Abstract
Background
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common childhood psychiatric disorders and negatively impacts caregivers’ lives. Factors including barriers to accessing care, dissatisfaction with support services, and lack of caregiver resources may contribute to this.
Objectives
To report caregivers’ experiences of ADHD diagnosis, behavioral therapy (BT), and supportive care for children/adolescents with ADHD.
Methods
The Caregiver Perspective on Pediatric ADHD (CAPPA) survey included caregivers of children/adolescents (6–17 years) from ten European countries who were currently receiving/had received ADHD pharmacotherapy in the previous 6 months. Caregivers reported experiences of obtaining an ADHD diagnosis, access to BT, availability of caregiver resources, and level of health care/school support. Pan-EU and country-specific descriptive statistics are reported; responses were compared across countries.
Results
Of 3,616 caregivers, 66% were female. Mean age of children/adolescents was 11.5 years; 80% were male. Mean time from the first doctor visit to diagnosis was 10.8 (95% confidence interval 10.2, 11.3) months; 31% of caregivers reported the greatest degrees of difficulty in obtaining an ADHD diagnosis; 44% of children/adolescents did not receive BT. Forty-seven percent of caregivers reported that sufficient resources were available, 44% were “very satisfied”/“satisfied” with medical care, and 50% found health care providers “very supportive”/“somewhat supportive”. Mainstream schools were attended by 82% of children/adolescents. Of those, 67% of caregivers thought schools could help more with the child/adolescent’s ADHD and 48% received extra help/special arrangement. Results varied significantly between countries (P<0.001, all parameters).
Conclusion
Almost a third of caregivers reported a high degree of difficulty in obtaining an ADHD diagnosis for their child/adolescent, less than half felt that sufficient resources were available, and gaps in support from health care providers/schools were identified. Findings underscore the need to improve access to diagnosis and provision of supportive services to enable better standards of care, and potentially reduce the impact of child/adolescent ADHD on caregivers’ lives.
Keywords: attention-deficit/hyperactivity disorder, burden of illness, caregivers, diagnosis, treatment
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common psychiatric disorders of childhood, affecting 3%–5% of children and adolescents worldwide,1,2 and is characterized by symptoms of inattention, hyperactivity, and impulsivity. ADHD can lead to substantial negative effects on quality of life among children/adolescents and their caregivers.3–6 Consequently, it is imperative to have an understanding of the difficulties experienced, and the obstacles encountered, by parents and caregivers of children and adolescents with ADHD. Identifying the barriers to accessing care, and dissatisfaction with services and support provided by school and health care systems, as well as insufficient caregiver resources may help guide policymaking on these issues by providing specific insights into the caregivers’ perspective.
Recent findings from a systematic review showed that barriers to accessing care for children with ADHD can operate at the individual, organizational, or societal level.7 In a longitudinal study (N=162), the majority of parents of children who used specialist services reported barriers to accessing services, with the most common barrier being the lack of information about who could help.8 Insufficient information for parents/caregivers of children/adolescents with ADHD was reported in a qualitative focus group study (n=16 parents).9 In a UK survey (N=176), around half of children with ADHD had not accessed specialist health care services, despite clinical practice guidelines recommending that only specialist services should perform diagnostic assessments and initiate pharmacotherapy for ADHD.10 Delayed diagnosis, inadequate access to information, and a lack of coordinated care have been frequently reported as reasons for parental dissatisfaction with services.11–13 A US longitudinal study (N=374) found that a low proportion of parents of adolescents with childhood ADHD reported having formal (health care provider [14%] or teacher [4%]) support.14 A large US study (N=5,495) of the partnership between families and their child’s health care providers found that a family–provider partnership was associated with fewer missed school days and more preventive care visits among children with ADHD.15
Established guidelines on ADHD treatment, including those of the UK National Institute for Health and Care Excellence (NICE), recommend a multimodal treatment approach that includes a combination of teacher involvement, caregiver education programs, medication, and behavioral therapy (BT).16–21 The combination of parent and school intervention programs has been shown to produce improvements in symptoms and academic outcomes among children with ADHD.22,23 However, studies have shown difficulties with implementation of guidelines in community practice settings. Recent feedback from clinicians in the UK, obtained using multiple methods (N=47) and rated using a Delphi survey method (n=12 panelists), identified the delivery of BT as one of the National Institute for Health and Care Excellence recommendations that is challenging to implement in routine practice.24 Additionally, a large European multinational chart review study found that 39% of children/adolescents with ADHD had not received BT at any time.25
The large, cross-sectional Caregiver Perspective on Pediatric ADHD (CAPPA) survey collected real-world information about caregivers’ experiences with ADHD diagnosis, treatment, and services in Europe.26 With the aim of identifying gaps in access to diagnosis and supportive care, we now report outcomes from the CAPPA survey related to the caregivers’ perspective of referral for, and diagnosis of, ADHD in children/adolescents, use of BT, and support for caregivers from the health care system and schools.
Methods
Study design
The CAPPA survey was designed to evaluate the burden associated with ADHD and its treatment, and identify the unmet needs in ADHD management. The survey methodology is reported in detail elsewhere, together with a descriptive summary of the data on sociodemographic and clinical characteristics, treatment use, and impact of ADHD, reported by country.26 Briefly, the survey of caregivers of children/adolescents diagnosed with ADHD was fielded online between November 2012 and April 2013 in ten European countries – Denmark, Finland, France, Germany, Italy, the Netherlands, Norway, Spain, Sweden, and the UK. Data from Denmark, Finland, and Norway were pooled because of small sample sizes and are referred to as “Other Nordic”. Responses were collected from caregivers of children who were prescribed ADHD medications (including stimulant and nonstimulant medication) at the time of, or within 6 months prior to, completion of the survey.
This analysis of data from the CAPPA survey was designed to evaluate caregivers’ experiences of ADHD diagnosis, BT, and supportive care for children/adolescents with ADHD.
Ethical review
The study was reviewed and approved by a central institutional review board (MaGil IRB, Rockville, MD, USA), and was performed in accordance with the ethical standards of the Declaration of Helsinki (2008).27 Caregivers were asked to provide written informed consent before completing the survey.
Participants
Potential participants were identified from patient panels of individuals (recruited using approaches including social media, and online communities and advertising) who had agreed to be contacted for participation in research studies. Eligible participants were screened using an electronic questionnaire.
Inclusion/exclusion criteria are reported in detail elsewhere.26 Briefly, participants were eligible for inclusion if they were a parent or legal guardian of a child/adolescent aged 6–17 years with a diagnosis of ADHD at least 6 months prior to study enrollment, and if the child/adolescent, at the time of the survey, was currently receiving or had received pharmacotherapy for ADHD in the previous 6 months and did not have a severe intellectual disability (cognitive impairment with intelligence quotient <70). Only one caregiver per child could participate, and the child had to reside with the caregiver for at least 50% of the time during the 6 months immediately prior to the survey.
This analysis excluded caregivers of children/adolescents who used non-ADHD (not specified or “other”) medications.
Data collection
Demographics
Data on demographics (nationality, age, and sex) of the children/adolescents included in these analyses were collected, as well as the following caregiver demographics: sex, caregiver role according to proportion of time the caregiver was in charge of the child (sole, primary, less than primary), marital status (single, married, divorced, widowed), highest educational level (less than A-level or equivalent, A-level or equivalent, university, or greater), work status (employed, unemployed – looking, unemployed – not looking, other), and number of children in caregivers’ household (1, 2, 3+).
Access to diagnosis services
The following variables were summarized from caregiver responses: 1) time (in months) from first noticing symptoms to first doctor visit; 2) time (in months) from first doctor visit to formal ADHD diagnosis; 3) number of doctors seen during the diagnosis process; 4) perceived difficulty obtaining a referral to a specialist; and 5) perceived difficulty obtaining a diagnosis. Responses to both perceived difficulty questions were provided on a five-point Likert scale (a great deal of difficulty, a lot of difficulty, some difficulty, a little difficulty, no difficulty).
