Abstract
Objective:
To systematically review the literature regarding rest and return to activity after sport-related concussion.
Data Sources:
The search was conducted in the Cochrane Central Register of Controlled Trials, CINAHL, SPORTDiscus, Educational Resources Information Center, Ovid MEDLINE, and PubMed using terms related to concussion, mild traumatic brain injury, physical and cognitive rest, and return to activity.
Study Selection:
Studies were included if they were published in English; were original research; and evaluated the use of, compliance with, or effectiveness of physical or cognitive rest or provided empirical evidence supporting the graded return-to-activity progression.
Data Extraction:
The study design, patient or participant sample, interventions used, outcome measures, main results, and conclusions were extracted, as appropriate, from each article.
Data Synthesis:
Articles were categorized into groups based on their ability to address one of the primary clinical questions of interest: use of rest, rest effectiveness, compliance with recommendations, or outcome after graded return-to-activity progression. A qualitative synthesis of the results was provided, along with summary tables.
Conclusions:
Our main findings suggest that rest is underused by health care providers, recommendations for rest are broad and not specific to individual patients, an initial period of moderate physical and cognitive rest (eg, limited physical activity and light mental activity) may improve outcomes during the acute postinjury phase, significant variability in the use of assessment tools and compliance with recommended return-to-activity guidelines exists, and additional research is needed to empirically evaluate the effectiveness of graded return-to-activity progressions. Furthermore, there is a significant need to translate knowledge of best practices in concussion management to primary care providers.
Key Words: return to play, cognitive rest, physical rest, academic adjustments, graded return-to-play progression, concussion guideline, return to learn, return to think
Key Points
An initial period of physical and cognitive rest in the early postinjury phase is likely beneficial in the recovery process, but the patient should be monitored closely and recommendations adjusted as symptoms resolve.
Significant variability is present among health care providers in the use of cognitive rest, concussion-assessment tools, and compliance with return-to-activity guidelines.
Educational efforts focusing on translating best-practice knowledge to primary care health care providers are needed to reduce variability and ensure that adequate rest is prescribed in the days immediately after a concussion.
Concussion is one of the most difficult athletic injuries to diagnose and manage. Because of the lack of a gold standard for diagnosis and variations in clinical presentation, influence of modifying factors, and course of recovery, an individualized approach to management has been advocated.1—7 Although an individualized approach to concussion management has been proposed, most position and consensus statements regarding concussion provide recommendations for both physical and cognitive rest, which may include academic adjustments (Table 1).1—7 However these guidelines do not provide information on the timing, duration, type, or other specifics related to physical and cognitive rest.
Table 1. .
Current Consensus and Position Statement Recommendations Regarding Returning to School and Activity Continued on Next Page
| Statement |
Return to School |
Return to Activity |
| American Academy of Pediatrics2 (2010) | Athletes with concussion should rest, both physically and cognitively, until symptoms have resolved at rest and with exertion.Teachers and school administrators should work with students to modify workloads to avoid exacerbating symptoms. | Pediatric and adolescent athletes should never RTP while symptomatic at rest or with exertion.Athletes should not RTP on same day of concussion, even if they become asymptomatic.Recovery course is longer for younger athletes than for collegiate and professional athletes, and a more conservative approach to RTP is warranted. |
| American Medical Society for Sports Medicine7 (2013) | Students will require cognitive rest and may require academic accommodations, such as reduced workload and extended time for tests, while recovering from concussion. | There is no same-day RTP for an athlete diagnosed with a concussion.Concussion symptoms should be resolved before returning to exercise.An RTP progression involves a gradual, stepwise increase in physical demands, sport-specific activities, and the risk of contact.If symptoms occur with activity, the progression should be halted and restarted at the preceding symptom-free step.After concussion, RTP should occur only with medical clearance from a licensed health care provider trained in evaluating and managing concussions. |
| American Academy of Pediatrics1 (2013) | Students with a concussion may need academic adjustments in school to help minimize a worsening of symptoms.Team approach consisting of medical team, school team, and family team is ideal in helping students return to learning.Education of all people involved with students who sustain concussion is necessary to provide adequate adjustments, accommodations, and long-term program modifications for students. | Students should be performing at their academic baseline before returning to sports, full physical activity, or other extracurricular activities after a concussion. |
| International Consensus Conference on Concussion in Sport4 (2013) | A sensible approach involves gradual return to school and social activities (before contact sports) in a manner that does not result in a significant exacerbation of symptoms.Concept of cognitive rest was highlighted with special reference to child's need to limit exertion with activities of daily living that may exacerbate symptoms.School attendance and activities may need to be modified to avoid exacerbating symptoms. | No RTP should occur on day of concussive injury.Cornerstone of concussion management is physical and cognitive rest until acute symptoms resolve, and then graded program of exertion should be followed before medical clearance and RTP.No return to sport or activity should occur before child or adolescent athlete has managed to return to school successfully.The RTP protocol after a concussion follows a stepwise process. |
| American Academy of Neurology3 (2013) | None | Team personnel should not permit athlete to RTP until assessment by experienced licensed health care provider with training in diagnosis and management of concussion and in recognition of more severe traumatic brain injury.To diminish risk of recurrent injury, persons supervising athletes should prohibit athlete with concussion from RTP (contact-risk activity) until licensed health care provider has judged that concussion has resolved.Licensed health care providers might develop individualized graded plans for return to physical and cognitive activity, guided by a carefully monitored, clinically based approach to minimize exacerbation of early postconcussive impairments. |
| National Association of School Nurses6 (2013) | As student returns to school after concussion, school nurse has significant role in supporting student.School nurse collaborates with parents, school staff, special service providers, health care professionals, and student in providing accommodations as student transitions back to school. | Children with diagnosed concussions require significant cognitive rest and graduated reentry plan to preconcussion activities as determined by licensed health care provider. |
| National Athletic Trainers' Association5 (2014) | Athletic trainers should work with school administrators and teachers to include appropriate academic accommodations in concussion-management plan. | Athlete with concussion should not return to athletic participation on day of injury.No athlete with concussion should return to physical activity without being evaluated and cleared by physician or designate (eg, athletic trainer) specifically trained and experienced in concussion evaluation and management.Physical-exertion progression should begin only after athlete demonstrates normal clinical examination, resolution of concussion-related symptoms, and return to preinjury scores on tests of motor control and neurocognitive function. |
Abbreviation: RTP, return to play.
The rationale for recommending cognitive and physical rest after a sport-related concussion includes reducing the potential for a repeat concussion while the brain may still be vulnerable from the initial concussion,8,9 preventing second-impact syndrome in younger patients,10,11 and facilitating recovery by reducing the stresses to the brain that may hinder restoration of normal neurotransmission and neurometabolic function.12,13 Theoretically, the rationale provided is sensible and offers a conservative management plan for clinicians to follow; yet some question whether rest is the best strategy after concussion.12 Furthermore, some evidence14,15 suggests that active treatment strategies may be beneficial to patients during the recovery process, specifically athletes, who are used to being active and are motivated to return to participation.
The motivation of a concussed athlete to return to competition is one reason the decision regarding return to activity is among the most challenging aspects of clinical concussion management. Currently, no validated, objective measures are available to diagnose concussion and to subsequently determine when true recovery has occurred. The return-to-play progression that has been advocated by most major organizations includes waiting until the patient is asymptomatic and has returned to baseline on adjunct assessments.2—5,7 This is followed by a gradual return-to-play progression that systematically challenges the cardiovascular and nervous systems in preparation for a full return to play. Symptoms are monitored at every step to ensure that the patient remains asymptomatic and has recovered from the concussion before being released to full activity.
Of concern for clinicians is the current lack of evidence to support the recommendations in the various position and consensus statements regarding rest after concussion or the effectiveness of the graded return-to-play progression. Therefore, the purpose of this article was to systematically review the literature and answer the following clinical questions regarding rest and return to activity:
-
1.
How often are physical and cognitive rest, including academic adjustments, used by health care providers in managing sport-related concussion?
-
2.
In patients with a concussion, does the use of physical and cognitive rest reduce the severity and duration of concussion-related impairments?
-
3.
How compliant are health care providers in following current return-to-activity guidelines?
-
4.
How effective are the graded return-to-activity protocols in improving patient outcomes after concussion?
METHODS
This systematic review was completed in accordance with the guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).16
Data Sources and Searches
An electronic search was conducted in 6 databases: the Cochrane Central Register of Controlled Trials, CINAHL, SPORTDiscus, Educational Resources Information Center, Ovid MEDLINE, and PubMed. The search terms were brain concussion AND academic accommodations, brain concussion AND cognitive rest, brain concussion AND rest, concuss* AND sports AND academic, concuss* AND sports AND rest, concuss* AND sports AND return to learn, concuss* AND sports AND return to play, mild traumatic brain injury AND rest, mild traumatic brain injury AND cognitive rest, mild traumatic brain injury AND return to activity, mild traumatic brain injury AND return to play, recurrent concussion AND sport (Table 2). We also performed hand searches for relevant articles from the reference lists of relevant papers. All searches were conducted from the date of inception of each database through October 7, 2015.
Table 2. .
