Abstract
Background and aims
The aim of this study was to determine the mortality and re-bleeding rates, and the risk factors involved, in a cohort of patients with previous diverticular bleeding (DB).
Methods
In 2007, data on 2462 patients with lower gastrointestinal (GI) bleeding were collected prospectively at several French hospitals. We studied the follow-up of patients with DB retrospectively. The following data were collected: age, mortality rates and re-bleeding rates, drug intake, surgery and comorbidities.
Results
Data on 365 patients, including 181 women (mean age 83.6 ± 9.8 years) were available. The median follow-up time was 3.9 years (IQR 25–75: 1.7–5.4). Of these, 148 patients died (40.5%). Among the 70 patients (19.2%) who had at least one re-bleeding episode, nine died and three underwent surgical procedures. Anticoagulation and antiplatelet therapy was discontinued in 70 cases (19.2%).
The independent risk factors contributing to mortality were age > 80 years (HR = 3.18 (2.1–4.9); p < 0.001) and a Charlson comorbidity score > 2 (1.91 (1.31–2.79); p = 0.003). Discontinuation of therapy was not significantly associated with a risk of death due to cardiovascular events. No risk factors responsible for re-bleeding were identified, such as antiplatelet and anticoagulant therapy in particular.
Conclusions
In this cohort, the rates of mortality and DB re-bleeding after a median follow-up time of 3.9 years were 19.2% and 40.5%, respectively. The majority of the deaths recorded were not due to re-bleeding.
Keywords: Aging, antiplatelet therapy, anticoagulant therapy, bleeding, diverticular bleeding, gastrointestinal bleeding, lower intestine, mortality, risk factors
Introduction
The estimated annual incidence of acute lower gastrointestinal bleeding (LGIB) ranges from 20.5 to 27.0 cases per 100,000 in the adult population at risk in the USA, and LGIB is a common indication for hospital admission.1 Diverticular bleeding (DB), which is the most common cause of LGIB, is involved in about one-third of LGIB cases.2–4 DB stops spontaneously in most cases (90%), although it can be severe.4,5 Diverticular bleeding is associated with mortality in up to 2–5% of cases.1,2,4 The 5-year re-bleeding rate reported after a first episode of DB ranges, depending on the series, from 6% to 25%.6 The frequency of diverticulosis increases with age: More than 60% of all people over 80 years of age have diverticula, and diverticular bleeding mainly affects the elderly.3,7–9 The risk factors responsible for diverticular bleeding have not yet been fully established.4,10,11 The most widely recognized risk factor is the use of non-steroidal anti-inflammatory drugs (NSAIDs),10,12 but cardiovascular risk factors such as hypertension and obesity may also be involved.13,14
Few long-term data are available so far on re-bleeding and mortality rates after the first episode of DB.6 The re-bleeding rates reported after a first episode of DB range from 6% to 25%, after an interval of 5 years.4,6,9 In 2007, we conducted a prospective 1-year multicentric study on LGIB at 102 French general hospitals, in which the data on 2462 patients were included, 790 (32%) of whom had DB.15 The aim of this retrospective study was to determine the mortality and re-bleeding rates due to DB, and the risk factors involved in this large cohort of patients.
Patients and methods
In 2007, data on 2462 patients presenting with LGIB were collected prospectively at 102 general hospitals in France during a period of 12 months. The procedure used in this observational study was approved by the CNIL (Commission Nationale de l’Informatique et des Libertés [French Commission on Information Technology and Liberties]). An endoscopy was performed on 2282 (92.7%) patients. The causes of LGIB were as follows: 790 patients (32%) had diverticular bleeding, 287 patients (11.7%) had ischemic colitis, 247 patients (10.0%) were bleeding from hemorrhoids, 222 patients (9.0%) were bleeding from tumors, 190 patients (7.7%) had traumatic ulceration of the rectum or anus, 100 patients (4.1%) had polyps, 79 patients (3.2%) had angiodysplasia, 76 patients (3.1%) had infectious colitis, 72 patients (2.9%) had inflammatory bowel disease (IBD), 55 patients (2.2%) had proctitis due to radiation treatments, 42 patients (1.7%) had non-steroidal anti-inflammatory drug (NSAID)-induced colitis, 35 patients (1.4%) had miscellaneous causes, while no cause was identified in 246 patients (10.0%). Among the 790 patients with DB, 17 (2.15%) died during their index episode in 2007.
In 2013, we decided to study the middle-term outcome of the surviving patients with DB (n = 773). To obtain follow-up data, the investigators at all centers were contacted by e-mail and phone: Answers were obtained on 437 patients. If no follow-up data were available, the general practitioner (GP); or as a last resort, the patient or the main GP mentioned at the patient’s first admission were contacted. Data could be properly analyzed in only 365 cases (83.5%) (Figure 1).
Figure 1.