BT utilization
Caregivers responded “yes – received BT before medication use”, “yes – received BT after medication use”, or “no BT”.
Caregiver resources
Caregivers were asked whether sufficient resources (such as ADHD education, training, and support groups) were available to help them with their child’s ADHD. Response options were “yes”, “no”, or “don’t know”.
Support from health care providers
Caregivers were asked two questions about their satisfaction with medical care and the support received from their health care provider, with responses on a seven-point Likert scale, as follows: 1) “Overall, how satisfied are you with the quality of medical care for ADHD?” (responses range from “very satisfied” to “very dissatisfied”), and 2) “How supportive are health care providers in helping you manage your child’s ADHD?” (responses range from “very supportive” to “very unsupportive”).
Support from schools
Caregivers were questioned about the type of school the child attended (mainstream school, school for ADHD or special needs, or other [eg, home school or vocational school]). The following questions assessed caregivers’ perceived school support: 1) “Could the school do more to help regarding your children’s ADHD?” (yes/no), and 2) “Did your children receive extra help or special arrangements at school?” (yes/no). For those who received extra help, caregivers were asked for the type of help received. The top three types of extra help (pan-EU) are presented.
Analyses
Pooled (pan-EU) and country-specific descriptive statistics are reported for each of the outcome questions and for the demographic variables. Responses were compared across countries using chi-square tests for categorical variables and analysis of variance F-tests for continuous variables. For time to diagnosis variables, 95% confidence intervals (CIs) for the means are reported. All statistical tests were two-sided with significance predetermined as P<0.05. There was no adjustment for multiple testing.
Results
Patient and caregiver characteristics
From the full analysis set of 3,688 caregivers in the CAPPA survey,26 72 caregivers had children/adolescents who had received non-ADHD medications or had no medication specified, leaving 3,616 caregivers included in this analysis (Table S1); 66% were female and 81% were married/had partners. Of the 3,616 children/adolescents with ADHD, the mean (standard deviation [SD]) age at the time of the survey was 11.5 (3.2) years and 80% were male.
The Netherlands and Sweden had the oldest mean age (12.4 years in both countries) and Italy had the youngest mean age (10.0 years). Significant differences in demographics were found across countries (P<0.001).
Diagnosis
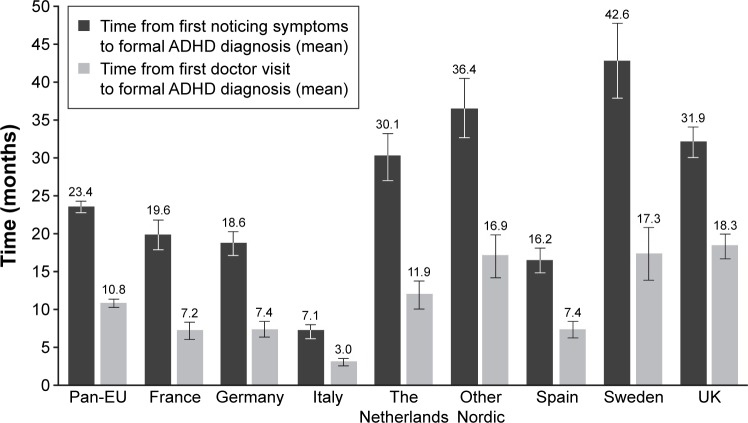
Overall, the mean time from caregivers first noticing symptoms of ADHD to formal ADHD diagnosis was 23.4 (95% CI 22.5, 24.3) months (range: 7.1 months [Italy] to 42.6 months [Sweden]; Figure 1). The mean time from first doctor visit to formal diagnosis was 10.8 (95% CI 10.2, 11.3) months (range: 3.0 months [Italy] to 18.3 months [UK]). The mean (SD) number of different doctors seen during the diagnosis process (Table 1) was 2.5 (1.6), ranging from 2.2 (Sweden) to 2.7 (UK).
Figure 1.
Time to formal diagnosis.
Notes: ANOVA F-test across countries, P<0.001 for both variables. Bars represent 95% confidence intervals.
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; ANOVA, analysis of variance.
Table 1.
Access to diagnosis services
| Pan-EU, N=3,616 |
France, n=477 |
Germany, n=581 |
Italy, n=450 |
The Netherlands, n=309 |
Other Nordic, n=247 |
Spain, n=571 |
Sweden, n=215 |
UK, n=766 |
P-valuea | |
|---|---|---|---|---|---|---|---|---|---|---|
| How many different doctors during the diagnosis process? mean (SD) | 2.5 (1.6) | 2.5 (1.3) | 2.5 (1.3) | 2.4 (1.6) | 2.3 (1.6) | 2.5 (1.3) | 2.5 (1.6) | 2.2 (1.2) | 2.7 (1.9) | <0.001 |
| How much difficulty in getting a referral to a specialist? n (%)b | n=3,103 | n=386 | n=492 | n=391 | n=268 | n=213 | n=501 | n=168 | n=684 | <0.001 |
| A great deal of difficulty | 435 (14) | 64 (17) | 20 (4) | 47 (12) | 23 (9) | 23 (11) | 90 (18) | 23 (14) | 145 (21) | |
| A lot of difficulty | 599 (19) | 141 (37) | 55 (11) | 74 (19) | 34 (13) | 25 (12) | 100 (20) | 42 (25) | 128 (19) | |
| Some difficulty | 744 (24) | 95 (25) | 75 (15) | 139 (36) | 63 (24) | 58 (27) | 109 (22) | 28 (17) | 177 (26) | |
| A little difficulty | 527 (17) | 64 (17) | 48 (10) | 73 (19) | 98 (37) | 35 (16) | 96 (19) | 28 (17) | 85 (12) | |
| No difficulty | 798 (26) | 22 (6) | 294 (60) | 58 (15) | 50 (19) | 72 (34) | 106 (21) | 47 (28) | 149 (22) | |
| How much difficulty in getting an ADHD/ADD diagnosis? n (%) | <0.001 | |||||||||
| A great deal of difficulty | 412 (11) | 54 (11) | 36 (6) | 32 (7) | 28 (9) | 17 (7) | 88 (15) | 23 (11) | 134 (17) | |
| A lot of difficulty | 724 (20) | 153 (32) | 98 (17) | 95 (21) | 37 (12) | 34 (14) | 105 (18) | 46 (21) | 156 (20) | |
| Some difficulty | 999 (28) | 151 (32) | 132 (23) | 168 (37) | 91 (29) | 55 (22) | 164 (29) | 40 (19) | 198 (26) | |
| A little difficulty | 709 (20) | 78 (16) | 108 (19) | 92 (20) | 101 (33) | 47 (19) | 131 (23) | 32 (15) | 120 (16) | |
| No difficulty | 772 (21) | 41 (9) | 207 (36) | 63 (14) | 52 (17) | 94 (38) | 83 (15) | 74 (34) | 158 (21) | |
Notes: Data shown as n (%) unless stated otherwise. Percentages may not total 100% due to rounding.
Calculated using chi-square tests for categorical variables and analysis of variance F-tests for continuous variables.
Only 3,103 of the 3,616 caregivers responded to this question.
Abbreviations: ADD, attention deficit disorder; ADHD, attention-deficit/hyperactivity disorder; SD, standard deviation.
Across the countries, around one-third (33%) of caregivers reported the greatest degrees of difficulty (“a great deal”/“a lot of difficulty”) in obtaining a referral; similarly, 31% reported “a great deal”/“a lot of difficulty” in obtaining a formal ADHD diagnosis (Table 1). The countries with the lowest rates of difficulty (“a great deal”/“a lot”) in obtaining a referral and an ADHD diagnosis were Germany (15% and 23%), the Netherlands (21% and 21%), and Other Nordic (23% and 21%), while the highest rates of difficulty were reported in France (53% and 43%). Significant variation was observed between countries for all of these variables (P<0.001).
