Abstract
A daily rest period (DRP; rest taken from daily work during a 24 h period), is essential to work recovery. This study examined DRPs’ distribution and association with health outcomes among information technology workers recruited from an internet panel (N=1,811). Participants completed a web questionnaire examining psychological distress as a primary outcome, along with non-restorative sleep, fatigue (stress reaction), and work performance. Logistic regression analysis showed elevated psychological distress when DRP was <12 h (OR: 2.54; 95% CI: 1.47–4.42) and <11 h (OR: 2.48, 95% CI: 1.17–5.26), although the 95% CI included 1 after adjusting for age, sex, and working and commuting hours. After the above adjustment, similar associations were found with non-restorative sleep and fatigue, but not work performance, when DRP was <12 h. These findings constitute the first analysis of a dose-response relationship between DRP and subjective health outcomes among white-collar workers.
Keywords: Daily rest period, Quick returns, Long working hours, Overtime work, IT workers
Long working hours (LWH) are associated with poor mental health, sleep conditions and coronary heart disease1); workers engaging in LWH experience sleep deficits and fatigue which can lead to workplace inefficiency and experience disruption of family and social activities, which are important determinants of mental health2, 3). The European working time directive has set a limit of at least 11 consecutive hours of rest between shifts within a 24 period4) to prevent hazardous long or abnormal work patterns. This period of rest (daily rest period; DRP), has only been studied regarding a limited range of occupational groups (e.g., shift workers5)); accordingly, the available evidence remains inadequate regarding the minimum necessary DRP duration, including among office workers. Since the regulation of minimum DRP is expected to be a preventive measure6), discussions about appropriate rest periods based on scientific evidence, and data on the association between length of rest hours and health outcomes are essential. In Japan, the information technology (IT) industry contains the largest proportion of workplaces in which at least one employee works ≥100 hours of overtime per month (13%; Ministry of Health, Labour and Welfare, 2015). IT jobs have among the longest working hours and characteristically include strict deadlines and huge productivity requirements; these factors have been linked to fatigue and sleep problems among IT workers7, 8). Therefore, a relatively large proportion of IT workers are expected to experience short DRPs. We recruited a cohort of workers employed in diverse IT-related enterprises to investigate 1-year longitudinal associations between DRP duration and health outcomes; this article presents cross-sectional results at baseline.
This study examined weekday DRP distribution and DRPs’ association with subjective health outcomes (i.e., psychological distress primarily and non-restorative sleep, fatigue (stress reaction), and work performance as secondary objectives) among Japanese IT workers in information technology related jobs, including after adjusting for working hours and commuting time. This study also examined the effect of the quality of on- and off-work time on workers’ health outcomes. We hypothesized that workers taking DRPs of <11 h would show high psychological distress and other poor outcomes after adjusting for working hours and commuting time. In addition, we also hypothesized that the shorter the DRP from the normal DRP, the worse the psychological distress and all other outcomes.
We conducted an internet-based survey in October, 2015. We aimed to examine 2000 regular full-time employees working in IT related jobs; this sample size was chosen in advance to permit retention of a suitable number of participants at follow-up for longitudinal analysis (≥1,000 participants). Samples were collected from an online survey panel (MyVoice Communications, Inc.) in Japan, recruitment was planned to cease after collection of 2,000 participants. Participants individually recorded and submitted the time they had commenced and ceased work for the previous 10 consecutive days. Each participant’s mean DRP was subsequently calculated as the difference (in minutes) between the participant’s time of commencing work and ceasing work the previous day. The data collection period included a Saturday, a Sunday, and a holiday; accordingly, participants recorded a maximum number of five DRPs.
