Abstract
Introduction:
Reducing unplanned hospital readmissions has become a national focus due to the Centers for Medicare and Medicaid Services’ (CMS) penalties for hospitals with high rates. A first step in reducing unplanned readmission is to understand which patients are at high risk for readmission, which readmissions are planned, and how well planned readmissions are currently captured in comparison to patient-level chart review.
Methods:
We examined all 5455 inpatient neurology admissions over a 2-year period to University of California San Francisco Medical Center and Johns Hopkins Hospital via chart review. We collected information such as patient age, procedure codes, diagnosis codes, all-payer diagnosis-related group, observed length of stay (oLOS), and expected length of stay. We performed multivariate logistic modeling to determine predictors of readmission. Discharge summaries were reviewed for evidence that a subsequent readmission was planned.
Results:
A total of 353 (6.5%) discharges were readmitted within 30 days. Fifty-five (15.6%) of the 353 readmissions were planned, most often for a neurosurgical procedure (41.8%) or immunotherapy (23.6%). Only 8 of these readmissions would have been classified as planned using current CMS methodology. Patient age (odds ratio [OR] = 1.01 for each 10-year increase, P < .001) and estimated length of stay (OR = 1.04, P = .002) were associated with a greater likelihood of readmission, whereas index admission oLOS was not.
Conclusions:
Many neurologic readmissions are planned; however, these are often classified by current CMS methodology as unplanned and penalized accordingly. Modifications of the CMS lists for potentially planned neurological and neurosurgical procedures and for acute discharge neurologic diagnoses should be considered.
Keywords: clinical specialty, general neurology, neurohospitalist, neurosurgery, quality, safety, techniques
Introduction
Reducing readmissions has become a focus of policy makers due to its potential to lower costs and improve transitions of care. In 2012, the Centers for Medicare & Medicaid Services (CMS) initiated the Hospital Readmissions Reduction Program, which penalizes hospitals with readmission rates that are deemed excessive. When the program began, it was limited to 3 index admission conditions: acute myocardial infarction, pneumonia, and congestive heart failure.1 Three additional conditions were added in 2014 (chronic obstructive pulmonary disease, total hip arthroplasty, and total knee arthroplasty).1 In 2013, CMS developed the hospital-wide all-cause unplanned readmission measure, a claim-based, risk-adjusted, publicly reported measure of care quality for hospitalized patients, including those admitted for neurology services.2 The Hospital Readmissions Reduction Program, with penalties now as high as 3% of a hospital’s total CMS payments, has prompted clinical interventions to improve discharge planning, ensure timely follow-up, and improve the inpatient to outpatient transition.3 Importantly, CMS recognizes that certain planned readmissions do not reflect poor care quality and thus has made an effort to identify and exclude planned readmissions from its hospital readmission measure. The CMS has defined planned readmissions as those for organ transplantation, maintenance chemotherapy, rehabilitation, or a list of procedures for nonacute discharge diagnoses (Table 1).4 Any nonacute hospital readmission with a discharge condition including one of these procedures is excluded from the hospital readmission calculation and therefore not penalized.
Table 1.
CMS Criteria for Planned Readmissions, Potentially Planned Neurological and Neurosurgical Procedures, and Acute Neurological and Neurosurgical Discharge Diagnosis Categories Classified as Never Planned.4
| CMS criteria for planned readmissions: |
| 1. Always planned readmission procedure and diagnosis categories |
| Transplant surgery |
| Maintenance chemotherapy |
| Rehabilitation |
| Cesarean section; forceps, vacuum, and breech delivery are included in all-payer population |
| Or |
| 2. A nonacute readmission for a planned procedure, excluding for acute illness or for complications of care |
| A procedure is performed that is in one of the categories that are always planned regardless of diagnosis |
| Or |
| The principle diagnosis is in one of the diagnosis categories that are always planned |
| Or |
| A procedure is performed that is in one of the potentially planned procedure categories, and the principle diagnosis is not in the list of acute discharge diagnoses |
| CMS potentially planned neurological and neurosurgical procedures: |
| Laminectomy, excision intervertebral disc |
| Insertion of catheter or spinal stimulator and injection into spinal |
| Other OR therapeutic nervous system procedures |
| Endarterectomy, vessel of head and neck |
| Other OR procedures on vessels of head and neck |
| Spinal fusion |
| CMS acute neurological and neurosurgical discharge diagnosis categories: |
| Meningitis (except that caused by tuberculosis or sexually transmitted disease) |
| Encephalitis (except that caused by tuberculosis or sexually transmitted disease) |
| Other CNS infection and poliomyelitis |
| Paralysis |
| Epilepsy, convulsions |
| Headache, including migraine |
| Coma, stupor, and brain damage |
| Blindness and vision defects |
| Conditions associated with dizziness or vertigo |
| Acute cerebrovascular disease |
| Transient cerebral ischemia |
| Spinal cord injury |
| Intracranial injury |
| Syncope |
| Delirium, dementia, amnestic, and other cognitive disorders |
Abbreviations: CMS, Centers for Medicare and Medicaid Services; CNS, central nervous system; OR, operating room.
