Abstract
Few reports of educational and counseling support resources exist for Lynch syndrome (LS), a disorder requiring multi-organ cancer screening and specialized medical care throughout adult life. Here we describe the development and efficacy of two resources designed to address this need, the Memorial Sloan Kettering Cancer Center Clinical Genetics Service annual Lynch Syndrome Educational Workshop (LSEW), and a quarterly Lynch Syndrome Patient Advocacy Network (LSPAN) support group. The LSEW and LSPAN were implemented beginning in 2012. Participant survey data evaluating satisfaction, clarity, and unmet needs for each event were retrospectively analyzed and summarized using descriptive statistics. Annual LSEW attendance ranged from 53 to 75 total participants. LSEW year 1 participants indicated a need for a support group, and preferred in-person meetings at a frequency of every 3–6 months. For LSEW year 2–5 participants, >96 % reported satisfaction with the LSEW, and >82 % expressed interest in secure online support. Common themes for improvement included increased time for question and answer sessions and additional introductory genetics education. Responding LSPAN participants (n = 57 total survey responses in 11 meetings) found the meetings helpful (100 %), information clear (91 %), and presence of a genetic counselor useful (67 %). Desired discussion topics included coping with stress and anxiety, development of a support network, family communication about LS, genetic testing decisions, and bereavement. Following genetic counseling, a need exists for ongoing educational and emotional support in LS. Implementation of resources such as the LSEW and LSPAN is feasible and perceived as helpful by participants.
Keywords: Lynch syndrome, Hereditary cancer, Family support, Genetic counseling, Colorectal cancer
Introduction
Lynch syndrome (LS) is an autosomal dominant cancer predisposition syndrome resulting from a germline mutation in one of the DNA mismatch repair (MMR) genes (Akiyama et al. 1997; Liu et al. 2001; Lynch et al. 1966; Miyaki et al. 1997). LS accounts for 3 % of all colon cancers, making it the most common hereditary form of colorectal cancer (Lynch and de la Chapelle 2003). Individuals with LS have up to a 70 % lifetime risk of developing colorectal cancer as well as an increased risk for other cancers including endometrial, ovarian, stomach, small intestine, upper urinary tract, and pancreas cancer (Aarnio et al. 1999; Bonadona et al. 2011; Dunlop et al. 1997; Kastrinos et al. 2009; Vasen et al. 1999; Yu et al. 2003). Consequently, disease management in LS is complex and involves commitment to multi-organ cancer surveillance and consideration of risk-reducing strategies, including prophylactic surgery, throughout adult life. The impact of LS on a patient's life is substantial, as one's cancer risk must be managed in the context of personal health concerns and risk for family members, often in the background of prior family illness and loss. These unique challenges necessitate both educational and emotional support systems to facilitate coping and living with LS.
Although genetic testing for LS provides clarity regarding family cancer history and a plan for preventive and specialized medical care, a positive genetic test result can also present many new challenges. Communication with family members about genetic status and associated cancer risks is difficult and may result in conflicting feelings of wanting to discuss familial cancer risk but without imparting anxiety or fear (Keller et al. 2008; Murakami et al. 2004). These discussions also can be accompanied by feelings of guilt (Hughes and Phelps 2010; McKinnon et al. 2007; Speice et al. 2002). Furthermore, a diagnosis of LS may have implications for an individual's global well-being. In a study of psychological distress after disclosure of genetic test results, 7 % of LS patients met criteria for minor depression and 5 % for post-traumatic stress symptoms at one-month follow-up (Murakami et al. 2004). Individuals with LS have also been found to experience a transient increase in depression and anxiety after receiving a positive genetic test result (Galiatsatos et al. 2015). Many individuals have reported feeling isolation, uncertainty, anxiety, and anger resulting from their genetic diagnosis (McKinnon et al. 2007). Individuals' psychological responses to LS genetic testing can have implications for their health behaviors; for example, among patients with LS, fear of dying soon was associated with non-compliance with cancer screenings (Aktan-Collan et al. 2013). For LS patients, finding continued support and understanding to manage these emotional challenges can be difficult given the rarity of the diagnosis. While genetic counseling remains the main venue for obtaining disease-related information as well as initial psychosocial support, it does not provide for a structure of long-term support and follow-up.
Continued educational and counseling support concerning disease, risk reduction, and screening options is beneficial to patients with specific medical diagnoses (Goodwin et al. 2001; Landsbergen et al. 2010; Plumridge et al. 2012; Spiegel et al. 1989). Dr. Henry T. Lynch, often referred to as the father of hereditary cancer prevention and detection and one of the first to have characterized LS, implemented a Family Information Service, which offers an effective personalized approach to providing education and counseling to extended families with hereditary cancer (Lynch 2001). Educational conferences, retreats, and support groups are effective for updating disease knowledge and improving adjustment and feelings of control in patients with cancer and hereditary cancer risk (Dunkel-Schetter 1984; McKinnon et al. 2007; Montazeri et al. 2001). Evidence suggests that informational support may be more helpful when supplemented with emotional and psychosocial resources (Landsbergen et al. 2010). Peer support groups provide a venue for open discussion amongst individuals facing similar situations and enable the exchange of information, mutual support and coping resources. They can create a sense of normalization, reduce feelings of undesirable emotions, as well as indirectly improve family communication by increasing confidence and stimulating discussion (Emilsson et al. 2012; Plumridge et al. 2012; Werner-Lin 2008).
Such support systems have been described in the literature for individuals with cancer as well as for carriers of BRCA1/2 mutations (Arrington 2010; Bell et al. 2010; Dunkel-Schetter 1984; Emilsson et al. 2012; Esplen et al. 2004; Hughes and Phelps 2010; Kwok and Ho 2011; McGovern et al. 2002; McKinnon et al. 2007; Speice et al. 2002; Stanton et al. 2005; Weis 2003; Werner-Lin 2008), but reports of sources for LS are limited. In one existing study of family communication in LS, relatives who received educational resources had higher likelihood of following up with a doctor, seeing a genetic counselor, and pursuing genetic testing (Dilzell et al. 2014). This underscores the importance of providing a venue through which both patients and their families can receive information on LS and the potential impact on seeking out genetic testing and proactive medical care. A study of a daylong interactive multidisciplinary conference for LS successfully met patient-reported informational needs in clinical care and research, but additional needs were identified for support groups and education about surveillance, protection, and nutrition (Bannon et al. 2014). Such findings highlight the need for continued education as well as peer psychosocial support.
