Abstract
Aim: To evaluate outcomes after implementing the women's health assessment tool (WHAT) and clinical decision support toolkit during annual well-women visits. Methods: An observational project involved women aged 45–64 years attending one of three medical sites in Washington (WA, USA). Responses to the WHAT questionnaire and patients' health resource utilization prepost toolkit implementation were analyzed. Results: A total of 110 women completed the WHAT questionnaire. Majority of women were postmenopausal (77.3%) and experienced depressive mood (63.6%), hot flashes (61.8%) or anxiety (60.9%) in the last 3 months. There was a 72.2% increase in the number of diagnoses made during the annual visit versus the previous 12 months. Conclusion: The WHAT/clinical decision support toolkit helped identify conditions relevant to mid-life women.
Keywords: clinical decision support system, health outcome, menopause
Background
As women enter mid-life, aged 45–64 years, many experience hormonal changes related to menopause transition resulting in new health issues. Some of the most common conditions among mid-life women include vasomotor symptoms (VMS), vulvovaginal atrophy (VVA), urinary incontinence (UI) and depression; with prevalence rates ranging from 10–80% of women [1–4]. Women can also suffer from other negative consequences associated with these conditions such as increased anxiety, sexual dysfunction and increased stress which can have a significant impact on women's health and overall health-related quality of life [4,5].
Despite the prevalence and impact of these conditions on mid-life women, research has shown that the healthcare needs of mid-life women are often overlooked or underprioritized due to other healthcare concerns in busy clinical practices [4,6]. One study found that only 30% of women aged 40–64 years reported seeking healthcare for their menopausal symptoms within the last 12 months [7]. Additionally, the infrequency of patient visits and the expansive list of topics to cover present doctors with challenges in prioritization during a patient's annual visit [8]. Computer-based instruments linked to electronic health record (EHR) systems such as computer-based clinical decision support (CDS) or online assessment tools have been developed and implemented in primary care to address these issues and have been shown to improve delivery of care and patient outcomes [9–11].
Given that mid-life women, aged 45–64 years, comprise the largest and fastest-growing population segment in the USA [12,13], an electronic health assessment instrument, the women's health assessment tool (WHAT)/ CDS toolkit, was recently developed to address these issues in the care of mid-life women (45–64 years of age). The WHAT/CDS toolkit is comprised of two components. The first is the WHAT, a 35-item patient self-reported questionnaire that assesses health conditions relevant to mid-life women. The WHAT questionnaire uses both existing measures and newly developed questions to evaluate highly prevalent symptoms such as hot flashes, depressive mood, anxiety, sexual dysfunction, vaginal dryness, bladder problems and breast pain which are commonly linked to diagnoses of UI, depression, VVA and VMS. Three previously validated measures that are included in the WHAT: the patient health questionnaire-9 (PHQ-9), the generalized anxiety disorder-2 (GAD-2) scale, 3 incontinence questions (3IQ), as well as a few questions from the female sexual function index-6 item (FSFI-6) [14–17]. The WHAT is administered through MyChart, an Epic Systems Corporation (WI, USA) patient portal of the EHR systems.
The second component of the WHAT/CDS toolkit is the CDS toolkit. The CDS toolkit is built within the EHR that support delivery of evidence-based care and shared decision-making. The CDS toolkit is comprised of condition-based components called SmartSets which provide information on diagnoses, laboratory tests, procedures/diagnostic tests, referrals and patient instructions/information as well as best practice alerts, which alert providers of additional questions to consider based on the patient's responses to the WHAT questionnaire. In addition, relevant information from the EHR including prior history, laboratories, imaging studies, reports in the form of discrete data or links to a section in the EHR are generated for the provider.
The main purpose of this pilot project was to evaluate the outcomes of implementing the WHAT/CDS toolkit at three clinical sites of an integrated delivery network (IDN) in Washington state through analysis of the responses to the WHAT questionnaire and EHR data collected from the WHAT/CDS toolkit. A secondary objective of this pilot project was to compare patients' diagnosis and health resource utilization (HRU) including tests, procedures, referral and follow-up visits 1 year before and after the implementation of the WHAT/CDS toolkit.
Methods
This was a prospective data collection pilot project involving mid-life women who attended one of the three participating clinical sites of the IDN serving communities in the South Puget Sound area of Washington state. To be eligible for participation, women were required to be existing 45–64-year-old female patients and registered MyChart users who were scheduled for an annual well-woman visit between 1 March and 31 July 2014. This pilot project was reviewed and approved by the Institutional Review Board of the participating IDN prior to patient recruitment and data collection.
Data collection
Eligible women were informed of the pilot project when scheduling their annual well-woman visit. They were then sent an email through their MyChart patient portal 1 week prior to their scheduled annual visit asking them to complete the WHAT questionnaire online. Women who had not completed the WHAT questionnaire 48 h prior to their scheduled well-woman visit received a reminder email at that time. Upon opening the WHAT, the first screen was an informed consent detailing the purpose and objectives of the pilot project. Each patient had to provide consent to participate before being allowed to proceed to the WHAT questionnaire.