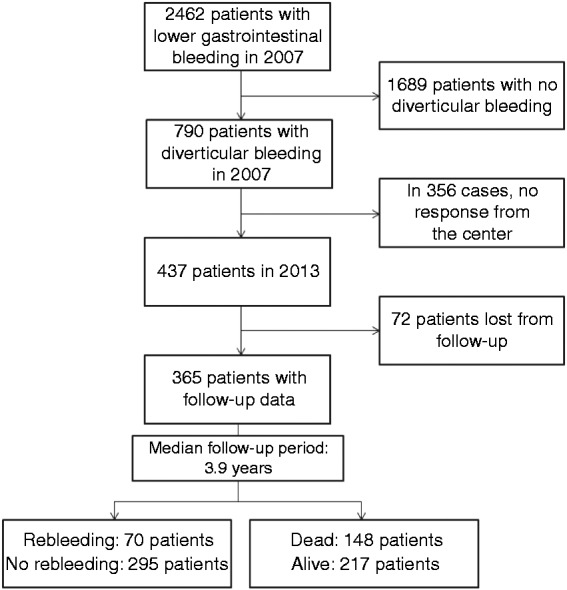
Flow chart.
The mean age of the 790 patients in the initial population (i.e. at the beginning of 2007) was 78.9 ± 10.2 years. This population consisted of 387 women (49%) and 402 men (51%). At their admission in 2007, the mean Charlson comorbidity score, which was available in the case of 675 patients, was 2.25 ± 1.90.
Patients who died at an early stage (before day 30 after the initial diverticular bleeding in 2007 (17 patients (2.15%)) were excluded from the study. Some patients had early re-bleeding (<30 days after the initial bleeding episode: 74 patients (9.4%)); these early re-bleeding events were not assimilated into the late re-bleeding group, but the patients in question were not excluded from the study.
In 2013, the following clinical data were recorded: age; gender; re-bleeding; death; cause of death; the use of NSAIDs, anticoagulants or antiplatelet drugs; surgery; discontinuation of antiplatelet or anticoagulants because of bleeding; the need for endoscopic therapeutic procedures or surgery; cardiovascular events such as stroke or ischemic heart disease. The Charlson comorbidity score and the presence of an initial hemoglobin level <7.0 g/dL recorded in 2007 were used as potential predictive factors of death and re-bleeding. All patients with re-bleeding had a colonoscopy. The diagnosis was based on Jensen's criteria: active bleeding from a diverticulum; the presence of non-bleeding visible vessels; adherent clots; fresh blood in a localized segment of the colon; diverticular ulceration with fresh blood in the vicinity; fresh blood not present in the ileum, but present in the colon; and no other causes of colonic bleeding identified.16
Statistical analysis
Data were expressed as means ± SDs, or median and interquartile ranges (IQRs) from 25–75%, in the case of continuous data. We used the Student’s t-test for quantitative variables and the Chi-square test or Fisher’s exact test for qualitative variables in the univariate analyses.
The endpoint used in the survival analysis was death and the data were removed from the analysis at the time of the last visit. The Kaplan-Meier method was used to estimate the cumulative mortality 1, 3 and 5 years after the initial bleeding episode. The following mortality risk factors were analyzed: age >80 years, gender, late re-bleeding, anticoagulant or antiplatelet therapy, ischemic events, hemoglobin <7 g/dl and initial Charlson comorbidity score >2 during the first episode of DB. We used these factors in the univariate analysis and the multivariate analysis, using regression analysis and the Cox method.
The endpoint adopted in the re-bleeding analysis was diverticular re-bleeding, and the data were removed from the analysis at the time of the last visit or death. The Kaplan-Meier method was used to estimate the rate of diverticular re-bleeding at 1, 3 and 5 years after the first bleeding episode. The factors possibly associated with re-bleeding were analyzed: age >80 years, gender, anticoagulant or antiplatelet therapy prior to re-bleeding, Charlson comorbidity score >2, and a past history of bleeding. These factors were tested by performing univariate analysis and multivariate analysis, using regression analysis and the Cox method. A p value of <0.05 was taken to be significant.
We performed all statistical analyses using the SPSS software program, version 13.0 (IBM, Armonk, New York, USA).
Results
Patient characteristics
The initial characteristics of patients (at their first admission in 2007 for DB) are presented in Supplementary Table 1: There were no clear-cut differences between the patients lost to follow-up, those for whom no information could be obtained from the hospital center, and the 365 patients constituting the present study population, except for the systolic blood pressure levels <10 mmHg, which occurred significantly more frequently in patients from the non-responding centers.
The main clinical characteristics of the 365 patients in our study at their first admission in 2007 and at the end of the follow-up period are presented in Table 1.
Table 1.