To address the need for psychosocial and educational support in LS, the Clinical Genetics Service (CGS) at Memorial Sloan Kettering Cancer Center (MSKCC) implemented a large-scale annual Lynch syndrome educational workshop (LSEW) and the Lynch Syndrome Patient Advocacy Network (LSPAN), a small-scale quarterly peer support group, to supplement individualized genetic counseling services. The LSEW is a multidisciplinary venue providing updated information, focusing on surveillance, risk reduction, surgical options, and research. The LSPAN provides the opportunity for mutual support amongst patients with the same rare diagnosis in a personal, regularly occurring and professionally led environment. Here, we report on our experience with the organization and delivery of these two LS support resources, patient-reported satisfaction and utility, and areas in which further provision of support is needed.
Methods
The LSEW was implemented in response to MSKCC CGS patient requests noted during clinical genetic counseling sessions. The LSEW began in March 2012. It and subsequent LSEWs occurred annually in honor of Lynch Syndrome International Awareness Day, March 22, and also coincided with Colorectal Cancer Awareness Month. The LSPAN began in November 2012. Meetings took place quarterly, with one meeting each year replaced by the LSEW (3 LSPAN meetings per year in total). LSPAN was designed in response to patient feedback gathered through a Support Group Needs Assessment (SGNA) survey instrument administered in LSEW year 1 (LSEW1). The LSEW and LSPAN are ongoing.
The LSEW and LSPAN were offered to MSKCC CGS patients with LS in clinical practice and evaluated through retrospective analysis of survey data collected for the intended purpose of improving clinical resources for patients and their families with LS. All survey instruments were designed by the planning committee for clinical utility and program development, not to assess patient outcomes. Surveys were composed of multiple choice, ranking, Likert scale measures, and free response items to assess satisfaction, informational and emotional needs of participants. An MSKCC Institutional Review Board approval was obtained for retrospective analysis of collected data.
Participants
Eligible participants for the LSEW1 were identified through a query of the MSKCC CGS genetic testing database for all living patients with LS, defined by having a known deleterious mutation in one of the MLH1, MSH2, MSH6, or PMS2 DNA MMR genes. Patients with variants of unknown significance were excluded. The list of eligible patients was reviewed by the genetic counselors to ensure verified diagnosis and survival status. Eligible patients were then mailed an invitation to the workshop. This process was repeated for all subsequent annual LSEWs, including 2013 (LSEW2), 2014 (LSEW3), 2015 (LSEW4), and 2016 (LSEW5). The LSEWs were also open to family members as guests of index LS patient attendees.
Eligible patients for LSPAN were identified in the same fashion as the LSEW. Mail invitations were sent once per year and included the schedule for all quarterly LSPAN meetings in that year. Meeting reminders for the LSPAN meetings in that year were sent to participants via secure email. The LSPAN was open to MSKCC CGS counseled patients only in order to ensure that all participants had been given the same general information and thus any common questions or misunderstandings could be corrected. Spouses were permitted when index patients brought them for support; this occurred in the LSPAN1 and LSPAN10.
MSKCC CGS patients receiving a diagnosis of LS after the yearly invitation mailing was sent were informed by their genetic counselors of both support resources and were also given a verbal or written invitation at the time of their result disclosure appointment. These patients were also added to the list for future invitation mailings and email communications. Each mail and email correspondence provided the option to opt-out of future LSEW and LSPAN communications.
Organization and Assessments
Educational Workshop
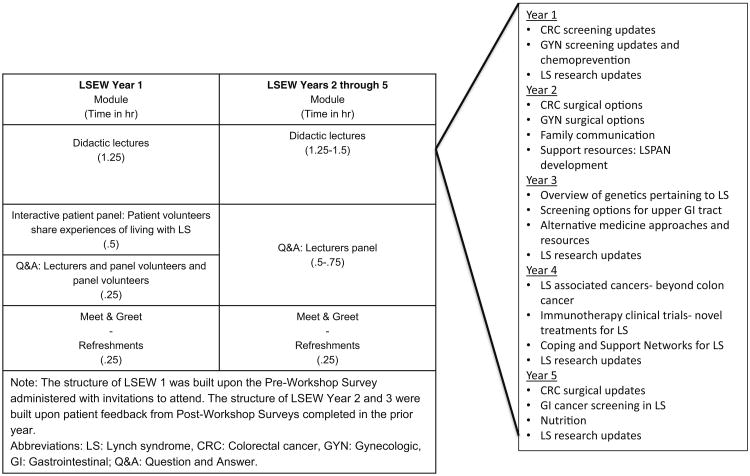
The planning committee was assembled prior to the LSEW1 in 2012 and was made up of two attending physicians, CGS genetic counselors, one patient and family advisory council member, and three research study assistants. The committee organized all LSEWs. Each LSEW took place during a weekday, in the evening after work hours, was 2.5 h in duration, and consisted of 3–4 didactic lectures, followed by a question and answer (Q&A) session and light refreshments. Lectures were given by practicing attending physicians and other medical professionals with expertise in managing LS at MSKCC and other local institutions on various LS-related topics (Table 1).
Table 1. LSEW content and organization in years 1-3.
LSEW didactic lectures were video-recorded and subsequently made available on the MSKCC CGS website. The patient panel in LSEW1 and Q&A in LSEW1 and 2 were not recorded to protect patient identities. In year 3, the Q&A was conducted using anonymized note cards and was included in the video recording for the MSKCC CGS website.
A Pre-Workshop Survey (Pre-WS) instrument was developed by the planning committee and administered prior to the LSEW1, included with the invitation mailing, to assess lecture topics of greatest interest to LS patients. Though family members could attend the LSEW, only index LS patients were asked to complete the Pre-WS. Respondents were asked to rank their interest in the following: cancer screening recommendations; chemoprevention; communication with adult family members about test results; communication with children about LS; family planning; personal testing decision and timing of testing; development of a support network; and bereavement. The second item asked invitees to suggest additional topics of interest through free response. The third item gave respondents the opportunity to volunteer to participate in and speak on a patient panel. Data collected from the Pre-WS were utilized to delineate lecture topics, identify speakers, and assemble the volunteer patient panel. LS patient panel volunteers signed a general HIPAA release form.
Index LS patients attending LSEW1 were also asked to complete a Support Group Needs Assessment (SGNA) instrument, which was designed by the planning committee and evaluated patient/family interest in and need for a peer support group as well as preferences for the structure of such a group (e.g., in person versus virtual meetings; meeting frequency; integration of ages, genders, cancer and treatment history; and topic-focused versus free-flowing discussions). These responses were considered in developing the LSPAN.
Following each LSEW, all workshop attendees (index LS patients and their guests) were also asked to complete a Post-Workshop Survey (Post-WS) instrument, through which respondents could evaluate overall satisfaction with the workshop, its organization, clarity of information presented, suggestions for future lectures, and areas needing improvement. Data collected from the Post-WS were used to evaluate workshop utility and to organize content of subsequent LSEWs.