Despite this focus on readmissions, little is known regarding readmissions for patients with a diverse set of neurologic conditions.5 Much of the previous work has focused on ischemic and hemorrhagic stroke6-14 and epilepsy,15 which represent only a fraction of the burden of neurological disease in the United States.16 Furthermore, even less is known regarding how many readmissions from neurological disease represent unplanned, and hence potentially preventable, encounters and how many represent planned neurological readmissions that CMS may or may not accurately identify using their current methodology.
Although national data sets can provide a “high-level” snapshot of readmission rates and predictors of readmission,5 examination of patient-level data via detailed chart review can more precisely understand the frequency and characteristics of planned readmissions among neurologic inpatients as well as general predictors of 30-day readmission. We aimed to answer these questions using an analysis by chart review of all admissions to 2 tertiary care academic hospitals in the United States.
Methods
The study design and procedures were approved by the institutional review board at Johns Hopkins University and the Committee on Human Research at the University of California San Francisco (UCSF). A waiver of informed consent was granted. We conducted a retrospective cohort study that included all inpatient encounters involving patients aged 18 years or older who were discharged from the neurologic services at UCSF Medical Center and Johns Hopkins Hospital between May 1, 2012, and April 30, 2014. The neurology inpatients at these tertiary academic hospitals are cared for by the general neurology, cerebrovascular, and epilepsy monitoring unit services. At both hospitals, the majority of patients with primary neurological diagnoses are admitted to or transferred to and subsequently discharged from these dedicated inpatient neurological services. We included all index admissions due to transfer to capture as many readmissions to the respective tertiary centers, recognizing that many such patients would be more likely to be readmitted to other institutions. We excluded all encounters that resulted in death before discharge and those patients who left against medical advice. We then identified which of these index encounters led to subsequent readmission to any service of the respective hospital within 30 days of discharge. For patients with many encounters, this methodology allows an admission to be considered both a readmission and an index admission. We calculated a readmission rate by dividing the number of readmissions by the number of index admissions, which is consistent with methodology for calculating readmission rates from Vizient (formerly University HealthSystem Consortium), the largest member-owned health-care company in the country that maintains a Clinical Data Base/Resource Manager (CDB/RM) with national administrative claims of extracted patient data for quality measurement and outcome improvement from participating academic medical centers in the United States.17 Of note, Vizient also excludes readmissions for chemotherapy, radiation therapy, routine inpatient dialysis, obstetrics, and rehabilitation when identifying unplanned readmissions.
To further characterize these encounters, we obtained administrative data from these encounters, including age, observed length of stay (oLOS), procedure codes, and All Patient Refined–Diagnosis-Related Groups (APR-DRGs). We then linked these data to Vizient’s CDB/RM to obtain expected length of stay (eLOS), a patient-specific risk-adjusted metric calculated using regression models that incorporates patient factors such as age, gender, race, socioeconomic status, admission source, comorbidities, and the severity of illness in light of billed diagnoses and procedures associated with that patient’s admission with respect to the patient population.18 Because there are over 400 APR-DRGs, we grouped the APR-DRGs into 31 diagnosis categories using our previous methodology for neurological diagnostic categories, with the addition of organ system categories for nonneurological diseases and procedures.5 The modifications to the neurological categories included incorporation of ischemic stroke with tissue plasminogen activator along with other ischemic strokes in the category “intracranial hemorrhage and ischemic stroke,” expansion of bacterial and nonbacterial infections to the nervous system in general and not limiting to the central nervous system, and expansion of malignancies of the nervous system to be a general category not limited to the central nervous system. The categories for nonneurological organ system categories were selected by consensus opinion of 3 authors (S.T.L., S.A.J., and J.C.P.).
