Abstract
The surgical technique for the management of a symptomatic os acromiale remains unclear. Several operative techniques have been described including open excision, open reduction–internal fixation (ORIF), arthroscopic acromioplasty or subacromial decompression, and arthroscopic excision. There are 4 types of os acromiale, with the meso-acromion being the most common and difficult to treat. The excision of a pre-acromion arthroscopically or in an open manner usually produces satisfactory results. However, the open excision of a meso-acromion can lead to persistent pain and deltoid weakness and atrophy. The management of a meso-acromial fragment with ORIF can also result in persistent pain and deltoid weakness and atrophy with nonunion of the fragments. The purpose of this article is to describe an alternative surgical technique to open excision or ORIF when presented with a symptomatic meso-acromiale.
An os acromiale is typically found incidentally during the evaluation for unrelated shoulder pathology because most patients are often asymptomatic for this condition.1 The overall prevalence of os acromiale is 7%, and it has a higher frequency in persons of black ancestry.2 The acromial apophysis develops from 4 main ossification centers: (1) the pre-acromion, (2) the meso-acromion, (3) the meta-acromion, and (4) the basi-acromion.3 The os acromiale represents a failure of fusion between 2 of these apophyses.3 The types of os acromiale are defined by the unfused segment immediately anterior to the site of nonunion.4 For example, failed fusion between the meta-acromion and meso-acromion ossification centers is called a “meso-acromiale.”4 The vast majority of os acromiale are meso-acromions.2, 5 The condition can be symptomatic due to inflammation at the pseudarthrosis site, the mobile fragment impinging on the rotator cuff,6 or arthritic changes of the acromioclavicular joint due to hypermobility of the os.3
Preoperative Diagnosis and Imaging
Preoperative diagnosis of a meso-acromion is often made incidentally on the axial view of plain radiographs when evaluating for another shoulder condition. Lee et al.7 described the double-density sign on a supraspinatus outlet view that was highly suggestive of an os acromiale. A meso-type of os acromiale can also be visualized by magnetic resonance imaging (MRI) and/or a computed tomography scan on the axial view. MRI in particular may show sclerotic or inflammatory changes at the site that may be indicative of degeneration in a symptomatic meso-acromion. Differentiating a meso-acromion from a normally developing acromial ossification center may be difficult because acromial fusion may not be complete until age 18 to 25 years. On MRI, a meso-acromion can be diagnosed by transverse orientation and irregular margins with marrow and interface edema, whereas in a normally developing acromial ossification center, the developing acromion has an arched interface and lobulated margins with no evidence of marrow or interface edema.8 Bone scans may also help illustrate the inflammatory response at the nonunion site of a meso-acromion.
The vast majority of cases of os acromiale are meso-acromions.2, 5 In cases of a meso-acromion that becomes symptomatic, patients often present with a mobile fragment that results in pain and tenderness at the nonunion site and positive impingement signs. There have also been reports of rotator cuff pathology ranging from tendinitis to full-thickness tearing associated with an os acromiale.9 The diagnosis can be confirmed by a selective injection of 5 mL of 1% lidocaine into the site with re-examination 10 minutes later. This diagnostic tool is useful to determine if the meso-acromiale is the source of the pain.10 If the lidocaine injection does help relieve or reduce pain, it is not unreasonable to then administer a one-time corticosteroid injection into the same region for therapeutic purposes, which may give symptomatic long-term pain relief in some patients. Table 1 lists the pearls and pitfalls of diagnosing a symptomatic meso-acromion.
Table 1.