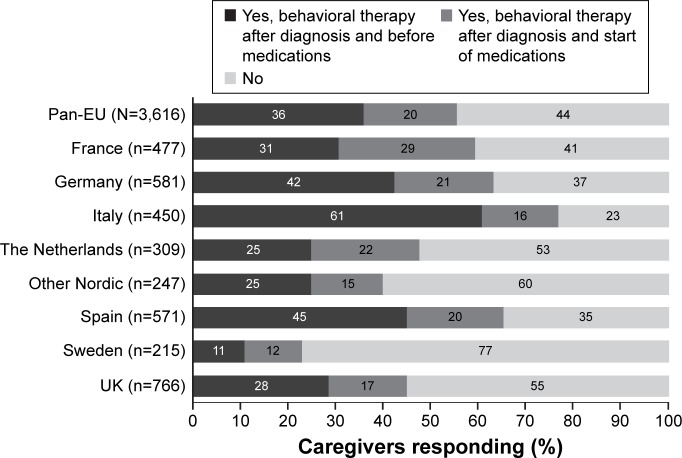
BT utilization
Overall, 44% of children/adolescents had not received BT, while 20% received BT at the time of, or after the start of, ADHD medication (Figure 2).
Figure 2.
Since being diagnosed with ADHD, has your child ever received behavioral therapy?
Notes: P<0.001 across countries (chi-square test). Percentages may not total 100% due to rounding.
Abbreviation: ADHD, attention-deficit/hyperactivity disorder.
Significant between-country variability was observed (P<0.001). The lowest utilization of BT was reported in Sweden (23%) and the highest was in Italy (77%). Sweden and Italy also had the lowest and highest BT utilization prior to starting medication (11% and 61%, respectively).
Caregiver resources
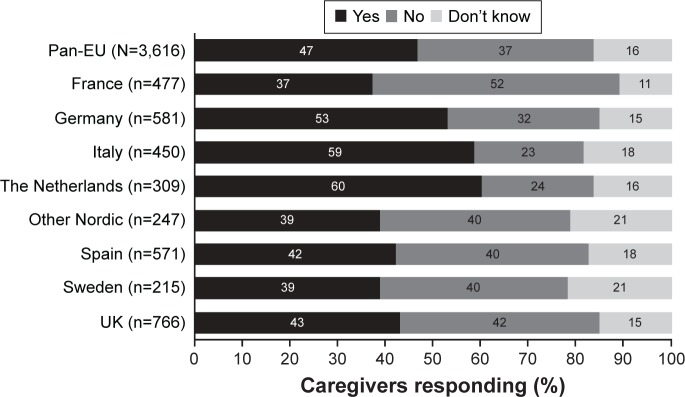
Among the pan-EU sample, 47% of caregivers reported that they had sufficient resources for helping them with their child’s ADHD (Figure 3).
Figure 3.
Do you have sufficient resources (such as ADHD education, training, and support groups) available to help you with your child’s ADHD?
Note: P<0.001 across countries (chi-square test).
Abbreviation: ADHD, attention-deficit/hyperactivity disorder.
The countries with the lowest and highest reporting rates of sufficient resources were France (37%) and the Netherlands (60%), respectively (between-country variability P<0.001).
Supportive care from health care providers
Across all countries, 44% of caregivers reported the greatest degrees of satisfaction (“very satisfied”/“satisfied”) with the quality of medical care (Table 2), and similarly, health care providers were reported to be “very supportive”/“somewhat supportive” by 50% of caregivers. Significant between-country variability was observed (both P<0.001). The lowest and highest rates of being “very satisfied”/“satisfied” with medical care were found in France (35%) and Germany (53%), respectively. The lowest and highest rates of “very supportive”/“somewhat supportive” health care providers were found in Sweden (31%) and Spain (59%), respectively.
Table 2.
Supportive care from health care providers
| Pan-EU, N=3,616 |
France, n=477 |
Germany, n=581 |
Italy, n=450 |
The Netherlands, n=309 |
Other Nordic, n=247 |
Spain, n=571 |
Sweden, n=215 |
UK, n=766 |
P-valuea | |
|---|---|---|---|---|---|---|---|---|---|---|
| Overall, how satisfied are you with the quality of medical care for ADHD? n (%) | <0.001 | |||||||||
| Very satisfied | 504 (14) | 39 (8) 75 (13) | 95 (21) | 27 (9) | 36 (15) | 99 (17) | 33 (15) | 100 (13) | ||
| Satisfied | 1,090 (30) | 129 (27) 234 (40) | 96 (21) | 131 (42) | 56 (23) | 185 (32) | 69 (32) | 190 (25) | ||
| Somewhat satisfied | 989 (27) | 174 (36) 119 (20) | 141 (31) | 69 (22) | 66 (27) | 143 (25) | 40 (19) | 237 (31) | ||
| Neither satisfied nor dissatisfied | 469 (13) | 75 (16) 57 (10) | 68 (15) | 36 (12) | 46 (19) | 56 (10) | 34 (16) | 97 (13) | ||
| Somewhat dissatisfied | 300 (8) | 34 (7) 47 (8) | 29 (6) | 20 (6) | 25 (10) | 54 (9) | 24 (11) | 67 (9) | ||
| Dissatisfied | 156 (4) | 17 (4) 28 (5) | 14 (3) | 17 (6) | 9 (4) | 19 (3) | 10 (5) | 42 (5) | ||
| Very dissatisfied | 108 (3) | 9 (2) 21 (4) | 7 (2) | 9 (3) | 9 (4) | 15 (3) | 5 (2) | 33 (4) | ||
| How supportive are health care providers in helping you manage child’s ADHD? n (%) | <0.001 | |||||||||
| Very supportive | 640 (18) | 63 (13) 112 (19) | 79 (18) | 59 (19) | 35 (14) | 127 (22) | 29 (13) | 136 (18) | ||
| Somewhat supportive | 1,151 (32) | 199 (42) 153 (26) | 164 (36) | 92 (30) | 58 (23) | 212 (37) | 37 (17) | 236 (31) | ||
| A little supportive | 776 (21) | 126 (26) 118 (20) | 90 (20) | 66 (21) | 71 (29) | 100 (18) | 49 (23) | 156 (20) | ||
| Neither supportive nor unsupportive | 553 (15) | 57 (12) 101 (17) | 55 (12) | 55 (18) | 33 (13) | 63 (11) | 76 (35) | 113 (15) | ||
| A little unsupportive | 207 (6) | 14 (3) 45 (8) | 35 (8) | 12 (4) | 20 (8) | 27 (5) | 15 (7) | 39 (5) | ||
| Somewhat unsupportive | 132 (4) | 10 (2) 25 (4) | 17 (4) | 10 (3) | 13 (5) | 13 (2) | 2 (1) | 42 (5) | ||
| Very unsupportive | 157 (4) | 8 (2) 27 (5) | 10 (2) | 15 (5) | 17 (7) | 29 (5) | 7 (3) | 44 (6) | ||
Notes: Data shown as n (%) unless stated otherwise. Percentages may not total 100% due to rounding.
Calculated using chi-square tests.
Abbreviation: ADHD, attention-deficit/hyperactivity disorder.
