Abstract
Despite growing recognition that cumulative adversity (total stressor exposure), including complex trauma, increases the risk for psychopathology and impacts development, assessment strategies lag behind: Trauma-related mental health needs (symptoms, functional impairment, maladaptive coping) are typically assessed in response to only one qualifying Criterion-A event. This is especially problematic for youth at-risk for health and academic disparities who experience cumulative adversity, including non-qualifying events (parental separations) which may produce more impairing symptomatology. Data from 118 delinquent girls demonstrate: 1) an average of 14 adverse Criterion-A and non-Criterion event exposures; 2) serious maladaptive coping strategies (self-injury) directly in response to cumulative adversity; 3) more cumulative adversity-related than worst-event related symptomatology and functional impairment; and 4) comparable symptomatology, but greater functional impairment, in response to non-Criterion events. These data support the evaluation of mental health needs in response to cumulative adversity for optimal identification and tailoring of services in high-risk populations to reduce disparities.
Keywords: Cumulative Adversity, Adverse Childhood Experiences, Loss, Functional Impairment, High-Risk Youth, Delinquent Girls
1. Introduction
Increasing evidence supports notable adversity exposure to stressful life events in child and adult community samples,1–6 with extreme levels among marginalized populations, such as child welfare and juvenile justice system-involved youth.7,8 Adversity exposure has been captured in research on ‘Adverse Childhood Experiences’ (‘ACEs’ include ten adversities: childhood physical, sexual or emotional abuse, emotional or physical neglect, household dysfunction related to divorce or a battered mother, a household member with substance abuse, mental illness and/or incarceration history),1,9 Post-traumatic Stress Disorder (PTSD, qualifying adversities are high-magnitude and typically ‘life-threatening’),10 poly-victimization (adversity defined as multiple types of victimizations),4 ‘low magnitude’ events (adversities such as death of a loved one),11 and microtraumas (accumulated adversities exceeding personal resources, with harm related to appraisals/interpretations: e.g., chronic bullying/humiliation).12 Complex trauma, capturing ongoing/repeated, often early-onset, inescapable interpersonal traumas such as childhood maltreatment, which produce symptom complexity13–19 and cumulative adversity (total stressor exposure, ranging from microtraumas to ACEs and complex trauma exposure)20 provide a theoretical framework that best captures the adversity pattern of delinquents, who experience numerous early-onset stressors.
Specifically, in large scale studies of detained youth, 45% of girls compared to 27% of boys experienced ≥5/10 ACEs.8 Among delinquent youth, those with high cumulative adversity exposure have more severe emotional and behavioral problems relative to low exposure delinquents,21 and those identified as high-risk for reoffending (psychosocial indicators such as past criminality, aggression, substance use)8 experienced significantly more adversities than delinquents identified as low-risk for reoffending. In addition to links with lifespan criminality,22,23 cumulative adversity literatures indicate significant mental and medical public health concerns, which increase disadvantage and widen disparities.
The impact of cumulative adversity on disparities is demonstrated through a dose-response, graded relationship between number of adversities and severity of health problems; 24,25 with more adverse experiences closely linked to more severe exposures, which impart the greatest morbidity.26 The experience of multiple types of adversity also increases the risk for psychopathology more than exposure to only one event-type, or even multiple instances of a single, very serious, event-type such as sexual abuse.3,4,27 Among youth, cumulative adversity is related to a range of poor outcomes, including negative neurological outcomes (e.g., smaller cerebral volume with maltreatment; reduced left pars opercularis surface area in delinquents with cumulative trauma, adversity and grief), cognitive dysfunction (e.g., poor attention), academic difficulties, mental health problems (e.g., anxiety, mood disturbance, suicidality), substance use, psychosocial issues (aggression, perpetration, victimization) and increased risk for PTSD in response to new stressors.22,28–32 These data indicate the urgency of directly addressing serious adversity among delinquent youth to reduce criminal engagement and promote optimal health.
Importantly, the cumulative adversity literatures have also expanded our understanding of what types of adverse experiences are linked to increased risk for serious health problems. In contrast, the Diagnostic and Statistics Manual [DSM]10,33,34 has consistently utilized a relatively narrow definition of “traumatic” adversities (e.g., rape), with many events not qualifying as Criterion precipitating events (emotional neglect, parental incarceration). From a diagnostic standpoint, PTSD requires a qualifying precipitating event that involves direct, witnessed or indirect (learned about) exposure to “actual or threatened death, serious injury, or sexual violence” (Criterion-A, page 271).10 Although Criterion-A modifications have occurred during DSM revisions (e.g., events are no longer required to be “outside the range of usual human experience”), the criterion event requirement still captures more extreme exposure-types and restricts diagnosis on event-type regardless of symptom severity or impairment. While narrowing the criteria to reduce over-pathologizing individuals is important, the result can be problematic because: 1) there is disagreement among clinicians and researchers with regards to whether some events qualify as Criterion-A;35 2) research indicates that non-Criterion events are often associated with more PTSD-type symptomatology, greater symptom severity than Criterion-A qualifying events, and higher rates of PTSD “diagnosis” when Criterion-A requirements are disregarded; 35–37 and 3) some non-qualifying events occurring during childhood (e.g., neglect, extended separations from caregivers) may have profound developmental consequences.14 This issue is especially salient in populations experiencing high cumulative adversity, such as delinquents, whose adversities include numerous non-Criterion events, which impact safety, security and livelihood (e.g., residential instability, death of a caregiver, poverty).30,38–41 Current criteria, however, preclude querying potentially clinically meaningful symptomatology related to these non-qualifying adversity experiences.
Similarly, querying symptoms and impairment in response to a single adverse event may pose significant barriers to accurate detection and treatment in populations experiencing high cumulative adversity who may struggle to: 1) identify a single ‘worst’ event amongst a variety of adversities; 2) discern which symptoms are associated with, or exacerbated by, a single event; and 3) determine whether that single event-response is what imparts functional impairment. This assessment oversight is important as converging evidence simultaneously points to extremely elevated rates of cumulative adversity exposure (e.g., total stressor exposures that include criterion traumatic and non-criterion stressful events),9,42 and yet highly variable rates of trauma-related disorders, among delinquent youth. Specifically, PTSD estimates among delinquent populations range between zero and 48.9% using a variety of samples and methods (e.g., current or lifetime focus; interviews versus self-reports; querying symptoms based on ‘worst’ event or event-independent methods).43,44 For example, restricting diagnosis to a single Criterion-A worst event among detained (pre-sentence) youth resulted in 14.7% of girls and 10.9% boys meeting PTSD diagnostic criteria in the last year.43 In contrast, among adjudicated (post-sentence) youth, 48.9% of girls, and 32.3% of males, meet PTSD criteria in the last three months when querying symptoms independent of any specific event.45 Although both studies show higher rates of PTSD among delinquent girls than boys and much higher rates among delinquents than community samples (6.3% of females and 3.7% of males met criteria for PTSD in the past six months),12 it is likely that actual symptom severity is underestimated when queries are limited to one Criterion-A worst event in a population experiencing cumulative adversities that include a range of event-types. Despite recognition of the relationship between cumulative adversity and psychiatric problems among children,13,14,46,47 symptom and functional impairment levels related to the youths’ self-identified ‘Worst-Event’ have yet to be directly compared to their response to cumulative adversity. Further, few studies directly compare responses to Criterion-A and non-Criterion events, and those studies focus on adults and/or community populations.36,37,48 Because of the potential for traditional assessment strategies to perpetuate health disparities in underserved populations through methodologically-based under-identification of needs, the present study addressed three primary aims among those at heightened risk for adversity exposure and PTSD, delinquent girls.
