Abstract
The murine monoclonal antibody LA-2 recognizes a clinically protective epitope on outer surface protein (OspA) of Borrelia burgdorferi, the causative agent of Lyme disease in North America. Human antibody equivalence to LA-2 is the best serologic correlate of protective antibody responses following OspA vaccination. Understanding the structural and functional basis of the LA-2 protective epitope is important for developing OspA-based vaccines and discovering prophylactic antibodies against Lyme disease. Here, we present a detailed structure-based analysis of the LA-2/OspA interaction interface and identification of residues mediating antibody recognition. Mutations were introduced into both OspA and LA-2 based on computational predictions on the crystal structure of the complex, and experimentally tested for in-vitro binding and borreliacidal activity. We find that Y32 and H49 on the LA-2 light chain, N52 on the LA-2 heavy chain and residues A208, N228 and N251 on OspA were the key constituents of OspA/LA-2 interface. These results reveal specific residues that may be exploited to modulate recognition of the protective epitope of OspA and have implications for developing prophylactic passive antibodies.
Introduction
Lyme disease is the most common tick-borne infection in temperate climate zones. The causative agent of Lyme disease, spirochete Borrelia is transmitted to human through the bite of infected Ixodes ticks. The incidence of Lyme disease has been increasing dramatically. The Centers for Disease Control and Prevention has estimated over 300,000 Americans are diagnosed with Lyme disease each year (Shapiro, 2014). The only currently available means to prevent Lyme disease is to avoid exposure to infected ticks.
Outer surface protein (OspA) is a 273 amino acid lipoprotein expressed on the surface of Borrelia spirochete. It has been well established that passively administered anti-OspA antibodies or active immunization with recombinant OspA vaccine is protective against Borrelia infection (Golde et al., 1997; Johnson et al., 1995; Schaible et al., 1990; Sigal et al., 1998). Anti-OspA antibodies are believed to block transmission by eliminating OspA expressing spirochetes in the midgut of the feeding ticks. The murine monoclonal antibody LA-2 recognizes a protective epitope on OspA. LA-2 has been viewed as a gold standard for measuring effective sera response after OspA vaccination (Golde et al., 1997; Johnson et al., 1995; Van Hoecke et al., 1999). Individuals who failed to develop antibodies against LA-2 epitopes were associated with vaccine failures in human vaccine trials.
Worldwide three main genospecies of Borrelia are associated with Lyme disease in humans. Borrelia burgdorferi is the main cause of Lyme disease in North America while Borrelia garinii and Borrelia afzelii are the prevalent strains that cause the disease in Europe and Asia (Stanek et al., 2012). OspA protein is heterogeneous across the three genospecies. There is no vaccine or therapeutic antibody currently available in the clinic for preventing Lyme disease caused by Borrelia burgdorferi, much less a treatment that would protect against all global Borrelia strains (Poland, 2011). Rational development of novel cross-reactive vaccine or prophylactic antibodies requires the identification and characterization of protective epitopes on the OspA proteins.
The structure of LA-2 antibody bound to B. burgdorferi OspA has been determined by nuclear magnetic resonance spectroscopy and X-ray crystallography (Ding et al., 2000; Li et al., 1997). The LA-2 protective epitope is mapped to three surface exposed loops located at the C-terminus of OspA protein (Figure 1). Since LA-2 protects only against B. burgdorferi and not B. afzelii or B. garinii, the sequence variability in the LA-2 epitope may have an implication for the binding specificity of LA-2.
Figure 1.
The structure of B. burgdorferi OspA and LA-2 complex. (A) The interface colored according to the extent of intermolecular van der Waals interactions, from blue to red. OspA N251 is the residue with the highest contact with the antibody (hence colored red). (B) The three surface-exposed OspA loops mediating the interaction, and hydrogen bonds between OspA residues (labeled in italics) and LA-2 heavy chain.
