social anxiety symptoms → Drinking to cope with social anxiety → Drinking problems Estimate = .21, SE = .09, 95% CI (.07, .45), PM = .31 | |||||||||||||||
| 3. Social anxiety symptoms → Acting with awareness → Drinking to Cope with social anxiety → Drinking problems Estimate = .04, SE = .04, 95% CI (−.02, .14), PM = .05 | |||||||||||||||
| C. Social Anxiety → Nonreactivity → Drinking to Cope → Drinking Problems Model | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (NonReact) |
M2 (DTC -SA) |
Y (Drinking Problems) |
|||||||||||||
| b | SE | p | β | b | SE | p | β | b | SE | p | β | ||||
| X (Social Anxiety) | a1 | .02 | .04 | .62 | .06 | a2 | .07 | .01 | <.01 | .47 | c’ | .44 | .17 | .01 | .24 |
| M1 (NonReact) | -- | -- | -- | -- | d21 | −.02 | .05 | .65 | −.05 | b1 | −.79 | .66 | .23 | −.13 | |
| M2 (DTC-SA) | -- | -- | -- | -- | -- | -- | -- | -- | b2 | 3.58 | 1.25 | <.01 | .28 | ||
| Total Effect (c) | |||||||||||||||
| b = .67, SE = .17, p < .001, β= .36 | |||||||||||||||
| Specific Indirect Effects | |||||||||||||||
| 1. Social anxiety symptoms → Nonreactivity → Drinking problems Estimate = −.01, SE = .04, 95% CI (−.14, .03), PM = −.02 | |||||||||||||||
| 2. Social anxiety symptoms → Drinking to cope with social anxiety → Drinking problems Estimate = .25, SE = .09, 95% CI (.09, .46), PM = .37 | |||||||||||||||
| 3. Social anxiety symptoms → Nonreactivity → Drinking to Cope with social anxiety → Drinking problems Estimate = −.001, SE = .008, 95% CI (−.03, .007), PM = −.001 | |||||||||||||||
| D. Social Anxiety → Observe → Drinking to Cope → Drinking Problems Model | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (Observe) |
M2 (DTC -SA) |
Y (Drinking Problems) |
|||||||||||||
| b | SE | p | β | b | SE | p | β | b | SE | p | β | ||||
| X (Social Anxiety) | a1 | .06 | .05 | .22 | .14 | a2 | .07 | .01 | <.01 | .47 | c’ | .45 | .17 | <.01 | .24 |
| M1 (Observe) | -- | -- | -- | -- | d21 | −.003 | .03 | .93 | −.009 | b1 | −.51 | .42 | .22 | −.11 | |
| M2 (DTC-SA) | -- | -- | -- | -- | -- | -- | -- | -- | b2 | 3.66 | 1.25 | <.01 | .29 | ||
| Total Effect (c) | |||||||||||||||
| b = .67, SE = .17, p < .001,(3 =.36 | |||||||||||||||
| Specific Indirect Effects | |||||||||||||||
| 1. Social anxiety symptoms → Observe → Drinking problems Estimate = −.03, SE = .04 , 95% CI (−.15, .01), PM = −.04 | |||||||||||||||
| 2. Social anxiety symptoms → Drinking to cope with social anxiety → Drinking problems Estimate = .25, SE = .09, 95% CI (.10, .47), PM = .37 | |||||||||||||||
| 3. Social anxiety symptoms → Observe → Drinking to Cope with social anxiety → Drinking problems Estimate = −.001, SE = .009, 95% CI (−.02, .03), PM = −.001 | |||||||||||||||
| E. Social Anxiety → Describe → Drinking to Cope → Drinking Problems Model | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (Describe) |
M2 (Drinking to Cope) |
Y (Drinking Problems) |
|||||||||||||
| b | SE | p | β | b | SE | p | β | b | SE | p | β | ||||
| X (Social Anxiety) | a1 | −.13 | .05 | <.01 | −.31 | a2 | .07 | .01 | <.01 | .45 | c’ | .34 | .18 | .07 | .18 |
| M1 (Describe) | -- | -- | -- | -- | d21 | −.02 | .04 | .61 | −.05 | b1 | −.68 | .52 | .19 | −.15 | |
| M2 (Drinking to Cope) |
-- | -- | -- | -- | -- | -- | -- | -- | b2 | 3.56 | 1.26 | <.01 | .28 | ||
| Total Effect (c) | |||||||||||||||
| b = .67, SE = .17, p <.001, β =.36 | |||||||||||||||
| Specific Indirect Effects | |||||||||||||||
| 1. Social anxiety symptoms → Describe → Drinking problems Estimate = .09, SE = .09, 95% CI (−.02, .32), PM = .13 | |||||||||||||||
| 2. Social anxiety symptoms → Drinking to cope with social anxiety → Drinking problems Estimate = .24, SE = .10, 95% CI (.08, .47), PM = .35 | |||||||||||||||
| 3. Social anxiety symptoms → Describe → Drinking to Cope with social anxiety → Drinking problems Estimate = .008, SE = .02, 95% CI (−.02, .07), PM = .01 | |||||||||||||||
Pointing to the robustness of these findings, the pattern for the specific indirect effects was the same across all five models when just evaluating participants who had received the FFMQ (N = 77), as well as when consumption was included as a covariate. Further, when all mindfulness facets were included in a single model, there was still a significant indirect effect of social anxiety symptoms on drinking problems via coping motives (Estimate = .22, SE = .10, 95% CI [.08, .49], PM = .33), but none of the other specific indirect effects were significant.
