Abstract
Objective
The best strategy in patients with acute ST-segment elevation myocardial infarction (STEMI) with multivessel coronary artery disease (CAD) regarding completeness of revascularisation of the non-culprit lesion(s) is still unclear. To establish which strategy should be followed, survival rates over a longer period should be evaluated. The aim of this study was to investigate whether complete revascularisation, compared with incomplete revascularisation, is associated with reduced short-term and long-term all-cause mortality in patients with first STEMI and multivessel CAD.
Methods
This retrospective study consisted of 518 patients with first STEMI with multivessel CAD. Complete revascularisation (45%) was defined as the treatment of any significant coronary artery stenosis (≥70% luminal narrowing) during primary or staged percutaneous coronary intervention prior to discharge. The primary end point was all-cause mortality.
Results
Incomplete revascularisation was not independently associated with 30-day all-cause mortality in patients with acute first STEMI and multivessel CAD (OR 1.98; 95% CI 0.62to6.37; p=0.25). During a median long-term follow-up of 6.7 years, patients with STEMI with multivessel CAD and incomplete revascularisation showed higher mortality rates compared with patients who received complete revascularisation (24% vs 12%, p<0.001), and these differences remained after excluding the first 30 days. However, in multivariate analysis, incomplete revascularisation was not independently associated with increased all-cause mortality during long-term follow-up in the group of patients with STEMI who survived the first 30 days post-STEMI (HR 1.53 95% CI 0.89-2.61, p=0.12).
Conclusion
In patients with acute first STEMI and multivessel CAD, incomplete revascularisation compared with complete revascularisation was not independently associated with increased short-term and long-term all-cause mortality.
Keywords: All-cause mortality, complete revascularization, multi-vessel disease, primary percutaneous coronary intervention
Key messages.
What is already known about this subject?
Whether incomplete revascularisation in patients with first ST-segment elevation myocardial infarction (STEMI) and multivessel coronary artery disease (CAD) is associated with worse outcome as compared with complete revascularisation remains debated. Current evidence is conflicting; smaller randomised trials demonstrated superior outcome after complete revascularisation, whereas large registries demonstrated no benefit of complete over incomplete revascularisation.
What does this study add?
To establish which strategy should be followed, survival rates over a longer period may be of importance. In this retrospective, observational study, incomplete revascularisation (corrected for baseline characteristics) was not associated with increased short-term and long-term all-cause mortality in patients with first STEMI with multivessel CAD, as compared with complete revascularisation.
How might this impact on clinical practice?
The current retrospective, observational study (with longer term follow-up) supports findings of previous registries (with shorter follow-up), suggesting that complete revascularisation has no benefit on all-cause mortality as compared with incomplete revascularisation in patients with first STEMI with multivessel CAD.
Introduction
Primary percutaneous coronary intervention (PCI) of the culprit vessel in patients with ST-segment elevation myocardial infarction (STEMI) is a standard clinical practice.1 However, in patients with STEMI and multivessel coronary artery disease (CAD), the best revascularisation strategy (complete vs incomplete revascularisation) remains debated. While primary PCI of the infarct-related artery (IRA) should be performed systematically, immediate revascularisation of the non-culprit vessel(s) is/are only recommended in patients with cardiogenic shock or persisting large areas of ischaemia.2 Recent landmark randomised trials such as the CvLPRIT (Complete versus Lesion-only Primary PCI trial), DANAMI-3-PRIMULTI (The Third Danish Study of Optimal Acute treatment of Patients with STEMI:Primary PCI in Multivessel disease) and the PRAMI (Preventive Angioplasty in Acute Myocardial Infarction) trials demonstrated reduced risk of adverse cardiovascular events in patients undergoing immediate complete revascularisation compared with patients with incomplete revascularisation.3–5 In contrast, large observational studies did not show differences in adverse cardiovascular event rates between the two revascularisation strategies.6–8 Furthermore, the effect of complete versus incomplete revascularisation on clinical outcomes has not been evaluated at long-term follow-up (>5 years).9 10
Therefore, the aim of the current retrospective, observational study was to investigate whether incomplete revascularisation, compared with complete revascularisation, is associated with increased short-term and long-term all-cause mortality in patients with acute first STEMI and multivessel CAD.
