Abstract
Total elbow arthroplasty can be a rewarding operation and is becoming increasingly used in the elderly fracture population. Multiple approaches are represented in the literature and deciding on the best approach is difficult. This review discusses approaches and their reported outcomes, aiming to allow surgeons to make an informed choice about which approach to use.
Keywords: approaches, outcomes, total elbow arthroplasty
Introduction
Total elbow arthroplasty (TEA) can be a rewarding operation in the right cohort of patients,1 including painful arthritis and post trauma sequalae, and is being increasingly used for the elderly acute distal humerus fracture population.2 Multiple approaches are represented in the literature and deciding on the best approach is difficult. The triceps-on approach, where the triceps mechanism is preserved on the ulna insertion, has been gaining popularity recently. It is perceived to be more technically demanding than the triceps off approaches where the triceps mechanism is elevated off the ulna or partly cut. A good approach for TEA should allow adequate exposure to properly position the implants, have a low risk of nerve damage, achieve a good range of movement and preserve triceps function.
The aim of this review is to present the current available literature in an attempt to answer whether the triceps-on approach can best fulfil these requirements.
Materials and Methods
An electronic search of Medline using the Pubmed search engine and the EMBASE bibliographical database for papers describing approaches for TEA in English published prior to 30 September 2015. The terms used were elbow arthroplasty, elbow replacement and approach. This gave a total of 197 papers. Thirty-one of these were published in a non-English language journal. A further 108 were not relevant, leaving 56 papers of interest. All abstracts were reviewed and relevant full articles were obtained. The references from these full articles were also reviewed for additional relevant publications.
Results
The majority of approaches to the elbow utilized a posterior midline skin incision with full thickness flaps and early identification of the ulnar nerve. Management of the ulnar nerve varies considerably. It is agreed that the nerve needs to be identified early and superficially decompressed.3 The nerve is at risk when being handled, and whether to transponse the nerve or not appears to be down to surgeon preference. Transposition is advocated in pre-existing nerve deficits or where the prosthesis affects the nerves usual course.4 However, the risk of injuring the nerve’s blood supply has led some authors to advocate leaving the nerve in its bed with its deep soft tissues, in an aim to reduce postoperative neuritis.5 The trans-olecranon osteotomy is rarely used as a result of the compromise of the ulna for component insertion and fixation.6 The approaches can be broadly categorized into triceps-on and triceps-off. Triceps-on approaches all maintain the triceps mechanism and its insertion on the ulna. Triceps off approaches involve some or all of the triceps being taken off its ulna insertion or cutting of the triceps mechanism at some point. The triceps-off group can be subdivided into triceps turndown, triceps elevating or triceps splitting. A triceps turndown involves cutting of the triceps tendon above the ulna insertion. A triceps elevating approach elevates the triceps off the ulna subperiosteally. A triceps splitting approach divides the triceps tendon longitudinally along its length and through its insertion.
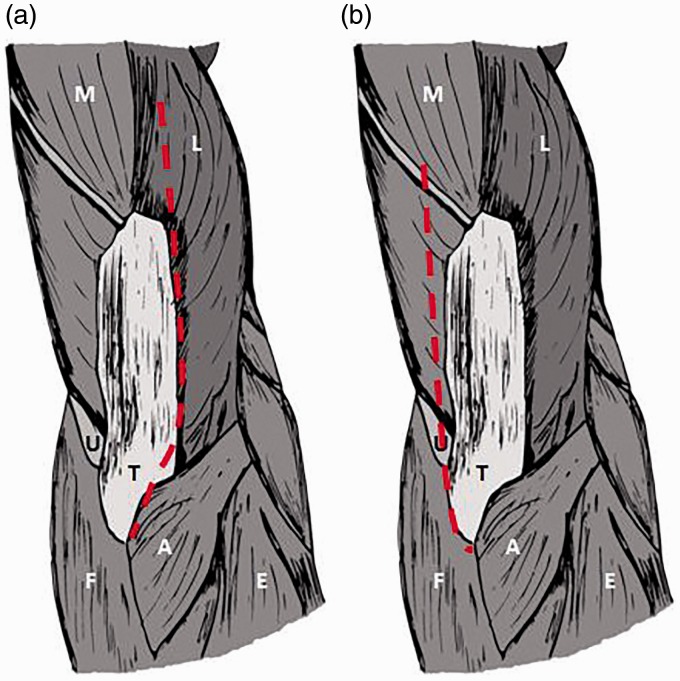
Triceps turndown approaches (Fig. 1)
Figure 1.
