Abstract
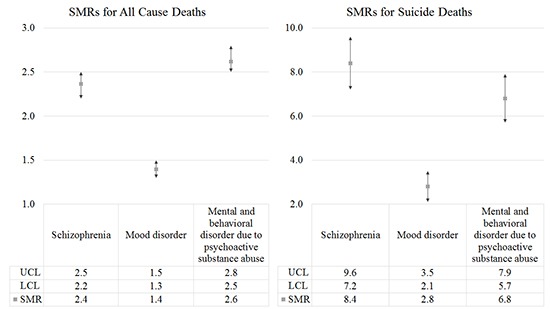
Individuals with psychoses show excess mortality, which is a major public health concern. This study examined all-cause and suicide mortality rates in Korean patients diagnosed with schizophrenia, mood disorder, or mental and behavioral disorder due to psychoactive substance use and to compare this with that of the general population. Data were from the National Health Insurance cohort, 2002 to 2013. A total of 107,190 cases aged 15 years or over were included. Mortality rates per 100,000 person years (PY) were obtained. Poisson regression modelling was conducted to quantify the effect of baseline characteristics on all-cause and suicide mortality risks. Standardized mortality ratios (SMRs) were also calculated. All-cause mortality was the highest among mental and behavioral disorder patients (1,051.0 per 100,000 PY), followed by schizophrenia (949.1 per 100,000 PY) and mood disorder patients (559.5 per 100,000 PY). Highest suicide mortality was found in schizophrenia (177.2 per 100,000 PY), mental and behavioral disorder (143.7 per 100,000 PY), and mood disorder patients (59.7 per 100,000 PY). The rate ratios (RRs) for all-cause and suicide mortality were reduced for younger populations and women. Psychoses patients had higher all-cause (schizophrenia, SMR 2.4; 95% confidence interval [CI] 2.2–2.5; mood disorder, SMR 1.4; 95% CI 1.3–1.5; mental and behavioral disorder, SMR 2.6; 95% CI 2.5–2.8) and suicide (schizophrenia, SMR 8.4; 95% CI 7.2–9.6; mood disorder, SMR 2.8; 95% CI 2.1–3.5; mental and behavioral disorder, SMR 6.8; 95% CI 5.7–7.9) mortality rates than the general population. These findings infer that efforts should be made to reduce excess mortality in psychoses.
Keywords: Schizophrenia, Mood Disorder, Mental and Behavioral Disorder, Mortality, Suicide, Korea
Graphical Abstract
INTRODUCTION
There is growing interest in outcomes of schizophrenia and other psychoses as psychoses have been associated with premature mortality and reductions in life expectancy (1). Several previous studies have explored the elevated mortality risks commonly found in mental disorder patients and have conveyed that individuals diagnosed with substance use disorder, schizophrenia, and bipolar disorder show higher risks for all-cause mortality (2). In fact, life expectancies of schizophrenia patients have been known to be 10 to 25 years shorter than that of the general population (3). Similarly, bipolar disorder has been associated with decreased life expectancy by around nine to 14 years and behavioral disorder resulting from alcohol and substance use has been related with an increased risk of death (4,5). Unsurprisingly, individuals with mental disorders also report higher standardized mortality ratios (SMRs) compared to the general population (6).
Natural and unnatural causes have been known to attribute to higher mortality commonly found in psychoses patients. Specifically, suicide mortality has been identified as the primary unnatural cause, with it being the most common cause of death among individuals with schizophrenia (1). Substantially increased suicide rates were also found in patients with depression, bipolar disorder, opioid use, and alcohol use disorder (6). Identifying excess all-cause and suicide mortality associated with mental disorders is particularly significant in Korea because major mental disorders are prevalent (schizophrenia and schizoaffective disorder 0.3%, major depressive disorder 5.6%, and nicotine and alcohol use disorder 16.4%) and its suicide rate is the highest among the Organization for Economic Cooperation and Development (OECD) countries (7,8).
Previous research investigating elevated mortality rates in patients with schizophrenia and other psychoses have mainly focused on Western European and North American countries (9). Additionally, few previous studies have examined mortality using a large, nationally representative sample (10). With regard to studies conducted on East Asia, a study by Saku et al. (11) revealed that Japanese bipolar patients exhibit significantly higher SMRs than the general population using longitudinal data from 1948 to 1982. As for studies in Korea, an investigation by Park et al. (12) reported higher mortality risks in psychiatric patients based on data from a general hospital. Hence, despite the substantial economic burden of psychoses in Korea, few Korean studies have investigated excess mortality associated with psychotic disease using a large, nationally representative sample of individuals with follow up data. Therefore, the aim of this study was to examine all-cause and suicide mortality in a nationally representative cohort of individuals with schizophrenia, mood disorder, and mental and behavioral disorders due to psychoactive substance use and to compare mortality in this cohort with that of the general population.
MATERIALS AND METHODS
Study population
This study used data from the Korea National Health Insurance (NHI) Service National Sample Cohort, 2002 to 2013. The NHI data consisted of 1,025,340 nationally representative random samples of the Korean population in 2002, which accounted for around 2.2% of the entire population. Data were collected by the Korean NHI Service (KNHIS) using a systematic sampling method to generate a representative sample of the 46,605,433 Korean residents recorded in 2002. Follow up data were available up to 2013 and included information on medical claims filed between 2002 and 2013.
In this study, all study participants with a diagnosis record of schizophrenia and schizoaffective disorders (International Classification of Diseases version 10 [ICD-10] F20, F25), mood disorders (F30–39), and mental and behavioral disorders due to psychoactive substance use (F10–19) were screened for inclusion at baseline. Individuals with at least 2 outpatient claims or one inpatient claim for the defined ICD-10 codes in primary, secondary, or tertiary hospitals were included. To ensure identification of individuals with a first diagnosis of the stated diseases, individuals diagnosed before 2005 were excluded from the analysis. Individuals aged below 15 years were also excluded, which led to the final inclusion of 9,387 schizophrenia and schizoaffective disorder cases, 86,922 mood disorder cases, and 10,881 mental and behavioral disorders due to psychoactive substance use cases. Categorization of subjects with multiple disorders was made according to the primary ICD-10 diagnosis recorded.