In this study, we interrogated the interface between LA-2 antibody and OspA to identify key residues mediating this interaction. We have carried out experimental Ala scanning on both the antibody and its protective epitope on OspA and measured the change in affinity with respect to the wild type complex. Further, mutations were engineered to guide antibody design selected with the aid of in silico structural analysis,. We identified critical residues on both LA-2 and OspA that influence their interaction and identified mutations that enhance antibody affinity, which may have implications for the structural basis for rational design of novel prophylactic biologics for Lyme disease.
Materials and Methods
Structural Analysis
The OspA/LA-2 complex crystal structure was obtained from the Protein Data Bank (PDB ID: 1FJ1) (Li et al., 1997) and processed using the Protein Preparation Wizard in Maestro (Schrodinger, Inc.), followed by in-silico mutagenesis of the residues in LA-2 that are involved in forming the OspA/LA-2 interface, using the Residue-Scanning and Mutation tool in BioLuminate (Zhu et al., 2014) (Beard et al., 2013) (Schrodinger, Inc.) with conformational search involving ±1 residue backbone adjustment. The Prime MM-GBSA (Schrodinger, Inc.) calculated changes in affinity (dAffinity) were compared to the in-vitro experimental affinities of mutant LA-2/OspA for validation and selecting other residue mutations. The intermolecular hydrogen bonds, % buried surface area and van der Waals complementarity were calculated using built-in functions of BioLuminate, and the van der Waals contact energies using an in-house script as described previously in detail (Ozen et al., 2012).
Homology Modeling
The B. burgdorferi OspA (PDB ID: 1FJ1) structure processed using the ‘Protein preparation Wizard’ above was used as the template structure. Target OspA sequences, generated by incorporating residue differences from B. afzelii or B. garinii into the B. burgdorferi OspA template sequence (Figure 1), were loaded in the ‘Multiple Sequence Viewer’ module and used for Knowledge-based homology modeling using Prime (Jacobson et al., 2002; Jacobson et al., 2004). The resulting homology models were processed using energy minimization with the OPLS2005 (Banks et al., 2005) force field and the ‘automatic’ approach that applies a conjugate gradient method with large gradients and a truncated Newton method with smaller gradients.
OspA Mutagenesis and Protein Expression
The nucleic acid sequence encoding the full length OspA from Borrelia burgdorferi B31 (Genbank accession number NP_045688) was synthesized and cloned into pET45-b in-frame with an N-terminal histidine (His) tag. Point mutations were introduced to OspA sequences using site-directed mutagenesis and the mutant constructs were sequenced to ensure intended mutations.
All cloned constructs were transformed into BL21-DE3 E. coli bacteria (Invitrogen) and protein expression was induced with 1 mM IPTG. Bacteria were lysed and the recombinant OspA proteins were purified with Ni-NTA agarose (Invitrogen) and eluted with 250 mM imidazole (Sigma). Protein integrity and purity were evaluated by Coomassie stained SDS-PAGE and Western blot using mouse anti-His antibody.
LA-2 Mutagenesis and Antibody Expression
The nucleic acid sequence encoding LA-2 (Genbank accession number 1FJ1_A, B) was synthesized and cloned into pcDNA 3.1expression vectors. Point mutations were introduced into antibody heavy and light chain gene sequences using site-directed mutagenesis and the mutant constructs were sequenced to ensure intended mutations. Vectors containing heavy chain and light chain antibody genes were co-transfected into 293T cells to produce LA-2 antibody and its mutant variants. Antibodies were purified by protein A chromatography (GE Healthcare), eluted with 100mM glycine pH 2.8, dialyzed and formulated in PBS buffer at 0.5–1 mg/mL. Antibody integrity and purity were verified by SDS-page gels.
Affinity Determination
Surface plasmon resonance (SPR) on a Biacore 3000 was used to determine the affinity of LA-2 to OspA-burgdorferi and their mutant variants. LA-2 and its mutant variants were captured on the surface of Biacore CM5 chips via anti-mouse antibody capture kit (GE healthcare). The captured antibodies were exposed to serial dilutions of OspA proteins. The kon and koff and the associated affinity (KD) were calculated by BIAevaluation software.
