Abstract
Context:
The determinants of over-the-counter (OTC) medication need to be understood to design adequate drug information policies.
Aim:
To determine the prevalence and predictors of OTC medication among the adult population of Berhampur town in Odisha, India.
Settings and Design:
It was a prospective, cross-sectional, observational study carried out in the private retail pharmacy on a convenience sample of 880 adults over a period of 6 months at Berhampur, Odisha, India.
Materials and Methods:
Medication use behavior was explored using a data collection form that had three parts. The first part captured data on the sociodemographic characteristics of drug consumers. The second and third part collected data on drug history and attitude toward the available health-care facility, respectively.
Statistical Analysis:
Descriptive statistics was used to represent the prevalence of OTC medication. Odds ratio and 95% confidence intervals (CIs) were used to determine the predictors of OTC medication.
Results:
The overall prevalence of OTC medication use was 18.72% (95% CI: 15.34–47.16%). Younger age, male gender, lower income, and poor lifestyle were the predictors of OTC medication. Perception of poor accessibility to health care, the presence of chronic diseases and having a symptom count of more than two significantly increased the likelihood of OTC medication (P < 0.05).
Conclusions:
Sociodemographic profile, drug history, and attitude toward health-care availability in the locality can predict OTC medication behavior. Interventions aimed at changing the perceptions of the public regarding accessibility, affordability of the health care is likely to influence OTC medication behavior and make it safer.
Keywords: Health care, over-the-counter medication, predictors, sociodemographic
INTRODUCTION
Over-the-counter (OTC) medication is the use of medicine by a person for treating a perceived or real health problem without consulting a physician.[1] The practice of OTC medication is common in India and many other parts of the world, especially in the economically deprived communities.[2] Many studies have shown that the use of OTC medication is twice as common as that of prescribed medications. Unregulated availability of a wide range of drugs coupled with inadequate health services promotes OTC medication as compared to prescribed drugs.[3] Although OTC medications are of proved efficacy and safety, their side effects and interactions have serious implications, especially in extremes of age, i.e., children, elderly and in special conditions such as pregnancy and lactation.[3,4] It has been reported that the drug use is influenced by the socioeconomic and demographic characteristics of consumers.[5] The high cost of medicines and nonavailability of doctors make health care unaffordable and inaccessible. Consequently, in developing countries, pharmaceutical outlets often serve as the first contact point of healthcare. Identifying the predictors of OTC medication will help to formulate targeted strategies to discourage unnecessary OTC medication, thereby preventing the occurrence of drug-related problems associated with it.
To the best of our knowledge, majority of the existing studies have focused on the socioeconomic determinants of self-medication. With this background, the community-based, cross-sectional, analytical study was carried out to determine the significant sociodemographic as well as drug use history and attitude toward available health care as the predictors of OTC medication.
MATERIALS AND METHODS
Study area
The study site - Berhampur - is one of the major cities in eastern India, in the state of Odisha. The population of in the city has good access to health facilities. There is one government medical college with super specialty and tertiary care hospital, one district Headquarter hospital, many dispensaries, more than 100 pharmacy shops, traditional healers, private, and other nongovernmental organization clinics.
Study design
It was a prospective, cross-sectional, observational study conducted in the pharmacy during the period from April 2015 to September 2015. For the study protocol, OTC medication was defined as the taking of drugs without relevant prescription (i.e., drugs sold without prescription, using an old prescription, or using drugs prescribed for another person).[6]
Ethical approval
The study protocol and patient informed consent procedures were approved by the Institutional Ethics Committee of MKCG Medical College, Berhampur, Odisha (protocol approval number IEC/344/16-02-2015).
Primary and secondary objectives
The primary objective was to find out whether OTC-medication use could be predicted by sociodemographic characteristics of drug consumers such as age, gender, marital status, education, income level, lifestyle, and perceptions on health care available in the locality. The secondary objectives were to find out the prevalence and pattern of OTC medication use.
Sample size calculation
Assuming the prevalence OTC-medication use to be 25% and an absolute precision of 3% at a confidence level of 95% (two-sided), the sample size was calculated to be 800 using nMaster 2.0 (Designed and Developed by Department of Biostatistics, Christian Medical College, Vellore, India). The calculated sample size was increased by 10% to account for nonresponses, resulting in a final sample size of 880.