The K6 was used to measure psychological distress9). The K6 contains 6 items examining the previous 30 days; responses use a 5-point scale (0=never, 4=all the time); higher scores indicate greater psychological distress. Scores ≥13 were considered to indicate severe psychological distress. Non-restorative sleep (NRS) was examined using the question, “How often do you feel tired upon awakening in the morning?” Response options were very rarely, several times a year, once or more a month, once or twice a week, three times or more a week, and almost every day. This symptom was examined instead of sleep duration because we aimed to examine DRP’s association with recovery after sleep, rather than its association with sleep duration, which is inextricably expected to associate with DRP5). In addition, NRS has more association with daytime functioning when compared with other insomnia symptom subtypes10). Fatigue was operationalized as general stress reactions that is assessed by 11 items of 5 subscales (consisting of fatigue, anxiety, depression, loss of appetite, and poor sleep) from the Brief Job Stress Questionnaire (BJSQ)11), which would be expected to be used in many workplaces in Japan, because the scale was recommended by the government for the Stress Check Program that is mandated by the Industrial Safety and Health Law12). Therefore, using the BJSQ allows wide comparability in the health effect of exposure. The BJSQ has an acceptable level of internal consistency, test-retest reliability, and validity11). The World Health Organization (WHO) Health and Work Performance Questionnaire (HPQ) is a reliable and valid self-report questionnaire13) that examines absenteeism and presenteeism; one item from the HPQ was used to examine presenteeism (“How would you rate your overall job performance on the days you worked during the past 4 weeks (28 days)?); responses used a scale ranging from 0 to 10, with higher scores indicating higher work performance in the previous 4 weeks. Regarding demographic variables, participants’ sex and age were recorded. Regarding work-related variables, we recorded total weekly hours worked in the previous month (1–34, 35–40, 41–50, 51–60, 61–65, 66–70, or ≥71 hours) and one-way commute time (29 mins or less, 30 mins–59 mins, 1 h–1 h 29 mins, 1 h 30 mins–1 h 59 mins, 2 h or more). We also recorded employment status (regular, contract employee, entrusted employee, or dispatched worker from temporary labor agency) and working hour system (ordinary labor system, irregular labor system, flex time system, discretionary labor system, or other). Psychosocial workplace factors were examined using the BJSQ (i.e., quantitative workload, job control, and supervisor and coworker support). We also examined participants’ exercise habits (times per week), smoking status (nonsmoker, ex-smoker, current smoker), and potential DRP confounds (i.e., living with children aged ≤12 years, care provider) as common mental health status covariates.
The reference mean DRP duration was set in 15 h–15 h 59 minutes, as a 15-hour DRP corresponds to a standard eight-hour work shift with one hour of lunchtime14). Non-restorative sleep was considered present if reported as occurring ≥3 times per week. The reference mean total weekly working hours was set to the standard value of 35–40 h. The reference one-way commute time was set at <0.5 h. Employment status and working hour system were dichotomized as non-standard or standard (regular), and fixed (ordinary labor system) or non-fixed, respectively. Logistic and linear regression analysis was used to calculate ORs for DRP’s association with binary and continuous health outcomes, respectively, for bivariate and adjusted models. In addition to a crude bivariate model, two additional models were constructed to test if the identified associations were dependent on weekly working hours, commuting time, sex, or age (Model 2) or on any potential covariates (Model 3). All statistical analysis was performed using Stata 14.1 (Stata Corp., College Station TX, USA). Scientific conclusions and policy decisions should not be based only on specific p-value thresholds15); therefore, we reported and interpreted effect sizes and 95% confidence intervals (95% CIs) instead of p-values. The ethical committee of the National Institute of Occupational Safety and Health reviewed and approved the present study (Number: H2719). All participants gave web-based informed consent to complete the survey.
Participants were 1,907 IT related workers. We excluded participants who did not report all work commencement and cessation times or reported the same commencement and cessation times for all weekdays (n=35), who apparently worked a night shift on a weekday (commencing work at 4 PM or later and ceasing work before 12 PM the following day or not reporting a work cessation time; n=27), and who reported less than two DRPs during weekdays (n=34). Questionable responses (that is, a once-off work commencement or cessation time of 0:00; a once-off single work cessation time) were excluded pairwise (49 time points). Responses of a single work cessation time were transformed to an early-morning work cessation time if the participant worked ≥51 hours per week (51 time points) and transformed to an afternoon work cessation time if the participant worked <51 hours per week (35 time points). Following all exclusions, 1,811 participants were included in the final analysis.