Borreliacidal Assay by Flow Cytometry
Borrelia spirochetes (B. burgdorferi B31) were obtained from ATCC (Cat# 35210). Spirochetes were cultured in BSK-H Complete Medium (Sigma-Aldrich) and working cell banks were generated and kept low passage numbers. Frozen suspensions of Borrelia were thawed and inoculated into fresh BSK-H medium and incubated at 37 °C for 72 hours prior to the assay. Spirochetes were counted using dark-field microscopy with a Petroff-Hausser counting chamber.
LA-2 wild type and mutant antibodies were diluted to 20 nM in 100 μL of BSK-H medium containing 10% of guinea pig complement (Sigma). 100 μL of Borrelia culture at a concentration of 5×106 spirochetes/mL was added to antibody dilutions and the mixture was incubated at 37°C for 16 hrs. After incubation, 100 μL was removed from the mixture; diluted 1:5 in PBS and 50 μL of acridine orange was added. The spirochete viability was then quantified by flow cytometry. All assays were performed in duplicate and an unrelated mouse monoclonal antibody was included as control.
Results
B. burgdorferi OspA/LA-2 Interface
The tripartite OspA/LA-2 interface is formed between the LA-2 antibody and three surface loops on OspA (Ding et al., 2000) (Figure 1). Key residues mediating this interaction with intermolecular van der Waals (vdW) contacts include OspA residues S206, A208, A214, A215 (loop 1), V227-K230 (loop 2), D249-N251 and T253 (loop 3). Two polar asparagine side chains, N228 in loop 2 and N251 in loop 3, further anchor the protein to the antibody by forming two hydrogen bonds each (Figure 1B). Two additional hydrogen bonds are formed by the side chains of K230 (loop 2) and S250 (loop 3). Loop 1 has no hydrogen bonds with the antibody and contributes the least to the intermolecular interactions among the three loops. Hence, residues with the most contribution to the interface are located at the tips of OspA loops 2 (S250-N251) and 3 (N228-S229-K230).
The OspA protective epitope is recognized by LA-2 antibody residues T30-S33, Y35, W50, N52, L100, and D101 of the heavy chain and Y32, H49, Y50, Q55, and L94-R96 of the light chain. While more light chain residues participate in van der Waals contacts with the OspA protein, all intermolecular hydrogen bonds are formed by the antibody heavy chain residues (T30, D31, T53, L100, D101; Figure 1B).
All residues that participate in intermolecular interactions were chosen for experimental alanine scanning to further characterize the interface and elucidate their role in protein-antibody interactions through measurement of binding affinities.
Residues Critical for Antibody Binding at the Protective Epitope of OspA
A series of alanine point mutations were introduced to OspA residues involved in the OspA/LA-2 interface at the 3 loops described above. The glycine and alanine at positions 208, 214 and 215 in OspA were mutated to lysine, to evaluate the effect of this charged residue at position 215 in the Borrelia garinii strain (Figure 2). Using a standard antibody capture technique (Materials and Methods), the affinity of LA-2 to OspA and engineered variants was determined by Surface Plasmon Resonance (SPR) analysis.
Figure 2.
Sequence alignment of OspA protein from three prevalent Borrelia genospecies including B. burgdorferi B31, B. afzelii BO23 and B. garinii PBi. Non-conserved amino acids that differ among species are in blue font. The three surface loops in the LA-2 recognition epitope, which were subjected to mutagenesis in this study, are highlighted in yellow.
OspA mutations A208K, N228A and N251A completely abolished binding with LA-2 (Figure 3). This result was confirmed with ELISA, using both the antigen direct coating as well as the antibody capture method (data not shown). In addition, K230A and T253A mutations decreased the affinity 2–7 fold compared to wild type OspA. While the amino acid sequence is conserved at positions N228, K230 and T253 across the three Borrelia strains, both B. garinii and B. afzelii have the changes A208Q and N251A relative to B. burgdorferi (Figure 2). Hence sequence differences at positions A208 and N251 may contribute to the loss of LA-2 recognition to other Borrelia strains.
Figure 3.
OspA residues important for LA-2 binding indicated on the protein structure, as revealed by the binding affinity results in the table. Residues with slightly decreased, worse, and better affinity to LA-2 when mutated are colored pink, red and green, respectively.