Case-tracing procedure
The study population was followed up for 9 years to identify all-cause and suicide deaths. Occurrences of death were recorded in the cohort based on the National Statistical Office (NSO) database. In Korea, all deaths are compulsory reported to the NSO through a death notice. Suicide deaths were separately recognized using the ICD-10 code X60–84.
Variables
Information on the age, sex, income, region, and Charlson Comorbidity Index (CCI) of the study participants were collected. Age was categorized into 15–24, 25–34, 35–44, 45–54, 55–64, 65–75, and 75 or above. Sex was classified into men or women, income into medical aid, low, middle, or high, region into Seoul/metropolitan cities or others, and CCI from 0 to 7. Schizophrenia was partitioned into schizophrenia and schizoaffective disorder. Income was categorized into medical aid, low, middle, and high based on the NHI contribution premium level of patients, which can be seen as a surrogate indicator of income. For workplace insured NHI, insurance contribution premiums are calculated depending on the average annual salary level of individuals. For regionally insured NHI, contributions premiums are calculated using taxable income and assets that can reflect individuals' living standards. Hence, contribution premiums can be seen as a proxy for the ability to pay. With regard to region, Seoul and the seven metropolitan cities of Korea were grouped into the same category and all other provinces into another category. CCI was adjusted to account for the potential effect of comorbidities. The CCI was calculated yearly using the Quan's method, in which 19 diseases were categorized into scores of 1, 2, 3, or 6 and the CCI per subject obtained by the sum of all scores (13).
Statistical analysis
Crude mortality rates were calculated for all-cause and suicide mortality per 100,000 person years (PY) stratified by baseline socio-demographic and health related characteristics. Date of first applicable record of schizophrenia, mood disorder, and mental and behavioral disorder due to psychoactive substance use was utilized as the entry point and date of death or end of follow up period as the end-point. Poisson regression modelling was conducted to quantify the effect of baseline socio-demographic and health related characteristics on risks of all-cause and suicide mortality while adjusting for confounders. SMRs with 95% confidence intervals (CIs) were calculated for all-cause and suicide mortality. SMRs refer to the ratio of the observed number of deaths in each psychiatric group to the expected number of deaths in the same cohort based on the general Korean population. All calculated P values were 2-sided and considered significant at < 0.05. Analysis was performed using the SAS software, version 9.4 (SAS Institute, Cary, NC, USA).
Ethics statement
The Korea NHI data are secondary data that do not contain any private information. Since the data were obtained as anonymized and de-identified prior to analysis, the study protocol was not subjected to review by the Institutional Review Board.
RESULTS
All-cause and suicide mortality rates by socio-demographic and health related characteristics for all-cause and suicide death are presented in Tables 1, 2, 3. All-cause mortality was the highest among mental and behavioral disorder due to psychoactive substance use patients (1,051.0 per 100,000 PY), followed by schizophrenia (949.1 per 100,000 PY), and mood disorder patients (559.5 per 100,000 PY). Mortality rates generally increased with age and were higher among men than in women. Participants scoring lower on the CCI showed lower mortality rates.
Table 1. Mortality rates (per 100,000 PY) by baseline characteristics in schizophrenia patients.
| Parameters | Cases | All deaths | Crude rate (95% CI) | Suicide | Crude rate (95% CI) |
|---|---|---|---|---|---|
| Total | 9,387 | 980 (10.4) | 949.1 (892.9–1,005.3) | 183 (2.0) | 177.2 (151.8–202.7) |
| Age, yr | |||||
| 15–24 | 1,068 | 34 (3.2) | 289.4 (193.7–385.1) | 30 (2.8) | 255.4 (210.0–345.5) |
| 25–34 | 1,799 | 84 (4.7) | 424.5 (335.8–513.1) | 56 (3.1) | 283.0 (130.7–355.9) |
| 35–44 | 2,225 | 100 (4.5) | 408.6 (330.3–486.8) | 45 (2.0) | 183.9 (57.7–237.0) |
| 45–54 | 1,900 | 108 (5.7) | 516.7 (422.1–611.4) | 21 (1.1) | 100.5 (97.3–143.2) |
| 55–64 | 985 | 132 (13.4) | 1,218.3 (1,024.9–1,411.7) | 19 (1.9) | 175.4 (39.6–253.4) |
| 65–74 | 724 | 195 (26.9) | 2,448.5 (2,154.8–2,742.3) | 9 (1.2) | 113.0 (5.1–186.4) |
| 75 or above | 686 | 327 (47.7) | 4,333.4 (3,993.6–4,673.2) | 3 (0.4) | 39.8 (151.8–84.6) |
| Sex | |||||
| Men | 4,532 | 520 (11.5) | 1,043.1 (958.7–1,127.4) | 103 (2.3) | 206.6 (167.2–246.1) |
| Women | 4,855 | 460 (9.5) | 861.3 (786.5–936.2) | 80 (1.7) | 149.8 (117.2–182.4) |
| Income | |||||
| Medical aid | 1,883 | 162 (8.6) | 782.1 (667.0–897.3) | 24 (1.3) | 115.9 (69.8–161.9) |
| Low | 2,546 | 228 (9.0) | 814.1 (713.3–914.9) | 48 (1.9) | 171.4 (123.4–219.4) |
| Middle | 2,764 | 281 (10.2) | 924.2 (821.8–1,026.6) | 49 (1.8) | 161.2 (116.4–205.9) |
| High | 2,194 | 309 (14.1) | 1,280.4 (1,148.0–1,412.7) | 62 (2.8) | 256.9 (193.9–319.9) |
| Region | |||||
| Seoul/metropolitan cities | 4,384 | 444 (10.1) | 920.7 (839.5–1,001.9) | 89 (2.0) | 184.6 (146.6–222.5) |
| Others | 5,003 | 536 (10.7) | 974.0 (896.0–1,051.9) | 94 (1.9) | 170.8 (136.6–205.0) |
| CCI | |||||
| 0 | 2,464 | 167 (6.8) | 616.1 (525.9–706.4) | 78 (3.2) | 287.8 (224.9–350.6) |
| 1 | 1,679 | 97 (5.8) | 525.2 (423.7–626.7) | 33 (2.0) | 178.7 (118.3–239.0) |
| 2 | 1,438 | 112 (7.8) | 708.1 (582.1–834.0) | 28 (2.0) | 177.0 (112.1–241.9) |
| 3 | 1,438 | 130 (9.0) | 821.8 (687.1–956.6) | 21 (1.5) | 132.8 (76.4–189.1) |
| 4 | 786 | 101 (12.9) | 1,168.2 (955.5–1,380.9) | 11 (1.4) | 127.2 (52.6–201.9) |
| 5 | 535 | 106 (19.8) | 1,801.2 (1,494.1–2,108.2) | 6 (1.1) | 102.0 (20.8–183.1) |
| 6 | 373 | 70 (18.8) | 1,706.1 (1,345.8–2,066.3) | 5 (1.3) | 121.9 (15.8–228.0) |
| 7 | 674 | 197 (29.2) | 2,657.1 (2,345.0–2,969.3) | 1 (0.2) | 13.5 (12.9–39.9) |
| Type | |||||
| Schizophrenia | 8,847 | 920 (10.4) | 945.4 (887.5–1,003.2) | 174 (2.0) | 178.8 (152.5–205.1) |
| Schizoaffective disorder | 540 | 60 (11.1) | 1,010.1 (769.1–1,251.1) | 9 (1.7) | 151.5 (53.4–249.7) |
PY = person years, CI = confidence interval, CCI = Charlson Comorbidity Index.