Search Terms, Databases, and Number of Articles Identified
| Search Terms |
Cochrane Central Register of Controlled Trials |
CINAHL |
SPORTDiscus |
Educational Resources Information Center |
Ovid MEDLINE |
PubMed |
Total |
| brain concussion AND academic accommodations | 0 | 6 | 3 | 0 | 6 | 10 | 25 |
| brain concussion AND cognitive rest | 1 | 12 | 14 | 0 | 10 | 69 | 106 |
| brain concussion AND rest | 0 | 47 | 39 | 0 | 10 | 134 | 230 |
| concuss* AND sports AND academic | 1 | 49 | 47 | 7 | 2 | 50 | 156 |
| concuss* AND sports AND rest | 5 | 0 | 50 | 2 | 2 | 92 | 151 |
| concuss* AND return to activity | 2 | 15 | 14 | 0 | 28 | 88 | 147 |
| concuss* AND sports AND return to learn | 0 | 3 | 3 | 0 | 1 | 31 | 38 |
| concuss* AND sport AND return to play | 9 | 137 | 200 | 7 | 10 | 337 | 700 |
| mild traumatic brain injury AND rest | 4 | 12 | 9 | 0 | 10 | 417 | 452 |
| mild traumatic brain injury AND cognitive rest | 1 | 1 | 6 | 0 | 11 | 100 | 119 |
| mild traumatic brain injury AND return to activity | 2 | 16 | 12 | 0 | 16 | 164 | 210 |
| mild traumatic brain injury AND return to play | 3 | 23 | 44 | 0 | 10 | 375 | 455 |
| recurrent concussion AND sport | 1 | 5 | 14 | 0 | 1 | 41 | 62 |
| Total | 29 | 326 | 455 | 16 | 117 | 1908 | 2851 |
Study Selection
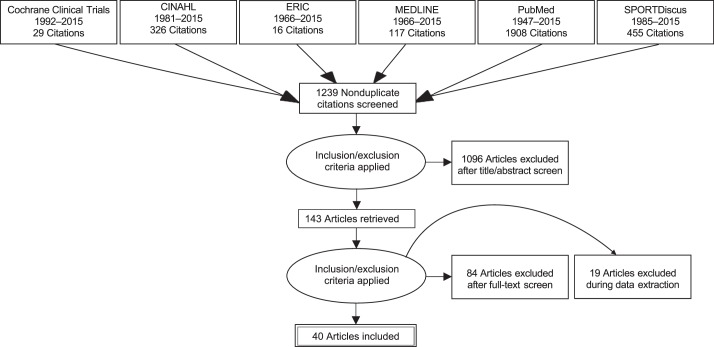
After removing duplicates, a 2-step process was used to identify appropriate articles for the review (Figure). Initial screenings of the titles and abstracts were completed independently by 3 of the authors (T.C.V.M., J.H.L., C.E.W.B.). A meeting was held to discuss any articles for which consensus on inclusion was not obtained. This was followed by a full-text review by the same 3 authors and an additional meeting to discuss the remaining articles for which consensus was not obtained. Articles were excluded if they did not meet the inclusion criteria.
Figure.
Search strategy and study selection process. Abbreviation: ERIC, Educational Resources Information Center.
Articles were included if they were published in English, were original research, and evaluated the use of, compliance with, or effectiveness of physical or cognitive rest after concussion or provided empirical evidence supporting the graded return-to-activity progression. Excluded articles consisted of narrative (clinical) reviews, editorials, critically appraised topics, commentaries, abstracts, animal research, studies of non–sport-related concussion, or original research that did not address the primary clinical questions of interest.
Data Extraction and Quality Assessment
Articles were categorized according to the clinical question of interest. The study design; patient or participant sample; instrumentation or interventions used; outcome measures; main results; and conclusions were extracted, as appropriate, from each article and entered on a standard data-collection form. Because many of the studies included primary and secondary outcomes, we limited extraction of the outcomes and presentation of the results to those outcomes that fit the clinical questions of interest. Studies were assigned a level of evidence as outlined by the 2011 Oxford Centre for Evidence-Based Medicine scale.17
Data Synthesis and Analysis
We critically analyzed the included studies to evaluate the patients, methods, and results. We summarized the conclusions using a qualitative synthesis of the findings. Articles were categorized into groups based on their ability to answer 1 of the primary clinical questions of interest: use of rest, rest effectiveness, compliance with recommendations, or outcomes after graded return-to-activity progression. If a study addressed more than 1 clinical question, it could be included in more than 1 area. Summary tables were developed to present the results. Because of the observational nature of many included studies and the heterogeneity of the patients, participants, interventions, or outcomes, we were unable to pool the data; therefore, a meta-analysis was not possible.
RESULTS
Results of Search
The literature search resulted in 2851 potential articles (Figure; Table 2). After we removed 1612 duplicates found across databases or with different search terms, we screened the remaining 1239 articles to meet the inclusion and exclusion criteria. After reading the title and abstract, we removed 1096 articles (194 narrative reviews, 34 commentaries, 8 editorials, 5 abstracts, 2 critically appraised topics, 1 unpublished dissertation, 68 not in English, 19 consensus statements, and 765 not relevant to the clinical questions), leaving 143 articles for full-text evaluation. Application of the exclusion criteria during the full-text review resulted in exclusion of 84 articles. Another 19 articles were excluded during the data-extraction process, leaving 40 articles from which data were extracted that were synthesized in the results. These consisted of 9 studies of use of rest, 10 studies of rest effectiveness, 17 studies evaluating compliance with guidelines, and 4 studies of return-to-activity outcomes.
Use of Rest
Nine studies evaluated the use of rest and associated academic adjustments by health care providers (Table 3). The study designs were prospective cohort (n = 1), retrospective cohort (n = 2), retrospective chart review (n = 2), and cross-sectional survey (n = 5); 1 study used 2 research designs (retrospective chart review and cross-sectional design).
Table 3. .
Summary of Studies Examining the Use of Cognitive Rest, Academic Adjustments, or Both Continued on Next Page
| Study |
Design |
Sample |
Data Collection or Instrumentation |
Intervention |
Key Results |
Level of Evidencea |
| Arbogast et al18 (2013) | Cross-sectional surveyRetrospective chart review | 89 of 191 Physicians (44% response rate) from the Children's Hospital of Philadelphia Care Network174 Adolescents (54.1% male; average age = 12.9 y) | Survey consisted of multiple questions to assess concussion knowledge, concussion management, and barriers to concussion management174 Medical records from a 10% random sample of 1760 potential records of children diagnosed with concussion or mild traumatic brain injury | None | 62% of Physicians described awareness of CR as part of management; only 2.4% described CR in detail11% of Charts reviewed included written CR recommendations | 3 |
| Carson et al21 (2014) | Retrospective chart review | 159 Patients with 170 documented sport-related concussions (105 males, 65 females) | 170 Charts for the 159 patients reviewed over a 5-y period (2006−2011)Data extracted included concussion history, results from cognitive and balance assessments, and Sport Concussion Assessment Tool or Sport Concussion Assessment Tool 2 scores | NonePremature RTL defined as documentation of worsening symptoms or recurrence of symptoms that accompanied RTL | Worsening of symptoms in 44.7% of patients after premature RTLPatients with history of concussion required more rest days before being cleared | 3 |
| Grubenhoff et al22 (2015) | Prospective cohort | 179 Adolescents of 273 patients presenting to an emergency department with concussion | Data collected included primary care and specialist visits, visits to other health care professionals, school absenteeism, and AAs | Participants split into 2 groups: PPCSs 1 month after injury or no PPCSs | Patients with PPCSs missed 50% more school days than those with no PPCSsAAs provided to 36% of patients with PPCSs and 53% of patients with no PPCSsAssociation between follow-up visits and receiving AAs (relative risk = 2.2; 95% confidence interval = 1.4, 3.5) | 2 |
| Olympia et al25 (2016) | Cross-sectional survey | 1033 of 3000 SNs (36% response rate) from National Association of School Nurses | Survey consisted of several questions to assess training in concussion detection and management, SN's responsibilities in preventing and detecting concussion, SN involvement in postconcussion care, and presence of RTL guidelines or protocols | None | 58% of SNs responsible for guiding students' graduated academic-reentry process | 3 |
| Upchurch et al19 (2015) | Retrospective cohort chart review | 497 Youth sport-related concussions documented from 392 908 emergency department visits from 2004−2012 | Data extracted included discharge instructions; instructions evaluated for physical and CR recommendations, primary care follow-up, and referral to specialist | None | CR not recommended to any patient before 2008CR only recommended to 12% of patients by 2012 | 3 |
| Weber et al24 (2015) | Cross-sectional survey | 1246 of 8000 SNs (15.6% response rate) from National Association of School Nurses | Beliefs, Attitudes and Knowledge of Pediatric Athletes with Concussion–School Nurse version consisted of several questions to assess concussion management, collaboration, and familiarity with and use of AAs | None | 59.4% of Student-athletes with concussion under care of an SN received AAs, yet only 27.7% of SNs always or almost always recommended AAs after sport-related concussion | 3 |
| Wilkins et al23 (2014) | Retrospective cohort chart review | 586 Adolescent patients (ages 0 to 18 y) suffering from 589 pediatric sport-related concussions | Data extracted included patient-specific, injury-specific, and medical evaluation–specific variables | Sports Concussion Clinic, which opened in August 2011, used standardized concussion guidelines; participants split into 2 groups: prestandardization (patients diagnosed January 1, 2007 to August 2, 2011) or poststandardization (patients diagnosed August 3, 2011 to December 31, 2011) | Instructions for return to thinking increased from 24% prestandardization to 98% poststandardization | 3 |
| Williams et al26 (2015) | Cross-sectional survey | 851 of 3286 Athletic trainers (26% response rate) employed in a secondary school setting | Beliefs, Attitudes and Knowledge of Pediatric Athletes with Concussion–Athletic Trainer version consisted of questions to assess concussion management, collaboration, and familiarity with and use of AAs | None | 41% of Student-athletes with concussion under care of an athletic trainer received AAs | 3 |
| Zemek et al20 (2015) | Cross-sectional survey | 115 of 176 Physicians (65% response rate) from Pediatric Emergency Research Canada Network | Survey consisted of questions to assess knowledge of concussion diagnosis, initial concussion management, use of existing concussion protocols, and barriers to protocol use | None | CR recommendations were limited; 40% of physicians did not recommend school absence, 30% did not recommend schoolwork reduction, and 35% did not recommend limiting screen time | 3 |
Abbreviations: AA, academic accommodation; CR, cognitive rest; PPCS, persistent postconcussive symptom; RTL, return to learning; SN, school nurse.
Levels of evidence are based on the Oxford Centre for Evidence-Based Medicine taxonomy.17
Three studies specifically addressed the use of cognitive-rest recommendations, and their findings were similar. Although 62% of physicians indicated understanding that cognitive rest should be part of the concussion-management plan, Arbogast et al18 reported that only 11% of adolescent medical records included written recommendations for cognitive rest. Similarly, Upchurch et al19 conducted a retrospective chart review and reported that cognitive-rest recommendations were not made to any patient before 2008, and recommendations for patients to rest increased only to 12% by 2012. Zemek et al20 also noted that cognitive-rest recommendations provided by physicians were limited.
Two studies addressed the effect of a patient's medical history and postconcussion symptoms on cognitive rest and return-to-learn progressions. After a retrospective chart review, Carson et al21 concluded that adolescents with a history of concussion required more days of rest than those without a history. Additionally, 44.7% of patients had worsening symptoms when they prematurely progressed through a return-to-learn protocol. Similarly, Grubenhoff et al22 observed that adolescents with persistent postconcussive symptoms (ie, >1 month) missed 50% more school days than adolescents without such symptoms. However, the percentage of patients who received academic adjustments did not differ between those with and those without postconcussive symptoms, suggesting underuse of academic adjustments for patients who would likely benefit.