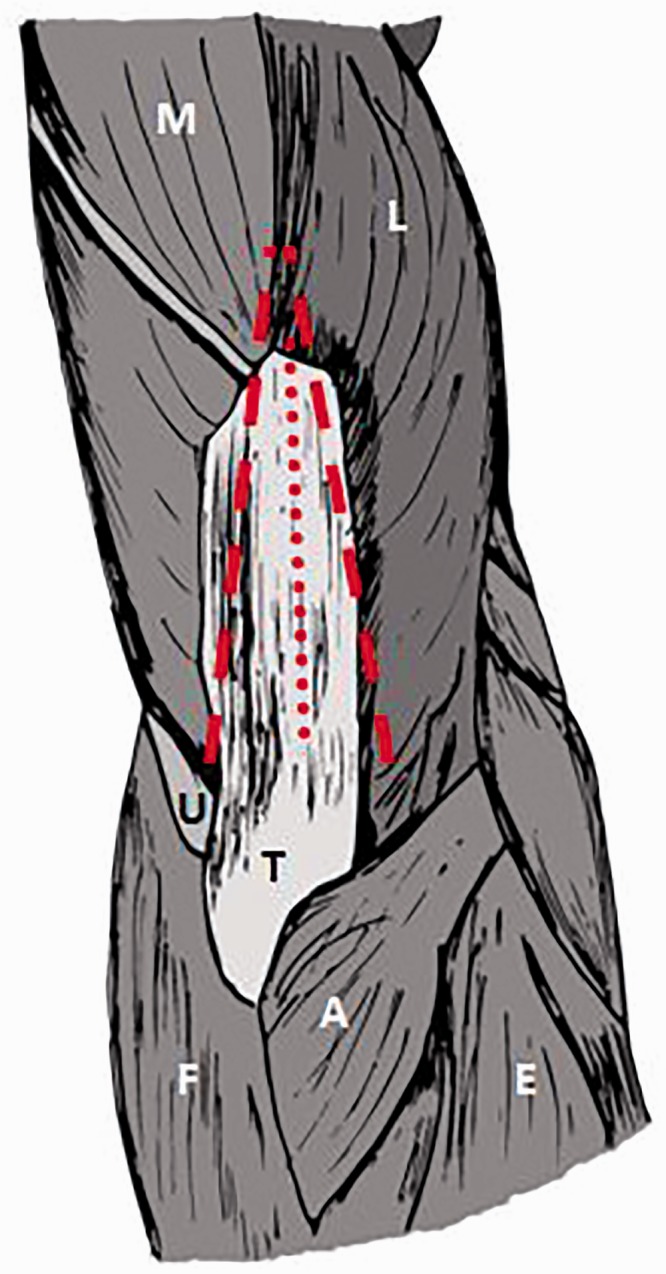
Triceps turndown techniques6. A, anconeus; E, extensors; F, flexors; L, lateral head of triceps; M, medial head of triceps; T, triceps tendon; U, ulnar nerve.
The original triceps turndown was described for interposition arthroplasty in ankylosed joints.7 The triceps aponeurosis is reflected downwards in a V-shaped tongue with the base on the olecranon. The underlying muscle is split in the midline and elevated off the humerus. Variations of the technique have been described with the underlying muscle being split,8,9 with an associated medial epicondyle and supinator tuberosity osteotomy10 or with a split and turn down of the deep intramuscular aponeurosis.11
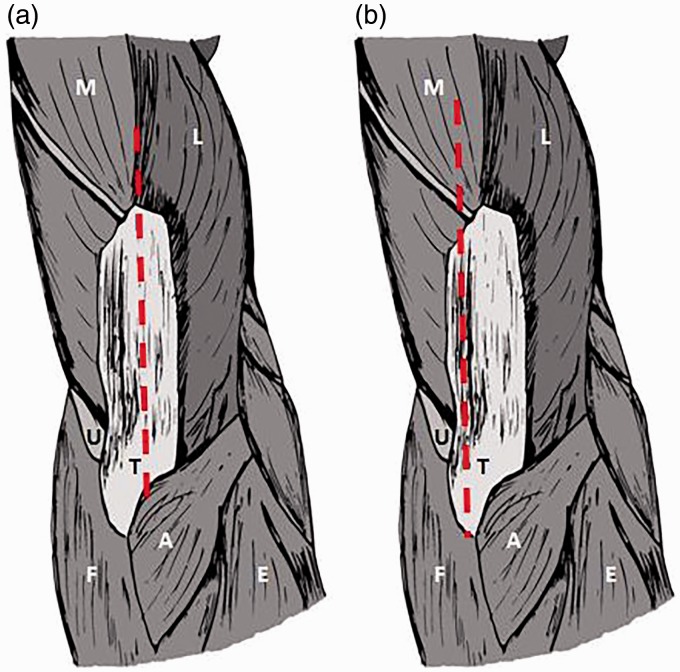
Triceps elevating approaches (Fig. 2)
Figure 2.
