Abstract
Background
Several guidelines have been reported for bone-directed treatment in women with early breast cancer (EBC) for averting fractures, particularly during aromatase inhibitor (AI) therapy. Recently, a number of studies on additional fracture related risk factors, new treatment options as well as real world studies demonstrating a much higher fracture rate than suggested by randomized clinical controlled trials (RCTs). Therefore, this updated algorithm was developed to better assess fracture risk and direct treatment as a position statement of several interdisciplinary cancer and bone societies involved in the management of AI-associated bone loss (AIBL).
Patients and methods
A systematic literature review identified recent advances in the management of AIBL. Results with individual agents were assessed based on trial design, size, follow-up, and safety.
Results
Several fracture related risk factors in patients with EBC were identified. Although, the FRAX algorithm includes fracture risk factors (RF) in addition to BMD, it does not seem to adequately address the effects of AIBL. Several antiresorptive agents can prevent and treat AIBL. However, concerns regarding compliance and long-term safety remain. Overall, the evidence for fracture prevention is strongest for denosumab 60 mg s.c. every 6 months. Additionally, recent studies as well as an individual patient data meta-analysis of all available randomized trial data support additional anticancer benefits from adjuvant bisphosphonate treatment in postmenopausal women with a 34% relative risk reduction in bone metastasis and 17% relative risk decrease in breast cancer mortality that needs to be taken into account when advising on management of AIBL.
Conclusions
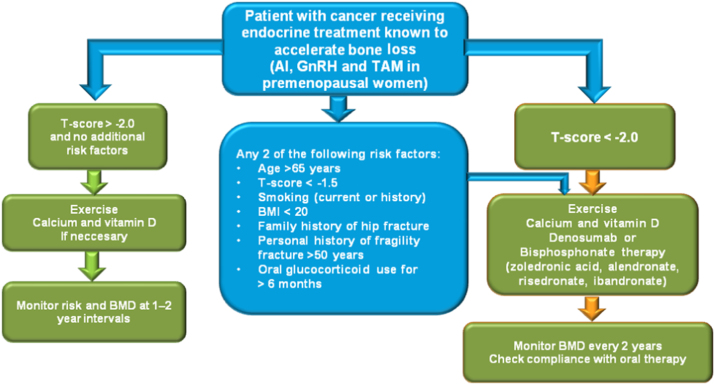
In all patients initiating AI treatment, fracture risk should be assessed and recommendation with regard to exercise and calcium/vitamin D supplementation given. Bone-directed therapy should be given to all patients with a T-score<−2.0 or with a T-score of <–1.5 SD with one additional RF, or with ≥2 risk factors (without BMD) for the duration of AI treatment. Patients with T-score>−1.5 SD and no risk factors should be managed based on BMD loss during the first year and the local guidelines for postmenopausal osteoporosis. Compliance should be regularly assessed as well as BMD on treatment after 12 - 24 months. Furthermore, because of the decreased incidence of bone recurrence and breast cancer specific mortality, adjuvant bisphosphonates are recommended for all postmenopausal women at significant risk of disease recurrence.
Keywords: Breast cancer, Osteoporosis, Endocrine treatment, Fracture, Bisphosphonate, Denosumab
1. Introduction
Breast cancer is the most frequent cancer in women leading to a significant morbidity and mortality [1]. Early diagnosis and improved treatment regimens have significantly increased survival leading to a greater potential for experiencing long term side effects from cancer treatments including bone loss and fractures. Skeletal homeostasis is achieved through coupled and balanced bone resorption and bone formation. Several local and systemic factors regulate these processes, including estrogen, a key regulator of bone resorption. Physiologic decreases in estrogen levels after menopause lead to an increased risk for osteoporosis (low bone mineral density [BMD]) and fractures, and this risk can be exacerbated by breast cancer and its therapies [2]. Systemic therapies for breast cancer can additionally interfere with bone turnover, either through their effects on gonadal steroid hormone production or by inhibiting peripheral aromatization into estrogen [2], [3], [4]. In addition, some therapies for breast cancer might directly affect bone formation [5]. Regardless of the underlying mechanism, patients with breast cancer are at risk for cancer treatment-induced bone loss (CTIBL).