Intriguingly, mutations A215K, S229A, D249A and S250A of OspA enhanced the LA-2 binding affinity by 2–8 fold. Position 215 is already a lysine in B. garinii and the other three positions are completely conserved across the Borrelia strains, hence the increased LA-2 binding affinity observed in these mutants could potentially be exploited for cross-strain targeting.
Residues of LA-2 Antibody Critical for OspA Recognition
To identify residues that can be mutated to improve antibody affinity to OspA, a two-step strategy was used combining in silico predictions with experimental testing. In the first step, we used experimental Ala scanning to identify residues important for OspA interaction. Nine residues in the light and heavy chains located at the intermolecular interface were selected and mutated to alanine by site directed mutagenesis. Of these nine mutants, L100A-Heavy and L46A-Light either did not express properly or adopted an abnormal antibody conformation that disrupted binding activity with an anti-Fc antibody. The other seven mutants were expressed similar to WT levels and their binding to OspA measured by SPR analysis, resulting in data that enabled determination of fold changes with respect to wild type LA-2 (Figure 4). The H49A mutation in the LA-2 light chain led to complete loss of binding, while N52A-Heavy and Y32A-Light mutations resulted in decreased OspA binding by 3–4 fold. To determine if the change in affinity to OspA has an impact on the bactericidal activity of the antibody, the alanine mutants were tested in borreliacidal activity against B. burgdorferi. All mutants showed comparable borrelicidal activity as the wild type antibody, except H49A-Light, which did not bind OspA in our SPR assay (Supplementary Figure 1). Hence, detectable OspA binding by the antibody in vitro assays correlate with borreliacidal activity against B. burgdorferi.
Figure 4.
LA-2 residues important for OspA recognition indicated on the antibody structure, as revealed by the binding affinity results in the table. Color scheme is the same as in Figure 2, in that residues that decrease or increase affinity to LA-2 when mutated are colored red and green, respectively. N52, which increases or decreases affinity depending on the specific mutation introduced, is in blue.
In the second phase of design, we explored in silico additional mutations other than Ala that may enhance OspA–LA-2 binding affinity. To determine which calculated biophysical parameters are the best indicators of experimental affinity, experimental results from the first step above (Ala scanning) were compared with in silico predictions (Supplementary Figures 2 and 3). Changes in van der Waals interaction energy was the best predictor of affinity change, and guided the selection of other mutations in this second step. An exhaustive set of variants with individual mutations to all amino acid types at the interface residues were computationally generated, starting from the wild type structure. Mutations were introduced to all the positions mutated in the first phase, except H49-Light where Ala mutation completely abrogated binding. Changes in interaction parameters for each variant to OspA was predicted using the Prime MM-GBSA method (Yu et al., 2006), and the selected mutations were experimentally tested with SPR as before. Two non-alanine mutations in the heavy chain, S33R-Heavy and N52I-Heavy, and one light chain mutation, T53H-Light, led to improved OspA binding of the LA-2.
Overall, four OspA and five LA-2 mutations (Figures 3 and 4, green highlights) increased protein-antibody affinity compared to the wild type complex.