Methods
Patients
The analysis concerns a retrospective analysis of patients who presented with a first acute STEMI and multivessel CAD at the Leiden University Medical Center (The Netherlands) between 2004 and 2008. The inclusion criteria were: (1) diagnosis of first acute STEMI that was defined as typical chest pain complaints <12 hours, elevated cardiac enzyme levels and significant ST-segment elevation or left bundle branch block on the ECG; (2) multivessel CAD on emergency coronary angiography (CAG) and (3) no history of CAD as defined by previous myocardial infarction, PCI or coronary artery bypass graft. All patients were treated according to the MISSION! protocol as described earlier, which was based on the most recent American College of Cardiology/American Heart Association and European Society of Cardiology guidelines for patients with acute myocardial infarction at that moment.11 The interventional cardiologist determined whether immediate or staged revascularisation of the non-culprit vessel(s) occurred. Patients with (1) emergent or staged revascularisation with coronary artery bypass graft surgery before discharge and (2) incomplete or uninterpretable CAG images were excluded. The primary end point was all-cause mortality. Mortality data were obtained from hospital’s files review or municipal civil registries. Demographic, clinical and angiographic data were prospectively entered in the departmental Cardiology Information System (EPD-Vision; Leiden University Medical Center, The Netherlands) and analysed retrospectively. The Institutional Review Board of the Leiden University Medical Centre approved the retrospective, observational study and waived the need for written informed consent for retrospective analysis of clinically acquired data.
Primary percutaneous coronary intervention and angiographic data analysis
CAG data were acquired from standardised angiographic projections according to the guidelines of the American College of Cardiology/American Heart Association and were stored digitally.12 CAG data were reviewed retrospectively by two experienced observers. During image analysis the following information was reported: (in)complete revascularisation, coronary vessel dominance, culprit vessel, severity of CAD and the results of primary PCI. IRA was determined by the evaluation of acute electrocardiographic changes on the ECG at admission.13 Complete revascularisation was defined as PCI of any significant coronary artery stenosis (≥70% luminal narrowing) of any vessel during the primary or staged PCI prior to discharge.
Statistical analysis
Normally distributed variables were expressed as mean±SD and non-normally distributed variables as median and IQR. Categorical variables were presented as frequencies and percentages. Differences in baseline characteristics between patients with complete revascularisation and patients with incomplete revascularisation were evaluated with the independent samples t-test, the Mann-Whitney U test or the χ2 test when appropriate. Survival analyses were performed using Kaplan-Meier analysis. Cumulative event rates for the end point of all-cause mortality were compared between patients with complete revascularisation and patients with incomplete revascularisation, using the log-rank test. The influence of differences in baseline characteristics on 30-day mortality post-STEMI was assessed by performing univariate and multivariate logistic regression analysis. To avoid any overfitting of the model, only a selection of variables with significant p values (<0.05) at univariate analysis were entered in the multivariate model: age, three-vessel CAD, culprit vessel left main, Killip class ≥2 and incomplete revascularisation. The results of the multivariate analysis were reported as adjusted OR with 95% CI. The independent associates of all-cause mortality at long-term follow-up were investigated using univariate and multivariate Cox regression analysis for those patients who survived the first 30 days. Only variables with significant p-values (<0.05) at univariate analysis were included in the multivariate model: age, diabetes mellitus, family history of CAD, three-vessel CAD, renal dysfunction (estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2), culprit vessel left main and incomplete revascularisation. The results of the multivariate Cox regression analysis were reported as HR and their respective 95% CI. Statistical analysis was performed using SPSS software (Version 22.0). A two-sided p value of <0.05 was considered statistically significant.
Results
Patients
Of 1133 patients with acute first STEMI, 542 had multivessel CAD on CAG. Additionally, 24 patients (4%) were excluded because of revascularisation with coronary artery bypass graft surgery before discharge (n=8) or incomplete or uninterpretable CAG data (n=16). The clinical baseline characteristics of the remaining 518 patients are shown in table 1. The majority of patients were male (76%), with a mean age of 63±12 years and in one-third of the patients emergent CAG showed three-vessel CAD. At presentation, 36 patients (7%) were in Killip class ≥2. Complete revascularisation was performed in 231 patients (45%): in 197 patients (85%) during primary PCI and in 34 patients (15%) during staged revascularisation before discharge. Differences in baseline characteristics between patients with incomplete and complete revascularisation are presented in table 1. Patients who received complete revascularisation before discharge were younger, presented less often with Killip class ≥2, had the left anterior descending coronary artery less often as culprit vessel, had more often two-vessel CAD and had more often preserved renal function as compared with patients who received incomplete revascularisation.
Table 1.