Support Group
Data collected through the SGNA during LSEW1, as described above, were used to design the LSPAN support group, resulting in an in-person, quarterly occurring meeting with index LS patient participants mixed with respect to age, gender, and cancer history. Each LSPAN was led by a MSKCC medical social worker specializing in oncology and attended by a CGS genetic counselor. The social workers did not have specific expertise in LS and, as such, they attended genetic counseling sessions to familiarize themselves with LS and the genetic counseling process prior to initiation of the LSPAN. To accommodate patients with daytime jobs, LSPANs took place during a weekday evening and were held at the MSKCC New York City campus. Each meeting was approximately 1.5 hours in duration.
Although the LSPAN was not expressly modeled after an existing framework, the structure of the group was most similar to a drop-in rolling model (Bauld et al. 2012; Berger 1984) allowing participants to attend or not attend meetings freely. Group meetings were structured yet supportive (Fawzy et al. 1993). LSPANs were psychoeducational (Bultz et al. 2000) in that the facilitator prepared and discussed specific skills for coping. LSPANs also shared elements with the supportive/expressive model, which has been utilized in psychosocial support groups for other populations, including breast cancer (Classen et al. 2001; Goodwin et al. 2001; Spiegel et al. 1989; Spiegel and Spira 1991). Greater detail regarding the group process is described in the Discussion.
For the first 5 meetings, discussion topics were chosen ahead of time and consisted of: (1) stress and anxiety; (2) coping strategies; (3) development of a support network; (4) communication with family members and children about LS; and (5) genetic testing decision and timing of testing. For remaining meetings, participants shaped the discussion, as it seemed to flow freely without the need for a pre-assigned topic. Prompts were prepared by the facilitator and included for example, ways in which an LS diagnosis impacts lifestyle choices, seeking accurate and helpful information on LS, communication, dating and disclosure, and anxiety surrounding annual screenings.
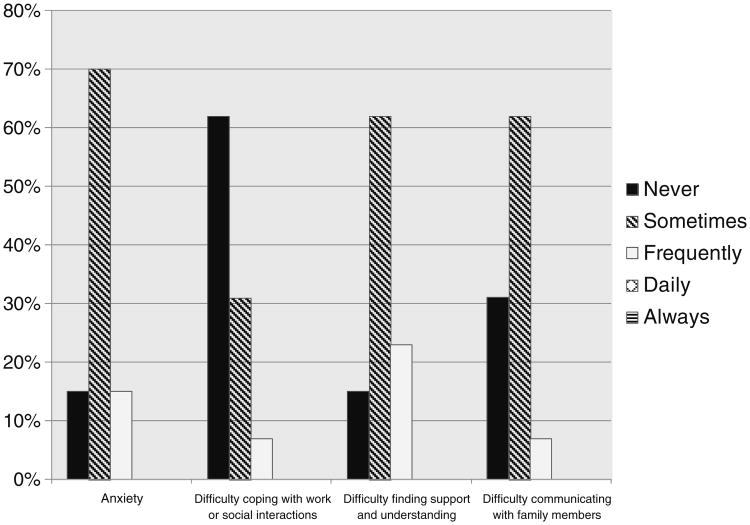
At the conclusion of each LSPAN meeting, all participants completed a Post-Support Group Survey (Post-SGS) instrument to rate: (1) clarity of information presented; (2) helpfulness of meeting; (3) group leader; (4) whether expectations were met; and (5) to provide suggestions for improvement. One Post-SGS also included a Psychosocial Aspects of LS Assessment instrument, which was developed by the planning committee and asked respondents to rank frequency of the following regarding their LS diagnosis: feeling anxiety; difficulty communicating with family members; difficulty finding support/understanding; and difficulty with social or work situations. This assessment was conducted to understand the makeup of the group on a spectrum of feelings in order to best address participants' needs. Another Post-SGS additionally assessed LS patients' preferred methods of receiving LSPAN communications. These items were of specific interest to the planning committee for directing further development of future LSPANs.
Data Analysis
Data used for retrospective analysis of the LSEW were collected in the Pre-WS and Post-WS evaluations. Data used for retrospective analysis of the need for and utility of the LSPAN were collected in the SGNA and Post-SGS evaluations (including the Psychosocial Aspects of LS Assessment). These data were summarized using descriptive statistics to assess the utility and helpfulness of the LSEW and LSPAN to participants as well as their ongoing unmet needs.
Results
Educational Workshop
The content and organization of each LSEW is detailed in Table 1, while the number of index LS patients invited, workshop participation, and satisfaction with various aspects of the LSEWs are detailed in Table 2. Respondent feedback to the LSEW was generally positive. In the LSEW1 Pre-WS survey instrument, 8 discussion topics were offered and the most desired topics were chemoprevention and cancer screening recommendations. Thus, lectures focused on these topics plus recent updates in LS research (Table 1). Common suggestions for future lecture topics included surgical and hormonal considerations for organs at risk in LS and family communication strategies. Common requests for improvement included separating the educational and emotional support aspects (e.g., lectures versus patient panel of experiences) and increasing the time for Q&A. Expression of these preferences led to the elimination of the patient panel in favor of a longer Q&A session in subsequent LSEWs and to the implementation of a separate peer support group (i.e., the LSPAN).
Table 2. LSEW participation and participant satisfaction in years 1–3.
| LSEW1 | LSEW2 | LSEW3 | LSEW4 | LSEW5 | |
|---|---|---|---|---|---|
| No. index LS patients invited | 213 | 232 | 284 | 336 | 361 |
| No. participants | 75 | 53 | 74 | 60 | 58 |
| Completed Post-WS (%) | 26 (35 %) | 23 (42 %) | 32 (43 %) | 22 (37 %) | 23 (40 %) |
| Overall organization of workshop | 100 % | 96 % | 100 % | 100 % | 100 % |
| Clarity of information presented | 96 % | 91 % | 88 % | 100 % | 96 % |
| Amount of information presented | 88 % | 91 %+ | 94 % | 100 % | 100 % |
| Clarity of responses during the Q&A session | 88 % | 78 %+ | 88 % | 100 % | 100 % |
| Technicality of information presented | N/A | 87 % | 91 % | 91 % | 91 % |
| Attended previous MSKCC events | N/A | 48 % | 52 % | 82 % | 57 %* |
| Interest in secure online support | N/A | 95 % | 90 % | 82 % | 87 % |
| Interest in patient matched telephone communication | N/A | N/A | 62 % | N/A | N/A |
Data collected from Post Workshop Survey in LSEW years 1–3. % indicates patients that were satisfied or extremely satisfied;
Accounts for responses left blank; n = 1 and n = 4 left blank in response to amount of information presented and clarity of responses during Q&A, respectively;
specifically indicated having attended a prior LSEW or LSPAN
No. number, LS Lynch syndrome, Q&A question and answer, N/A not assessed
For LSEW2, nearly all the responders were satisfied or extremely satisfied with the overall organization of the LSEW; however, we noted that only 87 % were satisfied or extremely satisfied with the technicality of information presented and 78 % were satisfied with the clarity of responses during Q&A. Some free response data indicated that the level of detail presented regarding surgical options could be intimidating and difficult for some attendees to understand. The most preferred topics suggested for the next year's workshop included a basic genetics review of LS, screening recommendations, updates on more rare LS associated cancers (e.g., urinary tract and small bowel), and the role of nutrition, dietary supplements, and complementary/alternative medicine in cancer prevention and treatment. Respondents most appreciated information about new treatments, detailed presentations, strategies for speaking with their children, visual aids, extended length of Q&A, and learning about the new LSPAN support group. Common requests for improvement included a desire for still more basic genetics information, greater clarification of implications for statistics presented, and even more time for Q&A.