We subsequently performed a chart review of each of these readmissions to assess which readmissions were planned. Readmissions were coded as planned or unplanned by authors (S.T.L. and J.C.P.) at their respective institutions on the basis of whether the procedures or treatment performed during the readmission had been specifically stated in the discharge summary for the discharge diagnosis of the index admission. If there was uncertainty regarding readmission classification, this was discussed with the other authoring neurologists at the respective institutions (S.A.J and H.A.P.). Also a readmission was considered planned if either the readmission or an outpatient visit to coordinate readmission for the procedure or treatment was scheduled and specifically stated in the discharge summary of the index admission.
We subsequently identified which of these readmissions would be classified as planned using CMS methodology (Table 1). Per CMS, there are specific, limited types of care that are always considered planned. Otherwise, a planned readmission is a nonacute readmission for a scheduled procedure and is never an admission for an acute illness or complication of care. A readmission is considered planned if it is for a procedure or diagnosis that has been defined by CMS as always planned.4
Analysis
We calculated readmission rates, percentage of readmissions that were planned, and percentage of readmissions classified as planned by CMS. Because some neurology patients were readmitted multiple times during our study period and some of these readmissions occurred within 30 days of a prior 30-day readmission, only the first 30 day readmission was included.4,6,11 To assess which factors were associated with readmission, logistic regression models were used to examine the impact of age, eLOS, and oLOS on likelihood of readmission. We performed both bivariate and multivariate modeling to assess the effect of each of these factors on likelihood of readmission.
We considered a 2-tailed p value of less than .05 as significant. All analyses were performed using Stata 13 (StataCorp LP, College Station, Texas).
Results
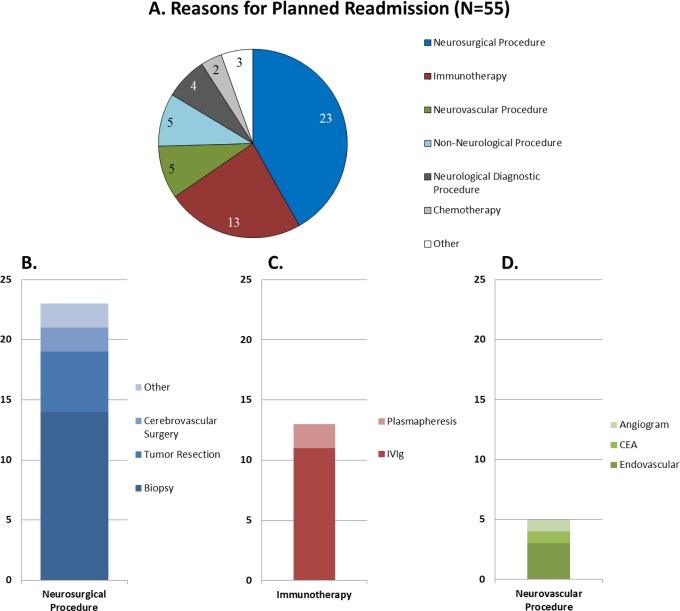
A total of 5455 admissions were identified, 353 (6.5%) of which resulted in an initial readmission within 30 days (Table 2). Fifty-five (15.6%) of the 353 readmissions were found to be planned (Figure 1). Forty-one (74.5%) of these planned readmissions occurred within 14 days of index discharge, with the mean interval duration from index discharge to readmission being 17.5 days (standard deviation [SD]: 9.4). The most common planned reasons for readmission were for a neurosurgical procedure such as craniotomy and biopsy (N = 23, 41.8%; Figure 1B), immunotherapy such as plasmapheresis or intravenous immunoglobulin infusion (N = 13, 23.6%; Figure 1C), a neurovascular procedure such as arteriogram and endovascular stenting (N = 5, 9.1%; Figure 1D), or a nonneurological procedure such as biopsy (N = 5, 9.1%). Only 8 (14.5%) of these readmissions would have been classified as planned using CMS methodology.
Table 2.
