Abstract
Background
Caring for older patients can be challenging in the Emergency Department (ED). A > 12 hr ED stay could lead to incident episodes of delirium in those patients. The aim of this study was to assess the incidence and impacts of ED-stay associated delirium.
Methods
A historical cohort of patients who presented to a Canadian ED in 2009 and 2011 was randomly constituted. Included patients were aged ≥ 65 years old, admitted to any hospital ward, non-delirious upon arrival and had at least a 12-hour ED stay. Delirium was detected using a modified chart-based Confusion Assessment Method (CAM) tool. Hospital length of stay (LOS) was log-transformed and linear regression assessed differences between groups. Adjustments were made for age and comorbidity profile.
Results
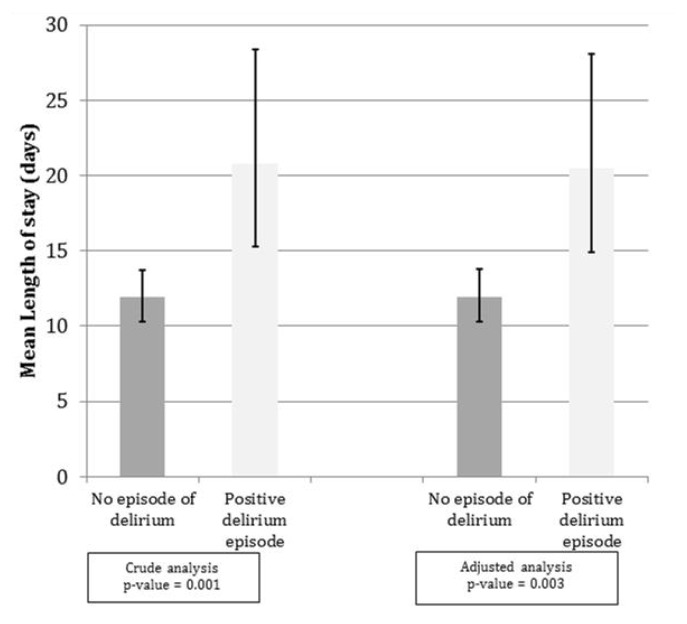
200 records were reviewed, 55.5% were female, median age was 78.9 yrs (SD:7.3). 36(18%) patients experienced ED-stay associated delirium. Nearly 50% of episodes started in the ED and within 36 hours of arrival. Comorbidity profile was similar between the positive CAM group and the negative CAM group. Mean adjusted hospital LOS were 20.5 days and 11.9 days respectively (p<.03).
Conclusions
1 older adult out of 5 became delirious after a 12 hr ED stay. Since delirium increases hospital LOS by more than a week, better screening and implementation of preventing measures for delirium could reduce LOS and overcrowding in the ED.
Keywords: elders, emergency department, incidence, delirium
INTRODUCTION
Over the coming decades, the demographic trends will change the make up of the population served by Emergency Departments (ED). In 2011, the first members of the baby boomer generation turned 65 years old. By 2031, the proportion of the population over 65 will nearly double.(1) Undeniably, the “Silver Tsunami”(2) will have consequences on the health care provided in EDs.
Delirium is a mental disorder of acute onset with a fluctuating course, characterized by a disturbance in consciousness, attention, orientation, memory, thoughts, perception, and behaviour.(3) It is a frequent problem among older adults referred to the hospital from other acute and long-term facilities, with a prevalence ranging from 9.6% to 89%.(4,5) The incidence of ED-stay associated delirium refers to the onset of delirium in previously non-delirious patients treated in the ED. The literature on ED-stay associated delirium is scant compared to that of intensive care units. In 2013, Inouye et al.(6,7) published a systematic review on delirium in older adults in which they found no robust study reporting the incidence of delirium in the ED. Since this review, a few studies prospectively assessed the incidence of delirium in the ED have been published.(8–11) To our knowledge, none were conducted in a Canadian ED setting.
Therefore, we sought to establish the incidence and impact of delirium in admitted ED patients. Our objectives were 1) to determine the incidence of delirium in patients aged ≥ 65 with an ED length of stay (LOS) of over 12 hrs, and 2) to evaluate the impact of ED-stay associated delirium on the hospitalization LOS in a Canadian health-care setting.