Triceps reflecting approaches: a11 and b5. A, anconeus; E, extensors; F, flexors; L, lateral head of triceps; M, medial head of triceps; T, triceps tendon; U, ulnar nerve.
Complete reflection of the triceps from lateral to medial12 or from medial to lateral6 has been described. Both of these approaches require careful subperiosteal elevation of the triceps insertion from the olecranon to avoid compromise of the extensor mechanism.
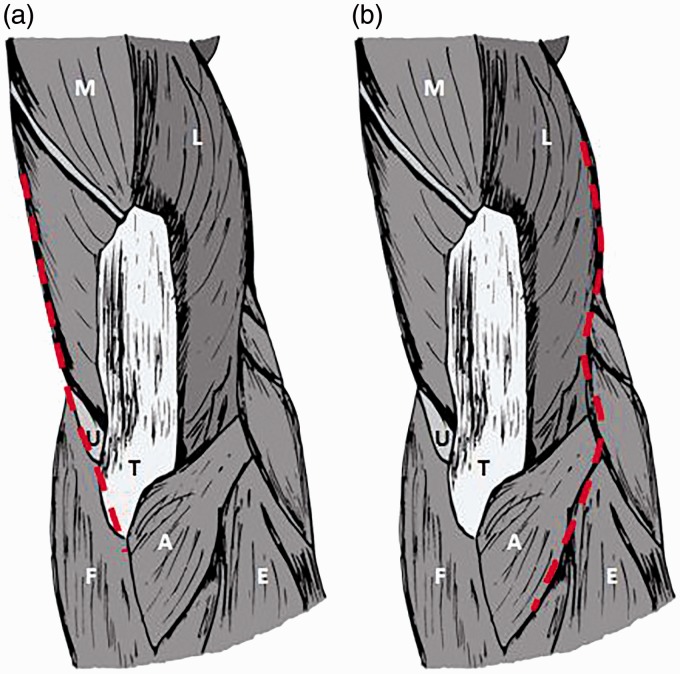
Triceps splitting approach (Fig. 3)
Figure 3.
Triceps splitting approaches: a12 and b13. A, anconeus; E, extensors; F, flexors; L, lateral head of triceps; M, medial head of triceps; T, triceps tendon; U, ulnar nerve.
Many of the triceps splitting techniques are modifications of the midline triceps split with elevation of each half of the triceps off the posterior humerus and ulna.13 The Shahane–Stanley posterior approach combines a split and reflection of the triceps.5 The triceps is split, with 75% laterally and 25% medially. The medial triceps is reflected medially with dissection beneath the ulnar nerve but maintained on the olecranon. The lateral triceps is reflected sub-periostally off the olecranon with the anconeus. Repair of the triceps is through transosseous sutures through the olecranon.
The triceps split and snip is a midline triceps split with subperiosteal mobilization of the lateral triceps. The medial portion is mobilized off the posterior humerus and if required a snip of the triceps tendon is made of the medial triceps portion 1 cm to 2 cm proximal to the ulna. At closure a side to side repair, as well as an end to end repair is required.14
The anconeus triceps lateral flap approach15 utilizes the Kocher interval on the lateral side between the anconeus and extensor carpi ulnaris, and a plane between the lateral triceps expansion and the true tendinous part of the triceps (triceps decussation). This triangular flap is then elevated proximally off the ulna to allow exposure to the joint. The medial tendinous part of the triceps remains on the ulna with proximal elevation off the back of the humerus.
Triceps on approach (single) (Fig. 4)
Figure 4.
Single triceps preserving approaches: a16 and b18. A, anconeus; E, extensors; F, flexors; L, lateral head of triceps; M, medial head of triceps; T, triceps tendon; U, ulnar nerve.
The triceps on approach is also called the triceps preserving or triceps retaining approaches. All maintain the triceps and triceps insertion in continuity with the olecranon. These can be further divided into single and dual approaches.