Pearls and Pitfalls
| Proper diagnosis before surgery is key because not all meso-acromions are symptomatic. |
| Proper imaging studies should be obtained, including a magnetic resonance imaging study that shows sclerosis and inflammatory changes at the synchondrosis of the meso-acromion. |
| As a diagnostic tool, selective injection of 5 mL of 1% lidocaine into the site with re-examination 10 minutes later can be performed. |
| Failure to diagnose a meso-acromion before arthroscopic surgery can lead to it being destabilized at the time of subacromial decompression. |
Surgical Options
When nonoperative management fails, surgery is the next treatment option for a symptomatic meso-acromion. A number of surgical techniques have been described such as open fragment excision, arthroscopic acromioplasty,1, 5, 11, 12 open reduction–internal fixation (ORIF) with cannulated screws or tension band wiring,3, 4, 5, 6, 10, 13, 14 ORIF with cannulated screws combined with Kirschner wires used in tension band wiring,14 and arthroscopic resection of the unstable fragment.5, 15, 16, 17 ORIF with iliac crest bone graft has also been described with favorable results.5, 10, 15, 16 ORIF is the most common surgical procedure and can lead to radiographic healing in a vast majority of patients.5, 10 Biomechanical studies have shown that cannulated screws with Kirschner wires in a tension band configuration lead to significantly higher repair strength at time zero in a cadaveric model when compared with cannulated screws alone.14
However, complications can occur after all of the aforementioned techniques. Open excision can lead to persistent pain, weakness, and deltoid atrophy.5, 18 Arthroscopic acromioplasty can sometimes destabilize the fragment, leading to persistent pain and weakness.18 After ORIF, hardware complications, nonunion, and the need for hardware removal are common even when radiographic union has occurred.1, 3, 4, 5, 6, 10, 13 Arthroscopic excision is a viable alternative and can be considered in some patients.15, 16, 17
It is important to discuss with the patient the different surgical options and the risks and benefits of each. For younger patients, ORIF may be a better alternative, whereas in older patients, arthroscopic resection may be a better option.17 However, good results have been reported with arthroscopic excision in a young, athletic patient population.16 The procedure described and shown in Video 1 in a 54-year-old male patient is a safe, effective technique for arthroscopic excision for a symptomatic meso-acromiale.
Surgical Technique
Preoperative Planning
Once the decision has been made for the patient to undergo surgery with arthroscopic excision of the symptomatic meso-acromion, careful preoperative planning is necessary to ensure a good result. Advanced arthroscopic skills are necessary, and surgeons should be comfortable using shavers, burrs, and radiofrequency devices in the subacromial space. Having a qualified and well-trained assistant along with an experienced team of nurses and an experienced anesthesiologist comfortable with hypotensive anesthesia is critical. Excessive bleeding can lead to poor visualization because of inadequate control of the blood pressure and can make this procedure difficult, if not impossible, to perform. Finally, the arthroscopic surgeon should have a checklist of all equipment needed that should be checked before bringing the patient into the operating room. A list of the proper equipment recommended for the procedure is shown in Table 2.
Table 2.
Equipment Required
| STARR sleeve with shoulder suspension device (Arthrex) |
| Hip positioning device for lateral decubitus position |
| Standard 30° arthroscope with monitor, tower, shaver, and radiofrequency device |
| Crystal smooth cannula, 5.75 mm × 7 cm (Arthrex) |
| ArthroCare 90° wand |
| 4.5-mm oval burr (Dyonics; Smith & Nephew) |
Positioning
After administration of general endotracheal anesthesia, the patient is placed in the lateral decubitus position with an axillary roll, pillows between the knees, and all bony prominences padded. A beanbag or other device (with posts anterior and posterior similar to a total hip position) can be used for positioning. Pneumatic compression devices are applied to both lower extremities to reduce the risk of deep venous thrombosis. This procedure can also be performed with the patient in the beach-chair position, but the lateral decubitus position is our preference. The nonoperative shoulder is strapped to an arm board at 90° to the operating table for support and stability. The surgeon performs an examination of the shoulder with the patient under general anesthesia, noting mobility of the glenohumeral joint and any crepitance related to the meso-acromion or the nearby acromioclavicular joint. The operative extremity is prepared and draped in a standard fashion. The operative arm is placed in a STARR sleeve (Arthrex, Naples, FL), which is then connected to a suspension device and placed in abduction.
Diagnostic Arthroscopy and Bursoscopy
By use of a standard posterior portal and an anterior portal placed in the rotator interval, a 15-point diagnostic arthroscopy of the glenohumeral joint is performed. Any intra-articular pathology can be addressed including loose body removal, labral debridement or repair, capsular release, and evaluation and debridement of the articular side of the rotator cuff. If a partial articular-sided rotator cuff tear is identified, a spinal needle can be placed percutaneously through the partial cuff tear and an absorbable suture can be threaded through the needle and the needle removed. This so-called marker suture technique can be used to then identify the bursal side of the cuff in this region when the subacromial space is entered. Once the glenohumeral examination has been performed, the arm is repositioned from abduction to adduction using the suspension device and the arthroscope is repositioned into the subacromial space using the same posterior portal. The same anterior portal is used for placement of an arthroscopic shaver (Dyonics 4.0-mm full-radius shaver; Smith & Nephew, Memphis, TN), and if bursitis is present in the subacromial space, it is debrided to create a “room with a view.” The bursal side of the rotator cuff is then inspected to make sure there is no partial or complete tearing of the tendon. If a marker suture has been placed, this is localized and the bursal side of the cuff in this region is again inspected to ensure there is no significant tearing.