The majority of breast malignancies are hormone responsive, and adjuvant endocrine therapy is used routinely to prevent breast cancer recurrence and death [6], [7]. Tamoxifen was the past treatment of choice for endocrine-responsive postmenopausal breast cancer and was found to preserve BMD in postmenopausal (but not premenopausal) women [8], and fracture risks remained similar in postmenopausal tamoxifen users and non-users [9]. However, aromatase inhibitors (AI) have now replaced tamoxifen as the treatment of choice for hormone-responsive breast cancer in most postmenopausal women because of both better efficacy and fewer serious side effects such as induction of uterine cancers and thromboembolic events.[6], [7], [10], [11] However, because AIs prevent peripheral estrogen production, they suppress estrogen levels beyond that attained from a natural menopause, thereby leading to accelerated bone loss and an increased fracture risk [12], [13], [14], [15].
Besides a reduction in quality of life, increased morbidity and treatment induced fractures lead to an increase in the health economic burden. A recent study reported that compared to the general population, breast cancer patients had fracture incidence rate ratios of 1.25 (95% CI: 1.23–1.28) and 1.18 (95% CI: 1.14–1.22) for hospitalization due to any bone fracture and hip fracture, respectively. These ratios remained significantly increased for 10 years. Women taking aromatase inhibitors were at an increased risk of fracture as compared with women taking tamoxifen (HR 1.48; 95% CI: 0.98–2.22). Additionally, breast cancer patients hospitalized for a bone fracture showed a higher risk of death (HR 1.83; 95% CI: 1.50–2.22) compared with those without bone fracture [16].
1.1. What is the size of the problem?
AI-associated bone loss (AIBL) leads to a marked increase of bone resorption, with a 2–4 fold increased bone loss compared to physiologic postmenopausal BMD loss.[12], [15], [17], [18], [19], [20], [21], [22], [23], [24] As a result, women receiving adjuvant AI therapy for breast cancer are at increased risk for fractures [25], [26], [27], [28], which leads to increased morbidity and mortality [29]. Randomized controlled trials (RCTs) including an AI for 5 years suggested an increased absolute fracture risk of around 10% indicating that one out of ten women will eventually fracture [25], [26], [27], [28]. However, these studies had stringent inclusion and exclusion criteria that may not reflect fracture risk in the unselected population seen in routine clinical practice. The real-world fracture risk has been investigated in a number of case-control studies, prescription based analysis as well as single center studies and even in a recent RCT. In the latter, the fracture incidence in women with BC on an AI was reported to be around 18–20% after 5 years follow-up indicating that in clinical practice, about one in five women will sustain an AI related fracture [30], [31], [32], [33], [34], [35], [36], [37], [38]. After termination of AI treatment, bone turnover normalizes, BMD and fracture risk can partially recover [25], [26], [27], [28]. Recently, conflicting evidence on the increased duration of AI treatment for up to 10 years has been reported [39], [40], [41], [42]. For those advocating an increased duration of AI treatment for up to 10 years, a further increased fracture risk, adding to the 2–3% per annum has to be taken into account.
1.2. How to assess osteoporosis related fracture risk
In 1993, the first operational definition of osteoporosis was based on a decreased in BMD eg. a T-score at the femur neck of <−2.5 [43], [44]. In the past years, we have accumulated an expanded understanding of fracture risk factors other than BMD [5], [45], resulting in several national and international bone health guidelines being updated to provide more comprehensive insights into fracture risk assessment and clinical decision making regarding antiresorptive therapy (Table 1) [5], [6], [11], [46], [47], [48], [49], [50], [51], [52], [53] A key advance in this field has been the development of the FRAX algorithm developed by the former WHO Collaborating Center at Sheffield, UK (http://www.sheffield.ac.uk/FRAX/), an easy-to-use online tool for assessing fracture risk in postmenopausal women with or without BMD data. The FRAX algorithm is based on data from large-scale, population-based cohorts from different parts of the world, and uses factors such as age, body mass index (BMI), smoking history, personal and family history of fracture, smoking, glucocorticoid use, and secondary causes of osteoporosis, to assess long-term fracture risk. However, FRAX is not designed to assess fracture risk in women with breast cancer, and indeed may substantially underestimate the effect of AI therapy—the “secondary osteoporosis” option in the FRAX tool has a much smaller effect on fracture risk than would be expected for AI therapy. Moreover, as clinical trials comparing AIs with tamoxifen mature, it is evident that AIs have a large effect on acute fracture risk during active treatment [26], [27], which might be underestimated by FRAX, an algorithm designed to provide long-term (10-year) fracture risk. As it appears that the independent fracture risk in AIBL is equivalent to that seen in RA, it has recently been suggested to use the bypass of rheumatoid arthritis in FRAX as it has been proposed in type 2 diabetes [54].
