Abstract
Background:
Severe adolescent obesity (body mass index (BMI) >99.6th centile) is a significant public health challenge. Current non-invasive treatments, including community-based lifestyle interventions, are often of limited effectiveness in this population, with NICE guidelines suggesting the use of bariatric surgery as the last line of treatment. Health professionals are understandably reluctant to commission bariatric surgery and as an alternative, the use of an intra-gastric balloon as an adjunct to a lifestyle programme might offer a reversible, potentially safer and less invasive option.
Objectives:
Explore the use of an intra-gastric balloon as an adjunct to a lifestyle support programme, to promote weight loss in severely obese adolescents. Outcomes included weight loss, waist and hip measurements, psychosocial outcomes including health-related quality of life (HRQoL) and physical self perceptions, physical activity and cardiorespiratory fitness.
Method:
Non-randomised pilot study.
Results:
Twelve severely obese adolescents (5 males, 7 females; mean age 15 years; BMI >3.5 s.d.; puberty stage 4 or more) and their families were recruited. Mean weight loss at 12 months (n=9) was 3.05 kg±14.69; d=0.002, P=0.550, and a BMI Z-score (n=12) change of 0.2 s.d.; d=0.7, P=0.002 was observed at 6 months with a large effect, but was not sustained at 12 months (mean change 0.1 s.d.; d=0.3, P=0.146). At 24 months (n=10), there was a weight gain from baseline of +9.9 kg±1.21 (d=0.4; P=0.433). Adolescent and parent HRQoL scores exceeded the minimal clinical important difference between baseline and 12 months for all domains but showed some decline at 24 months.
Conclusion:
An intra-gastric balloon as an adjunct to a lifestyle support programme represents a safe and well-tolerated treatment approach in severely obese adolescents, with short-term effects on weight change. Improvements in psychosocial health, physical activity and cardiorespiratory fitness were maintained at 12 months, with varying results at 24 months.
Introduction
Evidence shows that severe obesity (body mass index (BMI) >99.6th percentile) in children and adolescents is the fastest growing sub category of obesity.1 Severe obesity has been shown to have marked immediate and long-term consequences (Kelly et al.2) on health and well-being associated with significant physical morbidity (discussed in detail in Sachdev et al., this issue) as well as greater risk of developing psychiatric conditions such as mood issues hopelessness and suicide attempts.3 High BMI (that is, above the 99th centile) is associated with lower body image and self-esteem in young people,4 with many exhibiting social difficulties often due to enduring episodes of being bullied and teased about their weight. Obese children are also usually socially isolated and find it difficult to form relationships.5
In England, with 2.9% of girls and 3.9% boys aged 10-11 years classified severely obese,6, 7 this represents a large number of children whom require obesity treatment.7 Current treatment guidelines8 recommend multi-component lifestyle programmes, that focus on promotion of physical activity, healthy diets and behavioural change, with consideration of pharmacotherapy and bariatric surgery if the BMI is >+3.5 s.d. and comorbidities are present or +4 s.d. without comorbidity.9 In severely obese adolescents, for whom current treatments have proved ineffective at promoting significant and sustained weight loss, novel treatments are required that bridge the gap between lifestyle programmes and bariatric surgery, which many health professionals are understandably reluctant to consider and commission.2 Intra-gastric balloons were first used in adults over 25 years ago10 and have been demonstrated to offer a less invasive, reversible option, which potentially could be suitable for severely obese adolescents.11 Little data is available regarding the acceptability and potential efficacy of the combined use of an intra-gastric balloon and a lifestyle support programme with severely obese adolescents.11 The purpose of conducting this pilot study was to explore the use of an intra-gastric balloon as an adjunct to a lifestyle support programme specifically tailored to the needs of severely obese adolescents and their families, with the primary aim to induce weight loss. This paper presents study findings on BMI Z-score, physical activity and cardiorespiratory fitness and psychosocial well-being including health-related quality of life (HRQoL) and physical self perceptions, outcomes at 12 months (6 months post balloon removal) and 24 months (18 months post balloon removal). Additional biomedical outcomes are presented in Sachdev et al., this issue.
Materials and methods
A through explanation of the methods for this study, including a detailed description of the lifestyle programme content is published elsewhere.12 Briefly here, the lifestyle programme was underpinned by recognised models of health-related behaviour change including the transtheoretical model and theory of planned behaviour.13, 14 The primary aim of the lifestyle programme was to reduce weight and promote positive behaviour change, see Figure 1 for a diagram presenting an overview of the intervention. It also aimed to maintain positive outcomes in the longer term by encouraging young people and their families, to focus on achieving a healthy, active lifestyle as well as addressing emotional well-being. Integration of the home environment and family members were crucial in helping to identify and support progress. The multi-component intervention, led by research fellow (LR) at an English university, included behaviour change strategies to increase families' physical activity, improve eating behaviour, provide social support as well as deliver supervised exercise sessions.8, 9 Programme activities made links between thoughts and emotional responses that could affect an adolescent or family member's behaviour, all targeted on enhancing the families' ability to cope and respond to everyday tasks in a healthy way. A unique feature of the BOB (balloons in obesity study) intervention design, was the explicit mapping of all the behaviour change techniques involved within the protocol to the taxonomy of behaviour change for physical activity and healthy eating behaviours.12, 15
Figure 1.