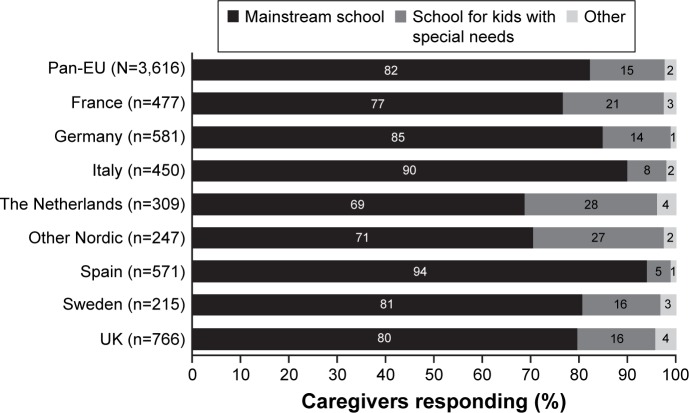
Support from schools
Overall, 82% of children/adolescents attended mainstream schools, 15% attended a school for special needs, and 2% were home-schooled or attended some other type of school (Figure 4). Significant between-country variability was observed (both P<0.001). Attendance of mainstream schools was highest for children with ADHD in Spain (94%) and Italy (90%) and lowest in the Netherlands (69%) and Other Nordic countries (71%). “Other schools” attendance made up <5% of the total across all countries.
Figure 4.
What type of school does your child attend?
Notes: P<0.001 across countries (chi-square test). Percentages may not total 100% due to rounding.
For children who attended mainstream schools, 67% (range: 50% [the Netherlands] to 78% [Spain]) of caregivers thought that the schools could do more to help, while extra help or special arrangements at school were provided for 48% (range: 26% [Germany] to 66% [Sweden]) of children/adolescents (Table 3). In comparison, for children who attended special schools for ADHD, 51% (range: 24% [the Netherlands] to 77% [Italy]) of caregivers thought that schools could do more to help (57% [37% {Germany} to 82% {Sweden}] received extra help or special arrangements at school).
Table 3.
Support from A) mainstream schools and B) special schools for ADHD
| Pan-EU | France | Germany | Italy | The Netherlands | Other Nordic | Spain | Sweden | UK | P-valuea | |
|---|---|---|---|---|---|---|---|---|---|---|
| A) Mainstream school | n=2,980 | n=367 | n=494 | n=407 | n=212 | n=175 | n=539 | n=174 | n=612 | |
| Do you think the school could do more to help regarding your child’s ADHD? Yes, n (%) | 1,996 (67) | 223 (61) | 337 (68) | 289 (71) | 106 (50) | 111 (63) | 420 (78) | 128 (74) | 382 (62) | <0.001 |
| Has your child received extra help or special allowances at school for his/her ADHD? Yes, n (%) | 1,428 (48) | 159 (43) | 126 (26) | 187 (46) | 100 (47) | 99 (57) | 292 (54) | 114 (66) | 351 (57) | <0.001 |
| Did your child receive extra help: extra attention from teacher? Yes, n (%) | 1,091 (76) | 111 (70) | 69 (55) | 164 (88) | 70 (70) | 75 (76) | 210 (72) | 90 (79) | 302 (86) | <0.001 |
| Did your child receive extra help: in-class aide? Yes, n (%) | 782 (55) | 110 (69) | 34 (27) | 102 (55) | 43 (43) | 48 (48) | 133 (46) | 76 (67) | 236 (67) | <0.001 |
| Did your child receive extra help: one-on-one instruction? Yes, n (%) | 750 (53) | 80 (50) | 33 (26) | 94 (50) | 25 (25) | 48 (48) | 149 (51) | 79 (69) | 242 (69) | <0.001 |
| B) Special school for ADHD | n=548 | n=98 | n=82 | n=35 | n=85 | n=66 | n=26 | n=34 | n=122 | |
| Do you think the school could do more to help regarding your child’s ADHD? Yes, n (%) | 279 (51) | 57 (58) | 48 (59) | 27 (77) | 20 (24) | 32 (48) | 19 (73) | 21 (62) | 55 (45) | <0.001 |
| Has your child received extra help or special allowances at school for his/her ADHD? Yes, n (%) | 315 (57) | 53 (54) | 30 (37) | 26 (74) | 41 (48) | 48 (73) | 16 (62) | 28 (82) | 73 (60) | <0.001 |
| Did your child receive extra help: extra attention from teacher? Yes, n (%) | 237 (75) | 28 (53) | 22 (73) | 22 (85) | 27 (66) | 35 (73) | 9 (56) | 27 (96) | 67 (92) | <0.001 |
| Did your child receive extra help: fewer students in class? Yes, n (%) | 226 (72) | 35 (66) | 17 (57) | 11 (42) | 37 (90) | 36 (75) | 11 (69) | 25 (89) | 54 (74) | <0.001 |
| Did your child receive extra help: statement of special needs? Yes, n (%) | 204 (65) | 20 (38) | 20 (67) | 15 (58) | 24 (59) | 37 (77) | 13 (81) | 17 (61) | 58 (79) | <0.001 |
Notes: Data shown as n (%) of caregivers responding “Yes” to the questions.
Calculated using chi-square tests.
Abbreviation: ADHD, attention-deficit/hyperactivity disorder.
The three most common types of extra help received in mainstream schools were extra attention from the teacher (76%), an in-class aide (55%), and one-on-one instruction (53%). In comparison, the three most common forms of extra help received in special ADHD schools were extra attention from the teacher (75%), fewer students in the class (72%), and a statement of special needs (65%). Significant variation was observed between countries in all of these variables (P<0.001).
Discussion
The CAPPA survey outcomes presented here provide insights into caregiver perceptions of the potential difficulty in accessing care, lack of support and dissatisfaction with services provided by school and health care systems, as well as the resources available (sufficient or insufficient) for child/adolescent ADHD. Such difficulties in obtaining the services and information needed may contribute to the caregiver burden and the less than optimal satisfaction with treatment that is commonly reported among caregivers of children/adolescents with ADHD.28,29
Almost a third of caregivers across ten European countries experienced difficulties and delays in obtaining a formal diagnosis for children/adolescents with ADHD. Furthermore, a wide range in time to diagnosis was observed across countries (range 3.0 months [Italy] to 18.3 months [UK]), which may represent differences in local diagnostic pathways, or in the specific model used for the health care system and its efficiency, and suggests there is potential for improvement in some countries relative to others. Both the perceived caregiver difficulty and the number of different doctors seen followed a similar outcome pattern to the time to diagnosis, with considerably fewer caregivers in Italy perceiving “a great deal of difficulty” in getting a diagnosis, compared with the UK. In addition, the UK had the highest mean number of different doctors seen and the largest proportion of caregivers reporting “a great deal of difficulty” in obtaining a referral to see a specialist. This is in line with results from an adjunct to the ADHD Observational Research in Europe (ADORE) survey, which highlighted the deficit in levels of service for ADHD in the UK.12
The UK also differed from other countries as the mean time from observation of symptoms to first doctor visit was shorter than the mean time from first doctor visit to formal ADHD diagnosis, possibly due to the emphasis on primary care in the UK health care system.30 For all other countries, it is interesting to note that the mean time from observing symptoms to the first doctor visit was about two to three times longer than the mean time from the first doctor visit to diagnosis. This time period may be longer because it includes the time taken for caregivers to become comfortable with initiating contact with a health care provider. The time it takes to initiate this contact depends on many factors, such as caregivers’ knowledge of ADHD, and may be affected by cultural differences between countries. For example, Scandinavian countries had the longest mean time from observation of symptoms to diagnosis, particularly in Sweden. These results tally with the findings of a recent qualitative study of caregivers of children/adolescents with ADHD in eight European countries, in which caregivers reported issues with diagnosis, including lack of recognition of ADHD symptoms, lengthy waiting periods before receiving a specialist referral, misdiagnosis, and visits to multiple doctors.4 In a survey of ADHD organizations from 19 European countries (the ADHD-Europe survey), all responding countries expressed some concern in this area, including long waiting times, lack of specialist, and difficulty in ADHD diagnosis due to frequent presence of comorbid conditions.31 The report notes that delays in diagnosis are detrimental to children, as they exacerbate poor educational, behavioral, and psychological outcomes, and cause some caregivers to feel obliged to use private services that are expensive in some countries, to obtain timely intervention. A delay in diagnosis may also increase the risk of depression and low self-esteem in the long term.32
Current European ADHD treatment guidelines recommend that BT should be initiated before prescription medications in all except severe cases of ADHD.16–21 The CAPPA survey found a disconnect between such guidelines and caregiver-reported standard of care with respect to BT; a substantial proportion of children (44%) had not received BT, even though onlŷ25% of caregivers reported their child had severe/very severe ADHD at the time of the survey.26 Our finding of low BT use tallies with the findings from a previous retrospective medical chart review study in six European countries.25 The Multimodal Treatment Study of Children with ADHD showed that BT combined with medication did not have significantly greater benefits on core ADHD symptoms over medication alone.33 Furthermore, results of recent meta-analyses suggest limited efficacy of nonpharmacologic interventions in ADHD;34–37 however, the relevant period of BT use in the present survey would have been prior to 2012, so these findings would not have been available at that time. Elsewhere, a systematic review of meta-analyses of nonpharmacologic treatment for ADHD found positive and significant effect sizes for some child impairment measures,38 and improved long-term outcomes have been reported using nonpharmacologic treatment in combination with medication.39 As such, it is possible that low rates of BT use may contribute to suboptimal treatment outcomes. Additional information on the reasons why children/adolescents did not receive BT is needed to differentiate between those who were not offered BT and those who were offered it but did not adhere to the program. The between-country variability (range 23%–77%) in the use of BT found in our survey is consistent with the substantial variability noted in a small-scale cross-national survey, which included psychiatrists/psychologists from several of the countries included in the CAPPA survey,40 and is also consistent with the between-country variability observed in a previous retrospective medical chart review study in six European countries (range 4.1%–50.7%).25 In our survey, caregivers in Italy, Germany, and Spain reported the highest rates of BT use, possibly reflecting practice and cultural preferences, and good adherence to current ADHD treatment recommendations in these countries.