Debridement and Visualization in Subacromial Space
Once adequate visualization has been obtained in the subacromial space, a lateral portal is established 2 fingerbreadths (approximately 2.5 cm) off the lateral edge of the acromion in line with the posterior aspect of the acromioclavicular joint. A 5.75-mm × 7-cm clear, smooth cannula (Crystal Cannula; Arthrex) is introduced to facilitate the passage of instruments and to avoid iatrogenic damage to the deltoid muscle with multiple passes of instruments through the soft tissues. Hypotensive anesthesia (systolic blood pressure ≤90 mm) is used to ensure adequate visualization in the subacromial space. Still viewing from the posterior portal, the surgeon inserts a radiofrequency device (ArthroCare 90° wand; ArthroCare, Austin, TX) into the subacromial space through the lateral portal. The soft tissues are taken off the undersurface of the acromion, and the coracoacromial ligament is released but not cut. A radiofrequency device is preferred versus a shaver because it causes less bleeding and allows for better visualization (Fig 1). The anterior, medial, and lateral edges of the acromion and the pseudarthrosis or synchondrosis site of the meso-acromion are identified and outlined using the radiofrequency device (Fig 2). Special care is taken to leave the deltoid fibers intact.
Fig 1.
Viewing anteriorly from the posterior portal in a left shoulder in the lateral decubitus position, the radiofrequency device (RF) (ArthroCare 90° wand) is inserted into the subacromial space through a lateral portal. This device is used to strip all the soft tissues off the undersurface of the acromion.
Fig 2.

Viewing the subacromial space anteriorly from the posterior portal in a left shoulder in the lateral decubitus position, the radiofrequency device has removed all soft tissues from the undersurface of the acromion. The posterior border of the meso-acromion (PB-MA), the synchondrosis site (SYN), and the acromion are all visualized.
Arthroscopic Resection of Meso-acromiale
Once the entire meso-acromion has been identified and stripped of all soft tissues, a 4.5-mm oval burr (Dyonics; Smith & Nephew) is inserted through the lateral portal (Fig 3). Arthroscopic excision using the burr is then performed, sweeping the burr along the undersurface of the meso-acromion from posterior to anterior with careful attention not to damage or disrupt the deltoid fibers, which are attached to the remaining portion of the acromion. Meticulous technique is required to prevent disruption of the deltoid fibers (Fig 4). Once the entire meso-acromion has been removed by the burr, co-planing of the distal aspect of the clavicle can be performed if necessary because a mobile meso-acromion often leads to osteoarthritic changes of the distal clavicle. The soft-tissue shaver can then be reinserted to debride any residual soft tissue and to ensure complete removal of the meso-acromion (Fig 5). Postoperative radiographs are obtained, including a supraspinatus outlet view, to make sure that the entire meso-acromial fragment has been removed (Fig 6). A list of key points to perform the described procedure is found in Table 3.
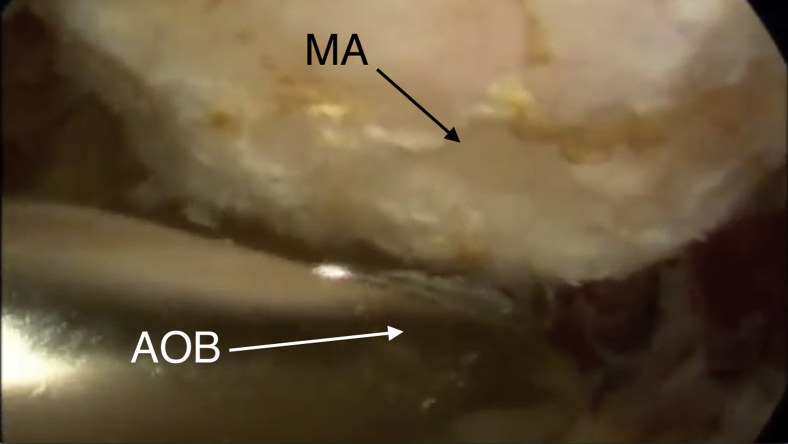
Fig 3.