A single medial triceps on approach involves releasing the ulnar nerve and retracting it anteriorly. The capsule and medial collateral ligament are excised along the ulna border of the humerus. Distally, the flexor carpi ulnaris is elevated off the ulna and proximally the triceps is elevated off the back of the humerus. This leaves the triceps intact and dislocation of the elbow can be achieved with pronation.16,17
A lateral extended Kocher approach is based on a lateral incision with elevation of the triceps off the lateral ridge and distally the plane is between the anconeus and extensor carpi ulnaris.18
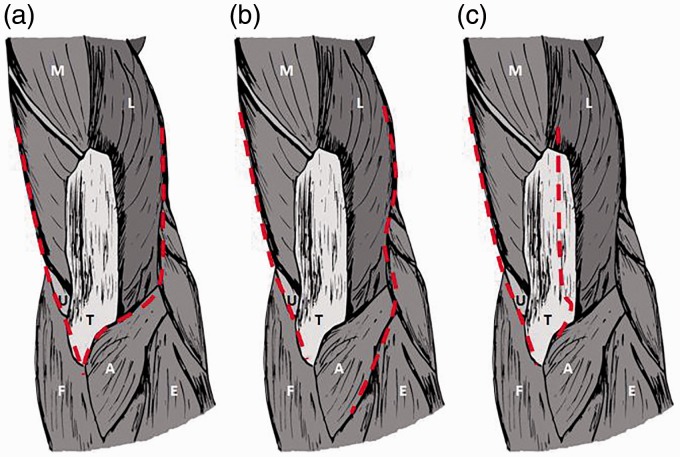
Triceps on approach (dual) (Fig. 5)
Figure 5.
Dual triceps preserving approaches: a19, b21 and C22. A, anconeus; E, extensors; F, flexors; L, lateral head of triceps; M, medial head of triceps; T, triceps tendon; U, ulnar nerve.
The Alonso-Llames approach19 was first described for supracondylar fractures in children but has subsequently been modified for total elbow arthroplasty. The triceps is elevated from each side off the intermuscular septum and posterior humerus. Distally, the approach is enlarged with two para-olecranon incisions. The ulnar nerve can be mobilized with a cuff of triceps fascia and capsule to allow closure at the end of the procedure and bring the nerve back into a stable position.20
One modification is to maintain the anconeus on the olecranon as well, with the dissection distally between the extensor carpi ulnaris and anconeus.21 The elbow can then be dislocated laterally and the ulna is maximally exposed for instrumentation by hyper-pronating the forearm. The lateral para-olecranon approach reflects the triceps off the posterior humerus on the medial side and splits the lateral edge of the triceps in line with the lateral edge of the ulna, so that the lateral triceps and the anconeus are elevated off laterally together.22
Exposure
Any approach for TEA should give a good exposure to the humerus and ulna to allow the optimal placement of the implants. The radial head may also require exposure if resection or replacement is going to be part of the arthroplasty and, importantly, the surgeon must be able to achieve clearance of any anterior structures that may impinge in deep flexion and cause potential loosening of the ulna component.23
The humeral exposure obtained by a triceps splitting approach,24 a triceps elevating approach6 and an olecranon osteotomy25 have been compared in cadavers26. This demonstrated that 35% of the articular surface could be visualized in the triceps split, 46% in the triceps elevating and 57% in the olecranon osteotomy. A similar study comparing a triceps turndown,9 a triceps splitting approach,24 a triceps elevating approach6 and an olecranon osteotomy25 allowed visualization of 75%, 35%, 37% and 51%, respectively (Table 1).9 A final study on this topic27 found that, when comparing three posterior approaches, the mean percentage of articular exposure for a dual triceps on approach,19 triceps splitting24 and olecranon osteotomy25 approach was 26%, 37% and 52%, respectively. There are no studies looking at the exposure of the ulna articular surface with different approaches.
Table 1.
| Approach | Mean articular surface exposed, % (n) |
|---|---|
| Triceps split | 36 (20) |
| Triceps elevating | 40.6 (10) |
| Olecranon osteotomy | 52.7 (20) |
| Triceps turndown | 75 (6) |
| Dual triceps on | 26 (10) |
The ultimate aim of TEA exposure is to allow correct implant positioning, and studies have shown that this has an impact on outcomes. Malrotation of the humeral component or mal-alignment in varus/valgus can load both unlinked and linked TEAs abnormally,28–30 and significantly affect the muscle movement arms of the muscles across the elbow, changing the kinematics of the implant.31
Mal-aligned components can be a predictor of loosening and the need for revision.32 There is also some evidence that implant positioning can also affect pain, extension strength and functional outcomes.33
No studies have compared approaches and implant alignment achieved. The triceps on approaches are perceived to make ulna component positioning more difficult and techniques to aid correct alignment have been suggested.34 One study16 has reported on the alignment after a triceps on approach and using specific jigs referencing the posterior humerus and ulna aspect of the ulna in 25 elbows. Although the humeral components were within 3° of the targeted alignment, the ulna components had 9.3° of pronation and 8.6° of flexion compared to the angle targeted.