Patient characteristics and angiographic data
| Total N=518 |
Incomplete revascularisation* n=287 |
Complete revascularisation* n=231 |
p Value | |
| Gender (male) | 76% | 74% | 78% | 0.24 |
| Age (years) | 63±12 | 64±13 | 62±12 | 0.02 |
| Obesity (BMI≥30 kg/m2) | 16% | 17% | 15% | 0.41 |
| Diabetes | 12% | 14% | 10% | 0.15 |
| Hypercholesterolaemia† | 17% | 19% | 15% | 0.30 |
| Hypertension‡ | 37% | 40% | 34% | 0.17 |
| Current smoker | 44% | 43% | 45% | 0.58 |
| Family history of CAD | 38% | 38% | 38% | 0.90 |
| Presenting in Killip class≥2 | 7% | 10% | 4% | 0.006 |
| Culprit vessel | ||||
| Left main | 1% | 1% | 2% | 0.50 |
| RCA | 42% | 39% | 45% | 0.20 |
| LAD | 41% | 46% | 35% | 0.02 |
| LCx | 16% | 14% | 18% | 0.19 |
| Three-vessel CAD | 33% | 42% | 22% | <0.001 |
| eGFR ≤60 mL/min/1.73 m² | 13% | 15% | 9% | 0.04 |
| Troponin T level | 4.57 (IQR 1.77–8.93) |
4.91 (IQR 1.86–9.22) |
4.40 (IQR 1.58–8.60) |
0.28 |
| Peak cardiac troponin T level ≥3.5 µg/L | 59% | 61% | 56% | 0.18 |
| LV ejection fraction | 47±10 | 46±10 | 47±10 | 0.07 |
| LV ejection fraction ≤40% | 28% | 31% | 25% | 0.13 |
| Blood pressure at discharge | ||||
| Systolic | 116±17 | 115±16 | 118±18 | 0.10 |
| Diastolic | 70±11 | 69±10 | 71±12 | 0.12 |
| Medication at discharge | ||||
| Beta-blocker | 93% | 92% | 94% | 0.36 |
| Aspirin | 96% | 96% | 97% | 0.75 |
| Clopidogrel | 99% | 99% | 99% | 0.80 |
| ACE inhibitor/ARB | 96% | 96% | 97% | 0.55 |
| Statin | 98% | 98% | 98% | 0.71 |
*Complete revascularisation was defined as treating all present significant coronary artery stenosis ≥70% during primary PCI or before discharge.
†Serum total cholesterol ≥230 mg/dL and/or serum triglycerides ≥200 mg/dL or treatment with lipid-lowering drugs.
‡Defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or the use of antihypertensive medication.
ARB, angiotensin receptor blockers; BMI, body mass index; CAD, coronary artery disease; eGFR, glomerular filtration rate estimated using the Cockroft-Gault formula; LAD, left anterior descending coronary artery; LCx, left circumflex coronary artery; LV, left ventricle; PCI, percutaneous coronary intervention; RCA, right coronary artery; STEMI, ST-segment elevation myocardial infarction.
A two-sided p value of <0.05 was considered statistically significant.
30-Day mortality
In the first 30 days post-STEMI, 31 patients (6%) died (28 during index hospitalisation). The cause of death was cardiac in 27 patients (87%), terminal postanoxic encephalopathy in 1 patient (3%) and unknown reason in 3 patients (10%). The cardiac causes of death were cardiogenic shock (17 patients, 63%), ventricular fibrillation (1 patient, 4%), left-ventricular free wall rupture (1 patient, 4%), terminal heart failure (6 patients, 22%) and reinfarction due to intrastent thrombosis (2 patients, 7%). Table 2 shows the differences in baseline characteristics between the deceased patients and those who survived the first 30 days post-STEMI. The variables (independently) associated with the end point 30-day mortality are shown in table 3. In the multivariate analysis age, Killip class ≥2 and left main coronary artery as the culprit vessel were independently associated with increased 30-day mortality post-STEMI. However, incomplete revascularisation was not independently associated with increased 30-day mortality post-STEMI (OR 1.98 (95% CI 0.62 to 6.37), p=0.25).
Table 2.
Differences in baseline characteristics between patients who died within the first 30 days post-STEMI and those who survived
| Deceased within the first 30 days post-STEMI n=31 |
Survived the first 30 days post-STEMI n=487 |
p Value | |
| Gender (male) | 55% | 77% | 0.005 |
| Age (years) | 74±12 | 62±12 | <0.001 |
| Obesity (BMI≥30 kg/m2) | 29% | 16% | 0.13 |
| Diabetes | 10% | 12% | 0.8 |
| Hypercholesterolaemia* | 14% | 17% | 0.63 |
| Hypertension† | 31% | 37% | 0.49 |
| Current smoker | 32% | 45% | 0.20 |
| Family history of CAD | 11% | 40% | 0.003 |
| Presenting in Killip class≥2 | 61% | 4% | <0.001 |
| Culprit vessel | |||
| Left main | 16% | 0.4% | <0.001 |
| RCA | 29% | 43% | 0.13 |
| LAD | 42% | 41% | 0.91 |
| LCx | 13% | 16% | 0.65 |
| Three-vessel CAD | 55% | 32% | 0.008 |
| Incomplete revascularisation‡ | 77% | 54% | 0.01 |
| eGFR≤60 mL/min/1.73 m2 | 48% | 11% | <0.001 |
| Peak cardiac troponin T level ≥3.5 µg/L | 83% | 58% | 0.01 |
| LV ejection fraction ≤40% | 70% | 27% | <0.001 |
Serum total cholesterol ≥230 mg/dL and/or serum triglycerides ≥200 mg/dL or treatment with lipid-lowering drugs.
Defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or the use of antihypertensive medication.
Complete revascularisation was defined as treating all present significant coronary artery stenosis ≥70% during primary PCI or before discharge.