Viewing the subacromial space anteriorly from the posterior portal in a left shoulder in the lateral decubitus position, the arthroscopic oval burr (AOB) (4.5 mm, Dyonics; Smith & Nephew) is inserted through the lateral portal. The meso-acromion (MA) can be visualized superior to the burr.
Fig 4.
Viewing the subacromial space anteriorly from the posterior portal in a left shoulder in the lateral decubitus position with the burr in the lateral portal, arthroscopic burring is performed by sweeping the arthroscopic oval burr (AOB) along the undersurface of the meso-acromion (MA) from posterior to anterior with meticulous technique to prevent disruption of the deltoid fibers.
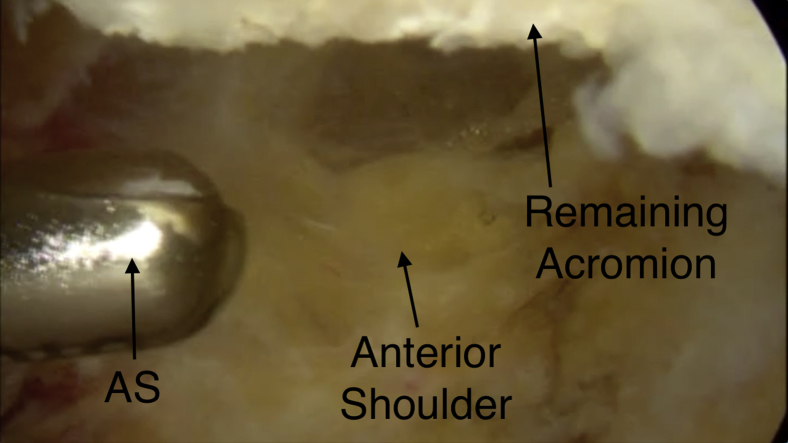
Fig 5.
Viewing the subacromial space anteriorly from the posterior portal in a left shoulder in the lateral decubitus position, the arthroscopic shaver (AS) is introduced through the lateral portal to remove any residual soft tissues from the remainder of the acromion and to make sure that the entire meso-acromion has been removed. The remaining acromion can be visualized superiorly.
Fig 6.

Postoperative radiograph of the left shoulder. The supraspinatus outlet view shows complete excision of the meso-acromiale fragment (circle).
Table 3.
Key Points
| An extensive preoperative evaluation is necessary to determine that the meso-acromion is the source of the patient's symptoms. |
| The surgeon should perform precise portal placement in the subacromial space with the lateral portal placed 2.5 cm off the lateral edge of the acromion in line with the posterior aspect of the acromioclavicular joint. |
| The surgeon should perform subperiosteal dissection of all soft tissues of the undersurface of the acromion with a radiofrequency device outlining the lateral, medial, and anterior aspects of the meso-acromion. |
| Hypotensive anesthesia should be used to ensure adequate visualization. |
| The surgeon should perform meticulous use of a burr to excise the meso-acromion but not disrupt the deltoid periosteal sleeve to the remainder of the acromion. |
Postoperative Care and Rehabilitation
Postoperatively, the patient is placed in a sling and immobilized for 2 weeks. Active elbow flexion and extension exercises along with gripping exercises, as well as pendulum exercises, are started immediately. An aggressive physical therapy program is initiated within the first 7 to 10 days postoperatively for active-assisted range of motion, followed by a strengthening program beginning at 6 weeks. Full range of motion is typically achieved at approximately 6 to 8 weeks postoperatively, and strength can be fully recovered as early as 3 months postoperatively. Patients typically return to full activities 3 to 4 months postoperatively.
