Abstract
Background and aims
Treatment for opioid use disorders (OUD) reduces the risk of mortality and infectious disease transmission; however, opportunities to quantify the potential economic benefits of associated decreases in drug-related crime are scarce. This paper aimed to estimate the costs of crime during and after periods of engagement in publicly-funded treatment for OUD to compare total costs of crime over a hypothetical 6-month period following initiation of opioid agonist treatment (OAT) versus detoxification.
Design
Retrospective, administrative data-based cohort study with comprehensive information on drug treatment and criminal justice systems interactions.
Setting
Publicly-funded drug treatment facilities in California, USA (2006–2010).
Participants
31,659 individuals admitted for the first time to treatment for OUD, and who were linked with criminal justice and mortality data, were followed during a median 2.3 years. Median age at first treatment admission was 32, 35.8% were women, and 37.1% primarily used prescription opioids.
Measurements
Daily costs of crime (2014$US) were calculated from a societal perspective and were composed of the costs of policing, court, corrections, and criminal victimization. We estimated the average marginal effect of treatment engagement in OAT or detoxification adjusting for potential fixed and time-varying confounders, including drug use and criminal justice system involvement prior to treatment initiation.
Findings
Daily costs of crime during treatment compared with after treatment were $126 lower for OAT (95% CI: $116, $136) and $144 lower for detoxification ($135, $154). Summing the costs of crime during and after treatment over a hypothetical 6-month period using the observed median durations of OAT (161 days) and detoxification (19 days), we estimated that enrolling an individual in OAT as opposed to detoxification would save $17,550 ($16,840, $18,383).
Conclusions
In publicly-funded drug treatment facilities in California USA, engagement in treatment for opioid use disorders is associated with lower costs of crime in the six months following initiation of treatment, and the economic benefits were far greater for individuals receiving time-unlimited treatment.
Keywords: Opioid agonist treatment, opioid use disorder, costs of crime, California, heroin, prescription opioids
Introduction
Treatment for opioid use disorders (OUD) has the potential to generate important benefits to society, particularly through the reduction of drug-related mortality, (1, 2) control of infectious diseases, (3) and improved quality of life for patients, (4–8) but also through lower associated criminality. (9–14) Over the past 20 years, the detrimental social consequences of illicit substance use have increasingly been viewed as a public health issue rather than a social problem requiring criminal justice system intervention. Yet, overdoses are the leading cause of injury death in the United States (15) and the incidence of opioid-related mortality is greater than all other forms of drug-related deaths combined. (16)
Substance use disorders have been estimated to impose annual societal costs of $220 billion (2014$US), equivalent to obesity or diabetes, (17, 18) and the $69.9 billion attributable to the criminal justice system represents the largest share of direct costs. (19) Although there has been a shift in funding towards treatment by the U.S. Federal government (from 31% of the National Drug Control Policy budget in 2003 to 38% in 2015), 56.9% of spending representing $14.7 billion remains focused on enforcement and interdiction efforts. (20) Funds allocated for enforcement and interdiction efforts are likely much higher when accounting for state and local expenditures.
California’s voter-initiated Substance Abuse and Crime Prevention Act, now an unfunded mandate, which allowed those convicted of nonviolent offenses, including drug possession and probation or parole violations to receive drug treatment in lieu of incarceration, resulted in taxpayer savings (21) despite only one in eight convicted individuals with OUD receiving time-unlimited (maintenance) treatment. (22) Furthermore, California is among the highest per capita spenders on corrections, (23) and it has one of the nation’s highest rates of unmet need for illicit drug use treatment. (24) More specifically, 89.5% of individuals in California needing treatment for substance use disorders did not access it in 2014. (25)
Direct or indirect means of crime prevention can reduce the burden imposed on victims, communities, and the criminal justice system, consequently generating substantial economic benefits. (26–33) Treatment for OUD carries significant stigma amongst policymakers in both health and criminal justice sectors. (34, 35) It is critical to quantify the broader societal economic benefits of evidence-based OUD treatment to provide a true representation of the overall benefits, (36) and further the case to expand access to this life-saving treatment. (37) While a systematic review of cost-benefit and cost-effectiveness analyses for the treatment of OUD by Doran (38) found that studies published prior to 2007 which include criminal activity consistently find benefits outweighing the costs, the information on criminal justice costs was found to be limited. In a review of economic evaluations focused on estimating costs associated with treatment for OUD, Murphy & Polsky (39) found that 12 of the 13 included studies only considered costs attributable to the healthcare system; the single exception reported costs of crime associated with treatment access in a Canadian setting. (40) To our knowledge, there has never been a population-level estimate of the costs of crime associated with treatment engagement for OUD compared to subsequent treatment discontinuation.
We undertook this study to: (i) compare the costs of crime during periods of engagement in publicly-funded treatment for OUD and those during post-treatment periods; and (ii) compare the total costs of crime that would accumulate over a hypothetical 6-month period following initiation of OAT versus detoxification. We hypothesized that the costs of crime during periods of treatment engagement would be lower compared to those following treatment discontinuation and that greater economic benefit would be associated with OAT compared to detoxification, consistent with prior findings. (40, 41) To fulfill our objectives, we used a linked administrative database for the state of California, with comprehensive information on interactions with the drug treatment and criminal justice systems.
Methods
Study Design
We conducted a retrospective cohort study of individuals admitted for the first time to treatment for OUD, including opioid agonist treatment (OAT) and detoxification, in publicly-funded drug treatment facilities in California from January 1, 2006 to December 31, 2010. Individual-level statewide administrative data were linked using individuals’ Social Security Number, full name, birth date, and sex. Databases included the California Outcomes Monitoring System (CalOMS), Automated Criminal History System (ACHS), Offender Based Information System (OBIS), and National Death Index. The study period was determined by earliest Social Security Number availability for linkage (2006) and the most recent mortality data available (2010) at the time of linkage. Individuals were included if they had no prior records of treatment for OUD in the CalOMS system dating back to 1991 (including the California Alcohol and Drug Data System), (41) and were excluded if linked criminal justice records were not uniquely identifiable. Subsequent treatment episodes during the study period were included if applicable. Data used for each individual in our study thus covered the period from the date of first treatment entry up to either the end of the study period or death.
Treatment data from CalOMS are recorded at treatment entry and discharge, and contains both self-reported data, including primary drug problem reported, as well as clinical information entered by treatment provider staff. Each publicly funded opioid treatment program licensed to dispense methadone is required to submit CalOMS data monthly. (42) Vital statistics data was obtained from the National Death Index, maintained by the Centers for Disease Control and Prevention, which contains records of all deaths occurring nationwide. Criminal records including arrests, convictions and sentences were obtained from the Automated Criminal History System (ACHS), maintained by the California Department of Justice (DOJ). The DOJ matching procedure has been shown to be the most sophisticated for identifying a particular person’s criminal justice record, resulting in a low under-linkage probability. (43) Corrections records, including prison incarceration and parole movement, were obtained from OBIS, maintained by the California Department of Corrections and Rehabilitation, where each individual has a unique identifier used to connect multiple OBIS records.
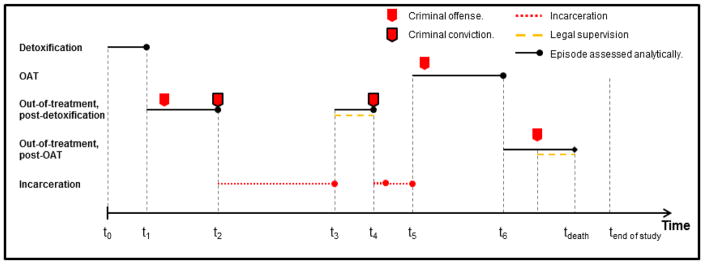
Discharge records are filed by treatment provider staff: (i) upon treatment completion; or (ii) when an individual in detoxification has missed appointments for ≥3 consecutive days without notifying the program, or for ≥14 consecutive days when in OAT. When successive treatment episodes were within the 3- and 14-day discontinuation thresholds for detoxification and OAT, respectively, they were merged to a single treatment episode. Otherwise, gaps between successive treatment or incarceration episodes were considered post-treatment episodes. Detailed construction of individual histories has been previously described. (41, 44) Dates of death were determined by probabilistic record linkage with the National Death Index database. Organization of the episodic dataset is shown in Figure 1.