Characteristics of the 365 patients with diverticular bleeding
| 2007 | End of follow-up | |
|---|---|---|
| Total patients, n (%) | 365 (100%) | 365 (100%) |
| Age in years, mean (SD) | 79.5 ± 10.0 | 83.6 ± 9.7 |
| Male patients, n (%) | 184 (50.4%) | 184 (50.4%) |
| Median follow-up time,years (median and IQR) | 3.9 (IQR 25–75: 1.7–5.4) | |
| Mortality rate, n (%) | - | 148 (40.5%) |
| Initial comorbidity,Charlson’s score; mean (SD) | 2.8 ± 1.8 | - |
| History of diverticular bleeding (prior to 2007), n (%) | 48 (13.1%) | - |
| Anticoagulant or antiplatelet therapy,n (%) | 244 (66.8%) | 217 (59.4%) |
| Aspirin, n (%) | 135 (37.0%) | 115 (31.5%) |
| Clopidogrel, n (%) | 50 (13.7%) | 40 (11.4%) |
| Antivitamin K, n (%) | 102 (27.9%) | 91 (24.9%) |
| Bitherapya, n (%) | 41 (10.3%) | 28 (7.7 %) |
| No treatment, n (%) | 121 (33.2%) | 148 (40.5%) |
Bitherapy: various combinations of antiplatelet and/or anticoagulant drugs. Treatment at discharge from hospital in 2007.
IQR: interquartile range; n: number of patients
The 365 patients included in this study, 184 of whom were men (50.4%), had a median follow-up time of 3.9 years (25–75% IQR: 1.7–5.4). Their mean age was 83.6 ± 9.7 years at the end of the follow-up period. We had 101 patients (27.7%) whom were over 90 years old at the last news. The women were significantly older than the men at the end of the follow-up period (mean age 86.3 ± 8.5 years versus 80.8 ± 10.2 years, respectively (p < 0.0001). There were 48 (13.1%) patients who had a history of prior DB, prior to 2007.
A total of 244 patients (66.8%) were under anticoagulant or antiplatelet therapy in 2007, as compared with 217 (59.4%) at the end of the follow-up period. A total of 109 patients (28.9%) had an initial Charlson comorbidity score >2.
Re-bleeding
There were 70 patients (19.2%) who had diverticular re-bleeding during the follow-up period. There were 22 patients (6.0%) who had more than one re-bleeding episode: 15 patients had two episodes, four patients had three episodes, two patients had four episodes and one patient had eight episodes. Their re-bleeding rate was 11% after 1 year and 21% after 3 years. The estimated 5-year re-bleeding rate was 30% (Figure 2).
Figure 2.
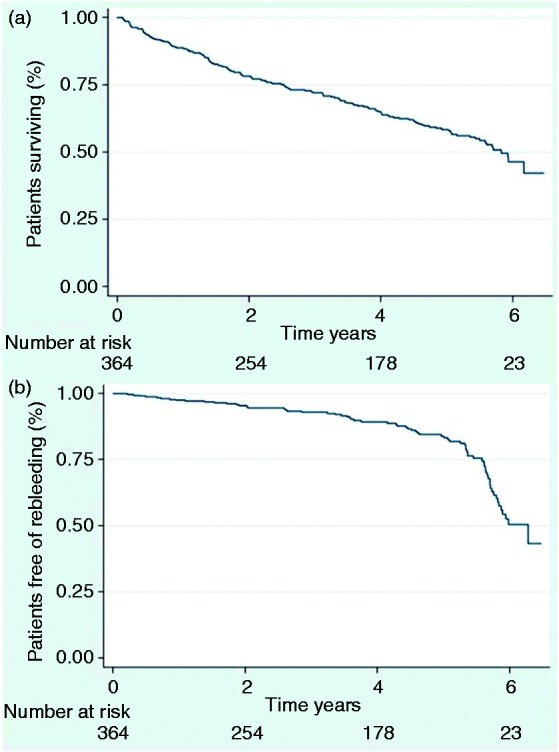
(a) Actuarial survival of 365 patients with DB and (b) Actuarial risk of re-bleeding in 365 patients with DB.
DB: diverticular bleeding
Two patients underwent endoscopic treatment (clips) and three patients (4.3%) had surgical treatment (an emergency colectomy). Of the 15 patients who underwent colectomy for the 2007 hemorrhage, three subsequently re-bled. Five patients had diverticulitis during the follow-up period, including one who had a colectomy.
Among the 70 patients with re-bleeding events, nine died (12.8%); which is a significantly higher mortality rate than that observed in 2007 among the whole initial population (17 out of 790 patients (2.15%); p < 0.001). The main characteristics of the re-bleeding and the non-re-bleeding patients are presented in Table 2.
Table 2.