Discussion
A symptomatic meso-acromion is an uncommon shoulder pathology with inconsistent outcomes using various surgical techniques. Open fragment excision of the symptomatic meso-acromion has had mixed results in the literature because of residual deltoid weakness, atrophy, and dysfunction postoperatively.4, 5, 18 Internal fixation with the use of tension band wires, cannulated screws, or a combination of both is technically difficult, has led to frequent nonunion rates, and often requires hardware removal as a result of postoperative irritation.1, 5, 10 Arthroscopic subacromial decompression and acromioplasty are used primarily when impingement with or without a rotator cuff tear is present and the nonunion site of the meso-acromion is non-tender, stable, and considered incidental.5, 9 However, this can lead to destabilization of the fragment with persistent pain and weakness.18
In a review of the literature, the studies of Pagnani et al.16 and Campbell et al.15 are the only ones dealing with the arthroscopic excision of symptomatic meso-acromions, in addition to an isolated case report by Kawaguchi et al.17 These studies provide few, if any, details of the arthroscopic technique used to perform the procedure. No details regarding the technique were provided by Campbell et al. and Kawaguchi et al., whereas Pagnani et al. noted the use of a bone-cutting arthroscopic shaver (Dyonics; Smith & Nephew) rather than a burr. The surgical technique that we have described is safe and effective, requires no special instrumentation, and may be reproducibly performed by surgeons familiar with arthroscopic techniques of the shoulder.
There are distinct advantages and disadvantages of the arthroscopic technique for removal of a symptomatic meso-acromion (Table 4). The advantages include more rapid rehabilitation, better range of motion, and shorter surgical time. There is also no need for a second operation for symptomatic metal removal, which is common after ORIF. The disadvantage of our technique is the advanced arthroscopic surgical skills that are necessary to perform the procedure. If the arthroscopic surgeon does not know the proper landmarks, iatrogenic damage to the spine of the scapula and to the remainder of the acromion can occur, leading to fracture. In addition, overzealous stripping of the deltoid aponeurosis off the acromion can lead to muscle weakness and atrophy of the deltoid.
Table 4.
Advantages and Risks of Arthroscopic Resection
| Advantages |
| The risk of postoperative pain, weakness, and deltoid atrophy and dysfunction is reduced. |
| The technique allows rapid rehabilitation, better range of motion, and a shorter surgical time. |
| There is no need for a second operation for symptomatic metal removal as is seen when open reduction–internal fixation is performed. |
| Risks |
| Iatrogenic damage to the deltoid can occur if the technique is performed improperly with deltoid stripping off the acromion, leading to deltoid weakness and dysfunction. |
| Iatrogenic damage to the spine of the scapula and to the remainder of the acromion can occur, leading to fracture. |
Even though both Pagnani et al.16 and Campbell et al.15 reported excellent results, many orthopaedic surgeons are reluctant to recommend or perform an arthroscopic excision for fear of resultant muscle weakness, cosmetic deformity, and/or perhaps the technical difficulty of performing such a procedure. However, if meticulous care is given to resecting the symptomatic meso-acromion, the deltoid aponeurosis and periosteal sleeve can be preserved, minimizing postoperative weakness, deformity, and pain. In addition, more and more orthopaedic surgeons now have extensive experience in arthroscopic shoulder surgery, which makes the technical difficulty less of an issue. It is our opinion that this is a better surgical treatment option than open resection or excision and may also be a better option than ORIF in most patients with symptomatic meso-acromions.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Arthroscopic excision of a meso-acromiale. The patient is a 54-year-old left hand–dominant man. Five years earlier, he underwent a left shoulder arthroscopic subacromial decompression and arthroscopic SLAP repair, from which he made a full recovery and returned to full activities. The patient returned 5 years later with pain and weakness of the left shoulder and the inability to perform his regular duties at work, which included overhead activities and lifting. The presence of the meso-acromion was noted preoperatively and intraoperatively during the initial surgical procedure, but it was asymptomatic and stable and, therefore, was not addressed surgically. After failure of 6 