Abstract
Accurate age of onset (AOO) measurement is vital to etiologic and preventive research. While AOO reports are known to be subject to recall error, few population-based studies have been used to investigate agreement in AOO reports over more than a decade. We examined AOO reports for depression, back/neck pain, and daily smoking, in a population-based cohort spanning 29 years. A stratified sample of participants from Zurich, Switzerland (n=591) completed a psychiatric and physical health interview 7 times between 1979, at ages 20 (males) and 21 (females), and 2008. We used one-way ANOVA to estimate intraclass correlations (ICCs) and weighted mixed models to estimate mean change over time and test for interactions with sex and clinical characteristics. Stratum-specific ICCs among those with 2+ reports were .19 and .29 for depression, .46 and .35 for back pain, and .66 and .75 for smoking. The average yearly increases in AOO report from the wave of first 12-month diagnosis or reported smoking, estimated in mixed models, were .57 years (95% confidence interval: .35, .79) for depression, .44 (95%CI: .28, .59) years for back pain, and .08 (95%CI: .03, .14) years for smoking. Initial impairment and frequency of treatment were associated with differences in average yearly change for depression. There is substantial variability in AOO reports over time and systematic increase with age. The degree of increase may differ by outcome, and for some outcomes, by participant clinical characteristics. Future studies should identify predictors of AOO report stability to ultimately benefit etiologic and preventive research.
Keywords: age of onset, agreement, consistency, recall, reliability, self-report
Accurate measurement of age of onset (AOO) is important in epidemiologic research. AOO is a key aspect of the natural history of disease, and knowledge of typical AOO may inform our understanding of course, treatment, and prevention (Kessler et al., 2007a). AOO may also indicate the degree of genetic liability of some diseases, a property that can be exploited to aid genetic discovery (Kendler et al., 2005; Lucking et al., 2000; Preisig et al., 2016; Selkoe, 2001). In addition, AOO indexes duration of exposure to a behavior or condition and can inform likely disease course, prognosis, and sequelae (Johnson and Mott, 2001). Finally, for diseases for which large-scale population-based incidence studies are cost-prohibitive, AOO reports from cross-sectional surveys may be used to estimate parameters such as incidence and lifetime risk (Kessler et al., 2007b; Stewart et al., 1989), thereby influencing assessments of disease burden and the potential public health impact of prevention (Brookmeyer et al., 1998; Kessler et al., 2009).
Accuracy and stability of AOO reports are of particular interest in psychiatric epidemiology, in which the lack of objective disease measures produces considerable reliance on self-report (Simon and Vonkorff, 1995). AOO reports are subject to recall error, and modern psychiatric surveys have implemented techniques to improve the accuracy of AOO reports (Friedenreich, 1994; Knäuper et al., 1999; Lyketsos et al., 1994). The term “forward telescoping” is used to describe the phenomenon in which events are postdated relative to the actual onset of an event (Janssen et al., 2006). It has been suggested that forward telescoping and forgetting of earlier episodes of mental disorder may explain apparent cohort effects generated by successive cross-sectional surveys (Giuffra and Risch, 1994; Patten et al., 2010) as well as discrepancies in lifetime prevalence estimates from cross-sectional vs. longitudinal studies (Angst, 1992; Moffitt et al., 2010).
The stability and change in AOO reports over periods longer than one year have been documented in several population based studies. The few studies of mental disorders have spanned 18 months to 6 years (Bromet et al., 1986; Fendrich et al., 1990; Prusoff et al., 1988; Warshaw et al., 1991). In the only community-based study, Bromet et al. reported intraclass correlations (ICCs) of .88 among women who consistently reported a single lifetime episode and .51 among women who consistently reported multiple lifetime episodes over a period of 18 months (Bromet et al., 1986). The long-term stability of AOO of alcohol, tobacco, and drug use, particularly among youth (Engels et al., 1997; Harris et al., 1994; Huerta et al., 2005; Johnson and Mott, 2001; Koenig et al., 2009; Labouvie et al., 1997; Parra et al., 2003; Shillington and Clapp, 2000; Shillington et al., 2011a; Shillington et al., 2011b; Shillington et al., 2010; Shillington et al., 2012) have been investigated in a larger number of studies. Fair to very good reliability of age of first cigarette use with mild increases in reported AOO over time has been reported (Johnson and Mott, 2001; Labouvie et al., 1997; Shillington et al., 2010). The longest of these studies covered a period of 14 years and found small increases in reports along with differences in reliability by sex (Kaestle, 2015). Finally, a small number of studies in which the long-term stability of AOO reports for physical conditions, including temporomandibular pain (Raphael and Marbach, 1997), essential tremor (Louis, 2013), and asthma (Pattaro et al., 2007) were evaluated. In the only community-based study, Pattaro et al. found a mean difference of - 0.2 years for reports of asthma AOO separated by 9 years, and that 54% reported the same AOO within one year (Pattaro et al., 2007). To our knowledge, the stability of AOO reports over more than a decade has not been previously published.
Here we investigated the stability and change over time of AOO reports in a population-based cohort followed from young adulthood to middle age. AOO of a variety of physical and mental health syndromes was asked five times over 29 years. We focused on a mental health condition, depression, a physical syndrome, back or neck pain, and a health behavior, smoking. We also examined whether a variety of clinical characteristics influenced average change in AOO reports over time. Based on prior studies of diagnosis recall and reliability of AOO, these included both current and cumulative indicators of diagnostic status, recency, duration, impairment, distress, treatment, and comorbidity (Aneshensel et al., 1987; Bromet et al., 1986; Fendrich et al., 1990; Foley et al., 1998; Raphael and Marbach, 1997; Thompson et al., 2004).
METHODS
Sample
The Zurich Cohort Study is a population-based cohort study of young adults from the canton of Zurich, Switzerland (Angst et al., 1984). Sampling occurred in two stages. In 1978, 2201 males and 2346 females were screened using a syndrome inventory and the Symptom Checklist-90 (Derogatis, 1977). Males were screened during military enrollment (0.3% refusal rate), which is compulsory for all males when they reach age 19. Females were 20 years old and were randomly sampled from electoral registers (50% of 20 year-old females) and contacted by mail (75% response rate). After screening, participants were divided into high (>=85th percentile) and low (<85th percentile) scorers based on the Global Severity Index. A stratified subsample of 591 participants (292 males and 299 females), consisting of two-thirds high scorers and one-third low scorers, was selected for follow-up. Seven waves of interviews were conducted: in 1979 (n=591; age 20/21), 1981 (n=456; age 22/23), 1986 (n=457; age 27/28), 1988 (n=424; age 29/30), 1993 (n=407; age 34/35), 1999 (n=367; age 40/41), and 2008 (n=335; age 49/50). Two hundred fifty-two participants completed all 7 interviews. The initial distribution of high and low scorers did not change over follow-up, but dropouts were more common among extreme scorers and women participated more than men (Eich et al., 2003). All participants provided informed consent. The study was approved by the institutional review board of the University of Zurich.