Table 1 presents distributions of sex, age, and health outcomes by DRP group (full information available on request). Participants reporting mean DRPs of <11 h tended to be male, 50–59 years old, and in standard employment. Five percent of participants reported mean DRPs of <11 h (n=83).
Table 1. Participant characteristics and outcomes by DRP group.
| Mean DRP during weekdays (hours) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <10 (n=28) |
10 h–10 h 59 mins (n=55) |
11 h–11 h 59 mins (n=137) |
12 h–12 h 59 mins (n=253) |
13 h–13 h 59 mins (n=379) |
14 h–14 h 59 mins (n=542) |
15 h–15 h 59 mins (n=349) |
≥16 (n=68) |
|||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |
| Sex | ||||||||||||||||
| Male | 27 | (96.4) | 53 | (96.4) | 129 | (94.2) | 233 | (92.1) | 339 | (89.5) | 449 | (82.8) | 272 | (77.9) | 38 | (55.9) |
| Female | 1 | (3.6) | 2 | (3.6) | 8 | (5.8) | 20 | (7.9) | 40 | (10.6) | 93 | (17.2) | 77 | (22.1) | 30 | (44.1) |
| Age | ||||||||||||||||
| 20–29 | 2 | (7.1) | 3 | (5.5) | 8 | (5.8) | 11 | (4.4) | 9 | (2.4) | 19 | (3.5) | 19 | (5.4) | 2 | (2.9) |
| 30–39 | 7 | (25.0) | 8 | (14.6) | 31 | (22.6) | 60 | (23.7) | 72 | (19.0) | 117 | (21.6) | 69 | (19.8) | 17 | (25.0) |
| 40–49 | 8 | (28.6) | 22 | (40.0) | 70 | (51.1) | 102 | (40.3) | 166 | (43.8) | 213 | (39.3) | 137 | (39.3) | 22 | (32.4) |
| 50–59 | 10 | (35.7) | 21 | (38.2) | 26 | (19.0) | 74 | (29.3) | 122 | (32.2) | 169 | (31.2) | 96 | (27.5) | 24 | (35.3) |
| 60–64 | 1 | (3.6) | 1 | (1.8) | 2 | (1.5) | 6 | (2.4) | 10 | (2.6) | 24 | (4.4) | 28 | (8.0) | 3 | (4.4) |
| Non-restorative sleep (instances per week) | ||||||||||||||||
| <3 | 15 | (53.6) | 27 | (49.1) | 86 | (62.8) | 188 | (74.3) | 272 | (71.8) | 412 | (76.0) | 255 | (73.1) | 50 | (73.5) |
| ≥3 | 13 | (46.4) | 28 | (50.9) | 51 | (37.2) | 65 | (25.7) | 107 | (28.2) | 130 | (24.0) | 94 | (26.9) | 18 | (26.5) |
| Fatigue (stress symptoms)* (range: 11–44) |
26.8 | (9.2) | 26.5 | (9.0) | 25.1 | (8.6) | 22.9 | (7.6) | 21.9 | (7.0) | 21.1 | (7.5) | 20.2 | (7.8) | 19.9 | (7.4) |
| Work performance* (range: 0–10) |
5.9 | (2.1) | 5.4 | (2.1) | 5.6 | (1.7) | 5.8 | (1.6) | 5.7 | (1.8) | 5.9 | (1.7) | 5.8 | (1.8) | 5.6 | (2.0) |
Note. N=1,811; *mean (standard deviation); full information for other variables available on request.
