Abstract
Objective:
To offer an overview of sport-related concussion (SRC) prevention and education strategies in the context of the socioecological framework (SEF). Athletic trainers (ATs) will understand the many factors that interact to influence SRC prevention and the implications of these interactions for effective SRC education.
Background:
Concussion is a complex injury that is challenging to identify and manage, particularly when athletes fail to disclose symptoms to their health care providers. Education is 1 strategy for increasing disclosure. However, limited information addresses how ATs can integrate the many factors that may influence the effectiveness of SRC education into their specific settings. Public health models provide an example through the SEF, which highlights the interplay among various levels of society and sport that can facilitate SRC prevention strategies, including education.
Description:
For ATs to develop appropriate SRC prevention strategies, a framework for application is needed. A growing body of information concerning SRC prevention indicates that knowledge alone is insufficient to change concussion-related behaviors. The SEF allows this information to be considered at levels such as policy and societal, community, interpersonal (relationships), and intrapersonal (athlete). The use of such a framework will facilitate more comprehensive SRC prevention efforts that can be applied in all athletic training practice settings.
Clinical Applications:
Athletic trainers can use this information as they plan SRC prevention strategies in their specific settings. This approach will aid in addressing the layers of complexity that exist when developing a concussion-management policy and plan.
Key Words: mild traumatic brain injuries, policies, public health
Concussion is a complex injury that is challenging to identify and manage, particularly when athletes fail to disclose symptoms of sport-related concussion (SRC) to their health care providers.1 Evidence suggests that more than 50% of concussions are unreported.2,3 This high proportion of unreported SRCs results in a lack of care and increased risk for future injury and long-term neurologic deficits, reducing the individual's quality of life and eventually burdening our health care systems.4,5
Due to the increased general awareness of and concern about SRC, many programmatic and educational efforts (specifically those geared toward coaches, parents, and athletes) have been developed to aid in better prevention, identification, and management. Numerous documents6–10 have been published concerning SRC knowledge and various educational techniques aimed at improving SRC knowledge across many levels of sport. These educational programs have largely been developed and implemented in response to SRC legislation and the policies of various organizations. However, existing educational approaches vary substantially. Important suggestions have been made for considering knowledge-translation principles in order to address the complexity of the multifaceted nature of sport and to increase the effectiveness of SRC educational efforts10,11; yet key studies2,12,13 illustrated that SRC knowledge may not always be the most appropriate outcome for evaluating the efficacy of various legislative, policy, and educational efforts, as increased SRC knowledge does not inevitably translate into the desired or appropriate behaviors.
The multifaceted nature of SRC prevention, identification, and management often makes it difficult for athletic trainers (ATs) to understand what role they should play in this process and which tools or strategies may be most effective for their specific setting. Proper education across many societal levels has the potential to be an important aspect of improving the prevention, identification, and ultimately overall management of SRC. However, this requires a multifaceted approach that includes many factors beyond increasing knowledge.
OVERVIEW OF THE SOCIOECOLOGICAL FRAMEWORK
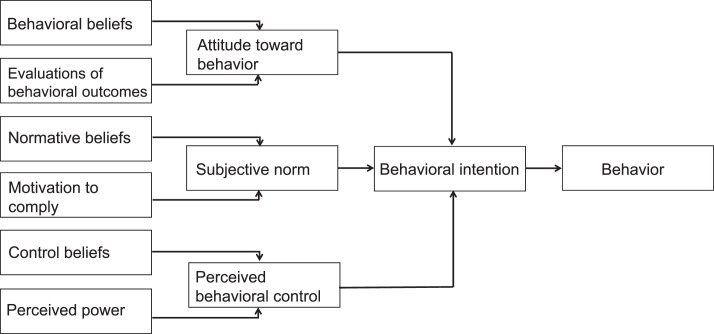
The socioecological framework (SEF)14 is a well-known and commonly used theoretical structure in public health aimed at illustrating and understanding how levels of society interact to influence each other with respect to a given health-related concern.15–21 The model itself is often presented with society and policy at the highest overarching level, followed by the community level (organizational, social, playing environments), and then the interpersonal level (relationships), ending with the intrapersonal level (the athlete; Figure 1). This model is useful for identifying areas in need of intervention concerning SRC. For example, Kerr et al19 highlighted the utility of this model in understanding SRC disclosure. When considering all the layers encapsulated by the SEF, one is able to situate an individual athlete's behaviors or outcomes in more distal influences, such as policy. The SEF is an organizing structure, and at each of its levels, more specific theories can guide our understanding of how factors at that level are interrelated. More specifically, existing literature focused on the interpersonal and intrapersonal levels has frequently included the theory of planned behavior22,23 to better understand these relationships (Figure 2). This theory addresses the relationships among beliefs, attitudes, social influences, perceived control over a behavior, intentions, and the behavior of interest. This model is a useful approach to injury prevention.
Figure 1. .
Socioecological framework.
Figure 2. .
Prevention of sport-related injury is a key domain of athletic training practice. As such, the AT can play a key role in facilitating integrative strategies into prevention initiatives. Prevention efforts should include primary prevention (averting a concussion before it occurs), secondary prevention (reducing the effects a concussion may have), and tertiary prevention (lessening the long-term effects of concussion) efforts. Comprehensive integration of these efforts is best understood in a framework that illustrates the key components and the relationships among important factors. Our purpose is to provide an overview of SRC prevention, with a particular focus on education, in the context of the SEF. The SEF provides ATs with an understanding of how many prevention- and education-related factors at multiple levels function as a system. Secondarily, through the SEF, we will provide an overview of the literature concerning effective educational strategies at each level of the framework.