Measures
Interviews were conducted using the “Structured Psychopathological Interview and Rating of the Social Consequences of Psychological Disturbances for Epidemiology,” a semi-structured interview that used a bottom-up approach to assess socio-demographics, 14 somatic and 13 psychiatric syndromes, psychopathology, substance use, medication, health services use, impairment, social activity, and more (Angst et al., 1984). Its reliability and validity have been reported (Angst et al., 2005). Interviews were conducted by trained psychologists or psychiatrists and diagnoses were based on the Diagnostic and Statistical Manual of Mental Disorders Third Edition (1979-1986)(American Psychiatric Association, 1980), Third Edition – Revised, (1988 and 1993)(American Psychiatric Association, 1987), and Fourth Edition (1999 and 2008)(American Psychiatric Association, 1994). Diagnoses focused on the past year and exclusion criteria were not applied.
Here we focus on 3 diagnostic modules: depression, back pain, and smoking. Each diagnostic module began with one or more stem questions that assessed the past-year presence of core features. If core symptoms were endorsed, the rest of the diagnostic section was administered, including questions about symptoms, duration, distress, help-seeking, and impairment. These were used to generate past-year diagnoses and obtain information on clinical characteristics (described below). Depression was defined as a Major Depressive Episode according to Diagnostic and Statistical Manual criteria. Back pain included pain in the neck, back, or lower back. A back pain syndrome was defined as extreme duration (>30 days), distress (rating >60 on a 100-point analog scale), or both in the past year. Smoking was defined as daily smoking.
Age of onset assessment
Each mental and physical diagnostic module was followed by a “history” section. This section was administered to all participants, regardless of their responses during the diagnostic module, and referred to time periods prior to the past year. Participants were first asked whether they had experienced the problem either ever before (in 1979-1993), or since the last interview (in 1999 and 2008). “The problem” referred to the phenomena discussed during the diagnostic section (at a minimum, the stem question). Those who responded positively were asked how old they were the first time they experienced the problem. AOO was not asked if the participant denied having the problem before the past year. AOO of depression and back pain was asked in 1979, 1986, 1993, 1999, and 2008. At most study waves, questions about smoking were contained in one module. AOO of daily smoking was asked in 1986, 1988, 1993, 1999, and 2008. In 1986 and 1988 daily smoking AOO was asked only of those who reported smoking in the past year; in the subsequent interviews it was asked of those who reported ever smoking daily. Because of these changes in interview structure across study waves, systematic comparison of agreement in history reports across the study period is not possible. However, for interested readers frequencies are provided in eTable 1 in the supplement.
Clinical characteristics
Time-varying clinical characteristics included: stem question(s) endorsement for depression or back pain, depression or back pain diagnosis, time (in years) since the most recent 12-month diagnosis or current smoking, presence and number of any (other) psychiatric disorders, number of (other) physical stem questions endorsed, presence and number of (other) physical syndromes present, subjective distress rating (0-100 scale), professional help seeking, and an work or social impairment. Time-invariant clinical characteristics included the percentage of waves at which a depression diagnosis or back pain syndrome was present; the number of different mental disorders and different physical syndromes diagnosed across follow-up, scaled by the number of waves of participation; the percentage of waves with distress ratings >50; the percentage of waves at which treatment was reported and at which impairment was reported; and the distress rating, impairment report, and treatment report of the first wave at which a past-year diagnosis was made. Details are given in the supplement.
Analysis
Participants were divided into “first diagnosis” groups according to the first wave at which a 12-month disorder (Major Depressive Episode or back pain syndrome) was present, or the wave at which they first reported current or prior daily smoking. Weighted mean AOO reports were calculated at each wave for each “first diagnosis” group. Weighted Generalized Estimating Equations with unstructured residuals and categorical time were used to test for interactions between time and “first diagnosis” group as well as between time and a time-varying indicator of current/prior disorder presence. Unweighted ICCs measuring absolute agreement were estimated using one-way weighted analysis of variance with the l1way command in Stata, restricting to those with 2 or more reports. These were estimated with and without restriction to reports given at or after a “first diagnosis” and are presented separately for the two sample strata (high and low scorers on the GSI).
Average change in AOO reports over time was estimated using weighted mixed models. For depression and back pain, these analyses were restricted to those with an MDE or back pain syndrome diagnosis. Time was counted from the wave of “first diagnosis” and AOO reports before this wave were ignored. All reports given at or after a “first diagnosis” were included and “first diagnosis” group was controlled for. Those with “first diagnosis” in 2008 were not included. Time was modeled continuously and random effects were included for each person and for time. An exponential within-person residual structure was included, as it improved model fit. Clinical predictors of change over time were assessed by testing for a time*predictor interaction. A 5% false discovery rate correction was used for the interaction tests within each outcome. Analyses were conducted using Stata Version 13 (StataCorp., College Station, TX).
RESULTS
Agreement
Table 1 displays estimated ICCs for AOO reports. Overall ICCs for depression and back pain were higher when a current/prior diagnosis was present. Overall ICCs were lower for depression (low scorers: .19; high scorers: .29) and back pain (low scorers: .46; high scorers: .35) than for smoking (low scorers: .66; high scorers: .75). In general, ICCs indicated that especially for depression and back pain, a large proportion of the variability in AOO reports exists within, as opposed to between, individuals.
Table 1.
Unweighted ICCs for Reported Age of Onset of Depression, Back/Neck Pain, and Smoking, by Sampling Stratum and Sex, Zurich Cohort Study, 1979-2008
| All Reports | Current or Prior Dx or Smoking Present | |||||||
|---|---|---|---|---|---|---|---|---|
| Low Scorers | High Scorers | Low Scorers | High Scorers | |||||
| N | ICC | N | ICC | N | ICC | N | ICC | |
| Depression | ||||||||
| Overall | 91 | .00 | 258 | .09 | 27 | .19 | 100 | .29 |
| Males | 39 | .00 | 111 | .09 | 8 | .00 | 28 | .40 |
| Females | 52 | .12 | 147 | .08 | 19 | .28 | 72 | .27 |
| Back Pain | ||||||||
| Overall | 110 | .16 | 249 | .12 | 29 | .46 | 78 | .35 |
| Males | 47 | .19 | 108 | .10 | 10 | .54 | 25 | .59 |
| Females | 63 | .14 | 141 | .14 | 19 | .40 | 53 | .24 |
| Smoking | ||||||||
| Overall | 62 | .66 | 164 | .75 | ||||
| Males | 33 | .56 | 81 | .75 | ||||
| Females | 29 | .68 | 83 | .74 | ||||
Mean reports over time
Table 2 displays the number and weighted mean of AOO reports at each wave, overall and according to “first diagnosis” group (the first wave at which a 12-month disorder or current/prior smoking was reported). Groups 1981 and 1988 are combined with 1986 and 1993, respectively, because AOO was not asked in 1981 or 1988. Gray shading indicates reports for which a past-year diagnosis (or reported current/prior smoking) was present at a current or prior wave. Unshaded areas reflect reports given at waves when the participant endorsed having the problem before, but a study diagnosis had not yet occurred. For example, if a participant endorsed prior experience of core features of depression at every wave, but did not meet criteria for a past-year MDE diagnosis until 1999, AOO reports given from 1979-1993 would contribute to the unshaded areas of Table 1 and reports given in 1999 and 2008 would contribute to the shaded areas.