Characteristics of Index Admissions and Readmissions.a
| Primary Admission Diagnosis | Number of Index Admissions | Number of Readmissions (Readmission Rate) | Planned Readmission (Proportion) |
|---|---|---|---|
| Neurological | |||
| Seizure | 1203 | 34 (2.8%) | 3 (8.8%) |
| Intracranial hemorrhagic and ischemic stroke | 1043 | 57 (5.5%) | 4 (7.0%) |
| Headache | 342 | 11 (3.2%) | 0 (0.0%) |
| Miscellaneous disorder of the nervous system including movement disorder, sleep disorder, myopathy, and myelopathy | 328 | 34 (10.4%) | 13 (38.2%) |
| Ataxia and demyelinating disease | 323 | 33 (10.2%) | 10 (30.3%) |
| Neurodegenerative disorder | 182 | 9 (4.9%) | 2 (22.2%) |
| Intravascular procedure | 161 | 11 (6.8%) | 3 (27.3%) |
| Nontraumatic coma | 128 | 7 (5.5%) | 0 (0.0%) |
| Transient ischemic attack | 123 | 6 (4.9%) | 1 (16.7%) |
| Other nonbacterial nervous system infection | 106 | 8 (7.5%) | 0 (0.0%) |
| Peripheral nerve disorder | 98 | 16 (16.3%) | 1 (6.3%) |
| Bacterial infection of nervous system | 65 | 9 (13.8%) | 1 (11.1%) |
| Nervous system malignancy | 63 | 12 (19.0%) | 4 (33.3%) |
| Spinal cord disorder | 43 | 3 (7.0%) | 1 (33.3%) |
| Viral meningitis | 36 | 3 (8.3%) | 0 (0.0%) |
| Traumatic brain injury | 27 | 2 (7.4%) | 0 (0.0%) |
| Total neurological | 4271 | 255 (6.0%) | 43 (16.9%) |
| Nonneurological | |||
| Psychiatric or mood disorder | 179 | 6 (3.4%) | 0 (0.0%) |
| Neurosurgical procedure | 153 | 15 (9.8%) | 0 (0.0%) |
| Orthopedic, plastic surgical, and skin disorders and procedures | 149 | 12 (8.1%) | 3 (25.0%) |
| Other | 148 | 17 (11.5%) | 4 (23.5%) |
| Disorders and procedures of eyes | 122 | 7 (5.7%) | 0 (0.0%) |
| Disorder or procedure of pulmonary system | 121 | 8 (6.6%) | 0 (0.0%) |
| Infectious disease, nonneurological | 89 | 9 (10.1%) | 2 (22.2%) |
| Disorder or procedure of cardiovascular system | 83 | 6 (7.2%) | 1 (16.7%) |
| Disorder of renal system including electrolyte imbalance | 37 | 5 (13.5%) | 0 (0.0%) |
| Endocrine diagnoses and procedures | 34 | 0 (0.0%) | - |
| Cancer, not of nervous system | 29 | 9 (31.0%) | 1 (11.1%) |
| Disorder of liver and gastrointestinal tract | 24 | 3 (12.5%) | 1 (33.3%) |
| Disorder or procedure of face, ears, nose, neck, or throat | 8 | 1 (12.5%) | 0 (0.0%) |
| Hematologic/immunologic | 5 | 0 (0.0%) | - |
| Burns and trauma | 3 | 0 (0.0%) | - |
| Total nonneurological | 1184 | 98 (8.3%) | 12 (12.2%) |
| Total | 5455 | 353 (6.5%) | 55 (15.6%) |
aOnly 8 (14.5%) of 55 considered planned using Centers for Medicare and Medicaid Services (CMS) methodology. Of note, no patients in this period were admitted or readmitted with diagnosis codes for the neurological categories “arterial stenosis” and “nonhypertensive encephalopathies.”
Figure 1.
Reasons for planned readmission. A, Categories of planned readmission with (B) specific neurosurgical procedures, (C) specific immunotherapies, and (D) specific neurovascular procedures.
Turning to neurological diagnosis groups, the highest volume of readmissions was seen in patients with ischemic or hemorrhagic stroke (N = 57), whereas the highest readmission proportions were seen among patients with cancer of the nervous system (19.0%) and not of the nervous system (31.0%; Table 1). The highest proportions of planned readmissions were among patients with miscellaneous disorders of the nervous system including movement disorder, sleep disorder, myopathy, and myelopathy (38.2%), nervous system malignancy (33.3%), and spinal cord disorders (33.3%; Table 1).