First, a broad range of potential precipitating events (non-Criterion events: neglect, family separation, interrupted pregnancy, bullying, alongside Criterion-A events) were queried that represent adversity exposures relevant to high-risk populations such as delinquent girls. We hypothesized that delinquent girls would endorse high exposure to both Criterion-A and non-Criterion events. Second, we assessed their maladaptive coping strategies (e.g., self-injury) directly in response to their cumulative adversity exposure. We hypothesized that delinquent girls would evidence serious maladaptive coping strategies in response to their total cumulative adversity burden. Third, we directly compared each girl’s symptoms and functional impairment in response to their self-identified ‘worst event’ (regardless of whether the precipitating event-type met Criterion-A requirements) to their response to their total cumulative adversity exposure. We hypothesized that cumulative adversity symptom and functional impairment levels would be higher than Worst-Event levels. Because Criterion-A and non-Criterion events were permitted as “worst events”, we included an additional robustness check to restrict our comparisons to only girls with Criterion-A Worst-Events (representing traditional PTSD assessment methods) relative to their cumulative adversity response. Finally, we explored the mental health impact of non-Criterion events by comparing symptom and functional impairment responses between girls who selected a qualifying Criterion-A precipitating event, and girls who selected non-qualifying events (non-Criterion), as their worst experience. We hypothesized that non-Criterion events would precipitate greater symptoms and impairment than Criterion-A events.
2. Methods
2.1 Participants: Eligibility, Screening and Consenting Procedures
Participants included 118 adjudicated adolescent girls, 14–18 years old, sentenced to a locked placement at the Girls’ Rehabilitation Facility (GRF) in San Diego, California. Like detention centers and locked facilities nationwide,49,50 girls at GRF have similar age and offense distributions with high proportions of racial/ethnic minorities (Table 1). All girls were detained for over a month and completed detoxification, if indicated, prior to GRF placement.
Table 1.
Demographic and Clinical Characteristics of Incarcerated Girls
| Sample Characteristics | Mean | SD | Range | Alpha |
|---|---|---|---|---|
| Age at Assessment | 15.91 | 1.05 | (14–18) | -- |
| Age Earliest Loss Exposure (LEC) | 3.84 | 4.42 | (0–16) | -- |
| Age Earliest Trauma Exposure (LEC) | 7.78 | 4.12 | (0–16) | -- |
| SCI-TALS Domains (# of lifetime items) | ||||
| Loss (# of types; 10) | 4.91 | 1.43 | (2–8) | -- |
| Trauma (# of types; 21) | 11.16 | 2.95 | (4–18) | -- |
| Re-experiencing (9) | 6.81 | 1.97 | (1–9) | 0.80 |
| Avoidance & Numbing (12) | 7.91 | 2.47 | (2–12) | 0.80 |
| Arousal Symptoms (5) | 4.15 | 1.01 | (1–5) | 0.76 |
| Maladaptive Coping (8) | 3.97 | 2.02 | (0–8) | 0.78 |
| Race | N | % | ||
| Latino | 69 | 58.5 | ||
| African American | 25 | 21.2 | ||
| Caucasian | 21 | 17.8 | ||
| Other | 3 | 2.5 | ||
These data were part of the screening and baseline evaluation in a randomized controlled trial of Seeking Safety (SS)51 with incarcerated girls. Because SS is designed for individuals with trauma-related and substance use disorders, eligibility criteria included: evidence of adversity exposure (trauma, loss) and current symptoms in response to those events (based on DSM-IV-TR criteria34, allowing for subsyndromal symptomatology that is known to be impairing);52 substance or alcohol use; and a Full Scale, Verbal and/or Performance IQ ≥70 (e.g., in the case of a verbal learning disability, Performance IQ was required to be ≥70). Girls were interviewed by extensively trained and supervised female interviewers with degrees in psychology or a related field. All GRF girls were screened for eligibility unless they were preparing for discharge from the facility, did not speak English (bilinguals were eligible), were too impaired to participate in the consent process or did not wish to be screened. All approached girls, however, voluntarily consented to be screened.
Study methods and consent forms were approved by the University of California, San Diego (UCSD) Institutional Review Board (IRB); and the US Office of Protection from Research Risks and Department of Health and Human Services, which provides guidance on the involvement of prisoners in research (HHS regulations at 45 CFR part 46, subpart C). Youths’ assent (if they were < 18 years) or consent (if they were ≥ 18 years) was always sought. When possible, parental consent was obtained. As previously reported,30 and based on regulatory standards, if a parent was unavailable then youth assent was additionally overseen by a knowledgeable participant-advocate who represented their interests and provided opportunities for the youth to ask questions or decline participation. A federal certificate of confidentiality was obtained from the National Institute of Health and Human Development in order to protect the privacy of research participants and confidentiality of sensitive data.