Characteristics of re-bleeding and non-rebleeding patients at the time of the index diverticular bleeding episode in 2007
| Characteristics | Re-bleeding patients | Non-rebleeding patients | Total | p |
|---|---|---|---|---|
| n | 70 | 295 | 365 | |
| Age at last news,mean (SD) | 81.4 ± 12.1 | 84.1 ± 9.1 | 83.6 ± 9.7 | 0.04 |
| Male gender, n (%) | 37 (52.9%) | 147 (49.8%) | 184 (50.4%) | 0.65 |
| Initial comorbidity Charlson’s score, mean (SD) | 1.90 ± 1.70 | 2.3 ± 1.9 | 2.8 ± 1.8 | 0.11 |
| History of diverticular bleeding (prior to 2007), n (%) | 18 (25.7%) | 49 (16.6%) | 67 (13.1%) | 0.077 |
| SBP < 100 mmHg, n (%) | 13 (18.6%) | 33 (11.2%) | 46 (12.6%) | 0.094 |
| Hb at admission, g/dL, mean (SD) | 10.7 ± 2.65 | 11.2 ± 2.4 | 11.1 ± 2.4 | 0.13 |
| Hb < 10 g/dL, n (%) | 26 (37.1%) | 85 (28.8%) | 111 (30.4%) | 0.17 |
| Transfusion, n (%) | 39 (55.7%) | 117 (39.7%) | 156 (42.7%) | 0.015 |
| Endoscopic treatment, n (%) | 4 (5.7%) | 11 (3.7%) | 15 (4.1%) | 0.68 |
| Surgical treatment, n (%) | 4 (5.7%) | 12 (4.1%) | 16 (4.4%) | 0.78 |
| Early re-bleeding, n (%) | 7 (10%) | 23 (7.7%) | 30 (8.2%) | 0.55 |
| Anticoagulant or antiplatelet therapy, n (%) | 51 (72.9%) | 193 (65.4%) | 244 (66.8%) | 0.23 |
| Aspirin, n (%) | 22 (31.4%) | 113 (38.3%) | 135 (37.0%) | 0.28 |
| Clopidogrel, n (%) | 14 (20%) | 36 (12.2%) | 50 (13.7%) | 0.09 |
| Antivitamin K, n (%) | 23 (32.9%) | 79 (26.8%) | 102 (27.9%) | 0.31 |
| Bi or tritherapy, n (%) | 7 (10%) | 34 (11.5%) | 41 (10.3%) | 0.72 |
| NSAIDs, n (%) | 3 (4.3%) | 6 (2.0%) | 9 (2.5%) | 0.51 |
Early re-bleeding: diverticular re-bleeding within the first 30 days of the index DB in 2007.
Treatment at discharge from hospital in 2007.
DB: diverticular bleeding; Hb: hemoglobin; mm Hg: pressure in millimeters of mercury; n: number of patients; NSAID: non-steroidal anti-inflammatory drugs; SBP: systolic blood pressure.
Mortality
Between 2007 and 2013, there were 148 (40.6%) patients who died. The survival rate was 78% after 1 year and 64% after 3 years. The estimated survival rate after 5 years was 48%. The cumulative survival times calculated using the Kaplan-Meier method are presented in Figure 2.
The main causes of death are shown in the Supplementary Table 2. Causes of death were: heart and respiratory failure (16.9%), multifactorial causes (15.5%), ischemic events (stroke, myocardial infarctions or critical limb ischemia; 11.5%), cancer (10.8%), other causes (6.8%), re-bleeding (6.1%), infection (6.1%) and dementia (3.4%). Only nine deaths (6.1%) were directly due to diverticular re-bleeding. The cause of death was unknown in 34 (23.0%) cases in which no access to the patients’ death certificates was available.
Possible risk factors for re-bleeding events ruled out
Age, gender, history of bleeding, a Charlson comorbidity score >2, and anticoagulant or antiplatelet therapy before re-bleeding were not found in the univariate and multivariate analyses to be associated with diverticular re-bleeding (Table 3).
Table 3.
Risk factors significantly associated with re-bleeding, based on univariate and multivariate analyses
| Univariate |
Multivariate |
||||
|---|---|---|---|---|---|
| n | OR (CI 95%) | p | OR (CI 95%) | p | |
| Age >80 years | 262 | 1.74 (0.97–3.11) | 0.06 | 0.71 (0.38–1.32) | 0.28 |
| Female patients | 181 | 0.89 (0.51–1.54) | 0.65 | 0.75 (0.41–1.39) | 0.36 |
| Anticoagulant or antiplatelet therapy prior to re-bleeding | 244 | 1.42 (0.77–2.64) | 0.23 | 0.66 (0.33–1.30) | 0.23 |
| Comorbidity Charlson score >2 | 109 | 0.52 (0.26–1.03) | 0.06 | 0.58 (0.30–1.12) | 0.10 |
| Previous history of bleeding | 48 | 1.74 (0.89–3.36) | 0.11 | 1.69 (0.82–3.49) | 0.16 |
n: number of patients; OR: odds ratio
Risk factors for mortality
In the univariate analysis, the following risk factors were found to contribute to mortality: age >80 years (OR = 3.37; 95% CI 1.94–5.88), female gender (OR = 1.55; 95% CI 1–2.41), and a Charlson comorbidity score >2 (OR = 2.12; 95% CI 1.28–3.54). Neither re-bleeding, an initial hemoglobin level <7 g/dl, anticoagulant or antiplatelet drug therapy prior to re-bleeding, nor ischemic events during the follow-up period were found to be associated with mortality.