Table 1.
| Source | Whom to treat | Antiresorptive | Dose | Duration of treatment |
|---|---|---|---|---|
| ESMO [5] | All women receiving AI therapy with ≥1 of the following T-score ≤ –2.0. Any 2 of the following risk factors T-score < –1.5, age >65 yr, low BMI (<20 kg/m2), family history of hip fracture, personal history of fragility fracture after age 50, oral corticosteroid use >6 mo, and smoking | Zoledronate | 4 mg IV q6mo | As long as AI therapy |
| Denosumab | ||||
| 60 mg SC q6mo | As long as AI therapy | |||
| SIOG [5] | ||||
| ASCO [48] | Women with T-score ≤ –2.5 | Alendronate | Not given | Not given |
| Women with T-score between –1.0 and –2.5 should receive individualized therapy | Risedronate | |||
| Zoledronate | ||||
| St. Gallen [6] | No treatment for women with normal BMD | — | — | — |
| UK Expert Group [49] | Premenopausal women with ovarian suppression/failure and ≥1 of the following | Alendronate | 70 mg/wk | Follow-up at 2 yr to reassess |
| Risedronate | 35 mg/wk | |||
| AI therapy and T-score < –1.0 | Ibandronate | 150 mg PO/mo or 3 mg IV q 3 mo | ||
| T-score < –2.0 | Zoledronate | |||
| Vertebral fracture | ||||
| Annual bone loss >4% at LS or TH | 4 mg IV q6mo | |||
| Postmenopausal women receiving AI therapy with ≥1 of the following | Alendronate | 70 mg/wk | Follow-up at 2 yr to reassess | |
| T-score < –2.0 | Risedronate | 35 mg/wk | ||
| Vertebral fracture | Ibandronate | 150 mg PO/mo or 3 mg IV q 3 mo | ||
| Annual bone loss > 4% at LS or TH | Zoledronate | |||
| 4 mg IV q6mo | ||||
| Belgian Bone Club [47] | Women with T-score < –2.5 or history of fragility fracture | Zoledronate Other BPs may be considered | 4 mg IV q6mo | As long as AI therapy |
| Women with T-score between –1.0 and –2.5 plus other risk factors | ||||
| International Expert Group (Hadji et al.) [5] | All women receiving AI therapy with ≥1 of the following T-score ≤ –2.0. Any 2 of the following risk factors T-score < –1.5, age >65 yr, low BMI (<20 kg/m2), family history of hip fracture, personal history of fragility fracture after age 50, oral corticosteroid use >6 mo, and smoking | Zoledronate | 4 mg IV q6mo | At least 2 yr, possibly as long as AI therapy |
| International Expert Panel (Aapro et al.) [46] | Women with ≥2 of the following risk factors: AI use, T-score < –1.5, age >65 yr, corticosteroid use >6 mo, family history of hip fracture, personal history of fragility fracture after age 50; T-score < –2.0 | Zoledronate | 4 mg IV q6mo | As long as AI therapy |
| ESCEO position paper | All women receiving AI therapy with (T-score hip/spine <−2.5 or ≥1 prevalent fragility fracture), to women aged ≥75 irrespective of BMD, and to patients with T-score <−1.5+≥1clinical risk factor or T-score <−1.0+≥2 clinical risk factors or FRAX-determined 10-year hip fracture probability ≥3% | Zoledronate Denosumab s.c., or possibly oral BP | 4 mg IV q6mo 60 mg s.c. q6mo | As long as AI therapy |
| (Rizzoli et al.) [50] |
Abbreviations: AI, aromatase inhibitor; ASCO, American Society of Clinical Oncology; BMD, bone mineral density; BMI, body mass index; BP, bisphosphonate; GnRH, gonadotropin-releasing hormone; IV, intravenous; LS, lumbar spine; mo, month; NCCN, National Comprehensive Cancer Network; PO, oral; q, every; TH, total hip; UK, United Kingdom; wk, week; yr, year.