Table2.
Weighted Mean Age of Onset Reports by Wave of Follow-up, According to the Wave of First 12-Month Diagnosis or Reported Smoking, Zurich Cohort Study, 1979-2008
| Wave of follow-up | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Wave of 1st 12m dx or reported smoking | 1979 | 1986 | 1993 | 1999 | 2008 | |||||
| N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | |
| Depression | ||||||||||
| 1979 | 33 | 7.35 (2.01) | 32 | 15.61 (0.80) | 23 | 20.61 (2.28) | 16 | 16.68 (1.19) | 21 | 22.88 (4.05) |
| 1981, 1986 | 47 | 7.05 (0.65) | 47 | 17.25 (1.01) | 37 | 19.12 (1.92) | 28 | 18.38 (1.97) | 39 | 28.34 (3.30) |
| 1988, 1993 | 37 | 7.38 (0.74) | 39 | 19.50 (0.96) | 42 | 17.63 (2.25) | 29 | 25.25 (2.37) | 32 | 29.48 (3.70) |
| 1999 | 16 | 8.37 (0.81) | 9 | 19.26 (2.23) | 12 | 18.24 (1.67) | 16 | 23.76 (3.75) | 16 | 28.85 (4.02) |
| 2008 | 6 | 4.63 (0.74) | 7 | 15.03 (0.55) | 6 | 27.50 (3.18) | 8 | 26.16 (2.75) | 12 | 41.99 (4.05) |
| Never | 212 | 6.19 (0.39) | 140 | 18.15 (0.65) | 121 | 19.82 (0.95) | 89 | 22.79 (1.48) | 102 | 34.45 (1.76) |
| Overall Combined | 351 | 6.53 (0.30) | 274 | 17.94 (0.46) | 241 | 20.81 (0.78) | 186 | 23.73 (1.03) | 222 | 31.65 (1.33) |
| Neck or Back Pain | ||||||||||
| 1979 | 10 | 5.53 (1.34) | 10 | 20.16 (0.78) | 10 | 17.23 (1.37) | 8 | 18.50 (1.71) | 10 | 25.53 (4.86) |
| 1981, 1986 | 27 | 5.47 (0.72) | 34 | 17.91 (1.30) | 30 | 20.74 (2.38) | 22 | 18.42 (2.30) | 25 | 27.01 (3.45) |
| 1988, 1993 | 36 | 6.86 (0.94) | 37 | 16.67 (1.24) | 43 | 21.72 (1.81) | 37 | 22.59 (2.06) | 42 | 28.91 (2.31) |
| 1999 | 22 | 6.33 (0.98) | 19 | 17.07 (1.03) | 19 | 21.90 (2.57) | 24 | 23.68 (2.69) | 22 | 30.53 (2.73) |
| 2008 | 13 | 6.42 (1.84) | 18 | 18.77 (1.74) | 18 | 23.08 (1.08) | 20 | 23.59 (2.12) | 24 | 32.70 (4.64) |
| Never | 176 | 5.99 (0.37) | 171 | 17.41 (0.65) | 160 | 22.07 (0.76) | 117 | 24.31 (1.13) | 155 | 31.92 (1.42) |
| Overall Combined | 284 | 5.89 (0.30) | 289 | 18.18 (0.48) | 280 | 22.86 (0.68) | 228 | 25.26 (0.83) | 278 | 30.09 (1.05) |
| Smoking | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1986 | 1988 | 1993 | 1999 | 2008 | ||||||
| N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | |
| 1986 | 174 | 17.04 (0.33) | 128 | 17.38 (0.30) | 140 | 18.13 (0.42) | 123 | 17.63 (0.45) | 108 | 19.61 (0.75) |
| 1988 | 35 | 19.67 (0.73) | 28 | 18.49 (0.75) | 19 | 18.36 (0.61) | 17 | 19.39 (0.37) | ||
| 1993 | 77 | 17.50 (0.46) | 60 | 17.30 (0.56) | 54 | 20.48 (1.74) | ||||
| 1999 | 17 | 18.56 (1.10) | 9 | 17.97 (0.93) | ||||||
| 2008 | 6 | 32.07 (4.54) | ||||||||
| Overall Combined | 174 | 17.04 (0.33) | 163 | 17.81 (0.30) | 245 | 17.97 (0.31) | 219 | 17.69 (0.32) | 194 | 20.40 (0.74) |
Note: Shaded areas indicate reports for which a 12-month diagnosis, or reported current or prior smoking, was present at a current or prior wave. N is the total number of age of onset reports given at each wave for each group.
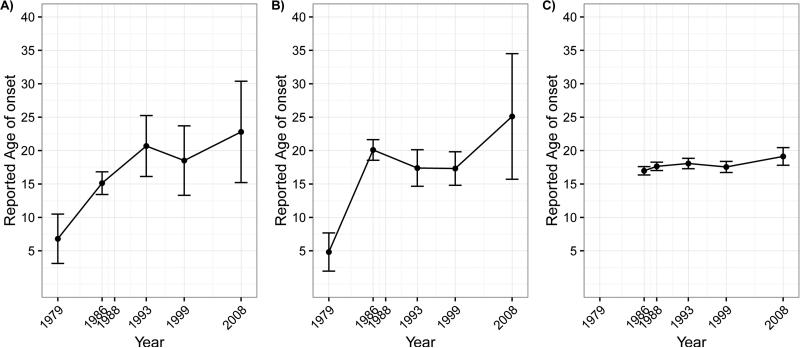
Mean reports for depression and back pain AOO over time did not differ according to the presence of a current or prior diagnosis (depression: , p=.38; back pain: , p=.34). Mean reports over time differed significantly by “first diagnosis” group for all 3 outcomes (depression: , p<.001; back pain: , p=.001; smoking: , p=.019). Mean reports for depression and back pain generally increased with time, especially from 1979 to 1986 and from 1999 to 2008. Smoking AOO reports stayed fairly constant across time. Depression and back pain reports also displayed more variability within waves compared to smoking. Means for the earliest “first diagnosis” groups are displayed in Figure 1, and those for all “first diagnosis” groups are displayed in eFigure 1 (supplementary material).
