Abstract
Association of cholesteryl ester transfer protein (CETP) Gene -629C/A Polymorphism with angiographically proven atherosclerosis CETP gene has been linked to CAD risk via its role in HDL and LDL metabolism. There is no agreement of whether CETP is atherogenic or not. Furthermore, various genotypes of CETP gene have been associated with CETP levels and thus with atherosclerosis risk. Our aim was to study the association of CETP -629C/A gene polymorphism with CETP and HDL levels and their association if any with atherosclerosis. Study population consisted of angiographically documented 50 cases with coronary artery atherosclerosis and 50 controls negative for atherosclerosis of coronary artery. Serum lipid profile was measured on SYNCHRON CX-9 using standard kits. Serum CETP levels were measured by ELISA method. CETP -629C/A gene polymorphism was studied using PCR–RFLP method. There was no significant difference in lipid profile of the two groups. However, serum CETP level was significantly higher (46.44 ± 21.75 ng/ml) in cases than controls (37.10 ± 21.92 ng/ml) with p value =0.035. The frequency of -629A allele was higher (0.85) in cases than that of controls (0.81). Homozygosity of A allele was more in subjects with atherosclerosis of coronary artery. We conclude that CETP is atherogenic and could be used as atherogenic risk predictor in angiographically proven atherosclerosis. Also A allele of -629C/A polymorphism is more prevalent in cases; indicating its effect on expression of CETP gene.
Keywords: Cholesteryl ester transfer protein, High density lipoprotein, Atherosclerosis, Coronary artery disease
Introduction
Lipoproteins have been shown to play significant role in the pathogenesis of atherosclerosis. HDL-C is a known independent risk factor for atherosclerosis [1–4]. Several epidemiological studies have shown an inverse correlation between HDL-C and incidence of CAD [5–7]. HDL is considered to be atheroprotective because of its ability to remove excess cholesterol from macrophage foam cells in atheromatous blood vessels and other tissues via reverse cholesterol transport pathway [8, 9]. CETP plays a significant role in HDL metabolism by mediating exchange of cholesteryl esters for TG from HDL to Apo B containing lipoprotein [10]. It is reported to show its atherogenicity via increasing the atherogenic lipoprotein LDL while as a facilitator of efflux of cholesterol it also can be seen as antiatherogenic [9].
Although environmental factors play an important role in atherosclerosis development, genetic factors have been reported to be strong determinants of atherosclerotic cardiovascular disease risk [11]. Genetic heterogeneity at CETP gene locus is associated with plasma CETP activity and HDL-C [12–15]. CETP is localized on chromosome 16q21 near LCAT gene locus [16] and contains 25 kilo bases genomic DNA with 16 exons [12]. Several CETP gene single nucleotide polymorphisms have been reported on CETP locus. CETP -629C/A is a newly studied functional gene polymorphism present in promoter region and it has been reported to be associated with the CETP and HDL-C levels [17]. Few studies have been done on this polymorphism and its association with CETP and HDL-C levels in Indian population. Therefore its association with CETP levels and atherosclerosis in Indian population is still not clear. Establishment of these genetic risk factors may help in recognition of the population at risk and ultimately in the management of disease.
Our aim was to study the association, if any, of CETP levels and CETP -629C/A gene polymorphism with angiographically proven atherosclerosis.
Materials and Methods
The study was carried out jointly in the Department of Biochemistry, Lady Hardinge Medical College and Smt. Sucheta Kriplani Hospital and Department of Cardiology, G.B. Pant Hospital, Delhi. With informed consent, age and sex matched 100 non-diabetic subjects undergoing angiography were selected from Cardiology Department of G.B. Pant Hospital. The study population was further divided into 2 groups on the basis of angiography; 50 subjects with atherosclerosis as proven by angiography were included as cases and 50 age and sex matched subjects with no blockage on angiography were enrolled as controls. Study groups were subjected to detailed history with special reference to the atherosclerosis followed by clinical examination. Our study was approved by the Ethical Committee of Lady Hardinge Medical College.