After completing the WHAT questionnaire, the responses were directly uploaded to the patient's EHR and were available for review by their healthcare provider prior to their well-woman visit. During the well-woman visit, relevant data from EHR such as previous diagnoses or laboratory tests and SmartSets, which provided a list of relevant action steps associated with a specific condition, were available to providers. Best practice alerts were also triggered during the patient's annual well-woman visit based on the responses to the WHAT questionnaire. All data collected through the CDS toolkit were also imbedded into the patients' EHR.
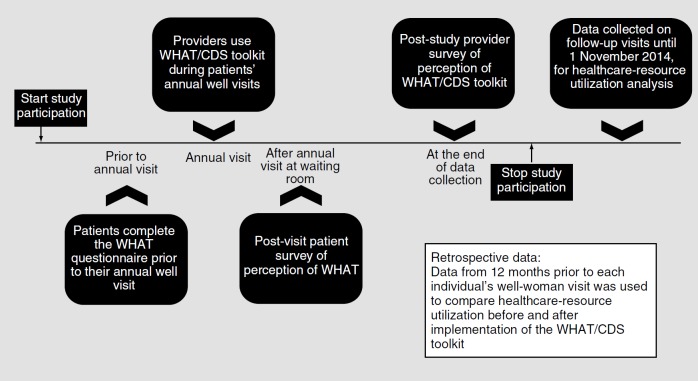
At the conclusion of the data collection period, a retrospective analysis of EHR data collected during the well-woman visit and the 12 months prior to the patient's well-woman visit was conducted for patients who completed the WHAT. The analysis intended to assess changes in patients' HRU, namely diagnoses, diagnostic tests and procedures, laboratory tests and referrals, before and after the implementation of WHAT/CDS toolkit. The patients' HRU focused on comparing patients' diagnosis, diagnostic tests/procedures, laboratory tests and follow-up visits. Figure 1 provides an overview of the data collection process.
Figure 1.
Women's health assessment tool project design.
CDS: Clinical decision support; WHAT: Women's health assessment tool.
Data analysis
All analyses were conducted using SAS version 9.4 [18]. Descriptive summary statistics (n, percentage, mean, standard deviation [SD] or range, as appropriate) were used to characterize the patient sociodemographic and clinical characteristics. Descriptive statistics were also used to examine the WHAT questionnaire responses and HRU data collected during the annual well-woman visit. The PHQ-9, GAD-2 and 3IQ were scored using the scoring algorithm for each instrument. Condition-specific (UI, depression, VVA and VMS) analyses were conducted for all HRU data. If patients had more than one diagnosis (e.g., UI and VMS), the HRU would be counted in both diagnosis tables as it was not possible to discern which condition the resource was attributable. Changes in HRU parameters such as diagnoses, referrals and follow-up visits from the prior year's visit to the current annual well-woman visit were analyzed using descriptive statistics (n, percentage). No missing data were imputed.
Results
Over the recruitment period, 370 women were asked to participate in the pilot project with 110 completing the WHAT questionnaire (29.7% response rate). Women mean age was 54.3 years (SD: 5.9; range: 45–64 years); the majority were white (90.0%) (Table 1). Prior to their well-woman visit, the women's most common comorbid conditions included diseases of the musculoskeletal system and connective tissue such as osteoarthritis and joint pain. This was followed by endocrine, nutritional and metabolic diseases, immunity disorders and gynecological diseases of the genitourinary tract (Table 1).
Table 1.
Demographic and clinical characteristics.