Sampling techniques
The study was performed at a convenience sample of ten busy retail private pharmacy outlets in the city. The busy pharmacy outlets who volunteered to participate were included in the study. To prevent selection bias, five of the participating pharmacies were selected nearer to the hospitals and another five were selected away from the hospital areas. The total sample size was divided among the ten pharmacy outlets included in the study. Hence, each of the participating pharmacies contributed 88 study subjects. As the rates of hourly visits of customers varied markedly within each day, time slots were defined a priori covering the 24-h day. Subsequently, these predefined time slots, throughout the 6 months of the study period, were randomly allocated for each participating pharmacy using a random digit table. This method was designed to limit the potential for sampling bias. During each data collection session, consecutive customers with a medication request were included in the absence of any exclusion criteria, only after obtaining their written informed consent.
Participant enrolment and data collection
All adult patients or their representatives asking for medicine or presenting a symptom at the participating pharmacy during one of the predefined time slots willing to participate in the study were included in the study. The investigators with one assistant specifically were trained for data collection.
Exclusion criteria
Patients unable to participate because of language barriers, having presented with an unstable medical illness, patients or representatives seeking medication for pediatric population (<14 years), and those declining participate in the study were excluded from the study.
Study tool
Medication behaviors of the study participants were explored using a data collection form that had been previously implemented and pretested on a convenience sample of thirty patients attending two of the participating pharmacies. The clarity and relevance of items were assessed, and certain modifications were made on the basis of the findings of the pretest. The data collection form had three parts. The first part captured data on the sociodemographic characteristics of drug consumers such as age, gender, companionship, level of education, income, and lifestyle. The second part collected data on drug history such as first-time or repeat OTC medication, name of the medication (main active substance), type of ailment, symptom count, presence of chronic illness, use of other drugs, vulnerability to accept lay advice on medicines, etc. The third part recorded data on the attitude of the participants toward the available health-care facility.
Statistical analysis of data
Descriptive statistics was used to represent the study population characteristics and prevalence of OTC medication use. Odds ratio (OR) and 95% confidence intervals (CIs) of the predictor variables for OTC medication were determined for each of the subcategories to study the association between OTC medication and dependent variables. All the data were entered after the dialog with the study participants in the data collection form which was randomly checked for quality and completeness by the investigators. Data were transferred from the case report forms to SPSS version 16.0 (copyright SPSS Inc. 2007, Chicago, IL, USA), and analysis was performed by the investigators.
RESULTS
The overall prevalence of OTC medication use was 18.72% (95% CI: 15.34–47.16%). Among the OTC medication users, 65% were males and 53% were < 45 years of age. Out of the 880 study participants, 165 requested for OTC medication at the pharmacy outlet.
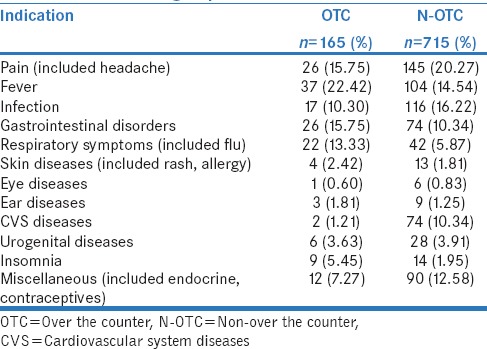
Indications for over-the-counter medication
The most common indication for OTC medication was fever (22.42%) followed by pain (15.75%) and gastrointestinal symptoms (15.75%). The pain was the most common indication (20.27%) followed by infection control (16.22%) for non-OTC medication [Table 1].
Table 1.
Indications for medication in over-the-counter and non-over-the-counter group
Drugs used for over-the-counter medication
Nonsteroidal anti-inflammatory drugs (NSAIDs) (38%), followed by gastrointestinal drugs (16%), cough remedies (14%), and antimicrobials (10%), were the commonly used drugs for OTC medication. OTC medication with atenolol and amlodipine for the treatment of chronic cardiovascular conditions such as hypertension was seen in 1.5% of participants in this group [Table 2].
Table 2.
List of drugs used for over-the-counter medication

Sociodemographic predictors of over-the-counter medication
Males and individuals with a lower income were more likely to use OTC medications with OR: 2.53, 95% CI: 1.72–3.71 and OR: 2.04, 95% CI: 1.42–2.94, respectively. Participants who were either smokers or alcoholic or both were 14 times more likely to use OTC medicines than nonsmokers and nonalcoholics. Younger respondents, with an age <45 years, are more likely to use OTC medication (OR: 1.08, 95% CI: 0.77–1.52) [Table 3].
Table 3.