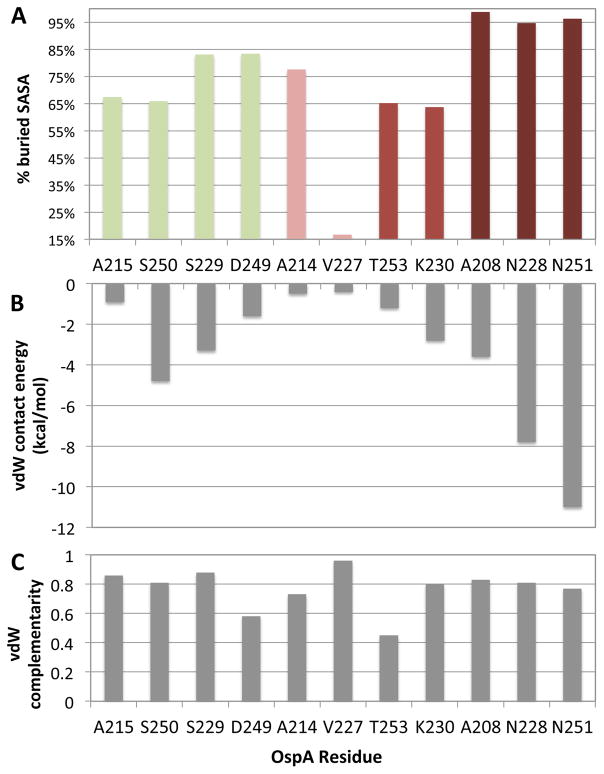
Residues with High Buried Surface Area Cannot Tolerate Mutations
Residues of the OspA protein and LA-2 antibody with experimental binding data (Figures 3 and 4) were further evaluated for their contribution to the binding interface by calculating the percent buried accessible surface area (% buried SASA), vdW contact energy, and vdW complementarity (Figures 5 and 6). OspA residues that completely abolish LA-2 binding when mutated (A208, N228, N251) have the highest percentage of buried SASA (darker red bars, Figure 5A). Of these three residues, N228 and N251 have extensive vdW contacts and two side chain hydrogen bonds each with the antibody as discussed above, which would be lost when they are replaced by an alanine and lead to complete loss of antibody binding. The remaining residue, A208, although not forming extensive interactions with the antibody (Figure 5B), is almost completely buried (Figure 5A) mostly within the protein itself, and other bulkier side chains including the Gln in B. afzelii and B. garnii (Figure 2), cannot be tolerated in the B. burgdorferi context. In agreement with these predictions, the reverse mutations A251N and Q208A in B. afzelii OspA abolished LA-2 binding in ELISA assays.
Figure 5.
Interaction of mutated OspA residues with LA-2 antibody evaluated in terms of (A) percent solvent accessible surface area (SASA) buried, (B) total van der Waals contact energy with the antibody and (C) complementarity of these vdW contacts. OspA residues are ordered on the horizontal axis from the best (green) to worst (ref) effect on LA-2 affinity when mutated, as in Figure 3.
Figure 6.
Interaction of mutated LA-2 residues with OspA protein evaluated in terms of (A) percent solvent accessible surface area (SASA) buried, (B) total van der Waals contact energy with the antibody and (C) complementarity of these vdW contacts. LA-2 residues are ordered on the horizontal axis from the best (green) to worst (red) effect on OspA affinity when mutated, as in Figure 4.
Similarly, antibody residue His49 on the light chain, which completely abolishes binding when mutated, has the highest percentage of buried SASA (darker red bar, Figure 6A) and extensive packing against OspA (Figure 6B). The other two residues that negatively affect OspA binding when mutated, Y32 on the light chain and N52 on heavy chain, are also characterized by more than 80% buried surface area and 3 kcal/mol contribution in vdW interactions with the protein. While the vdW complementarity fractions (Figures 5 and 6, panels C) did not seem to be correlated with effect on binding, high buried surface and vdW packing (panels A and B) were predictors of residues that cannot tolerate mutations at the binding interface.
Discussion
In this study, we investigated the Borrelia OspA–LA-2 antibody interface using in silico methods and in vitro experiments to characterize residue-level determinants that influence the formation and stability of this protein–antibody complex. Based on the X-ray crystal structure of the OspA-LA2 complex as the starting point (Li et al., 1997), an exhaustive set of mutants were generated that were prioritized for experimental testing, based on biophysical properties calculated in silico. The experimental results from in vitro affinity measurement techniques (SPR, ELISA) as well as cell-based borreliacidal assays revealed the functional importance of specific residues at the interface for both OspA and LA-2.