Figure 1. Episodic dataset organization.
The timeline presented represents a hypothetical individual’s history of treatment, incarceration, legal supervision, and post-treatment periods, constructed from the linked databases used in our study. Legal supervision includes probation and parole, while incarceration includes sentences in county jail or state prison. Periods of incarceration were not included in the analyses as there is no treatment information or records of criminal acts while an individual is incarcerated. Costs attributable to incarceration were added to the episode during which the conviction occurred. In this example, five arrests were recorded over the study period, and two resulted in convictions. There are two treatment episodes and one incarceration sentence that is composed of two prison episodes and a jail holding period. Two of the three post-treatment episodes are post-detoxification episodes with one of these while under parole. The last post-treatment episode is post-OAT, partially spent under probation and censored. Time t0 represents individuals’ initiation of treatment for opioid use disorders in California’s public drug treatment system. OAT: Opioid Agonist Treatment.
The Costs of Crime
We calculated the direct costs of crime from a societal perspective and therefore included costs borne by the criminal justice system as well as the costs of criminal victimization, presented in 2014 $US, but did not include fines, crime career opportunity costs or intangible costs (such as pain-and-suffering and risk-of-homicide costs). (45) We adhered to best practice guidelines for the conduct of economic analysis. (46) Criminal justice system costs were composed of the costs of policing, court, and corrections. Costs of criminal victimization accounted for medical expenses, cash losses, property theft and victimization-related consequences. (45) Table 1 shows the incident-based and daily costs used. (47–50) There is no treatment information in our data while an individual is incarcerated, and records of criminal acts while incarcerated are not collected in either ACHS or OBIS databases. Consequently, periods of incarceration were not included in the longitudinal follow-up, and all costs attributable to a period of incarceration were added to the episode during which conviction occurred. Finally, daily costs of crime for treatment and post-treatment episodes were derived by dividing the costs of crime incurred during the episode by the duration of the episode (in days).
Table 1.
Description of inflation-adjusted unit costs for the criminal justice system, composed of the costs of policing, court, corrections, and criminal victimization, all reported in 2014 USD.
| Component | Unit Cost | Description | Source |
|---|---|---|---|
| Justice system costs | |||
| Policing, incident-based | $5,053 | Average tax-supported cost, estimated by the WSIPP using expenditure and workload data for jurisdictions in WA. | Washington State Institute for Public Policy (2014) |
|
|
|||
| Court, including prosecution and adjudication | $8,128 | Average tax-supported cost, estimated by the WSIPP using expenditure and workload data for jurisdictions in WA. | Washington State Institute for Public Policy (2014) |
|
|
|||
| Corrections | |||
| Legal supervision, daily costs | |||
| Probation | $3.71 | Calculated from average daily population at county-level divided by number of probation officers. | Longshore et al. (2007) |
| Parole | $11.40 | Daily costs obtained from the CDCR | Longshore et al. (2007) |
| Incarceration, daily costs | |||
| Jail | $122.18 | Daily average costs across California counties. | Board of State and Community Corrections (2012) |
| Prison | $140.49 | Calculated from CA’s Annual Costs to Incarcerate an Inmate in Prison.* | Legislative Analyst’s Office (2009) |
|
| |||
| Victimization costs, by crime category | McCollister et al. (2010) | ||
| Murder | $800,575 | The victimization costs include crime-specific derived medical expenses, cash losses, property theft or damage, and lost earnings because of injury and other victimization-related consequences. | |
| Rape/sexual assault | $6,031 | ||
| Assault | $9,444 | ||
| Robbery | $3,581 | ||
| Arson | $12,431 | ||
| Larceny/theft | $521 | ||
| Motor vehicle theft | $6,637 | ||
| Household burglary | $1,478 | ||
| Others | $0 | ||
WSIPP: Washington State Institute for Public Policy; CDCR: California Department of Corrections & Rehabilitation; WA: Washington State; CA: California.
Includes costs for security, health care and operation.
Drug Treatment Status
We were primarily interested in differences in the costs of crime between periods of engagement in treatment for OUD and post-treatment periods. Estimating costs of crime within our sample of treatment-naïve individuals presenting for treatment allowed us to avoid the inherent selection bias that would otherwise be present in a comparison of individuals accessing treatment to those not accessing treatment, a counterfactual our data did not allow us to consider. However, individuals accessing OAT (as opposed to detoxification) are likely a selective cohort as fundamental differences exist between how OUD treatment modalities are accessed.
Whereas OAT is a time-unlimited form of treatment, detoxification is mandated to 21-day episodes by California regulations (some programmatic exceptions exist). (51) In addition, two failed detoxification attempts are required in order to access OAT (51) and strict requirements for participation in OAT are imposed by Federal regulations governing opioid treatment programs. (52)
As a result, despite the likelihood of having higher drug use severity (a factor which may only partially be captured in the covariates available to us), the stability and consistency required to maintain daily participation in OAT suggests that individuals engaging in OAT would already be less likely to be involved with the criminal justice system compared to individuals accessing detoxification. Therefore, the potential bias from unmeasured factors present in the comparison across treatment modalities would most likely favor detoxification as opposed to OAT.
Treatment status was first classified in three mutually-exclusive groups, including engagement in OAT, engagement in detoxification or post-treatment. As potentially unmeasured time-varying factors likely influenced selection into one form of treatment or another, we hypothesized that all post-treatment episodes might not be homogeneous and classified them as post-detoxification and post-OAT periods. We further hypothesized that unmeasured time-invariant factors likely influenced selection into one form of treatment or another over time and assigned individuals to mutually exclusive longitudinal treatment access patterns: OAT only; detoxification only; a single detoxification episode in addition to one or more OAT episodes; and multiple detoxification and OAT episodes.
Furthermore, we note the percentage of individuals receiving OAT or opioid detoxification with buprenorphine in opioid treatment programs in California ranged from 0.6% to 4.1% over the study period. (53) Thus in publicly-funded treatment facilities, OAT and detoxification predominantly entailed offering methadone to treated individuals, as opposed to offering buprenorphine, buprenorphine/naloxone or naltrexone.
Statistical analysis
Our statistical analysis proceeded in four steps. First, we compared individual characteristics at treatment initiation between those without any records of criminal justice involvement over the study period and those with at least one such record. We used the chi-square test or Fisher’s exact test for categorical variables and the Wilcoxon rank sum test for continuous variables, respectively.
Second, the study outcome was most frequently zero, and non-zero costs were right-skewed (P < 0.001, skewness-kurtosis test; Appendix Figure 1 shows the distribution). Thus, a two-part multiple regression model, or hurdle model, estimated using generalized linear modeling (GLM), was constructed to account for these aspects of the cost data. (54) The first part modeled the probability of having non-zero crime costs (or the probability of criminal involvement) using a logit model specification while the second part estimated costs among those with criminal involvement, using a Gamma distribution and log link. We estimated our models using Stata’s twopm procedure, (55, 56) and we accounted for intra-individual correlation across repeated observations by estimating clustered robust (Huber-White) standard errors.