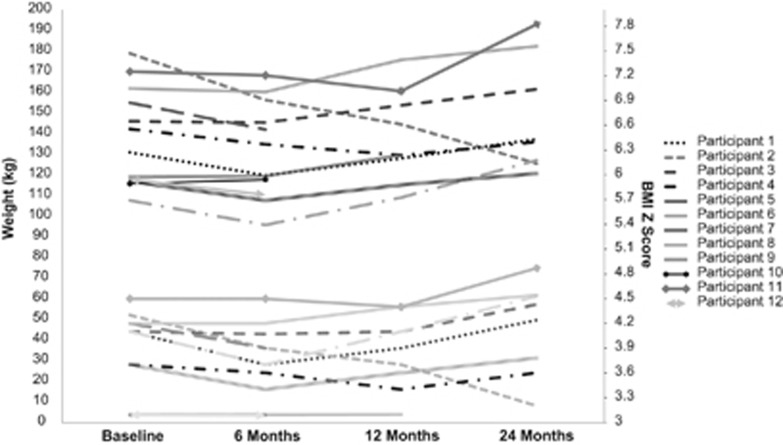
Individual weight and BMI Z-score at baseline, 3, 6, 12 and 24 months.
Participants were recruited from a pediatric clinic at Sheffield Children's Hospital, to participate in a non-randomised pilot study. The sample size (n=12) was selected as the optimal size for a pilot study,16 balancing the requirements of obtaining data on potential outcomes, and recruitment, with the number of individuals receiving an unproven treatment modality.16 BOB, involved the insertion of an intra-gastric balloon (ORBERA—inflated to 500 ml) placed in situ, endoscopically under general anaesthesia. The balloon remained in situ for 6-months. Participant's and their families received an intense lifestyle support programme for 9 months; beginning 1 month before balloon insertion, 6 months during balloon placement and two month's maintenance phase post balloon removal.
Outcome measures
The primary outcome was change in body weight and BMI Z-score at 12 months following adherence to the lifestyle programme for 9 months, and balloon insertion for 6 months. Change in body weight and BMI Z-score at 6 months were also assessed. Secondary outcomes assessed physical activity and cardiorespiratory fitness, psychosocial well-being including pediatric HRQoL and physical self perceptions, along with adherence to the lifestyle programme. Outcome measures at 24 months have also been given to show longer term impact.
Assessments
All secondary outcomes were assessed at baseline, 4 weeks before balloon insertion, balloon removal after 6, 12 (6 months post balloon removal) and 24 months (18 months post balloon removal).
Anthropometrics
Weight was measured to the nearest 0.1 kg using a balance scale. Height was measured using a wall-mounted stadiometer to the nearest 0.1 cm. BMI was converted to Z-scores based on the 1990 UK Growth Reference curves17 with s.d. >99.6th severely obese. All participants were classified as severely obese.
Health-related quality of life
Adolescent self-reported HRQoL was assessed via the pediatric quality of life inventory, PedsQL, 4.0 generic module18 for 13–18 year olds. The inventory is widely used with its feasibility, reliability and validity strongly tested in this population.19 In this paper, a score consisting of all 23 items is reported as a total score, with a psychosocial summary score combining all 15 items assessing emotional (‘I feel sad'), social (‘I have trouble getting along with other teenagers') and school functioning (‘I find it hard to pay attention in class') and a physical score including eight items (‘I find it difficult to bathe myself' ‘I find it difficult to run'). The parental proxy measures for the same components are also captured. Following reverse scoring, scores range from 0 to 100 with higher scores indicating a higher HRQoL. Individual scale scores are given and interpreted against the minimal clinically important difference specified, for example; a 4.4 change in the total scale score for child self-report is the minimal clinically meaningful difference. Likewise, a 4.5 change in the total scale score for parent proxy-report is a minimal clinically meaningful difference.20
Physical self perceptions (Fox and Corbin, 1989) and self perceptions (Harter, 1988)
Self-perception was measured on the subscale from the children and youth physical self-perception profile (CY-PSPP) developed in 1989 (ref. 21) and adapted for use in children in 1995.21 The CY-PSPP contains six subscales; sport/athletic, attractive body adequacy, condition and strength competence as well as physical and global self-worth. The CY-PSPP assessed the degree to which young people viewed themselves as competent in a variety of physical domains.22 Each question contains two statements relating to either a positive perception of competence or a negative perception of competence. Items measuring social acceptance, scholastic competence and global self-worth were taken from Harter's self-perception profile for adolescent.23 The social acceptance subscale assessed the degree to which the adolescent feels accepted by their peers, feels popular, has lots of friends and feels that he/she is easy to like. The scholastic competence items assessed participants' perception of their competence or ability within the school context. The global self-worth subscale assesses the extent to which participants like themselves as a person and the way they are living their lives. Score responses range from 1 (very slightly) to 5 (extremely).
Physical activity
The physical activity questionnaire for adolescents (PAQ-A)24 was used to capture self-reported data of the adolescent's participation in physical activity 7 days before completion. Questions focus on (1) spare time physical activity, (2) physical education, (3) lunchtime physical activity, (4) extracurricular activities, (5) evening activity and (6) weekend activity. Scores are on a scale of 1 (not active)–5 (very active), which are then totalled to provide an average PAQ-A, score.
Cardiorespiratory fitness
The modified Balke treadmill protocol was used to assess cardiorespiratory fitness.25, 26 Participants walk consistently at a speed of 3 miles per hour commencing at 6% gradient, which increases incrementally by 2% every 2 min. Heart rate and rating of perceived exertion—an individual's perception of exertion during physical effort27 are recorded each minute. The test ended when the adolescent felt they could no longer continue and time terminated is recorded.