Mindfulness Facets as Predictors
As depicted in Table 3, as expected, there were significant indirect effects of accepting without judgment on drinking problems via social anxiety symptoms and via social anxiety symptoms and drinking to cope with social anxiety acting in serial. Similarly, as expected, there were significant indirect effects of acting with awareness on drinking problems via social anxiety symptoms and via social anxiety symptoms and drinking to cope with social anxiety acting in serial. Finally, as expected, there were significant indirect effects of describe on drinking problems via social anxiety symptoms and via social anxiety symptoms and drinking to cope with social anxiety acting in serial. The total effect between both of the other mindfulness facets (Nonreactivity, Observe) and drinking problems were nonsignificant (ps > .10). Further, there were not significant indirect effects in the Nonreactivity or Observe models.
Pointing to the robustness of the key indirect effect findings, when all of the mindfulness facets were included simultaneously in a single model, the pattern was very similar. Over and above the other facets of mindfulness, there were still significant indirect effects of acting with awareness on drinking problems via social anxiety symptoms (Estimate = −.33, SE = .22, 95% CI [−.93, −.02], PM = .47) and via social anxiety symptoms and drinking to cope with social anxiety acting in serial (Estimate = −.12, SE = .09, 95% CI [−.45, −.02], PM = .18). Similarly, there were still significant indirect effects of describe on drinking problems via social anxiety symptoms (Estimate = −.24, SE = .17, 95% CI [−.71, −.003], PM = .33) and via social anxiety symptoms and drinking to cope with social anxiety acting in serial (Estimate = −.09, SE = .07, 95% CI [−.31, −.007], PM = .12), over and above the other facets of mindfulness. Further, there was still a significant indirect effect of accepting without judgment on drinking problems via social anxiety symptoms and drinking to cope with social anxiety acting in serial (Estimate = −.08, SE = .07, 95% CI [−.33, −.001], PM = .11), when controlling for the other facets of mindfulness. The specific indirect effect of accepting without judgment on drinking problems via social anxiety (Estimate = −.22, SE = .19, 95% CI [−.78, .01)] 90% CI [−.69, −.01], PM = .29) trended toward but did not reach statistical significance, when controlling for the other facets of mindfulness.
Discussion
Prior research has separately tested most of the specific links evaluated here. However, to our knowledge, this study provided the first test of each of these links operating together. The current findings advance prior work conducted largely with college students by suggesting that even in a sample with diagnosed alcohol dependence, individuals with greater social anxiety may experience greater drinking problems in part because they drink to cope with their social anxiety. Further, by testing a series of models that varied which variable was the predictor versus mediator, findings highlight the ways in which specific trait mindfulness facets and social anxiety symptoms may work together to drive alcohol use disorders.