Table 2. Mortality rates (per 100,000 PY) by baseline characteristics in mood disorder patients.
| Parameters | Cases | All deaths | Crude rate (95% CI) | Suicide | Crude rate (95% CI) |
|---|---|---|---|---|---|
| Total | 86,922 | 5,350 (6.2) | 559.5 (545.0–574.1) | 571 (0.7) | 59.7 (54.8–64.6) |
| Age, yr | |||||
| 15–24 | 7,851 | 47 (0.6) | 54.4 (38.9–69.9) | 30 (0.4) | 34.7 (22.3–47.1) |
| 25–34 | 10,494 | 130 (1.2) | 112.6 (93.4–131.9) | 82 (0.8) | 71.0 (55.7–86.4) |
| 35–44 | 14,132 | 242 (1.7) | 155.7 (136.2–175.1) | 91 (0.6) | 58.5 (46.6–70.5) |
| 45–54 | 17,812 | 430 (2.4) | 219.5 (199.0–240.0) | 109 (0.6) | 55.6 (45.2–66.0) |
| 55–64 | 14,585 | 700 (4.8) | 436.3 (404.8–467.9) | 99 (0.7) | 61.7 (49.6–73.8) |
| 65–74 | 13,457 | 1,519 (11.3) | 1,026.2 (977.6–1,074.8) | 97 (0.7) | 65.5 (52.5–78.5) |
| 75 or above | 8,591 | 2,282 (26.6) | 2,414.8 (2,329.9–2,499.7) | 63 (0.7) | 66.7 (50.3–83.1) |
| Sex | |||||
| Men | 31,007 | 2,659 (8.6) | 779.6 (751.3–807.9) | 308 (1.0) | 90.3 (80.3–100.3) |
| Women | 55,915 | 2,691 (4.8) | 437.5 (421.4–453.6) | 263 (0.5) | 42.8 (37.6–47.9) |
| Income | |||||
| Medical aid | 3,306 | 337 (10.2) | 926.7 (832.9–1,020.5) | 29 (0.9) | 79.7 (50.8–108.6) |
| Low | 24,544 | 1,453 (5.9) | 538.2 (511.3–565.0) | 158 (0.6) | 58.5 (49.4–67.6) |
| Middle | 32,557 | 1,763 (5.4) | 492.3 (469.9–514.6) | 221 (0.7) | 61.7 (53.6–69.8) |
| High | 26,515 | 1,797 (6.8) | 616.1 (588.6–643.6) | 163 (0.6) | 55.9 (47.3–64.4) |
| Region | |||||
| Seoul/metropolitan cities | 38,934 | 2,350 (6.0) | 548.7 (527.2–570.2) | 256 (0.7) | 59.8 (52.5–67.1) |
| Others | 47,988 | 3,000 (6.3) | 568.3 (548.6–588.0) | 315 (0.7) | 59.7 (53.1–66.2) |
| CCI | |||||
| 0 | 8,427 | 220 (2.6) | 237.3 (206.4–268.3) | 96 (1.1) | 103.6 (83.0–124.2) |
| 1 | 10,421 | 288 (2.8) | 251.2 (222.6–279.9) | 73 (0.7) | 63.7 (49.1–78.2) |
| 2 | 10,953 | 410 (3.7) | 340.3 (308.0–372.6) | 91 (0.8) | 75.5 (60.1–91.0) |
| 3 | 17,866 | 575 (3.2) | 292.6 (269.1–316.1) | 86 (0.5) | 43.8 (34.5–53.0) |
| 4 | 12,527 | 574 (4.6) | 416.6 (383.3–449.8) | 77 (0.6) | 55.9 (43.4–68.3) |
| 5 | 9,021 | 656 (7.3) | 661.1 (612.4–709.8) | 58 (0.6) | 58.4 (43.5–73.4) |
| 6 | 6,396 | 637 (10.0) | 905.4 (838.7–972.1) | 42 (0.7) | 59.7 (41.7–77.7) |
| 7 | 11,311 | 1,990 (17.6) | 1,599.4 (1,535.6–1,663.2) | 48 (0.4) | 38.6 (27.7–49.5) |
PY = person years, CI = confidence interval, CCI = Charlson Comorbidity Index.