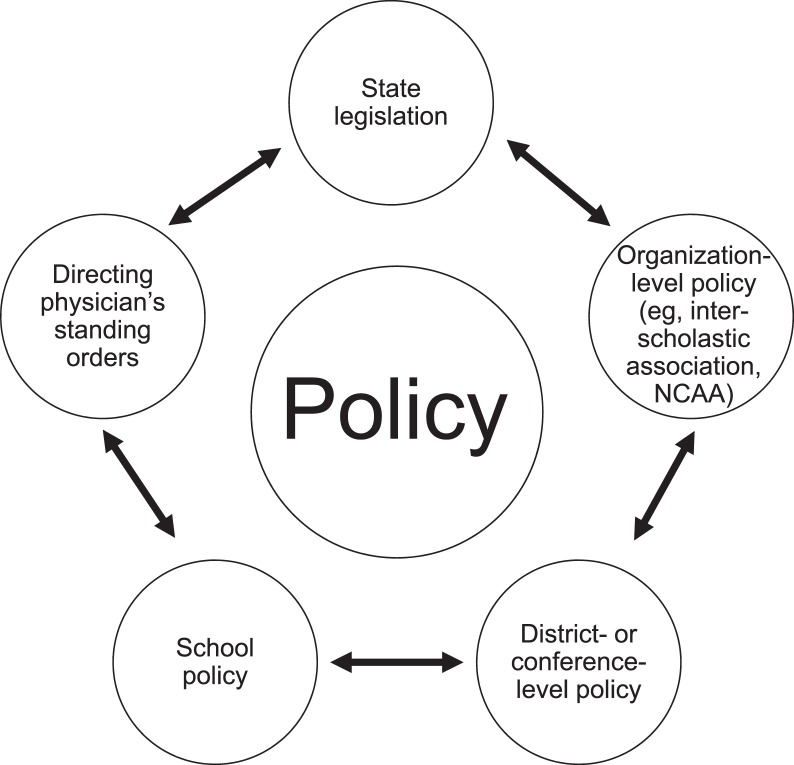
Policy Level
The policy level is housed within the highest (societal) level of the SEF and comprehensively includes all policies and rules regarding SRC, including legislation, league or organizational policies, and school or team policies. In this section, we focus on these domains of policy across different playing environments because not all policy levels affect each environment. Concussion policy in the United States is enacted in multiple domains and at multiple levels of sport competition (Figure 3). The broadest of these categories is state-based concussion legislation. All states and the District of Columbia adopted concussion legislation between 2009 and 2014. Most of the state laws are modeled after the Washington State Lystedt Law and include 3 provisions: (1) preseason concussion education for the coach, athlete, and parents and acknowledgment of its receipt by each party; (2) timely removal from play of any athlete suspected of having sustained an SRC; and (3) clearance from a medical professional before a concussed athlete returns to practice or competition.24 Nearly all state laws apply to high school and middle school students, and most state laws also apply to youth athletes.25
Figure 3. .
Multiple domains and levels of sport policies in the United States. Abbreviation: NCAA, National Collegiate Athletic Association.
Notably, the widely adopted tenets of state concussion legislation represent secondary and tertiary prevention mechanisms. A total of 22 states have amended their concussion laws. For example, 1 state has incorporated primary prevention mechanisms (eg, limiting contact during practices) in its laws.26 Other amendments have expanded the population covered by the laws or clarified existing provisions.26 For example, Alaska stated that ATs had the authority to clear athletes to return to play under the scope of the state's concussion law.26
Several groups have evaluated the implementation and effectiveness of state concussion laws. Lowrey and Morain27 found more successful implementation in states where policymakers worked with stakeholders (eg, individuals in the state's department of public health) whose involvement in implementation aided in accounting for contextual barriers and facilitators. Two groups28,29 found that implementation of the laws, including educational provisions for coaches, was associated with increased SRC knowledge among coaches. However, although coach knowledge increased, SRC education did not improve coaches' recognition of SRC in their athletes.30 Examinations of educational interventions for parents and athletes have also shown limited improvements.28 This may be due to a lack of specificity in the educational mandates, which results in substantial variability in the delivery of SRC education at the state level. In addition, athletes may not keep a copy of the concussion-information sheet, which they must sign and return to acknowledge receipt,25 yet indirect benefits of adopted concussion policy initiatives may exist, such as knowledge transfer through less formalized educational channels, such as media coverage of the policy change. Theoretically, more parents or athletes may consequently recognize potential injuries and report them to appropriate medical providers. Such indirect benefits may explain previous findings31,32 of improved rates of SRC diagnosis in states that have adopted concussion legislation.
At the collegiate level, the National Collegiate Athletic Association (NCAA) put forth its “Concussion Policy and Legislation” in 2010. This set of rules, which is binding on all member schools, is similar to state concussion legislation in requiring annual athlete SRC education and acknowledgment of its receipt, timely removal from play of athletes suspected of having sustained an SRC, and clearance by a physician or physician's designee before the concussed athlete returns to play. More recently, the NCAA33 has put forth a series of best practices endorsed by many stakeholder sports organizations. These include primary prevention strategies such as recommended limits on full-contact practices in football.34
Examinations of the NCAA policy have demonstrated mixed results with respect to policy implementation. Four years after the policy was enacted, most (but not all) member schools had a concussion-management plan in place.35 The NCAA is now working to ensure that all member institutions have protocols in place through review teams and verification processes, beginning with the Power 5 conference schools. However, recent evidence35 suggests that school concussion-management plans do not always incorporate all of the required components of the NCAA policy. Even when the required elements are present, variations in implementation may result in failure to adequately achieve the intended goal of protecting student-athletes' health. For example, an examination of SRC education provided to NCAA athletes showed wide variations in both the content and mode of delivery and limited overall effectiveness in changing safety-related cognitions.36 Clinical management practices at the collegiate level seem to be relatively more consistent with NCAA guidance. Kelly et al37 noted that clinical SRC management practices at NCAA Division I schools were often in line with recommended best practices. Buckley et al38 cited similar findings in a sample of NCAA Division II and III schools. Another group39 observed that more than 90% of schools surveyed had provided annual concussion education to student-athletes, had return-to-play policies, and monitored the number of previous concussions sustained by incoming student-athletes. However, only 63% had return-to-learn policies, and only 40% followed all of the recommended components of preparticipation examinations (largely due to a lack of balance testing).
It is important to note that, across all levels, policies represent the minimum acceptable standard. Individual schools, districts, conferences, or sports can implement procedures that go above and beyond the general requirements of the higher-level policy. Preliminary evidence indicates that this is occurring in some cases. For example, in a number of states, the SRC education plan created by the state high school athletic association exceeded the minimum expectations outlined in the state concussion legislation.25 Additionally, some conferences within the NCAA have implemented their own restrictions, such as limiting contact practices in sports (eg, football).40 Sport-specific rules have also been implemented as a means of prevention. For instance, in NCAA football, the kickoff position was moved forward to decrease the incidence of high-velocity return plays that may place athletes at risk of head injury and increase the incidence of touchbacks.41 The National Football League also made changes to the kickoff rule: the kickoff line was moved from the 30-yard line to the 35-yard line, and all players on the kickoff team except the kicker must line up no more than 5 yards behind the kickoff line.42 Ruestow et al42 reported a decrease in the injury incidence from kickoff plays after implementation of this rule, although the decrease was not significant when the kickoff was returned. In addition, reductions in the number of catastrophic injuries after rule changes, such as prohibiting spearing and the horse-collar tackle, further support the importance of sport-specific rules in decreasing injuries.43
In ice hockey, players participating in leagues where body checking was not allowed had decreases in overall injury and concussion risk compared with players in leagues that permitted body checking.44 However, in a subsequent study,45 the overall rate of injuries that resulted in 7 or more days of time loss was increased among individuals who were introduced to body checking at the Bantam (older) level versus the Pee Wee (younger) level. Authors of another study46 of body checking observed no change in overall injuries or neurotraumatic injuries such as concussion when body checking was introduced at a younger age level (Atom) compared with an older age level (Pee Wee). More recently, Black et al47 also noted a 3-fold reduction in concussion risk among Pee Wee players in leagues that did not permit body checking compared with those leagues that did permit body checking. Although reducing head impacts among younger athletes is a primary method of reducing exposures related to concussion, consideration of unintended consequences and increased injuries at higher levels is necessary when implementing developmental programming to introduce and teach skills such as body checking.