Four studies addressed health care professionals' involvement in return-to-learn protocols. Wilkins et al23 conducted a retrospective cohort chart review and found that instructions for a “return-to-think” progression increased from 24% to 98% after the implementation of standardized concussion guidelines by health care professionals in a sports concussion clinic. Three of the 4 studies used a cross-sectional survey to assess the role of school nurses or athletic trainers in implementing academic accommodations in the secondary school setting. Specifically, Weber et al24 showed that 59% of student-athletes with concussions who were under the care of a school nurse received academic accommodations, whereas Olympia et al25 demonstrated that 58% of school nurses were responsible for guiding the graduated academic-reentry process for student-athletes with concussions. Williams et al,26 on the other hand, reported that 41% of student-athletes under the care of an athletic trainer employed in the secondary school setting received academic accommodations after a sport-related concussion.
Effectiveness of Rest
Ten studies evaluated the effectiveness of rest in recovery (Table 4). The study designs and outcome measures had significant heterogeneity; some were focused on both cognitive and physical rest, and others only evaluated cognitive rest. Of the included studies, 4 were retrospective cohort, 3 were prospective cohort, and 3 were randomized controlled trials (RCTs). The outcome variables differed and included total symptom score, symptom duration, neurocognitive function, balance assessment, and clinical recovery, defined as a return to baseline on adjunct (cognitive and balance) assessments.
Table 4. .
Summary of Studies Evaluating the Effectiveness of Rest After Concussion Continued on Next Page
| Study |
Design |
Patients |
Intervention |
Outcome Measures |
Main Findings |
Conclusions |
Level of Evidencea |
| Brown et al30 (2014) | Prospective cohort | N = 335; 15 ± 2.6 y old (8 to 23 y old); 62% male; 21.8% ice hockey players; 20.6% football playersConcussion specialty clinic | No interventionPatients categorized by CA daysCA level assessed via a 5-point scale developed by authors (0 = complete cognitive rest, 1 = minimal cognitive activity, 2 = moderate cognitive activity, 3 = significant cognitive activity, 4 = full cognitive activity) | Duration of concussion symptoms | Overall mean duration of symptoms = 43 ± 53 dPatients in fourth quartile of CA days had delayed recovery compared with those in quartiles 1–3CA days associated with symptom duration (hazard ratio = 0.9942; 95% confidence interval = 0.9924, 0.9960) | Patients engaged in highest levels of CA took longest times for symptoms to resolveSimilar recovery trajectory noted for lower 3 quartiles, which suggests that complete cognitive rest may not be needed | 3 |
| Buckley et al33 (2016) | Prospective cohort | N = 50; rest group = 19.8 ± 1.2 y old and no-rest group = 19.4 ± 1.3 y oldCollege | No-rest group not prescribed any rest but was withheld from sport participationRest group prescribed cognitive and physical rest on day of concussion and next day was instructed to not attend class, team meetings, or study hall; to not use electronics; and to refrain from team and personal exercise | Concussion clinical battery, including graded symptom checklist, ImPACT computerized neurocognitive test, BESS, and SAC | Rest group symptomatic longer than no-rest group (5.2 ± 2.9 d versus 3.9 ± 1.9 d; P = .047)No differences found on SAC, BESS, or ImPACTNo difference in time until clinical recovery | 2 d Cognitive and physical rest not effective in altering recovery time as measured by clinical assessment battery | 3 |
| de Kruijk et al35 (2002) | RCT | N = 103; 51 in no–bed-rest group (39.9 ± 14.5 y old; 52% male; 13% sport-related mechanism of injury) and 52 in full– bed-rest group (34.1 ± 6.5 y old, 60% male, 6% sport-related mechanism of injury)Emergency department and outpatient clinic | No–bed-rest group instructed to be mobile and take ≤4 h of bed rest/d, which decreased until day 5, when they were to resume normal daily activitiesFull–bed-rest group instructed to take full bed rest during first 6 d after injury, then by progressive decrease in bed rest, as followed by no–bed-rest group initially | Severity of 16 post-traumatic complaints at 2 wk, 3 mo, and 6 mo after injuryPosttraumatic complaints categorized into cognitive, dysthymic, vegetative, and physical subgroupsMeasured with visual analog scaleMedical Outcomes Short Form-36 | No–bed-rest group had 17 h rest, whereas full–bed-rest group reported 57 h of bed restDuring first 4 d, patients in full–bed-rest group reported less dizziness but no differences seen for headache or nauseaAt 2-wk follow-up, full–bed-rest group had lower visual analog scale scores for feeling faint, but no other symptom complaints were different than in no-rest groupNo differences on any SF-36 subscale score | 6 d of Complete bed rest resulted in no differences between no–bed-rest and full–bed-rest groups in posttraumatic symptoms or general health status | 2 |
| Gibson et al32 (2013) | Retrospective cohort | N = 184; 15 ± 3 y old (8 to 26 y old); 72% maleConcussion specialty clinic | No interventionTreatment plans reviewed to determine whether cognitive rest was recommendedPatients grouped by symptom duration (≤30 d versus >30 d) | Recovery, defined as being symptom free at rest and with exertion, return to or above baseline on computerized neurocognitive testing and balance assessment | Cognitive rest recommended to 85 patients; a higher percentage of those were younger than age 15 (58% versus 37%; P < .01)Mean symptom duration longer in patients to whom cognitive rest was recommended (57 d versus 29 d; P < .001)After adjusting for covariates, no association found between rest recommendation and symptom duration (odds ratio = 0.50; 95% confidence interval = 0.18, 1.37) | No relationship between cognitive rest and duration of symptoms | 4 |
| Majerske et al29 (2008) | Retrospective cohort | N = 95; 15.9 ± 1.4 y old; 84% male; 59% football players; 41% had concussion history; no learning disabilities, attention-deficit/ hyperactivity disorder, or seizure disordersConcussion specialty clinic | No interventionPatients grouped into 1 of 5 activity levels by level of cognitive and physical activity on activity-intensity scale from information within medical chart | Neurocognitive function (ImPACT)PCSS total symptom score | Patients in 2 highest activity levels (school and sports game and school and sports–practice) performed worse on visual memory (P = .003) compared with patients who participated in school activity and light activity at homePatients in highest activity-level performed worse on reaction time (P < .001) compared with patients who participated in school activity and light activity at homeTrend between activity intensity level and total symptom score (P < .08)No differences between 2 lowest activity levels and moderate activity level | Patients engaged in highest levels of activity, including full school and game participation in sport, demonstrated impairments in 2 neurocognitive domainsModerate levels of activity (school activity and light activity at home) might be beneficial to patients | 4 |
| Maerlender et al31 (2015) | RCT | N = 28; standard group (12 female, 3 male) and exertion group (8 female, 5 male)College | Participants randomized to standard care or exertionStandard-care group instructed to engage in no systematic exertion beyond normal activities for schoolExertion group rode stationary bike at mild to moderate level for 20 min daily and wore activity monitor | Recovery, defined as return to baseline on neurocognitive, balance, and symptom scores | Median days to recovery did not differ by groups (P = .705)No group difference found in number of patients who took longer than 2 wk to recover (P = .464)Symptom increase after bike protocol not related to length of recovery (P = .252)Average amount of daily vigorous exertion related to recovery; more activity resulted in increased recovery time (P = .039) | Early mild to moderate exercise did not delay recoveryVigorous exercise associated with longer recovery | 2 |
| Moor et al34 (2015) | Prospective observational | N = 56; 15.2 ± 1.7 y old; 53.6% male; 32.7% football playersHospital-based sports medicine center | No interventionParticipants surveyed at discharge regarding recommendations for physical and cognitive rest, how receptive they were to recommendations, and how frequently they followed each recommendation | Recovery, defined as date of physician clearance | All patients received recommendations for physical rest; 71.3% were receptive to this recommendation and 87.5% reported adherence to recommendation92.9% of Patients received recommendations for mental rest with restrictions from electronics; 67.3% were receptive to and 76.9% adhered to recommendation92.8% of Patients received recommendations for mental rest with school restriction; 82.9% were receptive and 90.2% adhered to recommendation | None of variables for assessing adherence to rest were significant predictors of recovery | 3 |
| Moser et al27 (2012) | Retrospective cohort | N = 49; 15 ± 2.6 y old (14 to 23 y); 67% male; 27% ice hockey playersConcussion specialty clinic | 1 wk of Full rest, defined as no school, homework or tests, travel or shopping, driving, social activities, watching visually intense television, computer use, texting, reading, or physical exercise as well as increased sleepPatients grouped by length of time between sustaining concussion and first postconcussion assessment (1 to 7 d, 8 to 30 d, >31 d) | Neurocognitive function (ImPACT)PCSS | Improvement in cognitive function in all composite scores (P < .001 to P < .008)Total symptom score decreased after rest (P < .001)No main effect for time since concussion (P = .44) | 1 wk of Cognitive and physical rest decreased symptoms and increased cognitive scores, regardless of time between concussion and onset of rest | 4 |
| Moser et al28 (2015) | Retrospective chart review | N = 13; 15.1 ± 1.5 y old with persistent symptoms after concussion; 57% male; 77% self-reported attention-deficit/hyperactivity disorder, learning disability, or history of 2+ concussions | Patients instructed to complete 1 wk of full rest, defined as no school, homework or tests, travel or shopping, driving, social activities, watching visually intense television, computer usage, texting, reading, or physical exercise as well as increased sleep | Neurocognitive function (ImPACT)PCSS | Cognitive function for all 4 composite scores improved after rest (P = .002 to P = .017)Total symptom score decreased after rest (P = .02) | 1 wk of Prescribed rest decreased symptoms and improved cognition in 61.5% of patients | 4 |
| Thomas et al36 (2015) | RCT | N = 88; strict-rest group = 14.7 y old (13 to 15.5 y old); usual-care group = 13.1 y old (12.1 to 14.5 y old); 66% male; 71% sport mechanism; 27% football playersPediatric emergency department | Strict-rest (intervention) group was to maintain 5 d of strict rest at home, refraining from school, work, and physical activity followed by stepwise return to activityUsual-care (control) group received verbal recommendations as seen fit by treating physician | Activity diaryNeurocognitive function: computerized (ImPACT) and pencil-paper batteryBESSPCSS | Usual-care group reported more hours of moderate and high mental activity (8.33 versus 4.86 h; P = .03) from days 2–5 after injuryStrict-rest group reported higher PCSS total symptom score during follow-up period (187.9 versus 131.9; P < .03) and higher number of endorsed symptoms (70.4 versus 50.2; P < .03)No differences noted for computerized neurocognitive test scores or balance scores on days 3 or 10 postinjuryStrict-rest group performed better on Symbol Digit Modalities Test on day 3 (67.6 versus 59.9; P < .01) and worse on day 10 (67.6 versus 71.5; P = .04) but differences not found with other pencil-paper tests | Strict-rest group reported more symptoms and had slower symptom resolution than usual-care groupStrict rest may not be more beneficial than usual care | 2 |
Abbreviations: BESS, Balance Error Scoring System; CA, cognitive activity; ImPACT, Immediate Post-Concussion Assessment and Cognitive Test; PCSS, PostConcussion Symptom Scale; RCT, randomized controlled trial; SAC, Standardized Assessment of Concussion.