In the multivariate analyses, only age >80 years (HR = 3.18; 95% CI 2.1–4.9; p < 0.0001) and a Charlson comorbidity score >2 (HR = 1.91; 95% CI 1.31–2.79; p = 0.001) were found to be independently associated with mortality. Re-bleeding did not seem to be an independent factor contributing to mortality; however, this event was rare, and 9 out of the 70 re-bleeders died (see Supplementary Table 3).
Anticoagulant or antiplatelet therapy
Data on therapies were available on 355 patients (97.3%) during the follow-up period. During the index DB in 2007, information about anticoagulants and antiplatelet drugs were recorded on all the patients; during the follow-up period, no data about these treatments was available any longer in the case of 15 patients (4.1%). While 244 patients underwent anticoagulant or antiplatelet therapy in 2007, there were 217 (59.4%) who were undergoing treatment at the end of the follow-up period (Table 4).
Table 4.
Antithrombotic and antiplatelet treatment
| Index diverticular bleeding (2007) | Most frequent indication | At the end of follow-up | Most frequent indication | |
|---|---|---|---|---|
| Anticoagulant or antiplatelet drugs, n (%) | 244 (66.8%) | Coronary vascular disease, 66 (27.9%) | 217 (59.4%) | Coronary vascular disease, 61 (28.1%) |
| Antiplatelet drugs, n (%) | 160 (43.8%) | Coronary vascular disease, 66 (41.3%) | 141 (38.6%) | Coronary vascular disease, 61 (43.3%) |
| Aspirin, n (%) | 135 (37.0%) | Coronary vascular disease, 55 (40.7%) | 115 (31.5%) | Coronary vascular disease, 47 (40.9%) |
| Clopidogrel, n (%) | 50 (13.7%) | Coronary vascular disease, 26 (52%) | 40 (11.0%) | Coronary vascular disease, 24 (60%) |
| Anti-vitamin K, n (%) | 102 (27.9%) | Cardiac arrhythmia, 52 (51%) | 91 (24.9%) | Cardiac arrhythmia, 44 (48.3%) |
| Bitherapya, n (%) | 41 (11.2%) | Coronary vascular disease, 16 (39%) | 28 (7.7 %) | Coronary vascular disease, 10 (38.5%) |
| Heparin, n | 1 | 3 | ||
| No treatment, n (%) | 121 (33.2%) | 148 (40.5%) | ||
| No information, n (%) | 0 | 10 (2.7%) |
Bitherapy: two-fold anticoagulation or antiplatelet treatment.
n: number of patients
Table 5.
Diverticular re-bleeding after 1 year: Comparisons between various studies.
| Studies | Patients (n) | Prospective or retrospective | Re-bleeding after 1 year of follow-up (%) | Median follow-up time (months) |
|---|---|---|---|---|
| Poncet et al. 2010 | 133 | prospective | 3.8% | 47.5 |
| Niikura et al. 2012 | 72 | retrospective | 20% | 51.2 |
| Nishikawa et al. 2013 | 172 | prospective | 34.8% | 26.4 |
| Aytac et al. 2014 | 78 | retrospective | 30% | 8.1 |
| Okamoto et al. 2015 | 100 | prospective | 47% | 43.7 |
| Lorenzo et al. 2016 | 365 | retrospective | 11% | 46.8 |
At the end of the follow-up period, 217 patients were under anticoagulant or antiplatelet drugs (59.4%), 115 (31.5%) were taking aspirin, 40 (11.0%) were taking clopidogrel, 91 (24.9%) were taking antivitamin K, 28 patients (7.7%) were receiving combined drug therapy (13 patients (3.6%) were taking a combination of antiplatelet and anticoagulant drugs, 14 patients (3.8%) a combination of antiplatelet drugs and one patient was under tri-therapy). Nine patients (2.6%) were taking NSAIDs.
There were 70 patients (20%) who stopped their antiplatelet or anticoagulant treatment at least once, because of GI bleeding at some point in their history; 45 of them were taking this treatment at the end of the follow-up period. The characteristics of patients who discontinued antiplatelet or anticoagulant treatment are presented in Supplementary Table 4. Supplementary Table 5 gives details of the initial and last treatments, along with the risk of re-bleeding events or death.
Ischemic events
There were 35 ischemic events that occurred: 13 (37.1%) consisted of myocardial infarction, 18 of stroke (51.4%) and 4 (11.4%) were events of other kinds. Five events (three consisting of myocardial infarction and two of stroke) occurred after anticoagulant or antiplatelet withdrawal because of DB, and two of these patients died.
Discussion
The results obtained in this study on a large, unselected, prospectively recruited population of patients with DB show that one out of five of the patients in the study population ran a middle-term risk of re-bleeding again and the specific mortality rate of 13% that was recorded was higher than during the first episode of DB. In this elderly population, the mortality rate was high, but re-bleeding accounted for only 6% of the deaths; we identified age and comorbidities as the only independent risk factors contributing to mortality.