BMI, body mass index; CAD, coronary artery disease; eGFR, glomerular filtration rate estimated using the Cockroft-Gault formula; LAD, left anterior descending coronary artery; LCx, left circumflex coronary artery; PCI, percutaneous coronary intervention; LV, left ventricle; RCA, right coronary artery; STEMI, ST-segment elevation myocardial infarction.
A two-sided p value of <0.05 was considered statistically significant.
Table 3.
Influence of baseline characteristics on 30-day mortality post-STEMI
| Univariate | Multivariate | |||||
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Gender (male) | 0.36 | 0.17 to 0.75 | 0.006 | |||
| Age (years) | 1.09 | 1.05 to 1.13 | <0.001 | 1.10 | 1.05 to 1.15 | <0.001 |
| Diabetes | 0.85 | 0.25 to 2.91 | 0.80 | |||
| Hypercholesterolaemia* | 0.77 | 0.26 to 2.26 | 0.63 | |||
| Hypertension† | 0.75 | 0.34 to 1.69 | 0.49 | |||
| Current smoker | 0.59 | 0.26 to 1.33 | 0.20 | |||
| Family history of CAD | 0.19 | 0.06 to 0.64 | 0.007 | |||
| Presenting in Killip class≥2 | 38.42 | 16.32 to 90.43 | <0.001 | 29.00 | 10.78 to 77.99 | <0.001 |
| Culprit vessel | ||||||
| Left main | 46.64 | 8.63 to 251.88 | <0.001 | 48.16 | 4.43 to 523.47 | 0.001 |
| RCA | 0.55 | 0.25 to 1.22 | 0.14 | |||
| LAD | 1.05 | 0.50 to 2.18 | 0.91 | |||
| LCx | 0.78 | 0.26 to 2.28 | 0.65 | |||
| Three-vessel CAD | 2.63 | 1.26 to 5.46 | 0.01 | 0.90 | 0.33 to 2.44 | 0.84 |
| Incomplete revascularisation‡ | 2.92 | 1.24 to 6.91 | 0.02 | 1.98 | 0.62 to 6.37 | 0.25 |
| eGFR ≤60 mL/min/1.73 m2 | 7.31 | 2.96 to 18.02 | <0.001 | |||
| Peak cardiac troponin T level ≥3.5 µg/L | 3.69 | 1.24 to 10.95 | 0.02 | |||
| LV ejection fraction ≤40% | 6.43 | 2.42 to 17.11 | <0.001 | |||
CAD, coronary artery disease; eGFR, glomerular filtration rate estimated using the Cockroft-Gault formula; LAD, left anterior descending coronary artery; LCx, left circumflex coronary artery; LV, left ventricle; PCI, percutaneous coronary intervention; RCA, right coronary artery; STEMI, ST-segment elevation myocardial infarction.
Serum total cholesterol ≥230 mg/dL and/or serum triglycerides ≥200 mg/dL or treatment with lipid-lowering drugs.
Defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or the use of antihypertensive medication.
Complete revascularisation was defined as treating all present significant coronary artery stenosis ≥70% during primary PCI or before discharge.
A two-sided p value of <0.05 was considered statistically significant.
Long-term follow-up
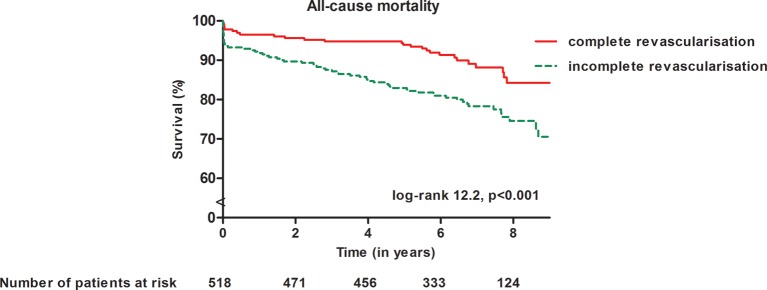
Long-term follow-up was complete in all patients with a median follow-up of 6.7 years (IQR 5.6–7.9 years). Ninety-eight patients died; 67 of them (68%) died after 30 days post-STEMI. The Kaplan-Meier survival curves stratified according to complete versus incomplete revascularisation are presented in figure 1. Patients with STEMI with multi-vessel CAD and incomplete revascularisation showed higher mortality rates compared with patients who received complete revascularisation (24% vs 12%, p<0.001).
Figure 1.
Kaplan-Meier curves for the end point all-cause mortality in the total patient population stratified according to complete/incomplete revascularisation. Patients with incomplete revascularisation had a statistically significant higher cumulative incidence of all-cause mortality (p (log-rank)<0.001) during long-term follow-up after ST-segment elevation myocardial infarction in comparison with patients with complete revascularisation.