METHODS
In 2013, a historical cohort study of 200 patients was constituted with a computerized random sampling program using a list of patients from the Emergency Department Information System patient tracking software. Patients admitted in 2009 and 2011 at the University-affiliated CHU de Québec—Hôpital de l’Enfant-Jésus were included if they were: 1) ≥ 65 yrs old, 2) non-delirious at arrival,(12) 3) exposed to the ED for a minimum of 12 hrs, and 4) admitted to any hospital ward. Patients were excluded if they: 1) were in a medically unstable condition that led to ICU or equivalent, 2) were residents or in transition to long-term care facilities (information found in their medical chart), and 3) had a history of severe dementia or psychiatric conditions such as schizophrenia and bipolar disorder. Delirium and hospitalization LOS data were collected using administrative benchmarks in the chart. LOS was calculated using the ED admission and hospital discharge date and time.
A health records review was done by medical students using a standardized data collection tool. Those students were trained by the study supervisor (ME) in order to ensure appropriate completion of the data collection tool. The following information was collected: 1) demographic data, 2) ED LOS and hospital LOS, 3) comorbidities (Charlson Comorbidity Index(13)), 4) number of medications at ED admission and new medications administered during ED stay according to Beers criteria,(14) and 5) main diagnosis during hospitalization.
Main Outcome
The presence of delirium was assessed using a chart-based CAM:(12) orientation, hallucinations, agitation, confusion, fluctuation, state of consciousness scale. Positive delirium episode were categorized as early onset (within 24 hrs after the required 12-hr ED exposition) or late onset (after 24 hrs of the 12-hr ED exposition).
Univariate and multivariate statistical analyses were performed in order to determine the incidence of delirium and its consequences. Hospital LOS was log-transformed and linear regression assessed differences between groups. Adjustments were made for age and comorbidity. In order to ensure that the use of the tool was standardized, inter-rater agreements were realized. Based on an alpha of 5%, 200 patients would allow 80% power for an estimated overall incidence proportion of 15% with 5% precision. Analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, NC).
The Comité d’éthique du CHU de Québec approved this study (project # 2014-1746). No consent was necessary as it was a retrospective chart review study. Patient records/information were anonymized prior to analysis.
RESULTS
The historical cohort characteristics are described in Table 1. 200 charts were randomly included over a two-year period. Up to 18% (n = 36) of patients became delirious, of whom 50% initiated their delirium within the first 24 hrs. 41.2% of the episodes started while patients were still in the ED.
Table 1.
Patients’ clinical and demographic characteristics