Of late, it has been asserted that sports leagues and policy makers have a moral duty to ensure that concussion policies are, in fact, having a positive effect in reducing the health burden of SRC,48 yet more research is needed to evaluate the effectiveness of concussion policies at all levels and examine whether these policies have any unintended consequences. Moreover, although numerous authors have found certain policies to be associated with reductions in injury incidence, numerous other policies must be evaluated through research studies, particularly those enacted recently, such as the elimination of heading in youth soccer players aged 10 years and under. Policy implementation and effectiveness research should consider the interaction between the policy and the other levels within the SEF.
Policy at all levels may also be influenced by the directions and positions of national and professional organizations such as the National Athletic Trainers' Association, the American Academy of Pediatrics, and the American College of Sports Medicine. These organizations develop position statements, task-force recommendations, and consensus documents that often drive best practices related to concussion. Education on these policies and the positions of these organizations is necessary so that all stakeholders involved in a sport setting, including administrators, coaches, parents, and athletes, understand the policies and their role in ensuring compliance with the policies. These statements and recommendations may also influence knowledge of and attitudes about concussion in sport. Athletic trainers are key agents in this process, as they are often well positioned to influence policy, disseminate policy-related information, and educate those in their settings. As such, ATs can advocate for and volunteer to serve on stakeholder boards that advise policy, become active in legislative efforts locally and nationally, educate other stakeholders about needed policy changes and implementation of current policies, and inform their specific organizations and athletic teams about the guidelines and mandates of the given policies. Athletic trainers are also often well positioned to collaborate on evaluation studies about the effect of the policies, both positive and negative, in their settings.
Community Level
Community has been defined as “a group of people with diverse characteristics who are linked by social ties, share common perspectives, and engage in joint action in geographical locations or settings.”49 We can conceptualize community as an organization, team, or school. This section will focus on the priorities and practices of organizations, with an understanding that these are often linked to policy and interpersonal considerations. These linked social ties commonly form key components in the perceptions of the culture of sport, as community perceptions may drive team behaviors.
One primary community-level consideration is whether or not a medical professional is present in a given athletic environment.50–53 Schools at the NCAA level are required to have an AT and team physician, but this is not a requirement at the secondary school level. Authors of a recent study54 characterized the athletic training services available in public secondary schools. Although 70% of schools indicated that athletic training services were available, a full-time AT was on staff at only 37% of their schools.54 It should be noted that having an AT on staff is not the same as having an AT onsite during games or practices. Increased access to or the presence of an AT is likely an important direct environmental modifier of injury, including SRC.
Few researchers have directly examined how staffing influences prevention, exposure, and injury outcomes. One study,55 published only as an abstract, compared injury rates among female soccer and basketball players at secondary schools with or without an AT; at schools with ATs, overall injury rates were reduced, but more SRCs were diagnosed. In another investigation,56 ATs who were full-time secondary school employees reported a higher overall football injury rate and a higher average number of athletic training services per injury in football players than did outreach ATs. However, limited evidence addresses the role of the medical professional's presence in influencing concussion rates and player behaviors, and more work is needed in this area. The medical professional serves as an appropriate authority to whom an athlete can report a potential SRC. Onsite ATs may see more collisions that require a full evaluation, leading to more concussion diagnoses. The presence of ATs may also influence reporting indirectly by helping to foster a trusting patient-provider relationship that results in athletes feeling more comfortable seeking care for suspected injuries. Consequently, there may be an increased emphasis on concussion safety and the importance of reporting suspected injuries.
The physical playing environment for a given school or team, including safety equipment, playing surface, and physical surroundings, may also have a role in SRC prevention and injury outcomes. Helmets are the most discussed piece of concussion-related protective equipment, and they reduce the risk of moderate to severe brain injury in cycling.57 However, the literature is not clear on their ability to prevent concussion in contact-sport athletes.58 Ongoing research is targeting the development of helmet materials that may reduce the concussion risk.59 Although mouthguards and other protective equipment may help reduce some injuries (eg, orofacial injuries), findings related to the role of protective equipment in preventing SRC are mixed. In general, the perception of safety afforded by protective equipment exceeds the actual reduction in SRC risk; it has been argued that this phenomenon—the technological imperative—is a prevailing, albeit misleading, way of framing the risk of SRC from contact sports and possible prevention strategies.60 Athletic equipment may indirectly influence concussive injuries, particularly when athletes are driven by false beliefs regarding the safety afforded by such equipment, which may lead to more aggressive or dangerous playing styles. Few authors have examined this phenomenon, and more research is needed. The playing surface may also be associated with concussion incidence. Contact with artificial turf surfaces may result in more severe concussive injuries than those sustained on natural grass,61,62 yet findings are limited. One study61 was underpowered to examine statistical significance; the other62 was an experiment using accelerometers that did not include human participants. Future researchers must better examine the risk associated with playing-surface type.
An additional contributor to the community and other levels of the SEF is the media. Messaging outlined and promoted by the media may shape and influence organizational structure, as well as community relationships and links. The media may also shape policy and the knowledge, attitudes, and behaviors of teammates and individuals. However, current concepts, policies, and community-level decisions may influence the media, too. No investigators to date have studied the role of the media in concussion-related behaviors. Even so, ATs should be aware of the current messaging and media packaging to appropriately answer questions, provide education, and help the media understand evidence-based findings concerning concussion.
For the benefit of the community and the environment, ATs should create a culture of safety, such as ensuring proper equipment fit and condition, reinforcing safe play, and following all rules. Education will help parents, athletes, coaches, and medical professionals better understand the importance and, in some cases, the modifiability of environmental influences on SRC.
Interpersonal Level
The interpersonal level encompasses the interactions that athletes have with others in their lives. These interactions can play important roles in preventing harm from SRC through both direct and indirect pathways and often form the basis of perceived norms regarding concussion. The theory of planned behavior (Figure 2), as mentioned previously, provides a framework for understanding these relationships and pathways in the context of concussion-related behaviors. Most existing literature28,63–65 has focused on parents, coaches, and teammates, as these stakeholders tend to be the most involved in an athlete's decision making and the overall response to SRC. However, relevant interpersonal dynamics could also include those between the athlete and other authority figures, such as medical providers or administrators, or between nonathlete stakeholders, such as coaches and parents.