The cumulative mortality rates at 1, 2 and 5 years of follow-up were significantly higher for patients who were treated with incomplete revascularisation compared with patients who underwent complete revascularisation (9.8%,12.2% and 18.8% vs 4.3%, 5.2% and 6.9%, respectively, p=0.02, p=0.006 and p<0.001, respectively). After excluding the patients who died within the first 30 days from the analysis, incomplete revascularisation was associated with worse long-term survival compared with complete revascularisation (p=0.012; figure 2). However, multivariate Cox regression analysis showed that incomplete revascularisation was not independently associated with increased all-cause mortality (table 4). Age and left main coronary artery as the culprit vessel were independently associated with the end point of all-cause mortality. After excluding patients presenting in cardiogenic shock (Killip class 4) on the day of admission (n=7), incomplete revascularisation was not independently associated with increased all-cause mortality (HR 1.56 (95% CI 0.91 to 2.69), p=0.11, see online supplementary table 1).
Figure 2.
Kaplan-Meier curve for all-cause mortality in the subgroup of survivors of the first 30 days after STEMI stratified according to complete/incomplete revascularisation. The survivors of the first 30 days post-STEMI with incomplete revascularisation compared with patients with complete revascularisation had a statistically significant higher cumulative incidence of all-cause mortality (p (log-rank)=0.012) during long-term follow-up after STEMI. STEMI, ST-segment elevation myocardial infarction.
Table 4.
Cox regression analysis for all-cause mortality during long-term follow-up in the group of patients with STEMI who survived the first 30 days post-STEMI
| Univariate | Multivariate | |||||
| HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Gender (male) | 0.99 | 0.56 to 1.73 | 0.96 | |||
| Age (years) | 1.07 | 1.04 to 1.09 | <0.001 | 1.05 | 1.03 to 1.08 | <0.001 |
| Diabetes | 2.28 | 1.27 to 4.12 | 0.006 | 1.82 | 0.99 to 3.34 | 0.054 |
| Hypercholesterolaemia* | 0.46 | 0.20 to 1.06 | 0.07 | |||
| Hypertension† | 1.20 | 0.74 to 1.96 | 0.46 | |||
| Current smoker | 0.91 | 0.56 to 1.48 | 0.71 | |||
| Family history of CAD | 0.57 | 0.33 to 0.97 | 0.04 | 0.75 | 0.43 to 1.32 | 0.32 |
| Presenting in Killip class≥2 | 1.47 | 0.53 to 4.05 | 0.46 | |||
| Culprit vessel | ||||||
| Left main | 9.49 | 2.31 to 38.94 | 0.002 | 8.40 | 1.89 to 37.39 | 0.005 |
| RCA | 0.86 | 0.52 to 1.40 | 0.54 | |||
| LAD | 1.24 | 0.77 to 2.00 | 0.39 | |||
| LCx | 0.71 | 0.34 to 1.48 | 0.35 | |||
| Three-vessel CAD | 1.95 | 1.21 to 3.16 | 0.006 | 1.34 | 0.80 to 2.23 | 0.26 |
| eGFR ≤60 mL/min/1.73 m2 | 2.50 | 1.40 to 4.44 | 0.002 | 0.93 | 0.48 to 1.80 | 0.83 |
| Peak cardiac troponin T level ≥3.5 µg/L | 1.31 | 0.79 to 2.17 | 0.30 | |||
| LV ejection fraction ≤40% | 1.43 | 0.85 to 2.41 | 0.18 | |||
| Medication at discharge | ||||||
| Beta-blocker | 0.75 | 0.30 to 1.87 | 0.54 | |||
| Aspirin | 0.50 | 0.18 to 1.37 | 0.18 | |||
| Clopidogrel | 20.28 | 0.00 to 4,6·107 | 0.69 | |||
| ACE inhibitor/ARB | 0.76 | 0.24 to 2.42 | 0.64 | |||
| Statin | 0.81 | 0.11 to 5.86 | 0.84 | |||
| Incomplete revascularisation‡ | 1.91 | 1.14 to 3.20 | 0.01 | 1.53 | 0.89 to 2.61 | 0.12 |
ARB, angiotensin receptor blockers; eGFR, glomerular filtration rate estimated using the Cockroft-Gault formula; LAD, left anterior descending coronary artery; LCx, left circumflex coronary artery; LV, left ventricle; PCI, percutaneous coronary intervention; RCA, right coronary artery; STEMI, ST-segment elevation myocardial infarction.
Serum total cholesterol ≥230 mg/dL and/or serum triglycerides ≥200 mg/dL or treatment with lipid-lowering drugs.
Defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or the use of antihypertensive medication.
Complete revascularisation was defined as treating all present significant coronary artery stenosis ≥70% during primary PCI or before discharge.
openhrt-2016-000541supp001.pdf (140.2KB, pdf)
Discussion
This study showed that patients with first acute STEMI and multivessel CAD who were treated with incomplete revascularisation had higher mortality rates at 30-day and long-term follow-up compared with patients who underwent complete revascularisation. However, after correcting for relevant clinical variables, incomplete revascularisation was not independently associated with increased all-cause mortality.