Range of movement
One retrospective study20 compares range of movement as an outcome following triceps on versus triceps-off group, which included triceps elevating, triceps splitting or triceps turndown. With a total of 82 patients, the triceps on group had a significantly better range of movement than triceps off. For rheumatoid arthritis, another study22 showed that a triceps splitting approach has a significantly greater flexion contracture, although the flexion range remained similar, in comparison to two triceps on approaches,19,22 whereas the flexion range remained similar.
Triceps function
Patients who have triceps insufficiency struggle to reach over their head, lift themselves from a chair using their arms for support and push open doors because adequate extension of the elbow is dependent on the triceps.35 The largest single centre cohort study of over 800 elbows with mixed triceps splitting and elevating approaches has reported a 2% triceps failure rate.36 A systematic review of 47 papers assessing triceps dehiscence or clinically significant weakness showed no significant difference in incidence between triceps split, triceps elevation or triceps turndown,4 with a reported rate of between 1.2% and 1.8%. The rate of insufficiency or failure is low, although this complication often requires complex and multiple operations with variable outcomes.35 It often presents late and may require an augmented repair with anconeus or an achilles tendon allograft.37
An overall triceps failure rate of 3% following TEA has been reported, with this complication reported in 47 out of 1676 elbows from 35 studies.38 When split by approach, there was an incidence of 11% when the triceps was taken off the ulna, 3% for a triceps elevating approach and 0.6% for a triceps turndown approach. The overall rate of triceps failure in our review following a triceps on approach for TEA was 0% in 532 elbows.6,11,16,17,20–22,39,40
Another retrospective study of 82 patients,20 comparing triceps on versus triceps off (which included triceps elevating, triceps splitting or triceps turndown) approaches, had no triceps ruptures in the triceps on group, but a 15% triceps rupture rate in the triceps off group.
The ultimate tensile strength of the triceps after a triceps split and snip approach or a triceps elevating approach in cadaveric specimens was 40% compared to the preserved control specimens and showed no difference between the approaches.6,14 A similar study41 in cadavers between a control and either a Campbells V-Y splitting approach (triceps turndown),7 a triceps elevating approach6 and a triceps splitting approach42 had an ultimate tensile strength well below 50% for all approaches compared to the preserved control group, with no significant differences between approaches. Unfortunately, no study included a triceps-on technique.
The results of a single triceps-on approach16 using specific jigs to aid alignment have been reported in 25 elbows with no triceps insufficiency or rupture. The manual muscle testing score43 was 5/5 in 23 elbows and 2/5 in one patient with bilateral replacements with pre-existing weakness.
In a clinical study, Morrey et al.44 compared triceps strength following exposures with the triceps elevating6 against a triceps splitting45 or modified Kocher approach. Pre- to postoperative triceps strength increased by 26% in the triceps on approach, and 6% with the other surgical exposures, and this strength increase was felt to be secondary to relief of pain. It was also noted that strength was influenced by component position, with an anatomic or distally placed centre of rotation improving extensor function, but did not further subdivide this finding by approach.
For rheumatoid arthritis, a triceps splitting approach has a significantly lower extension torque and strength compared to triceps on approaches,22 although this difference was not seen in fracture patients. Another study of semi-constrained elbow replacements compared 13 elbows performed by a triceps elevating approach with 10 performed by a triceps-on approach.40 Triceps function was graded as good in 90% of patients with a triceps-on approach, although only in 34% of those with a triceps elevating approach.
Nerve injury
The ulnar nerve is the most susceptible nerve during posterior approaches for elbow arthroplasty, and a significant ulnar nerve lesion was found in 2% to 3.2% of patients in a systematic review of almost 3000 TEAs with all types of approaches.4 No statistically significant difference was seen when comparing nerve injury rates in series with routine ulnar nerve transposition against those that did not routinely transpose the nerve. Transient ulnar nerve symptoms of less than 6 weeks have been reported in up to 21% of patients.46
The overall rate of ulnar nerve lesions following a triceps on approach was between 0% and 26%11,16,21,40,47 with a mean value of 3.5% (16 out of 451 elbows).
The only study to directly compare complications between approaches20 found that they had one palsy out of 37 cases (2.7%) in the triceps on group, and one palsy out of 46 cases (2.2%) in the triceps off group. No other comparative study discusses ulnar nerve lesions as an outcome.