Statistical analysis
Based upon the small size and the pilot nature of this data set, results are expressed as means, s.d's. with the corresponding 95% confidence interval (95% CI). Effect sizes (Cohen's d)28 are presented to highlight the magnitude of the change observed between groups, as recommended by Winter et al.29 In addition, paired analysis (two-sided paired t-tests) with the corresponding P-values is reported. Owing to the pilot nature of this study, P-values must be interpreted with caution.
Results
Sample characteristics
Participants were recruited between October 2012 and July 2013 following referral from pediatric consultants in the Yorkshire region. Informed consent was obtained for all participants. All balloon insertions and removals were completed by March 2014. The sample included 12 severely obese adolescents (5 males, 7 females; average age 15 years; BMI >3.5 s.d.; puberty stage 4 or more) and their families. Baseline characteristics are displayed in Table 1 as a group and split by gender. Ten families were from Caucasian descent with one black and one with mixed family origin. All but two of the families (Lincolnshire and Stockport) were living in the Yorkshire and Humber region with 11 families living in areas of highest deprivation (multiple deprivation quintiles 1 and 2) with 1 family living in quintile 3 (indices of multiple deprivation, 2010). All agreed to travel to Sheffield for the lifestyle sessions and committing to participate in the study for 2 years.
Table 1. Characteristics of all variables reported by group and split by gender mean±s.d.
| Both | Female | Male | |
|---|---|---|---|
| (n=12) | (n=7) | (n=5) | |
| Weight (kg) | 138.45±23.97 | 131.5±24.5 | 148.2±21.7 |
| %EBW | 73.6±20.68 | 69.83±22.2 | 78.89±19.3 |
| BMI Z-score | 4±0.29 | 4±0.3 | 4±0.2 |
| Waist (cm) | 128.25±19.06 | 123.5±21.04 | 135±15.4 |
| Hip (cm) | 136.21±13.38 | 135.8±14.4 | 139.1±13.3 |
| Peds QoL—adolescent | |||
| Physical | 56.2±17.2 | 61.66±24.31 | 63.33±18.75 |
| Emotional | 63.75±25.9 | 54.01±17.74 | 59.375±18.09 |
| Social | 67.08±25.9 | 59.01±21.28 | 61.96±17.03 |
| School | 56.25±28.61 | 62.86±25.96 | 65±28.94 |
| QoL total | 60.23±18.83 | 64.29±27.45 | 71±15.57 |
| Total physical summary | 56.25±17.27 | 57.86±28.99 | 54±31.30 |
| Total Psychosocial summary | 62.36±21.23 | 54.02±17.74 | 59.375±18.09 |
| Peds QoL—parents | |||
| Physical | 53.12±13.71 | 48.09±15.2 | 56.33±13.7 |
| Emotional | 55.83±18.44 | 47.77±8.8 | 50±16.2 |
| Social | 50.41±20.38 | 47.98±12.4 | 51±14.4 |
| School | 60±20.99 | 49.29 ±12.8 | 58±24.6 |
| QoL total | 54.61±12.73 | 49.28±24.2 | 52±16 |
| Total physical summary | 53.12±13.71 | 46.42±28.5 | 59±12.9 |
| Total psychosocial summary | 55.41±13.22 | 48.91±10.4 | 58.13±16.18 |
| Physical self perceptions (scores 1–4) | |||
| Sport competence | 2.86±0.26 | 2.82±0.17 | 2.94±0.29 |
| Conditioning comptence | 2.79±0.20 | 2.85±0.3 | 2.75±0.3 |
| Attractive body adequacy | 2.24±0.16 | 2.25±0.21 | 2.23±0.21 |
| Strength competence | 2.62±0.67 | 2.35±0.93 | 2.80±0.44 |
| Physical self-worth | 2.47±0.42 | 2.58±0.34 | 2.40±0.49 |
| Global self-worth | 2.65±0.3 | 2.53±0.3 | 2.16±0.38 |
| Self perceptions (scores 1–4) | |||
| Social | 2.7±0.23 | 2.6±0.2 | 2.7±0.26 |
| Scholastic | 2.5±0.21 | 2.4±0.34 | 2.56±0.3 |
| Physical activity (scores range 1–5) | |||
| PAQ-A | 1.94±0.66 | 1.73±0.45 | 2.22±0.85 |
| Cardiorespiratory fitness (termination time s) | 5.89±2.44 | 5.4±2.9 | 6.5±1.5 |
Abbreviations: BMI, body mass index; EBW, excess body weight; HRQoL, health-related quality of life; PAQ-A, physical activity questionnaire for adolescents; QoL, quality of life.
Protocol adherence
All 12 participants recruited completed their 6-month assessments with 9 participants (75%) attending their 12-month follow up and 10 attending 24 month follow-up (75%). Reasons for not attending; one lost to follow up, one experienced a severe mental health episode unrelated to the study requiring hospitalisation and one cancelled the appointment.
Adherence to the lifestyle programme, measured against the research protocol, from baseline to 12 months varied among the participants, with a group average of 16 sessions (42%) ranging from 3 to 29 sessions, (7–74% adherence with the protocol). During balloon insertion, an average attendance of 14 sessions (46%), ranging from 3 to 25 sessions (10–83%) occurred, which dropped markedly during the maintenance phase (1 month post balloon removal) (average 2 sessions; 19%).