2.2 Measures
2.2.1 Structured Clinical Interview for Trauma and Loss Spectrum [SCI-TALS]:53
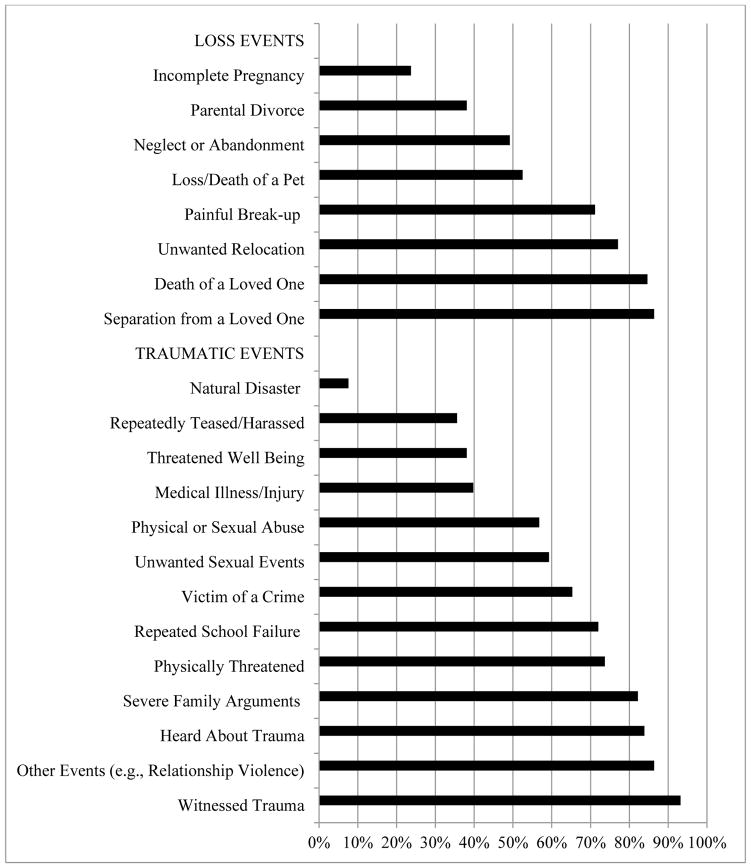
During eligibility screening, all girls were administered the SCI-TALS to determine their lifetime, and past three months, exposure to adversity (loss and trauma events), and cumulative adversity-related symptoms and maladaptive coping. This 116-item interview uses a dichotomous response-structure (yes = 1/no = 0) to assess cumulative adversity across nine lifetime Domains (endorsed items summed for each domain): Loss Events; Grief Reactions (symptoms, personal characteristics); Trauma Events; Reactions to Losses/Upsetting Events; Re-experiencing/Intrusion, Avoidance/Numbing, and Arousal/Reactivity symptoms in response to cumulative adversity; cumulative adversity-related Maladaptive Coping (reckless/destructive behaviors); and Personal Risk-Factors (characteristics, such as impulsivity, conceptualized to confer risk for stress-spectrum disorders but not queried in response to endorsed stressors). Loss Events (e.g., death of a loved one, unwanted separations, miscarriages) capture negative experiences which may cause grief responses, including complicated bereavement, intrusion, avoidance, re-experiencing, guilt/self-blame, increased emotionality, and failure to adapt.54,55 Trauma Events include Criterion-A traumas (e.g., rape, physical abuse) and potentially traumatic stressful experiences (e.g., bullying). Consistent with ACE studies, ‘event-types’ represent only the number of exposure types, not number of experienced events (physical abuse represents exposure to any physical abuse, but not physical abuse episodes/frequency), event severity or resulting symptomatology. Figure 1 provides event-types queried. Maladaptive coping items include risky self-destructive behaviors in direct response to cumulative adversity (e.g., substance use, intentional self-injury, neglect of serious medical needs, suicide attempts). The SCI-TALS has acceptable reliability and validity and has been well tolerated in clinical and community samples.53 Alpha levels for all symptom and maladaptive coping scales were acceptable among incarcerated girls (Table 1).
Figure 1.
SCI-TALS endorsed stressors (% endorsed by sample).
All girls experienced legal events (e.g., arrests), none had warzone exposure, three endorsed medical disabilities, and six endorsed ‘other’ loss events; these four event-types are not displayed with other Figure 1 event groupings due to low endorsement rate.
In addition to standardized SCI-TALS administration, we: 1) queried specific examples of ‘other traumatic events’ high-risk youth experience (intimate partner violence) in addition to the standard “any other upsetting events that happened to you that I haven’t asked you about?,” and 2) followed-up any lifetime symptom endorsement with queries about symptom experience in the last three months. A 14-item ‘Cumulative Adversity Score’ was calculated to capture event categories: experiencing failure at school; severe arguments in the family, physical or sexual abuse, an event that threatened well-being, natural disaster, being teased, threatened, or in a war zone, witnessing any events, and collapsing sexual (unwanted sexual experiences and rape), medical (illness and injury), victimization (being threatened by criminals or terrorists, being victim of a crime, and being kidnapped or held hostage), legal (disciplinary action or being arrested) and ‘other’ (e.g., intimate partner violence) event items.
2.2.2 Child PTSD Symptom Scale [CPSS]:56
This self-report assesses the frequency (0 = never to 3 = almost daily) of all 17 DSM-IV-TR PTSD symptoms (range 0–51) and seven PTSD-related functional impairment indicators, which determine whether symptoms had a negative impact on different life arenas (e.g., schoolwork) during the past two weeks. Functional impairment items are dichotomous; with higher scores (range 0–7) indicating a broader range of functional areas impacted. A total severity score is obtained by summing the first 17 items. Based on a homogeneous younger sample of youth (n=75, ages 8–15 years old, 89% Caucasian) experiencing an earthquake, a frequency cutoff of ≥11 was established by the CPSS developer to yield 95% sensitivity and 96% specificity in discriminating between youth with high versus low PTSD symptomatology.56 Based on a study with two, more diverse, samples of youth (treatment-seeking for a range of traumas versus presenting to hospitals for accidental and car-related injuries etc.), a revised cutoff score of ≥16 was recommended by Nixon and colleagues57 (hereafter referred to as Nixon’s cutoff). Because little or no CPSS data are available on Juvenile Justice-System involved samples, we present data for the percentage of girls meeting both cut-points. However, we are utilizing the more conservative 16-point cut-off for comparing Worst Event and Cumulative Adversity symptoms. In addition to the original CPSS format, assessing trauma-related symptoms relative to one worst event (‘Worst-Event’ CPSS), the CPSS was also administered in relation to the combined impact of total stressor exposure (a novel ‘Cumulative Adversity’ CPSS) immediately after SCI-TALS administration, with the past two week timeframe permitting characterization of their symptoms immediately prior to randomization. Alpha levels for symptom scales were acceptable for both Worst-Event and Cumulative Adversity CPSS (Table 2).
Table 2.
CPSS: Worst-Event and Cumulative Adversity symptoms and impairment rates.
| CPSS | Worst-Event | Cumulative Adversity | Effect Size | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Symptom Subscales | Mean | SD | Range | Alpha | Mean | SD | Range | Alpha | Cohen’sd |
| Re-experiencing** (5 items) | 5.65 | 3.59 | (0–13) | .807 | 7.27 | 3.77 | (0–15) | .801 | 0.44 |
| Avoidance** (7 items) | 7.92 | 5.54 | (0–21) | .819 | 10.3 | 5.22 | (0–21) | .774 | 0.44 |
| Arousal** (5 items) | 6.82 | 4.50 | (0–15) | .807 | 9.15 | 3.71 | (1–15) | .724 | 0.56 |
| Symptom Total** | 20.40 | 12.31 | (0–45) | .916 | 26.72 | 10.90 | (5–46) | .883 | 0.54 |
| Functional Impairment** (7 items) | 3.28 | 2.11 | (0–7) | .742 | 4.53 | 1.84 | (0–7) | .634 | 0.63 |
| Girls Meeting Symptom Cutoff | N | % | N | % | |||||
| Using 11-point cutoff** | 88 | 74.6 | 107 | 90.7 | |||||
| Using 16-point cutoff* | 75 | 63.6 | 95 | 80.5 | |||||
p < 0.01;
p < 0.001
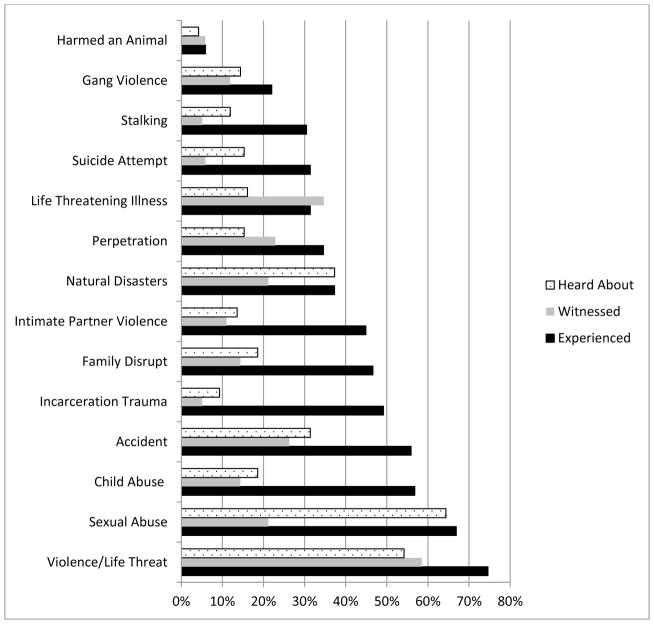
2.2.3 Life Event Checklist [LEC]:58
This self-report was developed concurrently with the Clinician-Administered PTSD Scale for DSM-IV (CAPS)59 and CAPS for Children and Adolescents (CAPS-CA)60 to identify the ‘worst’ trauma experienced prior to administering these PTSD interviews. The LEC has adequate psychometric properties as a stand-alone assessment of trauma exposure,58 and was administered because it: 1) was reasonably comparable to the life events section of the brief CPSS self-report used during screening and preceded our baseline CAPS-CA interview; 2) incorporates a broader range of precipitating events than the CPSS, including perpetration events which may be traumatic and are relevant among a variety of populations (inmates, military, gang members); 3) asks separately about physical and sexual (a common experience among incarcerated girls) abuse, unlike the SCI-TALS; and 4) assesses whether the youth experienced, witnessed, or heard about each event, unlike the CPSS and SCI-TALS.