Figure 1.
Weighted Predicted Mean Age of Onset Reports by Wave of Follow-up for Depression (A), Back Pain (B), and Smoking (C), Among Those with Past-Year Disorder in 1979 or Reported Daily Smoking in 1986, Zurich Cohort Study, 1979-2008
Table 3 displays the average absolute value of individual differences in AOO reports from the initial report across follow-up. Differences tended to increase with time and appeared substantially smaller for smoking than for depression and back pain.
Table 3.
Average absolute value of individual differences between current and initial age of onset reports across follow-up
| Wave of follow-up | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year of initial AOO report | 1979 | 1986 | 1993 | 1999 | 2008 | |||||
| N | Mean | N | Mean | N | Mean | N | Mean | N | Mean | |
| Depression | ||||||||||
| 1979 | 351 | 0.00 | 179 | 10.83 | 157 | 13.81 | 119 | 15.53 | 140 | 23.68 |
| 1986 | 95 | 0.00 | 51 | 5.65 | 38 | 7.03 | 46 | 16.58 | ||
| 1993 | 33 | 0.00 | 13 | 7.29 | 14 | 18.95 | ||||
| 1999 | 16 | 0.00 | 9 | 12.40 | ||||||
| 2008 | 13 | 0.00 | ||||||||
| Neck or Back Pain | ||||||||||
| 1979 | 284 | 0.00 | 168 | 10.81 | 159 | 13.91 | 131 | 15.28 | 152 | 22.62 |
| 1986 | 121 | 0.00 | 70 | 5.56 | 57 | 5.40 | 62 | 10.15 | ||
| 1993 | 51 | 0.00 | 23 | 5.35 | 30 | 8.31 | ||||
| 1999 | 17 | 0.00 | 11 | 7.12 | ||||||
| 2008 | 23 | 0.00 | ||||||||
| Smoking | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1986 | 1988 | 1993 | 1999 | 2008 | ||||||
| N | Mean | N | Mean | N | Mean | N | Mean | N | Mean | |
| 1986 | 184 | 0.00 | 131 | 1.19 | 144 | 1.59 | 126 | 1.46 | 112 | 2.81 |
| 1988 | 32 | 0.00 | 25 | 1.23 | 18 | 0.88 | 15 | 1.06 | ||
| 1993 | 76 | 0.00 | 59 | 1.37 | 53 | 3.03 | ||||
| 1999 | 16 | 0.00 | 8 | 0.58 | ||||||
| 2008 | 6 | 0.00 | ||||||||
Note: N's are unweighted counts of observations; means are weighted.
Average change over time
We next estimated the average yearly change in AOO reports after a 12-month diagnosis or smoking was present. Those who did not have a diagnosis at any study wave are not included. In these models, time “starts” at the first 12-month diagnosis or reported smoking, and “first diagnosis” group is adjusted for. Average yearly changes were .57 years (95% confidence interval (CI): .35, .79) for depression, .44 years (95%CI: .28, .59) for back pain, and .08 years (95%CI: .03, .14) for smoking. Average change over time did not differ by sex for any outcome. It also did not differ by “first diagnosis” group for depression or back pain (not shown). For smoking, average change over time differed overall by “first diagnosis” group ( , p=.012) and was less specifically for those with “first diagnosis” in 1988 (b=−0.107; 95%CI: -.182, -.033).
Clinical predictors of average change over time
Finally, we assessed whether the average change in AOO reports over time differed by clinical characteristics (Table 4). For depression, the percentage of waves with treatment reports over follow-up was inversely associated with change in reports over time (b=−.012, 95%CI: -.019, -.005). The presence of impairment at the first wave at which a past-year diagnosis was present was associated with greater change in reports over time (b=0.478, 95%CI: 0.158, 0.797). These two associations remained significant after false discovery rate correction.
Table 4.
Tests for Interaction between Average Change in AOO Reports Over Time and Clinical Characteristics, Zurich Cohort Study, 1979-2008
| Depression (Average change: .57)a | Back / Neck Pain (Average change: .44)a | Smoking (Average change: .08)a | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Clinical characteristic | χ2 | P-value | Estimate | χ2 | P-value | Estimate | χ2 | P-value | Estimate |
| Time-varying | |||||||||
| Stem question endorsed | 0.20 | .651 | −0.094 | 0.02 | .878 | −0.033 | |||
| Past-year disorder presence | 0.37 | .544 | 0.129 | 0.52 | .471 | −0.141 | |||
| Past-year disorder / smoking recency | 0.10 | .749 | −0.004 | 0.12 | .732 | 0.005 | 0.48 | .490 | 0.003 |
| (Other) MDs present | 1.56 | .212 | −0.220 | 1.61 | .205 | 0.177 | 1.38 | .241 | −0.049 |
| # (Other) MDs present | 0.23 | .634 | −0.028 | 3.36 | .067 | 0.103 | 0.55 | .457 | −0.013 |
| # Physical complaints | 2.71 | .100 | −0.083 | 1.17 | .280 | −0.053 | 2.37 | .124 | 0.014 |
| (Other) phys. syndromes present | 0.78 | .376 | 0.634 | 1.65 | .199 | 0.233 | 0.37 | .543 | 0.024 |
| # (Other) phys. disorders present | 0.00 | .983 | 0.002 | 0.31 | .579 | 0.064 | 0.01 | .941 | −0.002 |
| Distress rating | 2.95 | .086 | −0.004 | 0.33 | .566 | −0.001 | 0.03 | .864 | 0.000 |
| Impairment reported | 0.52 | .472 | −0.146 | 0.07 | .786 | 0.043 | 2.49 | .115 | −0.142 |
| Treatment reported | 2.66 | .103 | −0.332 | 0.07 | .794 | 0.056 | 3.53 | .060 | −0.144 |
| Smoking amount | 0.01 | .909 | −0.001 | ||||||
| Time-invariant | |||||||||
| Waves with diagnosis or smoking, % | 2.40 | .122 | −0.008 | 8.73 | .003 | −0.009 | 0.26 | .607 | −0.001 |
| Total # mental disorders, scaled | 3.22 | .073 | −0.390 | 1.60 | .205 | 0.255 | 0.90 | .343 | −0.060 |
| Total # physical syndromes, scaled | 1.14 | .285 | 0.529 | 0.47 | .493 | 0.243 | 0.96 | .327 | −0.060 |
| “First episode” distress | 0.47 | .492 | −0.003 | 0.19 | .664 | .002 | 1.66 | .197 | −.001 |
| “First episode” impairment | 8.58 | .003* | 0.478 | 0.02 | .893 | .024 | 0.70 | .401 | .151 |
| “First episode” treatment | 0.59 | .443 | −0.146 | 5.23 | .022 | .325 | 4.61 | .032 | −.097 |
| Waves with distress ratings >50, % | 0.15 | .695 | −0.002 | 0.04 | .841 | −0.001 | 5.64 | .018 | −0.004 |
| Waves with impairment reported, % | 0.83 | .364 | −0.003 | 5.14 | .023 | −0.006 | 0.89 | .345 | 0.004 |
| Waves with treatment reported, % | 10.82 | .001* | −0.012 | 0.34 | .558 | 0.002 | 2.46 | .117 | −0.002 |
| Tobacco use course (2df) | 0.08 | .963 | |||||||
Average change in AOO reports per year, starting from the first study wave at which a 12-month diagnosis was present or current/past smoking was reported Note: χ2 statistics have 1 degree of freedom unless otherwise noted. Asterisks denote significant tests maintaining a false discovery rate of 5%.