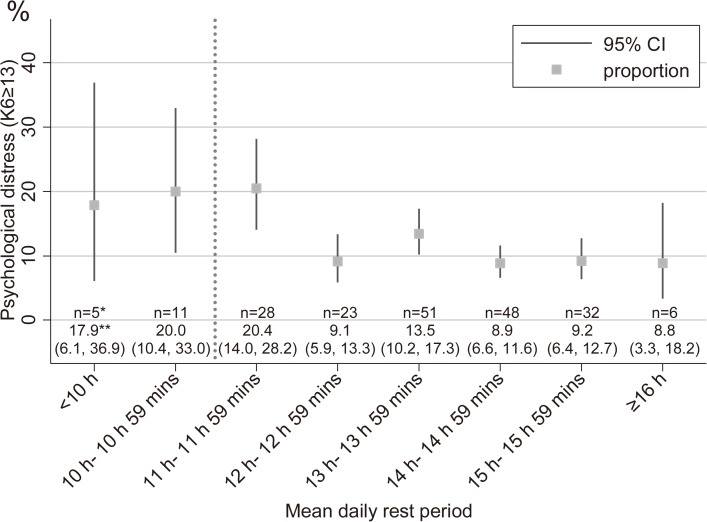
High psychological distress was approximately twice as prevalent among participants reporting mean DRPs of <12 or <11 h along with frequent non-restorative sleep, and heightened fatigue; however, work performance remained constant across each DRP hours (Fig. 1; Table 1). Regarding logistic regression analysis, participants reporting DRPs of 10 h–10 h 59 mins and 11 h–11 h 59 mins were approximately 1.7 times more likely to report high psychological distress than participants reporting the reference DRP duration, including after adjusting for weekly working hours, commuting time, sex, and age; however, the corresponding 95% CI included 1 (Table 2). This ratio was reduced almost to 1 after adjusting for all other examined covariates. Participants reporting DRPs of <10 h did not show this association. Additionally, a small peak in psychological distress was observed among participants reporting DRPs of 13 h–13 h 59 mins, which remained after adjusting for confounders. In Model 2 and compared with the reference DRP duration, participants reporting DRPs of 10 h–10 h 59 mins were approximately 2.5 times more likely to report frequent non-restorative sleep and reported greater mean fatigue by 3.5 points. The same patterns of associations were observed among participants reporting DRPs of 11 h–11 h 59 mins and <10 h, although the confidence interval included 1 regarding non-restorative sleep. The association between DRP and fatigue was reduced to near 0 after adjusting for all other covariates. All 95% CIs for reported work performance included 0; however, work performance was consistently impaired by approximately 0.4 points only among participants reporting 10 h–10 h 59 mins DRPs after adjusting for each set of covariates.
Fig. 1.
Prevalence of high psychological distress by DRP duration.
n=1,811; a dotted line is a reference line of 11 hours by the European working time directive; *numbers of high psychological distress (K6≥13); **proportions of high psychological distress (i.e., K6≥13) and 95% confidence intervals in parentheses
Table 2. DRP’s association with psychological distress, non-restorative sleep, stress symptoms, and work performance.
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate* | 95% CI | Estimate* | 95% CI | Estimate* | 95% CI | ||||
| Psychological distress | |||||||||
| DRP duration (h) | |||||||||
| <10 | 2.15 | (0.77, 6.05) | 1.35 | (0.44, 4.16) | 0.72 | (0.20, 2.51) | |||
| 10 h–10 h 59 mins | 2.48 | (1.17, 5.26) | 1.74 | (0.74, 4.10) | 0.96 | (0.37, 2.51) | |||
| 11 h–11 h 59 mins | 2.54 | (1.47, 4.42) | 1.86 | (0.96, 3.58) | 1.30 | (0.63, 2.69) | |||
| 12 h–12 h 59 mins | 0.99 | (0.56, 1.74) | 0.88 | (0.47, 1.63) | 0.59 | (0.30, 1.17) | |||
| 13 h–13 h 59 mins | 1.54 | (0.96, 2.46) | 1.51 | (0.89, 2.55) | 1.34 | (0.76, 2.35) | |||
| 14 h–14 h 59 mins | 0.96 | (0.60, 1.54) | 1.00 | (0.61, 1.64) | 0.93 | (0.55, 1.58) | |||
| 15 h–15 h 59 mins | (ref) | (ref) | (ref) | ||||||
| ≥16 | 0.96 | (0.38, 2.39) | 0.83 | (0.32, 2.12) | 0.78 | (0.28, 2.17) | |||
| Non-restorative sleep | |||||||||
| DRP duration (h) | |||||||||
| <10 | 2.35 | (1.08, 5.13) | 2.17 | (0.94, 5.03) | 1.70 | (0.70, 4.14) | |||
| 10 h–10 h 59 mins | 2.81 | (1.58, 5.02) | 2.54 | (1.33, 4.84) | 1.72 | (0.87, 3.41) | |||
| 11 h–11 h 59 mins | 1.61 | (1.06, 2.45) | 1.60 | (0.98, 2.61) | 1.24 | (0.74, 2.08) | |||