The LEC was modified to: 1) include separation from family (e.g., removed by Child Protective Services), suicide attempts, teen dating violence and traumatic incarceration experiences; 2) separate out assault experiences happening in their home versus the community; 3) expand perpetration event queries to include forced violence against others and harm to animals; and 4) assess age of trauma-exposure for each event-type. Experienced and witnessed events (not heard about) were used to calculate the reported age at first loss and trauma.
Based on the LEC, youth identified which event they felt was the worst – that is, the event they felt precipitated the most PTSD-type symptoms (i.e., girls were given examples of re-experiencing, arousal, and avoidance/numbing symptoms). There was no requirement regarding whether the youth’s worst event met Criterion-A requirements. Youth were then given the Worst-Event CPSS [traditional CPSS administration], while directed to think specifically about their self-identified worst event. LEC Worst Events were then categorized as Criterion-A (single events that meet DSM Criterion-A) or non-Criterion events strictly adhering to the DSM and following Anders and colleagues recommendations.36 Criterion-A events included: Any sudden, non-natural death of a loved one (overdose, suicide, car crash, homicide), being kidnapped/held hostage, experiencing any assault (partner violence, sexual abuse/rape, child abuse, being shot at), and witnessing domestic violence or homicide. Non-Criterion events include experiences not consistently conceptualized as traumatic (e.g., death of loved one by natural causes; incarceration; being jumped into a gang; upsetting/coerced violence perpetration).
2.5 Statistical Analysis
All analyses were conducted using SPSS version 22. Paired sample t-tests were used for all analyses assessing the difference between Worst-Event, and Cumulative Adversity, CPSS symptoms and Functional Impairment. For significant findings, Cohen’s d effect sizes are presented. McNemar’s Chi Square analysis with binomial distribution was used to assess the difference in the proportion of girls meeting Nixon’s Total Score ≥16 symptom cutoff 57 for the Worst-Event and Cumulative Adversity CPSS measures. Independent sample t-tests were used to compare the difference between Worst-Event CPSS symptom levels (re-experiencing, avoidance, arousal, total) and functional impairment in youth who identified a Criterion-A qualifying worst-event versus those who identified non-Criterion events. Chi-square tests were used to assess the difference in the proportion of girls meeting Nixon’s Total Score ≥16 symptom cutoff for Criterion-A versus non-Criterion events. Statistically significant findings (p < 0.05) are reported.
3. Results
Participation rates post-screening were high. One screened girl declined participation because of the time commitment, one consented girl demonstrated psychotic symptoms during baseline assessment requiring immediate alternative treatment and one girl dropped out post-randomization as she did not wish to participate in non-mandatory programming. Baseline evaluations were conducted prior to randomization to treatment condition (Treatment as Usual or SS). Of 119 participants, one subject was missing one measure and excluded from analyses. Two of the 118 girls failed to answer all of their functional impairment items and were therefore excluded only from functional impairment specific analyses (n =116).
Incarcerated girls endorsed high trauma and loss exposure rates (SCI-TALS: Figure 1, LEC: Figure 2). Loss-events included the death of a close friend or relative among 84.7%, and separation from a family member or close friend among 86.4%, of the girls. Within the ‘Other’ trauma category, 49.2% of all girls experienced dating violence, 71.2% experienced gang violence, and 16.9% experienced prostitution-related violence. All girls endorsed two or more loss-types (SCI-TALS), and three or more trauma-types (SCI-TALS; Trauma Index Score). On average, girls endorsed five of ten possible loss-types and nine of fourteen possible trauma-types (Trauma Index Score).
Figure 2.
Percent of incarcerated girls endorsing LEC items.
The LEC clarified exposure modes (directly experienced, witnessed, heard about) for each event-type, as reflected in Figure 2 (i.e., one girl may have directly experienced and witnessed a rape, both event exposures are reflected in the figure). Of 17 queried, directly experienced, LEC event-types (e.g., sexual abuse), 93.2% of girls reported experiencing two or more event-types; 79.7% endorsed at least four; and 15.3% endorsed at least ten. Very low event-type endorsements (e.g., toxin exposure reported by four participants) are not reflected in Figure 2. On average, girls experienced six LEC event-types. Life threatening violence, sexual abuse, and child abuse (physical abuse, being forced to stay in a locked closet) were the most commonly experienced stressors. Attempted suicide was endorsed by 31.4% of girls. The most common Worst-Event types identified were sexual abuse (39.8%), and death exposure (9.3% saw a dead body or saw/heard about the violent death of a loved one). All but one girl (99.2%) endorsed lifetime exposure to at least one Criterion-A event, even if they did not identify it as their Worst-Event. Most girls reported their Worst-Event as a Criterion-A qualifying event (n = 91) but some worst-events were non-Criterion (n = 27).
Lifetime symptom and maladaptive coping rates in response to cumulative adversity were high (SCI-TALS; Table 1). Endorsement of past three month/current re-experiencing (m = 6.15; SD = 2.11), avoidance/numbing (m = 7.39; SD = 2.49), and arousal (m = 3.91; SD = 1.11) symptoms and maladaptive coping strategies (m = 2.94; SD = 1.62) was also high (see Table 1). Notable lifetime Maladaptive Coping strategies, specifically in response to stressors, included 37.4% of girls endorsing non-suicidal self-injury (NSSI), 75.7% reporting serious risk-behaviors (promiscuous sex, drunk driving), 91.5 % using substances to calm themselves and/or relieve stress-related emotional pain, and 35.5% not taking care of medical problems/following medical advice.