Third, we generated the associated effect of treatment engagement on daily costs of crime by applying the product rule of calculus and summing the estimated marginal effect associated with treatment (compared to the post-treatment state) for both stages of the two-part models, estimated at each individual’s respective covariate values. Effects were then averaged across all individuals included in our analytic sample and we interpreted the average marginal effects (AME) as the population effect associated with treatment on daily costs of crime. The second and third part of our statistical analysis were repeated for all drug treatment status classifications described above. We also computed AMEs specific to primary use of prescription opioids and heroin, to secondary use of stimulants, and by gender.
We controlled for other individual-specific fixed and time-varying effects in our analyses that were hypothesized to be associated with both costs of crime and treatment. (30, 31) Fixed covariates for vital demographic and socio-economic characteristics were drawn from the first treatment admission, including age at first treatment admission, education, gender, and ethnicity. As past arrests are likely to be strong predictors of criminal activity, (57–59) we also included indicators capturing history of any felonies and prison terms prior to treatment initiation. Time-varying measures were captured at the start of each treatment episode and we imputed these variables for post-treatment episodes. These included a control for entry into treatment from coercion from law enforcement, as it could influence the motivation to refrain from criminal activity, as well as indicators for daily primary drug use, daily secondary drug-use and concurrent secondary use of stimulants, as drug use intensity and stimulant use have been shown to influence costs of crime. (40) In addition, we controlled for current unstable housing, recent employment and for the potentially differential effect of episode duration on daily costs of crime with the inclusion of interaction terms between treatment state and duration.
Fourth, we computed the total costs of crime that would accumulate over a hypothetical 6-month period for those engaging in OAT and detoxification, respectively, by multiplying the median number of days in and out of treatment with estimated daily costs of crime for each respective state, derived from the previously-described baseline regression analysis. Given that a majority of individuals accessed treatment once over the study period, we chose a 6-month period in order to capture the observed median duration of one treatment episode for either detoxification or OAT (Appendix Figure 2). We also computed specific total costs of crime by primary drug use, secondary use of stimulants and gender. Finally, we compared total costs of crime across treatment modalities.
Sensitivity analysis
We considered four sensitivity analyses to determine the robustness of our results. First, as controlling for time-invariant unmeasured confounding by using each individual as their own control (i.e. a fixed effects specification) is not currently possible with standard statistical packages for our two-part model, we executed fixed effects estimations on each part of our model separately. Second, to address potential bias introduced by unobserved confounding that would change over time, we conducted a stratified analysis on the subset of individuals that had criminal justice involvement over the study period. Bias introduced from a potential change in motivation to refrain from criminal activity should thus be attenuated given that these individuals did not refrain from criminal activity. Third, we assessed the robustness of our results to different methods of calculating the costs of crime (45) (Appendix Table 1). Lastly, we executed our analysis according to a third-party payer perspective, whereby only costs borne by the criminal justice system are considered. Statistical analyses were executed in SAS version 9.3 and Stata version 13.1.
Results
Our study population included 31,659 uniquely identifiable individuals (Appendix Figure 3); the median age at first treatment admission was 32, 35.8% were women, and 37.1% primarily used prescription opioids. Over the entire study period 13,688 individuals (43.2%) had some criminal justice involvement and thus had at least one observation with crime costs greater than zero. Compared to those not involved with the criminal justice system, these individuals were younger (71.9% under 40 vs. 58.6%) and fewer were women (32.1% vs. 38.7%) (Table 2).
Table 2.
Individual characteristics at treatment initiation, by criminal justice involvement†
| No involvement (N = 17,971) | Some involvement (N = 13,688) | Total (N = 31,659) | |
|---|---|---|---|
| Female*** (%) | 38.7 | 32.1 | 35.8 |
| Age at first treatment admission***(%) | |||
| <18 | 0.6 | 0.7 | 0.6 |
| 18–30 | 37.1 | 47.8 | 41.7 |
| 30–40 | 20.9 | 23.4 | 22.0 |
| 40–50 | 20.5 | 18.5 | 19.7 |
| 50+ | 20.9 | 9.6 | 16.0 |
| Race/ethnicity*** (%) | |||
| White | 16.9 | 19.5 | 18.0 |
| Hispanic | 68.2 | 66.2 | 67.3 |
| Black | 7.6 | 8.0 | 7.8 |
| Other | 7.3 | 6.2 | 6.9 |
| Less than High school education*** (%) | 74.1 | 79.2 | 76.3 |
| Employed, part-time or full-time*** (%) | 31.6 | 29.0 | 30.5 |
| Homeless*** (%) | 5.6 | 8.4 | 6.8 |
| Self-referred to treatment*** (%) | 91.8 | 77.9 | 85.8 |
| Primary prescription opioids use (%) | 41.5 | 31.3 | 37.1 |
| Daily use of primary drug *** (%) | 70.2 | 72.9 | 71.4 |
| Age first used primary drug*** (%) | |||
| <16 | 13.6 | 18.0 | 15.5 |
| 16–30 | 65.9 | 68.1 | 66.9 |
| 30+ | 20.4 | 13.9 | 17.6 |
| Secondary drug problem type*** (%) | |||
| None reported | 59.7 | 52.8 | 56.7 |
| Stimulants‡ | 1.9 | 2.1 | 2.0 |
| Alcohol | 4.3 | 5.2 | 4.7 |
| Marijuana | 12.7 | 18.3 | 15.1 |
| Heroin | 6.2 | 7.1 | 6.6 |
| Other opiates§ | 15.2 | 14.5 | 14.9 |
| Daily use of secondary drug *** (%) | 13.8 | 15.8 | 14.6 |
| Arrests prior to treatment initiation (Median [IQR]) | 0 [0, 2] | 16 [6, 36] | 3 [0, 17] |
| Felonies prior to treatment initiation (Median [IQR]) | 0 [0, 0] | 6 [2, 14] | 1 [0, 7] |
| Any court appearance prior to treatment initiation (%) | 8.3 | 32.3 | 18.7 |
| Any incarceration prior to treatment initiation (%) | 6.1 | 25.9 | 14.7 |
p <0.05;
p <0.01;
p <0.001;
IQR: Interquartile range.
Criminal justice involvement is defined as having any criminal justice records over the study period.
includes methamphetamine, crack cocaine, and powder cocaine.
Includes oxycodone/OxyContin, other opiates or synthetics, and non-prescribed methadone; and also includes prescription opioid users reporting use of more than one category of other opiates.
Our analytic sample included a total of 98,102 treatment (OAT, detoxification) and post-treatment episodes. The 29.5% treatment and post-treatment episodes with non-zero costs had mean daily costs of $353.95: policing accounted for 37.9%; court, 30.3%; corrections, 23.3%; and criminal victimization, 8.5% (Appendix Figure 4 shows composition by treatment state).
The median time spent in treatment was 130 days (IQR: 23, 443) over a median observation time of 2.3 years (IQR: 1.2, 3.6) (Appendix Table 2) with 62.3% of all individuals recording one treatment episode during study follow-up, and 13.2% recording ≥3 episodes. The majority of individuals accessed a single form of treatment over the study period (43.2% OAT only; 30.8% detoxification only), 19.0% had a single detoxification episode with one or more OAT episodes, and 7.0% had more than one episode of both treatment modalities.