The findings of the ADHD-Europe survey indicated that networking and communication between parents, teachers, and the treatment provider was often poor, and their training was insufficient.31 Although almost half of caregivers in our survey reported that available caregiver resources were sufficient, more than a third reported that caregiver resources were insufficient. This represents a gap in perceived support; such a lack of resources could affect how well the caregiver copes with the needs of their child/adolescent versus what their country or health care system can provide to help with their child/adolescent’s ADHD. Furthermore, caregivers may not be fully aware of their own resource needs. Indeed, many caregivers responded that they did not know if such resources were sufficient; however, it is not clear from the data whether these caregivers responded in this way because they were unaware of any support, or because they felt no need for support.
A considerable proportion of caregivers in the pan-EU sample described in the ADHD-Europe survey reported dissatisfaction with supportive care from their health care providers. Only about half of the caregivers thought their provider was “very” or “somewhat supportive” in helping them manage their child/adolescent’s ADHD. Caregivers reported being “somewhat dissatisfied”, “dissatisfied”, or “very dissatisfied” with the quality of medical care in 16% of cases, and a further 13% were “neither satisfied nor dissatisfied”. This perception may be due in part to difficulties with the diagnosis process, lack of coordination of care among the various services involved, and insufficient training and continuing education of health care providers.31
The majority (82%) of children/adolescents in our survey attended mainstream schools, but two-thirds of their caregivers perceived that mainstream schools could do more to help and reported that about half of these children had no extra or special arrangements at school for their ADHD. Schools for special needs provided better support than mainstream schools, but the degree of satisfaction ranged widely across countries. These findings are similar to those of an Australian study, which indicated that parents of children with ADHD who were mostly attending mainstream schools perceived that teachers had inadequate understanding, and schools insufficient resources, to support their child’s special needs.41 The Australian study concluded that schools need more resources, and teachers need more training, to promote positive experiences and outcomes for children with ADHD.41 This was also the conclusion of the 2009 ADHD-Europe survey; despite the high likelihood of students with ADHD being in any classroom, most European ADHD organizations said that teachers’ attitudes and knowledge were highly variable and classroom assistance was insufficient.31
Overall, for the outcomes examined, our findings indicated that caregiver-perceived support, quality of care, and care patterns for management of ADHD varied widely across countries. This may potentially reflect differences in availability and cost of diagnosis and treatment, awareness, training of health care professionals and teachers, or allocation of resources between countries;25,40 it may also be due to varying cultural beliefs and attitudes toward ADHD of the caregivers and society at large.
As previously reported,26 the study had a number of limitations that should be taken into account. Although CAPPA was a large, cross-sectional, observational survey, the generalizability of these results remains limited. Participants were recruited through patient panels as a convenience sample, and this may lead to selection bias. It is possible that caregivers who were dissatisfied with care were more likely to participate in the survey, and this may have negatively biased the results. Results may also be subject to reporting and/or recall biases, as the survey was based on the caregiver’s perspective. Diagnosis of ADHD and times of first symptoms, first doctor visit, and formal diagnosis were according to self-report by caregivers and were not confirmed by medical records. The reported information may be influenced by underlying characteristics such as caregivers’ cultural beliefs and knowledge about ADHD. As noted above, between-country variation in caregivers’ perceptions of availability and quality of services may in part be explained by these influences. Another factor that makes these data difficult to interpret is the lack of benchmark data from a cohort of age-matched caregivers to allow a comparison to be made between survey findings and a normative sample and thus help to determine what level should be considered reasonable for each parameter. This survey does, however, provide a valuable source of data from caregivers of patients with ADHD, which can be used as a benchmark for future studies and raise awareness of the issues faced by caregivers of patients with ADHD. Finally, the analysis examined only bivariate associations and, therefore, did not simultaneously control for risk factors and baseline characteristics.
Conclusion
This large cross-sectional survey in ten European countries provided valuable real-world information about caregivers’ perceptions of access to diagnosis and BT, and the quality of support they receive from health care and school systems, for children/adolescents diagnosed with ADHD who were currently receiving or had recently received pharmacotherapy for ADHD. As well as highlighting the wide variation across Europe with respect to availability and quality of child/adolescent ADHD services, responses to the CAPPA survey identified gaps in access to diagnosis and supportive care. These gaps in care may contribute to caregiver burden, and underscore the need for improved access to diagnosis, provision of supportive services, and tighter adherence to established guidelines that may lead to better standards of care. The findings also suggest a continued need for integration of supportive services, with better communication needed between parents, schools, health care providers, and their administrative services. Comprehensive and standardized professional training and guidance for teachers and parents may aid in alleviating the parental burden.
Supplementary materials
Table S1.