Patient age
DB usually affects people over 65 years of age.7,10,15,17,18 In this study, the patients’ mean age was higher (79.5 ± 10.2 years at the beginning of the study) than that of the patients included in previous studies, and 101 patients (27.7%) were over 90 years of age. In another recent prospective French study on 133 patients with DB, the mean age was 75.7 years,6 and in some recent Japanese studies, the mean age ranged between 63 and 72 years.19–22 Diverticular bleeding, therefore, seems to increasingly affect old to very old people.
Re-bleeding events
Incidence
The re-bleeding rates reported in previous studies after a first episode of DB range from 6% to 47% after 5 years,6 as is shown in Table 5. Some authors report very high re-bleeding rates, but these rates included early re-bleeding episodes.23,24 In the present study, the 1-year re-bleeding rate was 11%, the 3-year rate was 21%, and the predicted 5-year rate was 30%.
Risk factors
The main LGIB and DB risk factors identified in several studies on Caucasian and Asian populations were NSAIDs, aspirin, obesity, hypertension and ischemic heart disease.11,13,14,25–29 Two recent meta-analyses confirm the role of NSAIDs and aspirin in DB.26,27 The use of anticoagulants is not thought to be a risk factor for DB, but it increases the severity of the bleeding.11,22,30 Less information is available about the risk factors responsible for re-bleeding, which include: a past history of diverticular bleeding,3,9 regular use of NSAIDs (OR: 2.49–3.7),13,27,31 antiplatelet treatment (OR: 1.70–2.39),11,26,27 and obesity and visceral fat accumulation (OR: 1.00–3.19).14,22,32 In our study population, the rate of use of NSAIDs was low (nine patients, three of whom had re-bleeding episodes). Aytac et al.23 report that an advanced age at the time of initial bleeding is associated with re-bleeding events (p = 0.001).
In this study, neither antiplatelet nor anticoagulant treatments were found to be independent risk factors contributing to re-bleeding and mortality. In a recent single-center retrospective study by Aoki et al.,19 only non-aspirin and dual anti-platelet drugs, but not low-dose aspirin alone, were found in multivariate analyses to be independently associated with re-bleeding events.
Effects of previous treatment for DB
Few of the present patients’ initial diverticular bleeding events were treated by performing surgery or endoscopy, so we cannot say at the present stage whether this strategy may affect the natural history of the disease. Among the 171 cases of endoscopic treatment reported in the literature, 31 cases (18%) of early and late re-bleeding occurred, which is not very different from the classical re-bleeding rate of 25%.4,16,33 In the present study, four out of the nine patients who initially underwent endoscopic treatment subsequently re-bled; and three out of the 15 patients who were colectomized during the previous episode re-bled.
Mortality
Incidence
There are few data available on late mortality and mortality specifically due to re-bleeding. In this study, the mortality rate was found to be 40.5% and the re-bleeding rate was 19.2%.
The rates of early mortality and 30-day mortality reported in previous studies ranged between 0 and 7%,1,3,19 as compared with 2.15% in the present study. There are fewer data available on late mortality and mortality specifically due to re-bleeding events. In a recent Japanese study, the LGIB mortality rate was 6.1% during a mean follow-up period of 28 months, including bleeding-related deaths (0.6%).19
In a study by Jeyarajah et al.,18 the all-cause mortality rate 1 year after the occurrence of diverticular complications was 14.5%. In the present study, a high mortality rate was observed: 22% after 1 year, 36% after 3 years and 52% after 5 years: This is probably because of the advanced age of our study population (83.6 ± 9.8 years, mean) and the large number of comorbidities involved. The great majority of the deaths were due to common causes. DB accounted for only 6.1% of the causes of death in our study population, in line with the rates previously reported in the literature4,6,21,23; however, the mortality rate due to DB was 6 times higher after a re-bleeding episode than during the previous one (12.8% versus 2.15%). It is therefore possible that re-bleeding per se may increase the mortality rates, rather than age and comorbidities, as observed in this population.
Risk factors
The main risk factors known to be responsible for early mortality have mostly been studied in LGIB in general, and include: pulse ≥100/min, systolic blood pressure ≤115 mm Hg, syncope, absence of abdominal pain, rectal bleeding during the last 4 hours before evaluation, INR (international normalized ratio) > 1.5, taking aspirin and the presence of more than two co-morbidities.30,34
In an English study, the 1-year all-cause mortality risk factors identified after diverticular complications were: advanced age, a large number of co-morbidities and admission to an emergency ward.18 In the present study, only an advanced age and a large number of co-morbidities were found to be independently associated with long-term mortality in DB patients.
Effects of antiplatelet and anticoagulant drug withdrawal
In a large prospective study on peptic ulcer bleeding, withdrawal of antiplatelet treatment increased the risk of mortality, while continuation of the treatment slightly increased the risk of re-bleeding events.35 In the present study, among those patients whose anticoagulant or antiplatelet therapy was stopped after the index episode of DB, only five patients out of 70 had an ischemic event (including three cases of myocardial infarction and two strokes, two of whom died): This proportion was the same as in the patients who continued to take their treatment; however, the great majority of the patients’ treatments were continued, and these patients may have been carefully selected, in this context.