months of conservative management including rest, restriction of activities, physical therapy, and a subacromial cortisone injection, the patient returned for surgery. The patient is placed in the lateral decubitus position with an axillary roll and all bony eminences padded. The operative arm is placed in a STARR sleeve, connected to a suspension device, and positioned in abduction. By use of a standard posterior portal and an anterior portal placed in the rotator interval, a 15-point diagnostic arthroscopy of the glenohumeral joint is performed. This is performed to rule out any significant intra-articular pathology; in this case, it showed that the superior labrum had healed with no other intra-articular pathology. The arm is repositioned from abduction to adduction, and the arthroscope is repositioned into the subacromial space using the same posterior portal. The anterior portal is used for placement of a 4.0-mm full-radius arthroscopic shaver (Dyonics). Once adequate visualization has been obtained in the subacromial space, a lateral portal is established 2 fingerbreadths (approximately 2.5 cm) off the lateral edge of the acromion in line with the posterior aspect of the acromioclavicular joint. A 5.75-mm × 7-cm clear, smooth cannula (Crystal Cannula) is introduced to facilitate the passage of instruments and to avoid iatrogenic damage to the deltoid muscle. With the surgeon viewing from the posterior portal, a radiofrequency device (ArthroCare 90° wand) is inserted into the subacromial space through the lateral portal. The soft tissues are taken off the undersurface of the acromion, and the coracoacromial ligament is released but not cut. The anterior, medial, and lateral edges of the acromion and the synchondrosis site of the meso-acromion are identified and outlined with special care to leave the deltoid fibers intact. A 4.5-mm oval burr (Dyonics; Smith & Nephew) is inserted through the lateral portal. Arthroscopic excision using the burr is then performed, sweeping the burr along the undersurface of the meso-acromion from posterior to anterior with meticulous technique to prevent disruption of the deltoid fibers. Once the entire meso-acromion has been removed by the burr, co-planing of the distal aspect of the clavicle is performed.
References
- 1.Abboud J.A., Silverberg D., Pepe M. Surgical treatment of os acromiale with and without associated rotator cuff tears. J Shoulder Elbow Surg. 2006;15:265–270. doi: 10.1016/j.jse.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 2.Yammine K. The prevalence of os acromiale: A systematic review and meta-analysis. Clin Anat. 2014;27:610–621. doi: 10.1002/ca.22343. [DOI] [PubMed] [Google Scholar]
- 3.Atoun E., van Tongel A., Narvani A., Rath E., Sforza G., Levy O. Arthroscopically assisted internal fixation of the symptomatic unstable os acromiale with absorbable screws. J Shoulder Elbow Surg. 2012;21:1740–1745. doi: 10.1016/j.jse.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Kurtz C.A., Humble B.J., Rodosky M.W., Sekiya J.K. Symptomatic os acromiale. J Am Acad Orthop Surg. 2006;14:12–19. doi: 10.5435/00124635-200601000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Harris J.D., Griesser M.J., Jones G.L. Systematic review of the surgical treatment for symptomatic os acromiale. Int J Shoulder Surg. 2011;5:9–16. doi: 10.4103/0973-6042.80461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Warner J., Beim G.M., Higgins L. The treatment of symptomatic os acromiale. J Bone Joint Surg Am. 1998;80:1320–1326. doi: 10.2106/00004623-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Lee D.H., Lee K.H., Lopez-Ben R., Bradley E.L. The double-density sign: A radiographic finding suggestive of an os acromiale. J Bone Joint Surg Am. 2004;86:2666–2670. [PubMed] [Google Scholar]
- 8.Winfeld M., Rosenberg Z.S., Wang A., Bencardino J. Differentiating os acromiale from normally developing acromial ossification centers using magnetic resonance imaging. Skeletal Radiol. 2015;44:667–672. doi: 10.1007/s00256-015-2098-4. [DOI] [PubMed] [Google Scholar]
- 9.Johnston P.S., Paxton E.S., Gordon V., Kraeutler M.J., Abboud J.A., Williams G.R. Os acromiale: A review and an introduction of a new surgical technique for management. Orthop Clin North Am. 2013;44:635–644. doi: 10.1016/j.ocl.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 10.Barbier O., Block D., Dezaly C., Sirveaux F., Mole D. Os acromiale, a cause of shoulder pain, not to be overlooked. Orthop Traumatol Surg Res. 2013;99:465–472. doi: 10.1016/j.otsr.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 11.Trenhaile S.W., Field L.D., Savoie F.H., III Arthroscopic management of the mesoacromion. Tech Shoulder Elbow Surg. 2002;3:82–89. [Google Scholar]