Table 3. Mortality rates (per 100,000 PY) by baseline characteristics in mental and behavioral disorder due to psychoactive substance use patients.
| Parameters | Cases | All deaths | Crude rate (95% CI) | Suicide | Crude rate (95% CI) |
|---|---|---|---|---|---|
| Total | 10,881 | 1,258 (11.6) | 1,051.0 (996.4–1,105.7) | 172 (1.6) | 143.7 (122.4–165.0) |
| Age, yr | |||||
| 15–24 | 655 | 8 (1.2) | 111.0 (34.6–187.5) | 4 (0.6) | 55.5 (1.3–109.8) |
| 25–34 | 1,386 | 44 (3.2) | 288.6 (204.7–372.5) | 24 (1.7) | 157.4 (95.0–219.9) |
| 35–44 | 2,411 | 165 (6.8) | 622.1 (530.5–713.8) | 32 (1.3) | 120.7 (79.1–162.2) |
| 45–54 | 3,082 | 353 (11.5) | 1,041.2 (939.0–1,143.4) | 47 (1.5) | 138.6 (99.3–178.0) |
| 55–64 | 1,878 | 275 (14.6) | 1,331.2 (1,185.8–1,476.6) | 32 (1.7) | 154.9 (101.7–208.1) |
| 65–74 | 1,062 | 251 (23.6) | 2,148.6 (1,916.3–2,380.9) | 24 (2.3) | 205.4 (124.2–286.7) |
| 75 or above | 407 | 162 (39.8) | 3,618.5 (3,186.2–4,050.8) | 9 (2.2) | 201.0 (71.1–330.9) |
| Sex | |||||
| Men | 7,920 | 1,105 (14.0) | 1,268.4 (1,199.0–1,337.7) | 131 (1.7) | 150.4 (124.8–175.9) |
| Women | 2,961 | 153 (5.2) | 469.7 (397.3–542.2) | 41 (1.4) | 125.9 (87.6–164.1) |
| Income | |||||
| Medical aid | 936 | 168 (18.0) | 1,631.7 (1,408.2–1,855.2) | 20 (2.1) | 194.3 (110.0–278.5) |
| Low | 3,508 | 413 (11.8) | 1,070.3 (973.3–1,167.2) | 58 (1.7) | 150.3 (111.9–188.7) |
| Middle | 4,163 | 439 (10.6) | 958.7 (873.8–1,043.5) | 65 (1.6) | 141.9 (107.7–176.2) |
| High | 2,274 | 238 (10.5) | 951.5 (837.1–1,065.8) | 29 (1.3) | 115.9 (74.0–157.9) |
| Region | |||||
| Seoul/metropolitan cities | 4,737 | 528 (11.2) | 1,013.3 (931.8–1,094.8) | 77 (1.6) | 147.8 (115.0–180.5) |
| Others | 6,144 | 730 (11.9) | 1,080.1 (1,006.6–1,153.7) | 95 (1.6) | 140.6 (112.5–168.6) |
| CCI | |||||
| 0 | 1,589 | 120 (7.6) | 686.5 (568.4–804.6) | 32 (2.0) | 183.1 (120.3–245.9) |
| 1 | 1,591 | 137 (8.6) | 782.8 (657.5–908.1) | 25 (1.6) | 142.8 (87.3–198.4) |
| 2 | 1,609 | 135 (8.4) | 762.8 (639.6–885.9) | 19 (1.2) | 107.4 (59.4–155.3) |
| 3 | 2,086 | 175 (8.4) | 762.7 (654.5–870.8) | 27 (1.3) | 117.7 (73.6–161.8) |
| 4 | 1,356 | 165 (12.2) | 1,106.2 (948.0–1,264.4) | 24 (1.8) | 160.9 (97.1–224.7) |
| 5 | 895 | 117 (13.1) | 1,188.4 (987.6–1,389.2) | 14 (1.6) | 142.2 (68.3–216.1) |
| 6 | 648 | 123 (19.0) | 1,725.6 (1,451.1–2,000.1) | 14 (2.2) | 196.4 (94.6–298.2) |
| 7 | 1,107 | 286 (25.8) | 2,348.7 (2,114.3–2,583.1) | 17 (1.5) | 139.6 (73.8–205.5) |
PY = person years, CCI = Charlson Comorbidity Index, CI = confidence interval.
Highest suicide mortality was found in schizophrenia (177.2 per 100,000 PY), mental and behavioral disorder due to psychoactive substance use (143.7 per 100,000 PY), and mood disorder patients (59.7 per 100,000 PY). In schizophrenia patients, younger cases had higher suicide death rates. Such trends were reversed in patients diagnosed with other psychoses. Overall, suicide mortality rates were higher in men than in women.
Table 4 shows the results of the Poisson regression modelling. The rate ratios (RRs) for all-cause mortality were significantly lower for younger and women populations. Apart from schizophrenia patients, suicide mortality rates were also reduced in younger aged individuals. Women generally had lower suicide death rates and higher scores on the CCI were associated with decreased suicide mortality rates.
Table 4. RRs for all-cause and suicide mortality by baseline sociodemographic characteristics.
| Parameters | Schizophrenia | Mood disorder | Mental and behavioral disorder due to psychoactive substance use | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All causes | Suicide | All causes | Suicide | All causes | Suicide | |||||||
| RRs (95% CI) | P value | RRs (95% CI) | P value | RRs (95% CI) | P value | RRs (95% CI) | P value | RRs (95% CI) | P value | RR (95% CI) | P value | |
| Age, yr | ||||||||||||
| 15–24 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 25–34 | 1.47 (0.98–2.19) | 0.060 | 1.25 (0.80–1.96) | 0.325 | 2.18 (1.56–3.04) | < 0.001 | 2.32 (1.52–3.53) | < 0.001 | 2.36 (1.11–5.01) | 0.026 | 2.83 (0.98–8.19) | 0.054 |
| 35–44 | 1.43 (0.97–2.12) | 0.074 | 0.91 (0.57–1.45) | 0.686 | 3.05 (2.22–4.17) | < 0.001 | 2.07 (1.37–3.15) | < 0.001 | 4.37 (2.15–8.91) | < 0.001 | 2.15 (0.76–6.13) | 0.151 |