Anconeus
A consideration in the variety of approaches available is the different management of anconeus. The radial nerve supplies this muscle, as well as the triceps, and a number of the approaches will divide this nerve supply.8–13,19,20 The anconeus is supplied by the continuation of the branch of the radial nerve that supplies the medial head of triceps,48,49 which branches off the radial nerve proper on the medial side of the posterior humerus approximately 16.8 cm above the medial epicondyle. The nerve then travels laterally, and then distally, overlying the medial head of the triceps to pierce anconeus lateral to the olecranon. However, using the nerve to the triceps medial head and anconeus as a nerve graft has been shown to have no significant impact on elbow extension strength,49 suggesting minimal functional loss even if the anconeus is denervated. To the best of our knowledge, there are no papers that address this issue with regard to TEA.
Discussion
The major difficulty in interpreting the literature is the small numbers involved in many studies, the heterogeneity of approaches, experience of surgeons, implants, underlying pathology and quality of outcome data. Even within each subgroup of approaches, there are considerable variations that could impact on the exposure achieved, potential complications and functional outcome.
The conclusions that can be drawn from the present study are that the triceps on approaches do not allow as much exposure of the humeral articular surfaces as other approaches. Ulna exposure has not been quantified, although the positioning of the ulna implant may be inclined to be placed into flexion with a triceps on approach because the surgeon is having to work around the triceps insertion onto the olecranon.16
The range of movement and strength achieved following a triceps on approach would appear to be better than other approaches. Furthermore, no triceps failures have been reported in triceps on approaches. Complications to the ulnar nerve appear to be similar in all approaches, although these figures should be treated with caution, given the heterogenous nature of patients, pathologies and surgeon experience presented.
In summary, the triceps on approach has significant functional advantages over other approaches but gives a reduced exposure that may alter the positioning of implants. This information should help guide surgeons make an informed decision about the approach to choose, as well as the potential limitations of each approach.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical review and patient consent
References
- 1.Gill DR, Morrey BF. The Coonrad–Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. A ten to fifteen-year follow-up study. J Bone Joint Surg Am 1998; 80: 1327–1335. [DOI] [PubMed] [Google Scholar]
- 2.Cobb TK, Morrey BF. Total elbow arthroplasty as primary treatment for distal humeral fractures in elderly patients. J Bone Joint Surg 1997; 79: 826–832. [DOI] [PubMed] [Google Scholar]
- 3.Morrey BF, Sanchez-Sotelo J. Approaches for elbow arthroplasty: how to handle the triceps. J Shoulder Elbow Surg 2011; 20: S90–S96. [DOI] [PubMed] [Google Scholar]
- 4.Voloshin I, Schippert DW, Kakar S, Kaye EK, Morrey BF. Complications of total elbow replacement: a systematic review. J Shoulder Elbow Surg Am 2011; 20: 158–168. [DOI] [PubMed] [Google Scholar]
- 5.Shahane SA, Stanley D. A posterior approach to the elbow joint. J Bone Joint Surg Br 1999; 81: 1020–1022. [DOI] [PubMed] [Google Scholar]
- 6.Bryan RS, Morrey BF. Extensive posterior exposure of the elbow. A triceps-sparing approach. Clin Orthop 1982; 166: 188–192. [PubMed] [Google Scholar]
- 7.Campbell WC. Arthroplasty of the elbow. Ann Surg 1922; 76: 615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marinello PG, Peers S, Styron J, Pervaiz K, Evans PJ. Triceps fascial tongue exposure for total elbow arthroplasty: surgical technique and case series. Tech Hand Up Extrem Surg 2015; 19: 60–63. [DOI] [PubMed] [Google Scholar]