Additionally, past two-week symptoms were frequent and functional impairment rates were high in response to Cumulative Adversity and Worst-Event (CPSS; Table 2). The most commonly endorsed functional impairment item for Worst Event (62.5%) and Cumulative Adversity (76.6%) was problems in ‘general happiness with your life. Paired samples t-tests revealed that past two week Cumulative Adversity symptoms (re-experiencing: t(117) = 4.84, p < .001; avoidance: t(117) = 4.43, p < .001; arousal: t(117) = 5.93, p < .001; total: t(117) = 5.87, p < .001) and functional impairment (t(115) = 6.29, p < .001) were significantly higher than Worst-Event symptoms (Table 2). Medium effect sizes were observed (.44 – .63).
Proportionally more girls met the 16-point high-symptom cutoff using the Cumulative Adversity CPSS than the Worst-Event CPSS. McNemar’s test confirmed significant differences between Worst-Event, and Cumulative Adversity, CPSS (p < 0.01; Table 3) cutoff distributions. The test revealed movement across categories, with 29 girls (24.6%) exceeding the high-symptom cutoff using the Cumulative Adversity, but not Worst-Event, CPSS. Conversely, nine girls (7.6%) exceeded the high-symptom cutoff with the Worst-Event, but not the Cumulative Adversity, CPSS.
Worst-Event and Cumulative Adversity differences remained when limiting comparisons to only individuals whose Worst-Event qualified as Criterion-A. Cumulative Adversity symptoms (re-experiencing: t(117) = 4.35, p < .001; avoidance: t(117) = 4.45, p < .001; arousal: t(117) = 5.25, p < .001; total: t(117) = 5.41, p < .001) and functional impairment (t(115) = 6.06, p < .001) were significantly higher than Worst-Event symptoms. Again, McNemar’s test showed that proportionally more girls met the high-symptom cutoff using the Cumulative Adversity, than the Worst-Event, CPSS (girls exceeding cutoff: 76 and 56, respectively; p = 0.001).
Additional analyses showed that Worst-Event symptoms in response to Criterion-A events compared to non-Criterion Worst-Events did not significantly differ and there was no difference in the proportions of girls meeting the high-symptom cutoff. However, non-Criterion events precipitated significantly greater functional impairment rates than Criterion-A events (t(114)=2.28, p = 0.024). Follow-up analyses indicated that higher functional impairment levels noted among girls whose worst-event did not meet Criterion-A was primarily driven by a greater proportion of girls with non-Criterion worst-events (74.1%) endorsing academic impairment than girls with Criterion-A worst-events (39.3%; X2(1,116) = 10.03; p = 0.002).
4. Discussion
Cumulative adversity burden presents clinical challenges in high-risk populations, such as female delinquents. The present data underscore the: 1) high level of cumulative adversity exposure among incarcerated girls; with more than three-quarters endorsing directly experiencing ≥4 adversity event-types; 2) extremely elevated rates of severe Criterion-A traumatic experiences among incarcerated girls (99% endorsed a Criterion-A exposure; >75% life-threatening violence; ~50% dating violence exposures), many of which are the epitome of ongoing interpersonal ‘complex trauma’ (>64% sexual abuse, >55% child abuse); and 3) prominence of serious non-Criterion events, such as loss events (separation from, or death of, loved ones; >80% each) and severe family arguments (>80%). These data underscore the need to consider the cumulative impact of a range of adversities and address the complex treatment needs of high-risk populations such as incarcerated girls.
Significant improvements in understanding the clinical implications of experiencing cumulative adversity and complex trauma have occurred in recent years.13,15 However, most clinical and research assessments continue to query symptoms based only on the single worst identified, Criterion-A qualifying event. Among high-risk youth who experience significant cumulative adversity exposure,8,33 this assessment approach may miss the mental health impact of multiple severe experiences and non-Criterion events (family separations) and thereby fail to narrow extant health disparities. This is an important oversight given that cumulative exposure, including non-Criterion events (particularly losses), have significant developmental implications. For example, evidence suggests cumulative trauma, adversity and grief symptoms impact left frontal brain regions in delinquent youth and these regions are linked to language- and executive-related functions, aligning well with delinquent youths’ cognitive and behavioral difficulties.30
The present study indicates that symptoms and functional impairment are likely underestimated when assessments are limited to queries about one event in populations that experience cumulative adversity: delinquent girls’ symptom and functional impairment levels in response to cumulative adversity was greater than their response to their own self-identified Worst-Event. Further, many girls who did not exceed symptom cutoff levels based on one event, demonstrated high levels of current symptomatology in relation to cumulative adversity. Thus, one of the contributors to variability between exposure rates and PTSD diagnoses, even within similar populations, may be due to the diagnostic challenge of having a poly-victimized individual identify a single ‘worst’ event and focus on the symptom-impact of that event in their life. Both clinicians and researchers are likely to vary in how strictly they adhere to symptoms and impairment being linked to a single specific Criterion-A event. These results suggest that implementing the use of cumulative adversity assessments (i.e., considering all stressors, including non-Criterion events), is critical to ensure high-risk youth are properly identified and receive appropriate services. Of note, a few girls who fell at the high-symptom range for their worst event did not meet threshold in response to cumulative adversity, highlighting the specificity gained for some individuals when querying symptoms in reference to a single event. This suggests that orienting youth to specific events for symptoms that were not endorsed in response to all identified events, may further assist characterization and identification of treatment needs. While over-pathologizing is an important consideration, the appropriate identification of needs during childhood and adolescence is particularly critical because early detection and intervention have the greatest likelihood of improving lifespan outcomes.61,62 Further, addressing cumulative adversity symptoms and impairment may be optimal for reducing health disparities in vulnerable populations. These findings also lend support for the use of brief measures like the CPSS, which are well tolerated and can be used to elicit responses to both single worst events and cumulative adversity.
Further, an exclusive focus on one Criterion-A event likely underestimates functional disruption that has clinical relevance for intervening effectively in high-risk populations. While symptom levels were comparable for Criterion and non-Criterion events, functional impairment was greatest in response to “non-qualifying” events, falling outside of the scope of traditionally defined traumas. It may be that events perceived as traumatic by an individual, but not culturally acknowledged as traumas, may confer more ‘risk’ because of minimal social support and acceptance among family and social networks that also experience significant cumulative adversity exposure (e.g., minimize the event’s importance, perceive a ‘traumatic response’ as overblown or a sign of weakness). If these same “non-qualifying” events also receive diminished recognition from mental health professionals, then it may further reduce help-seeking behavior, increase treatment barriers among disenfranchised individuals and impart greater distress and disability. These results are consistent with a wider literature that also documents impairing ‘PTSD-like’ symptoms in response to non-qualifying events such as breast cancer or miscarriage.63–65 Because many non-qualifying events endorsed by delinquent girls are related to caregiver separations, heightened functional impairment may also occur because disruptions in caregiver status (parental incarceration or abandonment) reduce the child’s support, attachment and safety net. Finally, non-qualifying events such as caregiver disruption and/or bullying may disproportionately impact academic functioning (separation distress disrupting attention/concentration) and increase behaviors such as truancy (avoiding school bullies). Although this finding is preliminary given the sample size, academic disparities related to non-Criterion events appear likely to be overlooked when functional impairment assessments are yoked to traditionally “qualifying” events. This oversight would be critical because disruption in academic functioning is closely linked to lifespan economic and health disparities (poverty, chronic illness, premature death).66–68
The present data indicate that cumulative adversity resulted in serious maladaptive coping strategies that have significant health implications. Maladaptive coping strategies were both prevalent and severe, with girls endorsing self-destructive and risk-taking behaviors with serious individual (health) and social (economic) consequences (promiscuity, driving under the influence, not seeking needed medical attention, substance use, non-suicidal self-injury) specifically in response to their cumulative adversity exposure. While these behaviors are conceptualized as maladaptive coping strategies, they may also reflect symptomatology, functional impairment or even become traumatic events (e.g., suicide attempt). In fact, many maladaptive coping indicators are quite impairing (e.g., substance use) and likely lead to dysfunction across domains (i.e., adversity-related substance use could cause social and academic problems). Unfortunately, many commonly used trauma-relevant measures lack specific inquiry into a wide-range of harmful behavioral responses to stress. This is a critical oversight, as adversity-related maladaptive coping contextualizes the impact of cumulative adversity and guides treatment. Structured clinical interviews and self-report typically query global, social, and academic impairment, with few precise prompts to consistently delve into different facets of possible impairment and maladaptive coping strategies (e.g., NSSI, substance use). Nuanced questions geared towards adolescents may better tease out underlying deficits that may only otherwise emerge in skilled in-depth interviews. High endorsement of these maladaptive coping strategies suggests that these areas are quite relevant to cumulative adversity-exposed youth, and current measures likely underestimate overall impairment or fail to identify some of the most clinically meaningful problem areas.