Sociodemographic predictors of over-the-counter medication

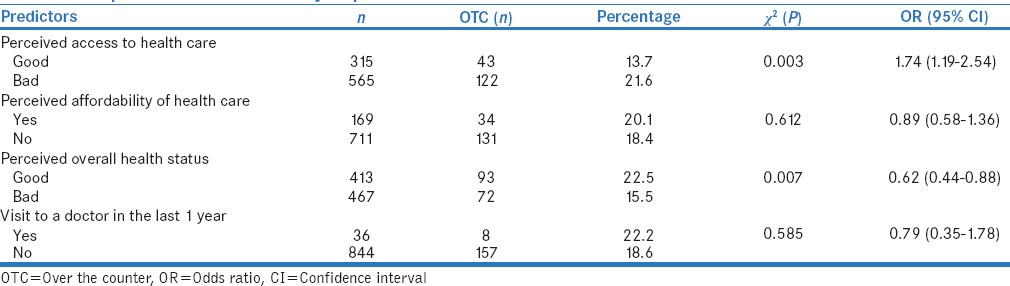
Perception of health-care facility as predictor of over-the-counter medication
Respondents who perceived that their access to health-care facility was poor were 1.74 times likely to use OTC medication (OR 1.74, 95% CI: 1.19–2.54). However, having negative attitudes that the available health care was not affordable, decreased the likelihood of OTC medication use (OR: 0.89, 95% CI: 0.58–1.36) [Table 4].
Table 4.
Perception of health-care facility as predictor of over-the-counter medication
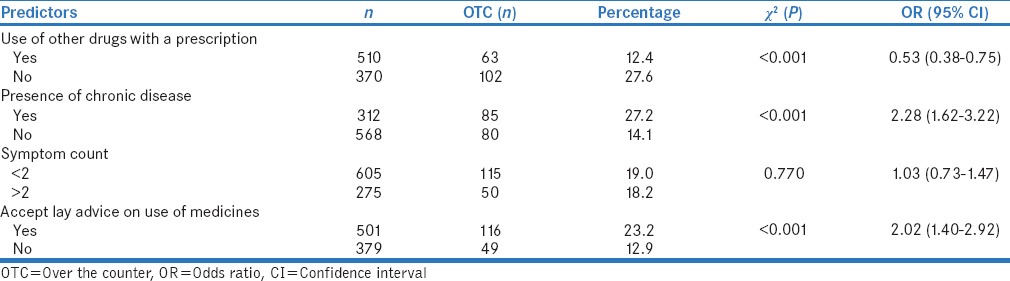
Drug use history as predictor of over-the-counter medication
The respondents who were already taking medicines that were procured using a prescription at the time of the study were less likely to use OTC medication (OR: 0.53, 95% CI: 0.38–0.75) which was a statistically significant (P < 0.001). The presence of chronic diseases such as hypertension, diabetes mellitus significantly (P < 0.05) increased the likelihood of OTC medication use by more than two times (OR: 2.28, 95% CI: 1.62–3.22). It was observed that respondents having a symptom count of more than two were more likely to use OTC medication than those symptom count of < 2 (OR: 1.03, 95% CI: 0.73–1.47). It was observed that those who accepted of lay advice on the use of medicines were significantly more likely to use OTC medicines (P < 0.05) [Table 5].
Table 5.
Drug use history as predictor of over-the-counter medication
DISCUSSION
In the present study, OTC medication was observed in 18.72% of the consumers. In studies done in other developing countries, it has been reported to be between 12.7% and 95% of the consumers.[6,7] The estimates of this study are lower than that of many other studies.[8] This substantiates the fact that there is a wide variation in the prevalence of OTC medication use in the country. This may be due to their varying nature of definitions used, region selected, and methodology adopted. In this study, the lower prevalence of self-medication as compared to other Indian studies may be due to a different study setting, i.e., the pharmacy counter was adapted for sampling.