Levels of evidence are based on the Oxford Centre for Evidence-Based Medicine taxonomy.17
The findings varied: 2 studies27,28 indicated that rest improved outcomes, 3 studies29−31 identified too much activity as detrimental to recovery and resulting in worse outcomes, 4 studies32−35 found no association between rest and outcomes, and 1 study36 showed that strict rest can lead to a longer recovery.
The authors27,28 reporting that rest was beneficial to recovery used a similar clinical sample of patients presenting to a concussion specialty clinic. In a retrospective chart review of 13 patients with persistent concussion symptoms, patients were evaluated in the clinic 24.8 ± 30.7 days after their concussion and prescribed 1 week of cognitive and physical rest.28 After the prescribed rest, patients had significant improvements in cognitive function and a reduction in the total symptom severity score. An earlier retrospective cohort study from the same clinic investigated how 1 week of prescribed cognitive and physical rest affected patients presenting with different durations of postconcussion symptoms.27 After the week of rest, a significant improvement in cognition and reduction in symptoms were noted among all patients; no effect was noted for the length of time patients were symptomatic, which suggests that rest can be an effective treatment, regardless of whether it is prescribed acutely after concussion or is delayed.27
In addition to these 2 studies, 3 other studies29−31 showed that moderate levels of rest resulted in better outcomes compared with higher levels of activity, which may hinder recovery. In one of the first studies to evaluate rest and activity after sport-related concussion, Majerske et al29 retrospectively analyzed how activity level influenced cognitive and symptom outcomes. The authors developed an activity intensity scale (AIS) that ranged from 0 to 4, with 0 indicating no school or exercise activity and 4 indicating school activity and participation in competitions. Using the AIS rating of 2 (school activity and light activity at home) as the reference, their analysis determined that AIS affected scores of visual memory and reaction time, with patients in the highest activity level (AIS = 4) having the worst visual memory and slowest reaction times.29 However, no differences were noted between the lower AIS levels and the reference level, suggesting that moderate amounts of cognitive and physical exertion may be an appropriate management strategy.
Similarly, a prospective study that examined how cognitive activity levels affected duration of concussion symptoms found that patients engaged in the highest levels of activity took longer to resolve symptoms.30 The authors developed a cognitive activity scale for patients to complete at each follow-up visit. The scale ranged from 0 to 4, with 0 indicating complete cognitive rest (no reading, homework, texting, video games) and 4 indicating full cognitive activity (no restrictions). Patients in the highest quartile of cognitive-activity days took significantly longer to recover than patients in the first to third quartiles, suggesting that too much activity may hinder recovery.30 However, the recovery times of patients within the lower quartiles did not differ, indicating that refraining from all cognitive activity may not be necessary and that some activity may be beneficial to the recovery process.
A negative association between activity and recovery was also noted in a pilot RCT of collegiate athletes.31 Patients were randomized either to standard care (no exertion beyond normal school activities) or to an exertion group, who rode a stationary bicycle for 20 minutes at mild to moderate intensity and wore an ActiGraph device to track activity. Although the median days to recovery did not differ by group, the average amount of daily vigorous exertion was related to recovery: more vigorous activity resulted in a longer recovery time. Similar to other results, early mild to moderate exercise did not delay recovery, suggesting that it may be useful in managing patients with concussion.31
Four studies32−35 found no association between rest and outcomes. De Kruijk et al35 evaluated the effect of 6 days of bed rest compared with no rest on patients presenting to an emergency department. Patients randomized to the bed-rest group reported less dizziness during the first 4 days after injury and a lower score for “feeling faint” at the 2-week follow-up, but other symptom scores and perceptions of quality of life did not differ between the groups at either time point, indicating that complete bed rest did not improve outcomes.35 Similarly, in a retrospective cohort study of patients presenting to a sport concussion clinic, cognitive rest was prescribed to just over 46% of the patients; the recommendation for cognitive rest resulted in a longer mean symptom duration compared with patients to whom cognitive rest was not recommended.32 However, once adjustments were made for other covariates, no association was noted between the rest recommendation and duration of symptoms.32 These findings are similar to those reported by Moor et al,34 who investigated adherence to rest and recovery time in adolescent athletes. Although patients generally followed the recommendations regarding physical and cognitive rest, adherence to rest was not a predictor of the length of time to recovery.37 Lastly, authors33 of a prospective study of collegiate athletes before and after a concussion policy change investigated the acute effects of 2 days (day of injury and 1 day after) of prescribed complete physical and cognitive rest on concussion-assessment measures, including cognition, balance, and symptoms. The group prescribed rest was symptomatic longer than the no-rest group, but no differences among groups were found on any of the other outcome measures.33
In contrast, too much rest was detrimental to recovery in 1 RCT.36 This study of patients with concussion presenting to a pediatric emergency department randomized patients into a usual-care group and a strict-rest group. Patients in the usual-care group were given verbal recommendations for activity from the treating physician. Patients in the strict-rest group were given discharge instructions for 5 days of strict rest at home that included no school, work, or physical activity. After the intervention, the strict-rest group reported a higher symptom severity score and had a slower resolution of symptoms compared with the usual-care group, but there were no meaningful differences on cognitive and balance testing, which suggested that restricting activity too much may result in unfavorable outcomes after concussion.36
Compliance With Return to Activity
Researchers in 17 studies evaluated provider knowledge, attitudes, and beliefs regarding return-to-activity guidelines as well as compliance with return-to-activity recommendations made in position or consensus statements (Table 5). All of the studies were descriptive in nature and varied regarding the providers surveyed; therefore, some may have limited generalizability.
Table 5. .
Summary of Studies Evaluating Compliance With Current Return-to-Activity Guidelines Continued on Next Page
| Study |
Design |
Sample |
Data Collection or Instrumentation |
Key Results |
Conclusions |
Level of Evidencea |
| Baugh et al48 (2015) | Cross-sectional survey | 32 150 Coaches, sports medicine clinicians, compliance administrators at all 1066 NCAA institutions2880 Individuals participatedResponse rate 9%907 Institutions had at least 1 respondentInstitution-level response rate 85% | E-mail survey with population-specific questions about institutional concussion management developed using NCAA's concussion policy; 3 overarching categories: individual- and school-level demographics, concussion-policy management and implementation, and individual perceptions of management | 92.7% Reported presence of institutional management plan, 1.1% reported none, and 6.2% were unsureMost respondents indicated that their concussion plan protected athletes well (32.3%) or very well (66.4%). However, 78.1% of respondents indicated improvement was needed.83.4% Responded that team physicians and/or ATs had final say on RTP decisions | Large majority of respondents indicated their school had a concussion-management plan. However, there was a lack of compliance with some specified components. Findings reinforce need for specific, implementable, and enforced guidelines at NCAA member schools. | 3 |
| Broshek et al44 (2014) | Cross-sectional survey | 1109 Active members of Child Neurology Society239 Members participated; response rate = 22% | Online survey with questions targeting demographics, clinical practice variables, perceived adequacy of training and continuing education in sport concussion practice, and use of collateral data to assess clinical practice management of concussion | 56% of Respondents exclusively used American Academy of Neurology's 1997 practice parameter, 8.2% used Zurich guidelines exclusively, and 8.6% reported using no guidelinesYears in practice and CME were significant predictors of RTP guidelines used. Those with more years in practice were more likely to use American Academy of Neurology's practice parameter. Those with more concussion-specific CME were more likely to use Zurich guidelines.73.4% of Respondents were comfortable making RTP decisions, 55.2% waited 2 wk after sign/symptom resolution, and 93.1% required gradual RTP | Few respondents relied on Zurich guidelines.More respondents who completed CME made decisions using Zurich guidelines, which support need for additional education in sport concussion at all levels. | 3 |
| Buckley et al41 (2015) | Cross-sectional survey | 1976 ATs at NCAA Division II and Division III institutions1880 ATs received survey; 755 participated; response rate = 40.2% | 65-Item online questionnaire with 3 sections on demographics and professional experience, concussion assessment, and concussion management specific to recovery and RTP procedures to descriptively define concussion-management practices of NCAA Division II and III ATs | During acute assessment, 76.9% of Division I respondents and 76.0% of Division II respondents used multifaceted assessmentFor determinations of recovery, 65.0% of Division I and 63.1% of Division II respondents reported using multifaceted assessmentAt baseline, numbers were lower: 43.1% of Division I and 41.0% of Division II respondents reporting using multifaceted assessment | Limited use of multifaceted assessment at baseline but higher rates at acute assessment and RTP time pointsPrimary reason cited for not using assessment was lack of funding or staffingMost reported management protocols consistent with recommendations | 3 |
| Covassin et al40 (2009) | Cross-sectional survey | 300 Program directors and 1200 ATs from 300 accredited athletic training programs513 PDs and ATs participatedResponse rate = 34.2% | 17-Question online survey addressing education level, years of certification, employment setting, concussion-assessment and RTP guidelines used, and clinical and teaching preferences. Vienna guidelines were provided to participants. | 61% of Respondents reported using NATA position statement method to assess and manage concussions, and 47% used it to make RTP decisions66% of Respondents had never heard of Vienna guidelines. After reading them, nearly 75% of participants agreed with them, 68% said they would use them, and 84% said they would teach them to students. | Majority of respondents used multidimensional approach to assess and manage concussion. NATA position statement and Vienna guidelines were underused in both classroom and clinical settings. | 3 |
| De Maio et al51 (2014) | Retrospective observational cohort | 68.4% of Study patients were male; mean age = 12.8 y350 Patients aged 6 to 18 y old evaluated in designated children's emergency department at level I trauma center in 2008 for acute head trauma218 (62%) Included in study | Systematic data extraction from electronic medical records. Data extracted included demographics, characteristics of injury, presenting signs and symptoms, radiographic orders and findings, final diagnoses, disposition, and discharge instructions. | Only 31% of patients had documented diagnosis of concussion, despite presenting with signs and symptoms. Yet, almost 67% of patients received discharge instructions specifying a concussion.Almost 67% of patients had no documentation of activity restrictions; recommendations highly variable for those who received them | Most children discharged without concussion-specific diagnoses or activity restrictions. Increased awareness and standardization for concussion management needed. | 3 |