| 45–54 | 1.80 (1.22–2.67) | 0.003 | 0.57 (0.32–1.01) | 0.053 | 4.19 (3.09–5.69) | < 0.001 | 2.23 (1.47–3.37) | < 0.001 | 6.47 (3.20–13.08) | < 0.001 | 2.48 (0.88–6.98) | 0.086 |
| 55–64 | 4.29 (2.92–6.31) | < 0.001 | 1.10 (0.60–2.00) | 0.760 | 7.65 (5.66–10.34) | < 0.001 | 2.76 (1.80–4.23) | < 0.001 | 7.67 (3.77–15.58) | < 0.001 | 2.87 (0.99–8.31) | 0.052 |
| 65–74 | 8.44 (5.77–12.34) | < 0.001 | 0.84 (0.38–1.83) | 0.660 | 16.60 (12.32–22.35) | < 0.001 | 3.25 (2.10–5.03) | < 0.001 | 12.13 (5.96–24.69) | < 0.001 | 4.00 (1.35–11.86) | 0.012 |
| 75 or above | 15.80 (10.88–22.97) | < 0.001 | 0.30 (0.09–1.03) | 0.055 | 39.77 (29.56–53.50) | < 0.001 | 3.41 (2.15–5.41) | < 0.001 | 22.71 (11.09–46.51) | < 0.001 | 4.08 (1.22–13.59) | 0.022 |
| Sex | ||||||||||||
| Men | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Women | 0.66 (0.58–0.75) | < 0.001 | 0.78 (0.58–1.05) | 0.108 | 0.53 (0.51–0.56) | < 0.001 | 0.48 (0.41–0.57) | < 0.001 | 0.45 (0.38–0.53) | < 0.001 | 0.92 (0.64–1.31) | 0.636 |
| Income | ||||||||||||
| Medical aid | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Low | 0.90 (0.73–1.11) | 0.335 | 1.60 (0.97–2.65) | 0.068 | 0.91 (0.81–1.02) | 0.111 | 0.83 (0.56–1.24) | 0.361 | 0.76 (0.63–0.91) | 0.002 | 0.80 (0.48–1.35) | 0.408 |
| Middle | 0.98 (0.80–1.20) | 0.852 | 1.50 (0.91–2.49) | 0.114 | 0.84 (0.75–0.94) | 0.003 | 0.85 (0.58–1.26) | 0.422 | 0.64 (0.54–0.77) | < 0.001 | 0.75 (0.45–1.24) | 0.262 |
| High | 0.98 (0.79–1.21) | 0.840 | 2.77 (1.69–4.55) | < 0.001 | 0.75 (0.67–0.85) | < 0.001 | 0.78 (0.52–1.16) | 0.222 | 0.52 (0.42–0.64) | < 0.001 | 0.60 (0.33–1.07) | 0.081 |
| Region | ||||||||||||
| Seoul/metropolitan cities | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Others | 0.97 (0.85–1.10) | 0.593 | 1.01 (0.75–1.35) | 0.962 | 0.89 (0.84–0.94) | < 0.001 | 1.00 (0.84–1.18) | 0.970 | 0.97 (0.87–1.09) | 0.594 | 0.93 (0.69–1.26) | 0.632 |
| CCI | ||||||||||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 1 | 0.72 (0.56–0.93) | 0.011 | 0.60 (0.40–0.90) | 0.015 | 0.77 (0.65–0.92) | 0.005 | 0.62 (0.46–0.84) | 0.002 | 1.01 (0.79–1.29) | 0.928 | 0.76 (0.45–1.29) | 0.306 |
| 2 | 0.82 (0.64–1.04) | 0.106 | 0.62 (0.40–0.95) | 0.030 | 0.82 (0.69–0.96) | 0.016 | 0.67 (0.50–0.90) | 0.008 | 0.92 (0.72–1.17) | 0.489 | 0.55 (0.31–0.98) | 0.043 |
| 3 | 0.88 (0.69–1.12) | 0.304 | 0.45 (0.28–0.73) | 0.001 | 0.68 (0.58–0.80) | < 0.001 | 0.40 (0.29–0.54) | < 0.001 | 0.97 (0.77–1.23) | 0.807 | 0.61 (0.36–1.03) | 0.064 |
| 4 | 0.82 (0.62–1.07) | 0.135 | 0.47 (0.25–0.90) | 0.023 | 0.68 (0.58–0.80) | < 0.001 | 0.46 (0.34–0.63) | < 0.001 | 1.14 (0.89–1.45) | 0.294 | 0.79 (0.46–1.37) | 0.401 |
| 5 | 0.95 (0.72–1.24) | 0.681 | 0.40 (0.17–0.94) | 0.036 | 0.81 (0.69–0.96) | 0.012 | 0.45 (0.32–0.64) | < 0.001 | 1.09 (0.84–1.42) | 0.518 | 0.66 (0.35–1.27) | 0.214 |
| 6 | 0.81 (0.59–1.09) | 0.167 | 0.48 (0.19–1.23) | 0.128 | 0.99 (0.84–1.16) | 0.892 | 0.44 (0.30–0.65) | < 0.001 | 1.46 (1.13–1.90) | 0.004 | 0.90 (0.47–1.73) | 0.745 |
| 7 | 1.04 (0.81–1.33) | 0.769 | 0.05 (0.01–0.39) | 0.004 | 1.46 (1.25–1.69) | < 0.001 | 0.26 (0.18–0.39) | < 0.001 | 1.83 (1.46–2.29) | < 0.001 | 0.61 (0.32-1.14) | 0.120 |
| Type | 1.00 | |||||||||||
| Schizophrenia | 1.00 | 1.00 | 2.36 (1.11–5.01) | |||||||||
| Schizoaffective disorder | 1.14 (0.87–1.48) | 0.337 | 0.83 (0.43–1.63) | 0.593 | 4.37 (2.15–8.91) | |||||||
RRs = rate ratios, CCI = Charlson Comorbidity Index, CI = confidence interval.
The SMRs for all-cause and suicide deaths are presented on Table 5. Schizophrenia, mood disorder, and mental and behavioral disorder due to psychoactive substance use patients showed increases in all-cause mortality compared to that of the general cohort (schizophrenia, SMR 2.4; 95% CI 2.2–2.5; mood disorder, SMR 1.4; 95% CI 1.3–1.5; mental and behavioral disorder due to psychoactive substance use, SMR 2.6; 95% CI 2.5–2.8). SMRs were more pronounced for cases in lower age groups. Patients also exhibited higher SMRs for suicide deaths (schizophrenia, SMR 8.4; 95% CI 7.2–9.6; mood disorder, SMR 2.8; 95% CI 2.1–3.5; mental and behavioral disorder due to psychoactive substance use, SMR 6.8; 95% CI 5.7–7.9). Likewise, younger participants had escalated SMRs, in particular schizophrenia patients.