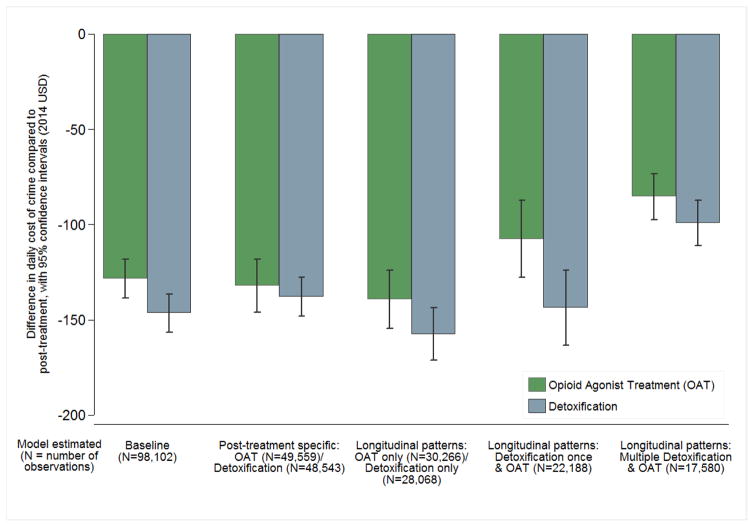
Treatment engagement and the costs of crime
OAT and detoxification were both associated with lower daily costs of crime compared to post-treatment periods in our baseline model (detailed results are presented in Table 3, Figure 2 & Appendix Table 3). When computing AMEs in models separating post-treatment episodes for OAT and detoxification, findings across treatment modalities remained of similar magnitude as in our baseline estimation but were closer to each other. Compared to our baseline model, individuals accessing a single form of treatment in our longitudinal treatment access patterns models had lower costs of crime with differences slightly larger in magnitude (versus post-treatment). While individuals with frequent repeated treatment periods also had lower costs of crime when compared to post-treatment periods, the differences were smaller in magnitude.
Table 3.
Daily costs of crime and difference estimated from average marginal effects (AME)† derived from a two-part multiple regression model‡ using CalOMS, DOJ, CDCR & CDC data, by treatment status classification|| (2014 USD).
| Daily costs of crime
|
Difference in daily costs of crime
|
||||
|---|---|---|---|---|---|
| Amount [95% C.I.]§ | Amount [95% C.I.] | % | |||
|
|
|
|
|||
| (A) Baseline (98,102 observations) | |||||
| Post-treatment | $167*** | [$158, $177] | Referent health state | ||
| OAT | $41*** | [$37, $45] | −$126*** | [−$136, −$116] | 75.4% |
| Detoxification | $23*** | [$19, $26] | −$144*** | [−$154, −$135] | 86.2% |
| (B) OAT/post-OAT (49,559 observations) | |||||
| Post-treatment | $169*** | [$155, $182] | Referent health state | ||
| OAT | $38*** | [$34, $42] | −$131*** | [−$144, −$117] | 77.5% |
| (B) Detoxification/post-Detoxification (48,543 observations) | |||||
| Post-treatment | $159*** | [$150, $169] | Referent health state | ||
| Detoxification | $24*** | [$21, $27] | −$136*** | [−$145, −$126] | 84.9% |
| (C) OAT only (30,266 observations) | |||||
| Post-treatment | $175*** | [$159, $190] | Referent health state | ||
| OAT | $35*** | [$31, $39] | −$140*** | [−$155, −$124] | 80.0% |
| (C) Detoxification only (28,068 observations) | |||||
| Post-treatment | $187*** | [$175, $200] | Referent health state | ||
| Detoxification | $33*** | [$27, $39] | −$154*** | [−$168, −$141] | 82.4% |
| (C) Detox once and OAT (22,188 observations) | |||||
| Post-treatment | $152*** | [$133, $171] | Referent health state | ||
| OAT | $10*** | [$8, $12] | −$104*** | [−$123, −$86] | 69.1% |
| Detoxification | $47*** | [$38, $57] | −$142*** | [−$160, −$124] | 93.4% |
| (C) Multiple OAT and detoxification (17,580 observations) | |||||
| Post-treatment | $118*** | [$107, $129] | Referent health state | ||
| OAT | $19*** | [$14, $24] | −$85*** | [−$97, −$73] | 72.0% |
| Detoxification | $33*** | [$28, $38] | −$99*** | [−$110, −$87] | 83.9% |
p-value<0.10
p-value<0.05
p-value<0.01;
CalOMS: California Outcomes Monitoring System; DOJ: California Department of Justice; CDCR: California Department of Corrections and Rehabilitation; CDC: Centers for Disease Control and Prevention, using the National Death Index; OAT: Opioid Agonist Treatment
AME are the average of the estimated marginal effect for every participant in the respective sample.
Model included covariates for gender, age at treatment entry, age at first use of primary drug, high school education, employment status, prescription opioid misuse, primary drug use intensity, secondary stimulant use, secondary drug use intensity, recent housing instability, duration of observation period, coercion into treatment from law enforcement and indicators for a history of incarceration or previous felonies.
Treatment status as described in the text: (A) Baseline with pooled post-treatment episodes; (B) Treatment specific post-treatment episodes; and (C) longitudinal treatment patterns.
Confidence intervals were derived using the delta method which relies on a first-order Taylor series expansion.
Figure 2.
Differences in daily costs of crime associated with opioid agonist treatment (OAT) and detoxification, (reference group: post-treatment) estimated from Average Marginal Effects (AME). Respective AME are generated from each distinct two-part model: baseline, treatment-specific post-treatment models using post-OAT and post-detoxification episodes, and for each of the mutually exclusive longitudinal treatment access patterns, defined as OAT only, detoxification only, detoxification once and OAT once or more, and multiple detoxification and OAT episodes.
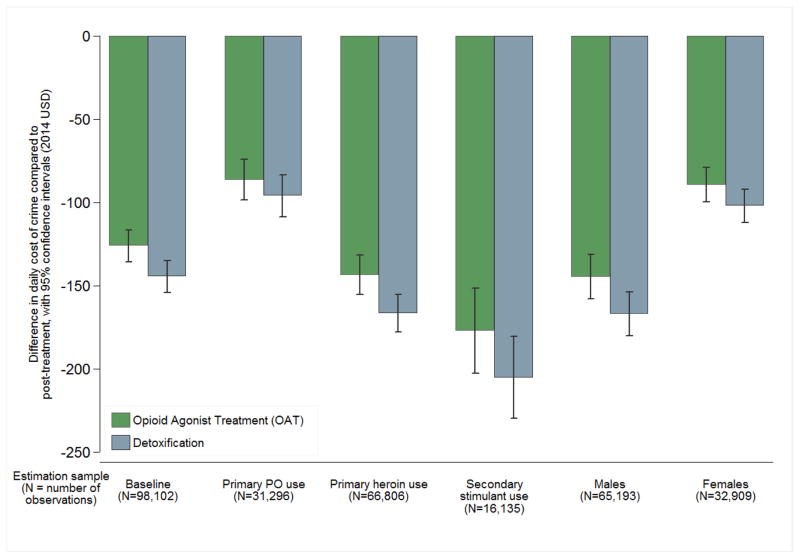
Figure 3 presents AME of treatment engagement estimated for different reported drug use and by gender. Associated cost differences compared to post-treatment periods were found to be greater for primary heroin use than for primary prescription opioids use, both for OAT ($143 lower (95% CI: $132, $155) vs. $86 lower ($74, $99)) and detoxification ($166 lower ($155, $178) vs. $96 lower ($84, $108)). Both forms of treatment were associated with even larger cost differences compared to post-treatment among individuals reporting secondary use of stimulants (OAT: $177 lower ($151, $203); detoxification: $205 lower ($180, $230)). Lastly, cost differences compared to post-treatment periods were found to be greater for males than for females, both for OAT ($145 lower ($131, $158) vs. $89 lower ($79, $100)) and detoxification ($166 lower ($154, $180) vs. $102 lower ($92, $112)).
Figure 3.
Differences in daily costs of crime associated with opioid agonist treatment (OAT) and detoxification (reference group: post-treatment), estimated from Average Marginal Effects (AME) in the baseline two-part model and compared to AME estimated in the baseline two-part model among individuals reporting primary drug use of PO or heroin, secondary use of stimulants, as well as by gender. PO: Prescription opioids.