| Variables | Total sample (n = 110) |
|---|---|
| Age (years): | |
| – Mean (SD) | 54.3 (5.9) |
| – Range (min-max) | 45.0–64.0 |
| Race, n (%): | |
| – American–Indian or Alaska Native | 1 (0.9) |
| – Asian | 3 (2.7) |
| – Black or African–American | 5 (4.5) |
| – Hawaiian or Pacific Islander | 1 (0.9) |
| – White or Caucasian | 99 (90.0) |
| – Hispanic or Latino | 1 (0.9) |
| Prior medical conditions and relevant diagnostic procedures, n (%)†‡: | |
| – Cancer screening | 19 (17.3) |
| – Congenital anomalies | 1 (0.9) |
| – Diseases of the blood and blood-forming organs | 3 (2.7) |
| – Diseases of the circulatory system | 7 (6.4) |
| – Diseases of the digestive system | 9 (8.2) |
| – Diseases of the genitourinary: gynecology | 20 (18.2) |
| – Diseases of the genitourinary: urology | 11 (10.0) |
| – Diseases of the musculoskeletal system and connective tissue | 23 (20.9) |
| – Diseases of the nervous system | 10 (9.1) |
| – Diseases of the respiratory system | 16 (14.5) |
| – Diseases of the sense organs | 11 (10.0) |
| – Diseases of the skin and subcutaneous tissue | 8 (7.3) |
| – Endocrine, nutritional and metabolic diseases, and immunity disorders | 20 (18.2) |
| – General symptoms | 13 (11.8) |
| – History of cancer | 2 (1.8) |
| – Infectious and parasitic diseases | 4 (3.6) |
| – Injury and poisoning | 7 (6.4) |
| – Mental disorders | 11 (10.0) |
| – Neoplasms | 4 (3.6) |
| – Nonspecific abnormal findings | 11 (10.0) |
| – Other symptoms involving abdomen and pelvis | 8 (7.3) |
| – Other urinary symptoms | 11 (10.0) |
| – Post-menopausal | 1 (0.9) |
| – Symptoms involving cardiovascular system | 2 (1.8) |
| – Symptoms involving digestive system | 5 (4.5) |
| – Symptoms involving head and neck | 2 (1.8) |
| – Symptoms involving nervous and musculoskeletal systems | 6 (5.5) |
| – Symptoms involving respiratory system and other chest symptoms | 7 (6.4) |
| – Vaccine | 11 (10.0) |
Categories are not mutually exclusive.
Prior conditions are those recorded in the 12 months prior to the well-woman visit but exclusive of the well-woman visit.
Max: Maximum; Min: Minimum; SD: Standard deviation.
Responses to the WHAT questionnaire
Among women completing the questionnaire, the majority of patients were postmenopausal (77.3%). For women who still had their period, most had noticed a change in the last 12 months (60.0%) (Table 2). Overall, the majority of women rated their overall health as at least ‘good’ (88.2%) and roughly, half of the women indicated that they ‘sometimes’ felt overwhelmed by stress.
Table 2.
Women's health assessment tool questionnaire responses.
| Questionnaire items | Questionnaire responses | |||||
|---|---|---|---|---|---|---|
| Excellent | Very good | Good | Fair | Poor | ||
| Overall health (n = 110), n (%) | 13 (11.8) | 45 (40.9) | 39 (35.5) | 10 (9.1) | 3 (2.7) | |
| Never | Rarely | Sometimes | Most of the time | Always | ||
| Overwhelmed/stressed (n = 110), n(%) | 2 (1.8) | 34 (30.9) | 58 (52.7) | 15 (13.6) | 1 (0.9) | |
| Menstruation questions, n (%): | Yes | No | Opt out† | |||
| – Had a period (12 months) (n + 110) | 25 (22.7) | 85 (77.3) | 0 (0.0) | |||
| – Period changed in last 12 months (n = 25)‡ | 15 (60.0) | 10 (40.0) | 0 (0.0) | |||
| – Period 7 days late for two months in a row (n = 15)§ | 8 (53.3) | 7 (46.7) | 0 (0.0) | |||
| – 2 months or more without a period (n = 8)¶ | 6 (75.0) | 2 (25.0) | 0 (0.0) | |||
| Presence and severity in past 3 months (n = 110), n (%)#: | Yes | None | Mild | Moderate | Severe | Very severe |
| – Hot flashes | 68 (61.8) | 42 (38.2) | 40 (36.4) | 20 (18.2) | 7 (6.4) | 1 (0.9) |
| – Depressive mood | 70 (63.6) | 40 (36.4) | 42 (38.2) | 18 (16.4) | 7 (6.4) | 3 (2.7) |
| – Anxiety | 67 (60.9) | 43 (39.1) | 44 (40.0) | 17 (15.5) | 5 (4.5) | 1 (0.9) |
| – Sexual dysfunction†† | 51 (46.4) | 53 (48.2) | 24 (21.8) | 13 (11.8) | 10 (9.1) | 4 (3.6) |
| – Vaginal dryness or discomfort‡‡ | 55 (50.0) | 52 (47.3) | 32 (29.1) | 15 (13.6) | 6 (5.5) | 2 (1.8) |
| – Bladder problems | 61 (55.5) | 49 (44.5) | 37 (33.6) | 20 (18.2) | 3 (2.7) | 1 (0.9) |
| – Breast pain | 25 (22.7) | 85 (77.3) | 20 (18.2) | 4 (3.6) | 1 (0.9) | 0 (0.0) |
Patients selected “I would not like to answer this question now and will discuss with my doctor.”
Only asked menstruating patients.
Only asked patients with change in period.
Only asked patients with late periods.
The number of patients who experienced at least mild symptoms and the symptom severity they were experiencing now or have experienced within the past 3 months.
For sexual dysfunction, n = 6 (5.5%) of patients selected to ‘opt out’ of answering the question.
For vaginal dryness and discomfort, n = 3 (2.7%) of patients selected to ‘opt out’ of answering the question.