| Gordon et al45 (2014) | Cross-sectional survey | 2600 Pediatric specialists and subspecialists from Canadian Pediatric Surveillance Program809 Specialists participatedResponse rate = 31% | 7-Item questionnaire, sent as part of Canadian Paediatric Surveillance Program, asked about encounters with and management of concussions/mild TBI in children | 96.7% of Respondents reported using 1 or more of presented guidelines84.9% of Respondents did not initiate RTP immediately after patients became asymptomatic; median wait time for RTP was 7 dMedian duration of RTP process = 7 d, though much variation reported | Concussion/mild TBI care appeared consistent with current guidelines, although variance found when current guidelines were less proscriptive | 3 |
| Haran et al52 (2016) | Prospective observational | 271 Children aged 5 to 18 y old with sport-related head injury presenting to an ED in Melbourne, Australia93 Children were included in study (34% of sample); 100% response rate to survey91.4% Response rate to follow-up phone call | Eligible children identified at initial presentation to ED and given a researcher-administered surveyParents of patients contacted with follow-up phone call 3 wk to 3 mo after surveyUpon discharge, patients provided with a sports fact sheet based on International Concussion in Sports Group guidelines | 42% of Concussions received during organized sport not managed according to recommended guidelines: 19% of participants not immediately removed from play, 29% allowed to return same day, and 27% not assessed by qualified personnel93% of Parents and 96% of patients unaware of RTP guidelines | Lack of on-field assessments in children with sport-related concussionMany children continued to play after injury. Awareness of RTP practices in coaches, teachers, parents, and children needs to be improved. | 2 |
| Hollis et al53 (2012) | Prospective cohort | Community rugby union players aged 14 to 48 y old in the Sydney metropolitan area, Australia1958 Included in cohortStudy length varied from 1 to 3 seasons 85% of cohort followed for 1 y | Self-administered questionnaire | Describe proportion of rugby union players who complied with RTP regulations after concussion | Lack of RTP advice given to community rugby players and high level of noncompliance with RTP regulations; need for better dissemination of information and improved understanding of causes of noncompliance | 2 |
| Hunt and Trombley47 (2010) | Cross-sectional survey | 120 Team physicians from 43 Division I colleges or universities contacted61 Physicians participated from 37 schoolsResponse rate = 50.8% | E-mailed online 19-item survey, adapted from 32-item survey used by Notebaert and Guskiewicz (2005)Participants described number of years in specialty, area of specialty, sports covered, primary focus of employment, number of sport concussions seen yearly, methods used to assess and diagnose concussion and for RTP decisions | 98% Reported they were responsible for RTP decisions; 72% reported access to neuropsychologistMost important method of assessing RTP reported by physicians: clinical examination (48%), symptom checklist (21.3%), concussion-grading scale guidelines (13.1%), player self-report (6.6%), Standardized Assessment of Concussion (4.9%), and neurocognitive testing (4.9%) | Variability observed with respect to tools used for RTP decisions; no statistical association for specialty or years of experienceClinical examinations and symptom checklists were most common methods for concussion assessment (no difference by specialty). | 3 |
| Kelly et al42 (2014) | Cross-sectional survey | 1774 ATs from NCAA Division I institutions610 ATs participatedResponse rate = 34.4% | Online questionnaire with 65 items3 Subsections: demographics, concussion-assessment practice patterns, and concussion recovery/return-to-participation practice patternsIncluded 21 items specific to recovery and return-to-participation procedures | 66.9% of Participants used multifaceted (at least 3) assessments for return to participation84.6% of Respondents aware of Third International Consensus Statement on ConcussionAlmost 2/3 of clinicians administered Balance Error Scoring System and Standardized Assessment of Concussion daily or every other day once symptom free; guidelines suggest no more than 2×/wk | More than half of NCAA Division I AT respondents used multifaceted concussion-assessment techniques, but there was room for improvement in specific practice patterns. | 3 |
| Kinnaman et al46 (2014) | Cross-sectional survey | 1305 Members of American Academy of Pediatrics Section on Adolescent Health, Sports Medicine and Fitness, Community Pediatrics and School Health220 RespondentsResponse rate = 17% | 17-Item online questionnaireEvaluated use of medications, neuropsychological testing, neuroimaging, and published guidelines in concussion management | 84% Reported using published guidelines to manage patients; Third International Consensus Statement on Concussion cited by 38%89% Managed patient symptoms with medications5% Allowed patients to return to sport while still taking medication68% Reported using neurocognitive testing | More than half of pediatrician respondents used neurocognitive testing, and vast majority used published guidelines. | 3 |
| Kroshus et al49 (2015) | Cross-sectional survey | 2462 ATs and 429 physicians from all 1066 NCAA member institutions789 ATs and 111 team physicians from 530 institutions respondedSchool-level response rate of 49.7% and individual-level response rate of 30.7% | Online survey to determine if participants experienced pressure from 3 stakeholder populations to prematurely return athletes to participation after concussion | 64.4% of Responding clinicians reported experiencing pressure from athletes, 53.7% from coaches, and 6.6% from other cliniciansWomen reported more pressure than menClinicians reported greater pressure from coaches if their departments were under supervisory purview of athletic department | More than half of clinicians reported pressure for athletes to RTP prematurely after concussion with female clinicians; those employed by athletic department reported greatest pressure. | 3 |
| LeBrun et al43 (2013) | Cross-sectional survey | 3154 Family physicians in Alberta, Canada, and 545 in North and South DakotaCanadian physicians recruited by mail; 80 participated, response rate = 2.5%US physicians recruited through database; 109 participated; response rate = 20% | 21-Item online surveyDiagnostic and management (rest and RTP) strategies for concussion and preferred knowledge transfer and exchange strategies | 63.4% of US physicians recognized RTP guidelines versus 23.8% of Canadian physiciansRTP decisions reportedly based on clinical examination (89.1% US versus 73.8% Canadian), symptom checklist (50.5% US versus 53.8% Canadian), player self-report (51.5% US versus 60% Canadian), balance testing (27.7% US versus 20% Canadian), neurocognitive testing (29.7% US versus 5% Canadian) | Published guidelines for concussion management not always followed, particularly recommendations for cognitive restMajority want more education | 3 |
| Lynall et al38 (2013) | Convenience sample, survey | Survey sent to 3222 certified ATs, members of NATA1053 ATs respondedResponse rate = 32.7% | 33- to 47-Item online survey (varies based on logic inside survey)Demographic and experience dataAssessed tools used to diagnose, manage, and return athletes to participationIncluded detailed questions about various concussion-assessment toolsAdditional questions about understanding of concussion research and familiarity with guidelines | Clinical assessment was most commonly reported method used to diagnose and assess concussion67% Stated they used return-to-participation guidelinesOnly about 21% of ATs used all 3 recommended areas of concussion assessment for RTPAbout 10% stated that athlete would be allowed to return to participation with normal clinical examination but abnormal findings on standardized methods of concussion assessment | Vast majority of ATs did not use all 3 recommended areas of concussion assessment for RTP decisionsHigh awareness of guidelines but significant room for improved application related to RTP | 3 |
| Meehan et al50 (2010) | Descriptive epidemiology study | 1056 Sport-related concussionsAll concussions recorded by High School Reporting Information Online Injury Surveillance system 2009−2010 | High School Reporting Information Online contains data from 192 US high schools for athletes participating in 20 sports. All have at least 1 AT affiliated with NATA. All concussions that occurred during an organized high school athletic event resulted in athlete receiving care from medical provider and were brought to attention of AT.Timing of RTP, type of provider returning athlete to play, and duration of symptoms recorded | 50.1% of RTP decisions made by physicians, 46.2% by ATs, and 2.5% by coaches or other nonmedical personnelPhysicians more likely to use neuropsychological testing for RTP than other providersNo association between timing of athlete returning and type of provider making RTP decision or level of competition (eg, varsity versus junior varsity) | RTP timing for high school athletes similar, regardless of provider making the decision | 3 |
| Notebaert and Guskiewicz39 (2005) | Cross-sectional survey | 2750 Certified ATs, members of NATA927 ATs respondedResponse rate = 33.7% | 32-Item online surveyEvaluated experience, methods of assessing concussion, and guidelines used for RTPCompliance with NATA position statement on sport-related concussion evaluated | Only 3% of ATs in the survey used triple modality in keeping with NATA guidelines for RTP decisionsTeam physician responsible for making RTP decisions 54.84% of time; AT, 26.04% of time; primary care physician, responsible 20.76% of time | Small portion of ATs followed NATA guidelines for RTP decisions. | 3 |
| Sarsfield et al54 (2013) | Retrospective chart review | 204 Patients aged 2 to 18 y, evaluated and treated for head injury at level I trauma center over 4-mo periodChildren with mild head injury, concussion, minor head trauma, or mild TBIExcluded if positive computed tomography or if patient admitted to hospital | Chart review, formal chart extraction form by single chart reviewerEvaluated age, sex, presumptive diagnosis, mechanism of injury, time since injury, care received before EDDischarge documentation evaluated for follow-up care recommendations, anticipatory guidance, symptomatic management, and any information about restrictions on activity or time frame for such restrictions | 95.1% Received instructions to follow up with physician15.2% Received specific restrictions from sports and 21.5% removed from sportsOf 30 patients with sport-related mild TBI, 53.3% given activity restrictions and 46.7% given time restrictions for activities | Children with head injuries, specifically with sport-related mild TBI, not appropriately instructed to restrict athletic activities upon discharge from trauma center | 3 |
Abbreviations: AT, athletic trainer; CME, continuing medical education; ED, emergency department; NATA, National Athletic Trainers' Association; NCAA, National Collegiate Athletic Association; PD, director of athletic training programs; RTP, return to play; TBI, traumatic brain injury.
Levels of evidence are based on the Oxford Centre for Evidence-Based Medicine taxonomy.17
Five studies38−42 were cross-sectional surveys of athletic trainers; the majority of the participants were members of the National Athletic Trainers' Association. These studies highlighted deficiencies in the use of multifaceted assessments for return-to-play decisions with varying levels of compliance. No study demonstrated full compliance with all 3 recommended areas of concussion assessment (graded symptom checklist, neuropsychological testing, and balance assessment) for return to play.