Primary outcome
A mean weight loss at 6months (n=12), balloon removal was 7.05 kg±7.13 (d=0.3; P=0.006) and at 12 months (n=9) was 3.05 kg±14.69 (d=0.002; P=0.550). At 24 months (n=10), there was a weight gain from baseline of +9.9 kg±1.21 (d=0.4; P=0.433). A BMI Z-score (n=12) change of 0.2 (d=0.7; P=0.002* (*P<0.05)), as observed at 6 months with a large effect, but was not sustained at 12 months (mean change 0.1 s.d.; d=0.3; P=0.146). At 24 months, BMI Z-score has increased by 0.2 ±0.2 (d=0.2; P=0.451). A reduction in waist circumference at 6 months (n=9) of 13.78±11.95 cm (d=0.6; P=0.16) was evident and at 12 months was (n=9), 10.47±17.46 cm (d=0.5; P=0.110), although hip circumference increased by 3.15 cm (d=0.2; P=0.799) at 12 months—higher than at baseline. This could be explained through individual variations within the sample. See Table 2 for all outcome data for the group at baseline, 6, 12 and 24 months.
Table 2. Group outcome at baseline, 6, 12 and 24 months expressed as mean±s.d. and 95% CI.
| Anthropometrics | Baseline mean±s.d. (95% CI min-max) | 6 months mean±s.d. (95% CI min-max) | 12 months mean±s.d. (95% CI min-max) | 24 months mean±s.d. (95% CI min-max) |
|---|---|---|---|---|
| n=12 | n=12 | n=9 | n=10 | |
| Weight (kg) | 138.45±23.97 (123.23–153.67) | 131.43±23.10 (16.76–146.1) | 138.4±21.85 (121.58–155.22) | 148.42±25.18 (130.43–166.41) |
| %EBWL | — | 9.55±9.16 (6.03–13.07) | 2.29±16.47 (−1.94–6.52) | 5.45±14.24 (−4.72–15.32) |
| BMI Z-score | 4±0.29 (3.82–4.18) | 3.8±0.32 (3.6–4) | 3.9±0.3 (3.64–4.16) | 4.1±0.5 (3.77–4.4) |
| Waist (cm) | 128.25±19.06 (116.15–140.35) | 115.86±15.48 (105.59–126.13) | 119.5±13.91 (108.79–130.21) | 138.72±21.21 (123.58–153.86) |
| Hip (cm) | 136.21±13.38 (127.72–144.7) | 133.15±13.18 (124.41–141.89) | 139.36±12.39 (129.82–148.9) | 138.5±12.61 (129.51–147.49) |
| Peds QoL—adolescent | Baseline mean±s.d. (95% CI) | 6 months mean±s.d. (95% CI) | 12 months mean±s.d. (95% CI) | 24 months mean±s.d. (95% CI min-max) |
| n=12 | n=10 | n=9 | n=8 | |
| Physical | 56.2±17.2 (45.46±67.17) | 70.3±12.8 (61.17–79.43) | 69.79±9.63 (62.38–77.2) | 64±25 (43.47–85.43) |
| Emotional | 63.75±25.9 (47.28±80.22) | 66±31.86 (43.24–88.76) | 70±27.61 (48.76–91.26) | 59.38±30.17 (34.21–84.53) |
| Social | 67.08±22.6 (57.23±81.43) | 74±22.21 (58.13–89.87) | 71.11±29.76 (48.19–94.03) | 67.5±31.1 (41.62–93.38) |
| School | 56.25±28.61 (38.07±74.42) | 57±27.6 (37.27–76.73) | 66.11±33.98 (39.95–92.27) | 70.6±21.6 (52.59-88.65) |
| QoL total | 60.23±18.83 (48.27±72.19) | 67.28±18.37 (54.25–80.41) | 69.32±20.59 (53.46–85.17) | 65±25.2 (45.08-85.62) |
| QoL physical summary | 56.25±17.27 (45.29±67.21) | 70.31±12.77 (61.68–79.44) | 69.79±9.63 (62.38–77.2) | 64.5±25.2 (43.47–84.75) |
| QoL psychosocial summary | 62.36±21.23 (48.88±75.84) | 65.66±23.78 (48.67–89.44) | 69.07±27.79 (47.68–90.46) | 66±26 (44.12–87.54) |
| Peds QoL—parents | Baseline mean±s.d. (95% CI) | 6 months mean±s.d. (95% CI) | 12 months mean±s.d. (95%CI) | 24 months mean±s.d. (95% CI min-max) |
| n=12 | n=9 | n=9 | n=7 | |
| Physical | 53.12±13.71 (44.41–61.83) | 60.41±25.33 (40.9–79.92) | 71.87±14.82 (60.46–86.69) | 67.9±18.2 (51.02–84.68) |
| Emotional | 55.83±18.4 (44.12–67.54) | 53.33±20.76 (37.34–69.32 | 71.11±19.96 (55.74–86.48) | 64.3±21.1 (44.76–83.8) |
| Social | 50.41±20.38 (37.47–63.35) | 57.77±28.51 (35.82–79.72) | 67.77±20.69 (44.91–90.63) | 57.9±33.5 (26.81–88.89) |
| School | 60±20.99 (46.67–73.33) | 62.77±22.92 (45.12–80.42) | 71.66±23.58 (53.6–89.82) | 58.6±30.9 (29.96–87.18) |
| QoL total | 54.61±12.73 (46.53–62.69) | 58.81±21.93 (41.92–75.7) | 70.77±18.31 (56.67–84.87) | 62.9±22.2 (42.35–83.41) |
| QoL physical summary | 53.12±13.71 (44.41–61.83) | 60.41±25.33 (40.9–79.92) | 71.87±14.82 (60.46–83.28) | 67.9±18.2 (51–84.68) |