All women were then asked information on their experience with seven health conditions including hot flashes, depressive mood, anxiety, sexual problems, dryness or discomfort of the vagina, bladder problems and breast pain. Nearly a third of the women (31.8%) did not experience any of the conditions. The remaining women indicated that they had experienced some level of hot flashes (61.8%), depressive mood (63.6%) or anxiety (60.9%) in the last 3 months. About half indicated that they had experienced some level of sexual problems (46.4%), dryness or discomfort of the vagina (50.0%) or bladder problems (55.5%). The majority of women (77.3%) indicated that they had not experienced breast pain.
Of patients who experienced hot flashes of moderate or greater severity (25.5%), most experienced 6 or less per day (82.2%). Women who reported at least mild depressive mood (63.6%) completed the PHQ–9 with a mean score of 5.9 (SD: 4.9) and scores ranging from 0 (indicating no depression) to 23 (indicating severe depression). Likewise, women who experienced mild anxiety or greater (60.9%) completed the GAD–2, with a mean score of 1.7 (SD: 1.4) and scores ranging from 0 (indicating no anxiety) to 6 (indicating severe anxiety). The majority of women who reported sexual dysfunction with moderate or greater severity (24.5%) reported being ‘somewhat’ (37.0%) or ‘a lot’ (33.3%) bothered by the condition.
At the conclusion of the WHAT questionnaire, women who had experienced at least one condition, were asked to rank their condition(s) according to which they considered to be the most bothersome and to impact their lives the most on a daily basis. Anxiety (22.7%) was considered the most bothersome followed by depression (13.6%), bladder problems (11.8%) and hot flashes (9.1%).
Diagnosis & HRU before & after the WHAT/CDS toolkit implementation
After the implementation of the WHAT/CDS toolkit, a third of the women (n = 37) had at least one current diagnosis of the four conditions assessed (UI, VVA, depression and VMS) during the well-woman visit (Table 3). The most common diagnosis at the well-woman visit among the four conditions was VMS (total VMS cases: n = 16). There were 31 new diagnoses made during the well-woman visit, representing a 72.2% change in the diagnoses rate compared with the visits from 12 months prior (previous 12 month diagnoses: n = 18).
Table 3.
Change in diagnoses and referrals (n = 110).
| Diagnoses and referrals | Previous 12 months (n) | Well-woman visit (n) | Newly identified (n)† |
|---|---|---|---|
| Diagnosis: | |||
| – At least one diagnosis below | 18 | 37 | 31 |
| – UI | 3 | 5 | 4 |
| – Depression | 4 | 10 | 9 |
| – VVA | 7 | 12 | 11 |
| – VMS | 7 | 16 | 15 |
| Referrals:‡ | |||
| – Total referrals | 5 | 9 | 8 |
| – Behavioral health | 0 | 2 | 2 |
| – Consultation | 0 | 1 | 1 |
| – Endocrinology | 0 | 2 | 2 |
| – General surgery | 1 | 1 | 1 |
| – OBGYN | 1 | 0 | 0 |
| – Psychiatric consultation/treatment | 0 | 1 | 1 |
| – Urology | 1 | 1 | 1 |
| – Urogynecology | 2 | 1 | 0 |
Newly identified is defined as count of patients with new conditions or referrals at the well-woman visit that did not occur in the previous 12 months.
This only includes patients who had at least one diagnosis in UI, VVA, depression or VMS at the annual well-woman visit.
OBGYN: Obstetrics and gynecology; UI: Urinary incontinence; VMS: Vasomotor symptoms; VVA: Vulvovaginal atrophy.
For all four conditions being analyzed, there was an increase in the number of new diagnoses made during the well-woman visit compared with the previous 12 months. VMS had the greatest number of new diagnoses during the well-woman visit (n = 15) when compared with the previous 12 months (n = 7). There were similar increases in VVA and depression diagnoses during the well-woman visit (VVA: n = 11; depression: n = 9) compared with the previous 12 months (VVA: n = 7; depression: n = 4) while UI diagnoses had the smallest changes (previous 12 months diagnoses: n = 3, new diagnoses during the well-woman visit: n = 4). There was a slight increase in the number of new referrals made during the well-woman visit (n = 9) compared with the previous 12 months (n = 5) and the most common referrals were for behavioral health (n = 2) or endocrinology (n = 2).
After the implementation of the WHAT/CDS toolkit, the number of laboratory tests ordered during the well-woman visit increased for patients diagnosed with UI (n = 16) and VVA (n = 17) compared with the previous 12 months (UI: n = 10; VVA: n = 5) while decreasing among patients diagnosed with VMS during the well-woman visit (n = 7) compared with the previous 12 months (n = 12) (Table 4). The number of laboratory tests ordered through the CDS toolkit during the well-woman visit ranged from 1 to 5 for individuals diagnosed with UI, depression, VVA and VMS.