For back pain, the percentage of waves with syndrome diagnoses and the percentage of waves with impairment reported were each inversely associated with change in AOO reports over time (b=−.009, 95%CI: -.016, -.003, and b=−.006, 95%CI: -.011, -.001, respectively). The presence of treatment at the first wave at which syndrome was present was associated with greater change in AOO reports over time (b=.325, 95%CI: .046, .603). For smoking, the percentage of waves with distress ratings >50 was inversely associated with average change in AOO reports over time (b= −0.004; 95%CI: −0.007, −0.001). The presence of treatment at the first wave at which current or prior smoking was reported was also inversely associated with change in AOO reports over time (b=−.097, 95%CI: −.186, −.008). None of the associations for back pain or smoking withstood false discovery rate correction.
DISCUSSION
In a population-based cohort interviewed 7 times over 29 years, we found low levels of agreement and increases with time of AOO reports of depression, back pain, and, to a lesser degree, daily smoking. Mean AOO reports for depression and back pain increased substantially as the cohort aged, while those for smoking increased only slightly. ICCs for depression and back pain calculated among reports during or after a wave at which a diagnosis was present were poor to moderate, ranging from .00 to .59. Those for smoking were slightly higher. The average change in AOO reports over time did not differ by sex, consistent with some (Louis, 2013; Pattaro et al., 2007; Prusoff et al., 1988; Shillington et al., 2010), but not all (Barkow et al., 2002; Farrer et al., 1989; Johnson and Mott, 2001), prior studies. Average change was influenced by indicators of impairment and treatment.
Although we did not have information on actual age of onset in this study, the fact that birth year is constant (within sex) in this cohort means that the positive average slopes we found over time are consistent with a phenomenon of forward telescoping of AOO reports that increases with age. AOO reports for depression and back pain increased on average by roughly one-half year per year of chronological time. This is similar to the mean one-year difference of 0.7 years among 18-19 year-olds in the Epidemiologic Catchment Area study, who were 4 years younger than the Zurich cohort participants (Farrer et al., 1989). Our estimate of yearly change is somewhat greater than those of previous reports derived from clinical samples (Fendrich et al., 1990; Prusoff et al., 1988; Warshaw et al., 1991); lower reliability of mental disorders in epidemiologic vs. clinical samples been noted previously with respect to episode recall (Foley et al., 1998). Our ICCs of .19 to .29 for depression are lower than all four prior long-term studies (Bromet et al., 1986; Fendrich et al., 1990; Prusoff et al., 1988; Warshaw et al., 1991), which could be due to the extended follow-up. While we located only one short-term study of the stability of back pain AOO (Bieringsorensen and Hilden, 1984), long-term studies of physical syndromes have yielded similar or smaller mean differences and higher ICCs (Louis, 2013; Pattaro et al., 2007; Raphael and Marbach, 1997).
We found substantially less change over time for AOO reports of daily smoking. Smoking was normative in this cohort, and most participants began smoking in young adulthood. Small amounts of forward telescoping of cigarette use AOO have been reported in an 11-year study of college students (Parra et al., 2003) and in the National Longitudinal Survey of Youth (Shillington et al., 2010). The ICCs and absolute mean differences we report here are similar to those reported for daily cigarette use in the National Longitudinal Survey of Youth (Johnson and Mott, 2001).
Few of the clinical characteristics were associated with average change in AOO reports over time, and even fewer were associated after maintaining a 5% false discovery rate. Associated characteristics were related to impairment, treatment, persistence, and distress. Some, but not all, of these factors were inversely related to change over time, implying that those with more severe disorder may exhibit more stability of recall. These inverse associations are generally consistent with prior literature on mental disorder episode recall (Aneshensel et al., 1987; Bromet et al., 1986; Fendrich et al., 1990; Foley et al., 1998; Kendler et al., 1993; Rice et al., 1992; Wells and Horwood, 2004). However, Bromet et al. reported higher ICCs among those with only one depressive episode compared to multiple episodes (Bromet et al., 1986). There were inverse associations for back pain in accordance with previous studies of facial pain (Raphael and Marbach, 1997) and essential tremor (Louis, 2013). Few studies of smoking AOO reliability have assessed clinical predictors of change over time (Shillington et al., 2012). However, the negative associations we found with treatment and distress are broadly consistent with the literature on mental and physical conditions (Simon and Vonkorff, 1995).
While we report single slope estimates of average change over time, the actual pattern of change for depression and back pain was non-linear (see Table 1 and Figure 1). There was a substantial increase in mean AOO reports for depression and back pain between 1979 and 1986, even among those with past-year diagnoses in 1979. This pattern could indicate that many childhood episodes reported by participants at age 20/21 are forgotten by age 27/28, an interpretation that is supported by the frequencies presented in eTable 1 in the supplement. A similar finding was reported in the Christchurch Health and Development Study: at age 25, only 44% recalled depressive episodes that were present at ages 14-21 (Wells and Horwood, 2004). As others have posited, forgetting of episodes occurring early in life may explain why longitudinal studies of mental disorders that start at a young age tend to yield higher estimates of risk than are implied by cross-sectional studies of the adult population (Angst, 1992; Copeland et al., 2011; Moffitt et al., 2010). On the other hand, this pattern may reflect differences in valuation of symptoms by age, rather than forgetting per se.
Our results suggest that AOO measurements for depression and back pain that are based on simple recall may be misclassified, while those for smoking AOO may be relatively accurate. Because modern surveys include techniques to improve recall (Knäuper et al., 1999; Lyketsos et al., 1994), the degree of misclassification in recent surveys may be less than is implied by our data. Nevertheless, this misclassification has implications for epidemiologic research. As mentioned above, the average AOO of some mental disorders may be earlier than surveys of the adult population suggest. This highlights the importance of etiologic and preventive research focusing on early life and development. Second, studies of comorbidity that rely on establishing order of onset of different types of disorders (e.g., Kessler et al., 2011) may be affected by differential rates of telescoping by disorder type. Third, depending on sample ascertainment and method of AOO measurement, there may be a degree of misclassification in population-based genetics studies that focus on early-onset cases to enrich the genetic load of the sample (Power et al., 2012; Power et al., 2016; Priebe et al., 2012). A greater proportion of cases from community samples may have early onset disorder than would be estimated based on self-reported AOO alone.