| QoL psychosocial summary | 55.41±13.22 (47.02–63.8) | 57.96±21.58 (41.35–74.57) | 70.18±22.36 (52.96–87.4) | 60.2±24.8 (37.22–83.18) |
| Physical self perceptions (score range 1–4) | Baseline mean±s.d. (95% CI min-max) | 6 months mean±s.d. (95% CI min-max) | 12 months mean±s.d. (95 %CI min-max) | 24 months mean±s.d. (95% CI min-max) |
| n=12 | n=12 | n=9 | n=8 | |
| Sport competence | 2.86±0.265 (2.09–6.52) | 2.793±0.32 (1.98–3.6) | 2.5±0.21 (0.86–4.14) | 2.45±0.27 (2.24–2.66) |
| Conditioning competence | 2.79±0.207 (2.11–3.47) | 2.63±0.31 (1.86–3.4) | 2.63±0.22 (0.88–4.38) | 2.43±0.31 (2.17–2.69) |
| Attractive body adequacy | 2.24±0.165 (1.65–2.83) | 2.2±0.21 (1.57–2.83) | 2.6±0.24 (2.37–2.83) | 2.61±0.28 (2.37–2.85) |
| Strength competence | 2.62±0.677 (1.81–3.43) | 3.13±1.49 (2.25–4.01) | 2.44±0.22 (0.7–4.14) | 2.21±0.17 (0.79–3.63) |
| Physical self-worth | 2.47±0.425 (1.79–3.15) | 2.46±0.188 (1.76–3.16) | 2.58±0.36 (1.82–3.34) | 2.80±0.38 (2.49–3.11) |
| Global self-worth | 2.65±0.31 (2.4–2.9) | 2.36±0.43 (2.02–2.71) | 2.55±0.40 (2.23–2.87) | 2.4±0.48 (2–2.8) |
| Self perceptions (score range 1–4) | Baseline mean±s.d. (95% CI min-max) | 6 months mean±s.d. (95% CI min-max) | 12 months mean±s.d. (95 %CI min-max) | 24 months mean±s.d. (95% CI min-max) |
| n=8 | n=9 | n=9 | n=8 | |
| Social | 2.7±0.23 (2.52–2.88) | 2.51±0.42 (2.19–2.83) | 2.42±0.35 (2.17–2.67) | 2.3±0.42 (1.95–2.65) |
| Scholastic | 2.5±0.21 (2.34–2.66) | 2.53±0.51 (2.14–2.92) | 2.4±0.40 (2.1–2.7) | 2.6±0.34 (2.32–2.88) |
| Physical activity / physical fitness | Baseline mean±s.d. (95% CI) | 6 months mean±s.d. (95% CI) | 12 months mean±s.d. (95% CI) | 24 months mean±s.d. (95% CI) |
| n=12 | n=9 | n=9 | n=8 | |
| PAQ-A | 1.94±0.66 (1.53–2.35) | 1.75±0.59 (1.35–2.15) | 1.85±0.86 (1.21–2.49) | 1.76±0.71 (1.17–2.35) |
| n=12 | n=8 | n=8 | n=2 | |
| Cardiorespiratory fitness (termination time seconds) | 353.7±146.98 (260.35–447.05) | 636.45±268.22 (377.94–894.96) | 520.95±234.07 (325.66–716.24) | par 1–722.4a par 2–213.6 |
Abbreviations: CI, confidence interval; EBWL, excess body weight lost; PAQ-A, physical activity questionnaire for adolescents; QoL, quality of life.
Displayed as indivdual score due to small sample size.
Secondary outcomes
Psychosocial outcomes
Health-related quality of life
HRQoL scores improved across all domains from baseline to 12 months for the adolescent's and their parents. Parental perceptions of their adolescents' scores were consistently lower than their adolescent scores. Largest change for adolescents was seen in the physical summary scores (mean difference 13.5; d=0.7; P=0.035) with parent's total HRQoL score (mean difference 16.16; d=1.2; P=0.838). A decline across HRQoL scores was observed between 12 and 24 months yet scores remained higher than at baseline.
Physical self perceptions
Reductions were observed in sport competence, conditioning competence, strength competence and global self-worth, when comparing baseline with 12 months. A large increase was seen in attractive body adequacy (mean difference 0.36; d= 3.6; P= 0.403). Social and scholastic scales also showed a reduction at 12 months. At 24 months scores were maintained yet an increase in physical self-worth was observed (mean difference 0.33; d=0.8; P=0.358).
Physical activity and cardiorespiratory fitness
Self-reported PAQ-A scores, marginally decreased at 6months (mean difference 0.19; d=0.3; P=0.891), returned to baseline at 12 months (mean difference 0.09; d=0.1; P=0.992) but decreasing at 24 months. Cardiorespiratory fitness peaked at 6 months (mean difference 282.7; d= 1.9; P=0.013* (*P<0.05)) with improvements maintained higher than baseline scores, at 12 months (167.2; d=1.14; P=0.069). Only two participants completed 24 month follow-up.