Table 4.
Change in laboratory tests by diagnosis (n = 110)†.
| Laboratory tests | Previous 12 months (n) | Well-woman visit (n) | Newly identified (n)‡ |
|---|---|---|---|
| Urinary Incontinence: | 10 | 16 | 11 |
| – POC urine dipstick | 1 | 2 | 2 |
| – POC urinalysis macroscopic | 2 | 3 | 3 |
| – Urinalysis | 1 | 2 | 1 |
| – Urinalysis culture | 3 | 2 | 1 |
| – Urinalysis macroscopic | 0 | 1 | 1 |
| – Urinalysis microscopic | 0 | 1 | 1 |
| – Urine culture | 3 | 5 | 2 |
| Depression: | 15 | 14 | 10 |
| – Basic metabolic panel | 3 | 2 | 0 |
| – CBC with diff | 3 | 4 | 3 |
| – Comprehensive metabolic panel | 4 | 3 | 2 |
| – Estradiol | 0 | 1 | 1 |
| – FSH | 0 | 1 | 1 |
| – Thyroid test | 1 | 0 | 0 |
| – TSH 3rd generation | 3 | 1 | 1 |
| – TSH reflex free T4 | 1 | 2 | 2 |
| Vulvovaginal atrophy: | 5 | 17 | 15 |
| – CA 125 | 0 | 2 | 2 |
| – Cytopathology cervical/vaginal thin layer | 2 | 5 | 4 |
| – Estradiol | 0 | 2 | 2 |
| – FSH | 1 | 2 | 1 |
| – HPV test | 1 | 3 | 3 |
| – POC wet mount | 1 | 0 | 0 |
| – STD test | 0 | 2 | 2 |
| – Vaginal pathogen screen | 0 | 1 | 1 |
| Vasomotor symptoms: | 12 | 7 | 3 |
| – Estradiol | 1 | 2 | 1 |
| – FSH | 2 | 2 | 0 |
| – LH | 1 | 0 | 0 |
| – Progesterone | 1 | 0 | 0 |
| – Thyroid test | 1 | 1 | 1 |
| – TSH third generation | 4 | 2 | 1 |
| – TSH reflex FT4 | 2 | 0 | 0 |
This only includes patients who were diagnosed with UI, depression, VVA or VMS during the well-woman visit.
Newly identified is defined as count of patients (n) with new laboratory tests at the well-woman visit that did not occur in the previous 12 months.
CA: Cancer antigen; CBC: Complete blood count; Diff: Differential; FSH: Follicle-stimulating hormone; FT4: Free thyroxine test; HPV: Human papillomavirus;
LH: Luteinizing hormone; POC: Point of care; STD: Sexually transmitted disease; TSH: Thyroid-stimulating hormone.
The number of procedures or diagnostic tests ordered through the CDS toolkit during the well-woman visit were same from the previous 12 months for patients diagnosed with UI (n = 2) or VMS (n = 13) (Table 5). However, there was a substantial increase in the number of procedures/diagnostic tests ordered among women diagnosed with VVA during the well-woman visit (n = 17) compared with the previous 12 months (n = 5). The procedures or diagnostic tests ordered through the CDS toolkit during the well-woman visit ranged from 1 to 10 among patients diagnosed.
Table 5.
Change in procedures or diagnostic tests by diagnosis (n = 110)†.
| Procedure or diagnostic tests | Previous 12 months (n) | Well-woman visit (n) | Newly identified (n)‡ |
|---|---|---|---|
| Urinary incontinence: | 2 | 2 | 2 |
| – Insertion of non-indwelling bladder catheter | 1 | 1 | 1 |
| – Scope of bladder and urethra | 0 | 1 | 1 |
| – Ultrasound urine capacity measure | 1 | 0 | 0 |
| Vulvovaginal atrophy: | 5 | 17 | 16 |
| – Cath/inject hysterosalpingogram | 0 | 1 | 1 |
| – Dilation of cervical canal | 0 | 1 | 1 |
| – Endometrial biopsy | 0 | 2 | 2 |
| – PAP smear | 2 | 5 | 4 |
| – Path spec routine (non PAP) | 1 | 3 | 3 |
| – Ultrasound hysterosonography | 1 | 1 | 1 |
| – Ultrasound pelvis, non-obstetric | 1 | 3 | 3 |
| – Ultrasound pelvis/transvaginal, non-obstetric | 0 | 1 | 1 |
| Vasomotor symptoms: | 13 | 13 | 7 |
| – Mammogram testing or screening | 12 | 10 | 4 |
| – Ultrasound hysterosonography | 0 | 1 | 1 |
| – Ultrasound pelvis, non-obstetric | 0 | 2 | 2 |
| – Ultrasound pelvis/transvaginal, non-obstetric | 1 | 0 | 0 |
This only includes patients who were diagnosed with urinary incontinence, vulvovaginal atrophy or vulvovaginal atrophy during the well-woman visit.