Prevalence of multivessel CAD and percutaneous revascularisation strategies
Multivessel CAD is present in 45%–55% of patients presenting with acute STEMI and is associated with 1.5-fold higher 30-day mortality rate compared with patients with STEMI with single-vessel CAD.8 14–17 It has been hypothesised that complete revascularisation may improve the outcomes of patients with STEMI with multivessel CAD. However, the results of various registries and randomised trials are conflicting.3 4 7 9 The randomised CvLPRIT trial demonstrated in 296 patients with STEMI with multivessel CAD a significant reduction of the combined end point consisting of all-cause mortality, recurrent myocardial infarction or heart failure in the complete revascularisation group compared with the IRA-only PCI group (4.7% and 13%; p=0.025).4 However, data of the large National CV Data Registry from the USA that involved 28 936 patients with STEMI with multivessel CAD, demonstrated a significantly higher mortality rate in patients with multivessel PCI (n=3134) in comparison with IRA-only PCI (n=25 802) (7.9% and 5.1%, respectively; p<0.01).7 After adjusting for potential confounders, complete revascularisation was not independently associated with increased risk of all-cause mortality.
Current guidelines recommend to consider complete revascularisation in selected patients with STEMI and multi-vessel CAD (class IIb, level of evidence B).2 In this study, 45% of the patients with STEMI and multivessel CAD underwent complete revascularisation (85% during primary PCI) before hospital discharge. In other registries, the rates of complete revascularisation varied between 11% and 30%.7 18 19 The disparities in complete revascularisation rates across the several studies may be explained by differences in patient populations and operator decision making. In this study, patients with complete revascularisation before discharge were younger, presented less often with Killip class ≥2, had the left anterior descending coronary artery less often as culprit vessel, had more often two-vessel CAD and had more often preserved renal function. This is in agreement with the National CV Data Registry where patients with complete revascularisation were more likely to be younger or presenting with cardiogenic shock.7
Incomplete revascularisation and 30-day mortality
In the current study, independent associates for the end point of 30-day mortality in patients with first STEMI with multivessel CAD were higher age, Killip class ≥2 and left main as culprit vessel. These observations are in line with the SHOCK trial, which demonstrated a high mortality rate in patients with acute myocardial infarction complicated by cardiogenic shock and lower prevalence of left main disease for in-hospital survivors.20 However, similar to other large registries, incomplete revascularisation was not independently associated with the end point of 30-day mortality in patients with first STEMI and multivessel CAD.7 8 18 20 The EUROTRANSFER Registry (European Registry on STEMI Patients Transferred for PCI with Upstream Use of Abciximab), including 777 patients with STEMI and multivessel CAD, showed that multivessel PCI (n=70) compared with IRA-only PCI (n=707) was associated with a higher risk of death at 30-day follow-up (12.9% vs 5.9%, respectively, p=0.04).8 However, this difference in mortality rate was no longer statistically significant after adjustment for covariates (adjusted OR 2.42 (95% CI 0.96 to 6.06)). Similar findings were reported by the large National CV Data Registry from the USA.7
These findings contrast with the results of two recent randomised trials demonstrating short-term benefit of complete revascularisation in comparison with incomplete revascularisation in patients with acute STEMI with multivessel CAD.3 4 The PRAMI trial enrolled 465 patients with STEMI with multivessel CAD randomly assigned to multivessel PCI (n=234) or IRA-only PCI (n=231) and compared the groups for the occurrence of combined end point of cardiac death, non-fatal myocardial infarction or refractory angina.3 This study was prematurely terminated because of a highly statistically significant difference (p<0.001) in the primary outcome, favouring multivessel PCI. Complete revascularisation was associated with risk reduction within 6 months after the procedure in comparison with the IRA-only PCI. These findings were similar to those reported by the CvLPRIT trial investigators.4 In this open-labelled randomised study, the impact of complete revascularisation at index admission (n=150) on short-term outcomes was compared with IRA-only PCI (n=146). At 30-day follow-up, patients allocated to the complete revascularisation arm showed lower rates of all-cause mortality, recurrent myocardial infarction, heart failure and ischaemic driven revascularisation compared with patients treated with PCI of the IRA-only (HR 0.45 (95% CI 0.19 to 1.04); p=0.055). These conflicting results may be explained by patient characteristics and selection bias. Patients included in the registries showed higher risk (older age, associated comorbidities and higher frequency of cardiogenic shock) compared with those included in the randomised trials.
A large meta-analysis by Moretti et al 21 demonstrated that the only benefit of complete revascularisation in patients with STEMI with multivessel CAD during short-term follow-up (1 year) related to less repeated revascularisation compared with patients with IRA-only revascularisation.