Table 5. SMRs for all causes and suicide deaths.
| Parameters | Schizophrenia | Mood disorder | Mental and behavioral disorder due to psychoactive substance use | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ED | ES | OD | SMR | 95% CI | OS | SMR | 95% CI | OD | SMR | 95% CI | OS | SMR | 95% CI | OD | SMR | 95% CI | OS | SMR | 95% CI | |
| Total | 458 | 24 | 980 | 2.4 | 2.2–2.5 | 229 | 8.4 | 7.2–9.6 | 5,350 | 1.4 | 1.3–1.5 | 571 | 2.8 | 2.1–3.5 | 1,258 | 2.6 | 2.5–2.8 | 172 | 6.8 | 5.7–7.9 |
| Age, yr | ||||||||||||||||||||
| 15–24 | 7 | 2 | 34 | 12.9 | 11.5–14.4 | 45 | 32.6 | 28.6–36.6 | 47 | 2.4 | 1.8–3.1 | 30 | 4.4 | 3.0–5.9 | 8 | 5.0 | 4.0–5.9 | 4 | 7.1 | 5.2–9.0 |
| 25–34 | 10 | 3 | 84 | 8.6 | 7.8–9.4 | 66 | 17.2 | 15.2–19.2 | 130 | 2.3 | 1.9–2.7 | 82 | 4.3 | 3.3–5.3 | 44 | 5.8 | 5.2–6.5 | 24 | 9.6 | 8.1–11.1 |
| 35–44 | 25 | 4 | 100 | 3.5 | 3.2–3.9 | 55 | 9.6 | 8.2–11.0 | 242 | 1.4 | 1.1–1.6 | 91 | 3.1 | 2.3–3.8 | 165 | 5.4 | 5.0–5.8 | 32 | 6.3 | 5.2–7.4 |
| 45–54 | 47 | 4 | 108 | 2.0 | 1.8–2.2 | 24 | 4.4 | 3.5–5.2 | 430 | 0.9 | 0.7–1.0 | 109 | 2.4 | 1.8–3.1 | 353 | 4.1 | 3.8–4.3 | 47 | 6.0 | 5.0–7.0 |
| 55–64 | 69 | 3 | 132 | 2.0 | 1.9–2.1 | 21 | 5.7 | 4.8–6.5 | 700 | 0.7 | 0.6–0.8 | 99 | 2.0 | 1.5–2.5 | 275 | 2.2 | 2.1–2.3 | 32 | 5.0 | 4.2–5.8 |
| 65–74 | 126 | 4 | 195 | 1.5 | 1.4–1.5 | 14 | 2.2 | 1.8–2.6 | 1,519 | 0.6 | 0.6–0.7 | 97 | 1.3 | 1.0–1.6 | 251 | 1.3 | 1.2–1.4 | 24 | 4.0 | 3.5–4.6 |
| 75 or above | 174 | 2 | 327 | 1.0 | 0.9–1.0 | 4 | 0.6 | 0.4–0.8 | 2,282 | 0.5 | 0.5–0.6 | 63 | 1.0 | 0.8–1.3 | 162 | 0.8 | 0.8–0.8 | 9 | 3.1 | 2.7–3.6 |
| Sex | ||||||||||||||||||||
| Men | 255 | 16 | 520 | 2.3 | 2.2–2.5 | 135 | 7.4 | 6.4–8.4 | 2,659 | 1.7 | 1.6–1.9 | 308 | 3.2 | 2.6–3.9 | 1,105 | 2.8 | 2.7–3.0 | 131 | 5.4 | 4.5–6.2 |
| Women | 202 | 8 | 460 | 2.4 | 2.3–2.6 | 94 | 10.5 | 8.8–12.2 | 2,691 | 1.2 | 1.1–1.4 | 263 | 3.0 | 2.1–3.9 | 153 | 1.3 | 1.2–1.5 | 41 | 8.8 | 7.3–10.3 |
| Income | ||||||||||||||||||||
| Medical aid | 39 | 1 | 162 | 0.7 | 0.6–0.7 | 29 | 3.6 | 2.9–4.2 | 337 | 0.8 | 0.7–0.8 | 29 | 2.5 | 1.9–3.0 | 168 | 1.4 | 1.3–1.5 | 20 | 6.0 | 5.2–6.9 |
| Low | 144 | 9 | 228 | 1.9 | 1.8–2.0 | 61 | 6.7 | 5.7–7.7 | 1,453 | 1.3 | 1.2–1.4 | 158 | 2.3 | 1.7–2.9 | 413 | 2.5 | 2.4–2.7 | 58 | 5.8 | 4.9–6.8 |
| Middle | 154 | 9 | 281 | 2.8 | 2.6–2.9 | 61 | 8.3 | 7.0–9.5 | 1,763 | 1.5 | 1.3–1.6 | 221 | 3.2 | 2.4–3.9 | 439 | 2.9 | 2.7–3.0 | 65 | 7.3 | 6.1–8.5 |
| High | 120 | 5 | 309 | 3.3 | 3.1–3.5 | 78 | 15.0 | 13.1–16.8 | 1,797 | 1.6 | 1.5–1.7 | 163 | 3.3 | 2.4–4.1 | 238 | 2.4 | 2.3–2.6 | 29 | 6.8 | 5.5–8.0 |
| Region | ||||||||||||||||||||
| Seoul/metropolitan cities | 183 | 10 | 444 | 2.7 | 2.5–2.9 | 107 | 9.8 | 8.4–11.2 | 2,350 | 1.6 | 1.5–1.7 | 256 | 3.2 | 2.4–4.0 | 528 | 3.0 | 2.8–3.2 | 77 | 7.8 | 6.6–9.1 |
| Others | 275 | 14 | 536 | 2.1 | 2.0–2.3 | 122 | 7.4 | 6.3–8.5 | 3,000 | 1.2 | 1.1–1.4 | 315 | 2.6 | 1.9–3.2 | 730 | 2.4 | 2.2–2.5 | 95 | 6.1 | 5.1–7.1 |
| CCI | ||||||||||||||||||||
| 0 | 41 | 7 | 167 | 4.3 | 3.9–4.6 | 99 | 12.4 | 11.0–13.8 | 220 | 1.6 | 1.4–1.9 | 96 | 4.5 | 3.6–5.3 | 120 | 4.8 | 4.4–5.1 | 32 | 7.9 | 6.8–9.0 |
| 1 | 46 | 3 | 97 | 2.7 | 2.5–2.9 | 42 | 12.8 | 10.9–14.7 | 288 | 1.3 | 1.1–1.5 | 73 | 4.6 | 3.4–5.7 | 137 | 4.0 | 3.8–4.3 | 25 | 10.3 | 8.6–11.9 |
| 2 | 48 | 4 | 112 | 2.5 | 2.4–2.7 | 34 | 8.4 | 7.1–9.6 | 410 | 1.2 | 1.1–1.3 | 91 | 3.6 | 2.8–4.4 | 135 | 2.7 | 2.5–2.9 | 19 | 5.1 | 4.1–6.0 |
| 3 | 55 | 4 | 130 | 3.0 | 2.8–3.3 | 27 | 7.7 | 6.4–9.0 | 575 | 1.1 | 1.0–1.2 | 86 | 2.5 | 1.8–3.3 | 175 | 2.8 | 2.6–3.0 | 27 | 6.8 | 5.6–8.0 |
| 4 | 48 | 2 | 101 | 2.3 | 2.1–2.4 | 11 | 4.9 | 4.1–5.8 | 574 | 0.8 | 0.7–0.9 | 77 | 2.2 | 1.6–2.7 | 165 | 2.1 | 2.0–2.3 | 24 | 6.2 | 5.2–7.2 |
| 5 | 51 | 2 | 106 | 2.0 | 1.9–2.1 | 9 | 3.4 | 2.7–4.0 | 656 | 0.7 | 0.7–0.8 | 58 | 1.9 | 1.4–2.4 | 117 | 1.3 | 1.2–1.4 | 14 | 4.7 | 3.9–5.5 |
| 6 | 46 | 1 | 70 | 1.3 | 1.3–1.4 | 6 | 3.5 | 2.9–4.1 | 637 | 0.7 | 0.7–0.8 | 42 | 1.7 | 1.3–2.1 | 123 | 1.4 | 1.3–1.4 | 14 | 5.6 | 4.8–6.4 |
| 7 | 122 | 2 | 197 | 1.2 | 1.1–1.2 | 1 | 0.5 | 0.2–0.7 | 1,990 | 0.7 | 0.7–0.7 | 48 | 1.3 | 0.9–1.7 | 286 | 1.0 | 1.0–1.1 | 17 | 4.8 | 4.0–5.6 |
ED = expected deaths, ES = expected suicides, OD = observed deaths, OS = observed suicides, SMR = standardized mortality ratio, CI = confidence interval, CCI = Charlson Comorbidity Index.
DISCUSSION