Newly identified is defined as count of patients (n) with new procedures or diagnostic tests at the well-woman visit that did not occur in the previous 12 months.
Cath/inject: Catheter or injection; PAP: Papanicolaou.
Discussion
The annual well-woman visit can play a vital role in the maintenance of women's health and becomes increasingly more important as women enter middle age given they experience a number of new health issues [19]. Unfortunately, with so many competing priorities of family, work and life, many of these conditions are ignored or overshadowed by other conditions which results in missed diagnoses [4]. The WHAT/CDS toolkit was designed to serve as a resource to healthcare providers to assist in the assessment of high prevalence diagnoses among women in mid-life.
This pilot project aimed to evaluate the health status of mid-life women as well as HRU outcomes associated with the implementation of the WHAT/CDS toolkit. Results from the WHAT questionnaire showed that nearly 70% of women experienced at least mild severity of one of the symptoms assessed through the WHAT questionnaire demonstrating the relevance of the questionnaire and reflecting prevalence rates consistent with other studies of mid-life women [1,4,5,20]. Depressive mood was the most commonly reported symptom captured in the WHAT questionnaire which supports other findings that women were more likely to experience a major depressive episode when they were perimenopausal or early postmenopausal [21]. Likewise, a systematic review of studies implementing assessment tools into primary care found better detection and reporting of mental health issues by patients compared with other primary care concerns [22]. Interestingly, there were only three new behavioral health/psychiatric referrals for this patient cohort. Given the prevalence or reported anxiety and depression, this may or may not be an underutilization of services depending upon the needs of the patients. It should be recognized that the well-woman visit is a primary opportunity for such referrals depending upon patient needs.
While management of chronic diseases such as cancer and diabetes have implemented electronic management tools similar to what is in the WHAT/CDS toolkit, there is limited research on the implementation and impact of condition-specific instruments within women's health [10,11]. The results from the well-woman visit show an increase in the number of diagnoses and laboratory tests ordered across all four assessed conditions during the visit compared with the previous 12 months. However, since this pilot project is cross sectional, it is not known whether the increase in the diagnoses is due to the increased attention to these conditions by the implementation of the WHAT questionnaire or due to the new development of these conditions. Future longitudinal research is needed to address this question.
The noted prevalence of the conditions observed in this pilot project indicates that the use of a patient self-reported questionnaire may provide a mechanism to identify patient conditions that may be missed during clinical visits. This is increasingly important in a time when primary care doctors have a multitude of content to cover and limited guidance in doing so [8]. Additionally, our participation rate shows that the women were willing to complete questionnaires about their health prior to their annual well-woman visit. This may be attributed to the fact that the WHAT questionnaire allowed women to complete the questionnaire in the privacy of their home at a time convenient to them which has been found to improve a patient's willingness to report issues that are embarrassing or sensitive, such as sexual functioning or vaginal dryness [23–25]. The WHAT questionnaire was also intended to minimize patient burden by requiring patients to complete only questions that are relevant based on a preliminary assessment of their symptoms. Evaluations of similar questionnaires in a primary care setting have shown that information feedback to providers from individual-focused questionnaires benefits provider diagnosis and management of patient conditions [22]. These benefits along with focusing patient–provider communication can help increase efficiencies within clinical practice and can be an incentive for providers to participate in the adoption of such integrated tools. Additionally, a review by Boyce and Browne found that these types of instruments are most effective when implemented in an outpatient population, such as primary care [26].
Strengths
The WHAT questionnaire covered symptoms and conditions relevant to mid-life women. The implementation of the WHAT questionnaire through a web-based portal enabled patients to complete the questionnaire prior to their well-woman visit and enabled healthcare providers to access and integrate the patient responses into the visit. Although a control group was not used in this project, having access to the retrospective data allowed for a historical comparison of diagnoses and HRU made before and after the WHAT/CDS implementation.
Limitations
Given that recruitment of patients was conducted within three clinical sites of one healthcare system in the northwest, the results cannot be generalized to other clinical sites and other IDNs. Additionally, generalizability is limited as only 30% of women invited to the project actually participated. This response rate may be due to the following reason. Having patients completing a health questionnaire at home prior to a primary care visit/gynecology visit is a relatively new practice procedure and was new for this IDN. Given that, there may be a lack of awareness of the invite since all invitations had only been sent via email. The use of MyChart and email as a patient communication portal for such health assessment tools needs further exploration and refinement. There was a lack of diversity (90% white) among the participants although there was an even distribution of mid-life ages. The majority of patients were recruited from the Women's health site, not from the two primary care centers, which may have biased the results.