Limited evidence for the use of other agents was available when these guidelines were written.
Calcium and vitamin D supplements are to be used in conjunction with BPs, and exercise when appropriate is recommended by most panels.
With regard to AIBL, a retrospective, case-controlled study in 402 postmenopausal women with newly diagnosed breast cancer demonstrated that using a combination of BMD and clinical risk factors identified more than 28% of these women as candidates for bone-directed therapy, compared with less than 10% identified by BMD criteria alone [55]. Additionally, Neuner et al. [56] reported that age and BMI were particularly associated with an increased hip fracture risk in women with breast cancer.
1.3. Additional anticancer benefits of adjuvant bisphosphonates
In past years, a large number of clinical trials investigating the use of antiresorptive agents, such as bisphosphonates and denosumab (a monoclonal antibody against the receptor activator of nuclear factor kappa B ligand [RANKL]), for the prevention and/or treatment of AIBL have been reported.
Population-based case-control studies suggest that oral bisphosphonate treatment for postmenopausal osteoporosis may reduce the incidence of invasive breast cancers [57], [58], [59]. Moreover, phase II studies have demonstrated direct anticancer effects of zoledronate on disseminated tumor cells in the bone marrow of patients with early breast cancer [60], [61], [62], [63], and subset analyses from ongoing trials show that the addition of zoledronate to neo-adjuvant chemotherapy can reduce residual tumor size and improve pathologic response rates compared with chemotherapy alone [64].
Early trials of adjuvant bisphosphonates for the prevention of bone metastases in early breast cancer were promising but inconclusive [65], [66], [67], [68] This was due to the broad inclusion criteria for many of the trials; it is now clear that adjuvant bisphosphonates have no effects on breast cancer recurrence or mortality in premenopausal women with all the benefits restricted to women who are either postmenopausal or have had a menopause induced postoperatively with goserelin [69], [70],
Recently, Coleman et al. confirmed the anticancer effect of bisphosphonates in a meta-analysis conducted by the Early Breast Cancer Clinical Trials Group (EBCTCG), decreasing the incidence of bone recurrence by 34% and breast cancer specific mortality by 17% [71]. Additionally, an expert panel of oncologists and bone experts has published a consensus statement for the use of adjuvant bisphosphonates in women with BC [72]. In light of these developments, we have updated our recommendations for the prevention and treatment of AIBL in postmenopausal women with early breast cancer [5].
2. Methods
2.1. Systematic literature review
With regard to clinical prognostic risk factors for fracture in breast cancer patients, we used a recent systematic review [5]. For prevention and treatment of AIBL, we undertook PubMed® searches of MEDLINE® (National Library of Medicine, Bethesda, MD) and other databases were performed to identify clinical trials of antiresorptive agents used for the prevention and treatment of AIBL from Jul 2010 through April 2016. In addition, the Cochrane Register of Controlled Trials and databases of ongoing and unpublished trials http://www.clinicaltrials.gov were searched. Additional information was obtained from abstracts presented at international meetings including the St. Gallen Breast Cancer Conference, European Breast Cancer Conference (EBCC), San Antonio Breast Cancer Symposium (SABCS), and ASCO annual meetings and breast cancer symposia (Table 2).
Table 2.