The most common indication for either medication was fever. Similar observations have been reported where the most commonly used drugs for self-medication were paracetamol (56.5%), followed by drugs for gastrointestinal problems (40.5%), NSAIDs (39.9%).[8,9,10] Similarly, pain followed by respiratory and gastrointestinal complaints were the most frequent symptoms in other studies.[11] This indicates that, universally, pain and fever are the most common symptoms for OTC medication. The observation that NSAIDs were the most common drug category used for OTC medication is corroborated by the findings of other studies done across India.[1,12] In the present study, it was observed that 10% of participants used antibiotics for OTC medication, and this is in contrast to the reports of a study done in South India where the OTC medication of antibiotics was as high as 39.3%.[13]
In this study, individuals with a younger age, male gender, lower income, and presence of proxy indicators of poor lifestyle such as smoking or alcoholism were more likely to use OTC medications, whereas the better educated were less predisposed to use OTC medications. Persons who lived in a family were also less likely to use OTC medicines. In a study done in the West, they have observed a higher prevalence of self-medication in older people.[7] This may be due to the different sociodemographic profiles of the study subjects. In the present study, those who have accepted lay advice on medications are almost twice as likely to use OTC medication. In a study conducted in Pakistan, they have reported that advice of family members was the major source of information on self-medication.[14]
In a systematic review on self-medication behavior, it was identified that contextual factors (education level, economic well-being of the community) and health-care system-related factors (regulation on sale of medicines) were the determinants of self-medication.[15] In the present study, a similar relationship was observed between the OTC use behavior and these factors. Persons with a perception that, they have poor access to health care, persons with chronic diseases, with a greater symptom count were predisposed to use OTC medicines. Many studies have shown that access to health care plays an important role in initiating self-medication behavior.[16,17,18,19] In the context of this study, it was observed that despite the availability of a well-developed public–private health-care network in the study area, the tendency to resort to OTC medication is widely prevalent. When there is a perceived poor access to health care, OTC medication use becomes a low-cost alternative. A lower income increased the likelihood of OTC medication. It indicates that people who are economically weak are less likely to consult a medical practitioner for a medical condition. A similar behavior has been demonstrated in a middle-income area of Brazil.[20] Indian studies have demonstrated that the mean cost of drugs purchased on the prescription of a doctor is almost twice that of drugs procured by OTC to treat a similar illness.[4] In such a situation, financial constraints very likely lead to the use of medicines purchased OTC. The symptom count acts as a proxy measure of the perceived severity of the illness for consumers to make a decision regarding physician consultation. A lower number of symptom count is a proxy measure of less severity of illness emerged as an important predictor of OTC medication use. Consumers with a lower symptom count rely on staff of retail drug stores. This phenomenon has also been observed in other studies.[21]
There are very few studies with a comparable design and setting. Many of the findings of this study were difficult to compare with the observations of other studies because of the divergence of the study designs and population. But still, the predictors enumerated in the study will assist to identify those that are likely to use OTC medication. There are some limitations in the present study, like, it does not describe the situation outside the pharmacy outlets, and hence, it may not be representative in general. The absence of a follow-up component in the study design may have reduced the objective assessment of the OTC medication behavior.
In this study, perceptions toward health care were assessed in a general context. Relating the recent experiences of the respondents of different government schemes related to healthcare and drug distribution would have increased the validity of the study. More importantly, generalization of our study findings to other areas of the country may be limited since OTC medication use is a self-initiated behavior which tends to vary from setting to setting.[22] In spite of the limitations, the results of this study underline that OTC medication behavior can be predicted.
CONCLUSIONS