The venous blood sample was collected from subjects under sterile conditions after overnight fasting. The blood samples for routine parameters were processed immediately for separation of serum and plasma. Serum sample for CETP analysis were stored at −20° till batch was analyzed. For genetic study venous blood was collected in EDTA vial. Plasma was separated by centrifugation at 2500 rpm for 10 min and cellular components were stored at −20 °C till DNA extraction. Routine parameters and lipid profile were measured by auto analyzer (SYNCHRON CX-9, Beckman Coulter) using standard reagents. Serum CETP was measured by using BMASSAY ELISA kit.
CETP -629C/A Gene Polymorphism
DNA extraction was done by using DNA extraction kit from QIGEN. DNA amplification was done using 25 µl of cocktail mixture containing 13 µl of nuclease free water; 1.5 µl of d NTP mix; 2.5 µl of 10× buffer; 0.5 µl of Taq polymerase; 2 µl of each forward and 2 µl reverse primer (2 pmol) and 2 µl of (2 pmol) of reverse primer on thermal cycler PTC BIORAD with primers flanking polymorphic region of -629CETP gene. Primer pairs were as follows: Forward Primer—AGAATTGAAATGCCACAGACATTCC and Reverse Primer—CCTTGATATGCATAAAATAACTCTCG. The Program for CETP -629 PCR assay was as follows: Initial denaturation at 95 °C for 5 min, cycle denaturation at 95 °C for 30 s, cycle annealing at 57 °C for 45 s, cycle extension at 72 °C for 30 s, final extension at 72 °C for 7 min. There were 35 cycles, and it was held at 4 °C till the PCR product was taken out. Amplified 127 bp PCR products were run on 2 % agarose check gel. For restriction fragment length polymorphism, 15 µl of PCR product was mixed with 1.5 µl (15 U) of AvaI restriction enzyme and incubated overnight at 37 °C with 10 µl of 10× buffer. Digested product was run on 3 % agarose gel stained with ethidium bromide. It was viewed by Alpha Gel Doc system. For determination of restriction length polymorphism on the gel picture DNA ladder of 100 bps was run along with the digested product.
In presence of C to A transition (AA), restriction site is lost and a single band of 127 bp was seen on gel picture and in absence of any transition (CC) a band of 100 bp was seen. And in heterozygous state (CA) two bands one with 127 bp and another with 100 bp were seen as shown in Fig. 1.
Fig. 1.
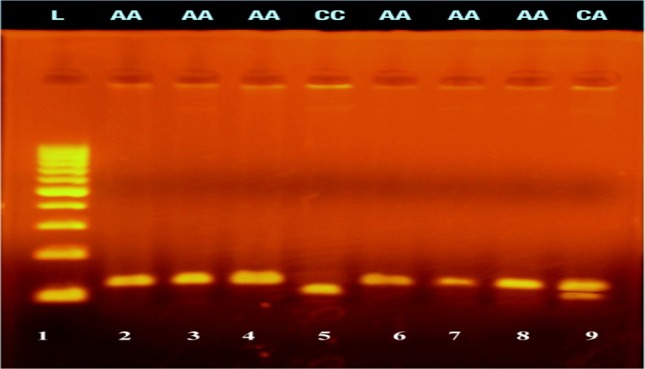
Gel picture (3 % agarose) of CETP -629 C/A polymorphism: Lane 1 is DNA molecular weight marker (100 bp). Lane 2–9 are RFLP of samples of study population; lane 2, 3, 4, 6, 7 and 8 represent AA (127 bp) genotype, lane 5 is CC (100 bp) and lane 9 is CA (127 and 100 bp) genotype
Statistical Analysis
Statistical analysis was performed with the SPSS version 20.0 software program. Continuous variables were expressed as mean ± SD. The variables were compared with a normal distribution by unpaired 2-tailed Student’s t test. A value of p ≤ 0.05 was considered statistically significant. Frequencies of genotypes were compared by chi-square test and checked for Hardy–Weinberg equilibrium.