Given that there was not strong empirical precedent to guide whether social anxiety symptoms predate trait mindfulness facets, or whether trait mindfulness facets predate symptoms of social anxiety, we tested two competing sets of models: one set in which social anxiety was the predictor, and another set in which the trait mindfulness facets were the predictor. Results suggested that low trait mindfulness may be the initial risk factor that leads to elevated social anxiety symptoms, followed by enhanced drinking to cope with social anxiety, and subsequent drinking problems. More specifically, findings expanded upon prior work in which accepting without judgment, acting with awareness, and describe were each associated with correlates of drinking (Bowen & Enkema, 2014; Fernandez et al., 2010; Karyadi & Cyders, 2015; Reynolds et al., 2015) and social anxiety symptoms (Parsons et al., 2015), and work suggesting that drinking to cope mediated the relationship between these trait mindfulness facets and drinking problems (Roos et al. 2015). In particular, we found that there was a significant indirect effect between each of these trait mindfulness facets (accepting without judgment, acting with awareness, and describe) and drinking problems via social anxiety symptoms and drinking to cope with social anxiety acting in serial.
In the context of the current study, it may be that individuals with greater ability to accept without judgment, act with awareness, and describe were better able to engage in the types of self-monitoring that allow one to make more adaptive choices in “hot” situations (see similar discussion in Reynolds et al., 2015). For instance, according to Wiers et al. (2010), there is often a conflict between one’s “cold,” or rational attitudes and beliefs about health risk behaviors (e.g., “it is stupid to drink 10 drinks in a night”), and one’s actual behavioral impulses in “hot,” or “tempting,” situations (e.g., “drinking will be my ‘social lubricant’ and help me get through this night”). If someone is able to act with awareness, or label and accept their internal experiences without judgment, they may be able to mindfully act and choose different responses other than drinking to manage their social anxiety (e.g., leave the party, engage in slow breathing). Consequently, they might be able to halt more automatic, spontaneous impulses to more fully consider the situation, and potentially limit the types of drinking known to lead to greater problems (e.g., drinking to cope with social anxiety).
Consistent with prior research (e.g., Buckner & Heimberg, 2010; Ham et al., 2009) and existing, cognitive-behavioral approaches (McCrady, 2008), findings from this study support the traditional focus of CBT on enhancing coping abilities to manage negative affect. Indeed, the finding that social anxiety coping motives mediated the relationship between social anxiety symptoms and drinking problems was robust across multiple models and follow-up tests. The findings also suggest that rather than trying to directly restructure or change negative cognitions and affect, another viable intervention strategy might be working to enhance clients’ specific mindfulness skills, which in turn might lead to less social anxiety and less drinking problems. More specifically, based on our findings, interventions focused on strengthening the mindfulness skills of accepting without judgment, acting with awareness, and describe could lead to less social anxiety, fewer coping motives to drink, and ultimately, fewer problems related to drinking.
It is interesting that although the specific goal of acceptance-based therapies is not to directly reduce anxiety, a byproduct of developing these mindfulness capacities is that an individual may be able to act in ways that result in less anxiety, as well as less harmful behaviors that are driven by anxiety. On the one hand, these findings may promote “buy in” from the many clients whose explicit goal in therapy is a reduction in negative affect, and who may be resistant to the idea of learning to identify, tolerate, and accept the full range of human emotions without trying to modify the content. On the other hand, findings from this study suggest that for the individual who is already experiencing heightened social anxiety, mindfulness may not be enough to break the link between social anxiety and harmful behaviors like drinking to cope. In particular, contrary to expectations, there were not indirect effects of social anxiety on drinking problems via any of the mindfulness facets tested here. This lack of significant indirect effects may be partially related to our sample. Specifically, individuals in the present study reported experiencing heightened social anxiety symptoms and they screened positive for alcohol dependence. Thus, the total effect between social anxiety and drinking problems was especially strong, leaving less room for potential mediators.