Comparing hypothetical 6-month total costs of crime across treatment modalities
Initiating OAT as opposed to detoxification was associated with savings of $17,550 (95% CI: $16,840, $18,383) when summing total costs of crime over a hypothetical 6-month period using observed median treatment durations (Table 4). OAT was also associated with savings compared to detoxification when summing specific costs of crime by primary drug use, secondary use of stimulants and gender; savings were greatest for individuals reporting secondary stimulant use, were larger for primary heroin users compared to primary PO users, and savings among males were larger than those among females.
Table 4.
Total costs of crime‡ savings associated with OAT compared to detoxification, by sample stratification (2014 USD).
| Daily costs of crime
|
Duration of treatment
|
Total costs of crime over a hypothetical 6-month period†
|
Savings associated with OAT compared to detoxification
|
||||
|---|---|---|---|---|---|---|---|
| Amount [95% C.I.]§ | Days (Median) | Amount [95% C.I.] | Amount [95% C.I.] | ||||
|
|
|
|
|
||||
| (A) Baseline (98,102 observations) | |||||||
| Post-treatment | $167*** | [$158, $177] | |||||
| OAT | $41*** | [$37, $45] | 161 | $9,774 | [$8,959, $10,608] | $17,550 | [$16,840, $18,383] |
| Detoxification | $23*** | [$19, $26] | 19 | $27,324 | [$25,799, $28,991] | Referent health state | |
| (A) Primary PO use (31,296 observations) | |||||||
| Post-treatment | $112*** | [$99, $124] | |||||
| OAT | $26*** | [$21, $30] | 193 | $4,680 | [$3,780, $5,400] | $13,560 | [$12,280, $14,860] |
| Detoxification | $16*** | [$11, $21] | 20 | $18,240 | [$16,060, $20,260] | Referent health state | |
| (A) Primary heroin use (66,806 observations) | |||||||
| Post-treatment | $193*** | [$182, $203] | |||||
| OAT | $49*** | [$43, $55] | 145 | $13,860 | [$12,605, $15,080] | $17,707 | [$17,115, $18,173] |
| Detoxification | $26*** | [$22, $30] | 19 | $31,567 | [$29,720, $33,253] | Referent health state | |
| (A) Secondary stimulant use (16,135 observations) | |||||||
| Post-treatment | $233*** | [$210, $256] | |||||
| OAT | $56*** | [$41, $70] | 148 | $15,744 | [$12,788, $18,552] | $22,096 | [$21,212, $23,128] |
| Detoxification | $28*** | [$20, $36] | 20 | $37,840 | [$34,000, $41,680] | Referent health state | |
| (A) Males (65,193 observations) | |||||||
| Post-treatment | $191*** | [$178, $204] | |||||
| OAT | $46*** | [$41, $52] | 145 | $13,355 | [$12,175, $14,680] | $17,685 | [$16,705, $18,520] |
| Detoxification | $24*** | [$20, $28] | 20 | $31,040 | [$28,880, $33,200] | Referent health state | |
| (A) Females (32,909 observations) | |||||||
| Post-treatment | $121*** | [$112, $130] | |||||
| OAT | $31*** | [$26, $37] | 190 | $5,580 | [$4,680, $5,580] | $14,262 | [$13,618, $14,707] |
| Detoxification | $19*** | [$14, $23] | 19 | $19,842 | [$18,298, $21,367] | Referent health state | |
p-value<0.10
p-value<0.05
p-value<0.01;
CalOMS: California Outcomes Monitoring System; DOJ: California Department of Justice; CDCR: California Department of Corrections and Rehabilitation; CDC: Centers for Disease Control and Prevention, using the National Death Index; OAT: Opioid Agonist Treatment
Confidence intervals were derived using the delta method which relies on a first-order Taylor series expansion.
Daily costs of crime were estimated from a two-part multiple regression model using CalOMS, DOJ, CDCR & CDC data; Baseline model (A) included covariates for gender, age at treatment entry, age at first use of primary drug, high school education, employment status, prescription opioid misuse, primary drug use intensity, secondary stimulant use, secondary drug use intensity, recent housing instability, duration of observation period, coercion into treatment from law enforcement and indicators for a history of incarceration or previous felonies.
Total costs of crime were computed by multiplying the median number of days in and out of treatment with estimated daily costs of crime for each respective state, derived from the baseline model. Given that a majority of individuals accessed treatment once over the study period, we chose a 6-month period in order to capture the observed median duration of one treatment episode for either detoxification or OAT.
Sensitivity analysis
Results of the sensitivity analyses are presented in the Appendix Table 4, 5 & 6. Our fixed-effect estimation results for the first-part of the model were identical, and relative estimated differences were robust for the second-part of the model. Similarly, relative differences from the stratified analysis on individuals with criminal justice involvement were also robust. Results using an alternative method for calculating costs remained robust. While smaller in magnitude, we believe that the quality of our data allowed for a highly detailed account of the costs imposed to the criminal justice system, with returning parolees and probationers driving this difference. Lastly, using a third-party payer perspective only resulted in a relatively small magnitude change.
Discussion
Using linked administrative data for the state of California (2006–2010) among individuals initiating treatment for OUD for the first time in publicly-funded treatment facilities, we found that engagement in treatment was associated with lower costs of crime compared to post-treatment periods, and that the accumulated differences have the potential to be far greater for OAT than for detoxification. While this finding of considerably greater economic benefits for time-unlimited treatment is intuitive given that individuals remain in OAT longer, (41) we did not compare against an untreated sample of individuals with OUD, a counterfactual our data did not allow us to consider. OUD is a chronic, recurrent illness characterized by cyclical episodes of treatment and relapse (61–65) and we interpret these cumulative differences between OAT and detoxification as indicative of the stabilizing effects of OAT, akin to previous results showing that OAT access among HIV positive individuals with OUD increased medication adherence and independently reduced all-cause mortality. (66, 67) Whereas the clinical importance of treatment for OUD in reducing opioid-related mortality, (1, 2) controlling infectious disease, (68) and improving patients’ lives (4–7) has been previously shown, we have demonstrated a compelling case for the importance of evidence-based treatment in reducing the economic burden imposed on society by OUD.
Another finding emerging from our results was that the differences in the costs of crime between treatment and post-treatment periods were found to be larger given more entrenched drug use, as characterized by poorer treatment outcomes and greater drug use severity associated with heroin use compared to prescription opioid use, (41, 69) as well as among individuals reporting concurrent stimulant use. This gradient effect is consistent with previous findings of higher levels of criminal activity with higher- intensity drug use and polydrug use. (70, 71)
While we are not aware of direct comparators for our findings, costs of crime estimates from limited-duration randomized control trial settings with treatment arms composed of individuals receiving OAT with methadone may provide some context, despite critical differences in study design. Given observed median durations of OAT engagement and subsequent post-treatment periods, our average daily costs of crime over a hypothetical 1-year period were $113 (CI: $105, $120), whereas Dijkgraaf et al. (5) found daily costs of crime to be $230 among OUD treatment-resistant individuals in the Netherlands, and Nosyk et al. (7) found daily costs of crime to be $212 among individuals with long-standing OUD and multiple failed treatment attempts in Canada. Beyond marked differences in study settings, we believe the dissimilarities were driven by the contrast between our treatment-naïve study population and the other studies’ marginalized patients that were not benefiting from OAT in terms of sustained abstention from the use of illicit opioids.
Our findings have important fiscal and public health implications. America’s public perception of OUD has been framed more often as a criminal justice issue than a treatable health condition. (72) However, the opioid-led drug overdose epidemic (73) and more recent evidence of individuals transitioning from prescription opioid use to heroin use (74–77) have led to calls to improve access to treatment, including a recent Presidential Memorandum. (16, 78–81) Far more individuals are in need of OUD treatment than can access it; (82) the primary reasons include lack of accessibility or availability as well as treatment costs, (37, 82) and as our findings have shown, individuals with OUD spend most of their time out of treatment. Transitions from treatment to abstinence are typically rare and short-lived, with frequent relapse, (63) and the substantial increases in mortality immediately following treatment interruption convey the serious risks associated with abstinence-based treatment for OUD. Specifically, as previously shown within this study’s cohort, the standardized mortality ratio in the two-week period following treatment discontinuation was 31.5 (95%CI: 26.2, 37.5) compared to 1.8 (1.6, 2.1) during treatment and 6.1 (5.7, 6.5) during all out-of-treatment periods. (1) Our observation that individuals with OUD had relatively little exposure to maintenance-oriented treatment over the duration of follow-up, despite its proven effectiveness, further highlights the need to improve treatment-engagement strategies.