This study has a number of strengths and limitations. The Zurich Cohort Study is the longest prospective study of a population-based sample of adults to assess a variety of mental disorders, physical conditions, and health behaviors. AOO was asked at 5 study waves spanning 29 years regardless of diagnostic status. All males and all females were born in the same year, eliminating cohort effects. The interview contained information on a number of relevant clinical characteristics that could be evaluated as potential modifiers. However, the sample size was relatively small, and there was attrition over the long follow-up. The sample was drawn from a particular geographic area and may not generalize to other settings. Analyses restricted to those with a 12-month diagnosis to maximize the changes that future AOO reports referred to disorder rather than to subthreshold symptoms. However, violation of this would likely bias our positive slopes over time towards the null. Other processes aside from forgetting, such as changes in valuation of symptoms with age and secular changes in attitudes toward mental disorders, may have impacted our estimates. Analysis of AOO stability was limited to those who consistently reported having experienced the problem before. To maximize sample size we considered each outcome separately. However, none of estimates of average change over time differed according to whether AOO reports were also given for another outcome (not shown). Finally, as mentioned above, the AOO questions in this study did not include techniques used in more recent surveys to increase recall accuracy.
Aspects of disorder measurement in epidemiology remain a challenge, particularly for psychiatric disorders, which generally lack biologic diagnostic markers. Our findings are consistent with substantial forward-telescoping of AOO reports of depression and back pain in a population-based cohort of adults over 29 years. AOO measurement may be improved both by efforts to elicit more accurate responses (Knäuper et al., 1999; Lyketsos et al., 1994), and by techniques that correct or calibrate reports after they are given (Klungsoyr et al., 2013; Roy and Stewart, 2010; Stewart et al., 1989). Unfortunately, we found few predictors of change over time that could be used to calibrate reports. Future studies should attempt to identify determinants of long-term AOO report reliability, which can be implemented both in clinical settings and community-based studies to improve the accuracy of AOO reporting.
Supplementary Material
Acknowledgments
This study was supported by the Intramural Research Program of the National Institute of Mental Health (ZIAMH002807) and grant numbers 3200-050881.97/1 and 32-50881.97 of the Swiss National Science Foundation. The sponsors had no role in study design; in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
This work was presented at the 106th annual meeting of the American Psychopathological Association on March 3, 2016 and the Epidemiology Congress of the Americas on June 21, 2016.
The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the US government.
Conflicts of interest: none.
Diana Paksarian designed the study, analyzed and interpreted the data, and drafted the manuscript. Lihong Cui analyzed and interpreted the data and revised the manuscript. Jules Angst conceived of the study, acquired the data, and revised the manuscript. Vladeta Ajdacic-Gross analyzed and interpreted the data and revised the manuscript. Wulf Rössler acquired the data and revised the manuscript. Kathleen Merikangas conceived of the study and revised the manuscript. All authors approved the final version of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Third edition (DSM-III) American Psychiatric Press; Washington, DC: 1980. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Third edition, revised (DSM-III-R) American Psychiatric Press; Washington, DC: 1987. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) American Psychiatric Press; Washington, DC: 1994. [Google Scholar]
- Aneshensel CS, Estrada AL, Hansell MJ, Clark VA. Social Psychological-Aspects of Reporting Behavior - Lifetime Depressive Episode Reports. J Health Soc Behav. 1987;28(3):232–246. [PubMed] [Google Scholar]
- Angst J. Epidemiology of Depression. Psychopharmacology. 1992;106:S71–S74. doi: 10.1007/BF02246240. [DOI] [PubMed] [Google Scholar]
- Angst J, Doblermikola A, Binder J. The Zurich Study - a Prospective Epidemiological-Study of Depressive, Neurotic and Psychosomatic Syndromes .1. Problem, Methodology. Eur Arch Psy Clin N. 1984;234(1):13–20. doi: 10.1007/BF00432878. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Neuenschwander M, Ajdacic-Gross V, Eich D, Rossler W, Merikangas KR. Prevalence of mental disorders in the Zurich Cohort Study: a twenty year prospective study. Epidemiologia E Psichiatria Sociale. 2005;14(2):68–76. doi: 10.1017/s1121189x00006278. [DOI] [PubMed] [Google Scholar]
- Barkow K, Heun R, Ustun TB, Gansicke M, Wittchen HU, Maier W. Test-retest reliability of self-reported age at onset of selected psychiatric diagnoses in general health care. Acta Psychiat Scand. 2002;106(2):117–125. doi: 10.1034/j.1600-0447.2002.02272.x. [DOI] [PubMed] [Google Scholar]
- Bieringsorensen F, Hilden J. Reproducibility of the History of Low-Back Trouble. Spine. 1984;9(3):280–286. doi: 10.1097/00007632-198404000-00010. [DOI] [PubMed] [Google Scholar]
- Bromet EJ, Dunn LO, Connell MM, Dew MA, Schulberg HC. Long-Term Reliability of Diagnosing Lifetime Major Depression in a Community Sample. Arch Gen Psychiat. 1986;43(5):435–440. doi: 10.1001/archpsyc.1986.01800050033004. [DOI] [PubMed] [Google Scholar]
- Brookmeyer R, Gray S, Kawas C. Projections of Alzheimer's disease in the United States and the public health impact of delaying disease onset. Am J Public Health. 1998;88(9):1337–1342. doi: 10.2105/ajph.88.9.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative Prevalence of Psychiatric Disorders by Young Adulthood: A Prospective Cohort Analysis From the Great Smoky Mountains Study. J Am Acad Child Psy. 2011;50(3):252–261. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90: Administration, Scoring, and Procedures Manual - I for the Revised Version and Other Instruments of the Psychopathology Rating Scale Series. Johns Hopkins University; Baltimore: 1977. [Google Scholar]
