Abstract
Purpose
Femoral osteochondritis dissecans (OCD) is a disorder of unknown aetiology and variable prognosis that causes knee pain. In this paper, the authors study the impact of lower limb malalignment on the development and prognosis of OCD.
Methods
After anteroposterior (AP) and lateral radiograph and MRI of the knee, 53 cases of OCD were diagnosed. All patients were studied by standing full-length AP radiograph of the lower extremities in order to analyse the relationship between the femorotibial and mechanical axis and the location and stability of the osteochondritis.
Results
The OCD lesion was located in the medial condyle (zone 2) in 75.5% of cases (40 cases). The lateral condyle was affected in 24.5% of cases (zone 4 in nine cases and zone 5 in four cases). The femorotibial angle (anatomical axis) was normally aligned in 68% of cases. A valgus deformity was observed in 9.5% of cases and a varus deformity in 22.5%. The mechanical axis of the limb appeared normal in only 32% of cases, with medial deviation in 53%, and lateral deviation in 15% of cases. When the OCD lesion was located in the medial condyle (40 cases), the mechanical axis also crossed the knee through the medial zone in 28 cases. When the OCD lesion was located in the lateral condyle (13 cases), the mechanical axis crossed the knee through zones 1 or 2 in four cases. In stable OCD, the mechanical axis and location of the lesion coincided in 19 of 36 cases (52%), compared with 16 of 17 cases (94%) in unstable OCD.
Conclusions
There is a high correlation between OCD location and lower limb mechanical axis deviation. The convergence of the mechanical axis with the location of the OCD lesion may be considered an associated factor in fragment instability. This convergence is more common in unstable OCD.
Keywords: osteochondritis dissecans, mechanical axis, tibiofemoral angle, genu varum, genu valgum
Introduction
Osteochondritis dissecans (OCD) is a knee disorder that affects children, adolescents and young adults with a prevalence of 0.05% to 0.08%. To date, the aetiology of OCD is unknown.1 Predisposing or possible causes include vascular factors (subchondral bone ischaemia may result in cartilaginous lesion), traumatic factors and repetitive microtrauma with the tibial intercondylar eminences or the meniscus pathology influence. None of these causes have been irrefutably confirmed and only explain some cases of OCD.1–3
To date, age has been considered the most important prognostic factor. Evolution is excellent in the youngest patients. In children, the disorder normally resolves spontaneously without special treatment measures. In adolescents close to skeletal maturation or young adults, however, the evolution is less predictable and sometimes torpid, especially if MRI reveals joint effusion, a lesion diameter of more than 20 mm or subchondral dissection. Surgery is often required to fix or remove the fragment.4
The OCD lesion is more commonly located in the lateral part of the medial condyle (57% to 83%) than in the lateral condyle (20%). Bilateral involvement is not uncommon (26%),5 but always affects the same condyle, either medial or lateral, making the lesions symmetrical. In contrast, bicondylar unilateral OCD has only been reported in patients with systemic diseases, genetic syndromes or predisposition.6
There is little mention in the literature of the potential influence of lower limb alignment on the development of OCD in the weight-bearing areas of the femoral condyles. Aichroth mentioned the relationship between alterations of the lower limb axis and the location of osteochondritis, and very few authors have indicated that treating femorotibial malalignment is required to resolve these lesions.5–8
In this paper, we review diagnosed cases of femoral OCD in children, adolescents and young adults, and the possible influence of the weight-bearing axis and the femorotibial angle of the lower limbs.
Patients and Methods
We carried out a retrospective cross-sectional observational study of patients with OCD of the femoral condyle diagnosed between January 2002 and December 2014. We excluded patients with osteochondritis secondary to treatments, systemic diseases, trauma and torsion defects, patients who had asymptomatic lesions with radiological images suggestive of normal variation of ossification and patients with incomplete radiological testing. Children with a history of any underlying neuromuscular disorder were also excluded.
The data collected for each patient were: age, sex, side, open or closed growth plates, location and degree of stability of the lesion, the lower limb femorotibial angle and the mechanical axis, defined as the line running from the centre of the femoral head to the centre of the ankle in a standing full-length anteroposterior (AP) radiograph of the lower extremities.
The location of the lesion in the AP radiography was described according to the classifications of Cahill and Berg (Fig. 1).9
Fig. 1.
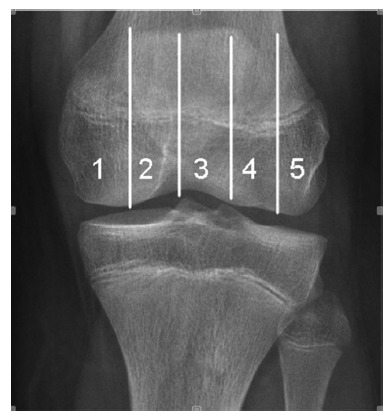
Cahill and Berg9 areas of the knee in anteroposterior projection: areas 1 and 2 are in the medial condyle, area 3 is the central zone bordered by the intercondylar tibial eminences, and areas 4 and 5 are in the lateral condyle.