For LSEW3, we focused on ensuring that the technicality of the information presented was improved based on the LSEW2 responses. The organizers ensured that the speakers for each topic were familiar with the audience and that medical vocabulary and concepts were appropriately introduced. In fact, among our LSEW3 responders, satisfaction with amount, clarity, and technicality of information presented were increased from the LSEW2 (Table 2). Through free response items, patients expressed an appreciation for new knowledge and discussion of patient requested topics from the year prior, and identified a need for repeated review of basic LS genetics and further ongoing emotional support through LSPAN.
In the LSEW4 and 5, survey results continued to be generally favorable. Of note, 82 % of respondents in LSEW4 had attended prior MSKCC events, and 57 % of respondents in LSEW5 had attended a prior LSEW or LSPAN. Respondents in these LSEWs expressed appreciation for clarity of descriptions, inclusion of nutrition information, updates on research and novel therapies (e.g., immunotherapy), and information on psychosocial support. Common requests included more updates on research and treatments for LS related cancers, coping with outcomes of prophylactic surgery for LS (e.g., colectomy), and discussing LS with family and especially children.
A majority of respondents in LSEW2 through 5 expressed interest in a secure online communication forum for individuals with LS, and 71 % of respondents in LSEW3 indicated willingness to volunteer in the program and complete a 30-minute training (Table 2).
Support Group
Design of LSPAN was informed by SGNA response data collected during LSEW1 (n = 23 respondents), in which 73 % of respondents felt a support group would be somewhat useful or extremely useful and 57 % felt a support group would have increased utility immediately following genetic testing. A total of 87 % of respondents preferred an in-person versus a virtual venue, and 73 % preferred a meeting frequency of every 3–6 months versus monthly.
Data collected through LSPAN are summarized in Table 3 and Table 4. Across 11 LSPAN sessions, patient evaluations of the clarity of information presented, helpfulness of the meeting, rating of the group leader, and the meeting of expectations were generally quite favorable. The development of an online communication forum was again a common request.
Table 3. Survey Items for ongoing LSPAN Development.
| Meeting assessed | Question | n | Result |
|---|---|---|---|
| LSPAN1 | Ever diagnosed with cancer | 13 | Yes 62 % |
| No 38 % | |||
| LSPAN1 | Undergoing or planning cancer treatment | 13 | Yes 0% |
| No 100 % | |||
| LSPAN2 | Preferred method of contact | 12 | Email 92 % |
| Phone 8 % | |||
| Mail 0 % | |||
| Other 0 % | |||
| LSPAN2 | Usefulness of having a genetic counselor present during support group sessions | 12 | Very useful 33 % |
| Useful 33 % | |||
| Somewhat useful 8 % | |||
| Not useful 25 % | |||
| LSPAN2 | Comfort level with having a genetic counselor present during support group sessions | 12 | Very comfortable 67 |
| Comfortable 25 % | |||
| Somewhat comfortable 8 % | |||
| Not comfortable 0% |
These items aided the development of LSPAN and were assessed in Post-Meeting Surveys from Lynch Syndrome Patient Advocacy Network Meetings 1 and 2
LSPAN Lynch Syndrome Patient Advocacy Network
Table 4. Overall Participant Satisfaction with LSPAN.
| Clarity of information presented | Helpfulness of meeting | Rating of group leader | Expectations | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||
| LSPAN Meeting | Clear | Somewhat clear | Not applicable | Very helpful | Helpful | Somewhat helpful | Excellent | Good | Exceeded | Met | Somewhat met |
| 1: Nov 2012 (n = 13) | 85 % | 15 % | 0% | 77 % | 23 % | 0% | 69 % | 31 % | 62 % | 23 % | 8% |
| 2: Feb. 2013 (n = 13) | 100 % | 0% | 0% | 85 % | 15 % | 0% | 77 % | 23 % | 38 % | 54 % | 8% |
| 3: May 2013 (n = 8) | 100 % | 0% | 0% | 63 % | 38 % | 0% | 75 % | 25 % | 50 % | 38 % | 13 % |
| 4: Sep. 2013 (n = 8) | 88 % | 13 % | 0% | 75 % | 25 % | 0% | 88 % | 13 % | 50 % | 50 % | 0% |
| 6: Jun 2014 (n = 5) | 100 % | 0% | 0% | 60 % | 40 % | 0% | 100 % | 0% | 20 % | 60 % | 20 % |
| 7: Sep. 2014 (n = 4) | 50 % | 25 % | 25 % | 50 % | 25 % | 25 % | 75 % | 25 % | 33 %* | 67 %* | 0 %* |
| 8: Dec 2014 (n = 3) | 100 % | 0% | 0% | 67 % | 33 % | 0% | 67 % | 33 % | 33 % | 67 % | 0% |
| 9: Jun 2015 (n = 6) | 83 % | 17 % | 0% | 17 % | 50 % | 33 % | 83 % | 17 % | 0% | 83 % | 17 % |
| 10: Sep. 2015 (n = 8) | 100 % | 0% | 0% | 38 % | 63 % | 0% | 63 % | 38 % | 13 % | 88 % | 0% |
| 11: Dec 2015 (n = 2) | 100 % | 0% | 0% | 50 % | 50 % | 0% | 100 % | 0% | 50 % | 50 % | 0% |
| MEAN | 91 % | 7% | 3% | 58 % | 36 % | 6% | 80 % | 20 % | 35 % | 58 % | 6% |
Survey data from LSPAN5 (Dec 2013, n = 3) unavailable. 0 % of participants rated clarity of information as unclear, helpfulness of meeting as somewhat or not helpful, group leader as fair or poor, and expectations as not met.
1 respondent left “expectations” blank, % is out of n = 3
All attendees of LSPAN1 also completed the Psychosocial Aspects of LS Assessment. These results are summarized in Fig. 1. Participants' comfort level with and perceived helpfulness of a genetic counselor's presence as well as preferred methods of contact, cancer status, and treatment status were also surveyed and are summarized in Table 3.