- 9.Amirfeyz R, Clark D, Quick T, Blewitt N. Newcastle approach to the elbow, a cadaveric study. Arch Orthop Trauma Surg 2011; 131: 747–751. [DOI] [PubMed] [Google Scholar]
- 10.de Vos MJ, Wagener ML, Verdonschot N, Eygendaal D. An extensive posterior approach of the elbow with osteotomy of the medial epicondyle. J Shoulder Elb Surg Am 2014; 23: 313–317. [DOI] [PubMed] [Google Scholar]
- 11.Rajeev A, Pooley J. A posterior approach to the elbow joint based on the blood supply to the triceps muscle. Eur J Orthop Surg Traumatol 2009; 19: 467–472. [Google Scholar]
- 12.Tsuge K, Murakami T, Yasunaga Y, Kanaujia RR. Arthroplasty of the elbow. Twenty years’ experience of a new approach. J Bone Joint Surg Br 1987; 69: 116–120. [DOI] [PubMed] [Google Scholar]
- 13.Campbell W. Campbells operative orthopaedics 1971; Volume 1 5th edition St Louis, MO: Mosby. [Google Scholar]
- 14.Poon PC, Foliaki S, Young SW, Eisenhauer D. Triceps split and snip approach to the elbow: surgical technique and biomechanical evaluation. ANZ J Surg 2013; 83: 774–778. [DOI] [PubMed] [Google Scholar]
- 15.Celli A. The anconeus-triceps lateral flap approach: new surgical exposure for total elbow arthroplasty. Tech Shoulder Elb Surg 2015; 16: 19–28. [Google Scholar]
- 16.Oizumi N, Suenaga N, Yoshioka C, Yamane S. Triceps-sparing ulnar approach for total elbow arthroplasty. Bone Joint J 2015; 97B: 1096–1101. [DOI] [PubMed] [Google Scholar]
- 17.Prokopis PM, Weiland AJ. The triceps-preserving approach for semiconstrained total elbow arthroplasty. J Shoulder Elb Surg Am 2008; 17: 454–458. [DOI] [PubMed] [Google Scholar]
- 18.Rydholm U, Ljung P. Surface replacement of the rheumatoid elbow through a lateral approach. Tech Orthop 2003; 18: 258–266. [Google Scholar]
- 19.Alonso-Llames M. Bilaterotricipital approach to the elbow. Its application in the osteosynthesis of supracondylar fractures of the humerus in children. Acta Orthop Scand 1972; 43: 479–490. [DOI] [PubMed] [Google Scholar]
- 20.Dachs RP, Fleming MA, Chivers DA, et al. Total elbow arthroplasty: outcomes after triceps-detaching and triceps-sparing approaches. J Shoulder Elb Surg Am 2015; 24: 339–347. [DOI] [PubMed] [Google Scholar]
- 21.Boorman RS, Page WT, Weldon EJ, Lippitt S, Matsen FA. A triceps-on approach to semi-constrained total elbow arthroplasty. Tech Shoulder Elb Surg 2003; 4: 139–144. [Google Scholar]
- 22.Studer A, Athwal GS, MacDermid JC, Faber KJ, King GJW. The lateral para-olecranon approach for total elbow arthroplasty. J Hand Surg 2013; 38: 2219–2226.e3–2219–2226.e3. [DOI] [PubMed] [Google Scholar]
- 23.Cheung EV, O’Driscoll SW. Total elbow prosthesis loosening caused by ulnar component pistoning. J Bone Joint Surg Am 2007; 89: 1269–1274. [DOI] [PubMed] [Google Scholar]
- 24.Gorder GWV. Surgical approach in supracondylar ‘T’ fractures of the humerus requiring open reduction. J Bone Joint Surg 1940; 22: 278–292. [Google Scholar]
- 25.MacAusland WR. Ankylosis of the elbow: With report of four cases treated by arthroplasty. J Am Med Assoc 1915, pp. LXIV:312–LXIV:312. [Google Scholar]
- 26.Wilkinson JM, Stanley D. Posterior surgical approaches to the elbow: a comparative anatomic study. J Shoulder Elb Surg Am 2001; 10: 380–382. [DOI] [PubMed] [Google Scholar]
- 27.Dakouré PWH, Ndiaye A, Ndoye J-M, et al. Posterior surgical approaches to the elbow: a simple method of comparison of the articular exposure. Surg Radiol Anat SRA 2007; 29: 671–674. [DOI] [PubMed] [Google Scholar]
- 28.Schuind F, O’Driscoll S, Korinek S, An KN, Morrey BF. Loose-hinge total elbow arthroplasty. An experimental study of the effects of implant alignment on three-dimensional elbow kinematics. J Arthroplasty 1995; 10: 670–678. [DOI] [PubMed] [Google Scholar]
- 29.Itoi E, King GJ, Neibur GL, Morrey BF, An KN. Malrotation of the humeral component of the capitellocondylar total elbow replacement is not the sole cause of dislocation. J Orthop Res Off Publ Orthop Res Soc 1994; 12: 665–671. [DOI] [PubMed] [Google Scholar]