- Eich D, Ajdacic-Gross V, Condrau M, Huber H, Gamma A, Angst J, Rossler W. The Zurich Study: participation patterns and Symptom Checklist 90-R scores in six interviews, 1979-99. Acta Psychiat Scand. 2003;108:11–14. doi: 10.1034/j.1600-0447.108.s418.3.x. [DOI] [PubMed] [Google Scholar]
- Engels RCME, Knibbe RA, Drop MJ. Inconsistencies in adolescents' self-reports of initiation of alcohol and tobacco use. Addict Behav. 1997;22(5):613–623. doi: 10.1016/s0306-4603(96)00067-6. [DOI] [PubMed] [Google Scholar]
- Farrer LA, Florio LP, Bruce ML, Leaf PJ, Weissman MM. Reliability of Self-Reported Age at Onset of Major Depression. J Psychiat Res. 1989;23(1):35–47. doi: 10.1016/0022-3956(89)90015-0. [DOI] [PubMed] [Google Scholar]
- Fendrich M, Weissman MM, Warner V, Mufson L. 2-Year Recall of Lifetime Diagnoses in Offspring at High and Low-Risk for Major Depression - the Stability of Offspring Reports. Arch Gen Psychiat. 1990;47(12):1121–1127. doi: 10.1001/archpsyc.1990.01810240041008. [DOI] [PubMed] [Google Scholar]
- Foley DL, Neale MC, Kendler KS. Reliability of a lifetime history of major depression: implications for heritability and co-morbidity. Psychol Med. 1998;28(4):857–870. doi: 10.1017/s0033291798006977. [DOI] [PubMed] [Google Scholar]
- Friedenreich CM. Improving Long-Term Recall in Epidemiologic Studies. Epidemiology. 1994;5(1):1–4. [PubMed] [Google Scholar]
- Giuffra LA, Risch N. Diminished Recall and the Cohort Effect of Major Depression - a Simulation Study. Psychol Med. 1994;24(2):375–383. doi: 10.1017/s0033291700027355. [DOI] [PubMed] [Google Scholar]
- Harris TR, Wilsnack RW, Klassen AD. Reliability of Retrospective Self-Reports of Alcohol-Consumption among Women - Data from a Us National Sample. J Stud Alcohol. 1994;55(3):309–314. doi: 10.15288/jsa.1994.55.309. [DOI] [PubMed] [Google Scholar]
- Huerta M, Chodick G, Balicer RD, Davidovitch N, Grotto I. Reliability of self-reported smoking history and age at initial tobacco use. Prev Med. 2005;41(2):646–650. doi: 10.1016/j.ypmed.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Janssen SMJ, Chessa AG, Murre JMJ. Memory for time: How people date events. Mem Cognition. 2006;34(1):138–147. doi: 10.3758/bf03193393. [DOI] [PubMed] [Google Scholar]
- Johnson TP, Mott JA. The reliability of self-reported age of onset of tobacco, alcohol and illicit drug use. Addiction. 2001;96(8):1187–1198. doi: 10.1046/j.1360-0443.2001.968118711.x. [DOI] [PubMed] [Google Scholar]
- Kaestle CE. Age of Smoking Milestones: Longitudinal Inconsistencies and Recanting. J Adolescent Health. 2015;56(4):382–388. doi: 10.1016/j.jadohealth.2014.12.005. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gatz M, Gardner CO, Pedersen NL. Age at onset and familial risk for major depression in a Swedish national twin sample. Psychol Med. 2005;35(11):1573–1579. doi: 10.1017/S0033291705005714. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. The Lifetime History of Major Depression in Women - Reliability of Diagnosis and Heritability. Arch Gen Psychiat. 1993;50(11):863–870. doi: 10.1001/archpsyc.1993.01820230054003. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, Ustun TB, Wang PS. The global burden of mental disorders: An update from the WHO World Mental Health (WMH) Surveys. Epidemiol Psichiat S. 2009;18(1):23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatr. 2007a;20(4):359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Angermeyer M, Anthony JC, de Graaf R, Demyttenaere K, Gasquet I, de Girolamo G, Gluzman S, Gureje O, Haro JM, Kawakami N, Karam A, Levinson D, Mora MEM, Browne MAO, Posada-Villa J, Stein DJ, Tsang CHA, Aguilar-Gaxiola S, Alonso J, Lee S, Heeringa S, Pennell BE, Berglund P, Gruber MJ, Petkhova M, Chatterji S, Ustun TB, Conso WWMHS. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. 2007b;6(3):168–176. [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Stein DJ, Zaslavsky AM, Aguilar-Gaxiola S, Alonso J, Andrade L, Benjet C, de Girolamo G, de Graaf R, Demyttenaere K, Fayyad J, Haro JM, Hu CY, Karam A, Lee S, Lepine JP, Matchsinger H, Mihaescu-Pintia C, Posada-Villa J, Sagar R, Ustun TB. Development of Lifetime Comorbidity in the World Health Organization World Mental Health Surveys. Arch Gen Psychiat. 2011;68(1):90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klungsoyr O, Sexton J, Sandanger I, Nygard JF. A time-varying measurement error model for age of onset of a psychiatric diagnosis: applied to first depressive episode diagnosed by the Composite International Diagnostic Interview (CIDI). J Appl Stat. 2013;40(4):843–861. [Google Scholar]
- Knäuper B, Cannell CF, Schwarz N, Bruce ML, Kessler RC. Improving accuracy of major depression age-of-onset reports in the US National Comorbidity Survey. International Journal of Methods in Psychiatric Research. 1999;8(1):39–48. [Google Scholar]
- Koenig LB, Jacob T, Haber JR. Validity of the Lifetime Drinking History: A Comparison of Retrospective and Prospective Quantity-Frequency Measures. J Stud Alcohol Drugs. 2009;70(2):296–303. doi: 10.15288/jsad.2009.70.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labouvie E, Bates ME, Pandina RJ. Age of first use: Its reliability and predictive utility. J Stud Alcohol. 1997;58(6):638–643. doi: 10.15288/jsa.1997.58.638. [DOI] [PubMed] [Google Scholar]
- Louis ED. Age of Onset: Can We Rely on Essential Tremor Patients to Report This? Data from a Prospective, Longitudinal Study. Neuroepidemiology. 2013;40(2):93–98. doi: 10.1159/000341903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucking CB, Durr A, Bonifati V, Vaughan J, De Michele G, Gasser T, Harhangi BS, Meco G, Denefle P, Wood NW, Agid Y, Brice A, Suscep ECG, Stu FPDG. Association between early-onset Parkinson's disease and mutations in the parkin gene. New Engl J Med. 2000;342(21):1560–1567. doi: 10.1056/NEJM200005253422103. [DOI] [PubMed] [Google Scholar]