The results of this study reveal that adults diagnosed with schizophrenia, mood disorder, or mental and behavioral disorder due to psychoactive substance use die at approximately 2.4, 1.4, and 2.6 times the rate of the general population. The results are in line with previous studies in which psychoses were associated with higher mortality risks. A previous study reported significantly higher all-cause mortality for severe mental disorders in French participants (14). In schizophrenia patients, the SMR for all-cause mortality was analyzed to be 2.98 based on a meta-analysis of 38 studies (15). Elevated SMR was also found among late onset schizophrenia patients aged 60 or above, inferring that schizophrenia also increases mortality in old age (16). With regard to mood disorders, all-cause mortality increased 2-fold among Swedish patients with bipolar disorder in prior research (17). Alcohol, drug use, and antisocial personality disorders were also related with a higher risk of death in a study focussing on American participants (5).
Increased mortality risk was also found for suicide deaths, with the SMRs rating 8.4 for schizophrenia, 2.8 for mood disorder, and 6.8 for mental and behavioral disorder due to psychoactive substance use. The study findings are consistent with prior evidence as suicide mortality has been repetitively reported to be high for psychoses patients (18,19). The tendencies toward higher SMRs were particularly pronounced in younger aged groups, particularly for schizophrenia. This may have resulted due to the low expected death rates of younger Korean populations (12) and the fact that schizophrenia patients often exhibit a reduced age of death. In fact, a previous Danish study revealed that schizophrenia patients experience shortened life expectancies, with it being 18.7 years for men and 16.3 years for women (20). Similarly, decreases in life expectancy have also been reported in other United States, Swedish, and Finnish studies and this mortality gap has increased in recent years (20). Apart from age, males had higher suicide mortality risks than females, which is also consistent with prior research (21).
The large health risks observed in individuals diagnosed with schizophrenia, mood disorder, and mental and behavioral disorder due to psychoactive substance use highlight the need for effective medical care provision to psychoses patients. Studies have documented that patients with severe mental disorders are less likely to use general medical services and that these individuals often receive lower quality medical care (17,22). Several explanations have been proposed to elucidate the reasons for disparities in quality of care often received between psychoses and non-psychoses patients. First, patients with mental disorders are frequently unable to effectively communicate with health care providers due to cognitive disturbance or affective instability (23). Furthermore, non-psychiatrist physicians may be biased against psychoses patients, leading to poorer medical management and quality of care (24). Non-psychiatrist providers may also lack experience in treating mental illnesses, which requires the need for adequate cooperation between non-psychiatrists and psychiatrists (25). Psychoses patients with poor socioeconomic status may also have poor access to health services and may face difficulties in receiving adequate medical care (22). Therefore, considering the tendencies of East Asian individuals to express psychiatric problems less frequently, efforts should be made on addressing the risk factors for mortality and to monitor vulnerable groups of individuals in the aim of reducing the mortality gap of psychoses (26).
This study has some limitations. First, the data used in this study classified medical illnesses based on ICD-10 codes. The ICD-10 codes were used to identify and analyze patients diagnosed with schizophrenia, mood disorder, and mental and behavioural disorder due to psychoactive substance use. Other standard classification systems, such as the Diagnostic and Statistical Manual of Mental Disorders (DSM) could not be utilized. Hence, there may have been inaccuracies in diagnoses as recordings were made by different individuals. Second, information was not available on several key risk factors, including education level, smoking status, and alcohol consumption status. Third, because the date of death was only given up to the year and month in the NHI data, there may have been some inaccuracies in estimating date of death. Despite the limitations described above, this study offers insights, as it is the first to investigate excess mortality in Korean psychiatric patients using a large nationally representative sample.