Results from this study must be interpreted in light of several limitations. First, the design of this study was cross-sectional, so the question of whether social anxiety precedes deficits in trait mindfulness, or vice versa, cannot be disentangled with these data. Future research using a longitudinal design will be critical to address this meaningful question. Notwithstanding, according to Hayes (2013), one of the leading experts on contemporary approaches to mediation, it is reasonable to conduct mediation analysis even if one cannot firmly establish causality due to limitations of one’s design (e.g., correlational data collected at one time point). Thus, while bearing in mind the necessary caveats to interpret these findings, the solid theoretical rationale provides a firm foundation upon which the present tests of mediation were based. Another limitation is that we only evaluated one type of drinking motive—drinking to cope with social anxiety. Future research will need to evaluate other potential mediators, particularly other drinking motivations (Cooper, 1994). Third, while this study advances prior research by using a sample with co-occurring symptoms of social anxiety and alcohol dependence, future research may want to consider other comorbidities as well. For instance, we cannot rule out that these effects are specific to social anxiety, as opposed to due to aspects of social anxiety that overlap with related problems like depression. Fourth, findings will need to be replicated with more participants, as a limitation of this research was our use of a relatively small sample size for tests of mediation (Fritz & MacKinnon, 2007). That said, while roughly 27% of the sample were missing data on the mindfulness measure, our use of full information maximum likelihood was a strength of this study as it helped us to preserve statistical power and the structure of the data set (Graham, 2009).
In spite of these limitations, the present study contributes novel findings that highlight the ways in which specific trait mindfulness facets and social anxiety symptoms may work together to drive drinking problems. Moreover, this research builds upon existing studies that have largely been conducted with college students by evaluating mediators of drinking problems in a community-based sample with alcohol dependence. It is also worth highlighting that unlike most other work conducted in this area, roughly half of our sample identified as black or African American. This is meaningful given that there is a pressing need to include more individuals who identify as racial minorities in psychological research (Sue, 1999). Most notably, this research suggests that individuals who have a reduced capacity to accept without judgment, act with awareness, and describe their internal experiences may be at heightened risk for drinking problems. Further, this relationship may be fueled by greater levels of social anxiety and drinking to cope with that anxiety.
Acknowledgments
The authors are thankful for the statistical consultation on handling missing data provided by Dr. Elizabeth Kiel, as well as the statistical consultation on using Mplus provided by Dr. Aaron Luebbe. We would also like to thank Karina Del Valle, Robert Gibler, Susan McDonald, Tricia Minton, Namratha Sandella, and Rebecca Wang for their research assistance.
Funding: This research was supported by a National Institute on Alcohol Abuse and Alcoholism R21AA021151 grant awarded to the first author.
Footnotes
Compliance with Ethical Standards
Conflict of Interest: We have no actual or potential conflict of interests to disclose.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed Consent was obtained from all individual participants included in the study.
References
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10:125–143. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bowen SB, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Marlatt A. Mindfulness-Based Relapse Prevention for substance use disorders: A pilot efficacy trial. Substance Abuse. 2009;30:295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Enkema MC. Relationship between dispositional mindfulness and substance use: Findings from a clinical sample. Addictive Behaviors. 2014;39:532–537. doi: 10.1016/j.addbeh.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, Larimer ME. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry. 2014;71:547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG. Drinking behaviors in social situations account for alcohol-related problems among socially anxious individuals. Psychology of Addictive Beahviors. 2010;24:640–648. doi: 10.1037/a0020968. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG, Ecker AH, Vinci C. A biopsychosocial model of social anxiety and substance use. Depression and Anxiety. 2013;30:276–284. doi: 10.1002/da.22032. [DOI] [PubMed] [Google Scholar]