Given the cross-sectional nature of this pilot project and lack of control group, it is impossible to infer any causal relationship between the WHAT/CDS toolkit and the changes in diagnosis and HRUs. Finally, the benefits from the implementation of the WHAT/CDS toolkit suggest improvements in the delivery of care; however, success is heavily reliant on the adaption of the toolkit into routine practice. A successful adaption requires full engagement of hospital staff and resources (e.g., IT infrastructure). Some healthcare systems may lack such capacity to integrate the WHAT/CDS toolkit.
Conclusion
The WHAT questionnaire covers the conditions relevant to mid-life women. An increase across all four assessed conditions in the number of diagnoses made during the well-woman visit after the implementation of the WHAT/CDS toolkit was observed. The use of the WHAT may provide a way to identify conditions that may be missed during clinical visits among the middle-aged women. This was a pilot project to evaluate the WHAT/CDS toolkit therefore, additional research should be conducted at more clinical sites over a long-term period with an inclusion of control group to better assess how the implementation of the WHAT/CDS toolkit can impact patient outcomes.
Author contributions
All authors reviewed and approved of the final manuscript.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
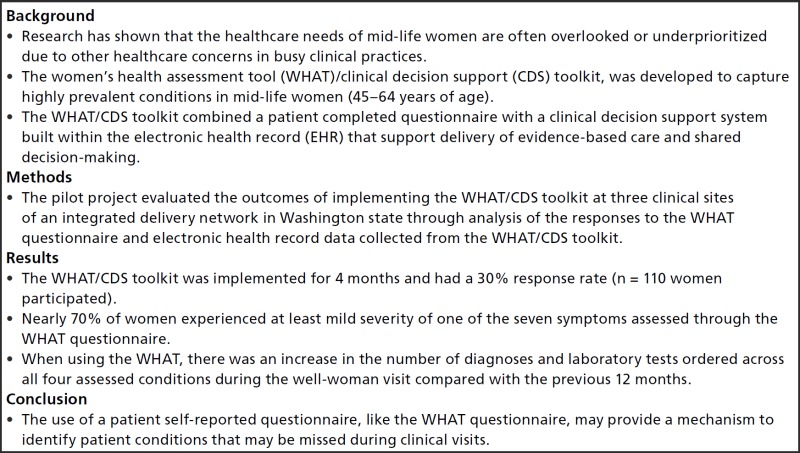
Executive summary
- Background
- Research has shown that the healthcare needs of mid-life women are often overlooked or underprioritized due to other healthcare concerns in busy clinical practices.
- The women's health assessment tool (WHAT)/clinical decision support (CDS) toolkit, was developed to capture highly prevalent conditions in mid-life women (45–64 years of age).
- The WHAT/CDS toolkit combined a patient completed questionnaire with a clinical decision support system built within the electronic health record (EHR) that support delivery of evidence-based care and shared decision-making.
- Methods
- The pilot project evaluated the outcomes of implementing the WHAT/CDS toolkit at three clinical sites of an integrated delivery network in Washington state through analysis of the responses to the WHAT questionnaire and electronic health record data collected from the WHAT/CDS toolkit.
- Results
- The WHAT/CDS toolkit was implemented for 4 months and had a 30% response rate (n = 110 women participated).
- Nearly 70% of women experienced at least mild severity of one of the seven symptoms assessed through the WHAT questionnaire.
- When using the WHAT, there was an increase in the number of diagnoses and laboratory tests ordered across all four assessed conditions during the well-woman visit compared with the previous 12 months.
- Conclusion
- The use of a patient self-reported questionnaire, like the WHAT questionnaire, may provide a mechanism to identify patient conditions that may be missed during clinical visits.
Financial & competing interests disclosure
This project was funded by Pfizer, Inc. K Coyne and A Steenrod are employees of Evidera who were paid consultants by Pfizer in connection with this project and development of this manuscript. D Gross, C Esinduy, A Kodsi, L Abraham, A Bushmakin and, X Luo are employees of Pfizer. G Slifka was an employee of Pfizer at the time the project was conducted. A Araiza is a former employee of Atrium Staffing, who were paid contractors to Pfizer for the development of this manuscript and project management. T Silvestrin is affiliated with MultiCare Tacoma Women's Specialists in Tacoma, WA, USA. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Formatting support for this manuscript was provided by Kawthar Nakayima, from Evidera and was funded by Pfizer.