Strengths and limitations of this study
The strengths of our study are the large number of patients followed, who were representative of our index population attending 53 centers located all over France during a period of 1 year in 2007; the prospective nature of the initial recruitment, which meant that it was possible to obtain a clearly-defined initial diagnosis; and the overall quality of the information obtained during the follow-up period.
This study has several limitations:
First, because of its retrospective nature, some patients were lost as follow-up patients, some data were missing, and a selection bias may have been present (initial presentation was similar; however, between the patients who were included and those not included in the study, see the Supplementary Table 1).
Second, the information about patients’ treatment was collected in 2007 and at the end of the follow-up period, and there the need to stop treatment for bleeding was noted. We had no information about the patients’ drug observance; however, some patients may have stopped and resumed their treatment several times.
Third, we had no information about the patients’ body mass index, although it was suggested in previous studies that obesity may be associated with the risk of re-bleeding events.22
Conclusions
In this retrospective nationwide study on DB, re-bleeding events occurred in one out of five patients, and the mortality rate (12%) was 6 times higher than that associated with the first episode. The mortality rate was high in these fairly elderly patients with multiple diseases, but re-bleeding was only responsible for 6% of the deaths recorded during the study period. No significant increase in the risks of re-bleeding or the mortality was observed in patients whose antiplatelet therapy and anticoagulant therapy was continued, nor was a particularly high risk of ischemic events observed in those patients who had treatment discontinued.
Supplementary Material
Disclosures
The authors declare that there are no conflicts of interest. Also, the sponsors were not involved in any way in the study design nor in the collection, analysis or interpretation of the data.
Funding
This work was supported by Sanofi-Aventis (unrestricted grant).
Note
Alexandre Pariente and Stéphane Nahon contributed equally to this paper.
References
- 1.Farrell JJ, Friedman LS. Review article: The management of lower gastrointestinal bleeding. Aliment Pharmacol Ther 2005; 21: 1281–1298. [DOI] [PubMed] [Google Scholar]
- 2.Strate LL, Syngal S. Timing of colonoscopy: Impact on length of hospital stay in patients with acute lower intestinal bleeding. Am J Gastroenterol 2003; 98: 317–322. [DOI] [PubMed] [Google Scholar]
- 3.Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: A population-based study. Am J Gastroenterol 1997; 92: 419–424. [PubMed] [Google Scholar]
- 4.Adams JB, Margolin DA. Management of diverticular hemorrhage. Clin Colon Rectal Surg 2009; 22: 181–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strate LL, Saltzman JR, Ookubo R, et al. Validation of a clinical prediction rule for severe acute lower intestinal bleeding. Am J Gastroenterol 2005; 100: 1821–1827. [DOI] [PubMed] [Google Scholar]
- 6.Poncet G, Heluwaert F, Voirin D, et al. Natural history of acute colonic diverticular bleeding: A prospective study in 133 consecutive patients. Aliment Pharmacol Ther 2010; 32: 466–471. [DOI] [PubMed] [Google Scholar]
- 7.Farrell JJ, Friedman LS. Gastrointestinal bleeding in the elderly. Gastroenterol Clin North Am 2001; 30: 377–407. [DOI] [PubMed] [Google Scholar]
- 8.Schoetz DJ. Diverticular disease of the colon: A century-old problem. Dis Colon Rectum 1999; 42: 703–709. [DOI] [PubMed] [Google Scholar]
- 9.Raphaeli T, Menon R. Current treatment of lower gastrointestinal hemorrhage. Clin Colon Rectal Surg 2012; 25: 219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jansen A. Risk factors for colonic diverticular bleeding: A westernized community-based hospital study. World J Gastroenterol 2009; 15: 457–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Strate LL, Liu YL, Huang ES, et al. Use of aspirin or nonsteroidal anti-inflammatory drugs increases risk for diverticulitis and diverticular bleeding. Gastroenterology 2011; 140: 1427–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laine L, Smith R, Min K, et al. Systematic review: The lower gastrointestinal adverse effects of non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther 2006; 24: 751–767. [DOI] [PubMed] [Google Scholar]
- 13.Okamoto T, Watabe H, Yamada A, et al. The association between arteriosclerosis-related diseases and diverticular bleeding. Int J Colorectal Dis 2012; 27: 1161–1166. [DOI] [PubMed] [Google Scholar]