OspA residues in each of the three loop regions, A208 (loop 1), N228 (loop 2) and N251 (loop 3), are critical for LA-2 antibody recognition and binding (Figures 1 and 3). While N228 is conserved across the three Borrelia strains, A208 and N251 are different in B. burgdorferi compared to B. afzelii and B. garinii. This difference may be responsible for the specificity of the antibody to the B. burgdorferi OspA protein. We identified OspA mutations that both reduce (A214K, V227A, K230A, and T253A) and increase (A215K, S229A, D249A and S250A) the binding affinity to LA-2 (red and green in Figure 3, respectively). Intriguingly, A215K mutation, which introduces the amino acid present in the other two strains at this position, increases the binding affinity 7.5-fold. Identification of residues on the B. burgdorferi OspA epitope that can be mutated to modulate binding affinity suggests the opportunity to engineer the antibody for specific or cross-strain recognition. Using the B. burgdorferi OspA crystal structure as a template, we generated B. garinii and B. afzelii OspA homology models. These in silico models (available upon request) may provide a useful tool for structure-based design of antibodies and vaccines against Lyme disease.
The LA-2 mutagenesis indicates that the wild-type antibody does not have the strongest affinity for OspA. Mutations can be introduced, in both light and heavy chains, to improve the binding affinity between LA-2 and B. burgdorferi OspA. Residues S33 and N52 in the heavy chain, and T53 in the light chain can be mutated to substantially improve LA-2/OspA binding affinity (Figure 4). However, selecting the right mutation, as exemplified by the opposite effects from N52A and N52I mutations in the LA-2-Heavy chain, is critical to success. While these residues can tolerate mutations and present opportunities for optimization, some residues such as H49-Light are so essential for this interaction that any change is likely to completely abrogate binding as well as any borrelicidal effect. Similarly, N30 and Y32 in the light chain are key contributors to binding and any mutagenesis leads to worse binding affinities than the wild-type antibody. Thus, even when computational predictions suggest specific mutations that may enhance binding affinity, residues that are highly buried may not tolerate any mutations.
Our OspA and LA-2 mutagenesis results suggest challenges that should be overcome in targeting cross-strain OspA with a fairly small subset of mutations in LA-2. Challenges will arise in cases where the antibody mutated to increase the affinity to a particular strain has a lower binding affinity to another OspA protein than wild-type LA-2, thus requiring multiple rounds of optimization and possibly compensatory mutations to enhance the affinity toward the latter strain. Intriguingly, any level of detectable binding, as observed with Surface Plasmon Resonance, was sufficient to exert a borrelicidal effect. This result, coupled with combinatorial mutagenesis, wherein the affinity-enhancing mutations are introduced alongside mutations that enable cross-strain targeting, promises to be a valid strategy for developing future LA-2 variants that are borrelicidal and have binding affinities that may approach wild-type LA-2.
In conclusion, our study highlights the role of specific residues in the OspA/LA-2 interaction and provides insight into potential strategies for modulating their binding affinity. These findings have implications for expanding the application of LA-2 derived antibodies to OspA proteins from other Borrelia strains and developing novel prophylactic biologics for Lyme disease.
Supplementary Material
Acknowledgments
Funding information
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1-TR001453. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- Banks JL, Beard HS, Cao Y, Cho AE, Damm W, Farid R, Felts AK, Halgren TA, Mainz DT, Maple JR, Murphy R, Philipp DM, Repasky MP, Zhang LY, Berne BJ, Friesner RA, Gallicchio E, Levy RM. Integrated Modeling Program, Applied Chemical Theory (IMPACT) J Comput Chem. 2005;26:1752–1780. doi: 10.1002/jcc.20292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard H, Cholleti A, Pearlman D, Sherman W, Loving KA. Applying physics-based scoring to calculate free energies of binding for single amino acid mutations in protein-protein complexes. PLoS One. 2013;8:e82849. doi: 10.1371/journal.pone.0082849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding W, Huang X, Yang X, Dunn JJ, Luft BJ, Koide S, Lawson CL. Structural identification of a key protective B-cell epitope in Lyme disease antigen OspA. J Mol Biol. 2000;302:1153–1164. doi: 10.1006/jmbi.2000.4119. [DOI] [PubMed] [Google Scholar]