In a time where California and other states contend with historically difficult budget conditions, the important economic benefits to society we found to be associated with treatment for OUD highlight that policy concerns regarding access to time-unlimited treatment should be seen as complimentary, rather than contrary to the notion of fiscal responsibility.
The strengths of this study include the large and ethnically diverse sample, inclusion of all publicly funded treatment facilities statewide, and a comprehensive accounting of individual-level criminal justice system interactions with few parallels in scope and data granularity in the published literature. Nonetheless, our analysis had several limitations. First, while some misclassification is inherent in research conducted using administrative databases, we implemented a number of decision rules from previously-implemented methodology to minimize linkage and data preparation errors. (41, 44) Second, we did not measure effects of treatment provided in other settings (e.g. office-based buprenorphine treatment, treatment in non-publicly funded facilities). However, while buprenorphine treatment is available in office-based settings in California, prior studies have suggested that those accessing office-based treatment are unlikely to have also accessed treatment at publicly-funded facilities. (83) Third, given that our study population was characterized by low levels of educational attainment and employment, and that California applies regulations for OUD treatment that are more stringent than existing federal regulations, (51) caution must be exercised in applying our findings to other populations or settings. Nonetheless, we believe our results provide considerable insight into the effects of treatment for OUD on criminal justice system involvement. Fourth, given the nature of criminal justice policies in California, caution must also be exercised in generalizing these results to other jurisdictions. Also, the Californian Assembly passed the Public Safety Realignment Act in 2011 (AB109) in order to mitigate prison overcrowding as a response to the U.S. Supreme Court (Brown v. Plata, 2011) and realignment has been impacting every stage and level of the criminal justice process. (84) Greater access to treatment was at the core of AB109 but initially only a small portion of budgetary allotment was given to agencies providing treatment services. (85) These recent policy changes would surely impact the results presented, although the direction of the effect is unclear. Fifth, linkage to health administrative databases was not possible and we did not measure effects of other forms of public support. Given California’s high rate of unmet need for illicit drug use treatment, (24) it is unlikely that the effects of support not specifically targeted at OUD would change the conclusions from our findings. Furthermore, the median observation time was 2.3 years. Individuals often require three or more treatment episodes over a number of years before sustaining abstinence (86) and remain engaged in OAT far longer than in detoxification. Although our sample was restricted to individuals accessing treatment, as opposed to individuals not accessing treatment, and that we attempted to control, in several ways, for factors that could influence motivation to refrain from criminal activity and for selection into either form of treatment (OAT or detoxification), selection effects may still have been influenced by unmeasured factors. Of course, an experimental design to generate unbiased estimates of the effects of drug treatment on the costs of crime is not ethically feasible. Given our expectation that OAT individuals had greater addiction severity, if observed over a longer time horizon, the cumulative economic benefits associated with OAT may be greater than demonstrated by the present study.
Conclusion
Our results suggest that the lower costs of crime associated with treatment engagement compared to post-treatment periods can substantially alleviate the economic burden to society of OUD, and that the economic benefits can be far greater for individuals receiving time-unlimited treatment. These findings serve to further underline the need for widespread and unencumbered access to evidence-based treatment for individuals with opioid use disorder.
Supplementary Material
Acknowledgments
Supported by: NIDA R01DA031727 (PI: Nosyk) R01DA032551 (PI: Nosyk) P30DA016383 (PI: Hser)
Footnotes
Conflicts of interest: None.
References
- 1.Evans E, Li L, Min J, Huang D, Urada D, Liu L, et al. Mortality among individuals accessing pharmacological treatment for opioid dependence in California, 2006–10. Addiction. 2015;110(6):996–1005. doi: 10.1111/add.12863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Degenhardt L, Bucello C, Mathers B, Briegleb C, Ali H, Hickman M, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction. 2011;106(1):32–51. doi: 10.1111/j.1360-0443.2010.03140.x. [DOI] [PubMed] [Google Scholar]
- 3.Volkow N, Montaner J. The urgency of providing comprehensive and integrated treatment for substance abusers with HIV. Health Aff (Millwood) 2011;30(8):1411–9. doi: 10.1377/hlthaff.2011.0663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abuse Treat. 2005;28(15925266):321–9. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 5.Dijkgraaf MGW, van der Zanden BP, de Borgie CAJM, Blanken P, van Ree JM, van den Brink W. Cost utility analysis of co-prescribed heroin compared with methadone maintenance treatment in heroin addicts in two randomised trials. BMJ. 2005;330(15933353):1297. doi: 10.1136/bmj.330.7503.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gossop M, Marsden J, Stewart D, Kidd T. The National Treatment Outcome Research Study (NTORS): 4–5 year follow-up results. Addiction. 2003;98(3):291–303. doi: 10.1046/j.1360-0443.2003.00296.x. [DOI] [PubMed] [Google Scholar]
- 7.Nosyk B, Guh DP, Bansback NJ, Oviedo-Joekes E, Brissette S, Marsh DC, et al. Cost-effectiveness of diacetylmorphine versus methadone for chronic opioid dependence refractory to treatment. CMAJ. 2012;184(22410375):317–28. doi: 10.1503/cmaj.110669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Werb D, Kerr T, Marsh D, Li K, Montaner J, Wood E. Effect of methadone treatment on incarceration rates among injection drug users. Eur Addict Res. 2008;14(18552490):143–9. doi: 10.1159/000130418. [DOI] [PubMed] [Google Scholar]
- 9.Prendergast ML, Podus D, Chang E, Urada D. The effectiveness of drug abuse treatment: a meta-analysis of comparison group studies. Drug Alcohol Depend. 2002;67(1):53–72. doi: 10.1016/s0376-8716(02)00014-5. [DOI] [PubMed] [Google Scholar]
- 10.Rajkumar AS, French MT. Drug abuse, crime costs, and the economic benefits of treatment. J Quant Criminol. 1997;13(3):291–323. [Google Scholar]
- 11.Marsch LA. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: a meta-analysis. Addiction. 1998;93(4):515–32. doi: 10.1046/j.1360-0443.1998.9345157.x. [DOI] [PubMed] [Google Scholar]
- 12.Hall W. Methadone maintenance treatment as a crime control measure [letter, see comments] BMJ. 1996;312:1162. [Google Scholar]
- 13.Sheerin I, Green T, Sellman D, Adamson S, Deering D. Reduction in crime by drug users on a methadone maintenance therapy programme in New Zealand. N Z Med J. 2004;117:15107898. [PubMed] [Google Scholar]
- 14.Farabee David, Shen Haikang, Hser Yih-Ing, Grella Christine E, Douglas Anglin M. The effect of drug treatment on criminal behavior among adolescents in DATOS-A. J Adolesc Res. 2001;16(6):679–96. [Google Scholar]