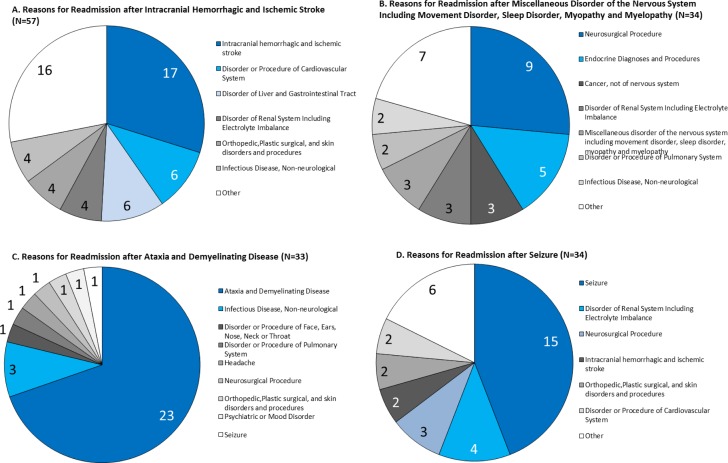
The reasons for readmission varied across index admission neurological diagnosis, as demonstrated among the diagnosis groups with highest volume of readmissions (Figure 2). For instance, a neurosurgical procedure was the leading reason for readmission among readmitted patients within the miscellaneous disorder of the nervous system diagnosis group, whereas it was the third most frequent reason for readmission among readmitted patients with seizure.
Figure 2.
Reasons for readmission vary by index admission diagnosis. A, Reasons for readmission after intracranial hemorrhage and ischemic stroke (n = 57). B, Reasons for readmission after miscellaneous disorder of the nervous system including movement disorder, sleep disorder, myopathy, and myelopathy (n = 34). C, Reasons for readmission after ataxia and demyelinating disease (n = 33). D, Reasons for readmission after seizure (n = 34).
Patient age (odds ratio [OR] = 1.01 for each 10-year increase, p < .001) and eLOS (OR = 1.03, p < .001) were associated with a greater likelihood of readmission in bivariate multivariate logistic regression models (Supplemental File 1). Observed length of stay was not associated with likelihood of readmission in either the bivariate or the multivariate models.
Discussion
In this retrospective cohort study of patients treated at 2 academic centers, 6.5% of discharged patients were readmitted to their respective hospital within 30 days. Approximately 16% of these initial 30-day readmissions were for planned procedures and treatments, the majority of which would not be captured as planned readmissions using current CMS methodology. This chart-level description of reasons for readmission complements prior work in describing rates of readmission across the neurological patient population.5
The 30-day readmission rate is considered by CMS and other organizations as a standard measure of inpatient care quality and efficiency of health-care utilization. After 30 days, factors outside a hospital provider’s control, such as patient behavior, care provided by others, and patient’s comorbidities, are felt to have a substantial impact on risk for readmission.4 It is important to note that the 6.5% initial 30-day readmission rate observed here is comparable to prior single-center studies of readmission in epilepsy and ischemic stroke, less than the 11% observed for neurologic disorders using the Vizient database, and less than the national 13.7% readmission rate for the neurology cohort and 16.0% for all qualifying Medicare patients recently observed by CMS.5,10,12,15
Important exceptions to the 30-day readmission rate are planned readmissions that occur within 30 days but reflect a scheduled part of a patient’s plan of care rather than the product of an acute complication. The designation of planned readmission has been limited by CMS to a defined list of indications.4 Potentially planned neurological and neurosurgical procedures as currently defined by CMS include laminectomy, insertion of a spinal catheter or stimulator, therapeutic operative procedures of the nervous system, operative procedures of the vessels of the head and neck, endarterectomy, and spinal fusion (Table 1).4 Here, detailed chart review of readmissions allowed for designation of initial readmissions as planned or unplanned, granularity not available using national databases.5 Among the 353 readmissions identified here, only 8 met CMS criteria, whereas an additional 45 readmissions were planned for procedures such as immunotherapy infusions, elective craniotomy, and biopsy. These additional readmissions reflect nonpreventable portions of a patient’s care plan, suggesting an opportunity for neurology-specific additions to the planned readmission definition used by CMS and others. For example, an adult patient initially admitted for evaluation of seizures who is found to have a brain mass through the course of index admission, discharged after achieving seizure control for rehabilitation and outpatient neurosurgical follow-up for biopsy planning, and then readmitted for neurosurgical biopsy, the potential resection would be categorized as an unplanned readmission using current CMS definitions. At the moment, neurologists and hospitals are potentially being penalized for such nonpreventable readmissions, which reflect well-coordinated care rather than unplanned complications of care delivered. Patient-level observations such as those provided here can inform proposed refinements to current planned readmission definitions, including additions to the list of potentially planned procedures for nonacute diagnoses (Table 3).