- 30.Brownhill JR, Pollock JW, Ferreira LM, Johnson JA, King GJW. The effect of implant malalignment on joint loading in total elbow arthroplasty: an in vitro study. J Shoulder Elb Surg Am 2012; 21: 1032–1038. [DOI] [PubMed] [Google Scholar]
- 31.Schuind F, O’Driscoll SW, Korinek S, An KN, Morrey BF. Changes of elbow muscle moment arms after total elbow arthroplasty. J Shoulder Elb Surg Am 1994; 3: 191–199. [DOI] [PubMed] [Google Scholar]
- 32.Brinkman J-M, de Vos MJ, Eygendaal D. Failure mechanisms in uncemented Kudo type 5 elbow prosthesis in patients with rheumatoid arthritis: 7 of 49 ulnar components revised because of loosening after 2–10 years. Acta Orthop 2007; 78: 263–270. [DOI] [PubMed] [Google Scholar]
- 33.Lenoir H, Micallef JP, Djerbi I, et al. Total elbow arthroplasty: Influence of implant positioning on functional outcomes. Orthop Traumatol Surg Res 2015; 101: 721–727. [DOI] [PubMed] [Google Scholar]
- 34.Morrey ME, Morrey BF. Finding the canal: a novel technique for identifying and instrumenting ulnar canals during total elbow arthroplasty. Tech Shoulder Elb Surg 2015; 16: 15–18. [Google Scholar]
- 35.Celli A, Arash A, Adams RA, Morrey BF. Triceps insufficiency following total elbow arthroplasty. J Bone Joint Surg Am 2005; 87: 1957–1964. [DOI] [PubMed] [Google Scholar]
- 36.Kim JM, Mudgal CS, Konopka JF, Jupiter JB. Complications of total elbow arthroplasty. J Am Acad Orthop Surg 2011; 19: 328–339. [DOI] [PubMed] [Google Scholar]
- 37.Sanchez-Sotelo J, Morrey BF. Surgical techniques for reconstruction of chronic insufficiency of the triceps. Rotation flap using anconeus and tendo achillis allograft. J Bone Joint Surg Br 2002; 84: 1116–1120. [DOI] [PubMed] [Google Scholar]
- 38.Little CP, Graham AJ, Carr AJ. Total elbow arthroplasty: a systematic review of the literature in the English language until the end of 2003. J Bone Joint Surg Br 2005; 87: 437–444. [DOI] [PubMed] [Google Scholar]
- 39.Ljung P, Jonsson K, Rydholm U. Short-term complications of the lateral approach for non-constrained elbow replacement. Follow-up of 50 rheumatoid elbows. J Bone Joint Surg Br 1995; 77: 937–942. [PubMed] [Google Scholar]
- 40.Pierce TD, Herndon JH. The triceps preserving approach to total elbow arthroplasty. Clin Orthop 1998; 354: 144–152. [DOI] [PubMed] [Google Scholar]
- 41.Guerroudj M, de Longueville J-C, Rooze M, Hinsenkamp M, Feipel V, Schuind F. Biomechanical properties of triceps brachii tendon after in vitro simulation of different posterior surgical approaches. J Shoulder Elb Surg Am 2007; 16: 849–853. [DOI] [PubMed] [Google Scholar]
- 42.Gschwend N. Our operative approach to the elbow joint. Arch Orthop Trauma Surg Arch Für Orthop Unf-Chir 1981; 98: 143–146. [DOI] [PubMed] [Google Scholar]
- 43.Frese E, Brown M, Norton BJ. Clinical reliability of manual muscle testing. Middle trapezius and gluteus medius muscles. Phys Ther 1987; 67: 1072–1076. [DOI] [PubMed] [Google Scholar]
- 44.Morrey BF, Askew LJ, An KN. Strength function after elbow arthroplasty. Clin Orthop 1988; 234: 43–50. [PubMed] [Google Scholar]
- 45.Anson B, Maddock W. Callander’s surgical anatomy, 4th edition Philidelphia, PA: WB Saunders Company, 1958. [Google Scholar]
- 46.Dwyer T, Henry PDG, Cholvisudhi P, Chan VWS, Theodoropoulos JS, Brull R. Neurological complications related to elective orthopedic surgery: part 1: common shoulder and elbow procedures. Reg Anesth Pain Med 2015; 40: 431–442. [DOI] [PubMed] [Google Scholar]
- 47.Hildebrand KA, Patterson SD, Regan WD, MacDermid JC, King GJ. Functional outcome of semiconstrained total elbow arthroplasty. J Bone Joint Surg Am 2000; 82A: 1379–1386. [DOI] [PubMed] [Google Scholar]
- 48.Özer H, Açar Hİ, Cömert A, Tekdemir İ, Elhan A, Turanli S. Course of the innervation supply of medial head of triceps muscle and anconeus muscle at the posterior aspect of humerus (anatomical study). Arch Orthop Trauma Sur 2006; 126: 549–553. [DOI] [PubMed] [Google Scholar]
- 49.Bertelli JA, Ghizoni MF. Nerve transfer from triceps medial head and anconeus to deltoid for axillary nerve palsy. J Hand Surg 2014; 39: 940–947. [DOI] [PubMed] [Google Scholar]