The results of the study show that OTC medication behavior can be predicted form the sociodemographic profile, drug history, and attitude of an individual toward the available health-care facility. This implies that interventions aimed at changing the perceptions of the public regarding accessibility, affordability of the health care are likely to influence OTC medication behavior. The predictors can be used to implement drug information programs to make OTC medication safer on priority groups who are more likely to use OTC medication.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Montastruc JL, Bagheri H, Geraud T, Lapeyre-Mestre M. Pharmacovigilance of self-medication. Therapie. 1997;52:105–10. [PubMed] [Google Scholar]
- 2.Sclafer J, Slamet LS, de Visscher G. Appropriateness of self-medication: Method development and testing in urban Indonesia. J Clin Pharm Ther. 1997;22:261–72. doi: 10.1046/j.1365-2710.1997.10075100.x. [DOI] [PubMed] [Google Scholar]
- 3.Choonara I, Gill A, Nunn A. Drug toxicity and surveillance in children. Br J Clin Pharmacol. 1996;42:407–10. doi: 10.1046/j.1365-2125.1996.04563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dineshkumar B, Raghuram TC, Radhaiah G, Krishnaswamy K. Profile of drug use in urban and rural India. Pharmacoeconomics. 1995;7:332–46. doi: 10.2165/00019053-199507040-00007. [DOI] [PubMed] [Google Scholar]
- 5.Sharma R, Verma U, Sharma CL, Kapoor B. Selfmedication among urban population of Jammu city. Indian J Pharmacol. 2005;37:37–45. [Google Scholar]
- 6.Shankar PR, Partha P, Shenoy N. Self-medication and non-doctor prescription practices in Pokhara Valley, Western Nepal: A questionnaire-based study. BMC Fam Pract. 2002;3:17. doi: 10.1186/1471-2296-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Figueiras A, Caamaño F, Gestal-Otero JJ. Sociodemographic factors related to self-medication in Spain. Eur J Epidemiol. 2000;16:19–26. doi: 10.1023/a:1007608702063. [DOI] [PubMed] [Google Scholar]
- 8.Phalke VD, Phalke DB, Durgawale PM. Self-medication practices in rural Maharashtra. Indian J Community Med. 2006;31:34–5. [Google Scholar]
- 9.Kaushal J, Gupta MC, Jindal P, Verma S. Self-medication patterns and drug use behavior in housewives belonging to the middle income group in a city in Northern India. Indian J Community Med. 2012;37:16–9. doi: 10.4103/0970-0218.94013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arrais PS, Coelho HL, Batista Mdo C, Carvalho ML, Righi RE, Arnau JM. Profile of self-medication in Brazil. Rev Saude Publica. 1997;31:71–7. doi: 10.1590/s0034-89101997000100010. [DOI] [PubMed] [Google Scholar]
- 11.Eickhoff C, Hämmerlein A, Griese N, Schulz M. Nature and frequency of drug-related problems in self-medication (over-the-counter drugs) in daily community pharmacy practice in Germany. Pharmacoepidemiol Drug Saf. 2012;21:254–60. doi: 10.1002/pds.2241. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad A, Patel I, Mohanta G, Balkrishnan R. Evaluation of self medication practices in rural area of town Sahaswan at Northern India. Ann Med Health Sci Res. 2014;4(Suppl 2):S73–8. doi: 10.4103/2141-9248.138012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar N, Kanchan T, Unnikrishnan B, Rekha T, Mithra P, Kulkarni V, et al. Perceptions and practices of self-medication among medical students in coastal South India. PLoS One. 2013;8:e72247. doi: 10.1371/journal.pone.0072247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khan H, Maheen S, Alamgeer, Abbas G, Mahmood A, Sarfraz RM, et al. Determinants of increasing trend of self-medication in a Pakistani community. [Last accessed on 2015 Oct 15];Trop J Pharm Res 2014;13:437-43. 2014 13:437–43. Available online at http://www.tjpr.org http://dx.doi.org/10.4314/tjpr.v13i3.19 . [Google Scholar]
- 15.Shaghaghi A, Asadi M, Allahverdipour H. Predictors of self-medication behavior: A systematic review. Iran J Public Health. 2014;43:136–46. [PMC free article] [PubMed] [Google Scholar]
- 16.Abosede OA. Self-medication: An important aspect of primary health care. Soc Sci Med. 1984;19:699–703. doi: 10.1016/0277-9536(84)90242-9. [DOI] [PubMed] [Google Scholar]
- 17.Klinkenberg E, Van der Hoek W, Amerasinghe FP, Jayasinghe G, Mutuwatte L, Gunawardane DM. Malaria and land use: A spatial and temporal risk analysis in Southern Sri Lanka. Colombo, Sri Lanka: International Water Management Institute; 2003. [Last accessed on 2015 Oct 15]. Available from: http://www.iwmi.cgiar.org/Publications/IWMI_Research./Report68.pdf . [Google Scholar]
- 18.Shveta S, Jagmohan S. A study of self-medication pattern in Punjab. Indian J Pharm Pract. 2011;4:43–6. [Google Scholar]
- 19.Weerasinghe MC, Gunatunge MW. Self-medication in the Panadura MOH area. J Coll Community Physicians Sri Lanka. 2003;8:27–31. [Google Scholar]
- 20.Sumathipala A, Murray J. New approach to translating instruments for cross-cultural research: A combined qualitative and quantitative approach for translation and consensus generation. Int J Methods Psychiatr Res. 2000;9:87–95. [Google Scholar]
- 21.Zafar SN, Syed R, Waqar S, Zubairi AJ, Vaqar T, Shaikh M, et al. Self-medication amongst university students of Karachi: Prevalence, knowledge and attitudes. J Pak Med Assoc. 2008;58:214–7. [PubMed] [Google Scholar]
- 22.Ahmed SM, Tomson G, Petzold M, Kabir ZN. Socioeconomic status overrides age and gender in determining health-seeking behaviour in rural Bangladesh. Bull World Health Organ. 2005;83:109–17. [PMC free article] [PubMed] [Google Scholar]