| 12 h–12 h 59 mins | 0.94 | (0.65, 1.36) | 0.98 | (0.65, 1.47) | 0.80 | (0.52, 1.23) | |||
| 13 h–13 h 59 mins | 1.07 | (0.77, 1.48) | 1.13 | (0.79, 1.63) | 0.99 | (0.68, 1.44) | |||
| 14 h–14 h 59 mins | 0.86 | (0.63, 1.16) | 0.91 | (0.66, 1.26) | 0.87 | (0.62, 1.23) | |||
| 15 h–15 h 59 mins | (ref) | (ref) | (ref) | ||||||
| ≥16 | 0.98 | (0.54, 1.76) | 0.84 | (0.46, 1.54) | 0.84 | (0.44, 1.58) | |||
| Fatigue (stress symptoms) | |||||||||
| DRP duration (h) | |||||||||
| <10 | 6.61 | (3.67, 9.56) | 3.39 | (0.33, 6.46) | 0.93 | (−1.88, 3.73) | |||
| 10 h–10 h 59 mins | 6.25 | (4.07, 8.42) | 3.46 | (1.13, 5.78) | 0.64 | (−1.50, 2.79) | |||
| 11 h–11 h 59 mins | 4.86 | (3.35, 6.37) | 2.26 | (0.57, 3.95) | 0.38 | (−1.19, 1.95) | |||
| 12 h–12 h 59 mins | 2.70 | (1.47, 3.94) | 1.18 | (−0.16, 2.51) | −0.25 | (−1.49, 0.99) | |||
| 13 h–13 h 59 mins | 1.72 | (0.61, 2.83) | 0.58 | (−0.62, 1.78) | −0.47 | (−1.57, 0.64) | |||
| 14 h–14 h 59 mins | 0.87 | (−0.15, 1.90) | 0.44 | (−0.62, 1.49) | 0.12 | (−0.85, 1.08) | |||
| 15 h–15 h 59 mins | (ref) | (ref) | (ref) | ||||||
| ≥16 | −0.34 | (−2.33, 1.65) | −0.48 | (−2.47, 1.50) | −0.33 | (−2.14, 1.48) | |||
| Work performance | |||||||||
| DRP duration (h) | |||||||||
| <10 | 0.08 | (−0.60, 0.76) | 0.16 | (−0.57, 0.88) | 0.24 | (−0.43, 0.92) | |||
| 10 h–10 h 59 mins | −0.41 | (−0.91, 0.09) | −0.38 | (−0.93, 0.17) | −0.36 | (−0.88, 0.15) | |||
| 11 h–11 h 59 mins | −0.14 | (−0.49, 0.21) | −0.10 | (−0.50, 0.29) | −0.15 | (−0.53, 0.22) | |||
| 12 h–12 h 59 mins | 0.06 | (−0.23, 0.34) | 0.04 | (−0.28, 0.35) | 0.03 | (−0.26, 0.33) | |||
| 13 h–13 h 59 mins | −0.07 | (−0.33, 0.19) | −0.11 | (−0.39, 0.17) | −0.14 | (−0.41, 0.12) | |||
| 14 h–14 h 59 mins | 0.08 | (−0.16, 0.31) | 0.03 | (−0.21, 0.28) | 0.00 | (−0.23, 0.23) | |||
| 15 h–15 h 59 mins | (ref) | (ref) | (ref) | ||||||
| ≥16 | −0.21 | (−0.67, 0.24) | −0.13 | (−0.60, 0.34) | −0.24 | (−0.68, 0.19) | |||
Note. n=1,811; *Estimates are odds ratios for psychological distress and non-restorative sleep, and coefficients of linear regression for fatigue and work performance; odds ratios in bold do not include 1; linear regression coefficients in bold do not include 0; Model 1, bivariate model without any covariates; Model 2, added covariates were age (continuous), sex, weekly working hours and commuting time, Model 3, added covariates (relative to model 2) were employment status, working schedule, exercise (continuous), smoking, having children, caregiving, quantitative workload (continuous), control (continuous), supervisor support (continuous), and coworker support (continuous)
The present results indicate that approximately 1 in 22 Japanese IT workers experience mean DRPs of <11 h between weekdays over 10 consecutive days. Workers experiencing DRPs of <11 and <12 h were more likely to show high psychological distress. These associations were not independent of working and commuting time or demographic variables. After adjusting for diverse confounders including health behavior, caring for family members, and job stress, the associations between short DRP and high psychological distress got even closer to null. In contrast, increased levels of non-restorative sleep and fatigue were associated with DRP durations of <12 h including after controlling for age, sex, weekly working hours, and commuting time. Workers reporting DRPs of 10 h–10 h 59 mins showed the greatest impairment in work performance; however, the relevant 95% CI included 0.