Results
In our study population, smoking followed by hypertension were the two most prevalent risk factors (Table 1). No statistically significant difference was observed in lipid profile of cases and controls (Table 2). Serum CETP level was significantly higher (46.44 ± 21.75 ng/ml) in cases than controls (37.10 ± 21.92 ng/ml) with p value =0.035 (Table 2). Frequency of AA genotype was found 72 % of in cases and 64 % in control group. CA genotype was found in 26 % of cases and 34 % of the control group. One CC genotype was found in each group. However, the variation of genotypic distribution was (p > 0.05) not significant (Table 3).
Table 1.
Demography of study groups
| Case (mean ± SD) | Control (mean ± SD) | p value | |
|---|---|---|---|
| Age | 51.22 ± 7.6 | 48 ± 7.2 | 0.105 |
| Sex (M) | 35 (70 %) | 33 (66 %) | 0.668 |
| (F) | 15 (30 %) | 17 (34 %) | |
| BMI | 22.9 ± 3.4 | 22.5 ± 2.4 | 0.544 |
| Hypertension | 22 (44 %) | 9 (18 %) | 0.005 |
| Smoking | 30 (60 %) | 11 (22 %) | 0.000 |
| F/H/O CAD | 4 (8 %) | 3 (6 %) | 0.695 |
p value ≤0.05 is considered statistically significant
Table 2.
Levels of lipid profile parameters and CETP in study groups
| Parameters | Case (mean ± SD) | Controls (mean ± SD) | p value |
|---|---|---|---|
| CETP (ng/ml) | 46.44 ± 21.75 | 37.10 ± 12.92 | 0.035 |
| T.CHOL (mg/dl) | 143.4 ± 42.30 | 142.14 ± 37.30 | 0.875 |
| TG (mg/dl) | 146.08 ± 67.67 | 134.36 ± 63.89 | 0.375 |
| HDL (mg/dl) | 41.700 ± 8.83 | 43.580 ± 12.55 | 0.389 |
| LDL (mg/dl) | 81.580 ± 37.57 | 77.940 ± 34.64 | 0.616 |
| VLDL (mg/dl) | 29.22 ± 13.51 | 26.84 ± 12.52 | 0.375 |
| LDL/HDL | 1.97 ± 0.80 | 1.82 ± 0.67 | 0.308 |
| T CHOL/HDL | 3.58 ± 1.31 | 3.38 ± 0.89 | 0.382 |
p value ≤0.05 is considered statistically significant
Table 3.
Distribution of Genotypes and Alleles in Study Groups
| Genotype | Cases | Control | |
|---|---|---|---|
| AA | 36 (72 %) | 32 (64 %) |
P = 0.681 X2 = 0.769 |
| CA | 13 (26 %) | 17 (34 %) | |
| CC | 1 (2 %) | 1 (2 %) |
Allelic frequency of A allele was 0.85 in cases and 0.81 in controls while frequency of C allele was 0.15 in cases and 0.18 in controls
Discussion
We studied 100 subjects with coronary artery blockage and divided them into cases and controls on the basis of angiography. Serum CETP levels and lipid profile (Total Cholesterol, TG, HDL-C, LDL-C and VLDL) of both cases and controls were measured. Mean serum CETP levels of cases were found significantly higher than cases but no statistically significant difference was found in lipid profile of cases and controls.
CETP is synthesized primarily in liver, spleen and adipose tissue [9]. Cholesteryl ester transport protein mediates the exchange of cholesteryl ester and triglycerides between HDL and Apo B containing lipoproteins [10]. In our study significantly higher CETP levels in cases that had positive angiography for atherosclerosis as compared to the controls suggests an association of CETP with atherosclerosis. CETP is reported to show its atherogenic effect by transferring the cholesteryl ester from HDL to LDL and thus increasing the atherogenic LDL-C [10]. In our study there was no statistically significant difference in HDL-C and LDL-C levels of cases and controls as both of our study groups were on statins. This finding of increase in CETP levels in cases with angiographically proven atherosclerosis as compare to controls shows its association with atherosclerosis.