Fig. 1.
Psychosocial Aspects of LS Assessment. Patient reported frequency of feelings resulting from LS diagnosis (n = 13). Figure generated from Post-Support Group Survey data collected at the first LSPAN meeting (LSPAN1)
Discussion
This study is the first to provide and examine a comprehensive informational and psychosocial support system for LS patients and their families. Although reports of educational conferences, retreats, and peer support groups exist for patients with cancer and other genetic conditions, few such resources have been described for LS. A previous study showed positive outcomes in meeting the educational needs of LS patients through a one-time multidisciplinary conference, but underscored the necessity for continued provision of updated information and additional psychosocial support (Bannon et al. 2014). This study provides methodology for organizing both an ongoing educational workshop (LSEW) and peer support group (LSPAN) to address these needs, and accounts for patient preferences in organization and specific disease knowledge. Results highlight the need for disseminating a diverse range of educational topics in LS including basic genetics, detailed updates in screening, prevention, treatment, and research as well as psychosocial resources. Specific aspects of psychosocial support that must be addressed in peer support groups for LS have also been described (e.g., anxiety, difficulties in finding understanding of one's diagnosis, communication with family, and interference with occupation and social life). Individuals utilizing the LSEW and LSPAN are generally satisfied and perceive them to be helpful.
Educational Workshop
Overall, patients expressed a high level of satisfaction with the LSEW organization and information presented in all 5 LSEWs. Based on data collected in LSEW2, we observed slightly lower patient satisfaction with the technicality of information presented and clarity of Q&A responses compared to other measures of satisfaction with the workshop. Topics in LSEW2 were heavily based on surgical approaches and screening procedures, which may be challenging for clinicians to address comprehensively without a substantial baseline fund of medical vocabulary and detail. Provision of information on such complex topics thus may require explicit definition as well as simplified description of potentially new terms to engage individuals with varying degrees of medical knowledge. Correspondingly, respondents expressed a desire for repeated basic genetics information pertaining to LS, which was then provided in LSEW3. Interestingly, increased satisfaction with workshop technicality was observed in LSEW3 compared to LSEW2, which could be partly attributed to providing this foundation. A general overview of LS and related genetics is necessary prior to addressing more complex issues such as surgery, chemoprevention, risk reduction, and screening to provide a background for additional knowledge. This is particularly important when participants may have undergone genetic counseling several years prior and guests of patients may not have had genetic counseling or testing. To ensure an appropriate amount of genetics review and level of medical detail, a planning committee must carefully review lecture content prior to their presentation.
The Q&A session is highly valued by patients, as evidenced by multiple requests for increased Q&A time. Given the amount and variety of information presented, adequate time for questions must be given to address uncertainties and misconceptions. This observation supports that discussions triggered by individual concerns could become informational to the whole group, improving educational efficiency of the meeting.
Support Group
A separate quarterly support group meeting was implemented to help LS patients in need of further emotional guidance, and was designed to accommodate patient preferences for separation between didactic and psychosocial resources per SGNA survey data. Respondents expressed a preference for gender, age, cancer history, and treatment history-mixed participants. This promotes discussion of varying experiences and perspectives, and enables diversified mutual support. Consistent with previous literature (Esplen et al. 2004; Hughes and Phelps 2010; McKinnon et al. 2007), we have not observed any adverse consequences from these inclusion criteria.
Each LSPAN meeting began with a brief welcome. The social worker facilitated introductions, asking everyone to briefly tell what brought them to the group that day, allowing each participant to tell their story of being diagnosed with LS, cancer if relevant, and any other details they wished to share. Participants would tell their own stories, often sharing emotional dimension with others and discussing both negative and positive feelings. Prompts proposed by the facilitator provided a springboard for discussion, Q&A, and open forum sharing/ psychosocial support. Common themes included sharing the history of one's diagnosis and impact on one's children, details of deciding when to pursue genetic testing, effective methods of communicating with family, and differing experiences between members of a family. Sometimes a patient would present a personal dilemma, such as consideration of risk-reducing total abdominal hysterectomy/bilateral salpingo-oophorectomy, asking for input and inquiring about the experiences of others.
Some individuals came to all or most meetings, and others came one or a few times. The group seemed to become more cohesive with regular members becoming familiar with each other, and welcoming new ones. The group seemed comfortable with open-ended discussion, and discussion flowed freely, facilitated by the experienced social worker. The genetic counselor deliberately took a passive role. The facilitator's emphasis was on encouraging the open expression of feelings in an emotionally supportive environment, and maintaining the focus on psychosocial needs rather than individual genetic counseling issues. When it was perceived that medical/genetic information was important to the discussion, the counselor provided this information and the conversation was quickly re-directed back to psychosocial aspects. Patients were referred back to their own counselor if seeking advice regarding personal medical care or genetic counseling.
Contact was encouraged between meetings. Patients seemed to be exchanging contact information on their own, suggesting extension of the support network beyond LSPAN meetings. The provision of specific coping skills, flexibility in free-flowing discussion, and the ability of the group to “normalize” patients' experiences with LS by connecting them with other members of the LS community appeared to be the most helpful to the entire group. Participants found it to be a place where they share information, receive psychoeducation, and support on their experiences with LS.
Overall, participants reported a high level of satisfaction and perceived helpfulness of LSPAN. The respondents reported feelings of anxiety and difficulty in finding understanding regarding one's diagnosis, which is consistent with existing literature in other hereditary cancer syndromes (Hughes and Phelps 2010; Landsbergen et al. 2010; Speice et al. 2002; Werner-Lin 2008). Although most respondents reported that their diagnosis did not interfere with work or social interactions, a substantial proportion (38 %) affirmed this impairment, underscoring the need for effective coping strategies and supportive venues especially in this subset.
While LS patient needs for support can fluctuate throughout the trajectory of their diagnosis and clinical management, especially at times of scheduled screenings and procedures and reaching milestone ages (McKinnon et al. 2007; Plumridge et al. 2012), we did not observe large fluctuations in attendance. However, we did not survey patients on current details of their clinical care/surveillance, which is a limitation to this observation. We did observe consistently lower attendance in the month of December across all years. We speculate that this was due to holiday and cultural events. Attendance at meetings outside of December varied by patient availability. We would therefore advise others to avoid holding such events in the month of December.
A majority of SGNA survey respondents indicated that a support group would have increased utility immediately following genetic testing. This suggests that patients have a greater need for coping strategies, advice, and support at this time, likely due to new feelings of vulnerability, isolation, and uncertainty related to one's diagnosis, as similarly reported in existing work (McKinnon et al. 2007; Speice et al. 2002; Werner-Lin 2008).