Incomplete revascularisation and long-term follow-up
Data on the impact of complete revascularisation in patients with STEMI with multivessel CAD on long-term outcome are limited. The PRAMI trial showed a non-significant risk reduction of cardiac death in the multivessel PCI group (n=234) in comparison with the IRA-only PCI (n=231) during a mean follow-up of 23 months (HR 0.34; 95% CI 0.11 to 1.08; p=0.07).3 Similar findings were reported by the DANAMI-3-PRIMULTI which showed no significant difference in all-cause mortality in 627 patients randomly allocated to no further invasive treatment or to complete fractional flow reserve (FFR)-guided revascularisation before discharge (HR 1.40; 95% CI 0.63 to 3.00, p=0.43).5 Furthermore, in a study including 214 patients with STEMI with multivessel CAD, there were no differences in mortality rates at 2.5 years follow-up between IRA-only PCI, staged revascularisation and complete revascularisation during primary PCI (15.5%, 6.2% and 9.2% respectively, p=0.17).10 In addition, Hannan et al9 showed comparable 12-, 24- and 42-month mortality rates in patients with IRA-only PCI (n=503) and multivessel PCI (n=503). After exclusion of patients with haemodynamic instability, left-ventricular ejection fraction ≤20% and malignant-ventricular arrhythmia, there were no differences in mortality rates between the two groups.
The results of this study are in line with the above-mentioned studies. Patients with STEMI with multivessel CAD who received incomplete revascularisation showed an increased long-term mortality rate compared with patients who underwent complete revascularisation (24% vs 12%, p<0.001). However, multivariate analysis showed that incomplete revascularisation was not independently associated with increased all-cause mortality.
The results of the COMPLETE trial (ClinicalTrials.gov Identifier NCT01740479), including more than 3900 patients who will be randomised and followed-up during a mean of 4 years, may shed light on this clinically relevant question.
Limitations
This study has some limitations that need to be addressed. First, this is a retrospective study. Second, patients with cardiogenic shock were not all completely revascularised. Following current guidelines, in this subgroup of patients, if there were truly critical (≥90%) stenoses or highly unstable lesions and if there was persistent ischaemia after PCI of the culprit lesion, complete revascularisation was performed.2 However, non-culprit lesions without critical stenoses were not routinely stented.2 Additional analysis after excluding patients in cardiogenic shock at the time of admission demonstrated similar results: incomplete revascularisation was not independently associated with increased all-cause mortality during long-term follow-up. Third, the characteristics of the stents used during PCI in the current study were not taken into account. Furthermore, the presence of chronic total occlusions of the coronary arteries was not recorded. In addition, to avoid misclassification of the cause of death, this study investigated only all-cause mortality.22 Moreover, although patients are advised to follow a cardiac rehabilitation programme after hospital discharge, data on adherence to these programmes were not available, and this could have influenced the survival rate.
Conclusion
Incomplete revascularisation in patients with acute first STEMI and multivessel CAD was not independently associated with increased short-term and long-term all-cause mortality.
Footnotes
Contributors: All authors have contributed significantly to the submitted work and approved submission of the manuscript.
Funding: The Department of Cardiology has received research grants from Biotronik, Medtronic, Boston Scientific Corporation and Edwards Lifesciences.
Competing interests: VD received speaking fees from Abbott Vascular.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional unpublished data is available without consulting the authors.
References
- 1. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003;361:13–20. 10.1016/S0140-6736(03)12113-7 [DOI] [PubMed] [Google Scholar]
- 2. Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the task force on myocardial revascularization of the European society of cardiology (ESC) and the European Association for cardio-thoracic surgery (EACTS) developed with the special contribution of the European Association of percutaneous cardiovascular interventions (EAPCI). Eur Heart J 2014;35:2541–619. 10.1093/eurheartj/ehu278 [DOI] [PubMed] [Google Scholar]
- 3. Wald DS, Morris JK, Wald NJ, et al. ; PRAMI Investigators. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med 2013;369:1115–23. 10.1056/NEJMoa1305520 [DOI] [PubMed] [Google Scholar]
- 4. Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol 2015;65:963–72. 10.1016/j.jacc.2014.12.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Engstrøm T, Kelbæk H, Helqvist S, et al. ; DANAMI-3—PRIMULTI Investigators. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet 2015;386:665–71. 10.1016/S0140-6736(15)60648-1 [DOI] [PubMed] [Google Scholar]