- 14.Suzuki K, Uchiyama S, Imajyo K, et al. Risk factors for colonic diverticular hemorrhage: Japanese multicenter study. Digestion 2012; 85: 261–265. [DOI] [PubMed] [Google Scholar]
- 15.Bour B, Pilette C, Lesgourgues B, et al. Hémorragies digestives basses aiguës: Résultats préliminaires d’une étude de l’ANGH sur plus de 1000 malades. Endoscopy 2008; 40 (2008, accessed 20 July 2015). [Google Scholar]
- 16.Jensen DM, Machicado GA, Jutabha R, et al. Urgent colonoscopy for the diagnosis and treatment of severe diverticular hemorrhage. N Engl J Med 2000; 342: 78–82. [DOI] [PubMed] [Google Scholar]
- 17.Kaltenbach T, Watson R, Shah J, et al. Colonoscopy with clipping is useful in the diagnosis and treatment of diverticular bleeding. Clin Gastroenterol Hepatol 2012; 10: 131–137. [DOI] [PubMed] [Google Scholar]
- 18.Jeyarajah S, Faiz O, Bottle A, et al. Diverticular disease hospital admissions are increasing, with poor outcomes in the elderly and emergency admissions. Aliment Pharmacol Ther 2009; 30: 1171–1182. [DOI] [PubMed] [Google Scholar]
- 19.Aoki T, Nagata N, Niikura R, et al. Recurrence and mortality among patients hospitalized for acute lower gastrointestinal bleeding. Clin Gastroenterol Hepatol 2015; 13: 488–494. [DOI] [PubMed] [Google Scholar]
- 20.Tanaka Y, Motomura Y, Akahoshi K, et al. Predictive factors for colonic diverticular rebleeding: A retrospective analysis of the clinical and colonoscopic features of 111 patients. Gut Liver 2012; 6: 334–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fujino Y, Inoue Y, Onodera M, et al. Risk factors for early re-bleeding and associated hospitalization in patients with colonic diverticular bleeding. Colorectal Dis 2013; 15: 982–986. [DOI] [PubMed] [Google Scholar]
- 22.Nagata N, Sakamoto K, Arai T, et al. Visceral fat accumulation affects risk of colonic diverticular hemorrhage. Int J Colorectal Dis 2015; 30: 1399–1406. [DOI] [PubMed] [Google Scholar]
- 23.Aytac E, Stocchi L, Gorgun E, et al. Risk of recurrence and long-term outcomes after colonic diverticular bleeding. Int J Colorectal Dis 2014; 29: 373–378. [DOI] [PubMed] [Google Scholar]
- 24.Nishikawa H, Maruo T, Tsumura T, et al. Risk factors associated with recurrent hemorrhage after the initial improvement of colonic diverticular bleeding. Acta Gastro Enterol Belg 2013; 76: 20–24. [PubMed] [Google Scholar]
- 25.Wilcox CM, Alexander LN, Cotsonis GA, et al. Nonsteroidal anti-inflammatory drugs are associated with both upper and lower gastrointestinal bleeding. Dig Dis Sci 1997; 42: 990–997. [DOI] [PubMed] [Google Scholar]
- 26.Yuhara H, Corley DA, Nakahara F, et al. Aspirin and non-aspirin NSAIDs increase risk of colonic diverticular bleeding: A systematic review and meta-analysis. J Gastroenterol 2014; 49: 992–1000. [DOI] [PubMed] [Google Scholar]
- 27.Kvasnovsky CL, Papagrigoriadis S, Bjarnason I. Increased diverticular complications with nonsteriodal anti-inflammatory drugs and other medications: A systematic review and meta-analysis. Colorectal Dis 2014; 16: 189–196. [DOI] [PubMed] [Google Scholar]
- 28.Sugihara Y, Kudo S-E, Miyachi H, et al. Analysis of risk factors for colonic diverticular bleeding: A matched case-control study. Gut Liver 2015; 10: 244–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamada A, Sugimoto T, Kondo S, et al. Assessment of the risk factors for colonic diverticular hemorrhage. Dis Colon Rectum 2008; 51: 116–120. [DOI] [PubMed] [Google Scholar]
- 30.Lee KK, Shah SM, Moser MA. Risk factors predictive of severe diverticular hemorrhage. Int J Surg Lond Engl 2011; 9: 83–85. [DOI] [PubMed] [Google Scholar]
- 31.Niikura R, Nagata N, Yamada A, et al. Recurrence of colonic diverticular bleeding and associated risk factors. Colorectal Dis 2012; 14: 302–305. [DOI] [PubMed] [Google Scholar]
- 32.Strate LL, Liu YL, Aldoori WH, et al. Obesity increases the risks of diverticulitis and diverticular bleeding. Gastroenterology 2009; 136: 115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Akutsu D, Narasaka T, Wakayama M, et al. Endoscopic detachable snare ligation: A new treatment method for colonic diverticular hemorrhage. Endoscopy 2015; 47: 1039–1042. [DOI] [PubMed] [Google Scholar]
- 34.Strate LL, Ayanian JZ, Kotler G, et al. Risk factors for mortality in lower intestinal bleeding. Clin Gastroenterol Hepatol 2008; 6: 1004–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sung JJY, Lau JYW, Ching JYL, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: A randomized trial. Ann Intern Med 2010; 152: 1–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