| Characteristic | Total N (%) (n=200) | No Delirium Episode N (%) (n=164) | Positive Delirium Episode ≤ 24 hrs N (%) (n=18) | Positive Delirium Episode > 24 hrs N (%) (n=18) | p-value |
|---|---|---|---|---|---|
| Age (years) | |||||
| 65–74 | 61 (30.5) | 56 (34.1) | 4 (22.2) | 1 (5.6) | NS |
| 75–84 | 88 (44.0) | 70 (42.7) | 8 (44.5) | 10 (55.5) | |
| ≥85 | 51 (25.5) | 38 (23.2) | 6 (33.3) | 7 (38.9) | |
| Age (mean±SD) | 78.9±7.3 | 78.2±7.4 | 81.5±7.2 | 82.8±5.4 | 0.011 |
| Male | 91 (45.5) | 76 (46.3) | 9 (50.0) | 6 (33.3) | NS |
| Presence of New Delirium Episode | 36 (18.0) | -- | 18 (50.0) | 18 (50.0) | – |
| Medication Received in ED | |||||
| Presence of one dose of opiate | 63 (35.0) | 46 (31.3) | 10 (58.8) | 7 (43.8) | NS |
| Presence of Any BEER criteria | 6 (3.3) | 5 (3.4) | 0 (0.0) | 1 (6.3) | NS |
| Final Diagnoses Category | |||||
| Cardio-vascular (1) | 33 (16.5) | 29 (17.7) | 3 (16.7) | 1 (5.5) | – |
| Respiratory (2) | 33 (16.5) | 30 (18.3) | 2 (11.1) | 1 (5.5) | |
| Gastro-intestinal (3) | 22 (11.0) | 21 (12.8) | 0 (0.0) | 1 (5.5) | |
| Urinary tract disease (4) | 11 (5.5) | 9 (5.5) | 2 (11.1) | 0 (0.0) | |
| Musculo-Skeletal (5) | 6 (3.0) | 2 (1.2) | 3 (16.7) | 1 (5.5) | |
| Injury (6) | 32 (16.0) | 20 (12.2) | 5 (27.8) | 7 (38.9) | |
| Psychiatry (7) | 12 (6.0) | 9 (5.5) | 1 (5.5) | 2 (11.1) | |
| Neurology (8) | 22 (11.0) | 18 (11.0) | 1 (5.5) | 3 (16.7) | |
| Metabolic (9) | 5 (2.5) | 5 (3.1) | 0 (0.0) | 0 (0.0) | |
| Hematologic (10) | 3 (1.5) | 3 (1.8) | 0 (0.0) | 0 (0.0) | |
| Infectious (13) | 3 (1.5) | 2 (1.2) | 0 (0.0) | 1 (5.5) | |
| Tumor (14) | 11 (5.5) | 11 (6.7) | 0 (0.0) | 0 (0.0) | |
| Other (15) | 7 (3.5) | 5 (3.1) | 1 (5.5) | 1 (5.5) | |
| Comorbidities (Charlson Index) | |||||
| Low (0) | 30 (15.1) | 26(16.0) | 2 (11.1) | 2 (11.1) | NS |
| Medium (1–2) | 80 (40.2) | 60 (36.8) | 11 (61.1) | 9 (50.0) | |
| High (3–4) | 60 (30.1) | 51 (31.3) | 4 (22.2) | 5 (27.8) | |
| Very High (≥ 5) | 29 (14.6) | 26 (16.0) | 1 (5.6) | 2 (11.1) | |
| Deceased in Hospital | 7 (3.5) | 6 (3.7) | 1 (5.6) | 0 (0.0) | NS |
Age distribution showed a slightly skewed distribution of ED-stay associated delirium. Out of the 36 delirious episodes recorded, 5 patients (13.8%) were 65–74 years old, 18 (50.0%) were 75–84 years old, and 13 (37.2%) were over 85 years old. Patients with a positive delirium episode had a longer median ED LOS compared to non-delirious patients, 34.3 hrs (IQ: 27.1–54.4) and 30.2 (21.8–47.6), respectively (p > .05). Patients with positive ED-stay associated delirium received more opioid-related medications in the ED.
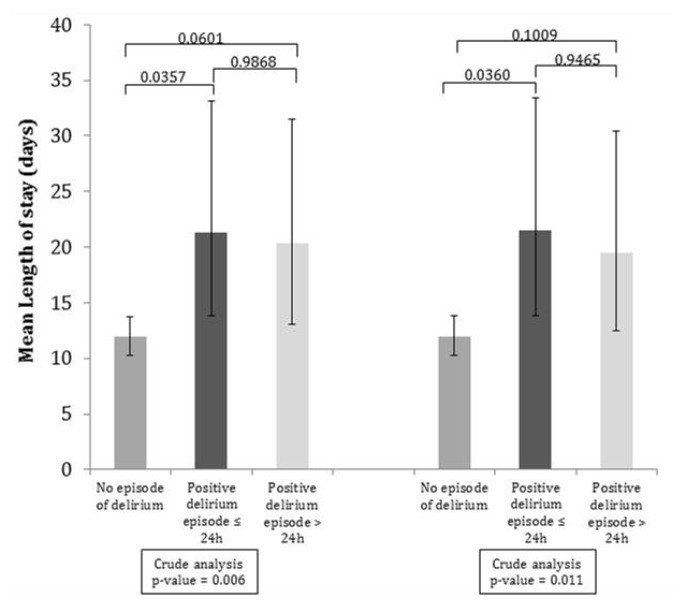
ED-stay associated delirium significantly increases the median hospital mean LOS (Figure 1). Results of the increased hospital LOS were similar when stratified by an early onset of delirium (< 24 hrs) versus a late onset (> 24 hrs) (Figure 2). Median LOS was increased from 10.2 days (IR: 6.2–21.3) to 23.7 (10.9–49.7) in early onset group and 17.9 day (11.1–24.2) in late onset group after adjusting for age and comorbidities (p < .05).