- 6. Bainey KR, Mehta SR, Lai T, et al. Complete vs culprit-only revascularization for patients with multivessel disease undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. Am Heart J 2014;167:1–14. 10.1016/j.ahj.2013.09.018 [DOI] [PubMed] [Google Scholar]
- 7. Cavender MA, Milford-Beland S, Roe MT, et al. Prevalence, predictors, and in-hospital outcomes of non-infarct artery intervention during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (from the National Cardiovascular Data Registry). Am J Cardiol 2009;104:507–13. 10.1016/j.amjcard.2009.04.016 [DOI] [PubMed] [Google Scholar]
- 8. Dziewierz A, Siudak Z, Rakowski T, et al. Impact of multivessel coronary artery disease and noninfarct-related artery revascularization on outcome of patients with ST-elevation myocardial infarction transferred for primary percutaneous coronary intervention (from the EUROTRANSFER Registry). Am J Cardiol 2010;106:342–7. 10.1016/j.amjcard.2010.03.029 [DOI] [PubMed] [Google Scholar]
- 9. Hannan EL, Samadashvili Z, Walford G, et al. Culprit vessel percutaneous coronary intervention versus multivessel and staged percutaneous coronary intervention for ST-segment elevation myocardial infarction patients with multivessel disease. JACC Cardiovasc Interv 2010;3:22–31. 10.1016/j.jcin.2009.10.017 [DOI] [PubMed] [Google Scholar]
- 10. Politi L, Sgura F, Rossi R, et al. A randomised trial of target-vessel versus multi-vessel revascularisation in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart 2010;96:662–7. 10.1136/hrt.2009.177162 [DOI] [PubMed] [Google Scholar]
- 11. Liem S-S, van der Hoeven BL, Oemrawsingh PV, et al. MISSION!: optimization of acute and chronic care for patients with acute myocardial infarction. Am Heart J 2007;153:14.e1–14.e11. 10.1016/j.ahj.2006.10.002 [DOI] [PubMed] [Google Scholar]
- 12. Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee on coronary angiography). Developed in collaboration with the society for cardiac angiography and interventions. J Am Coll Cardiol 1999;33:1756–824. [DOI] [PubMed] [Google Scholar]
- 13. Cowley MJ, Vandermael M, Topol EJ, et al. Is traditionally defined complete revascularization needed for patients with multivessel disease treated by elective coronary angioplasty? Multivessel Angioplasty Prognosis Study (MAPS) Group. J Am Coll Cardiol 1993;22:1289–97. [DOI] [PubMed] [Google Scholar]
- 14. Dirksen MT, Vink MA, Suttorp MJ, et al. ; Paclitaxel-Eluting Stent versus Conventional Stent, in Myocardial Infarction with ST-Segment Elevation (PASSION) investigators. Two year follow-up after primary PCI with a paclitaxel-eluting stent versus a bare-metal stent for acute ST-elevation myocardial infarction (the PASSION trial): a follow-up study. EuroIntervention 2008;4:64–70. 10.4244/EIJV4I1A12 [DOI] [PubMed] [Google Scholar]
- 15. Mehta RH, O'neill WW, Harjai KJ, et al. ; Primary Angioplasty in Myocardial Infarction (PAMI) and the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) Investigators. Prediction of one-year mortality among 30-day survivors after primary percutaneous coronary interventions. Am J Cardiol 2006;97:817–22. 10.1016/j.amjcard.2005.09.131 [DOI] [PubMed] [Google Scholar]
- 16. Park HW, Yoon CH, Kang SH, et al. ; KAMIR/KorMI Registry. Early- and late-term clinical outcome and their predictors in patients with ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction. Int J Cardiol 2013;169:254–61. 10.1016/j.ijcard.2013.08.132 [DOI] [PubMed] [Google Scholar]
- 17. Park DW, Clare RM, Schulte PJ, et al. Extent, location, and clinical significance of non-infarct-related coronary artery disease among patients with ST-elevation myocardial infarction. JAMA 2014;312:2019–27. 10.1001/jama.2014.15095 [DOI] [PubMed] [Google Scholar]
- 18. Santos AR, Piçarra BC, Celeiro M, et al. ; Investigadores do Registo Nacional de Síndromes Coronárias Agudas. Multivessel approach in ST-elevation myocardial infarction: impact on in-hospital morbidity and mortality. Rev Port Cardiol 2014;33:67–73. 10.1016/j.repce.2013.07.015 [DOI] [PubMed] [Google Scholar]
- 19. Corpus RA, House JA, Marso SP, et al. Multivessel percutaneous coronary intervention in patients with multivessel disease and acute myocardial infarction. Am Heart J 2004;148:493–500. 10.1016/j.ahj.2004.03.051 [DOI] [PubMed] [Google Scholar]
- 20. Webb JG, Lowe AM, Sanborn TA, et al. ; SHOCK Investigators. Percutaneous coronary intervention for cardiogenic shock in the SHOCK trial. J Am Coll Cardiol 2003;42:1380–6. 10.1016/S0735-1097(03)01050-7 [DOI] [PubMed] [Google Scholar]
- 21. Moretti C, D'Ascenzo F, Quadri G, et al. Management of multivessel coronary disease in STEMI patients: a systematic review and meta-analysis. Int J Cardiol 2015;179:552–7. 10.1016/j.ijcard.2014.10.035 [DOI] [PubMed] [Google Scholar]
- 22. Lauer MS, Blackstone EH, Young JB, et al. Cause of death in clinical research: time for a reassessment? J Am Coll Cardiol 1999;34:618–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2016-000541supp001.pdf (140.2KB, pdf)