Five studies43−47 were cross-sectional surveys of various types of physicians, including team physicians, pediatricians, family physicians, and members of the Child Neurology Society, and determined that knowledge of and compliance with concussion guidelines varied. The clinical examination was the most frequently cited method for making return-to-activity decisions; however, respondents differed in their preferred methods for evaluating athletes. These results emphasize the need for additional provider education related to return-to-activity decisions.
Two groups48,49 evaluated a mixed sample of coaches, clinicians or physicians, and athletic trainers using a cross-sectional survey design. Baugh et al48 found that although most schools had concussion-management plans, compliance with specific components was lacking. Kroshus et al49 assessed clinicians' perceived pressure to return patients to play and observed that female providers and those supervised directly by the athletic department perceived higher levels of pressure from coaches.
In 5 studies,50−54 investigators used epidemiologic data, chart reviews, or cross-sectional surveys to identify the recommendations given to those with concussion and adherence to guidelines. Emergency department or trauma center chart reviews51,54 indicated that children were discharged without adequate concussion-specific activity restrictions (eg, restriction from athletic participation, avoidance of activities that require attention to visual or auditory stimuli). When patients were surveyed, a lack of appropriate return-to-play advice was evident.52,53 Using high school injury registry data, Meehan et al50 found no association between the timing of the athlete returning to play and the type of provider who made the return-to-play decision. These authors did not look at details of the type of assessments used.
Effectiveness of Graded Return-to-Activity Progression
No studies specifically addressed the effectiveness of graded return-to-activity progressions in improving patient outcomes; however, 4 groups55—58 evaluated aspects of the Zurich guidelines (Table 6). Of those, 3 studies examined return to sport after a standardized protocol based on the Zurich guidelines.55−57 Echlin et al55 investigated recovery duration in junior ice hockey athletes using a clinical evaluation guided by the Zurich return-to-play protocol. Postinjury management was guided by the Zurich protocol, resulting in an average time of 12.8 ± 7.0 days before clinical recovery and return to hockey.55 Chermann et al57 studied the use of a standard protocol based on the Zurich guidelines in rugby athletes with concussions and reported a median of 6 days until symptoms resolved, with female athletes taking longer than male athletes. The mean number of days until patients returned to sport was 21 (range, 7–45 days), even after the mandatory International Rugby Board rule of removal from play for 3 weeks was phased out in 2011. Darling et al56 evaluated return to activity using the Zurich guidelines combined with a standardized exertional treadmill test, the Buffalo Concussion Treadmill Test (BCTT). On average, patients took 16 ± 15 days from the time of the concussion until they reported being asymptomatic, with female athletes taking longer than male athletes. However, the time from concussion to physiologic recovery, as defined by passing the BCTT, was longer, and there was a minimal difference between the sexes.56 All patients returned to sport within the week after passing the BCTT, which kept them out of sport participation for approximately 1 month. The authors56 suggested that a combination of the Zurich guidelines and the BCTT may provide a useful paradigm for making safe return-to-activity decisions.
Table 6. .
Summary of Studies Evaluating Outcomes After the Use of a Graded Return-to-Activity Progression Continued on Next Page
| Study |
Design |
Patients |
Intervention |
Outcomes |
Main Findings |
Conclusions |
Level of Evidencea |
| Chermann et al57 (2014) | Prospective cohort | 35 Patients (30 males, 5 females; 23.1 ± 5.5 y), all rugby athletes | Followed standardized management protocol based on Zurich guidelines that included immediate removal, imaging, cognitive assessment, and return-to-exercise progression before clearance | SymptomsDelay before returning to sportRecurrent (repeat) concussion | Median of 6 d until symptoms resolved (females: 15 d, range = 10–210 d; males: 4 d, range = 0.5–270 d)Mean return to sport at 21 d (range = 7−45 d)Only 2 athletes sustained repeat concussions; both had concussion history, and initial concussion was grade 3 injury (Cantu revised scale) | Use of structured protocol based on Zurich guidelines successful in returning patients to activity with minimal risk of repeat injury | 3 |
| Darling et al56 (2014) | Retrospective chart review and follow-up | 117 Patients (15.5 ± 1.6 y, 75% male) with clinician-diagnosed concussion; 41.2% football players and 25% ice hockey players | Evaluation of BCTT with the Zurich guidelines | Neurocognitive function (Automated Neuropsychological Assessment Metrics or ImPACT)Symptom severity (SCAT2)Physiologic recovery (BCTT) | On average, patients took 16 ± 15 d (range = 0–61 d) from time of concussion until reporting to be asymptomaticFemale athletes took longer than male athletes (22 ± 18 d versus 14 ± 13 d) to be asymptomaticTime from concussion to physiologic recovery longer (24 ± 19 d, range = 3–108 d) with minimal difference between sexes | The BCTT in combination with Zurich guidelines seemed to be safe and successful for returning patients to activity. | 4 |
| Echlin et al55 (2010) | Prospective, cohort | 15 Patients aged 18.2 ± 1.2 y, all ice hockey players | Evaluation of duration of medical restriction after physician-observed and -diagnosed concussion following Zurich return-to-play guidelines | Duration of medical restrictionNeurocognitive function (ImPACT and SCAT2) | Average time interval before clinical recovery and return to hockey of 12.8 ± 7.0 d (range = 7–29 d)5 of 17 Patients (29%) sustained repeat injury with mean interval between injuries of 78.6 ± 39.8 d | Return-to-activity decisions augmented by ImPACT and SCAT2 results and fell in line with Zurich guidelines that clinical decisions should be based on multifactorial input | 3 |
| McCrea et al58 (2009) | Prospective, nonrandomized cohort | Combined data from 3 large datasets (n = 16 624 player seasons)N = 562 | No interventionGroup assignment determined by SFWP or no SFWP | Extent to which SFWP was implementedRecurrent (repeat) concussionClinical outcome defined by scores on the Graded Symptom Checklist, BESS, and Standardized Assessment of Concussion | 60.3% of Patients had SFWPNo differences between groups for demographics or baseline outcome scoresNo differences between groups for duration of symptoms or for Graded Symptom Checklist or Standardized Assessment of Concussion score at time of injury or 2 to 3 h after injuryPatients in the no-SFWP group returned to sport participation 1.22 d (95% confidence interval = –0.89, –1.55 d) before reaching full symptom resolution and 7.10 d (95% confidence interval = 5.67, 8.53 d) earlier than the SFWP group. | An SFWP did not influence recovery from concussion or decrease risk of repeat injury. | 3 |
Abbreviations: BCTT, Buffalo Concussion Treadmill Test; BESS, Balance Error Scoring System; ImPACT, Immediate Post-Concussion Assessment and Cognitive Test; SAC, Standardized Assessment of Concussion; SCAT2, Sport Concussion Assessment Tool-2; SFWP, symptom-free waiting period.
Levels of evidence are based on the Oxford Centre for Evidence-Based Medicine taxonomy.17
McCrea et al58 evaluated whether a symptom-free waiting period (SFWP) affected clinical outcome and risk of repeat injury among high school and collegiate athletes. Just over 60% of patients had an SFWP, but no differences were found between groups for duration of symptoms, symptom severity score, balance score, or Standardized Assessment of Concussion score at the time of injury or 2 to 3 hours after injury. Patients in the no-SFWP group returned to sport participation approximately 1.2 days before reaching full symptom resolution and 7.1 days earlier than the SFWP group.58 No differences were noted for the rate of same-season repeat injury. The authors58 proposed that the use of an SFWP neither improved clinical outcomes nor decreased the risk of a same-season repeat concussion.
DISCUSSION
Despite the significant increase in the number of concussion studies published in medical and scientific journals since the early 2000s, some of the most important decisions regarding concussion management have been based primarily on expert opinion and consensus. In this article, we aimed to systematically review the literature and evaluate the evidence for use of rest, effectiveness of rest, use of and compliance with return-to-activity protocols, and effectiveness of return-to-activity protocols. Our main findings suggest that rest is underused by health care providers, recommendations for cognitive rest do not provide guidance for clinicians during individualized patient care, an initial period of moderate physical and cognitive rest (eg, light physical and mental activity) may improve outcomes during the acute postinjury phase, significant variability exists in the use of assessment tools and compliance with recommended return-to-activity guidelines, and additional research is needed to empirically assess the effectiveness of graded return-to-activity progressions.
The findings regarding the use of rest and compliance with published recommendations also suggest that there is a critical need for education and dissemination of information regarding best practices to community primary care providers for postinjury management and collaboration with concussion specialists and school personnel. Despite the emphasis on cognitive rest and academic adjustments in several consensus and position statements,1,4,5 authors of most of the included studies identified limited prescription of cognitive rest or academic adjustments for patients after concussion. Further, these studies highlighted deficiencies in the use of multifaceted assessments (graded symptom checklist, neuropsychological testing, and balance assessment) for return-to-play decisions.38−42 One reason for these findings may be the isolation of health care providers from other members of the concussion-management team. Effective concussion management requires a team-based approach, in which the family, medical providers, and school personnel work together to manage the patient with concussion.59 However, in some settings, there may be a disconnect because physical activity is managed independently of academic activity and communication among team members is limited.60 Strategies must be developed to educate all team members and build a collaborative network that includes a standardized approach to evaluate each patient for needed cognitive and physical rest and provide individualized recommendations based on the patient's medical history and clinical presentation. In 1 study,23 the development of a standardized evaluation and management protocol reduced the variability in the instructions provided to patients regarding return to activity and return to school.
With respect to postinjury management, clinicians need to consider balancing rest and active treatments. Although our findings in this review highlight that too much activity can hinder recovery, they also suggest that strict rest can do the same. The critical message may be that rest is important in the first 1–2 days after concussion but that moderate amounts of physical and cognitive activity, under the direction of a health care provider, may be beneficial in the recovery process. Including moderate-intensity activities may improve the psychological wellbeing of patients, especially in the athletic population.12 In patients with persistent symptoms, 1 retrospective chart review27 showed that a 2-week period of rest may be beneficial in reducing symptoms; however, light activity has also been noted to improve recovery in similar patient populations.14,61 Until additional research has identified the most effective timing and intensity of such early interventions, each clinician must determine the optimal balance of rest and activity for each patient, taking into account the patient's past medical history and current complaints. For athletic trainers, these decisions should be made in conjunction with their directing physician and in collaboration with other concussion-management team members.