- 15.US Department of Health and Human Services. Addressing prescription drug abuse in the United States: current activities and future opportunities. 2013. [Google Scholar]
- 16.Han B, Compton WM, Jones CM, Cai R. Nonmedical Prescription Opioid Use and Use Disorders Among Adults Aged 18 Through 64 Years in the United States, 2003–2013. JAMA. 2015;314(14):1468–78. doi: 10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- 17.Association AD. Economic costs of diabetes in the US in 2012. Diabetes Care. 2013;36(4):1033–46. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes, metabolic syndrome and obesity: targets and therapy. 2010;3:285. doi: 10.2147/DMSOTT.S7384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Drug Intelligence Center. The Economic Impact of Illicit Drug Use on American Society. U.S. Department Of Justice; 2011. Report No.: Product No. 2011-Q0317-002. [Google Scholar]
- 20.Office of the National Drug Control Policy. National Drug Control Budget: FY 2015 Funding Highlights. 2014. [Google Scholar]
- 21.Anglin MD, Nosyk B, Jaffe A, Urada D, Evans E. Offender Diversion Into Substance Use Disorder Treatment: The Economic Impact of California’s Proposition 36. Am J Public Health. 2013;103(6):1096–102. doi: 10.2105/AJPH.2012.301168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anglin MD, Urada D, Brecht ML, Hawken A, Rawson R, Longshore D. Criminal justice treatment admissions for methamphetamine use in California: a focus on Proposition 36. J Psychoactive Drugs. 2007;(Suppl 4):367–81. doi: 10.1080/02791072.2007.10399898. [DOI] [PubMed] [Google Scholar]
- 23.Kyckelhahn T. Justice Expenditure and Employment Extracts, 2010-Final. 2014. [Google Scholar]
- 24.Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: 2014. Contract No.: HHS Publication No. (SMA) 14–4863. [PubMed] [Google Scholar]
- 25.US Department of Health Human Services. Results from the 2014 National Survey on Drug Use and Health: Summary of national findings. Substance Abuse and Mental Health Services Administration; Rockville, MD, USA: 2015. [Google Scholar]
- 26.Anglin MD, Perrochet B. Drug use and crime: a historical review of research conducted by the UCLA Drug Abuse Research Center. Subst Use Misuse. 1998;33(9):1871–914. doi: 10.3109/10826089809059325. [DOI] [PubMed] [Google Scholar]
- 27.Farabee David, Joshi Vandana, Douglas Anglin M. Addiction careers and criminal specialization. Crime & Delinquency. 2001;47(2):196–220. [Google Scholar]
- 28.Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch Gen Psychiatry. 2001;58(5):503–8. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- 29.Wall R, Rehm J, Fischer B, Brands B, Gliksman L, Stewart J, et al. Social costs of untreated opioid dependence. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2000;77(4):688–722. doi: 10.1007/BF02344032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeBeck K, Shannon K, Wood E, Li K, Montaner J, Kerr T. Income generating activities of people who inject drugs. Drug Alcohol Depend. 2007;91(1):50–6. doi: 10.1016/j.drugalcdep.2007.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bukten A, Roislien J, Skurtveit S, Waal H, Gossop M, Clausen T. A day-by-day investigation of changes in criminal convictions before and after entering and leaving opioid maintenance treatment: a national cohort study. BMC Psychiatry. 2013;13(1):1–7. doi: 10.1186/1471-244X-13-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldstein A, Herrera J. Heroin addicts and methadone treatment in Albuquerque: a 22-year follow-up. Drug Alcohol Depend. 1995;40(2):139–50. doi: 10.1016/0376-8716(95)01205-2. [DOI] [PubMed] [Google Scholar]
- 33.Brecht M, Huang D, Evans E, Hser Y. Polydrug use and implications for longitudinal research: ten-year trajectories for heroin, cocaine, and methamphetamine users. Drug Alcohol Depend. 2008;96(3):193–201. doi: 10.1016/j.drugalcdep.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nunn A, Zaller N, Dickman S, Trimbur C, Nijhawan A, Rich JD. Methadone and buprenorphine prescribing and referral practices in US prison systems: results from a nationwide survey. Drug Alcohol Depend. 2009;105(1–2):83–8. doi: 10.1016/j.drugalcdep.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Samet JH, Fiellin DA. Opioid substitution therapy—time to replace the term. The Lancet. 2015;385(9977):1508–9. doi: 10.1016/S0140-6736(15)60750-4. [DOI] [PubMed] [Google Scholar]
- 36.Weil AR. High-Cost Populations, The ACA, And More. Health Affairs. 2016;35(1):7. doi: 10.1377/hlthaff.2015.1562. [DOI] [PubMed] [Google Scholar]
- 37.Nosyk B, Anglin MD, Brissette S, Kerr T, Marsh DC, Schackman BR, et al. A call for evidence-based medical treatment of opioid dependence in the United States and Canada. Health Affairs. 2013;32(8):1462–9. doi: 10.1377/hlthaff.2012.0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Doran CM. Economic evaluation of interventions to treat opiate dependence: a review of the evidence. PharmacoEconomics. 2008;26(5):371–93. doi: 10.2165/00019053-200826050-00003. [DOI] [PubMed] [Google Scholar]
- 39.Murphy SM, Polsky D. Economic Evaluations of Opioid Use Disorder Interventions. PharmacoEconomics. 2016:1–25. doi: 10.1007/s40273-016-0400-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krebs E, Kerr T, Montaner J, Wood E, Nosyk B. Dynamics in the costs of criminality among opioid dependent individuals. Drug Alcohol Depend. 2014;144:193–200. doi: 10.1016/j.drugalcdep.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nosyk B, Li L, Evans E, Urada D, Huang D, Wood E, et al. Utilization and outcomes of detoxification and maintenance treatment for opioid dependence in publicly-funded facilities in California, USA: 1991–2012. Drug Alcohol Depend. 2014;143:149–57. doi: 10.1016/j.drugalcdep.2014.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.California Department of Health Care Services. California Outcome Measurement System Treatment (CalOMS TX) Data Compliance Standards. 2014. Contract No.: Document 3S Version 2.0. [Google Scholar]
- 43.Hser Y-I, Evans E. Cross-system data linkage for treatment outcome evaluation: Lessons learned from the California Treatment Outcome Project. Evaluation and Program Planning. 2008;31(2):125–35. doi: 10.1016/j.evalprogplan.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krebs E, Min JE, Evans E, Li L, Liu L, Huang D, et al. Estimating state transitions for opioid use disorders. Medical Decision Making (2nd review) 2016 doi: 10.1177/0272989X16683928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McCollister KE, French MT, Fang H. The cost of crime to society: New crime-specific estimates for policy and program evaluation. Drug Alcohol Depend. 2010;108(1–2):98–109. doi: 10.1016/j.drugalcdep.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Garrison LP, Mansley EC, Abbott TA, Bresnahan BW, Hay JW, Smeeding J. Good Research Practices for Measuring Drug Costs in Cost-Effectiveness Analyses: A Societal Perspective: The ISPOR Drug Cost Task Force Report-Part II. Value Health. 2010;13(1):8–13. doi: 10.1111/j.1524-4733.2009.00660.x. [DOI] [PubMed] [Google Scholar]
- 47.Board of State and Community Corrections. Average daily cost to house inmates in type II and III local detention facilities. 2012. [Google Scholar]
- 48.Legislative Analyst’s Office. How much does it cost to incarcerate an inmate? 2009 [Available from: http://www.lao.ca.gov/PolicyAreas/CJ/6_cj_inmatecost.