CETP -629C/A is a functional polymorphism identified 629 bp upstream of transcription site and it modulates not only the transcription rate of CETP promoter but also plasma CETP mass [17]. This polymorphism occurs in transcription factor binding site and affects splicing Sp1/Sp3 binding [18]. In our study, we didn’t find any significant difference in the frequency of alleles probably because of small sample size and ethnic variation. Though A allele was more prevalent (0.85) in cases as compared to the controls (0.81), and we hypothesize that the effect of this polymorphism is to enhance promoter activity of CETP gene as evidenced by the significantly increased CETP levels in patients with positive angiography for atherosclerosis. This was supported by the findings of Borggereve et al. [19] and Samami et al. [20] where despite of high HDL-C levels, A allele was associated with increased CAD risk indicating that there may be mechanisms other than HDL-C mediated by which -629C/A is associated with increased CAD risk. However, our finding was not in accordance with that of Dachet et al. [18], according to which A allele is associated with lower promoter activity than C allele. As our sample size was small we could find only one CC genotype in each of our study group. This discrepancy also may be because of difference in ethnicity and genetic susceptibility of population as it has been reported that the association of CETP and HDL-C with their impact on disease varies with nature, size and ethnicity of population under study. Further studies are required to establish the association of -629C/A CETP polymorphism with atherosclerosis.
We conclude CETP levels are associated with angiographically proven atherosclerosis and could be a biomarker in such subjects. AA genotype of CETP (-629C/A) may be associated with higher risk of atherosclerosis as it was found to be more prevalent in cases than controls. More study on larger population is required to validate CETP as a biomarker of atherosclerosis.
Acknowledgments
Funding
Study was part of thesis and was non-funded.
Compliance with Ethical Standards
Conflict of interest
None.
Ethical Compliance
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Despres JP, Lemieux GR, Dagenais B, Cantin B, Lamarche B. HDL-C as a marker of coronary heart disease risk: the Quebec cardiovascular study. Atherosclerosis. 2000;153:263–272. doi: 10.1016/S0021-9150(00)00603-1. [DOI] [PubMed] [Google Scholar]
- 2.Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease: the Framingham Study. Am J Med. 1977;62:707–714. doi: 10.1016/0002-9343(77)90874-9. [DOI] [PubMed] [Google Scholar]
- 3.Rubins HB, Robins SJ, Collins D, Fye CL, Anderson JW, Elam MB, et al. Gemfibrozil for the low levels of high density lipoprotein cholesterol. Veterans Affairs High Density Lipoprotein Cholesterol Intervention Trial Study Group. N Engl J Med. 1999;341:410–418. doi: 10.1056/NEJM199908053410604. [DOI] [PubMed] [Google Scholar]
- 4.Manninen V, Elo MO, Frick MH, Happa K, Heinonen OP, Helo P, et al. Lipid alterations and decline in the incidence of coronary heart disease in the Helsinki Heart Study. J Am Med Assoc. 1988;260:641–651. doi: 10.1001/jama.1988.03410050061031. [DOI] [PubMed] [Google Scholar]
- 5.Miller NE, Thelle DS, Forde OH, Mjos OD. The Tromso heart study: high density lipoprotein and coronary heart disease: a prospective case-control study. Lancet. 1977;1(8019):965–968. doi: 10.1016/S0140-6736(77)92274-7. [DOI] [PubMed] [Google Scholar]