- Golde WT, Piesman J, Dolan MC, Kramer M, Hauser P, Lobet Y, Capiau C, Desmons P, Voet P, Dearwester D, Frantz JC. Reactivity with a specific epitope of outer surface protein A predicts protection from infection with the Lyme disease spirochete, Borrelia burgdorferi. Infect Immun. 1997;65:882–889. doi: 10.1128/iai.65.3.882-889.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson MP, Friesner RA, Xiang Z, Honig B. On the role of the crystal environment in determining protein side-chain conformations. J Mol Biol. 2002;320:597–608. doi: 10.1016/s0022-2836(02)00470-9. [DOI] [PubMed] [Google Scholar]
- Jacobson MP, Pincus DL, Rapp CS, Day TJ, Honig B, Shaw DE, Friesner RA. A hierarchical approach to all-atom protein loop prediction. Proteins. 2004;55:351–367. doi: 10.1002/prot.10613. [DOI] [PubMed] [Google Scholar]
- Johnson BJ, Sviat SL, Happ CM, Dunn JJ, Frantz JC, Mayer LW, Piesman J. Incomplete protection of hamsters vaccinated with unlipidated OspA from Borrelia burgdorferi infection is associated with low levels of antibody to an epitope defined by mAb LA-2. Vaccine. 1995;13:1086–1094. doi: 10.1016/0264-410x(95)00035-y. [DOI] [PubMed] [Google Scholar]
- Li H, Dunn JJ, Luft BJ, Lawson CL. Crystal structure of Lyme disease antigen outer surface protein A complexed with an Fab. Proc Natl Acad Sci U S A. 1997;94:3584–3589. doi: 10.1073/pnas.94.8.3584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozen A, Haliloglu T, Schiffer CA. HIV-1 Protease and Substrate Coevolution Validates the Substrate Envelope As the Substrate Recognition Pattern. J Chem Theory Comput. 2012:8. doi: 10.1021/ct200668a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poland GA. Vaccines against Lyme disease: What happened and what lessons can we learn? Clin Infect Dis. 2011;52(Suppl 3):s253–258. doi: 10.1093/cid/ciq116. [DOI] [PubMed] [Google Scholar]
- Schaible UE, Kramer MD, Eichmann K, Modolell M, Museteanu C, Simon MM. Monoclonal antibodies specific for the outer surface protein A (OspA) of Borrelia burgdorferi prevent Lyme borreliosis in severe combined immunodeficiency (scid) mice. Proc Natl Acad Sci U S A. 1990;87:3768–3772. doi: 10.1073/pnas.87.10.3768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro ED. Lyme disease. N Engl J Med. 2014;371:684. doi: 10.1056/NEJMc1407264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigal LH, Zahradnik JM, Lavin P, Patella SJ, Bryant G, Haselby R, Hilton E, Kunkel M, Adler-Klein D, Doherty T, Evans J, Molloy PJ, Seidner AL, Sabetta JR, Simon HJ, Klempner MS, Mays J, Marks D, Malawista SE. A vaccine consisting of recombinant Borrelia burgdorferi outer-surface protein A to prevent Lyme disease. Recombinant Outer-Surface Protein A Lyme Disease Vaccine Study Consortium. N Engl J Med. 1998;339:216–222. doi: 10.1056/NEJM199807233390402. [DOI] [PubMed] [Google Scholar]
- Stanek G, Wormser GP, Gray J, Strle F. Lyme borreliosis. Lancet. 2012;379:461–473. doi: 10.1016/S0140-6736(11)60103-7. [DOI] [PubMed] [Google Scholar]
- Van Hoecke C, Lebacq E, Beran J, Parenti D. Alternative vaccination schedules (0, 1, and 6 months versus 0, 1, and 12 months) for a recombinant OspA Lyme disease vaccine. Clin Infect Dis. 1999;28:1260–1264. doi: 10.1086/514779. [DOI] [PubMed] [Google Scholar]
- Yu Z, Jacobson MP, Friesner RA. What role do surfaces play in GB models? A new-generation of surface-generalized born model based on a novel gaussian surface for biomolecules. J Comput Chem. 2006;27:72–89. doi: 10.1002/jcc.20307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu K, Day T, Warshaviak D, Murrett C, Friesner R, Pearlman D. Antibody structure determination using a combination of homology modeling, energy-based refinement, and loop prediction. Proteins. 2014;82:1646–1655. doi: 10.1002/prot.24551. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.