Demographics of children/adolescents and their caregivers included in the present analysis
| Pan-EU, N=3,616a |
France, n=477 |
Germany, n=581 |
Italy, n=450 |
The Netherlands, n=309 |
Other Nordic,b n=247 |
Spain, n=571 |
Sweden, n=215 |
UK, n=766 |
P-valuec | |
|---|---|---|---|---|---|---|---|---|---|---|
| Child/adolescent | ||||||||||
| Age, mean (SD) | 11.5 (3.2) | 10.6 (3.0) | 11.9 (2.9) | 10.0 (2.9) | 12.4 (3.1) | 12.1 (3.1) | 11.6 (3.2) | 12.4 (3.1) | 11.6 (3.3) | <0.001 |
| Sex, n (%) | <0.001 | |||||||||
| Male | 2,875 (80) | 400 (84) | 455 (78) | 351 (78) | 231 (75) | 200 (81) | 448 (78) | 151 (70) | 639 (83) | |
| Female | 741 (20) | 77 (16) | 126 (22) | 99 (22) | 78 (25) | 47 (19) | 123 (22) | 64 (30) | 127 (17) | |
| Caregiver | ||||||||||
| Sex, n (%) | <0.001 | |||||||||
| Male | 1,239 (34) | 163 (34) | 193 (33) | 152 (34) | 81 (26) | 107 (43) | 227 (40) | 83 (39) | 233 (30) | |
| Female | 2,377 (66) | 314 (66) | 388 (67) | 298 (66) | 228 (74) | 140 (57) | 344 (60) | 132 (61) | 533 (70) | |
| Married? Yes, n (%) | 2,926 (81) | 403 (84) | 466 (80) | 422 (94) | 236 (76) | 177 (72) | 491 (86) | 156 (73) | 575 (75) | <0.001 |
| Relationship to child, n (%) | <0.001 | |||||||||
| Mother | 2,308 (64) | 305 (64) | 373 (64) | 295 (66) | 222 (72) | 135 (55) | 339 (59) | 131 (61) | 508 (66) | |
| Father | 1,071 (30) | 150 (31) | 157 (27) | 137 (30) | 70 (23) | 92 (37) | 207 (36) | 70 (33) | 188 (25) | |
| Other | 237 (7) | 22 (5) | 51 (9) | 18 (4) | 17 (6) | 20 (8) | 25 (4) | 14 (7) | 70 (9) | |
| Caregiver role, n (%) | <0.001 | |||||||||
| Sole | 787 (22) | 136 (29) | 139 (24) | 81 (18) | 54 (17) | 40 (16) | 70 (12) | 43 (20) | 224 (29) | |
| Primary | 1,218 (34) | 191 (40) | 189 (33) | 189 (42) | 90 (29) | 58 (23) | 169 (30) | 65 (30) | 267 (35) | |
| Less than primary | 1,611 (45) | 150 (31) | 253 (44) | 180 (40) | 165 (53) | 149 (60) | 332 (58) | 107 (50) | 275 (36) | |
| Educational level, n (%) | <0.001 | |||||||||
| Less than A-leveld or equivalent | 1,011 (28) | 69 (14) | 340 (59) | 24 (5) | 53 (17) | 69 (28) | 142 (25) | 20 (9) | 294 (38) | |
| A-leveld or equivalent | 1,170 (32) | 134 (28) | 133 (23) | 138 (31) | 152 (49) | 89 (36) | 172 (30) | 135 (63) | 217 (28) | |
| University or greater | 1,435 (40) | 274 (57) | 108 (19) | 288 (64) | 104 (34) | 89 (36) | 257 (45) | 60 (28) | 255 (33) | |
| Work status, n (%) | <0.001 | |||||||||
| Employed | 2,677 (74) | 374 (78) | 436 (75) | 378 (84) | 209 (68) | 184 (74) | 420 (74) | 164 (76) | 512 (67) | |
| Unemployed – looking | 202 (6) | 23 (5) | 15 (3) | 18 (4) | 28 (9) | 16 (6) | 64 (11) | 17 (8) | 21 (3) | |
| Unemployed – not looking | 717 (20) | 77 (16) | 123 (21) | 54 (12) | 69 (22) | 44 (18) | 84 (15) | 33 (15) | 233 (30) | |
| Other | 20 (1) | 3 (1) | 7 (1) | 0 (0) | 3 (1) | 3 (1) | 3 (1) | 1 (0) | 0 (0) | |
| Number of children, n (%) | <0.001 | |||||||||
| 1 | 1,113 (31) | 132 (28) | 206 (35) | 205 (46) | 36 (12) | 71 (29) | 189 (33) | 61 (28) | 213 (28) | |
| 2 | 1,617 (45) | 212 (44) | 253 (44) | 190 (42) | 170 (55) | 107 (43) | 284 (50) | 91 (42) | 310 (40) | |
| 3+ | 886 (25) | 133 (28) | 122 (21) | 55 (12) | 103 (33) | 69 (28) | 98 (17) | 63 (29) | 243 (32) | |
Notes: Data shown as n (%) unless stated otherwise. Percentages may not total 100% due to rounding.
Excludes ten patients who had no medication specified (Germany n=2, Italy n=5, the Netherlands n=1, Other Nordic n=1, Spain n=1) and 62 patients who only used non-ADHD (“other”) medications (France n=9, Germany n=6, Italy n=13, the Netherlands n=6, Other Nordic n=1, Spain n=2, Sweden n=4, UK n=21).
Pooled data from Denmark, Finland, and Norway.
Calculated using chi-square tests for categorical variables and analysis of variance F-tests for continuous variables.
Secondary school leaving qualification (noncompulsory), generally required for university entrance.
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; SD, standard deviation.
Acknowledgments
The research was funded by Shire Development, LLC. The study was conducted by ICON Clinical Research, Gaithersburg, MD, USA in collaboration with Global Perspectives, Berkshire, UK and Survey Sampling International, Shelton, CT, USA. Data presented here were analyzed by Moshe Fridman. Under the direction of the authors, Joanna Wright DPhil and Hannah Wills MBChB, employees of Caudex, Oxford, UK provided writing assistance for this publication. Editorial assistance in formatting, proofreading, copyediting, and fact checking the manuscript, and coordination and collation of comments was also provided by Caudex. Shire International GmbH provided funding to Caudex, Oxford, UK for support in writing, editing, and managing this manuscript.
Although employees of Shire were involved in the design, collection, analysis, interpretation, and fact checking of information, the content of this manuscript, interpretation of the data, and the decision to submit the manuscript for publication in Neuropsychiatric Disease and Treatment was made by the authors independently.
The authors thank Valerie Harpin of Ryegate Children’s Centre, Sheffield, UK for her contribution to this study.
Footnotes
Disclosures
MF is an employee of AMF Consulting and serves as a paid consultant to Shire. TB has served in an advisory or consultancy role for Hexal Pharma, Lilly, Medice, Novartis, Otsuka, Oxford Outcomes (now ICON), PCM Scientific, Shire, and Vifor Pharma. He is/has been involved in clinical trials conducted by Lilly, Shire, and Vifor Pharma. TB has received conference attendance support and conference support or speaker’s fees from Lilly, Medice, Novartis, and Shire. The present work is unrelated to the above grants and relationships. VS was an employee of, and owned stock/stock options in, Shire at the time of the study. JQ is a speaker or member of an advisory board for FEAADAH, Proyecto DAH, Shire, Grünenthal, and Janssen Pharmaceuticals, and has an unrestricted research grant from Otsuka. KSC is an employee of, and owns stock/stock options in, Shire. The authors have no other conflicts of interest in this work.