- 12.Wright R.W., Heller M.A., Quick D.C., Buss D.D. Arthroscopic decompression for impingement syndrome secondary to an unstable os acromiale. Arthroscopy. 2000;16:595–599. doi: 10.1053/jars.2000.9239. [DOI] [PubMed] [Google Scholar]
- 13.Peckett W.R.C., Gunther S.B., Harper G.D., Hughes J.S., Sonnabend D.H. Internal fixation of symptomatic os acromiale: A series of twenty-six cases. J Shoulder Elbow Surg. 2004;13:381–385. doi: 10.1016/j.jse.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 14.Spiegl U.J.A., Smith S.D., Todd J.N., Wijdicks C.A., Millett P.J. Biomechanical evaluation of internal fixation techniques for unstable meso-type os acromiale. J Shoulder Elbow Surg. 2015;24:520–526. doi: 10.1016/j.jse.2014.09.040. [DOI] [PubMed] [Google Scholar]
- 15.Campbell P.T., Nizlan N.M., Skirving A.P. Arthroscopic excision of os acromiale: Effects on deltoid function and strength. Orthopedics. 2012;35:e1601–e1605. doi: 10.3928/01477447-20121023-16. [DOI] [PubMed] [Google Scholar]
- 16.Pagnani M.J., Mathis C.E., Solman C.G. Painful os acromiale (or unfused acromial apophysis) in athletes. J Shoulder Elbow Surg. 2006;15:432–435. doi: 10.1016/j.jse.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 17.Kawaguchi S., Fukuta S., Tsutsui T. Arthroscopic excision of unstable os acromiale associated with impingement syndrome: A case report. J Med Invest. 2016;63:131–134. doi: 10.2152/jmi.63.131. [DOI] [PubMed] [Google Scholar]
- 18.Neyton L., Noël E., Walch G., Pons-Villanueva J. Acromion reconstruction after failed subacromial decompression in shoulders with os acromiale (meso-acromion): The tongue-and-groove assembly. J Shoulder Elbow Surg. 2014;23:e261–e265. doi: 10.1016/j.jse.2014.07.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic excision of a meso-acromiale. The patient is a 54-year-old left hand–dominant man. Five years earlier, he underwent a left shoulder arthroscopic subacromial decompression and arthroscopic SLAP repair, from which he made a full recovery and returned to full activities. The patient returned 5 years later with pain and weakness of the left shoulder and the inability to perform his regular duties at work, which included overhead activities and lifting. The presence of the meso-acromion was noted preoperatively and intraoperatively during the initial surgical procedure, but it was asymptomatic and stable and, therefore, was not addressed surgically. After failure of 6 months of conservative management including rest, restriction of activities, physical therapy, and a subacromial cortisone injection, the patient returned for surgery. The patient is placed in the lateral decubitus position with an axillary roll and all bony eminences padded. The operative arm is placed in a STARR sleeve, connected to a suspension device, and positioned in abduction. By use of a standard posterior portal and an anterior portal placed in the rotator interval, a 15-point diagnostic arthroscopy of the glenohumeral joint is performed. This is performed to rule out any significant intra-articular pathology; in this case, it showed that the superior labrum had healed with no other intra-articular pathology. The arm is repositioned from abduction to adduction, and the arthroscope is repositioned into the subacromial space using the same posterior portal. The anterior portal is used for placement of a 4.0-mm full-radius arthroscopic shaver (Dyonics). Once adequate visualization has been obtained in the subacromial space, a lateral portal is established 2 fingerbreadths (approximately 2.5 cm) off the lateral edge of the acromion in line with the posterior aspect of the acromioclavicular joint. A 5.75-mm × 7-cm clear, smooth cannula (Crystal Cannula) is introduced to facilitate the passage of instruments and to avoid iatrogenic damage to the deltoid muscle. With the surgeon viewing from the posterior portal, a radiofrequency device (ArthroCare 90° wand) is inserted into the subacromial space through the lateral portal. The soft tissues are taken off the undersurface of the acromion, and the coracoacromial ligament is released but not cut. The anterior, medial, and lateral edges of the acromion and the synchondrosis site of the meso-acromion are identified and outlined with special care to leave the deltoid fibers intact. A 4.5-mm oval burr (Dyonics; Smith & Nephew) is inserted through the lateral portal. Arthroscopic excision using the burr is then performed, sweeping the burr along the undersurface of the meso-acromion from posterior to anterior with meticulous technique to prevent disruption of the deltoid fibers. Once the entire meso-acromion has been removed by the burr, co-planing of the distal aspect of the clavicle is performed.