Table 3.
Possible Modifications to CMS Criteria for Planned Readmission.
| Suggested additions to list of potentially planned neurological and neurosurgical procedures |
| Neurosurgical incision and excision |
| Procedures of vessels of head and neck other than endarterectomy |
| Immunotherapy including plasmapheresis and intravenous immunoglobulin |
| Suggested deletions from list of acute neurological and neurosurgical discharge diagnoses |
| Epilepsy; convulsions |
| Acute cerebrovascular disease |
| Transient cerebral ischemia |
Abbreviation: CMS, Centers for Medicare and Medicaid Services.
Prior studies of readmission of patients with epilepsy or after ischemic stroke have excluded planned readmissions either per CMS criteria or if for elective procedures, with focus resting on unplanned and potentially preventable readmissions.10-12,15 In single-center studies of readmission in ischemic stroke by detailed medical record review, the number of readmissions for planned procedures ranged from to 4.2% to 41%.10,12 Because a number of 30-day readmissions for neurology patients are for elective procedures, the suggestion has been made to either ensure completion of elective procedures during the index admission and potentially increase the oLOS or defer elective procedures for greater than 30 days after discharge.10 Such practices would likely compromise care quality, with either accumulated risks of medical complications in the setting of extended hospitalization or risks of deferred care to meet a quality metric.
Here, the most common index admission diagnosis category for readmitted patients was intracranial hemorrhage and ischemic stroke, as has been observed among the Medicare neurology cohort but not the Vizient database where patients with peripheral nerve disorders were most commonly readmitted.4,5 Importantly, the reason for readmission varied by index admission diagnosis. These differences could potentially be used to guide neurology-specific quality improvement interventions at the institutional and national levels. Such directed interventions may be further refined by studying those at risk for readmission and for what reasons within a matter of days from discharge as opposed to weeks. As observed within the general medicine population, those with a longer length of stay and greater acuity of illness appear more likely to be readmitted within 7 days of index hospitalization.19
Patient-specific factors, generally captured here by the eLOS incorporating patient-specific factors, medical severity, and patient age, were associated with likelihood of readmission, whereas oLOS was not. A variety of factors have previously been associated with patient risk for readmission, from patient-specific factors11,15,20,21 to characteristics of index hospitalizations,10-12 neurological service structure,22 hospital practice8 and attributes,23 and regional differences.24 Also, increased severity of neurological disease and the presence of related comorbidities and medical complications of index hospitalization are associated with increased rates of readmission.5,11,12,20,21 As presented here, the association of patient-specific factors with readmission extends throughout the neurological inpatient population. The degree and direction of association of oLOS on likelihood for readmission have been observed to vary in different neurology patient populations, perhaps accounting for oLOS here not being associated with likelihood of readmission.10,12 It should be noted that the ORs for readmission in relation to patient age and eLOS are small, likely reflecting other factors predicting readmission not captured in our study design. Also, the number of variables collected for each admission in the combined multi-institutional data set limited the control for confounders in regression analyses of predictors for readmission.
The major limitations of this study are that it is retrospective and that it was performed at tertiary academic medical centers with associated limits of generalizability. Individual chart review performed here allowed for the confirmation of the indication for readmission and associated index admission, as well as the determination of whether readmission was planned by providers, details not readily available for review through national databases nor captured in administrative and billing data.