- Lyketsos CG, Nestadt G, Cwi J, Heithoff K, Eaton WW. The Life Chart Interview - a Standardized Method to Describe the Course of Psychopathology. International Journal of Methods in Psychiatric Research. 1994;4(3):143–155. [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40(6):899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra GR, O'Neill SE, Sher KJ. Reliability of self-reported age of substance involvement onset. Psychol Addict Behav. 2003;17(3):211–218. doi: 10.1037/0893-164X.17.3.211. [DOI] [PubMed] [Google Scholar]
- Pattaro C, Locatelli F, Sunyer J, de Marco R. Using the age at onset may increase the reliability of longitudinal asthma assessment. J Clin Epidemiol. 2007;60(7):704–711. doi: 10.1016/j.jclinepi.2006.10.010. [DOI] [PubMed] [Google Scholar]
- Patten SB, Gordon-Brown L, Meadows G. Simulation studies of age-specific lifetime major depression prevalence. Bmc Psychiatry. 2010;10 doi: 10.1186/1471-244X-10-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power RA, Keers R, Ng MY, Butler AW, Uher R, Cohen-Woods S, Ising M, Craddock N, Owen MJ, Korszun A, Jones L, Jones I, Gill M, Rice JP, Hauser J, Henigsberg N, Maier W, Zobel A, Mors O, Placentino AS, Rietschel M, Souery D, Kozel D, Preisig M, Lucae S, Binder EB, Aitchison KJ, Tozzi F, Muglia P, Breen G, Craig IW, Farmer AE, Muller-Myhsok B, McGuffin P, Lewis CM. Dissecting the Genetic Heterogeneity of Depression Through Age at Onset. Am J Med Genet B. 2012;159B(7):859–868. doi: 10.1002/ajmg.b.32093. [DOI] [PubMed] [Google Scholar]
- Power RA, Tansey KE, Buttenschøn HN, Cohen-Woods S, Bigdeli T, Hall LS, Kutalik Z, Lee SH, Ripke S, Steinberg S. Genome-wide association for major depression through age at onset stratification. Biological Psychiatry. 2016 doi: 10.1016/j.biopsych.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preisig M, Strippoli MPF, Castelao E, Merikangas KR, Gholam-Rezaee M, Marquet P, Aubry JM, Vandeleur CL. The specificity of the familial aggregation of early-onset bipolar disorder: A controlled 10-year follow-up study of offspring of parents with mood disorders. J Affect Disorders. 2016;190:26–33. doi: 10.1016/j.jad.2015.10.005. [DOI] [PubMed] [Google Scholar]
- Priebe L, Degenhardt FA, Herms S, Haenisch B, Mattheisen M, Nieratschker V, Weingarten M, Witt S, Breuer R, Paul T, Alblas M, Moebus S, Lathrop M, Leboyer M, Schreiber S, Grigoroiu-Serbanescu M, Maier W, Propping P, Rietschel M, Nothen MM, Cichon S, Muhleisen TW. Genome-wide survey implicates the influence of copy number variants (CNVs) in the development of early-onset bipolar disorder. Mol Psychiatr. 2012;17(4):421–432. doi: 10.1038/mp.2011.8. [DOI] [PubMed] [Google Scholar]
- Prusoff BA, Merikangas KR, Weissman MM. Lifetime Prevalence and Age of Onset of Psychiatric-Disorders - Recall 4 Years Later. J Psychiat Res. 1988;22(2):107–117. doi: 10.1016/0022-3956(88)90075-1. [DOI] [PubMed] [Google Scholar]
- Raphael KG, Marbach JJ. When did your pain start? Reliability of self-reported age of onset of facial pain. Clin J Pain. 1997;13(4):352–359. doi: 10.1097/00002508-199712000-00014. [DOI] [PubMed] [Google Scholar]
- Rice JP, Rochberg N, Endicott J, Lavori PW, Miller C. Stability of Psychiatric Diagnoses - an Application to the Affective-Disorders. Arch Gen Psychiat. 1992;49(10):824–830. doi: 10.1001/archpsyc.1992.01820100068012. [DOI] [PubMed] [Google Scholar]
- Roy J, Stewart WF. Estimation of age-specific incidence rates from cross-sectional survey data. Stat Med. 2010;29(5):588–596. doi: 10.1002/sim.3831. [DOI] [PubMed] [Google Scholar]
- Selkoe DJ. Alzheimer's disease: Genes, proteins, and therapy. Physiol Rev. 2001;81(2):741–766. doi: 10.1152/physrev.2001.81.2.741. [DOI] [PubMed] [Google Scholar]
- Shillington AM, Clapp JD. Self-report stability of adolescent substance use: are there differences for gender, ethnicity and age? Drug Alcohol Depen. 2000;60(1):19–27. doi: 10.1016/s0376-8716(99)00137-4. [DOI] [PubMed] [Google Scholar]
- Shillington AM, Clapp JD, Reed MB. The Stability of Self-Reported Marijuana Use across Eight Years of the National Longitudinal Survey of Youth. J Child Adoles Subst. 2011a;20(5):407–420. doi: 10.1080/1067828x.2011.614873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shillington AM, Clapp JD, Reed MB, Woodruff SI. Adolescent Alcohol Use Self-Report Stability: A Decade of Panel Study Data. J Child Adoles Subst. 2011b;20(1):63–81. [Google Scholar]
- Shillington AM, Reed MB, Clapp JD. Self-Report Stability of Adolescent Cigarette Use Across Ten Years of Panel Study Data. J Child Adoles Subst. 2010;19(2):171–191. [Google Scholar]
- Shillington AM, Woodruff SI, Clapp JD, Reed MB, Lemus H. Self-Reported Age of Onset and Telescoping for Cigarettes, Alcohol, and Marijuana: Across Eight Years of the National Longitudinal Survey of Youth. J Child Adoles Subst. 2012;21(4):333–348. doi: 10.1080/1067828X.2012.710026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon GE, Vonkorff M. Recall of Psychiatric History in Cross-Sectional Surveys - Implications for Epidemiologic Research. Epidemiol Rev. 1995;17(1):221–227. doi: 10.1093/oxfordjournals.epirev.a036180. [DOI] [PubMed] [Google Scholar]
- Stewart W, Brookmyer R, Vannatta M. Estimating Age Incidence from Survey Data with Adjustments for Recall Errors. J Clin Epidemiol. 1989;42(9):869–875. doi: 10.1016/0895-4356(89)90100-5. [DOI] [PubMed] [Google Scholar]
- Thompson R, Bogner HR, Coyne JC, Gallo JJ, Eaton WW. Personal characteristics associated with consistency of recall of depressed or anhedonic mood in the 13-year follow-up of the Baltimore Epidemiologic Catchment Area Survey. Acta Psychiat Scand. 2004;109(5):345–354. doi: 10.1111/j.1600-0447.2003.00284.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warshaw MG, Klerman GL, Lavori PW. Are Secular Trends in Major Depression an Artifact of Recall. J Psychiat Res. 1991;25(3):141–151. doi: 10.1016/0022-3956(91)90007-w. [DOI] [PubMed] [Google Scholar]
- Wells JE, Horwood LJ. How accurate is recall of key symptoms of depression? A comparison of recall and longitudinal reports. Psychol Med. 2004;34(6):1001–1011. doi: 10.1017/s0033291703001843. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.