Coaches can influence primary, secondary, and tertiary prevention of harm from SRC. Their direct influence on primary prevention involves controlling athletes' exposure to situations that carry an elevated risk of brain trauma by restricting contact during practices and by the style of team play they reinforce. Recent studies66–69 of biomechanical impact data support these potential prevention metrics by highlighting the effects of practice structure and current head-impact biomechanics in various settings. Some football leagues have instituted polices that restrict the frequency with which contact practices can be conducted.70 However, coaches must choose to adhere to these guidelines. Critically, in sports such as ice hockey that have no policy-level guidelines on contact, coaches play an even more central role in making contact-related practice decisions. Education for coaches on SRC may influence contact-related coaching decisions. At the youth football level, the Heads Up Football educational program includes SRC education for coaches and restrictions on contact in practices. Athletes on teams that implemented this safety program sustained fewer injuries and impacts in practice than athletes on teams that did not implement this program.71,72 Still, the extent to which coach education influenced this outcome above and beyond the policy-level restrictions on contact in practice is not clear. Strengthening our understanding of how coach education affects contact-related decisions is an important direction for future research.
Coaches can also play a central role in the secondary prevention of harm from SRC through both direct and indirect pathways. According to the National Athletic Trainers' Association, even with an AT present, coaches have the responsibility to recognize the signs and symptoms of SRC.73 Critically, not all teams have a medical professional on the sidelines of games and practices. In these scenarios, coaches play an even more important role in ensuring that athletes with a possible SRC are removed from participation until they have been evaluated by an appropriate medical professional. Several studies provide preliminary evidence suggesting that exposure to SRC education may influence coaches' identification of athletes who have sustained an SRC. However, these evaluation studies had methodologic limitations, including examining only coach-described behavioral changes in the absence of randomization or a control group74,75 or measuring coaches' cognitions about identification of behavior rather than the behavior itself.76 Stronger evaluation studies of existing educational programming for coaches are needed to understand the extent to which exposure to these programs is associated with coaches' identification and removal from play of athletes with suspected SRC.
Coaches can also indirectly influence early identification. Because many symptoms of SRC are not easily or immediately observable, early identification and removal from play of symptomatic athletes is often contingent on athlete self-report. Athletes who believe that their coach does not want them to report symptoms of a suspected SRC77 and athletes who have experienced pressure from coaches to continue playing while experiencing the symptoms of a possible concussion78 are less likely to seek medical attention. Coaches' communication to athletes about the extent to which SRC reporting is a valued behavior is thus a critical element in changing these perceptions. Increasing coaches' communications in support of reporting is not simply a function of ensuring that coaches are sufficiently knowledgeable about SRCs. In fact, evidence from collegiate coaches suggests that those who have greater SRC knowledge are not more likely to communicate with athletes in support of SRC safety.79 Understanding the coach-level factors that predict support of reporting is an important direction for future research and can inform the development of effective coach education to encourage this behavior. Athletic trainers should discuss the importance of supportive communication with coaches.
Teammates, too, play an important role in the early identification of SRC. Perceived team norms are an important determinant of whether an athlete reports a suspected concussion.80,81 Norms are shaped by observations of and interactions with members of the referent population.82 Within large teams may be smaller subgroups with their own norms regarding concussion; for example, differences were noted among collegiate football players across positions.83 Communication among teammates that explicitly supports concussion reporting has the potential to shape safer perceived norms; however, to date, no concussion education has focused on the role of the uninjured teammate in preventing harm from SRC. Kroshus et al84 suggested the potential relevance of a bystander model for concussion education, in which teammates are engaged in a prosocial (voluntary behavior intended to benefit another) and reporting-supportive role. Engaging teammates as prosocial bystanders may increase early identification of SRC by shaping safer team norms, which in turn would be expected to make athletes more likely to report. Such an approach also has the potential to increase SRC identification directly, to the extent that teammates choose to alert a team coach or medical personnel if the injured athlete is not seeking care.
Although interactions with coaches and teammates occur regularly in the sport setting, the role of parents must also be considered, particularly with respect to younger players. Parents play a direct role in controlling exposure to cumulative impacts, such as deciding the age at which children are first enrolled in a contact or collision sport such as football or ice hockey. Once a child is participating in a given contact or collision sport, the influence of parents in preventing harm from SRC becomes increasingly indirect. When present at sport games or interacting with their children postgame, parents are another set of eyes to help identify whether an athlete should seek medical evaluation for a possible SRC. Parental education about SRC may support this identification process; however, limited evidence63,65,85 indicates whether greater SRC knowledge necessarily translates into more accurate SRC identification among parents. Prospective research on behavioral outcomes is necessary to determine the components of effective education for parents to support them in identifying SRCs and seeking medical care for their children if necessary.
In addition, parents can influence SRC identification indirectly even into young adulthood. College students who perceived pressure from their parents to continue playing while experiencing the symptoms of an SRC were less likely to report a suspected future SRC.64 Understanding how this pressure is communicated between parents and athletes and how the nature of this communication changes by sport context and athlete age is an important direction for future investigation. For example, Kroshus et al64 suggested that pressure from some parents may not be communicated directly but that athletes internalize the investment parents have made and infer parental reporting preferences.64 If this pathway is accurate, parents may be unaware that they are indirectly, and potentially unintentionally, influencing unsafe SRC-reporting behaviors. Understanding more about the influence of pressure or support from parents on athletes is necessary for the design of appropriate parent-focused education.
Intrapersonal Level
The intrapersonal level focuses on the individual athlete, the individual characteristics that influence his or her behavior, and the role that education can play in modifying the individual athlete's behavior. A frequently used theoretical approach to understanding how these individual-level factors relate to behavior is the theory of planned behavior (Figure 2). A critical individual behavior is disclosure of, or seeking care for, his or her concussive injury. Other relevant behaviors could include any behavior related to risk taking, such as playing technique, following the rules of the game, and playing with good sportsmanship. All of these behaviors may be influenced by education at the athlete level or at other levels of the framework.78,86 As discussed in previous sections, athlete-level factors (personal knowledge, attitudes, normative perceptions, behaviors) are influenced by aspects of other levels of the SEF. A number of other individual-level factors have the potential to influence athletes' behaviors regarding SRC. For example, athletes deal with a range of interpersonal pressures related to concussion disclosure.64 Each person's resilience and ability to respond to those pressures may modify the way in which these interpersonal influences are manifested in attitudes, norms, and ultimately behaviors.
Most literature focused on athletes includes the assessment of knowledge levels and the effectiveness of various educational methods in changing knowledge. Knowledge components include awareness of factors that will aid in recognizing and responding to concussion, such as signs and symptoms, steps to take after the injury, and potential consequences of the injury. Results of these studies2,6,87 tend to suggest that athletes have a moderate level of knowledge, with some gaps concerning the signs and symptoms of SRC. Furthermore, although some educational programs have been effective in increasing knowledge among athletes,7,88 others have shown little to no effectiveness and potential negative effects on measures such as normative perceptions of concussion-related behaviors.9 Critically, it is not evident that changes in knowledge will necessarily lead to changes in relevant concussion safety-related behaviors.