- 6.Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease: Framingham Heart Study. Am J Med. 1977;62:707–714. doi: 10.1016/0002-9343(77)90874-9. [DOI] [PubMed] [Google Scholar]
- 7.Assmann G, Schulte H, Oberwitter W, Hause WH. New aspects in the prediction of coronary artery disease: the Prospective Cardiovascular Munster Study. In: Fidge NH, Nestel PJ, editors. Atherosclerosis VII. Amsterdam: Elsevier; 1986. pp. 19–24. [Google Scholar]
- 8.Lewis GF, Rader DJ. New insights into the regulation of HDL metabolism and reverse cholesterol transport. Circ Res. 2005;96:1221–1232. doi: 10.1161/01.RES.0000170946.56981.5c. [DOI] [PubMed] [Google Scholar]
- 9.Tall AR. Plasma cholesteryl ester transfer protein. J Lipid Res. 1993;34:1255–1274. [PubMed] [Google Scholar]
- 10.Grooth GJ, Klerkx AH, Stroes ES, Staleenhoef AF, Kastelein JJ, Kuivenhoven JA. A review of CETP and its relation to atherosclerosis. J Lipid Res. 2004;45:1967–1973. doi: 10.1194/jlr.R400007-JLR200. [DOI] [PubMed] [Google Scholar]
- 11.Kovacic S, Bakran M. Genetic susceptibility to atherosclerosis. Stroke Res Treat. 2012;10:1–5. doi: 10.1155/2012/362941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agellon L, Quinet E, Gillette T, Drayana D, Brown M, Tall AR. Organization of the human cholesteryl ester transfer protein gene. Biochemistry. 1990;29:1372–1376. doi: 10.1021/bi00458a004. [DOI] [PubMed] [Google Scholar]
- 13.Daryana D, Lawn R. Multiple RFLPs at human cholesteryl ester transfer protein locus. Nucleic Acids Res. 1987;15:4698. doi: 10.1093/nar/15.11.4698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freeman D, Shepherd J, Packard CJ, Humphries SE, Gaffney D. An StuI RFLP at human cholesteryl ester transfer protein locus. Nucleic Acids Res. 1989;17:2880. doi: 10.1093/nar/17.7.2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zullani G, Hobbs HH. EcoNI polymorphism in the human cholesteryl ester transfer protein gene. Nucleic Acids Res. 1990;18:2834. doi: 10.1093/nar/18.9.2834-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luis AJ, Zollman S, Sparkes S, Klisak I, Drayana D, Lawn RM, et al. Assignment of the human gene for cholesteryl ester transfer protein to chromosome 16q21–16q21. Genomics. 1987;1(3):232–235. doi: 10.1016/0888-7543(87)90049-8. [DOI] [PubMed] [Google Scholar]
- 17.Kondo I, Berg K, Daryana D, Lawn R. DNA polymorphism at locus for human cholesteryl ester transfer protein is associated with high density lipoprotein cholesterol and apolipoprotein levels. Clin Genet. 1989;35(1):49–56. doi: 10.1111/j.1399-0004.1989.tb02904.x. [DOI] [PubMed] [Google Scholar]
- 18.Dachet C, Poirier O, Cambien F, Luc G, Chapman J, Rouis M. New functional promoter polymorphism, C-629A, in cholesteryl ester transfer protein gene related to CETP mass and HDL cholesterol levels: role of Sp1/Sp3 in transcriptional regulation. Atheroscler Thromb Vasc Biol. 2000;20:507–515. doi: 10.1161/01.ATV.20.2.507. [DOI] [PubMed] [Google Scholar]
- 19.Borggereve SE, Hillege HL, de Jong PE, Zurrmann MW, Dullart RP, van Tol A, et al. An increased coronary risk is paradoxically associated with common cholesteryl ester transfer protein gene variations that relate to higher high density lipoprotein cholesterol: a population based study. JCEM. 2006;91(9):3382–3388. doi: 10.1210/jc.2005-2322. [DOI] [PubMed] [Google Scholar]
- 20.Samami KG, Noori M, Nobar MR, Chaleshtori MH, Farrokhi E, Amin MD. I405 V and -629C/A polymorphism of cholesteryl ester transfer protein in patients with coronary artery disease. Iran Biomed J. 2009;13(2):103–108. [PubMed] [Google Scholar]