These data also raise serious public health and policy concerns. In particular, over 30% of incarcerated girls had attempted suicide, a rate three times that found among general population girls.69 Additionally, 75% reported engaging in risk-behaviors (including illegal activities), and more than 90% endorsed substance use, in direct response to their stressful life experiences. The role of cumulative adversity in these youths’ poor functional outcomes indicates significant mental health needs that will not be ameliorated through justice system solutions alone. Further, the cumulative adversity-related failure to attend to medical needs among 36% of girls indicates that stress exposure during development plays a critical role in medical “non-compliance,” further hindering the ability to effectively intervene with vulnerable youth. These maladaptive coping strategies have profound negative health implications and represent significant individual, familial and societal costs. Understanding an individual’s adversity-related behavioral pattern is key to creating relevant interventions, enhancing the therapeutic alliance, improving lifespan outcomes, addressing disparity-amplifying behavioral patterns amenable to change and developing more effective social policies. It is imperative that researchers and clinicians consider impairment areas that are meaningful to high-risk youth, and that occur in response to cumulative adversity, in order to adequately assess, detect, characterize and treat adversity-related disorders.70
5. Limitations and Future Directions
It is important to note that some events (e.g., maltreatment) discussed here overlap with traditional ACE studies, 1 yet other events (gang violence, incarceration, teen dating violence) and losses (death of a loved one, miscarriage, painful breakups) queried are not captured by ACEs. Future research should consider a broader range of adversities, including traditional ACEs and other experiences common to high-risk populations (poverty, homelessness, parental deportation), in order to better understand health, cognitive, and behavioral consequences. Comparing pre- and post-treatment symptom and impairment changes in response to cumulative adversity and worst-events will also provide a meaningful context for appropriately tailoring interventions. By allowing a range of events to be considered as a youth’s worst event, our study finds that youth endorse both Criterion-A and non-Criterion events. Non-Criterion events, however, were endorsed as Worst-Events by fewer girls; and the unequal sample sizes limit statistical comparisons. Future studies should explicitly compare symptoms and functional impairment for each person’s worst-identified non-Criterion with their worst-identified Criterion-A event for intra-individual comparisons.
The present study focuses on incarcerated females, a population known to have high trauma exposure. Future studies should include a broader range of non-incarcerated delinquents, including males, as well as other high-risk youth and adults (e.g., military personnel with complex war-related traumas that may occur against the backdrop of previous loss and trauma). Lastly, this study was cross-sectional, symptom focused (i.e., non-diagnostic), and comprised of youths’ self-report data. Future studies would benefit from a longitudinal design and cross-informant reporting. However, obtaining other informant data on mental health symptoms (e.g., parent and teacher) is particularly difficult in high-risk populations where youth may be separated from parents, truant from school, or whose parents may be suffering from their own mental health problems that affect accurate reporting of youth’s symptoms.71–73
Finally, our current diagnostic options (PTSD) and theoretical classifications (e.g., Disorder of Extreme Stress, Developmental Trauma Disorder, Complex-PTSD) may inadequately capture the range of events that occur early in the lifespan and may be chronic and/or co-occurring, but not invariably “extreme” (loss) or universally accepted as “traumatic” (poverty) or may even occur prenatally and impart vulnerability to stressful and chaotic environments (prenatal substance/alcohol exposure). Diagnostic classifications are needed that capture the range of symptoms and impairment that occur when stress, trauma and loss disrupt development and impact regulatory abilities and attachment.74
Highlights.
Significant cumulative adversity exposure occurs among delinquent girls
Cumulative adversity is associated with serious maladaptive coping strategies
Cumulative adversity symptom/impairment levels are higher than worst-event levels
Non-Criterion worst-events lead to greater impairment than Criterion-A worst-events
High Criterion-A and non-Criterion adversity exposures underscore assessment needs
Acknowledgments
This work was supported by the National Institute of Child and Human Development grants R01HD066161, and R01HD066161-01S1 and -05S1 Diversity Supplements. The project was also partially supported by the National Institutes of Health, University of California, San Diego’s [UCSD] Clinical and Translational Research Institute, Grant 1UL1RR031980-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH. We are also in appreciation for the support received from the UCSD’s Academic Senate Health Sciences Research Grant Committee. We thank our participants for their time and willingness to participate, our talented project staff, and the San Diego County Probation Department [SDCPD] for their cooperation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Lucenko B, Sharkova I, Mancuso D, Felver B. Adverse childhood experiences associated with behavioral health problems in adolescents. Findings from administrative data for youth age. 2012:12–17. [Google Scholar]
- 3.Macdonald A, Danielson CK, Resnick HS, Saunders BE, Kilpatrick DG. PTSD and comorbid disorders in a representative sample of adolescents: The risk associated with multiple exposures to potentially traumatic events. Child abuse & neglect. 2010;34(10):773–783. doi: 10.1016/j.chiabu.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 4.Turner HA, Finkelhor D, Ormrod R. Poly-victimization in a national sample of children and youth. American journal of preventive medicine. 2010;38(3):323–330. doi: 10.1016/j.amepre.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 5.Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. Journal of consulting and clinical psychology. 2003;71(4):692. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- 6.Green BL, Goodman LA, Krupnick JL, et al. Outcomes of single versus multiple trauma exposure in a screening sample. Journal of traumatic stress. 2000;13(2):271–286. doi: 10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- 7.Greeson JK, Briggs EC, Kisiel CL, et al. Complex trauma and mental health in children and adolescents placed in foster care: Findings from the National Child Traumatic Stress Network. Child Welfare. 2011;90(6):91. [PubMed] [Google Scholar]
- 8.Baglivio M, Epps N, Swartz K, Huq M, Sheer A, Hardt N. The prevalence of Adverse Childhood Experiences (ACE) in the lives of Juvenile Offenders. OJJDP Journal of Juvenile Justice. 2014;3(2):1–23. [Google Scholar]