References
- 1.Bromberger JT, Kravitz HM. Mood and menopause: findings from the study of Women's Health Across the Nation (SWAN) over 10 years. Obstet. Gynecol. Clin. North Am. 38(3), 609–625 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dooley Y, Kenton K, Cao G, et al. Urinary incontinence prevalence: results from the National Health and Nutrition Examination Survey. J. Urol. 179(2), 656–661 (2008). [DOI] [PubMed] [Google Scholar]
- 3.Gold EB, Colvin A, Avis N, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women's health across the nation. Am. J. Public Health 96(7), 1226–1235 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parish SJ, Nappi RE, Krychman ML, et al. Impact of vulvovaginal health on postmenopausal women: a review of surveys on symptoms of vulvovaginal atrophy. Int. J. Womens Health 5, 437–447 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thurston RC, Bromberger JT, Joffe H, et al. Beyond frequency: who is most bothered by vasomotor symptoms? Menopause 15(5), 841–847 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris SS, Link CL, Tennstedt SL, Kusek JW, Mckinlay JB. Care seeking and treatment for urinary incontinence in a diverse population. J. Urol. 177(2), 680–684 (2007). [DOI] [PubMed] [Google Scholar]
- 7.Williams RE, Kalilani L, Dibenedetti DB, Zhou X, Fehnel SE, Clark RV. Healthcare seeking and treatment for menopausal symptoms in the United States. Maturitas 58(4), 348–358 (2007). [DOI] [PubMed] [Google Scholar]
- 8.Fitzgerald T, Glynn A, Davenport K, Waxman J, Johnson PA. Well-woman visits: guidance and monitoring are key in this turning point for women's health. Womens Health Issues 25(2), 89–90 (2015). [DOI] [PubMed] [Google Scholar]
- 9.Delbanco T, Walker J, Bell SK, et al. Inviting patients to read their doctors' notes: a quasi-experimental study and a look ahead. Ann. Intern. Med. 157(7), 461–470 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldberg HI, Ralston JD, Hirsch IB, Hoath JI, Ahmed KI. Using an Internet comanagement module to improve the quality of chronic disease care. Jt. Comm. J. Qual. Saf. 29(9), 443–451 (2003). [DOI] [PubMed] [Google Scholar]
- 11.Tamblyn R, Ernst P, Winslade N, et al. Evaluating the impact of an integrated computer-based decision support with person-centered analytics for the management of asthma in primary care: a randomized controlled trial. J. Am. Med. Inform. Assoc. 22(4), 773–783 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.US Census Bureau. 2012 National Population Projections: Summary Tables (2012). www.census.gov/population/projections/data
- 13.US Census Bureau. 2005 Population Estimates: National Tables (2005). www.census.gov/popest
- 14.Brown JS, Bradley CS, Subak LL, et al. The sensitivity and specificity of a simple test to distinguish between urge and stress urinary incontinence. Ann. Intern. Med. 144(10), 715–723 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donker T, Van Straten A, Marks I, Cuijpers P. Quick and easy self-rating of generalized anxiety disorder: validity of the Dutch web-based GAD-7, GAD-2 and GAD-SI. Psychiatry Res. 188(1), 58–64 (2011). [DOI] [PubMed] [Google Scholar]
- 16.Isidori AM, Pozza C, Esposito K, et al. Development and validation of a 6-item version of the female sexual function index (FSFI) as a diagnostic tool for female sexual dysfunction. J. Sex. Med. 7(3), 1139–1146 (2010). [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The PHQ–9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16(9), 606–613 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.SAS Institute Inc. SAS® 9.4 Software (2013). Cary, NC, USA [Google Scholar]
- 19.Harvard Health Publications. Why regular check-ups are still a good idea. An annual “well woman” visit has important health benefits – especially the doctor-patient relationship it fosters. Harv. Womens Health Watch 14(9), 1–3 (2007). [PubMed] [Google Scholar]
- 20.Thom D. Variation in estimates of urinary incontinence prevalence in the community: effects of differences in definition, population characteristics, and study type. J. Am. Geriatr. Soc. 46(4), 473–480 (1998). [DOI] [PubMed] [Google Scholar]
- 21.Bromberger JT, Kravitz HM, Chang YF, Cyranowski JM, Brown C, Matthews KA. Major depression during and after the menopausal transition: Study of Women's Health Across the Nation (SWAN). Psychol. Med. 41(9), 1879–1888 (2011b). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haywood K, Marshall S, Fitzpatrick R. Patient participation in the consultation process: a structured review of intervention strategies. Patient Educ. Couns. 63(1–2), 12–23 (2006). [DOI] [PubMed] [Google Scholar]
- 23.Kurth AE, Martin DP, Golden MR, et al. A comparison between audio computer-assisted self-interviews and clinician interviews for obtaining the sexual history. Sex. Transm. Dis. 31(12), 719–726 (2004). [DOI] [PubMed] [Google Scholar]
- 24.Slack WV, Kowaloff HB, Davis RB, et al. Evaluation of computer-based medical histories taken by patients at home. J. Am. Med. Inform. Assoc. 19(4), 545–548 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science 280(5365), 867–873 (1998). [DOI] [PubMed] [Google Scholar]
- 26.Boyce MB, Browne JP. Does providing feedback on patient-reported outcomes to healthcare professionals result in better outcomes for patients? A systematic review. Qual. Life Res. 22(9), 2265–2278 (2013). [DOI] [PubMed] [Google Scholar]