Validation of the existing return-to-activity progressions is also needed. Current recommendations suggest waiting until the patient is asymptomatic and has returned to baseline on assessments of cognition and balance before beginning a progressive protocol to return to competition. Yet the literature is unclear as to what constitutes being asymptomatic or whether an earlier introduction to light activity may facilitate recovery.12 This latter point may be supported by the work of Darling et al,56 who combined the BCTT with the Zurich guidelines and the advice of those suggesting that light activity may be beneficial to recovery.29−31,36 Furthermore, some evidence supports early active exercise among patients who are otherwise slow to recover14 or those with postconcussion syndrome.61
In addition to the limited evidence supporting the return-to-activity progression, recommendations have been made to individualize the approach and take into account potential modifying factors, such as age, sex, past medical history, and comorbid conditions (eg, learning disabilities, attention-deficit/hyperactivity disorder).4,5,62 For pediatric patients, both the Concussion in Sport Group4 and the American Academy of Pediatrics2 advocate lengthening this progression by recommending that patients be asymptomatic for a longer period (eg, SFWP) before starting the graded return-to-activity progression. The American Academy of Pediatrics2 recommended a minimum of 5 days to progress through the stages to a full return to activity, with additional time built in for patients having a prolonged recovery or those with a history of concussion.
Although the graded return-to-activity progression has been accepted by most medical professionals as the standard of care for returning athletes to sport participation, this approach has not been substantiated with prospective, randomized controlled comparative-effectiveness trials of this approach on patient outcomes, return to activity, or risk of repeat injury, nor is it considered appropriate for children and adolescents.63 Only 1 research group,64—66 to date, has aimed to develop pediatric-specific protocols for return to activity and return to school. Using scoping methods, DeMatteo et al64 aimed to identify and describe the management strategies used by health care providers and the evidence supporting or refuting each strategy. The review of 400 possible articles included information from 10 studies and 3 Web sites; however, none of the guidelines were specific to the younger population. As a result of these findings, follow-up studies using the National Institute of Health and Care Excellence procedures were conducted to develop pediatric-specific return-to-activity66 and return-to-school65 protocols. These protocols take a more conservative approach, strive to find a balance between allowing the brain to heal and addressing the need to participate in some activity, and emphasize that different pathways are likely required during the recovery process.66 After the development of the protocols, pilot testing was conducted with health care providers, and all strongly agreed that using the protocol changed their clinical practice, increased their knowledge, and enhanced their confidence in treating children with concussion.66 Similar findings were noted among health care providers who pilot tested the return-to-school protocol: 95% strongly agreed that the protocol gave specific and clear directions for applying the recommendations, 80% indicated that it increased their knowledge, and 85% strongly agreed that their confidence in managing children with concussion improved.65 These findings are positive and demonstrate a more evidence-based approach to developing return-to-activity progressions, but future authors needs to empirically evaluate how these approaches affect patient outcomes before protocols such as these are used routinely in clinical practice.
FUTURE RESEARCH DIRECTIONS
Additional research is warranted to determine the effectiveness of rest, treatment, and returning to activity. The literature and clinical practice would benefit from multisite comparative-effectiveness studies to evaluate the timing, duration, and levels of rest compared with other active treatments. In addition, studies evaluating the effectiveness of the graded return-to-activity progression are needed to provide clinicians with additional information with which to manage patients with concussion. Lastly, studies of knowledge translation for primary care providers are needed. Most of the studies evaluating rest were done in concussion specialty clinics under the supervision of concussion specialists. However, most young patients are evaluated and treated in emergency department or urgent care clinics or by their pediatrician or primary care provider. Efforts are required to disseminate best-practice information regarding rest and return to activity to those providers and evaluate how that knowledge affects patient care.
LIMITATIONS
This systematic review is not without limitations. Because of the descriptive nature of most of the included studies, we did not evaluate the risk of bias. In addition, because of the small numbers of studies included, we were unable to find any studies specifically investigating the effectiveness of the graded return-to-activity progression or differentiating findings based on age or sex. Although we were able to include 40 studies in this review, only 6 were considered level 2 evidence (RCTs or inception cohort studies); of the rest, 29 studies were considered level 3 (nonrandomized cohort or follow-up study), and 5 were level 4 (case control or case series). It is important for clinicians to understand the effect of level of evidence on the ability to assign a strength of recommendation. The findings from studies with lower levels of evidence need to be evaluated cautiously before they are used regularly in clinical practice. Furthermore, the limited number of studies included did not allow us to evaluate the outcomes by setting (emergency department versus clinic) or timing after concussion, which may significantly alter how this information is used for clinical decision making in various environments.
CONCLUSIONS
This systematic review presents a descriptive analysis of the use and effectiveness of rest and return to activity after sport-related concussion. Specifically, physical rest and cognitive rest were underused by health care providers (strength of recommendation = B), moderate physical and cognitive rest may facilitate recovery during the initial days after concussion (strength of recommendation = B), significant variability exists in the use of assessment tools and compliance with recommended return-to-activity guidelines (strength of recommendation = B), and little evidence supports the effectiveness of the graded return-to-activity progression (strength of recommendation = D). High-quality, prospective studies evaluating the influence of rest, early light exercise, and other treatment options are needed to provide an evidence-based road map for managing patients with sport-related concussion. Until additional research has been published, it is prudent for clinicians to approach concussion management and return to activity in a conservative manner that evaluates the clinical presentation and the needs of each patient.
ACKNOWLEDGMENTS
We thank Casey Erickson, ATC, and Krista Hixson, ATC, for their assistance in organizing the search results for this manuscript.
REFERENCES
- 1. Halstead ME, McAvoy K, Devore CD, Carl R, Lee M, Logan K. . Returning to learning following a concussion. Pediatrics. 2013; 132 5: 948– 957. [DOI] [PubMed] [Google Scholar]
- 2. Halstead ME, Walter KD. . American Academy of Pediatrics. Clinical report−sport-related concussion in children and adolescents. Pediatrics. 2010; 126 3: 597– 615. [DOI] [PubMed] [Google Scholar]
- 3. Giza CC, Kutcher JS, Ashwal S, et al. . Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013; 80 24: 2250– 2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McCrory P, Meeuwisse W, Aubry M, et al. . Consensus statement on concussion in sport—the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Clin J Sport Med. 2013; 23 2: 89– 117. [DOI] [PubMed] [Google Scholar]
- 5. Broglio SP, Cantu RC, Gioia GA, et al. . National Athletic Trainers' Association position statement: management of sport concussion. J Athl Train. 2014; 49 2: 245– 265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Diaz AL, Wyckoff LJ. . NASN position statement: concussions—the role of the school nurse. NASN Sch Nurse. 2013; 28 2: 110– 111. [DOI] [PubMed] [Google Scholar]
- 7. Harmon KG, Drezner JA, Gammons M, et al. . American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013; 47 1: 15– 26. [DOI] [PubMed] [Google Scholar]
- 8. Giza CC, Hovda DA. . The new neurometabolic cascade of concussion. Neurosurgery. 2014; 75 suppl 4: S24– S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Guskiewicz KM, McCrea M, Marshall SW, et al. . Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA concussion study. JAMA. 2003; 290 19: 2549– 2555. [DOI] [PubMed] [Google Scholar]
- 10. Cantu RC, Gean AD. . Second-impact syndrome and a small subdural hematoma: an uncommon catastrophic result of repetitive head injury with a characteristic imaging appearance. J Neurotrauma. 2010; 27 9: 1557– 1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Saunders RL, Harbaugh RE. . The second impact in catastrophic contact-sports head trauma. JAMA. 1984; 252 4: 538– 539. [PubMed] [Google Scholar]
- 12. Silverberg ND, Iverson GL. . Is rest after concussion “the best medicine?”: recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil. 2013; 28 4: 250– 259. [DOI] [PubMed] [Google Scholar]
- 13. Valovich McLeod TC, Gioia GA. Cognitive rest: the often neglected aspect of concussion management. Athl Ther Today. 2010; 15 2: 1– 3. [Google Scholar]
- 14. Gagnon I, Galli C, Friedman D, Grilli L, Iverson GL. . Active rehabilitation for children who are slow to recover following sport-related concussion. Brain Inj. 2009; 23 12: 956– 964. [DOI] [PubMed] [Google Scholar]
- 15. Alsalaheen BA, Mucha A, Morris LO, et al. . Vestibular rehabilitation for dizziness and balance disorders after concussion. J Neurol Phys Ther. 2010; 34 2: 87– 93. [DOI] [PubMed] [Google Scholar]
- 16. Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009; 151 4: W65– W94. [DOI] [PubMed] [Google Scholar]
- 17. OCEBM levels of evidence. Centre for Evidence-Based Medicine Web site. http://www.cebm.net/ocebm-levels-of-evidence. Accessed March 18, 2016. [Google Scholar]
- 18. Arbogast KB, McGinley AD, Master CL, Grady MF, Robinson RL, Zonfrillo MR. . Cognitive rest and school-based recommendations following pediatric concussion: the need for primary care support tools. Clin Pediatr (Phila). 2013; 52 5: 397– 402. [DOI] [PubMed] [Google Scholar]
- 19. Upchurch C, Morgan CD, Umfress A, Yang G, Riederer MF. . Discharge instructions for youth sports-related concussions in the emergency department, 2004 to 2012. Clin J Sport Med. 2015; 25 3: 297– 299. [DOI] [PubMed] [Google Scholar]