Discussion
To the best of our knowledge, this is the first study focusing on the treatment of severe obesity (>99.6th centile) in adolescents that adopts a novel approach, combining an intra-gastric balloon as an adjunct to a lifestyle support programme delivered over a 12 month period.
This unique holistic treatment demonstrates its safety and acceptability in a small pilot of severely obese adolescents. The intra-gastric balloon was well-tolerated with all participants experiencing minimal side effects such as sickness and diarrheoa, with all participants living with the balloon for the full 6-month period. Obesity treatment programmes are commonly associated with high attrition and drop out rates.8 In this study, 75% of participants and families remained in the study at 12 months and attended their follow-up appointment. Adherence with the lifestyle protocol varied significantly, ranging from 7– to 74%— a finding similar to previous studies.30 Although there is a need for effective treatment, identifying the variables associated with attrition could have a direct implication on enhancing adherence rates, thereby potentially enhancing effectiveness.31 No criteria was set for distance to travel for the intervention, resulting in participants from across the Yorkshire and Humber and outside the region as well-being recruited, which could have affected adherence rates.
Intra-gastric balloon treatment is temporary, placing great importance on weight maintenance post balloon removal. Previous evidence in adults11, 32 infers a weight loss at treatment completion not only sufficient to obtain health benefits, but of higher efficacy estimations than for alternative treatments including Orlistat.33, 34 However, available follow-up data shows the majority of weight lost is regained 1 year post treatment.11 The results from this pilot study appear to support the short-term effects observed in adults, with adolescents achieving a BMI Z-score reduction of 0.2 s.ds. at 6-months offering health benefits33 yet were not maintained at 12 months. It is recommended to incorporate strategies on weight loss maintenance and relapse prevention for weight regain into treatment approaches.8 Despite, a structured 8-week maintenance phase built into the BOB study design, uptake from participants and families was poor following balloon removal. Additional research into the effective strategies for adolescents at this time is needed to maximise treatment success and prevent weight regain post treatment.35
Overweight and obese young people who have a higher cardiorespiratory fitness have been associated with a lower overall total adiposity.36 Waist circumference, a measure of adiposity, was lower at 12 months and highlighted a large effect in this sample, inferring the potential additional benefit the combination of intra-gastric balloon and lifestyle programme had in promoting a physically active lifestyle. Although only modest changes were self-reported on the physical activity questionnaire in the 7 days before conducting the assessment(s), improvements in physical fitness were observed and maintained at 12 months. Coupled with maximal efforts received using the pictorial children's effort rating table for children27 data here demonstrate not only the adolescents ability to work to perceived maximum effort, but the importance of including an objective measure of fitness combined with the self-reported physical activity measure.
HRQoL is a comprehensive and multidimensional construct19 that includes physical, emotional, social and school functioning—all influential when working with adolescents.19 Obese adolescents reportedly have lower HRQoL scores than their healthy weight counterparts.37 A previous study found obese children and adolescents reported significant impairment not only in total scale score (mean score was 67 for obese children and adolescents compared with 83 for healthy children and adolescents), but also across all domains—physical, psychosocial, emotional, social and school functioning—in comparison with healthy children and adolescents.38 Noticeably in this study, child self-report baseline scores (Table 1) across all domains (physical, emotional, social and school) were low when compared with other studies in overweight and obese adolescents, inferring HRQoL worsens with the degree of obesity.39 Changes in total score; physical summary score and psychosocial summary scores between baseline and 12 months all exceeded the minimally important clinical difference criterion expressed by Varni et al.20 Of interest, scores remained higher at 12 months from baseline across all domains irrespective of the pattern of weight regain, suggesting other variables, such as treatment approach, physical activity and life events, could have independent effects on improving HRQoL.20, 40, 41 Yet, many studies continue to combine child and adolescent age groups42 making it difficult to determine adolescent-specific outcomes.43 What these results reinforce is the need for treatment to focus specifically on severely obese adolescents as a distinct population to begin to understand the complexity.
Parental proxy measures reported here (mean total score of 54.61 at baseline), were low when compared with the parents of obese children and adolescents (mean total score of 63.3) and parents of healthy weight children (mean total score of 87.6).37 All change values exceeded the minimal clinical important difference specified.39 In addition, parents throughout this study consistently perceived a worse QoL for their child in line with previous findings.44 The reason for this discrepancy is unknown, but not unique to obesity. A possibility could be parent's catastrophise the situation or lack understanding of their child's lived experience.20 Given the role parents have in seeking obesity treatment, it is critical that their perspective is captured. Further research is needed to elicit the degree of weight change needed to influence QoL scores and to explore mediators of this relationship.
Physical and self perceptions scores were similar to scores reported by overweight and obese counterparts.45 Obese adolescents have lower self-esteem than healthy weight counterparts but the way they view and feel about their bodies is likely to be heavily implicated in the development and continuing presence of more-serious psychopathologic conditions.45 Positive changes observed and maintained across 6, 12 and 24 month follow-up period within the physical self-perception domain (general feelings of satisfaction and confidence regarding the self in the physical domain) and body attractiveness scale (attractiveness of their bodies and how confident they feel about their appearance), in addition to a large effect within the strength domain at 6 months (perception of strength and muscle development), infers participation in a tailored physical activity and lifestyle intervention enables severely obese adolescents to view themselves and their bodies more favourably in the shorter term.