References
- 1.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 2.Polanczyk G, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual Research Review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345–365. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 3.Danckaerts M, Sonuga-Barke EJ, Banaschewski T, et al. The quality of life of children with attention deficit/hyperactivity disorder: a systematic review. Eur Child Adolesc Psychiatry. 2010;19(2):83–105. doi: 10.1007/s00787-009-0046-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sikirica V, Flood E, Dietrich CN, et al. Unmet needs associated with attention-deficit/hyperactivity disorder in eight European countries as reported by caregivers and adolescents: results from qualitative research. Patient. 2015;8(3):269–281. doi: 10.1007/s40271-014-0083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riley AW, Coghill D, Forrest CB, Lorenzo MJ, Ralston SJ, Spiel G, ADORE Study Group Validity of the health-related quality of life assessment in the ADORE study: parent report form of the CHIP-child edition. Eur Child Adolesc Psychiatry. 2006;15(Suppl 1):i63–i71. doi: 10.1007/s00787-006-1009-6. [DOI] [PubMed] [Google Scholar]
- 6.Varni JW, Burwinkle TM. The PedsQL as a patient-reported outcome in children and adolescents with Attention-Deficit/Hyperactivity Disorder: a population-based study. Health Qual Life Outcomes. 2006;4:26. doi: 10.1186/1477-7525-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wright N, Moldavsky M, Schneider J, et al. Practitioner review: pathways to care for ADHD – a systematic review of barriers and facilitators. J Child Psychol Psychiatry. 2015;56(6):598–617. doi: 10.1111/jcpp.12398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sayal K, Mills J, White K, Merrell C, Tymms P. Predictors of and barriers to service use for children at risk of ADHD: longitudinal study. Eur Child Adolesc Psychiatry. 2015;24(5):545–552. doi: 10.1007/s00787-014-0606-z. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed R, Borst JM, Yong CW, Aslani P. Do parents of children with attention-deficit/hyperactivity disorder (ADHD) receive adequate information about the disorder and its treatments? a qualitative investigation. Patient Prefer Adherence. 2014;8:661–670. doi: 10.2147/PPA.S60164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sayal K, Ford T, Goodman R. Trends in recognition of and service use for attention-deficit hyperactivity disorder in Britain, 1999–2004. Psychiatr Serv. 2010;61(8):803–810. doi: 10.1176/ps.2010.61.8.803. [DOI] [PubMed] [Google Scholar]
- 11.Dennis T, Davis M, Johnson U, Brooks H, Humbi A. Attention deficit hyperactivity disorder: parents’ and professionals’ perceptions. Community Pract. 2008;81(3):24–28. [PubMed] [Google Scholar]
- 12.Tettenborn M, Prasad S, Poole L, et al. The provision and nature of ADHD services for children/adolescents in the UK: results from a nationwide survey. Clin Child Psychol Psychiatry. 2008;13(2):287–304. doi: 10.1177/1359104507086347. [DOI] [PubMed] [Google Scholar]
- 13.Caci H, Cohen D, Bonnot O, et al. Health care trajectories for children with ADHD in France: results from the QUEST survey. J Atten Disord. 2016 Jan 21; doi: 10.1177/1087054715618790. Epub. [DOI] [PubMed] [Google Scholar]
- 14.Bussing R, Meyer J, Zima BT, Mason DM, Gary FA, Garvan CW. Childhood ADHD symptoms: association with parental social networks and mental health service use during adolescence. Int J Environ Res Public Health. 2015;12(9):11893–11909. doi: 10.3390/ijerph120911893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hinojosa MS, Fernandez-Baca D, Knapp C. Factors associated with family-provider partnership among children with ADHD. Fam Med. 2012;44(7):463–470. [PubMed] [Google Scholar]
- 16.Deutsche Gesellschaft für Kinder- und Jugendpsychiatrie und Psychotherapie . In: Hyperkinetische Störungen (F90). Leitlinien zur Diagnostik und Therapie von psychischen Störungen im Säuglings-, Kindes- und Jugendalter [Guidelines for diagnosis and treatment of mental disorders in infancy, childhood and adolescence] Auflage über-arbeitete., editor. Cologne: Deutsche Ärzte Verlag; 2007. p. 3. German. [Google Scholar]
- 17.Health Ministry of Spain Guía de Práctica Clínica sobre el Trastorno por Déficit de Atención con Hiperactividad (TDAH) en Niños y Adoles-centes [Clinical Practice Guidelines on Attention Deficit Hyperactivity Disorder (ADHD) in Children and Adolescents] [Accessed July 21, 2016]. Available from: http://www.guiasalud.es/GPC/GPC_477_TDAH_AIAQS_compl.pdf. Spanish.
- 18.Landelijke Stuurgroep Multidisciplinaire richtlijn ADHD bij kinderen en jeugdigen; Versie 1.0 [Multidisciplinary guideline for ADHD in children and adolescents; Version 1.0] [Accessed July 21, 2016]. Available from: http://www.ggzrichtlijnen.nl/index.php?pagina=/richtlijn/item/pagina.php&richtlijn_id=29. Dutch.
- 19.NICE Attention deficit hyperactivity disorder: diagnosis and management. 2008. [Accessed July 21, 2016]. (National clinical practice guideline number 72). includes 2016 updates. Available from: https://www.nice.org.uk/guidance/cg72.
- 20.SINPIA Linee-guida per la diagnosi e la terapia farmacologica del Disturbo da Deficit Attentivo con Iperattività (ADHD) in età evolutiva [Guidelines for the diagnosis and pharmacological therapy of attention deficit disorder with hyperactivity (ADHD) in children] [Accessed July 21, 2016]. Available from: http://www.aidaiassociazione.com/documents/Linee_guida_SINPIA_Diagnosi.pdf. Italian.
- 21.Taylor E, Dopfner M, Sergeant J, et al. European clinical guidelines for hyperkinetic disorder – first upgrade. Eur Child Adolesc Psychiatry. 2004;13(Suppl 1):i7–i30. doi: 10.1007/s00787-004-1002-x. [DOI] [PubMed] [Google Scholar]
- 22.Ostberg M, Rydell AM. An efficacy study of a combined parent and teacher management training programme for children with ADHD. Nord J Psychiatry. 2012;66(2):123–130. doi: 10.3109/08039488.2011.641587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pfiffner LJ, Villodas M, Kaiser N, Rooney M, McBurnett K. Educational outcomes of a collaborative school-home behavioral intervention for ADHD. Sch Psychol Q. 2013;28(1):25–36. doi: 10.1037/spq0000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hall CL, Taylor JA, Newell K, Baldwin L, Sayal K, Hollis C. The challenges of implementing ADHD clinical guidelines and research best evidence in routine clinical care settings: Delphi survey and mixed-methods study. BJPsych Open. 2016;2(1):25–31. doi: 10.1192/bjpo.bp.115.002386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Setyawan J, Fridman M, Grebla R, Harpin V, Korst LM, Quintero J. Variation in presentation, diagnosis, and management of children and adolescents with ADHD across European countries. J Atten Disord. 2015 Aug 5; doi: 10.1177/1087054715597410. Epub. [DOI] [PubMed] [Google Scholar]
- 26.Flood E, Gajria K, Sikirica V, et al. The caregiver perspective of paediatric ADHD (CAPPA) survey: understanding sociodemographic and clinical characteristics, treatment use, and impact of ADHD in Europe. J Affect Disord. 2016;200:222–234. doi: 10.1016/j.jad.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 27.World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. [Accessed January 17, 2017]. Available from: http://www.wma.net/en/30publications/10policies/b3/
- 28.Fridman M, Banaschewski T, Sikirica V, Quintero J, Erder MH, Chen K. Factors associated with caregiver burden among pharmacotherapy-treated children/adolescents with ADHD in the Caregiver Perspective on Pediatric ADHD (CAPPA) survey in Europe. Neuropsychiatr Dis Treat. 2017;13:373–386. doi: 10.2147/NDT.S121391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fridman M, Banaschewski T, Sikirica V, Quintero J, Erder MH, Chen K. Caregiver perspective on pediatric attention-deficit/hyperactivity disorder (CAPPA): medication satisfaction and symptom control. Neuropsychiatr Dis Treat. 2017;13:443–455. doi: 10.2147/NDT.S121639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tatlow-Golden M, Prihodova L, Gavin B, Cullen W, McNicholas F. What do general practitioners know about ADHD? attitudes and knowledge among first-contact gatekeepers: systematic narrative review. BMC Fam Pract. 2016;17(1):129. doi: 10.1186/s12875-016-0516-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clark S. Diagnosis and Treatment of AD/HD in Europe: Differences, Problems and Progress. [Accessed July 21, 2016]. Available from: http://www.adhdeurope.eu/images/files/20090513_Survey.pdf.