In contrast with our hypothesis, participants reporting DRPs of <12 h were most likely to show high psychological distress; however this association’s strength decreased at <10 h. Workers experiencing poor mental health may be unable to tolerate very short DRPs; these workers may therefore have been preferentially selected out of the group experiencing DRPs of <10 h, resulting in an artificially reduced strength of association between psychological distress and DRP duration at very low duration values. Additionally, adding age, sex, weekly working hours, and commuting time into the model reduced ORs between DRP duration and psychological distress, suggesting that those factors explained the apparent increase in psychological distress among workers reporting DRPs <12 h.
When DRP was less than 12 h, non-restorative sleep was found to increase. More clear results were obtained for fatigue, this symptom elevated in a DRP dependent manner, including after adjusting for age, sex, weekly working hours, and commuting time. These results resemble those of previous studies examining shift workers6, 16), although they used a general measure of sleep problems rather than the NRS. Nonetheless, DRP’s association with non-restorative sleep and fatigue was mostly attenuated after adjusting for all examined potential covariates (i.e., in Model 3), suggesting that the examined covariates importantly influence DRP duration’s effect on sleep and fatigue. DRP duration was observed to be weakly associated with reported work performance, although the relevant CI included 0. Notably, this association remained largely stable after adjusting for all covariates. Future research should further examine short DRPs’ effect on work performance. The difference of association with DRP among health outcomes may be attributed to the nature of the phase of cumulated fatigue by each individual and to the tolerability to the short DRP5). As noted above, workers with high psychological distress, which is thought of as the most severe health outcome in our study, may be unable to tolerate short DRP; most workers with relatively mild symptoms such as NRS or fatigue and low work performance, that is healthy workers, could in contrast continue to engage in short DRP.
This study has the following limitations. First, workers with consistently short DRPs and poor mental health may have been less common among the online survey panel’s members or less likely to participate in an online survey, making the sample potentially less representative of IT related workers in general. Additionally, among participants who completed the survey, poor mental health may have made participants more likely to work less, resulting in longer DRPs. Second, we measured DRP duration via self-report, and prolonged exposure to short DRPs may have reduced participants’ response accuracy regarding their DRP duration, potentially making DRP reporting less accurate among participants experiencing shorter DRPs. Future research should independently and directly measure participants’ DRP duration, particularly among participants experiencing short DRPs, and consider that official records of working hours may be inaccurate due to the proliferation of unpaid overtime.
To our knowledge, this study is the first to examine DRP’s dose-response relationship with subjective health outcomes among white-collar workers, adjusting for working hours and commuting time. The present results indicate that workers experiencing mean DRP durations of <12 hours are more likely to experience the possibility of a small increase in psychological distress, non-restorative sleep, and fatigue symptoms. This result may call for the reconfirmation of 11 consecutive hours of rest between shifts within a 24 period, the criteria developed by The European working time directive4). Toward this end, future research should prospectively examine DRP’s association with psychological distress, non-restorative sleep, fatigue, and work performance for promoting the preventive policy. We believe that our study addresses an important topic in occupational medicine which serves as a basis for further discussion for DRP.