- Carpenter KM, Hasin D. A prospective evaluation of the relationship between reasons for drinking and DSM-IV Alcohol-use Disorders. Addictive Behaviors. 1998;23:41–46. doi: 10.1016/s0306-4603(97)00015-4. [DOI] [PubMed] [Google Scholar]
- Cheetham A, Allen NB, Yucel M, Lubman DI. The role of affective dysregulation in drug addiction. Clinical Psychology Review. 2010;30:621–634. doi: 10.1016/j.cpr.2010.04.005. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use & Misuse. 2014;49:492–512. doi: 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- Clerkin EM, Magee JC, Wells TT, Beard C, Barnett NP. Randomized controlled trial of attention bias modification in a racially diverse, socially anxious, alcohol dependent sample. 2016 doi: 10.1016/j.brat.2016.08.010. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–20. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. [Google Scholar]
- Desrosiers A, Klemanski DH, Nolen-Hoeksema S. Mapping mindfulness facets onto dimensions of anxiety and depression. Behavior Therapy. 2013;44:373–384. doi: 10.1016/j.beth.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez AC, Wood MD, Stein AR, Rossi JS. Measuring mindfulness and examining its relationship with alcohol use and negative consequences. Psychology of Addictive Behaviors. 2010;24:608–616. doi: 10.1037/a0021742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forcehimes AA, Tonigan JS, Miller WR, Kenna GA, Baer JS. Psychometrics of the Drinker Inventory of Consequences (DrInC) Addictive Behaviors. 2007;32:1699–1704. doi: 10.1016/j.addbeh.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: Results of a randomized controlled pilot trial. Journal of Psychoactive Drugs. 2010;42:177–192. doi: 10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Graham JW, Schafer JL. On the performance of multiple imputation for multivariate data with small sample size. In: Hoyle R, editor. Statistical strategies for small sample research. Thousand Oaks, CA: Sage; 1999. pp. 1–29. [Google Scholar]
- Goldin PR, Ramel W, Gross JJ. Mindfulness meditation training and self-referential processing in social anxiety disorder: Behavioral and neural effects. Journal of Cognitive Psychotherapy. 2009;23:242–257. doi: 10.1891/0889-8391.23.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Mediation, moderation, and conditional process analysis. New York, NY: Guilford; 2013. [DOI] [PubMed] [Google Scholar]
- Ham LS, Zamboanga BL, Bacon AK, Garcia TA. Drinking motives as mediators of social anxiety and hazardous drinking among college students. Cognitive Behaviour Therapy. 2009;38:133–145. doi: 10.1080/16506070802610889. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Horner KJ, Juster HR, Safren SA, Brown EJ, Schneier FR. Psychometric properties of the Liebowitz social anxiety scale. Psychological medicine. 1999;29(1):199–212. doi: 10.1017/s0033291798007879. [DOI] [PubMed] [Google Scholar]
- Herbert JD, Cardaciotto L. An acceptance and mindfulness-based perspective on social anxiety disorder. In: Orsillo SM, Roemer L, editors. Acceptance and mindfulness-based approaches to anxiety: Conceptualizations and treatment. New York, NY: Springer; 2005. pp. 189–212. [Google Scholar]
- Jazaieri H, Goldin PR, Werner K, Ziv M, Gross JJ. A randomized trial of MBSR versus aerobic exercise for social anxiety disorder. Journal of Clinical Psychology. 2012;68:715–731. doi: 10.1002/jclp.21863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelicic H, Phelps E, Lerner RM. Use of missing data methods in longitudinal studies: the persistence of bad practices in developmental psychology. Developmental Psychology. 2009;45:1195–1199. doi: 10.1037/a0015665. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. New York, NY: Delacorte; 1990. [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are: Mindfulness meditation in everyday life. New York, NY: Hyperion; 1994. [Google Scholar]
- Karyadi KA, Cyders MA. Elucidating the association between trait mindfulness and alcohol use behaviors among college students. Mindfulness. 2015;6:1242–1249. doi: 10.1007/s12671-015-0386-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanagh D, Andrade J, May J. Imaginary relish and exquisite torture: The elaborated intrusion theory of desire. Psychological Review. 2005;112:446–467. doi: 10.1037/0033-295X.112.2.446. [DOI] [PubMed] [Google Scholar]