- 9.Edwards VJ, Anda R, Dube S, Dong M, Chapman D, Felitti V. Child Victimization: Maltreatment, Bullying, and Dating Violence Prevention and Intervention. Kingston, NJ: Civic Research Institute; 2005. The wide-ranging health consequences of adverse childhood experiences; pp. 8–1. [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- 11.Costello EJ, Erkanli A, Fairbank JA, Angold A. The prevalence of potentially traumatic events in childhood and adolescence. Journal of traumatic stress. 2002;15(2):99–112. doi: 10.1023/A:1014851823163. [DOI] [PubMed] [Google Scholar]
- 12.Seides R. Should the current DSM-IV-TR definition for PTSD be expanded to include serial and multiple microtraumas as aetiologies? Journal of psychiatric and mental health nursing. 2010;17(8):725–731. doi: 10.1111/j.1365-2850.2010.01591.x. [DOI] [PubMed] [Google Scholar]
- 13.Cloitre M, Stolbach BC, Herman JL, et al. A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of traumatic stress. 2009;22(5):399–408. doi: 10.1002/jts.20444. [DOI] [PubMed] [Google Scholar]
- 14.Ford JD, Courtois CA. Treating complex traumatic stress disorders in children and adolescents: Scientific foundations and therapeutic models. Guilford Press; 2013. [Google Scholar]
- 15.van der Kolk BA, Pynoos RS, Cicchetti D, et al. Proposal to include a developmental trauma disorder diagnosis for children and adolescents in DSM-V. 2009 Unpublished manuscript. Verfügbar unter: http://www.cathymalchiodi.com/dtd_nctsn.pdf (Zugriff: 20.5. 2011)
- 16.Herman JL. Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of traumatic stress. 1992;5(3):377–391. [Google Scholar]
- 17.Pynoos R, Steinberg A, Wraith R. Developmental Psychopathology. Vol. 2. Risk, Disorder, and Adaptation. New York, NY: John Wiley & Sons; 1995. A Developmental Model of Childhood Traumatic Stress. [Google Scholar]
- 18.Shipman K, Edwards A, Brown A, Swisher L, Jennings E. Managing emotion in a maltreating context: A pilot study examining child neglect. Child abuse & neglect. 2005;29(9):1015–1029. doi: 10.1016/j.chiabu.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 19.Kisiel CL, Fehrenbach T, Torgersen E, et al. Constellations of interpersonal trauma and symptoms in child welfare: Implications for a developmental trauma framework. Journal of Family Violence. 2014;29(1):1–14. [Google Scholar]
- 20.Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. Journal of health and social behavior. 1995:360–376. [PubMed] [Google Scholar]
- 21.Ford JD, Grasso DJ, Hawke J, Chapman JF. Poly-victimization among juvenile justice-involved youths. Child abuse & neglect. 2013;37(10):788–800. doi: 10.1016/j.chiabu.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Duke NN, Pettingell SL, McMorris BJ, Borowsky IW. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125(4):e778–e786. doi: 10.1542/peds.2009-0597. [DOI] [PubMed] [Google Scholar]
- 23.Reavis JA, Looman J, Franco KA, Rojas B. Adverse childhood experiences and adult criminality: how long must we live before we possess our own lives? The Permanente Journal. 2013;17(2):44. doi: 10.7812/TPP/12-072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006 Apr;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gilbert LK, Breiding MJ, Merrick MT, et al. Childhood adversity and adult chronic disease: an update from ten states and the District of Columbia, 2010. American journal of preventive medicine. 2015;48(3):345–349. doi: 10.1016/j.amepre.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 26.Schilling EA, Aseltine RH, Gore S. The impact of cumulative childhood adversity on young adult mental health: measures, models, and interpretations. Social science & medicine. 2008;66(5):1140–1151. doi: 10.1016/j.socscimed.2007.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Finkelhor D, Ormrod RK, Turner HA. Lifetime assessment of poly-victimization in a national sample of children and youth. Child abuse & neglect. 2009;33(7):403–411. doi: 10.1016/j.chiabu.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 28.De Bellis MD. The psychobiology of neglect. Child maltreatment. 2005;10(2):150–172. doi: 10.1177/1077559505275116. [DOI] [PubMed] [Google Scholar]
- 29.Cohen JA Issues TWGOQ, Issues AWGoQ. Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(4):414–430. [PubMed] [Google Scholar]
- 30.Lansing AE, Virk A, Notestine R, Plante WY, Fennema-Notestine C. Cumulative Trauma, Adversity and Grief Symptoms associated with Fronto-temporal Regions in Life-course Persistent Delinquent Boys. Psychiatry Research: Neuroimaging. 2016;254(30):92–102. doi: 10.1016/j.pscychresns.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Noble KG, Houston SM, Brito NH, et al. Family income, parental education and brain structure in children and adolescents. Nature neuroscience. 2015;18(5):773–778. doi: 10.1038/nn.3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zatzick DF, Kang S-M, Müller H-G, et al. Predicting posttraumatic distress in hospitalized trauma survivors with acute injuries. American Journal of Psychiatry. 2002;159(6):941–946. doi: 10.1176/appi.ajp.159.6.941. [DOI] [PubMed] [Google Scholar]
- 33.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. Washington, DC: Author; 1980. [Google Scholar]
- 34.American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-IV-TR fourth edition (text revision) 2000. [Google Scholar]
- 35.Van Hooff M, McFarlane AC, Baur J, Abraham M, Barnes DJ. The stressor Criterion-A1 and PTSD: A matter of opinion? Journal of Anxiety Disorders. 2009;23(1):77–86. doi: 10.1016/j.janxdis.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 36.Anders SL, Frazier PA, Frankfurt SB. Variations in criterion A and PTSD rates in a community sample of women. Journal of Anxiety Disorders. 2011;25(2):176–184. doi: 10.1016/j.janxdis.2010.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Long ME, Elhai JD, Schweinle A, Gray MJ, Grubaugh AL, Frueh BC. Differences in posttraumatic stress disorder diagnostic rates and symptom severity between Criterion A1 and non-Criterion A1 stressors. Journal of Anxiety Disorders. 2008;22(7):1255–1263. doi: 10.1016/j.janxdis.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 38.Perkins-Dock RE. Family interventions with incarcerated youth: A review of the literature. International Journal of Offender Therapy and Comparative Criminology. 2001;45(5):606–625. [Google Scholar]
- 39.Dong M, Anda RF, Felitti VJ, et al. Childhood residential mobility and multiple health risks during adolescence and adulthood: the hidden role of adverse childhood experiences. Archives of pediatrics & adolescent medicine. 2005;159(12):1104–1110. doi: 10.1001/archpedi.159.12.1104. [DOI] [PubMed] [Google Scholar]
- 40.Evans GW, Kim P. Childhood poverty and health cumulative risk exposure and stress dysregulation. Psychological Science. 2007;18(11):953–957. doi: 10.1111/j.1467-9280.2007.02008.x. [DOI] [PubMed] [Google Scholar]
- 41.Jelleyman T, Spencer N. Residential mobility in childhood and health outcomes: a systematic review. Journal of Epidemiology and Community Health. 2008;62(7):584–592. doi: 10.1136/jech.2007.060103. [DOI] [PubMed] [Google Scholar]