FIGURE 1.
Length of stay for incident delirium episode (n=200)
FIGURE 2.
Length of stay for incident delirium episode: onset before or after 24 hrs (n=200)
Inter-observer agreement was high for the incidence of delirium (main outcome) with kappa greater than 0.6.
DISCUSSION
Since the systematic review by Inouye and colleagues, a few prospective studies have been published on the incidence of delirium in the ED.(8–11) Unfortunately, literature is scant on the incidence of ED-stay associated delirium and its potential impacts on hospital LOS, functional status, and unplanned ED returns in Canadian settings. The onset of such complication in the ED could influence hospital LOS(15) and reflect back on ED crowding.(15) This may have a negative impact on preventive ED interventions such as the “senior-friendly approach”.(16)
In 2012, Dr. Roger Wong, president of the Canadian Geriatrics Society stated: “Many patients, when they come to a hospital, they enter through the emergency department. That is their portal of entry. That is their first stop. The ED is a very busy place with a high turnover. It’s not an ideal place for recognizing, let alone treating, delirium.”(17) Emergency care will become even more important for older adults in the future and exposure to this environment could trigger complications such as delirium. This Canadian historical cohort study is a first attempt to measure the importance of ED-stay associated delirium.
Experts suggest that prevalent and incident delirium in acute care hospitals may increase hospital stays by seven days(15) which could then have a significant impact on ED overcrowding and health-care costs. In 2003, McCusker et al.(15) followed in-patients with mostly prevalent and fewer incident delirium episodes. They observed that the latter added an average of 7.8 days to each hospital LOS. We had similar results with an increase of hospital LOS by nearly nine days in the delirium group.
Unrecognized delirium is a well-documented problem. Previous studies conducted in various clinical settings (including EDs and acute care hospitals) have revealed that over 50% of cases are left undetected.(4,5,18–20) According to Han et al.(21) the situation is even worse, as approximately 75% of cases are missed in the ED. Lack of knowledge about delirium and its clinical importance has been identified as a factor associated with non-detection of delirium by nurses.(22)
Older ED patients are particularly vulnerable to delirium. In 1993, Inouye et al.(23,24) demonstrated that an ED stay of ≥ 12 hrs was one of the strongest independent predictors of the onset of subsequent delirium in older patients. Bo et al.(8) also found a strong association between an ED stay of > 10 hrs and the onset of delirium in their cohort of patients aged 75 and over. However, their study did not assess the impact of delirium on the patient’s overall hospital length of stay. Their patients were older than our cohort (median age 82.8 (79.2–87.0)). The tool they used in order to detect delirium was the 4AT,(25) which obtained a sensitivity of 89.7% and a specificity of 84.1% for delirium when administered by a geriatrician, but was not validated within the ED context. Han et al.(10) had found similar results in their study including elderly patients who were in the ED for less than 12 hrs. However, their population is not representative of the actual ED context, since many seniors stay in the ED for long periods of time and those patients are more at risk of developing a delirium.(23,24)
An American study aimed to determine if delirium screening by triage nurses would decrease unplanned ED returns.(9) The paper provides no descriptive data on the population other than that they are all aged 65 and over. The tools used for delirium screening were the Richmond Assessment Sedation Scale (RASS),(26) combined with the brief Confusion Assessment Method (bCAM).(21) To our knowledge, no other study has evaluated the performance of the combination of those two tools in the detection of delirium. A single assessment using a modified version of the RASS alone has shown a sensitivity of only 64% and a specificity of 93% for the detection of delirium.(27) However, a more recent study found that the RASS had a sensitivity of 84% and a specificity of 87.6% for the detection of delirium when administered by an RA.(28) The bCAM by itself had a sensitivity of 78% and a specificity of 96.9% when administered by an RA.(21)
Our study presents some limitations. The retrospective nature may have underestimated the incidence of delirium since professionals may omit to recognize and report onset of delirium, as previously reported.(4,6,25–27) This under detection would have underestimated our delirium incidence and could suggest that more than one in five patients could have ED-stay associated delirium. Similarly, the chart-based CAM tool has been shown to be less sensitive than in-person delirium detection tools. The sensitivity was reported at 74% and a specificity at 83% compared to in-person interview with the CAM.(12) Again, this could have underestimated our ED-stay associated delirium incidence. It is also possible that some delirium cases were mixed with dementia; this would have overestimated our results. The chart-based CAM has shown a high rate of misclassification for patients with high baseline delirium risk, severe illness, and dementia.(12) This may have overestimated our delirium incidence. However, patients with dementia were excluded from our cohort and only 12 patients had a Charlson Index score that was classified as high and very high over a total of 89 patients within those two categories.