Other cognitions, such as attitudes about concussion disclosure, may be more relevant than knowledge for understanding why athletes do or do not engage in healthy concussion-related behaviors. Attitudes encompass what an individual believes about a certain (target) behavior, such as the belief that SRC is a serious injury2 or that disclosing SRC symptoms to a coach or medical professional is difficult and may harm his or her current or future athletic career. These beliefs may also be modified by previous experience with an SRC, both personally and from observation.89 Attitudes among athletes have been examined in a small number of studies.2,13,90 These findings suggest that attitude may be more strongly related to concussion-related behaviors and intentions than to knowledge.
Another critical athlete cognition is perceived norms. In the SRC context, perceived norms reflect what an athlete thinks important people in his or her environment would do with respect to concussion reporting. Athletes who more strongly believe that their teammates or most athletes would report the symptoms of a suspected concussion are more likely to engage in this behavior themselves.81 Athletic identity interacts with perceived norms to influence SRC-disclosure behavior; athletes who more strongly identify with the athlete role are more likely to behave in the way that they think most athletes would regarding SRC disclosure.80 However, critically, norms may be misperceived. The results of a recent investigation81 suggest that both male and female collegiate athletes tend to think their teammates have less safe attitudes about concussion safety than they themselves do. Correcting these misperceptions may be a central strategy for increasing the effectiveness of concussion education; potential approaches to norm-correcting concussion education have been described elsewhere.81
Another component of effective educational interventions is athletes' perceived control of concussion-related behaviors, such as disclosure and playing technique, as well as their self-efficacy regarding these behaviors. Perceived control of concussion behaviors may include an athlete feeling that he or she can control playing behavior; the related term self-efficacy refers to an individual's belief that he or she possesses the skills or means necessary to control those behaviors or actions.89–93 These factors have been suggested to be strongly associated with individuals pursuing specific health behaviors.90–93 Despite the known importance of these factors in a public health model, few educational interventions have addressed either factor. However, these factors should be considered when educating athletes about SRC recognition and response. Well-established approaches to increasing behavioral self-efficacy include providing opportunities for observational learning and mastery experiences94; incorporating these approaches in concussion education may be an important strategy for increasing educational efficacy that ATs can use.
Appropriate SRC education for athletes should be developed in conjunction with interventions at the other levels of the SEF to set the stage for the transfer and sustainability of the information and skills that are integrated at the athlete level. Recent literature supports a framework that includes relevant messaging, including the athletes' needs and preferences,95 and the means to support the transfer of information to reach all levels of the SEF.10
CONCLUSIONS
Athletic trainers are in a unique position as they often interact regularly with individuals and constructs at all levels of the SEF. As such, they are key stakeholders in supporting the need for policy enforcement and educating those involved about the mandates and implementation of such policies. Athletic trainers can be influential in creating a safer social and playing environment by providing an ongoing medical professional presence and implementing the appropriate plans and procedures to enhance this environment. They also have the knowledge and training to educate coaches, parents, and athletes about appropriate SRC recognition and response and best practices73 for managing SRC (Table). The approach to SRC prevention should be multifactorial and encompass more than simply providing an education sheet and a video for athletes and coaches. Measures of the effectiveness of concussion policies and programs should extend beyond knowledge to intention, behaviors, and injury outcomes. In sum, it is critical that ATs consider the levels of the SEF as they develop concussion-related policies, procedures, and educational strategies for their various settings.
Table.
Strategies for Athletic Trainers (AT) to Address Concussion Prevention and Education at Each Level of the Socioecological Framework
| Framework Level |
Strategies |
Example |
| Society and policy | Understand state law and work to educate other stakeholders about the law27 Understand state interscholastic association or National Collegiate Athletic Association policy and work with administrators to ensure their policy meets any requirements34 Develop good relationship and sound concussion policy with directing physician72 Communicate regularly with directing physician Support and conduct research on policy effectiveness | AT works with directing physician, school administrators, and risk-management personnel to develop concussion plan based on best practices, taking into account any specifics from interscholastic association policy and state law to ensure compliance AT educates appropriate stakeholders about policy and law to meet any requirements for education and informed consent |
| Community | Ensure AT and medical-provider presence at games and practices54,55 Implement and practice organization's concussion safety and policy measures72 Promote communication about concussion and positive messaging to other stakeholders63,78 Facilitate use of appropriate equipment and playing surfaces57 | AT works with other health care providers and school administrators to determine event coverage, practice of emergency action plan, equipment fitting, etc |
| Interpersonal | Educate coaches and parents63,89 on appropriate recognition and response to concussion Help foster supportive communication between coaches and athletes about concussion safety63,78 Encourage teammates in concussion safety and concussion disclosure83 | During preseason, AT holds parent-team meetings to educate about concussion, review appropriate policies, and discuss postinjury management scenarios AT provides postinjury anticipatory guidance to patients and families throughout recovery course |
| Intrapersonal | Educate athletes and provide opportunities for experiential and observational learning93 Address attitudes about concussion disclosure13,89 Encourage and support concussion disclosure63 Correct misperceived concussion-related norms79,80 Educate athletes about appropriate sport skills aimed at keeping head out of play and following rules43 | Ensure that concussion education being provided to athletes has been evaluated and demonstrated effectiveness in changing at least knowledge but ideally other relevant factors (eg, attitudes, norms, and reporting intention) Remind athletes about importance of concussion safety throughout season |