The stability of the lesion was classified using the radiographs and MRI images, according to the criteria of Dipaol, Nelson and Colville.10 Groups I and II are stable forms, while groups III and IV are considered to be unstable forms.10–12
All of the patients had full-length standing AP radiographs of both lower extremities using a standardised computed radiography technique, with the patient facing the radiography tube and both patellae pointing anteriorly (‘patella forward’ position). The femorotibial angles were measured (normal 173º ± 5º), as were the mechanical or weight-bearing axes, with physiological axes defined as those running between the tibial intercondylar eminences (Zone 3 of Cahill and Berg). These parameters were measured with a goniometer or using the Centricity 2006 GE Medical Systems programme for patients, with images in digital format.
The epidemiological and radiological data collected were analysed with the programme SPSS Inc. (Chicago, Illinois). A descriptive study was performed, describing the quantitative variables as means and the qualitative variables as absolute values and percentages (%). The statistical significance of the qualitative variables was measured with the chi-squared test (open or closed physis, location of the lesion, mechanical axis and stability of the osteochondral fragment).
Results
We studied 53 cases of OCD in 48 patients. The mean age was 13.7 years (8 to 35). Of the 48 patients, 77% were male (41 cases) and 23% were female (12 cases). With regard to laterality, 27 lesions were located in the right knee and 26 in the left (five patients had bilateral forms). The growth plate was open in 43 patients.
The lesion was stable in 68% of cases (grade 1 in 16 cases and grade 2 in 20 cases) and unstable in 32% (grade 3 in eight cases and grade 4 in nine cases). The mean age of the patients with stable lesions (11.6 years) was significantly lower than for unstable forms (18.4 years) (p < 0.001).
If we take into account the skeletal maturity, comparing patients with open and closed physis regarding the stability of the lesion, we may observe that mature patients present a much higher proportion of unstable forms than those presenting open physis (p = 0.0003).
The OCD lesion was located in zone 2 of the Cahill and Berg classification in 40 cases (75.5%), in zone 4 in nine cases (17%) and in zone 5 in four cases (7.5%). The lateral condyle was affected in 24.5% and the medial condyle in 75.5% of cases. We did not find any relationship between the location of the lesion and stability.
The femorotibial angle was normally aligned (173º ± 5º) in 36 cases (68%). We found a valgus deformity in five cases (9.5%) and a varus deformity in 12 cases (22.5%). No connection with the degree of stability was apparent. We found, however, that in one-third of our cases (32.1%), the medial or lateral location of the lesion coincided with the varus or valgus deformity, respectively (Table 1).
Table 1.
Relationship between location of osteochondritis dissecans (OCD) lesion and femorotibial axis.
| OCD | Varus | Neutral | Valgus |
|---|---|---|---|
| 1 | |||
| 2 | 12 | 28 | |
| 4 | 8 | 3 | |
| 5 | 2 |
The weight-bearing or mechanical axis ran through zone 1 in four cases (7.5%), through zone 2 in 24 cases (45.3%), through zone 3 (normal alignment) in 17 cases (32.1%), through zone 4 in six cases (11.3%) and through zone 5 in two cases (3.8%). There were statistically significant differences (p < 0.01) in the relationship between the presence of mechanical axis alteration and the location of the osteochondritis. In 97% of the cases with malalignment, the mechanical axis and the location of the lesion coincided (Table 2). We have found a lower coincidence between the location of the lesion and the mechanical axis in immature patients presenting open physis (26 out of 43 patients), as compared with patients presenting closed physis (9 out of 10) (p = 0.07).
Table 2.
Location of osteochondritis dissecans (OCD) lesion in relation to the mechanical axis. In 35 cases, the site of osteochondritis coincided with the mechanical axis of the limb. In 18 patients, there was no convergence. These findings show a statistically significant difference (p < 0.01).
| OCD\AXIS | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1 | |||||
| 2 | 4 | 24 | 11 | 1 | |
| 4 | 6 | 3 | |||
| 5 | 2 | 2 |
Shaded areas represent coincidence between the mechanical axis and location of the lesions
In the unstable forms, the rate of convergence between the mechanical axis and the location of the OCD lesion was 94% (16 of 17 cases) and the mean age of patients was 18.4 years, while in the stable forms the rate of convergence was only 53% (19 of 36 cases) and the mean age was 11.6 years (p < 0.01) (Table 3). We have found similar results when relating it with the skeletal maturity. In immature patients, 34 out of 43 present stable lesion, while in patients with closed physis, we only found two stable lesions out of ten.