- 42.Abram KM, Teplin LA, King DC, et al. PTSD, trauma, and comorbid psychiatric disorders in detained youth. Juvenile Justice Bulletin. 2013;1:13. [Google Scholar]
- 43.Abram KM, Teplin LA, Charles DR, Longworth SL, McClelland GM, Dulcan MK. Posttraumatic stress disorder and trauma in youth in juvenile detention. Archives of general psychiatry. 2004;61(4):403–410. doi: 10.1001/archpsyc.61.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Duclos CW, Beals J, Novins DK, Martin C, Jewett CS, Manson SM. Prevalence of common psychiatric disorders among American Indian adolescent detainees. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37(8):866–873. doi: 10.1097/00004583-199808000-00017. [DOI] [PubMed] [Google Scholar]
- 45.Cauffman E, Feldman SS, Waterman J, Steiner H. Posttraumatic stress disorder among female juvenile offenders. J Am Acad Child Adolesc Psychiatry. 1998;37(11):1209–1216. [PubMed] [Google Scholar]
- 46.Benjet C, Borges G, Medina-Mora ME. Chronic childhood adversity and onset of psychopathology during three life stages: childhood, adolescence and adulthood. Journal of psychiatric research. 2010;44(11):732–740. doi: 10.1016/j.jpsychires.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 47.Cook A, Blaustein M, Spinazzola J, Van der Kolk B. Complex trauma in children and adolescents: White paper from the national child traumatic stress network complex trauma task force. Los Angeles: National Center for Child Traumatic Stress; 2003. [Google Scholar]
- 48.Alessi EJ, Meyer IH, Martin JI. PTSD and sexual orientation: An examination of criterion A1 and non-criterion A1 events. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5(2):149. doi: 10.1037/a0026642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sickmund M, Puzzanchera C. Juvenile offenders and victims: 2014 national report. 2014. [Google Scholar]
- 50.Sickmund M, Sladky T, Kang W. Census of juveniles in residential placement databook. Washington, DC: US Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 2008. [Google Scholar]
- 51.Najavits LM. Seeking safety: A treatment manual for PTSD and substance abuse. Guilford Press; 2002. [DOI] [PubMed] [Google Scholar]
- 52.Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: findings from a community survey. American Journal of Psychiatry. 1997;154(8):1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- 53.Dell’Osso L, Shear MK, Carmassi C, et al. Validity and reliability of the Structured Clinical Interview for the Trauma and Loss Spectrum (SCI-TALS) Clin Pract Epidemiol Ment Health. 2008 Jan 28;4(2):1–7. doi: 10.1186/1745-0179-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prigerson HG, Horowitz MJ, Jacobs SC, et al. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Med. 2009;6(8):e1000121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Horowitz MJ, Siegel B, Holen A, Bonanno GA, Milbrath C, Stinson CH. Diagnostic criteria for complicated grief disorder. Focus. 2003;1(3):290–298. doi: 10.1176/ajp.154.7.904. [DOI] [PubMed] [Google Scholar]
- 56.Foa EB, Johnson KM, Feeny NC, Treadwell KR. The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of clinical child psychology. 2001;30(3):376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- 57.Nixon RD, Meiser-Stedman R, Dalgleish T, et al. The Child PTSD Symptom Scale: An update and replication of its psychometric properties. Psychological assessment. 2013;25(3):1025. doi: 10.1037/a0033324. [DOI] [PubMed] [Google Scholar]
- 58.Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- 59.Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician-administered PTSD scale. Journal of traumatic stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 60.Nader KO, Kriegler J, Blake D, Pynoos R, Newman E, Weathers F. Clinician Administered PTSD scale for children and adolescents. National Center for PTSD. 1996 [Google Scholar]
- 61.Satcher D. Report of the surgeon general’s conference on children’s mental health: A national action agenda. Taylor & Francis; 2000. [PubMed] [Google Scholar]
- 62.Prince M, Patel V, Saxena S, et al. No health without mental health. The lancet. 2007;370(9590):859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 63.Cordova MJ, Andrykowski MA, Kenady DE, McGrath PC, Sloan DA, Redd WH. Frequency and correlates of posttraumatic-stress-disorder-like symptoms after treatment for breast cancer. Journal of consulting and clinical psychology. 1995;63(6):981. doi: 10.1037//0022-006x.63.6.981. [DOI] [PubMed] [Google Scholar]
- 64.Dutton DG. Trauma symptoms and PTSD-like profiles in perpetrators of intimate abuse. Journal of traumatic stress. 1995;8(2):299–316. doi: 10.1007/BF02109566. [DOI] [PubMed] [Google Scholar]
- 65.Sherman JJ, Turk DC, Okifuji A. Prevalence and impact of posttraumatic stress disorder-like symptoms on patients with fibromyalgia syndrome. The Clinical journal of pain. 2000;16(2):127–134. doi: 10.1097/00002508-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 66.Boisjoly J, Harris KM, Duncan GJ. Initial welfare spells: trends events and duration. 1997. [Google Scholar]
- 67.Laird J, Lew S, DeBell M, Chapman C. National Center for Education Statistics. 2006. Dropout Rates in the United States: 2002 and 2003. ED TAB. NCES 2006–062. [Google Scholar]
- 68.Moore KA, Glei DA, Driscoll AK, Zaslow MJ, Redd Z. Poverty and welfare patterns: Implications for children. Journal of Social Policy. 2002;31(02):207–227. [Google Scholar]
- 69.Cash SJ, Bridge JA. Epidemiology of youth suicide and suicidal behavior. Current opinion in pediatrics. 2009;21(5):613. doi: 10.1097/MOP.0b013e32833063e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kling JR, Congdon WJ, Mullainathan S. Policy and choice: Public finance through the lens of behavioral economics. Brookings Institution Press; 2011. [Google Scholar]
- 71.Schreier H, Ladakakos C, Morabito D, Chapman L, Knudson MM. Posttraumatic stress symptoms in children after mild to moderate pediatric trauma: a longitudinal examination of symptom prevalence, correlates, and parent-child symptom reporting. Journal of Trauma and Acute Care Surgery. 2005;58(2):353–363. doi: 10.1097/01.ta.0000152537.15672.b7. [DOI] [PubMed] [Google Scholar]
- 72.Stover CS, Hahn H, Im JJ, Berkowitz S. Agreement of parent and child reports of trauma exposure and symptoms in the early aftermath of a traumatic event. Psychological Trauma: Theory, Research, Practice, and Policy. 2010;2(3):159. doi: 10.1037/a0019156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Youngstrom E, Loeber R, Stouthamer-Loeber M. Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. Journal of consulting and clinical psychology. 2000;68(6):1038. doi: 10.1037//0022-006x.68.6.1038. [DOI] [PubMed] [Google Scholar]
- 74.D’Andrea W, Ford J, Stolbach B, Spinazzola J, van der Kolk BA. Understanding interpersonal trauma in children: why we need a developmentally appropriate trauma diagnosis. American Journal of Orthopsychiatry. 2012;82(2):187–200. doi: 10.1111/j.1939-0025.2012.01154.x. [DOI] [PubMed] [Google Scholar]