Conclusions and limitations
This study is one of the first to specifically tailor a treatment approach for severely obese adolescents and their families. Findings contribute to the existing literature on the safety and acceptability of an intra-gastric balloon, as an adjunct to a lifestyle support programme, to induce short-term weight loss and produce clinically important improvements in HRQoL.
These results must be interpreted with several limitations in mind. First, this is an un-controlled pilot study with a small sample; therefore inferences to efficacy and effectiveness of the intervention cannot be reported. This study fulfills the purpose of a pilot study, gathering information on the design, assessment procedures, and implementation of the novel intervention to inform a future research controlled trial. In light of this, a conscious choice to include the metric of meaningfulness, namely effect size27 with the presentation of 95% CIs were used to allow a meaningful interpretation of the data set, alongside statistical null hypothesis testing, therefore strengthening this study. Second, the lifestyle programme was delivered within a university research environment, reinforcing a key challenge for obesity treatment—the transition from a supportive intervention to longer term behaviour change at home.33 Further work is needed to explore the integration of families' real world environment within intervention programmes to support long-term behavioural change.
The use of an intra-gastric balloon and the delivery of a lifestyle behavioural programme is a safe, acceptable and well-tolerated technique within a pilot sample of severely obese adolescents. This novel approach offers potential to produce short-term reductions in BMI Z-score and physical fitness, which is known to have beneficial impact on health and well-being later in life.2 Results also exceeded the minimal clinical important differences in all domains of HRQoL, with improvements sustained at 12 months. Furthermore, the detailed reporting on the lifestyle programmes content12 provides important and pragmatic information to assist researchers and practitioners in the design and implementation of future programmes tailored to severely obese adolescents and their families. Further research is needed on the maintenance of positive changes longer term and the integration of programmes within families' home life.
Acknowledgments
We thank all the families participating in this research and Lizzy DeAngelis for providing the dietetic support in this study. This paper presents independent research as part of the Obesity Theme within the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care for South Yorkshire (NIHR CLAHRC SY). The views and opinions expressed are those of the authors, and not necessarily those of the NHS, the NIHR or the Department of Health. CLAHRC SY would also like to acknowledge the participation and resources of our partner organisations. Further details can be found at www.clahrc-sy.nihr.ac.uk.
Footnotes
The authors declare no conflict of interest.
References
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011; 378: 815–825. [DOI] [PubMed] [Google Scholar]
- Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation 2013; 128: 1689–1712. [DOI] [PubMed] [Google Scholar]
- Pesa JA, Syre TR, Jones E. Psychosocial differences associated with body weight among female adolescents: the importance of body image. J Adolesc Health 2000; 26: 330–337. [DOI] [PubMed] [Google Scholar]
- Cornette R. The emotional impact of obesity on children. Worldviews Evid Based Nurs 2008; 5: 136–141. [DOI] [PubMed] [Google Scholar]
- Wills W, Backett-Milburn K, Gregory S, Lawton J. Young teenagers' perceptions of their own and others' bodies: A qualitative study of obese, overweight and ‘normal'weight young people in scotland. Soc Sci Med 2006; 62: 396–406. [DOI] [PubMed] [Google Scholar]
- Cole TJ. Growth monitoring with the British 1990 growth reference. Arch Dis Child 1997; 76: 47–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ells LJ, Hancock C, Copley VR, Mead E, Dinsdale H, Kinra S et al. Prevalence of severe childhood obesity in England: 2006–2013. Arch Dis Child 2014; 100: 631–636. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. Managing overweight and obesity in children and young people: lifestyle weight management services, 2013.
- Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP et al. Interventions for treating obesity in children. Cochrane Database Syst Rev e-pub ahead of print 21 January 2009 doi:10.1002/14651858.CD001872.pub2. [DOI] [PubMed]
- Dogan UB, Gumurdulu Y, Akin MS, Yalaki S. Five percent weight lost in the first month of intra-gastric balloon treatment may be a predictor for long-term weight maintenance. Obes Surg 2013; 23: 892–896. [DOI] [PubMed] [Google Scholar]
- Dumonceau J. Evidence-based review of the Bioenterics intra-gastric balloon for weight loss. Obes Surg 2008; 18: 1611–1617. [DOI] [PubMed] [Google Scholar]
- Reece L, Copeland R, Sachdev P, Thomson M, Wales J. Protocol for: the use of intra-gastric balloons as an adjunct to a lifestyle support programme to promote weight loss in severely obese adolescents. J Child Adolesc Behav 2014; 2: 173. [Google Scholar]
- Prochaska JO, DiClemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychother Theory Res Pract 1982; 19: 276. [Google Scholar]
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991; 50: 179–211. [Google Scholar]
- Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011; 26: 1479–1498. [DOI] [PubMed] [Google Scholar]
- Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat 2005; 4: 287–297. [Google Scholar]
- Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child 1995; 73: 25–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni JW, Burwinkle TM. The PedsQL as a patient-reported outcome in children and adolescents with attention-deficit/hyperactivity disorder: a population-based study. Health Qual Life Outcomes 2006; 4: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales in healthy and patient populations. Med Care 2001; 39: 800–812. [DOI] [PubMed] [Google Scholar]
- Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 2003; 3: 329–341. [DOI] [PubMed] [Google Scholar]
- Fox CL, Farrow CV. Global and physical self-esteem and body dissatisfaction as mediators of the relationship between weight status and being a victim of bullying. J Adolesc 2009; 32: 1287–1301. [DOI] [PubMed] [Google Scholar]
- Raustrop A, Stahle A, Gudasic H, Kinnunen A, Mattsson E. Physical activity and self-perception in school children assessed with the children and youth- physical self-perception profile. Scand J 2005; 15: 126–134. [DOI] [PubMed] [Google Scholar]
- Harter S. Manual for the Self-Perception Profile for Adolescents. University of Denver: Denver, 1988. [Google Scholar]
- Crocker PR, Bailey DA, Faulkner RA, Kowalski KC, McGrath R. Measuring general levels of physical activity: preliminary evidence for the physical activity questionnaire for older children. Med Sci Sports Exerc 1997; 29: 1344–1349. [DOI] [PubMed] [Google Scholar]
- Rowland TW, Rambusch JM, Staab JS, Unnithan VB, Siconolfi SF. Accuracy of physical working capacity (PWC170) in estimating aerobic fitness in children. J Sports Med Phys Fitness 1993; 33: 184–188. [PubMed] [Google Scholar]
- Marinov B, Kostianev S, Turnovska T. Ventilatory efficiency and rate of perceived exertion in obese and non-obese children performing standardized exercise. Clin Physiol Funct Imag 2002; 22: 254–260. [DOI] [PubMed] [Google Scholar]
- Yelling M, Lamb KL, Swaine IL. Validity of a pictorial perceived exertion scale for effort estimation and effort production during stepping exercise in adolescent children. Eur Phys Educ Rev 2002; 8: 157–175. [Google Scholar]
- Cohen J. A power primer. Psychol Bull 1992; 112: 155. [DOI] [PubMed] [Google Scholar]
- Winter EM, Abt GA, Nevill AM. Metrics of meaningfulness as opposed to sleights of significance. J Sports Sci 2014; 32: 901–902. [DOI] [PubMed] [Google Scholar]
- Skelton J, Beech B. Attrition in pediatric weight management: a review of the literature and new directions. Obes Rev 2011; 12: e273–e281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelalian E, Hart C N, Mehlenbeck R S, Lloyd-Richardson E E, Kaplan J D, Flynn-O'Brien K T et al. Predictors of attrition and weight loss in an adolescent weight control program. Obesity 2008; 16: 1318–1323. [DOI] [PubMed] [Google Scholar]
- Imaz I, Martínez-Cervell C, García-Álvarez EE, Sendra-Gutiérrez JM, González-Enríquez J. Safety and effectiveness of the intra-gastric balloon for obesity: a meta-analysis. Obes Surg 2008; 18: 841–846. [DOI] [PubMed] [Google Scholar]
- Li Z, Maglione M, Tu W, Mojica W, Arterburn D, Shugarman LR et al. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med 2005; 142: 532–546. [DOI] [PubMed] [Google Scholar]
- Ford AL, Hunt LP, Cooper A, Shield JP. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardio metabolic health? Arch Dis Child 2010; 95: 256–261. [DOI] [PubMed] [Google Scholar]
- Altman M, Wilfley DE. Evidence update on the treatment of overweight and obesity in children and adolescents. J Clin Child Adolesc Psychol 2015; 44: 521–537. [DOI] [PubMed] [Google Scholar]
- Ortega F, Ruiz J, Castillo M, Sjöström M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes 2008; 32: 1–11. [DOI] [PubMed] [Google Scholar]
- Buttitta M, Iliescu C, Rousseau A, Guerrien A. Quality of life in overweight and obese children and adolescents: a literature review. Qual Life Res 2014; 23: 1117–1139. [DOI] [PubMed] [Google Scholar]
- Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA 2003; 289: 1813–1819. [DOI] [PubMed] [Google Scholar]
- Burke SM, Shapiro S, Petrella RJ, Irwin JD, Jackman M, Pearson ES et al. Using the RE-AIM framework to evaluate a community-based summer camp for children with obesity: a prospective feasibility study. BMC Obes 2015; 2: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsiros MD, Olds T, Buckley JD, Grimshaw P, Brennan L, Walkley J et al. Health-related quality of life in obese children and adolescents. Int J Obes 2009; 33: 387–400. [DOI] [PubMed] [Google Scholar]
- Morrison KM, Shin S, Tarnopolsky M, Taylor VH. Association of depression & health related quality of life with body composition in children and youth with obesity. J Affect Disord 2015; 172: 18–23. [DOI] [PubMed] [Google Scholar]
- Doyle AC, Goldschmidt A, Huang C, Winzelberg AJ, Taylor CB, Wilfley DE. Reduction of overweight and eating disorder symptoms via the Internet in adolescents: a randomized controlled trial. J Adolesc Health 2008; 43: 172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinbeck K, Baur L, Cowell C, Pietrobelli A. Clinical research in adolescents: challenges and opportunities using obesity as a model. Int J Obes 2009; 33: 2–7. [DOI] [PubMed] [Google Scholar]
- Zeller MH, Modi AC. Predictors of health-related quality of life in obese youth. Obesity 2006; 14: 122–130. [DOI] [PubMed] [Google Scholar]
- Daley A J, Copeland R J, Wright N P, Roalfe A, Wales J K H. Exercise therapy as a treatment for psychopathologic conditions in obese and morbidty obese adolescents: a randomized, controlled trial. Pediatrics 2006; 118: 2126–2134. [DOI] [PubMed] [Google Scholar]