Table 3.
Relationship of convergence or lack of convergence between osteochondritis dissecans (OCD) site and mechanical axis with the stability of the osteochondral fragment and average age. In 94% of grade II to IV cases, the location of the OCD lesion converged with the mechanical axis. These findings show a statistically significant difference (p < 0.01).
| Convergence + | Convergence - | Mean age (yrs) | |
|---|---|---|---|
| GRADE I-II | 19 | 17 | 11.6 |
| GRADE III-IV | 16 | 1 | 18.4 |
Discussion
It is well known that age is a prognostic factor in OCD, with good evolution common among younger patients, especially those aged under ten years old. In adolescents and young adults, however, the prognosis is uncertain and the disorder often develops into unstable forms that require surgical treatment.4 There have been several hypotheses on the singularity of this critical age in the unstable forms of OCD, such as the hypothesis developed by Robertson, Kelly and Green,13 who postulated that repeated microtrauma could interrupt the tenuous epiphyseal blood supply during the period of rapid growth in adolescence. In our series, we found statistically significant differences (p < 0.001) in the relationship between age and skeletal maturity and lesion stability.
In the cases subject to study, we have included patients with open (43 cases) and closed physis (ten cases). Although it is well known that there is a different prognosis for the two groups, we think that this allows us to confirm it. In addition, it supports the thesis that those patients that present (1) coincidence between mechanical axis and location of the lesion and (2) since their growth is over and they cannot alter the limb axis, are those that present a higher risk of developing unstable forms of OCD.
One constant finding in cases of OCD is the tendency of the most lateral part of the medial condyle to be affected, suggesting that friction or microtraumas with the intercondylar tibial eminences may be involved in the aetiology of the disorder. It is also common for bilateral lesions to mirror each other. It is exceptional, however, for both condyles of the same knee to be affected. This supports the fact that the alignment of the lower limbs could influence the development and location of the femoral OCD lesion.
To date, few studies have made a connection between the development of OCD and the mechanical axis of the limb.14,15 In our series, we observed a convergence between the weight-bearing axis and the location of the osteochondritis in 66% of cases. This rate increases to 97% if we consider only the cases with axis misalignment. We found statistically significant differences (p < 0.01) in the relationship between the presence of mechanical axis alteration and the location of the osteochondritis.
This fact may be closely connected to the stability of the lesion, since, in the unstable forms, the mechanical axis converged with the OCD lesion in 94% of cases, while in the stable forms this convergence was present in only 53% of cases (p > 0.01) (Fig. 2). The mean that age of the patients with stable lesions (11.6 years) was significantly lower than for unstable forms (18.4 years) (p < 0.001).
Fig. 2.
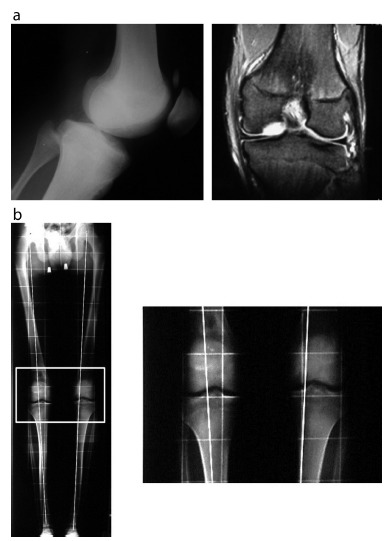
(a) Radiograph and MRI of a 16-year-old boy with unstable medial condyle osteochondritis dissecans (OCD) with an intra-articular free body. (b) Anteroposterior stand-up radiograph of lower limbs showing convergence between the OCD lesion and the mechanical axis of the left limb.
We found that the femorotibial angle was altered in only one-third of cases, which means that this radiological parameter cannot be so readily associated with the site of osteochondritis. However, in the cases in which we observed a varus or valgus deviation (32% of cases), we found that the osteochondritis coincided in all cases with location on the medial or lateral condyle, respectively. We have not been able to establish a connection between axis alteration and lesion stability.
There is little mention in the literature of the potential importance of frontal plane lower limb alignment in the development of OCD in the weight-bearing areas of the femoral condyles. In a study on 100 patients with OCD, Aichroth performed a clinical evaluation of the limbs and found a 14% rate of misalignment.5 Bruns and Klima observed that in 109 lesions in 97 patients, there was a connection between varus deformity of the knee and development of OCD in the medial condyle.6 Slawski treated seven knees in six adult patients with OCD and without knee osteoarthritis through proximal tibial osteotomy. In all cases there was varus deformity of the knee which improved significantly after treatment.8 Jacobi et al,15 in their study on 103 cases of OCD, found greater mechanical axis deviation in the cases in which the lesion was located in the medial condyle compared to the lateral condyle. The authors indicated that the alteration of this axis results in overload and may be a co-factor in the pathogenesis of OCD. Consistent with these authors, the misalignment of the limbs affected by OCD may be subtle, and for this reason the femorotibial axis may not be as effective an indicator of these slight misalignments as the mechanical axis.