High levels of appreciation were observed for the support group being primarily facilitated by a social worker and attended by a genetic counselor. An initial concern discussed by the planning committee was that a genetic counselor might impede patients from fully expressing their feelings and experiences with genetic counseling and testing. However, patients reported both a high level of comfort with and helpfulness of having a genetic counselor present.
Future Directions
While patients expressed a preference for in-person LSPAN meetings, an interest in supplemental online support was identified. With increasing advances in technology and influences of social media, an online venue for individuals with LS to communicate may contribute to providing a more comprehensive support network. Younger people, those who prefer anonymity, and those limited geographically may also find support through web-based resources (Hilgart et al. 2012; Hughes and Phelps 2010; McGill and McVittie 2007; Thewes et al. 2003). It is imperative that such a resource be secure. We suggest that an informed professional, such as a genetic counselor or interdisciplinary committee, should monitor the online venue in order to identify/correct any potential misleading information and to provide guidelines for appropriate discussion.
A patient-matched communication system may also provide an alternative and more personalized mechanism for patients to support one another (Hughes and Phelps 2010). It is noteworthy that 62 % of LSEW3 respondents indicated an interest in participating in a patient-to-patient network, in which individuals would be matched based on clinical features and/or personal characteristics for telephone communication. Patients seem altruistic and mutually supportive, as demonstrated by a majority of respondents expressing willingness to volunteer and complete necessary training to participate. Efforts are underway to develop this future program, which could then be modified for use with other hereditary cancer predisposition syndromes.
Study Limitations
The main limitation of this study is its retrospective nature. The survey instruments were initially designed for clinical utility to assess our progress and ability to address the needs of patients participating in the support resources. As a result, these instruments were not based on established, standardized measures of relevant outcomes such as satisfaction and perceived utility. Future studies should utilize more reliable measures in order to assess the efficacy of such supportive programs, for example, modified versions of the Genetic Counseling Satisfaction Scale (DeMarco et al. 2004) or the Patient Satisfaction with Cancer-Related Care Scale (Jean-Pierre et al. 2011). This study also analyzes a small study sample of program participants, which may not be reflective of the entire population of LS. Furthermore, respondents may be biased as those utilizing the LSEW and LSPAN meetings may be in greatest need of support. In addition, participants most interested and satisfied with these resources continue to utilize them and provide feedback, which may potentially skew survey data progressively toward more positive findings each year. In relation to the LSEW meetings, all attendees (patients and guest family members) were able to provide feedback in the Post-WS. Index patients and guests may have perceived the utility of these resources differently, which could not be controlled or accounted for in this analysis given the anonymous nature of the data. Demographic details of participants were not collected, such as education, ethnicity, race, and family structure, thus we cannot comment on how these relate to participation or perceived utility. Lastly, while participants generally perceived the LSEW and LSPAN as helpful, this study does not quantify their effect on increasing disease knowledge or psychosocial well-being, nor compliance with screening/risk-reducing surgery, which are important areas for future research.
Practice Implications
Resources such as the LSEW and LSPAN can be used to augment genetic counseling to more comprehensively provide care to LS patients and their families. In addition to providing education and counseling, these resources serve to update health care providers on specific educational and support needs of LS to take back into their clinical practice.
The LSEW provides a venue for LS patients and their families to broaden their disease knowledge, for example by providing details on screening procedures and cancer prevention. This may be especially useful for patients who cope through information seeking, as it provides a controlled venue with provision of evidence-based information. Knowledge empowers LS patients to assume a proactive role in the management of their condition and may help them to better handle their diagnosis. Dissemination of information in this setting provides the opportunity for enhanced communication and sharing of disease knowledge amongst family members. The LSEW may be of specific interest to at-risk LS family members planning to undergo genetic testing who are seeking information. It may also help family members to better understand the challenges of their loved ones living with LS and thus facilitate familial support.
The LSPAN may be incorporated into clinical practice to provide an organized method of psychosocial support. Results of this study suggest that this may be of particular utility immediately following genetic testing. A support group specific for LS enables genetic counselors to offer an additional resource to help patients seeking emotional support and an opportunity for LS patients to converse with others who have the same rare diagnosis. An important role for the genetic counselor in the LS support group has been identified; he/she attends as a safety backup to answer specific genetic-related questions and correct common misconceptions, while being mindful to allow the attendees to dictate the emotional nature and content of the discussion.
Research Recommendations
Further studies are needed to identify and quantify the effect of the LSEW and LSPAN resources on improving family communication and medical decision-making. Additional work must be done using validated measures to determine if there is a significant effect on psychological well-being, such as on feelings of anxiety, distress, and isolation experienced by participants. Additional studies may be conducted to determine whether demographics and aspects in clinical care (e.g., scheduled screenings) are correlated with attendance and needs for educational and/or emotional support. Separate analyses of the index LS patient and family member feedback would be useful in assessing whether these groups perceive utility of the educational workshop differently. This study identifies a desire for an online support system specific to LS; however, future work is needed to delineate methodology and utility of this resource.
Conclusions
This study provides a methodology for organizing a comprehensive educational and emotional support system for LS patients and their families. It identifies a need for additional Internet-based as well as patient-matched support resources. We have experienced positive uptake and response to both a yearly LS educational workshop and a quarterly professionally led LS support group. Sources of informational and psychosocial support must evolve to meet changing patient needs, which can be achieved through ongoing survey administration and analysis of feedback. We would encourage implementation of similar resources more broadly across institutions offering clinical genetic testing, counseling, and medical care for families with LS. Future directions for the development of a more comprehensive support network for LS at MSKCC include creation of a secure online support venue and a patient-matched communication program.
Acknowledgments
We would like to thank our patients and their families for participating in the LSEW and LSPAN, and for their valuable feedback. We also thank the Robert and Kate Niehaus Clinical Cancer Genetics Initiative at MSKCC and The Romeo Milio Lynch Syndrome Foundation for supporting this work. This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
Footnotes
Compliance with Ethical Standards: Conflicts of Interest Marina J. Corines, Jada G. Hamilton, Emily Glogowski, Chris A. Anrig, Rachael Goldberg, Kate Niehaus, Erin Salo-Mullen, Megan Harlan, Margaret R. Sheehan, Magan Trottier, Asad Ahsraf, Christina Tran, Lauren Jacobs, Rohini Rau-Murthy, Anne G. Lincoln, Mark E. Robson, Jose G. Guillem, Arnold J. Markowitz, Kenneth Offit, and Zsofia K. Stadler declare that they have no conflict of interest.
Human Studies and Informed Consent All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). For this type of study formal consent is not required.
Animal Studies No animal studies were carried out by the authors for this article.