In conclusion, the results of this study confirm that individuals diagnosed with schizophrenia, mood disorder, and mental and behavioral disorder due to psychoactive substance use show excess mortality in Korea. Higher risks of mortality were found for suicide deaths, particularly among younger aged populations. Taking into account the number of psychoses patients and the fact that Korea ranks first among OECD countries in suicide, efforts should be made on targeting and addressing vulnerable groups of individuals to reduce the mortality gap of mental illnesses in the coming decades.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Kim W, Park EC. Data curation: Park EC. Formal analysis: Kim W, Park EC. Supervision: Park EC. Writing - original draft: Kim W, Park EC. Writing - review & editing: Kim W, Park EC, Jang SY, Chun SY, Lee TH, Han KT.
References
- 1.Healy D, Le Noury J, Harris M, Butt M, Linden S, Whitaker C, Zou L, Roberts AP. Mortality in schizophrenia and related psychoses: data from two cohorts, 1875-1924 and 1994-2010. BMJ Open. 2012;2:e001810. doi: 10.1136/bmjopen-2012-001810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dickerson F, Stallings C, Origoni A, Schroeder J, Khushalani S, Yolken R. Mortality in schizophrenia: clinical and serological predictors. Schizophr Bull. 2014;40:796–803. doi: 10.1093/schbul/sbt113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dickerson F, Origoni A, Schroeder J, Schweinfurth LA, Stallings C, Savage CL, Katsafanas E, Banis M, Khushalani S, Yolken R. Mortality in schizophrenia and bipolar disorder: clinical and serological predictors. Schizophr Res. 2016;170:177–183. doi: 10.1016/j.schres.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Eaton WW, Roth KB, Bruce M, Cottler L, Wu L, Nestadt G, Ford D, Bienvenu OJ, Crum RM, Rebok G, et al. The relationship of mental and behavioral disorders to all-cause mortality in a 27-year follow-up of 4 epidemiologic catchment area samples. Am J Epidemiol. 2013;178:1366–1377. doi: 10.1093/aje/kwt219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13:153–160. doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim SW, Yoon JS. Suicide, an urgent health issue in Korea. J Korean Med Sci. 2013;28:345–347. doi: 10.3346/jkms.2013.28.3.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cho MJ, Seong SJ, Park JE, Chung IW, Lee YM, Bae A, Ahn JH, Lee DW, Bae JN, Cho SJ, et al. Prevalence and correlates of DSM-IV mental disorders in South Korean adults: the Korean Epidemiologic Catchment Area Study 2011. Psychiatry Investig. 2015;12:164–170. doi: 10.4306/pi.2015.12.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72:1172–1181. doi: 10.1001/jamapsychiatry.2015.1737. [DOI] [PubMed] [Google Scholar]
- 10.Nordentoft M, Wahlbeck K, Hällgren J, Westman J, Osby U, Alinaghizadeh H, Gissler M, Laursen TM. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS One. 2013;8:e55176. doi: 10.1371/journal.pone.0055176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saku M, Tokudome S, Ikeda M, Kono S, Makimoto K, Uchimura H, Mukai A, Yoshimura T. Mortality in psychiatric patients, with a specific focus on cancer mortality associated with schizophrenia. Int J Epidemiol. 1995;24:366–372. doi: 10.1093/ije/24.2.366. [DOI] [PubMed] [Google Scholar]
- 12.Park S, Kim SY, Hong JP. Cause-specific mortality of psychiatric inpatients and outpatients in a general hospital in Korea. Asia Pac J Public Health. 2015;27:164–175. doi: 10.1177/1010539512452755. [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Lemogne C, Nabi H, Melchior M, Goldberg M, Limosin F, Consoli SM, Zins M. Mortality associated with depression as compared with other severe mental disorders: a 20-year follow-up study of the GAZEL cohort. J Psychiatr Res. 2013;47:851–857. doi: 10.1016/j.jpsychires.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 15.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–1131. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- 16.Talaslahti T, Alanen HM, Hakko H, Isohanni M, Häkkinen U, Leinonen E. Patients with very-late-onset schizoprhenia-like psychosis have higher mortality rates than elderly patients with earlier onset schizophrenia. Int J Geriatr Psychiatry. 2015;30:453–459. doi: 10.1002/gps.4159. [DOI] [PubMed] [Google Scholar]
- 17.Crump C, Sundquist K, Winkleby MA, Sundquist J. Comorbidities and mortality in bipolar disorder: a Swedish national cohort study. JAMA Psychiatry. 2013;70:931–939. doi: 10.1001/jamapsychiatry.2013.1394. [DOI] [PubMed] [Google Scholar]
- 18.Reininghaus U, Dutta R, Dazzan P, Doody GA, Fearon P, Lappin J, Heslin M, Onyejiaka A, Donoghue K, Lomas B, et al. Mortality in schizophrenia and other psychoses: a 10-year follow-up of the ӔSOP first-episode cohort. Schizophr Bull. 2015;41:664–673. doi: 10.1093/schbul/sbu138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee H, Lee K, Koo JW, Park SC. Suicide in patients with schizophrenia: a review on the findings of recent studies. Korean J Schizophr Res. 2015;18:5–9. [Google Scholar]
- 20.Nielsen RE, Uggerby AS, Jensen SO, McGrath JJ. Increasing mortality gap for patients diagnosed with schizophrenia over the last three decades--a Danish nationwide study from 1980 to 2010. Schizophr Res. 2013;146:22–27. doi: 10.1016/j.schres.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 21.Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24:81–90. doi: 10.1177/1359786810385490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roshanaei-Moghaddam B, Katon W. Premature mortality from general medical illnesses among persons with bipolar disorder: a review. Psychiatr Serv. 2009;60:147–156. doi: 10.1176/ps.2009.60.2.147. [DOI] [PubMed] [Google Scholar]
- 23.Bowie CR, Harvey PD. Cognition in schizophrenia: impairments, determinants, and functional importance. Psychiatr Clin North Am. 2005;28:613–633. doi: 10.1016/j.psc.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Jackson JL, Kroenke K. Difficult patient encounters in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med. 1999;159:1069–1075. doi: 10.1001/archinte.159.10.1069. [DOI] [PubMed] [Google Scholar]
- 25.Lester H, Tritter JQ, Sorohan H. Patients’ and health professionals’ views on primary care for people with serious mental illness: focus group study. BMJ. 2005;330:1122–1126. doi: 10.1136/bmj.38440.418426.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park JH, Kim KW. A review of the epidemiology of depression in Korea. J Korean Med Assoc. 2011;54:362–369. [Google Scholar]