Although the aetiology of OCD is unknown, we believe that, in light of these results, lower limb axiality may be a factor that influences the stability and severity of OCD. In this regard, the physiological variation of the mechanical axis16 that occurs during childhood may contribute to this phenomenon.
In conclusion, although our series is limited by the number of cases and requires specific follow-up of the patients who are still growing (an objective of the second part of our study), we would like to highlight the high convergence between femoral OCD development and lower limb axis alteration. The mechanical axis is a more reliable indicator than the femorotibial axis of slight varus or valgus alterations. The development of OCD in which the weight-bearing axis converges with the site of the osteochondral lesion should be considered a factor of poor prognosis. In these at-risk patients with open physis, we are carrying out a temporary hemiepiphysiodesis to normalise the mechanical axis in order to try to change the natural course of this process, and our results are still in development.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Kocher MS, Tucker R, Ganley TJ, Flynn JM.. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med 2006;34:1181–1191. [DOI] [PubMed] [Google Scholar]
- 2. Flynn JM, Kocher MS, Ganley TJ.. Osteochondritis dissecans of the knee. J Pediatr Orthop 2004;24:434–443. [DOI] [PubMed] [Google Scholar]
- 3. Camathias C, Hirschmann MT, Vavken P, et al. . Meniscal suturing versus screw fixation for treatment of osteochondritis dissecans: clinical and magnetic resonance imaging results. Arthroscopy 2014;30:1269–1279. [DOI] [PubMed] [Google Scholar]
- 4. Hefti F, Beguiristain J, Krauspe R, et al. . Osteochondritis dissecans: a multicentric study of the European Pediatric Orthopedic Society. J Pediatr Orthop 1999;8:231–245. [PubMed] [Google Scholar]
- 5. Aichroth P.. Osteochondritis dissecans of the knee. A clinical survey. J Bone Joint Surg [Br] 1971;53-B:440–447. [PubMed] [Google Scholar]
- 6. Bruns J, Klima H. [Osteochondrosis dissecans of the knee and sports]. Sportverletz Sportschaden 1993;7:68–72. (In German) [DOI] [PubMed] [Google Scholar]
- 7. Bruns J, Volkmer M, Luessenhop S.. Pressure distribution at the knee joint. Influence of varus and valgus deviation without and with ligament dissection. Arch Orthop Trauma Surg 1993;113:12–19. [DOI] [PubMed] [Google Scholar]
- 8. Slawski DP.. High tibial osteotomy in the treatment of adult osteochondritis dissecans. Clin Orthop Relat Res 1997;341:155–161. [PubMed] [Google Scholar]
- 9. Cahill BR, Berg BC.. 99m-Technetium phosphate compound joint scintigraphy in the management of juvenile osteochondritis dissecans of the femoral condyles. Am J Sports Med 1983;11:329–335. [DOI] [PubMed] [Google Scholar]
- 10. Dipaola JD, Nelson DW, Colville MR.. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy 1991;7:101–104. [DOI] [PubMed] [Google Scholar]
- 11. O’Connor MA, Palaniappan M, Khan N, Bruce CE.. Osteochondritis dissecans of the knee in children. A comparison of MRI and arthroscopic findings. J Bone Joint Surg [Br] 2002;84-B:258–262. [DOI] [PubMed] [Google Scholar]
- 12. Pill SG, Ganley TJ, Milam RA, et al. . Role of magnetic resonance imaging and clinical criteria in predicting successful nonoperative treatment of osteochondritis dissecans in children. J Pediatr Orthop 2003;23:102–108. [PubMed] [Google Scholar]
- 13. Robertson W, Kelly BT, Green DW.. Osteochondritis dissecans of the knee in children. Curr Opin Pediatr 2003;15:38–44. [DOI] [PubMed] [Google Scholar]
- 14. González-Herranz P, de la Fuente C, Castro Torre M.. Femoral osteochondritis dissecans. Prognostic value of the load axis. J Bone Joint Surg [Br] 2006;88-B(Suppl II):327. [Google Scholar]
- 15. Jacobi M, Wahl P, Bouaicha S, Jakob RP, Gautier E.. Association between mechanical axis of the leg and osteochondritis dissecans of the knee: radiographic study on 103 knees. Am J Sports Med 2010;38:1425–1428. [DOI] [PubMed] [Google Scholar]
- 16. Salenius P, Vankka E.. The development of the tibiofemoral angle in children. J Bone Joint Surg [Am] 1975;57-A:259–261. [PubMed] [Google Scholar]