The secondary outcome of hospital LOS could have suffered from lack of adjustment. We adjusted for non-modifiable risk factors of delirium, such as age and comorbidities. However, our sample prevents us from adjusting for final diagnosis. This could have overestimated the LOS impact, although our results are similar to previous in-patient studies.(15)
CONCLUSION
After a 12-hr exposure to the ED, almost one in five patients aged over 65 waiting to be admitted to ward develop a delirium, half of which occur within the first day after exposition. ED-stay associated delirium increases the hospitalization LOS by approximately one week. Future senior-friendly approaches in the ED may help reduce the burden of delirium and reduce ED overcrowding.
ACKNOWLEDGEMENTS
Special thanks to Isabelle Gagné for the review of this manuscript and support, and to Xavier Neveu for statistical analyses and critical review of results.
Footnotes
This work was presented at the 2013 annual conference of the Quebec association of emergency physicians (AMUQ) and at the Canadian Association of Emergency Physicians (CAEP) 2014 annual conference in Ottawa.
CONFLICT OF INTEREST DISCLOSURES
The authors declare that no conflicts of interest exist.
REFERENCES
- 1.Heffler S, Levitt K, Smith S, et al. Health spending growth up in 1999; faster growth expected in the future. Health Affairs. 2001;20(2):193–203. doi: 10.1377/hlthaff.20.2.193. [DOI] [PubMed] [Google Scholar]
- 2.Delafuente JC. The silver tsunami is coming: will pharmacy be swept away with the tide? Am J Pharmaceut Edu. 2009;73(1):1. doi: 10.5688/aj730101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7–21. doi: 10.1097/00019442-200401000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Elie M, Rousseau F, Cole M, et al. Prevalence and detection of delirium in elderly emergency department patients. CMAJ. 2000;163(8):977–81. Epub 2000/11/09. [PMC free article] [PubMed] [Google Scholar]
- 5.Lemiengre J, Nelis T, Joosten E, et al. Detection of delirium by bedside nurses using the confusion assessment method. J Am Geriatr Soc. 2006;54(4):685–89. doi: 10.1111/j.1532-5415.2006.00667.x. [DOI] [PubMed] [Google Scholar]
- 6.Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22. doi: 10.1016/S0140-6736(13)60688-1. Epub 2013/09/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kishi Y, Iwasaki Y, Takezawa K, et al. Delirium in critical care unit patients admitted through an emergency room. Gen Hospital Psychiatry. 1995;17(5):371–79. doi: 10.1016/0163-8343(95)00056-W. Epub 1995/09/01. [DOI] [PubMed] [Google Scholar]
- 8.Bo M, Bonetto M, Bottignole G, et al. Length of stay in the emergency department and occurrence of delirium in older medical patients. J Am Geriatr Soc. 2016;64(5):1114–19. doi: 10.1111/jgs.14103. Epub 2016/05/11. [DOI] [PubMed] [Google Scholar]
- 9.Delaney M, Pepin J, Somes J. Emergency department delirium screening improves care and reduces revisits for the older adult patient. J Emerg Nurs. 2015;41(6):521–24. doi: 10.1016/j.jen.2015.08.013. Epub 2015/09/28. [DOI] [PubMed] [Google Scholar]
- 10.Han JH, Eden S, Shintani A, et al. Delirium in older emergency department patients is an independent predictor of hospital length of stay. Acad Emerg Med. 2011;18(5):451–57. doi: 10.1111/j.1553-2712.2011.01065.x. Epub 2011/04/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van de Meeberg EK, Festen S, Kwant M, et al. Improved detection of delirium, implementation and validation of the CAM-ICU in elderly Emergency Department patients. Eur J Emerg Med. 2016 doi: 10.1097/MEJ.0000000000000380. Epub 2016/02/20. [DOI] [PubMed] [Google Scholar]