References
- Aarnio M, Sankila R, Pukkala E, Salovaara R, Aaltonen L, de la Chapelle A, et al. Cancer risk in mutation carriers of DNA-mismatch-repair genes. International Journal of Cancer. 1999;81(2):214–218. doi: 10.1002/(sici)1097-0215(19990412)81:2<214::aid-ijc8>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Akiyama Y, Sato H, Yamada T, Nagasaki H, Tsuchiya A, Abe R, Yuasa Y. Germ-line mutation of the hMSH6/GTBP gene in an atypical hereditary nonpolyposis colorectal cancer kindred. Cancer Research. 1997;57(18):3920–3923. [PubMed] [Google Scholar]
- Aktan-Collan K, Kääriäinen H, Järvinen H, Peltomäki P, Pylvänäinen K, Mecklin JP, Haukkala A. Psychosocial consequences of predictive genetic testing for Lynch syndrome and associations to surveillance behaviour in a 7-year follow-up study. Familial Cancer. 2013;12(4):639–646. doi: 10.1007/s10689-013-9628-9. [DOI] [PubMed] [Google Scholar]
- Arrington M. Theorizing about social support and health communication in a prostate cancer support group. Journal of Psychosocial Oncology. 2010;28(3):260–268. doi: 10.1080/07347331003678337. [DOI] [PubMed] [Google Scholar]
- Bannon S, Mork M, Vilar E, Peterson S, Lu K, Lynch P, et al. Patient-reported disease knowledge and educational needs in lynch syndrome: findings of an interactive multidisciplinary patient conference. Hereditary Cancer in Clinical Practice. 2014;12(1):1. doi: 10.1186/1897-4287-12-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauld L, Ferguson J, McEwen A, Hiscock R. Evaluation of a drop-in rolling-group model of support to stop smoking. Addiction. 2012;107(9):1687–1695. doi: 10.1111/j.1360-0443.2012.03861.x. [DOI] [PubMed] [Google Scholar]
- Bell K, Lee J, Foran S, Kwong S, Christopherson J. Is there an “ideal cancer” support group? Key findings from a qualitative study of three groups. Journal of Psychosocial Oncology. 2010;28(4):432–449. doi: 10.1080/07347332.2010.488140. [DOI] [PubMed] [Google Scholar]
- Berger JM. Crisis intervention: a drop-in support group for cancer patients and their families. Social Work in Health Care. 1984;10(2):81–92. doi: 10.1300/j010v10n02_07. [DOI] [PubMed] [Google Scholar]
- Bonadona V, Bonaïti B, Olschwang S, Grandjouan S, Huiart L, Longy M, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in lynch syndrome. Journal of the American Medical Association. 2011;305(22):2304–2310. doi: 10.1001/jama.2011.743. [DOI] [PubMed] [Google Scholar]
- Bultz BD, Speca M, Brasher PM, Geggie PH, Page SA. A randomized controlled trial of a brief psychoeducational support group for partners of early stage breast cancer patients. Psycho-Oncology. 2000;9(4):303–313. doi: 10.1002/1099-1611(200007/08)9:4<303::aid-pon462>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Classen C, Butler LD, Koopman C, Miller E, DiMiceli S, Giese-Davis J, et al. Supportive-expressive group therapy and distress in patients with metastatic breast cancer: a randomized clinical intervention trial. Archives of General Psychiatry. 2001;58(5):494–501. doi: 10.1001/archpsyc.58.5.494. [DOI] [PubMed] [Google Scholar]
- DeMarco TA, Peshkin BN, Mars BD, Tercyak KP. Patient satisfaction with cancer genetic counseling: A psychometric analysis of the Genetic Counseling Satisfaction Scale. Journal of Genetic Counseling. 2004;13(4):293–304. doi: 10.1023/b:jogc.0000035523.96133.bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilzell K, Kingham K, Ormond K, Ladabaum U. Evaluating the utilization of educational materials in communicating about Lynch syndrome to at-risk relatives. Familial Cancer. 2014;13(3):381–389. doi: 10.1007/s10689-014-9720-9. [DOI] [PubMed] [Google Scholar]
- Dunkel-Schetter C. Social support and cancer: findings based on patient interviews and their interpretations. Journal of Social Issues. 1984;40(4):98–99. [Google Scholar]
- Dunlop M, Farrington S, Carothers A, Wyllie A, Sharp L, Burn J, et al. Cancer risk associated with germline DNA mismatch repair gene mutations. Human Molecular Genetics. 1997;6(1):105–110. doi: 10.1093/hmg/6.1.105. [DOI] [PubMed] [Google Scholar]
- Emilsson S, Svensk A, Tavelin B, Lindh J. Support group participation during the post-operative radiotherapy period increases levels of coping resources among women with breast cancer. European Journal of Cancer Care. 2012;21:591–598. doi: 10.1111/j.1365-2354.2012.01343.x. [DOI] [PubMed] [Google Scholar]
- Esplen M, Hunter J, Leszcz M, Warner E, Narod S, Metcalfe K, et al. A multicenter study of supportive-expressive group therapy for women with BRCA1/BRCA2 mutations. Cancer. 2004;101(10):2327–2340. doi: 10.1002/cncr.20661. [DOI] [PubMed] [Google Scholar]
- Fawzy FI, Fawzy NW, Hyun CS, Elashoff R, Guthrie D, Fahey JL, et al. Malignant melanoma. Effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later. Archives of General Psychiatry. 1993;50(9):681–689. doi: 10.1001/archpsyc.1993.01820210015002. [DOI] [PubMed] [Google Scholar]
- Galiatsatos P, Rothenmund H, Aubin S, Foulkes WD. Psychosocial impact of Lynch syndrome on affected individuals and families. Digestive Diseases and Sciences. 2015;60(8):2246–2250. doi: 10.1007/s10620-015-3626-8. [DOI] [PubMed] [Google Scholar]
- Goodwin P, Leszcz M, Ennis M, Koopmans J, Vincent L, Guther H, et al. The effect of group psychosocial support on survival in metastatic breast cancer. New England Journal of Medicine. 2001;345(24):1719–1726. doi: 10.1056/NEJMoa011871. [DOI] [PubMed] [Google Scholar]
- Hilgart J, Hayward J, Iredale R. E-genetics: Exploring the acceptability and feasibility of using technology in cancer genetics services. Clinical Genetics. 2012;81(6):514–520. doi: 10.1111/j.1399-0004.2011.01813.x. [DOI] [PubMed] [Google Scholar]
- Hughes L, Phelps C. The bigger the network the bigger the bowl of cherries…: Exploring the acceptability of, and preferences for, an ongoing support network for known BRCA 1 and BRCA 2 mutation carriers. Journal of Genetic Counseling. 2010;19(5):487–496. doi: 10.1007/s10897-010-9300-6. [DOI] [PubMed] [Google Scholar]