REFERENCES
- 1. McCrory P, Meeuwisse WH, Aubry M, et al. . Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013; 47 5: 250– 258. [DOI] [PubMed] [Google Scholar]
- 2. Register-Mihalik JK, Guskiewicz KM, McLeod TC, Linnan LA, Mueller FO, Marshall SW. . Knowledge, attitude, and concussion-reporting behaviors among high school athletes: a preliminary study. J Athl Train. 2013; 48 5: 645– 653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. . Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004; 14 1: 13– 17. [DOI] [PubMed] [Google Scholar]
- 4. Moran LM, Taylor HG, Rusin J, et al. . Quality of life in pediatric mild traumatic brain injury and its relationship to postconcussive symptoms. J Pediatr Psychol. 2012; 37 7: 736– 744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McLeod TC, Bay C, Snyder AR. . Self-reported history of concussion affects health-related quality of life in adolescent athletes. Athl Train Sports Healthc. 2010; 2 4: 219– 226. [Google Scholar]
- 6. Echlin PS, Johnson AM, Riverin S, et al. . A prospective study of concussion education in 2 junior ice hockey teams: implications for sports concussion education. Neurosurg Focus. 2010; 29 5: E6. [DOI] [PubMed] [Google Scholar]
- 7. Bagley AF, Daneshvar DH, Schanker BD, et al. . Effectiveness of the SLICE program for youth concussion education. Clin J Sport Med. 2012; 22 5: 385– 389. [DOI] [PubMed] [Google Scholar]
- 8. Bramley H, Patrick K, Lehman E, Silvis M. . High school soccer players with concussion education are more likely to notify their coach of a suspected concussion. Clin Pediatr (Phila). 2012; 51 4: 332– 336. [DOI] [PubMed] [Google Scholar]
- 9. Kroshus E, Baugh CM, Hawrilenko M, Daneshvar DH. . Pilot randomized evaluation of publically available concussion education materials: evidence of a possible negative effect. Health Educ Behav. 2015; 42 2: 153– 162. [DOI] [PubMed] [Google Scholar]
- 10. Caron JG, Bloom GA, Falcao WR, Sweet SN. . An examination of concussion education programmes: a scoping review methodology. Inj Prev. 2015; 21 5: 301– 308. [DOI] [PubMed] [Google Scholar]
- 11. Provvidenza CF, Johnston KM. . Knowledge transfer principles as applied to sport concussion education. Br J Sports Med. 2009; 43 suppl 1: i68– i75. [DOI] [PubMed] [Google Scholar]
- 12. Kroshus E, Baugh CM, Daneshvar DH, Nowinski CJ, Cantu RC. . Concussion reporting intention: a valuable metric for predicting reporting behavior and evaluating concussion education. Clin J Sport Med. 2015; 25 3: 243– 247. [DOI] [PubMed] [Google Scholar]
- 13. Kroshus E, Baugh CM, Daneshvar DH, Viswanath K. . Understanding concussion reporting using a model based on the theory of planned behavior. J Adolesc Health. 2014; 54 3: 269– 274. [DOI] [PubMed] [Google Scholar]
- 14. Stokols D. . Establishing and maintaining healthy environments: toward a social ecology of health promotion. Am Psychol. 1992; 47 1: 6– 22. [DOI] [PubMed] [Google Scholar]
- 15. Wiese-Bjornstal DM, Smith AM, Shaffer SM, Morrey MA. . An integrated model of response to sport injury: psychological and sociological dynamics. J Appl Sport Psychol. 1998; 10 1: 46– 69. [Google Scholar]
- 16. Hughes R. . A socioecological analysis of the determinants of national public health nutrition work force capacity: Australia as a case study. Fam Community Health. 2006; 29 1: 55– 67. [DOI] [PubMed] [Google Scholar]
- 17. English KC, Fairbanks J, Finster CE, Rafelito A, Luna J, Kennedy M. . A socioecological approach to improving mammography rates in a tribal community. Health Educ Behav. 2008; 35 3: 396– 409. [DOI] [PubMed] [Google Scholar]
- 18. Levin Martin S, Moeti R, Pullen-Seufert N. Implementing safe routes to school: application for the socioecological model and issues to consider. Health Promot Pract. 2009; 10 4: 606– 614. [DOI] [PubMed] [Google Scholar]
- 19. Kerr ZY, Register-Mihalik JK, Marshall SW, Evenson KR, Mihalik JP, Guskiewicz KM. . Disclosure and non-disclosure of concussion and concussion symptoms in athletes: review and application of the socio-ecological framework. Brain Inj. 2014; 28 8: 1009– 1021. [DOI] [PubMed] [Google Scholar]
- 20. Gielen AC, Sleet D. . Application of behavior-change theories and methods to injury prevention. Epidemiol Rev. 2003; 25: 65– 76. [DOI] [PubMed] [Google Scholar]
- 21. Trifiletti LB, Gielen AC, Sleet DA, Hopkins K. . Behavioral and social sciences theories and models: are they used in unintentional injury prevention research? Health Educ Res. 2005; 20 3: 298– 307. [DOI] [PubMed] [Google Scholar]
- 22. Ajzen I. . Theories of cognitive self-regulation: the theory of planned behavior. Organ Behav Hum Decis Process. 1991; 50 2: 179– 211. [Google Scholar]
- 23. Glanz K, Rimer BK, Lewis FM, . Health Behavior and Health Education: Theory, Research and Practice. 3rd ed. San Francisco, CA: Jossey-Bass; 2002: 67– 98. [Google Scholar]
- 24. Harvey HH. . Reducing traumatic brain injuries in youth sports: youth sports traumatic brain injury state laws, January 2009–December 2012. Am J Public Health. 2013; 103 7: 1249– 1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Baugh CM, Kroshus E, Bourlas AP, Perry KI. . Requiring athletes to acknowledge receipt of concussion-related information and responsibility to report symptoms: a study of the prevalence, variation, and possible improvements. J Law Med Ethics. 2014; 42 3: 297– 313. [DOI] [PubMed] [Google Scholar]
- 26. Lowrey K. . State laws addressing youth sports-related traumatic brain injury and the future of concussion law and policy. J Bus Technol Law. 2015; 10 1: 61– 72. [Google Scholar]
- 27. Lowrey KM, Morain SR. . State experiences implementing youth sports concussion laws: challenges, successes, and lessons for evaluating impact. J Law Med Ethics. 2014; 42 3: 290– 296. [DOI] [PubMed] [Google Scholar]
- 28. Chrisman SP, Schiff MA, Chung SK, Herring SA, Rivara FP. . Implementation of concussion legislation and extent of concussion education for athletes, parents, and coaches in Washington State. Am J Sports Med. 2014; 42 5: 1190– 1196. [DOI] [PubMed] [Google Scholar]
- 29. Shenouda C, Hendrickson P, Davenport K, Barber J, Bell KR. . The effects of concussion legislation one year later–what have we learned: a descriptive pilot survey of youth soccer player associates. PM R. 2012; 4 6: 427– 435. [DOI] [PubMed] [Google Scholar]
- 30. Rivara FP, Schiff MA, Chrisman SP, Chung SK, Ellenbogen RG, Herring SA. . The effect of coach education on reporting of concussions among high school athletes after passage of a concussion law. Am J Sports Med. 2014; 42 5: 1197– 1203. [DOI] [PubMed] [Google Scholar]
- 31. Gibson TB, Herring SA, Kutcher JS, Broglio SP. . Analyzing the effect of state legislation on health care utilization for children with concussion. JAMA Pediatr. 2015; 169 2: 163– 168. [DOI] [PubMed] [Google Scholar]