It is important to note that in this study, all patients 18 years of age and older were included, whereas the Medicare cohort is limited to patients 65 years of age and older. The differing readmission rates observed may potentially reflect the effect of accrued comorbidities with age in the Medicare population as opposed to the general neurology population. However, this rate is likely an underestimate for multiple additional reasons. First, this inpatient neurological services readmission rate is likely an underestimate of all readmitted patients with neurological disease discharged from the respective tertiary hospitals. Patients may have been admitted for other nonneurological reasons to other services initially, which may have been captured in previous analyses but not here.5 With dedicated cerebrovascular, epilepsy monitoring, general neurology services, and neurocritical care units, the vast majority of patients with primary neurological reasons for admission are admitted to or transferred to the inpatient services at the study centers but potentially not all patients with neurological disease. Second, readmission was determined by readmission to the discharging tertiary center. As both medical centers care for patients transferred for tertiary-level care, some patients discharged from each center may have been readmitted within 30 days to another facility, and this was not captured in this study. This also likely explains why the rate of readmission observed here is lower than other population-based studies but similar to other single-center studies.10,11,15 To address this limitation, agencies such as the Maryland Health Services Cost Review Commissions have developed algorithms to reliably match patients and admissions across multiple hospitals.25 Future studies on rates of readmission may benefit from the use of such state-wide and national readmission databases not limited to certain age groups to build on the findings provided here.
Patients could potentially have been readmitted multiple times during our study period, many of whom within 30 days of a prior 30-day readmission. Here, only the first 30-day readmission in a series was included, consistent with publicly reported disease and procedure-specific readmission measures as well as prior studies exploring reasons for readmission in neurological disease.4,6,11 Additionally, some readmissions were to other nonneurological inpatient services at the respective hospitals, including for potentially planned procedures, and subsequent readmissions within the 30-day period would be potentially attributable to care received during those readmissions rather than the care received during the index admission. In the future, it would be important to study patients with multiple 30-day readmissions to identify factors associated with multiple, frequent readmissions in this particularly at-risk group.
In terms of other limitations, some developing hospital practices may lead to apparent reductions in rates of readmission, such as utilization of emergency department observation units for the acute care of neurological patients.26 Such brief observation stays were not studied specifically, though warrant further study. Finally, the most commonly readmitted neurological diagnoses noted here differ from those observed in a recent review of admissions for neurological diagnoses using the Vizient database.5 This may be the consequence of the billing-based classifications used in the Vizient database across patients treated by neurologists and other physicians in comparison with the chart review methods of inpatients treated by neurologists employed here.
Conclusion
Many readmissions following index admission to an inpatient neurology service are not preventable, often reflecting continuation of planned care rather than reflecting poor care quality. The majority of these planned readmissions are not captured by current CMS methodologies, and here, we provide evidence to inform potential revised definitions of planned and unplanned care across the spectrum of neurological diseases. In addition, neurological patient complexity is a primary and potentially intervenable factor associated with readmission, whether by further refinements in diagnosis and treatment of neurological diseases or implementation of interventions to prevent or mitigate associated medical complications.
Supplementary Material
Footnotes
Authors’ Note: Mr. Le and Dr. Probasco participated in study conception and design, data collection, data analysis, manuscript drafting, and manuscript revision. Dr. Josephson participated in study conception and design, data collection, data analysis, and manuscript revision. Dr. Puttgen participated in study conception and design, data collection, and manuscript revision. Ms. Gibson, Dr. Graf, and Ms. Leicester participated in data collection. Dr. Guterman participated in manuscript revision.
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Josephson receives personal compensation as editor in chief of NEJM Journal Watch and in an editorial capacity for Continuum Audio; Dr. Probasco received a grant as a section editor for Oxford University Press.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr. Probasco received a grant as a section editor for Oxford University Press.
References
- 1. Readmissions Reduction Program. 2015. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed October 7, 2016.
- 2. Hospital-Wide All-Cause Unplanned Readmission Measure. 2012. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed October 7, 2016.
- 3. Josephson SA. Focusing on transitions of care A change is here. Neurol Clin Pract. 2015;6(2):183–189. doi:10.1212/CPJ. 0000000000000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Measure Updates and Specifications Report: Hospital-Wide all-Cause Unplanned Readmission Version 3.0. 2014. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed October 7, 2016.