- 49.Longshore D, Urada D, Hawken A. Evaluation of the Substance Abuse and Crime Prevention Act Final Report. Department of Alcohol and Drug Programs California Health and Human Services Agency; 2007. [Google Scholar]
- 50.Washington State Institute for Public Policy. Benefit-cost technical documentation. Olympia, WA: 2014. [Google Scholar]
- 51.Stephenson D. Guideline for physicians working in California opioid treatment programs. San Francisco, CA: California Society of Addiction Medicine CSAM Committee on Treatment of Opioid Dependence; 2008. pp. 1–152. [Google Scholar]
- 52.Substance Abuse and Mental Health Services Administration. Federal Guidelines for Opioid Treatment Programs. Rockville, MD: 2015. Report No.: HHS Publication No. (SMA) PEP15-FEDGUIDEOTP. [Google Scholar]
- 53.Substance Abuse and Mental Health Services Administration. Data on Substance Abuse Treatment Facilities DASIS Series S–59, HHS Publication No(SMA) 2011. National Survey of Substance Abuse Treatment Services (N–SSATS): 2010; pp. 11–4665. [Google Scholar]
- 54.Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465–88. doi: 10.1016/j.jhealeco.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 55.Belotti F, Deb P, Manning WG, Norton EC. twopm: Two-part models. Stata J. 2015;15(1):3–20. [Google Scholar]
- 56.StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- 57.Bayer P, Hjalmarsson R, Pozen D. Building Criminal Capital Behind Bars: Peer Effects in Juvenile Corrections. Q J Econ. 2009;124(1):105–47. [Google Scholar]
- 58.Glaeser EL, Sacerdote B, Scheinkman JA. Crime and social interactions. Q J Econ. 1996;111(2):507–48. [Google Scholar]
- 59.Nurco DN. A long-term program of research on drug use and crime. Subst Use Misuse. 1998;33(9):1817–37. doi: 10.3109/10826089809059323. [DOI] [PubMed] [Google Scholar]
- 60.Manning WG, Mullahy J. Estimating log models: To transform or not to transform? Journal of Health Economics. 2001;20(4):461–94. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 61.Bell J, Burrell T, Indig D, Gilmour S. Cycling in and out of treatment; participation in methadone treatment in NSW, 1990–2002. Drug Alcohol Depend. 2006;81(1):55–61. doi: 10.1016/j.drugalcdep.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 62.Hser Y, Longshore D, Anglin M. The life course perspective on drug use: a conceptual framework for understanding drug use trajectories. Eval Rev. 2007;31(6):515–47. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- 63.Nosyk B, Anglin MD, Brecht ML, Lima VD, Hser YI. Characterizing Durations of Heroin Abstinence in the California Civil Addict Program: Results From a 33-Year Observational Cohort Study. Am J Epidemiol. 2013;177(7):675–82. doi: 10.1093/aje/kws284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nosyk B, MacNab YC, Sun H, Marsh DC, Fischer B, Schechter MT, et al. Proportional hazards frailty models for recurrent methadone maintenance treatment. Am J Epidemiol. 2009;170(6):783–92. doi: 10.1093/aje/kwp186. [DOI] [PubMed] [Google Scholar]
- 65.McLellan T, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA: the journal of the American Medical Association. 2000;284(13):1689–95. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 66.Nosyk B, Min JE, Evans E, Li L, Liu L, Lima VD, et al. The effects of opioid substitution treatment and highly active antiretroviral therapy on the cause-specific risk of mortality among HIV positive people who inject drugs. Clinical Infectious Diseases. 2015:civ476. doi: 10.1093/cid/civ476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nosyk B, Min JE, Colley G, Lima V, Yip B, Milloy M, et al. The causal effect of opioid substitution treatment on highly active antiretroviral treatment adherence. Drug Alcohol Depend. 2015;146:e53–e4. [Google Scholar]
- 68.Volkow ND, Montaner J. The urgency of providing comprehensive and integrated treatment for substance abusers with HIV. Health Aff (Millwood) 2011;30(8):1411–9. doi: 10.1377/hlthaff.2011.0663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Meyer AC, Miller ME, Sigmon SC. Lifetime history of heroin use is associated with greater drug severity among prescription opioid abusers. Addictive behaviors. 2015;42:189–93. doi: 10.1016/j.addbeh.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Best D, Sidwell C, Gossop M, Harris J, Strang J. Crime and Expenditure amongst Polydrug Misusers Seeking Treatment The Connection between Prescribed Methadone and Crack Use, and Criminal Involvement. Br J Criminol. 2001;41(1):119–26. [Google Scholar]
- 71.Stewart D, Gossop M, Marsden J, Rolfe A. Drug misuse and acquisitive crime among clients recruited to the National Treatment Outcome Research Study (NTORS) Crim Behav Ment Health. 2000;10(1):10–20. [Google Scholar]
- 72.McGinty EE, Kennedy-Hendricks A, Baller J, Niederdeppe J, Gollust S, Barry CL. Criminal Activity or Treatable Health Condition? News Media Framing of Opioid Analgesic Abuse in the United States, 1998–2012. Psychiatr Serv. 2015 doi: 10.1176/appi.ps.201500065. [DOI] [PubMed] [Google Scholar]
- 73.Centers for Disease Control and Prevention. CDC Grand Rounds: Prescription Drug Overdoses — a U.S. Epidemic. 2012. Contract No.: 1. [PubMed] [Google Scholar]
- 74.Dasgupta N, Creppage K, Austin A, Ringwalt C, Sanford C, Proescholdbell SK. Observed transition from opioid analgesic deaths toward heroin. Drug Alcohol Depend. 2014;145:238–41. doi: 10.1016/j.drugalcdep.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 75.Hedegaard H, Chen L, Warner M. Drug-poisoning deaths involving heroin: United States, 2000–2013. Hyattsville, MD: CDC. National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 76.Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D. “Every ‘never’I ever said came true”: transitions from opioid pills to heroin injecting. International Journal of Drug Policy. 2014;25(2):257–66. doi: 10.1016/j.drugpo.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Unick GJ, Rosenblum D, Mars S, Ciccarone D. Intertwined epidemics: national demographic trends in hospitalizations for heroin-and opioid-related overdoses, 1993–2009. PloS one. 2013;8(2):e54496. doi: 10.1371/journal.pone.0054496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Meyer R, Patel AM, Rattana SK, Quock TP, Mody SH. Prescription opioid abuse: a literature review of the clinical and economic burden in the United States. Population health management. 2014;17(6):372–87. doi: 10.1089/pop.2013.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Saloner B, Karthikeyan S. Changes in Substance Abuse Treatment Use Among Individuals With Opioid Use Disorders in the United States, 2004–2013. JAMA. 2015;314(14):1515–7. doi: 10.1001/jama.2015.10345. [DOI] [PubMed] [Google Scholar]
- 80.The White House. Presidential Memorandum -- Addressing Prescription Drug Abuse and Heroin Use. Office of the Press Secretary; 2015. [Available from: https://www.whitehouse.gov/the-press-office/2015/10/21/presidential-memorandum-addressing-prescription-drug-abuse-and-heroin. [Google Scholar]
- 81.Wu L-T, Woody GE, Yang C, Mannelli P, Blazer DG. Differences in onset and abuse/dependence episodes between prescription opioids and heroin: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Substance abuse and rehabilitation. 2011;2011(2):77. doi: 10.2147/SAR.S18969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jones CM, Campopiano M, Baldwin G, McCance-Katz E. National and state treatment need and capacity for opioid agonist medication-assisted treatment. American journal of public health. 2015;105(8):e55–e63. doi: 10.2105/AJPH.2015.302664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Andrews CM, D’Aunno TA, Pollack HA, Friedmann PD. Adoption of evidence-based clinical innovations: the case of buprenorphine use by opioid treatment programs. Med Care Res Rev. 2013 doi: 10.1177/1077558713503188. 1077558713503188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Petersilia J. California Prison Downsizing and Its Impact on Local Criminal Justice Systems. Harvard Law & Policy Review. 2014;8(2):327–57. [Google Scholar]
- 85.McCray A, Newhall K, Snyder JG. Realigning the revolving door? An analysis of California counties’ AB 109 implementation plans. Stanford Law School Criminal Justice Center; 2012. [Google Scholar]
- 86.Hser Y. Predicting long-term stable recovery from heroin addiction: findings from a 33-year follow-up study. J Addict Dis. 2007;26(1):51–60. doi: 10.1300/J069v26n01_07. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.