- 32. Bompadre V, Jinguji TM, Yanez ND, et al. . Washington State's Lystedt law in concussion documentation in Seattle public high schools. J Athl Train. 2014; 49 4: 486– 492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. National Collegiate Athletic Association. Guideline 21: sports related concussion. : 2013–2014 NCAA Sports Medicine Handbook. Indianapolis, IN: National Collegiate Athletic Association; 2013. [Google Scholar]
- 34. Concussion guidelines: diagnosis and management of sports-related concussion. National Collegiate Athletic Association Web site. http://www.ncaa.org/health-and-safety/concussion-guidelines. Accessed May 15, 2015. [Google Scholar]
- 35. Baugh CM, Kroshus E, Daneshvar DH, Filali NA, Hiscox MJ, Glantz LH. . Concussion management in United States college sports compliance with National Collegiate Athletic Association concussion policy and areas for improvement. Am J Sports Med. 2015; 43 1: 47– 56. [DOI] [PubMed] [Google Scholar]
- 36. Kroshus E, Daneshvar DH, Baugh CM, Nowinski CJ, Cantu RC. . NCAA concussion education in ice hockey: an ineffective mandate. Br J Sports Med. 2014; 48 2: 135– 140. [DOI] [PubMed] [Google Scholar]
- 37. Kelly KC, Jordan EM, Joyner AB, Burdette GT, Buckley TA. . National Collegiate Athletic Association Division I athletic trainers' concussion-management practice patterns. J Athl Train. 2014; 49 5: 665– 673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Buckley TA, Burdette G, Kelly K. . Concussion-management practice patterns of National Collegiate Athletic Association Division II and III athletic trainers: how the other half lives. J Athl Train. 2015; 50 8: 879– 888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kerr ZY, Snook EM, Lynall RC, Dompier TP, Sales L, Parsons JT. . Concussion-related protocols and preparticipation assessments utilized for incoming student-athletes in National Collegiate Athletic Association member institutions. J Athl Train. 2015; 50 11: 1174– 1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ivy League Ad Hoc Concussion Committee. Report regarding the Ivy League review of concussions in football. Ivy League Sports Web site. http://www.ivyleaguesports.com/sports/fball/2011-12/releases/Football_Concussion_Report-July_2011.pdf. Accessed October 23, 2015. [Google Scholar]
- 41. Changes approved for 2012 football season. National Collegiate Athletic Association Web site. http://www.ncaa.com/news/football/article/2012-02-24/changes-approved-2012-season. Accessed June 15, 2015. [Google Scholar]
- 42. Ruestow PS, Duke TJ, Finley BL, Pierce JS. . Effects of the NFL's Amendments to the Free Kick Rule on Injuries during the 2010 and 2011 seasons. J Occup Environ Hyg. 2015; 12 12: 875– 882. [DOI] [PubMed] [Google Scholar]
- 43. Cantu RC, Mueller FO. . Fatalities and catastrophic injuries in high school and college sports, 1982–1997 lessons for improving safety. Phys Sportsmed. 1999; 27 8: 35– 48. [DOI] [PubMed] [Google Scholar]
- 44. Emery CA, Kang J, Shrier I, et al. . Risk of injury associated with body checking among youth ice hockey players. JAMA. 2010; 303 22: 2265– 2272. [DOI] [PubMed] [Google Scholar]
- 45. Emery C, Kang J, Shrier I, et al. . Risk of injury associated with bodychecking experience among youth hockey players. CMAJ. 2011; 183 11: 1249– 1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kukaswadia A, Warsh J, Mihalik JP, Pickett W. . Effects of changing body-checking rules on rates of injury in minor hockey. Pediatrics. 2010; 125 4: 735– 741. [DOI] [PubMed] [Google Scholar]
- 47. Black AM, Macpherson AK, Hagel BE, et al. . Policy change eliminating body checking in non-elite ice hockey leads to a threefold reduction in injury and concussion risk in 11- and 12-year-old players. Br J Sports Med. 2016; 50 1: 55– 61. [DOI] [PubMed] [Google Scholar]
- 48. Lowrey KM, Morain SR, Baugh CM. . Do ethics demand evaluations of public health laws? Shifting scientific sands and the case of youth sports-related traumatic brain injury laws. J Health Care Law Policy. 2016; 19 1: 99– 117. [PMC free article] [PubMed] [Google Scholar]
- 49. MacQueen KM, McLellan E, Metzger DS, et al. . What is community? An evidence-based definition for participatory public health. Am J Public Health. 2001; 91 12: 1929– 1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Adams WM, Mazerolle SM, Casa DJ, Huggins RA, Burton L. . The secondary school football coach's relationship with the athletic trainer and perspectives on exertional heat stroke. J Athl Train. 2014; 49 4: 469– 477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lynall RC, Laudner KG, Mihalik JP, Stanek JM. . Concussion-assessment and -management techniques used by athletic trainers. J Athl Train. 2013; 48 6: 844– 850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Miller MD. . Team physicians to appreciate what a certified athletic trainer expects and understands in order to work together as a team to optimize the care of athletes: foreword. Clin Sports Med. 2010; 29(1):xi. [DOI] [PubMed] [Google Scholar]
- 53. Yang J, Schaefer JT, Zhang N, Covassin T, Ding K, Heiden E. . Social support from the athletic trainer and symptoms of depression and anxiety at return to play. J Athl Train. 2014; 49 6: 773– 779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pryor RR, Casa DJ, Vandermark LW, et al. . Athletic training services in public secondary schools: a benchmark study. J Athl Train. 2015; 50 2: 156– 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Corlette JD, La Bella CR, Collins CL, Henke NM, Fields SK, Comstock RD. . A comparative analysis of injury rates and patterns among girls' soccer and basketball players at schools with and without athletic trainers from 2006/07–2008/09 [abstract]. Clin J Sport Med. 2013; 23 2: 149. [Google Scholar]
- 56. Kerr ZY, Lynall R, Mauntel TC, Dompier TP. . High school football injury rates and services by athletic trainer employment status. J Athl Train. 2016; 51 1: 70– 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dagher JH, Costa C, Lamoureux J, de Guise E, Feyz M. . Comparative outcomes of traumatic brain injury from biking accidents with or without helmet use. Can J Neurol Sci. 2016; 43 1: 56– 64. [DOI] [PubMed] [Google Scholar]
- 58. Daneshvar DH, Baugh CM, Nowinski CJ, McKee AC, Stern RA, Cantu RC. . Helmets and mouth guards: the role of personal equipment in preventing sport-related concussions. Clin Sports Med. 2011; 30 1: 145– 163, x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hoshizaki TB, Post A, Oeur RA, Brien SE. . Current and future concepts in helmet and sports injury prevention. Neurosurgery. 2014; 75 suppl 4: S136– S148. [DOI] [PubMed] [Google Scholar]
- 60. Bachynski KE, Goldberg DS. . Youth sports & public health: framing risks of mild traumatic brain injury in American football and ice hockey. J Law Med Ethics. 2014; 42 3: 323– 333. [DOI] [PubMed] [Google Scholar]
- 61. Guskiewicz KM, Weaver NL, Padua DA, Garrett WE Jr. . Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000; 28 5: 643– 650. [DOI] [PubMed] [Google Scholar]
- 62. Naunheim R, McGurren M, Standeven J, Fucetola R, Lauryssen C, Deibert E. . Does the use of artificial turf contribute to head injuries? J Trauma. 2002; 53 4: 691– 694. [DOI] [PubMed] [Google Scholar]