- Jean-Pierre P, Fiscella K, Freund KM, Clark J, Darnell J, Holden A, et al. Group P.N.R.P. Structural and reliability analysis of a patient satisfaction with cancer-related care measure: A multisite patient navigation research program study. Cancer. 2011;117(4):854–861. doi: 10.1002/cncr.25501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kastrinos F, Mukherjee B, Tayob N, Wang F, Sparr J, Raymond V, et al. Risk of pancreatic cancer in families with lynch syndrome. Journal of the American Medical Association. 2009;302(16):1790–1795. doi: 10.1001/jama.2009.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller M, Jost R, Haunstetter CM, Sattel H, Schroeter C, Bertsch U, et al. Psychosocial outcome following genetic risk counselling for familial colorectal cancer. A comparison of affected patients and family members. Clinical Genetics. 2008;74(5):414–424. doi: 10.1111/j.1399-0004.2008.01089.x. [DOI] [PubMed] [Google Scholar]
- Kwok C, Ho M. Development and evaluation of a culturally sensitive support group programme for Chinese-Australian women with breast cancer: A pilot study. European Journal of Cancer Care (English) 2011;20(6):795–802. doi: 10.1111/j.1365-2354.2011.01266.x. [DOI] [PubMed] [Google Scholar]
- Landsbergen K, Brunner H, Manders P, Hoogerbrugge N, Prins J. Educational-support groups for BRCA mutation carriers satisfy need for information but do not affect emotional distress. Genetic Counseling (Geneva, Switzerland) 2010;21(4):423–437. [PubMed] [Google Scholar]
- Liu T, Yan H, Kuismanen S, Percesepe A, Bisgaard M, Pedroni M, et al. The role of hPMS1 and hPMS2 in predisposing to colorectal cancer. Cancer Research. 2001;61(21):7798–7802. [PubMed] [Google Scholar]
- Lynch H. Family information service and hereditary cancer. Cancer. 2001;91(4):625–628. doi: 10.1002/1097-0142(20010215)91:4<625::aid-cncr1044>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Lynch H, de la Chapelle A. Hereditary colorectal cancer. New England Journal of Medicine. 2003;348(10):919–932. doi: 10.1056/NEJMra012242. [DOI] [PubMed] [Google Scholar]
- Lynch H, Shaw M, Magnuson C, Larsen A, Krush A. Hereditary factors in cancer. Study of two large midwestern kindreds. Archives of Internal Medicine. 1966;117(2):206–212. [PubMed] [Google Scholar]
- McGill M, McVittie C. Support information and identity: Online discussions of male breast cancer patients. Health Psychology Update. 2007;16(3):433–456. [Google Scholar]
- McGovern R, Heyman E, Resnick M. An examination of coping style and quality of life of cancer patients who attend a prostate cancer support group. Journal of Psychosocial Oncology. 2002;20(3):57–68. [Google Scholar]
- McKinnon W, Naud S, Ashikaga T, Colletti R, Wood M. Results of an intervention for individuals and families with BRCA mutations: A model for providing medical updates and psychosocial support following genetic testing. Journal of Genetic Counseling. 2007;16(4):433–456. doi: 10.1007/s10897-006-9078-8. [DOI] [PubMed] [Google Scholar]
- Miyaki M, Konishi M, Tanaka K, Kikuchi-Yanoshita R, Muraoka M, Yasuno M, et al. Germline mutation of MSH6 as the cause of hereditary nonpolyposis colorectal cancer. Nature Genetics. 1997;17(3):271–272. doi: 10.1038/ng1197-271. [DOI] [PubMed] [Google Scholar]
- Montazeri A, Jarvandi S, Haghighat S, Vahdani M, Sajadian A, Ebrahimi M, Haji-Mahmoodi M. Anxiety and depression in breast cancer patients before and after participation in a cancer support group. Patient Education and Counseling. 2001;45(3):195–198. doi: 10.1016/s0738-3991(01)00121-5. [DOI] [PubMed] [Google Scholar]
- Murakami Y, Okamura H, Sugano K, Yoshida T, Kazuma K, Akechi T, Uchitomi Y. Psychologic distress after disclosure of genetic test results regarding hereditary nonpolyposis co-lorectal carcinoma. Cancer. 2004;101(2):395–403. doi: 10.1002/cncr.20363. [DOI] [PubMed] [Google Scholar]
- Plumridge G, Metcalfe A, Coad J, Gill P. The role of support groups in facilitating families in coping with a genetic condition and in discussion of genetic risk information. Health Expectations. 2012;15(3):255–266. doi: 10.1111/j.1369-7625.2011.00663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speice J, McDaniel S, Rowley P, Loader S. Family issues in a psychoeducation group for women with a BRCA mutation. Clinical Genetics. 2002;62(2):121–127. doi: 10.1034/j.1399-0004.2002.620204.x. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Spira J. Supportive-expressive group therapy: a treatment manual of psychosocial intervention for women with recurrent breast cancer. Stanford: California: Psychosocial Treatment Laboratory, Stanford University School of Medicine; 1991. [Google Scholar]
- Spiegel D, Bloom J, Kraemer H, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2(8668):888–891. doi: 10.1016/s0140-6736(89)91551-1. [DOI] [PubMed] [Google Scholar]
- Stanton A, Ganz P, Rowland J, Meyerowitz B, Meyerowitz J, Sears S. Promoting adjustment after treatment for cancer. Cancer. 2005;104(11 Suppl):2608–2613. doi: 10.1002/cncr.21246. [DOI] [PubMed] [Google Scholar]
- Thewes B, Meiser B, Tucker M, Tucker K. The unmet information and support needs of women with a family history of breast cancer: A descriptive study. Journal of Genetic Counseling. 2003;12(1):61–76. doi: 10.1023/A:1021447201809. [DOI] [PubMed] [Google Scholar]
- Vasen H, Watson P, Mecklin J, Lynch H. New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC. Gastroenterology. 1999;116(6):1453–1456. doi: 10.1016/s0016-5085(99)70510-x. [DOI] [PubMed] [Google Scholar]
- Weis J. Support groups for cancer patients. Supportive Care in Cancer. 2003;11(12):763–768. doi: 10.1007/s00520-003-0536-7. [DOI] [PubMed] [Google Scholar]
- Werner-Lin A. Formal and informal support needs of young women with BRCA mutations. Journal of Psychosocial Oncology. 2008;26(4):111–133. doi: 10.1080/07347330802359776. [DOI] [PubMed] [Google Scholar]
- Yu HA, Lin K, Ota D, Lynch H. Hereditary nonpolyposis colorectal cancer: Preventive management. Cancer Treatment Reviews. 2003;29(6):461–470. doi: 10.1016/s0305-7372(03)00084-7. [DOI] [PubMed] [Google Scholar]