- Kocovski NL, Fleming JE, Rector NA. Mindfulness and acceptance based group therapy for social anxiety disorder: an open trial. Cognitive and Behavioral Practice. 2009;16:276–289. [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25:841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Krueger R, Frye B, Peterson J. Epidemiological perspectives on co-occurring anxiety disorder and substance use disorder. In: Stewart SH, Conrod P, editors. Anxiety and substance use disorders: The vicious cycle of comorbidity. New York, NY: Springer; 2008. pp. 3–17. [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Marlatt GA. Addiction, mindfulness, and acceptance. In: Hayes SC, Jacobson NS, V. Follette M, Dougher MJ, editors. Acceptance and change: Content and context in psychotherapy. Reno, NV: Context Press; 1994. pp. 175–197. [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–47. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- McCrady BS. Alcohol Use Disorders. In: Barlow DH, editor. Clinical Handbook of Psychological Disorders: A Step-by-step Treatment Manual. New York, NY: Guilford Press; 2008. pp. 492–546. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse: Test manual (No. 95) US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- Mennin DS, Fresco DM, Heimberg RG, Schneier FR, Davies SO, Liebowitz MR. Screening for social anxiety disorder in the clinical setting: Using the Liebowitz Social Anxiety Scale. Journal of Anxiety Disorders. 2002;16:661–673. doi: 10.1016/s0887-6185(02)00134-2. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- Parsons EM, Luebbe AM, Peterman K, Clerkin EM. Mindfulness facets as moderators of the relationship between social anxiety schemas and behavioral and desired avoidance; Chicago, IL. Poster presented at the annual meeting of the Association for Behavioral and Cognitive Therapies.Nov, 2015. [Google Scholar]
- Pittman B, Gueorguieva R, Krupitsky E, Rudenko AA, Flannery BA, Krystal JH. Multidimensionality of the Alcohol Withdrawal Symptom Checklist: A factor analysis of the Alcohol Withdrawal Symptom Checklist and CIWA-Ar. Alcoholism: Clinical and Experimental Research. 2007;31:612–618. doi: 10.1111/j.1530-0277.2007.00345.x. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rasmussen MK, Pidgeon AM. The direct and indirect benefits of dispositional mindfulness on self-esteem and social anxiety. Anxiety, Stress, & Coping. 2011;24:227–233. doi: 10.1080/10615806.2010.515681. [DOI] [PubMed] [Google Scholar]
- Reynolds A, Keough MT, O’Connor RM. Is being mindful associated with reduced risk for internally-motivated drinking and alcohol use among undergraduates? Addictive Behaviors. 2015;42:222–226. doi: 10.1016/j.addbeh.2014.11.027. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, Heimberg RG. The reverse of social anxiety is not always the opposite: The reverse-scored items of the social interaction anxiety scale do not belong. Behavior Therapy. 2007;38:192–206. doi: 10.1016/j.beth.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Roos CR, Pearson MR, Brown DB. Drinking motives mediate the negative associations between mindfulness facets and alcohol outcomes among college students. Psychology of Addictive Behaviors. 2015;29:176–183. doi: 10.1037/a0038529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmertz SK, Masuda A, Anderson PL. Cognitive processes mediate the relation between mindfulness and social anxiety within a clinical sample. Journal of Clinical Psychology. 2012;68:362–371. doi: 10.1002/jclp.20861. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-1. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Sher KJ, Grekin ER, Williams NA. The Development of Alcohol Use Disorders. Annual Review of Clinical Psychology. 2005;1:493–523. doi: 10.1146/annurev.clinpsy.1.102803.144107. [DOI] [PubMed] [Google Scholar]
- Smith JP, Randall CL. Anxiety and alcohol use disorders: comorbidity and treatment considerations. Alcohol research: current reviews. 2012;34:414–431. [PMC free article] [PubMed] [Google Scholar]
- Sue S. Science, ethnicity, and bias: Where have we gone wrong? American Psychologist. 1999;54:1070–1077. doi: 10.1037/0003-066x.54.12.1070. [DOI] [PubMed] [Google Scholar]
- Thomas SE, Randall CL, Carrigan MH. Drinking to cope in socially anxious individuals: A controlled study. Alcoholism: Clinical and Experimental Research. 2003;27:1937–1943. doi: 10.1097/01.ALC.0000100942.30743.8C. [DOI] [PubMed] [Google Scholar]
- Veilleux JC, Skinner KD, Reese KD, Reese ED, Shaver JA. Negative affect intensity influences drinking to cope through facets of emotion regulation. Personality and Individual Differences. 2014;59:95–101. [Google Scholar]
- Vujanovic AA, Bonn-Miller MO, Marlatt GA. Posttraumatic stress and alcohol use coping motives among a trauma-exposed community sample: The mediating role of non-judgmental acceptance. Addictive Behaviors. 2011;36:707–712. doi: 10.1016/j.addbeh.2011.01.033. [DOI] [PubMed] [Google Scholar]
- Widaman KF. III. Missing data: What to do with or without them. Monographs of the Society for Research in Child Development. 2006;71:42–64. [Google Scholar]
- Wiers RW, Houben K, Roefs AJ, de Jong P, Hofmann W, Stacy AW. Implicit cognition in health psychology: Why common sense goes out of the window. In: Payne K, Gawronski B, editors. Handbook of implicit social cognition: Measurement, theory, and applications. New York, NY: Guilford Press; 2010. pp. 463–488. [Google Scholar]
- Witkiewitz K, Bowen S. Depression, craving and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology. 2010;78:362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]