- 63. Lin AC, Salzman GA, Bachman SL, et al. . Assessment of parental knowledge and attitudes toward pediatric sports-related concussions. Sports Health. 2015; 7 2: 124– 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kroshus E, Garnett B, Hawrilenko M, Baugh CM, Calzo JP. . Concussion under-reporting and pressure from coaches, teammates, fans, and parents. Soc Sci Med. 2015; 134: 66– 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Gourley MM, . Valovich McLeod TC, Bay RC. Awareness and recognition of concussion by youth athletes and their parents. Athl Train Sports Health. 2010; 2 5: 205– 218. [Google Scholar]
- 66. Cobb BR, Urban JE, Davenport EM, et al. . Head impact exposure in youth football: elementary school ages 9–12 years and the effect of practice structure. Ann Biomed Eng. 2013; 41 12: 2463– 2473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Broglio SP, Martini D, Kasper L, Eckner JT, Kutcher JS. . Estimation of head impact exposure in high school football: implications for regulating contact practices. Am J Sports Med. 2013; 41 12: 2877– 2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Daniel RW, Rowson S, Duma SM. . Head acceleration measurements in middle school football. Biomed Sci Instrum. 2014; 50: 291– 296. [PubMed] [Google Scholar]
- 69. Reed N, Taha T, Keightley M, et al. . Measurement of head impacts in youth ice hockey players. Int J Sports Med. 2010; 31 11: 826– 833. [DOI] [PubMed] [Google Scholar]
- 70. Football practice guidelines. National Collegiate Athletic Association Web site. http://www.ncaa.org/health-and-safety/football-practice-guidelines. Accessed October 2015. [Google Scholar]
- 71. Kerr ZY, Yeargin S, Valovich McLeod TC, et al. . Comprehensive coach education and practice contact restriction guidelines result in lower injury rates in youth American football. Orthop J Sports Med. 2015; 3 7: 2325967115594578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Kerr ZY, Yeargin SW, . Valovich McLeod TC, Mensch J, Hayden R, Dompier TP. Comprehensive coach education reduces head impact exposure in American youth football. Orthop J Sports Med. 2015; 3 10: 2325967115610545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Broglio SP, Cantu RC, Gioia GA, et al. . National Athletic Trainers' Association position statement: management of sport concussion. J Athl Train. 2014; 49 2: 245– 265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Sarmiento K, Mitchko J, Klein C, Wong S. . Evaluation of the Centers for Disease Control and Prevention's concussion initiative for high school coaches: “Heads Up: concussion in high school sports.” J Sch Health. 2010; 80 3: 112– 118. [DOI] [PubMed] [Google Scholar]
- 75. Covassin T, Elbin RJ, Sarmiento K. . Educating coaches about concussion in sports: evaluation of the CDC's “Heads Up: Concussion in Youth Sports” initiative. J Sch Health. 2012; 82 5: 233– 238. [DOI] [PubMed] [Google Scholar]
- 76. Glang A, Koester MC, Beaver SV, Clay JE, McLaughlin KA. . Online training in sports concussion for youth sports coaches. Int J Sports Sci Coach. 2010; 5 1: 1– 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Chrisman SP, Quitiquit C, Rivara FP. . Qualitative study of barriers to concussive symptom reporting in high school athletics. J Adolesc Health. 2013; 52 3: 330– 335.e3. [DOI] [PubMed] [Google Scholar]
- 78. Baugh CM, Kroshus E, Daneshvar DH, Stern RA. . Perceived coach support and concussion symptom-reporting: differences between freshmen and non-freshmen college football players. J Law Med Ethics. 2014; 42 3: 314– 322. [DOI] [PubMed] [Google Scholar]
- 79. Kroshus E, Baugh CM, Hawrilenko MJ, Daneshvar DH. . Determinants of coach communication about concussion safety in US collegiate sport. Ann Behav Med. 2015; 49 4: 532– 541. [DOI] [PubMed] [Google Scholar]
- 80. Kroshus E, Kubzansky LD, Goldman RE, Austin SB. . Norms, athletic identity, and concussion symptom under-reporting among male collegiate ice hockey players: a prospective cohort study. Ann Behav Med. 2015; 49 1: 95– 103. [DOI] [PubMed] [Google Scholar]
- 81. Kroshus E, Garnett BR, Baugh CM, Calzo JP. . Social norms theory and concussion education. Health Educ Res. 2015; 30 6: 1004– 1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Festinger L. . A Theory of Cognitive Dissonance. Stanford, CA: Stanford University Press; 1957. [Google Scholar]
- 83. Baugh CM, Kiernan PT, Kroshus E, et al. . Frequency of head-impact–related outcomes by position in NCAA Division I collegiate football players. J Neurotrauma. 2014; 32 5: 314– 326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Kroshus E, Garnett BR, Baugh CM, Calzo JP. . Engaging teammates in the promotion of concussion help seeking. Health Educ Behav. 2016; 43 4: 442– 451. [DOI] [PubMed] [Google Scholar]
- 85. Coghlin CJ, Myles BD, Howitt SD. . The ability of parents to accurately report concussion occurrence in their bantam-aged minor hockey league children. J Can Chiropr Assoc. 2009; 53 4: 233– 250. [PMC free article] [PubMed] [Google Scholar]
- 86. Malinauskas R. . College athletes' perceptions of social support provided by their coach before injury and after it. J Sports Med Phys Fit. 2008; 48 1: 107– 112. [PubMed] [Google Scholar]
- 87. Sye G, Sullivan SJ, McCrory P. . High school rugby players' understanding of concussion and return to play guidelines. Br J Sports Med. 2006; 40 12: 1003– 1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Glang AE, Koester MC, Chesnutt JC, et al. . The effectiveness of a web-based resource in improving postconcussion management in high schools. J Adolesc Health. 2015; 56 1: 91– 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Register-Mihalik JK, Linnan LA, Marshall SW, McLeod TC, Mueller FO, Guskiewicz K. . Influence of previous concussion history on knowledge, attitude, and reporting of concussion in high school athletes: a preliminary analysis [abstract]. J Athl Train. 2010; 45 suppl 3: S-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Register-Mihalik JK, Linnan LA, Marshall SW, . Valovich McLeod TC, Mueller FO, Guskiewicz KM. Using theory to understand high school aged athletes' intentions to report sport-related concussion: implications for concussion education initiatives. Brain Inj. 2013; 27 7–8: 878– 886. [DOI] [PubMed] [Google Scholar]
- 91. AbuSabha R, Achterberg C. . Review of self-efficacy and locus of control for nutrition- and health-related behavior. J Am Diet Assoc. 1997; 97 10: 1122– 1132. [DOI] [PubMed] [Google Scholar]
- 92. Bandura A. . Self-Efficacy: The Exercise of Control. New York, NY: W. H. Freeman; 1997. [Google Scholar]
- 93. Steese S, Dollette M, Phillips W, Hossfeld E, Matthews G, Taormina G. . Understanding Girls' Circle as an intervention on perceived social support, body image, self-efficacy, locus of control, and self-esteem. Adolescence. 2006; 41 161: 55– 74. [PubMed] [Google Scholar]
- 94. Bandura A. . Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 95. Kroshus E, Baugh CM. . Concussion education in U.S. collegiate sport: what is happening and what do athletes want? Health Educ Behav. 2016; 43 2: 182– 190. [DOI] [PMC free article] [PubMed] [Google Scholar]