Major trials of antiresorptive agents for prevention of aibl in postmenopausal women with breast cancer.
| Antiresorptive agent (Trial) | N | BMD data, na | Dose | Treatment duration | Follow-up, months | Mean BMD increase from baseline, % |
|
|---|---|---|---|---|---|---|---|
| LS | TH | ||||||
| Zoledronate | 1,065 | 1,065 | 4 mg q6mo | 5 yr | 36b | 4.39 | 1.9 |
| (ZO-FAST) [69] | |||||||
| Zoledronate | 602 | 602 | 4 mg q6mo | 5 yr | 61 | 6.19 | 2.57 |
| (Z-FAST) [81] | |||||||
| Zoledronate | 558 | 395 | 4 mg q6mo | 5 yr | 24 | 4.94 | 1.22 |
| (N03CC) [82] | |||||||
| Zoledronate | 527 | 527 | 4 mg q6mo | 5 yr | 36 | 5.98 | NR |
| (E-ZO-FAST) [83] | |||||||
| Denosumab | 252 | 252 | 60 mg q6mo | 2 yr | 24 | 6.2c | 3.7c |
| (HALT-BC) [84] | 3420 | 3420 | 60 mg q 6mo | 3 yr | 36 | 10,2 | 7,92 |
| Denosumab | Fracture reduction: | ||||||
| (ABCSG-18) [92], [93] | |||||||
| OR 0.53 (CI 0.333–0.85, p=0.009) | |||||||
| Risedronate | 154 | 111 | 35 mg/wk | 2 yr | 24 | 2.2 | 1.8 |
| (SABRE) [85] | |||||||
| Risedronate [86] | 87 | 87 | 35 mg/wk | 2 yr | 24 | 0.4 | 0.9 |
| Clodronate [87] | 61 | 61 | 1,600 mg/day | 3 yr | 60 | –1.0 | –0.1 |
| Risedronate (IBIS II- Stratum II) [88] | 260 | 150 | 35 mg/wk | 3 yr | 36 | 1.1 | -0.7 |
| 1410 | 903 | 35 mg/wk | 3 yr | 36 | 1,1% | -0,7% | |
| 213 | 132 | 35 mg/wk | 2 yr | 24 | 5,7% | 1,6% | |
| Risedronate | |||||||
| (IBIS II) [106] | |||||||
| Risedronate | |||||||
| (ARBI) [106] | |||||||
| Ibandronate | 131 | 50 | 150 mg/mo | 5 yr | 60 | 5.01% | 1.19% |
| (ARIBON) [89] | |||||||
| Risedronate [90] | 118 | 11 | 35 mg/wk | 1 yr | 12 | 4.1 | 1.8 |
| 303 | 303 | 70 mg/wk | 3 yr | 36 | 15.6 (osteoporosic) | 5.6 (osteoporotic) | |
| Alendronate | |||||||
| (BATMAN)[109]. | 6.3 (osteopenic) | 6.3 (osteopenic) | |||||
Abbreviations: AI, aromatase inhibitor; AIBL, aromatase inhibitor-associated bone loss; BMD, bone mineral density; LS, lumbar spine; mo, months; NR, not reported; TH, total hip; yr, years.
Number of patients randomized to bisphosphonate vs placebo and evaluable for BMD at the reported timepoint;
BMD data available for 36 months’ follow-up; disease recurrence outcomes available for 48 months’ follow-up.
Estimates based on published graph.
An evidence-based medicine approach was used to determine when to initiate antiresorptive therapy for AIBL, to determine the appropriate antiresorptive therapy, and to define follow-up/monitoring procedures. All reports were reviewed and the available data assessed for the level of evidence used to guide treatment recommendations (Table 3).
Table 3.
Summary of key clinical points and levels of evidence for adjuvant BP treatment recommendations.
| Summary of key clinical points and levels of evidence for adjuvant BP treatment recommendations |
|---|
| Prevention of AIBL |
| Postmenopausal women at low risk of recurrence |
|
|
|
|
|
|
| (BPscan include zoledronic acid (4 mg IV Q6 months) (II,A), risedronate (35 mg PO weekly) (lll,A), ibandronate (150 mg PO monthly) (IV, A) alendronate (70 mg PO weekly), (IV, A) |
| Prevention of metastases and improving disease outcomes |
| Premenopausal women on adjuvant ovarian suppression |
|
|
|
|
| Postmenopausal women at intermediate or high risk of recurrence |
|
|
|
|
Source:Adapted by Hadji et al. [72].