- 32.Young S, Bramham J, Gray K, Rose E. The experience of receiving a diagnosis and treatment of ADHD in adulthood: a qualitative study of clinically referred patients using interpretative phenomenological analysis. J Atten Disord. 2008;11(4):493–503. doi: 10.1177/1087054707305172. [DOI] [PubMed] [Google Scholar]
- 33.MTA Cooperative Group A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal treatment study of children with ADHD. Arch Gen Psychiatry. 1999;56(12):1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- 34.Cortese S, Ferrin M, Brandeis D, et al. Cognitive training for attention-deficit/hyperactivity disorder: meta-analysis of clinical and neuropsychological outcomes from randomized controlled trials. J Am Acad Child Adolesc Psychiatry. 2015;54(3):164–174. doi: 10.1016/j.jaac.2014.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daley D, Van der Oord S, Ferrin M, et al. Behavioral interventions in attention-deficit/hyperactivity disorder: a meta-analysis of randomized controlled trials across multiple outcome domains. J Am Acad Child Adolesc Psychiatry. 2014;53(8):835–847. doi: 10.1016/j.jaac.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 36.Rapport MD, Orban SA, Kofler MJ, Friedman LM. Do programs designed to train working memory, other executive functions, and attention benefit children with ADHD? a meta-analytic review of cognitive, academic, and behavioral outcomes. Clin Psychol Rev. 2013;33(8):1237–1252. doi: 10.1016/j.cpr.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 37.Sonuga-Barke EJ, Brandeis D, Cortese S, et al. Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. Am J Psychiatry. 2013;170(3):275–289. doi: 10.1176/appi.ajp.2012.12070991. [DOI] [PubMed] [Google Scholar]
- 38.Fabiano GA, Schatz NK, Aloe AM, Chacko A, Chronis-Tuscano A. A systematic review of meta-analyses of psychosocial treatment for attention-deficit/hyperactivity disorder. Clin Child Fam Psychol Rev. 2015;18(1):77–97. doi: 10.1007/s10567-015-0178-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arnold LE, Hodgkins P, Caci H, Kahle J, Young S. Effect of treatment modality on long-term outcomes in attention-deficit/hyperactivity disorder: a systematic review. PLoS One. 2015;10(2):e0116407. doi: 10.1371/journal.pone.0116407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hinshaw SP, Scheffler RM, Fulton BD, et al. International variation in treatment procedures for ADHD: social context and recent trends. Psychiatr Serv. 2011;62(5):459–464. doi: 10.1176/ps.62.5.pss6205_0459. [DOI] [PubMed] [Google Scholar]
- 41.Efron D, Sciberras E, Hassell P. Are schools meeting the needs of students with ADHD? Australasian J Special Educ. 2008;32(2):187–198. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Demographics of children/adolescents and their caregivers included in the present analysis
| Pan-EU, N=3,616a |
France, n=477 |
Germany, n=581 |
Italy, n=450 |
The Netherlands, n=309 |
Other Nordic,b n=247 |
Spain, n=571 |
Sweden, n=215 |
UK, n=766 |
P-valuec | |
|---|---|---|---|---|---|---|---|---|---|---|
| Child/adolescent | ||||||||||
| Age, mean (SD) | 11.5 (3.2) | 10.6 (3.0) | 11.9 (2.9) | 10.0 (2.9) | 12.4 (3.1) | 12.1 (3.1) | 11.6 (3.2) | 12.4 (3.1) | 11.6 (3.3) | <0.001 |
| Sex, n (%) | <0.001 | |||||||||
| Male | 2,875 (80) | 400 (84) | 455 (78) | 351 (78) | 231 (75) | 200 (81) | 448 (78) | 151 (70) | 639 (83) | |
| Female | 741 (20) | 77 (16) | 126 (22) | 99 (22) | 78 (25) | 47 (19) | 123 (22) | 64 (30) | 127 (17) | |
| Caregiver | ||||||||||
| Sex, n (%) | <0.001 | |||||||||
| Male | 1,239 (34) | 163 (34) | 193 (33) | 152 (34) | 81 (26) | 107 (43) | 227 (40) | 83 (39) | 233 (30) | |
| Female | 2,377 (66) | 314 (66) | 388 (67) | 298 (66) | 228 (74) | 140 (57) | 344 (60) | 132 (61) | 533 (70) | |
| Married? Yes, n (%) | 2,926 (81) | 403 (84) | 466 (80) | 422 (94) | 236 (76) | 177 (72) | 491 (86) | 156 (73) | 575 (75) | <0.001 |
| Relationship to child, n (%) | <0.001 | |||||||||
| Mother | 2,308 (64) | 305 (64) | 373 (64) | 295 (66) | 222 (72) | 135 (55) | 339 (59) | 131 (61) | 508 (66) | |
| Father | 1,071 (30) | 150 (31) | 157 (27) | 137 (30) | 70 (23) | 92 (37) | 207 (36) | 70 (33) | 188 (25) | |
| Other | 237 (7) | 22 (5) | 51 (9) | 18 (4) | 17 (6) | 20 (8) | 25 (4) | 14 (7) | 70 (9) | |
| Caregiver role, n (%) | <0.001 | |||||||||
| Sole | 787 (22) | 136 (29) | 139 (24) | 81 (18) | 54 (17) | 40 (16) | 70 (12) | 43 (20) | 224 (29) | |
| Primary | 1,218 (34) | 191 (40) | 189 (33) | 189 (42) | 90 (29) | 58 (23) | 169 (30) | 65 (30) | 267 (35) | |
| Less than primary | 1,611 (45) | 150 (31) | 253 (44) | 180 (40) | 165 (53) | 149 (60) | 332 (58) | 107 (50) | 275 (36) | |
| Educational level, n (%) | <0.001 | |||||||||
| Less than A-leveld or equivalent | 1,011 (28) | 69 (14) | 340 (59) | 24 (5) | 53 (17) | 69 (28) | 142 (25) | 20 (9) | 294 (38) | |
| A-leveld or equivalent | 1,170 (32) | 134 (28) | 133 (23) | 138 (31) | 152 (49) | 89 (36) | 172 (30) | 135 (63) | 217 (28) | |
| University or greater | 1,435 (40) | 274 (57) | 108 (19) | 288 (64) | 104 (34) | 89 (36) | 257 (45) | 60 (28) | 255 (33) | |
| Work status, n (%) | <0.001 | |||||||||
| Employed | 2,677 (74) | 374 (78) | 436 (75) | 378 (84) | 209 (68) | 184 (74) | 420 (74) | 164 (76) | 512 (67) | |
| Unemployed – looking | 202 (6) | 23 (5) | 15 (3) | 18 (4) | 28 (9) | 16 (6) | 64 (11) | 17 (8) | 21 (3) | |
| Unemployed – not looking | 717 (20) | 77 (16) | 123 (21) | 54 (12) | 69 (22) | 44 (18) | 84 (15) | 33 (15) | 233 (30) | |
| Other | 20 (1) | 3 (1) | 7 (1) | 0 (0) | 3 (1) | 3 (1) | 3 (1) | 1 (0) | 0 (0) | |
| Number of children, n (%) | <0.001 | |||||||||
| 1 | 1,113 (31) | 132 (28) | 206 (35) | 205 (46) | 36 (12) | 71 (29) | 189 (33) | 61 (28) | 213 (28) | |
| 2 | 1,617 (45) | 212 (44) | 253 (44) | 190 (42) | 170 (55) | 107 (43) | 284 (50) | 91 (42) | 310 (40) | |
| 3+ | 886 (25) | 133 (28) | 122 (21) | 55 (12) | 103 (33) | 69 (28) | 98 (17) | 63 (29) | 243 (32) | |
Notes: Data shown as n (%) unless stated otherwise. Percentages may not total 100% due to rounding.
Excludes ten patients who had no medication specified (Germany n=2, Italy n=5, the Netherlands n=1, Other Nordic n=1, Spain n=1) and 62 patients who only used non-ADHD (“other”) medications (France n=9, Germany n=6, Italy n=13, the Netherlands n=6, Other Nordic n=1, Spain n=2, Sweden n=4, UK n=21).
Pooled data from Denmark, Finland, and Norway.
Calculated using chi-square tests for categorical variables and analysis of variance F-tests for continuous variables.
Secondary school leaving qualification (noncompulsory), generally required for university entrance.
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; SD, standard deviation.