- 5. Guterman EL, Douglas VC, Shah MP, Parsons T, Barba J, Josephson SA. National characteristics and predictors of neurologic 30-day readmissions. Neurology. 2016;86(7):669–675. doi:10.1212/WNL.0000000000002379. [DOI] [PubMed] [Google Scholar]
- 6. Bjerkreim AT, Thomassen L, Brøgger J, Waje-Andreassen U, Næss H. Causes and predictors for hospital readmission after ischemic stroke. J Stroke Cerebrovasc Dis. 2015;24(9):2095–2101. [DOI] [PubMed] [Google Scholar]
- 7. Bjerkreim AT, Thomassen L, Waje-Andreassen U, Selvik HA, Næss H. Hospital readmission after intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2016;25(1):157–162. [DOI] [PubMed] [Google Scholar]
- 8. Burke JF, Skolarus LE, Adelman EE, Reeves MJ, Brown DL. Influence of hospital-level practices on readmission after ischemic stroke. Neurology. 2014;82(24):2196–2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lahiri S, Navi BB, Mayer SA, et al. Hospital readmission rates among mechanically ventilated patients with stroke. Stroke. 2015;46(10):2969–2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nahab F, Takesaka J, Mailyan E, et al. Avoidable 30-day readmissions among patients with stroke and other cerebrovascular disease. Neurohospitalist. 2012;2(1):7–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lichtman JH, Leifheit-Limson EC, Jones SB, Wang Y, Goldstein LB. Preventable readmissions within 30 days of ischemic stroke among Medicare beneficiaries. Stroke. 2013;44(12):3429–3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shah SV, Corado C, Bergman D, et al. Impact of poststroke medical complications on 30-day readmission rate. J Stroke Cerebrovasc Dis. 2015;24(9):1969–1977. [DOI] [PubMed] [Google Scholar]
- 13. Bravata DM, Ho SY, Meehan TP, Brass LM, Concato J. Readmission and death after hospitalization for acute ischemic stroke: 5-year follow-up in the Medicare population. Stroke. 2007;38(6):1899–1904. [DOI] [PubMed] [Google Scholar]
- 14. Lichtman JH, Jones SB, Leifheit-Limson EC, Wang Y, Goldstein LB. 30-day mortality and readmission after hemorrhagic stroke among Medicare beneficiaries in Joint Commission primary stroke center-certified and noncertified hospitals. Stroke. 2011;42(12):3387–3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Caller TA, Chen JJ, Harrington JJ, Bujarski KA, Jobst BC. Predictors for readmissions after video-EEG monitoring. Neurology. 2014;83(5):450–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hirtz D, Thurman D, Gwinn-Hardy K, Mohamed M, Chaudhuri AR, Zalutsky R. How common are the “common” neurologic disorders? Neurology. 2007;68(5):326–337. [DOI] [PubMed] [Google Scholar]
- 17. Sutton JM, Hayes AJ, Wilson GC, et al. Validation of the University HealthSystem Consortium administrative data set: concordance and discordance with patient-level institutional data. J Surg Res. 2014;190(2):484–490. [DOI] [PubMed] [Google Scholar]
- 18. Meurer SJ. Mortality Measurement: Mortality Risk Adjustment Methodology for University Health System Consortium 2009. https://archive.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/mortality/Meurer.html. Accessed October 7, 2016.
- 19. Graham KL, Wilker EH, Howell MD, Davis RB, Marcantonio ER. Differences between early and late readmissions among patients: a cohort study. Ann Intern Med. 2015;162(11):741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kind AJ, Smith MA, Frytak JR, Finch MD. Bouncing back: patterns and predictors of complicated transitions 30 days after hospitalization for acute ischemic stroke. J Am Geriatr Soc. 2007;55(3):365–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lin HJ, Chang WL, Tseng MC. Readmission after stroke in a hospital-based registry: risk, etiologies, and risk factors. Neurology. 2011;76(5):438–443. [DOI] [PubMed] [Google Scholar]
- 22. Douglas VC, Scott BJ, Berg G, Freeman WD, Josephson SA. Effect of a neurohospitalist service on outcomes at an academic medical center. Neurology. 2012;79(10):988–994. [DOI] [PubMed] [Google Scholar]
- 23. Horwitz LI, Lin Z, Herrin J, et al. Association of hospital volume with readmission rates: a retrospective cross-sectional study. BMJ. 2015;350:h447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lichtman JH, Allen NB, Wang Y, Watanabe E, Jones SB, Goldstein LB. Stroke patient outcomes in US hospitals before the start of the Joint Commission primary stroke center certification program. Stroke. 2009;40(11):3574–3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Maryland Hospital Preventable Re-Admissions (MHPR). http://www.hscrc.state.md.us/init_qi_mhpr.cfm. Accessed October 7, 2016.
- 26. Venkatesh AK, Wang C, Ross JS, et al. Hospital Use of Observation Stays: Cross-sectional Study of the Impact on Readmission Rates. Med Care. 2016;54(12):1070–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.