- 20. Zemek R, Eady K, Moreau K, et al. . Canadian pediatric emergency physician knowledge of concussion diagnosis and initial management. CJEM. 2015; 17 2: 115– 122. [DOI] [PubMed] [Google Scholar]
- 21. Carson JD, Lawrence DW, Kraft SA, et al. . Premature return to play and return to learn after a sport-related concussion: physician's chart review. Can Fam Physician. 2014; 60(6):E310, E312−E315. [PMC free article] [PubMed] [Google Scholar]
- 22. Grubenhoff JA, Deakyne SJ, Comstock RD, Kirkwood MW, Bajaj L. . Outpatient follow-up and return to school after emergency department evaluation among children with persistent post-concussion symptoms. Brain Inj. 2015. May 25: 1– 6. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wilkins SA, Shannon CN, Brown ST, et al. . Establishment of a multidisciplinary concussion program: impact of standardization on patient care and resource utilization. J Neurosurg Pediatr. 2014; 13 1: 82– 89. [DOI] [PubMed] [Google Scholar]
- 24. Weber ML, Welch CE, Parsons JT, . Valovich McLeod TC. School nurses' familiarity and perceptions of academic accommodations for student-athletes following sport-related concussion. J Sch Nurs. 2015; 31 2: 146– 154. [DOI] [PubMed] [Google Scholar]
- 25. Olympia RP, Ritter JT, Brady J, Bramley H. . Return to learning after a concussion and compliance with recommendations for cognitive rest. Clin J Sport Med. 2016; 26 2: 115– 119. [DOI] [PubMed] [Google Scholar]
- 26. Williams RM, Welch CE, Parsons JT, McLeod TC. . Athletic trainers' familiarity with and perceptions of academic accommodations in secondary school athletes after sport-related concussion. J Athl Train. 2015; 50 3: 262– 269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moser RS, Glatts C, Schatz P. . Efficacy of immediate and delayed cognitive and physical rest for treatment of sports-related concussion. J Pediatr. 2012; 161 5: 922– 926. [DOI] [PubMed] [Google Scholar]
- 28. Moser RS, Schatz P, Glenn M, Kollias KE, Iverson GL. . Examining prescribed rest as treatment for adolescents who are slow to recover from concussion. Brain Inj. 2015; 29 1: 58– 63. [DOI] [PubMed] [Google Scholar]
- 29. Majerske CW, Mihalik JP, Ren D, et al. . Concussion in sports: postconcussive activity levels, symptoms, and neurocognitive performance. J Athl Train. 2008; 43 3: 265– 274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Brown NJ, Mannix RC, O'Brien MJ, Gostine D, Collins MW, Meehan WP. . Effect of cognitive activity level on duration of post-concussion symptoms. Pediatrics. 2014; 133 2: E299– E304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Maerlender A, Rieman W, Lichtenstein J, Condiracci C. . Programmed physical exertion in recovery from sports-related concussion: a randomized pilot study. Dev Neuropsychol. 2015; 40 5: 273– 278. [DOI] [PubMed] [Google Scholar]
- 32. Gibson S, Nigrovic LE, O'Brien M, Meehan WP. . The effect of recommending cognitive rest on recovery from sport-related concussion. Brain Inj. 2013; 27 7−8: 839– 842. [DOI] [PubMed] [Google Scholar]
- 33. Buckley TA, Munkasy BA, Clouse BP. . Acute cognitive and physical rest may not improve concussion recovery time. J Head Trauma Rehabil. 2016; 31 4: 233– 241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Moor HM, Eisenhauer RC, Killian KD, et al. . The relationship between adherence behaviors and recovery time in adolescents after a sports-related concussion: an observational study. Int J Sports Phys Ther. 2015; 10 2: 225– 233. [PMC free article] [PubMed] [Google Scholar]
- 35. de Kruijk JR, Leffers P, Meerhoff S, Rutten J, Twijnstra A. . Effectiveness of bed rest after mild traumatic brain injury: a randomised trial of no versus six days of bed rest. J Neurol Neurosurg Psychiatry. 2002; 73 2: 167– 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Thomas DG, Apps JN, Hoffmann RG, McCrea M, Hammeke T. . Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics. 2015; 135 2: 213– 223. [DOI] [PubMed] [Google Scholar]
- 37. Boden BP, Griffin LY, Garrett WE. . Etiology and prevention of noncontact ACL injury. Phys Sportsmed. 2000; 28 4: 53– 60. [DOI] [PubMed] [Google Scholar]
- 38. Lynall RC, Laudner KG, Mihalik JP, Stanek JM. . Concussion-assessment and -management techniques used by athletic trainers. J Athl Train. 2013; 48 6: 844– 850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Notebaert AJ, Guskiewicz KM. . Current trends in athletic training practice for concussion assessment and management. J Athl Train. 2005; 40 4: 320– 325. [PMC free article] [PubMed] [Google Scholar]
- 40. Covassin T, Elbin R, Stiller-Ostrowski JL. . Current sport-related concussion teaching and clinical practices of sports medicine professionals. J Athl Train. 2009; 44 4: 400– 404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Buckley TA, Burdette G, Kelly K. . Concussion-management practice patterns of National Collegiate Athletic Association Division II and III athletic trainers: how the other half lives. J Athl Train. 2015; 50 8: 879– 888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kelly KC, Jordan EM, Joyner AB, Burdette GT, Buckley TA. . National Collegiate Athletic Association Division I athletic trainers' concussion-management practice patterns. J Athl Train. 2014; 49 5: 665– 673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lebrun CM, Mrazik M, Prasad AS, et al. . Sport concussion knowledge base, clinical practises and needs for continuing medical education: a survey of family physicians and cross-border comparison. Br J Sports Med. 2013; 47 1: 54– 59. [DOI] [PubMed] [Google Scholar]
- 44. Broshek DK, Samples H, Beard J, Goodkin HP. . Current practices of the child neurologist in managing sports concussion. J Child Neurol. 2014; 29 1: 17– 22. [DOI] [PubMed] [Google Scholar]
- 45. Gordon KE, Do MT, Thompson W, McFaull S. . Concussion management by paediatricians: a national survey of Canadian paediatricians. Brain Inj. 2014; 28 3: 311– 317. [DOI] [PubMed] [Google Scholar]
- 46. Kinnaman KA, Mannix RC, Comstock RD, Meehan WP. . Management of pediatric patients with concussion by emergency medicine physicians. Pediatr Emerg Care. 2014; 30 7: 458– 461. [DOI] [PubMed] [Google Scholar]
- 47. Hunt TN, Trombley A. . Physician management of sport-related concussions at the collegiate level. Athl Train Sports Health Care. 2010; 2 5: 227– 234. [Google Scholar]
- 48. Baugh CM, Kroshus E, Daneshvar DH, Filali NA, Hiscox MJ, Glantz LH. . Concussion management in United States college sports: compliance with National Collegiate Athletic Association concussion policy and areas for improvement. Am J Sports Med. 2015; 43 1: 47– 56. [DOI] [PubMed] [Google Scholar]
- 49. Kroshus E, Baugh CM, Daneshvar DH, Stamm JM, Laursen RM, Austin SB. . Pressure on sports medicine clinicians to prematurely return collegiate athletes to play after concussion. J Athl Train. 2015; 50 9: 944– 951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Meehan WP, d'Hemecourt P, Comstock RD. . High school concussions in the 2008−2009 academic year: mechanism, symptoms, and management. Am J Sports Med. 2010; 38 12: 2405– 2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. De Maio VJ, Joseph DO, Tibbo-Valeriote H, et al. . Variability in discharge instructions and activity restrictions for patients in a children's ED postconcussion. Pediatr Emerg Care. 2014; 30 1: 20– 25. [DOI] [PubMed] [Google Scholar]
- 52. Haran HP, Bressan S, Oakley E, Davis GA, Anderson V, Babl FE. . On-field management and return-to-play in sports-related concussion in children: are children managed appropriately? J Sci Med Sport. 2016; 19 3: 194– 199. [DOI] [PubMed] [Google Scholar]
- 53. Hollis SJ, Stevenson MR, McIntosh AS, Shores EA, Finch CF. . Compliance with return-to-play regulations following concussion in Australian schoolboy and community rugby union players. Br J Sports Med. 2012; 46 10: 735– 740. [DOI] [PubMed] [Google Scholar]
- 54. Sarsfield MJ, Morley EJ, Callahan JM, Grant WD, Wojcik SM. . Evaluation of emergency medicine discharge instructions in pediatric head injury. Pediatr Emerg Care. 2013; 29 8: 884– 887. [DOI] [PubMed] [Google Scholar]
- 55. Echlin PS, Tator CH, Cusimano MD, et al. . Return to play after an initial or recurrent concussion in a prospective study of physician-observed junior ice hockey concussions: implications for return to play after a concussion. Neurosurg Focus. 2010; 29 5: E5. [DOI] [PubMed] [Google Scholar]
- 56. Darling SR, Leddy JJ, Baker JG, et al. . Evaluation of the Zurich Guidelines and exercise testing for return to play in adolescents following concussion. Clin J Sport Med. 2014; 24 2: 128– 133. [DOI] [PubMed] [Google Scholar]
- 57. Chermann JF, Klouche S, Savigny A, Lefevre N, Herman S, Bohu Y. . Return to rugby after brain concussion: a prospective study in 35 high level rugby players. Asian J Sports Med. 2014; 5 4: E24042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. McCrea M, Guskiewicz K, Randolph C, et al. . Effects of a symptom-free waiting period on clinical outcome and risk of reinjury after sport-related concussion. Neurosurgery. 2009; 65 5: 876– 882, discussion 882−883. [DOI] [PubMed] [Google Scholar]
- 59. Valovich McLeod TC, Houston MN, Welch CE. A pediatric perspective on sport-related concussion. Kinesiol Rev. 2015; 4 2: 131– 155. [Google Scholar]
- 60. Sleight AJ, . Valovich McLeod TC, Kay ME, Erickson CD, Welch CE. Athletic trainers' perceived challenges toward the implementation of academic accommodations for student-athletes following a sport-related concussion in the secondary school setting [abstract]. J Athl Train. 2015; 50 suppl 6: S247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Leddy JJ, Kozlowski K, Donnelly JP, Pendergast DR, Epstein LH, Willer B. . A preliminary study of subsymptom threshold exercise training for refractory post-concussion syndrome. Clin J Sport Med. 2010; 20 1: 21– 27. [DOI] [PubMed] [Google Scholar]
- 62. Makdissi M, Davis G, Jordan B, Patricios J, Purcell L, Putukian M. . Revisiting the modifiers: how should the evaluation and management of acute concussions differ in specific groups? Br J Sports Med. 2013; 47 5: 314– 320. [DOI] [PubMed] [Google Scholar]
- 63. Purcell L. . What are the most appropriate return-to-play guidelines for concussed child athletes? Br J Sports Med. 2009; 43 suppl 1: I51– I55. [DOI] [PubMed] [Google Scholar]
- 64. DeMatteo C, McCauley D, Stazyk K, et al. . Post-concussion return to play and return to school guidelines for children and youth: a scoping methodology. Disabil Rehabil. 2015; 37 12: 1107– 1112. [DOI] [PubMed] [Google Scholar]
- 65. DeMatteo C, Stazyk K, Giglia L, et al. . A balanced protocol for return to school for children and youth following concussive injury. Clin Pediatr (Phila). 2015; 54 8: 783– 792. [DOI] [PubMed] [Google Scholar]
- 66. DeMatteo C, Stazyk K, Singh SK, et al. . Development of a conservative protocol to return children and youth to activity following concussive injury. Clin Pediatr (Phila). 2015; 54 2: 152– 163. [DOI] [PubMed] [Google Scholar]