Acknowledgments
This research was supported by JNIOSH project research (N-P26-01).
References
- 1.Bannai A, Tamakoshi A (2014) The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health 40, 5–18. [DOI] [PubMed] [Google Scholar]
- 2.Harrington JM. (2001) Health effects of shift work and extended hours of work. Occup Environ Med 58, 68–72. [Google Scholar]
- 3.Marchand A, Durand P, Haines V 3rd, Harvey S (2015) The multilevel determinants of workers’ mental health: results from the SALVEO study. Soc Psychiatry Psychiatr Epidemiol 50, 445–59. [DOI] [PubMed] [Google Scholar]
- 4.European Parliament, Council of the European Union (2003) Directive 2003/88/EC of the European Parliament and of the Council of 4 November 2003 concerning certain aspects of the organisation of working time.
- 5.Vedaa Ø, Harris A, Bjorvatn B, Waage S, Sivertsen B, Tucker P, Pallesen S (2016) Systematic review of the relationship between quick returns in rotating shift work and health-related outcomes. Ergonomics 59, 1–14. [DOI] [PubMed] [Google Scholar]
- 6.Flo E, Pallesen S, Moen BE, Waage S, Bjorvatn B (2014) Short rest periods between work shifts predict sleep and health problems in nurses at 1-year follow-up. Occup Environ Med 71, 555–61. [DOI] [PubMed] [Google Scholar]
- 7.Karita K, Nakao M, Nishikitani M, Iwata T, Murata K, Yano E (2006) Effect of overtime work and insufficient sleep on postural sway in information-technology workers. J Occup Health 48, 65–8. [DOI] [PubMed] [Google Scholar]
- 8.Kivistö M, Härmä M, Sallinen M, Kalimo R (2008) Work-related factors, sleep debt and insomnia in IT professionals. Occup Med (Lond) 58, 138–40. [DOI] [PubMed] [Google Scholar]
- 9.Furukawa TA, Kawakami N, Saitoh M, Ono Y, Nakane Y, Nakamura Y, Tachimori H, Iwata N, Uda H, Nakane H, Watanabe M, Naganuma Y, Hata Y, Kobayashi M, Miyake Y, Takeshima T, Kikkawa T (2008) The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int J Methods Psychiatr Res 17, 152–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, Kessler RC (2006) Sleep problems, comorbid mental disorders, and role functioning in the national comorbidity survey replication. Biol Psychiatry 60, 1364–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inoue A, Kawakami N, Shimomitsu T, Tsutsumi A, Haratani T, Yoshikawa T, Shimazu A, Odagiri Y (2014) Development of a short questionnaire to measure an extended set of job demands, job resources, and positive health outcomes: the new brief job stress questionnaire. Ind Health 52, 175–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawakami N, Tsutsumi A (2016) The Stress Check Program: a new national policy for monitoring and screening psychosocial stress in the workplace in Japan. J Occup Health 58, 1–6. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, Pronk N, Simon G, Stang P, Ustun TB, Wang P (2003) The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Environ Med 45, 156–74. [DOI] [PubMed] [Google Scholar]
- 14.Virtanen M, Kivimäki M (2012) Saved by the bell: does working too much increase the likelihood of depression? Expert Rev Neurother 12, 497–9. [DOI] [PubMed] [Google Scholar]
- 15.Wasserstein RL, Lazar NA (2016) The ASA’s Statement on p-Values: Context, Process, and Purpose. Am Stat 70, 129–33. [Google Scholar]
- 16.Eldevik MF, Flo E, Moen BE, Pallesen S, Bjorvatn B (2013) Insomnia, excessive sleepiness, excessive fatigue, anxiety, depression and shift work disorder in nurses having less than 11 hours in-between shifts. PLoS One 8, e70882. [DOI] [PMC free article] [PubMed] [Google Scholar]