- 12.Inouye SK, Leo-Summers L, Zhang Y, et al. A chart-based method for identification of delirium: validation compared with interviewer ratings using the Confusion Assessment Method. J Am Geriatr Soc. 2005;53(2):312–18. doi: 10.1111/j.1532-5415.2005.53120.x. [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Diseases. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Fick DM, Cooper JW, Wade WE, et al. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163(22):2716–24. doi: 10.1001/archinte.163.22.2716. Epub 2003/12/10. [DOI] [PubMed] [Google Scholar]
- 15.McCusker J, Cole MG, Dendukuri N, et al. Does delirium increase hospital stay? J Am Geriatr Soc. 2003;51(11):1539–46. doi: 10.1046/j.1532-5415.2003.51509.x. Epub 2003/12/23. [DOI] [PubMed] [Google Scholar]
- 16.Department of Health and Social Services, Government of Québec. Approche adaptée à la personne âgée en milieu hospitalier. 2011. [Google Scholar]
- 17.Collier R. Hospital-induced delirium hits hard. CMAJ. 2012;184(1):23–24. doi: 10.1503/cmaj.109-4069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Culp K, Tripp-Reimer T, Wadle K, et al. Screening for acute confusion in elderly long-term care residents. J Neurosci Nurs. 1997;29(2):86–88. 95–100. doi: 10.1097/01376517-199704000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Inouye SK, Foreman MD, Mion LC, et al. Nurses’ recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med. 2001;161(20):2467–73. doi: 10.1001/archinte.161.20.2467. [DOI] [PubMed] [Google Scholar]
- 20.Voyer P, Cole MG, McCusker J, et al. Accuracy of nurse documentation of delirium symptoms in medical charts. Int J Nurs Pract. 2008;14(2):165–77. doi: 10.1111/j.1440-172X.2008.00681.x. [DOI] [PubMed] [Google Scholar]
- 21.Han JH, Wilson A, Vasilevskis EE, et al. Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief Confusion Assessment Method. Ann Emerg Med. 2013;62(5):457–65. doi: 10.1016/j.annemergmed.2013.05.003. Epub 2013/08/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCarthy MC. PhD thesis. University of California San Francisco; San Francisco, CA: 1991. Interpretation of confusion in the aged: conflicting models of clinical reasoning among nurses. [Google Scholar]
- 23.Inouye SK, Viscoli CM, Horwitz RI, et al. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med. 1993;119(6):474–81. doi: 10.7326/0003-4819-119-6-199309150-00005. [DOI] [PubMed] [Google Scholar]
- 24.Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852–57. doi: 10.1001/jama.1996.03530350034031. [DOI] [PubMed] [Google Scholar]
- 25.Bellelli G, Morandi A, Davis DH, et al. Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing. 2014;43(4):496–502. doi: 10.1093/ageing/afu021. Epub 2014/03/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Han JH, Wilber ST. Altered mental status in older patients in the emergency department. Clin Geriatr Med. 2013;29(1):101–36. doi: 10.1016/j.cger.2012.09.005. Epub 2012/11/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chester JG, Beth Harrington M, Rudolph JL. Serial administration of a modified Richmond Agitation and Sedation Scale for delirium screening. J Hospital Med. 2012;7(5):450–53. doi: 10.1002/jhm.1003. Epub 2011/12/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Han JH, Vasilevskis EE, Schnelle JF, et al. The diagnostic performance of the Richmond Agitation Sedation Scale for detecting delirium in older emergency department patients. Acad Emerg Med. 2015;22(7):878–82. doi: 10.1111/acem.12706. Epub 2015/06/27. [DOI] [PMC free article] [PubMed] [Google Scholar]