3. Identification of fracture risk in women with breast cancer
Several additional clinical risk factors have been validated in large, prospective, population-based studies in postmenopausal women and were previously characterized according to their impact on overall fracture risk independently of both age and BMD (Evidence level IA) [5]. Risk factors found to increase fracture risk in women with breast cancer in addition to AI therapy included, T-score <–1.5, age >65 years, low BMI (<20 kg/m2), family history of hip fracture, personal history of fragility fracture after age 50, oral corticosteroid use >6 months, rheumatoid arthritis, and smoking [73], [74], [75], [76], [77], [78], [79] (Evidence level IA). Additionally, a recent study suggests that cancer associated muscle weakness leads to increased immobility with an increased risk for osteoporosis and fracture [80]. Recent data suggest that BMD measurement alone should not be the sole criterion for determining fracture risk, and that an overall fracture risk assessment that combines risk factors provides a more accurate evaluation. It is also important to note that the use of corticosteroids at a dose of >2.5 mg prednisolone (or equivalent) daily for more than 3 months is an established risk factor based on data from non-malignant disease settings. When combined with chemotherapy regimens, the doses of oral corticosteroids are typically higher, and might negatively impact bone health over a shorter period of time. Finally, in order to identify and manage secondary causes of osteoporosis, complete baseline laboratory assessments should include serum levels of calcium, phosphate, 25-OH vitamin D, C-reactive protein, alkaline phosphatase, thyroid-stimulating hormone, and gamma-glutamyl transpeptidase; complete blood count; creatinine clearance; and protein electrophoresis (serum and/or urine).
4. Selecting a treatment to prevent AIBL
Available data from randomized clinical trials in more than 6000 patients suggest that denosumab, intravenous and oral bisphosphonates can effectively prevent AIBL in patients with breast cancer (Table 2) [69], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90]. Although the majority of these trials were not designed with a fracture prevention endpoint, data from the osteoporosis setting support the use of BMD improvements as a surrogate for fracture prevention [91]. Therefore, data from these large RCTs may be considered level II evidence for preserving skeletal health during AI therapy.
4.1. Denosumab
4.1.1. Level of evidence: I
The Adjuvant Denosumab in Breast Cancer Trial (ABCSG-18) is the only study to have fracture incidence as the primary endpoint and was adequately powered to investigate the effect on fracture risk [31]. The trial compared adjuvant denosumab (60 mg s.c. twice yearly) with placebo in 3425 postmenopausal women receiving adjuvant AI and calcium and Vitamin D if warranted [92], [93]. Postmenopausal women with hormone receptor positive breast cancer treated with denosumab had a significant risk reduction of any clinical fracture (hazard ratio [HR] 0.50 [95% CI 0.39–0·65], p<0.0001). Denosumab treatment furthermore significantly decreased the number of incident morphometric vertebral fractures and worsening of prevalent vertebral fractures over 36 months (odds ratio 0.54 [95% CI 0.34–0·84], p=0.007). The fracture risk reduction appeared to be irrespective of age and baseline BMD. As a result, study patients were offered optional unblinding so that women in the placebo group could receive denosumab.
The total number of adverse events did not differ between the groups. Specifically, the risk for osteonecrosis of the jaw (ONJ) was monitored proactively and no case out of 31 suspected cases met the diagnostic criteria. This result contrasts with reports from trials of monthly denosumab 120 mg in the metastatic setting, which revealed an ONJ risk of around 1% per year on treatment that is similar to the ONJ risk during long term 3–4 weekly IV bisphosphonate therapy [94], [95], [96]. Preventive dental care and the use of antibiotics during dental procedures to minimize ONJ risk are recommended for all patients initiating denosumab treatment. Further long-term safety data are warranted to fully elucidate ONJ risks with six monthly denosumab in the AIBL setting. After discontinuation of denosumab treatment, a rebound effect has been reported leading to an increase of markers of bone turnover exceeding baseline levels as well an accelerated BMD loss [97], [98]. Recently, several case reports describe multiple vertebral fractures after treatment cessation of denosumab. Therefore, a sequential treatment with an i.v. bisphosphonate after stopping denosumab has been proposed [99], [100].
4.2. IV bisphosphonates
4.2.1. Level of evidence: II
The data supporting IV bisphosphonate therapy to prevent AIBL in postmenopausal women with early breast cancer comes predominantly from 4 independent studies with a total of more than 2700 postmenopausal women with early breast cancer (Table 2) [69], [81], [82], [83]. The 3 companion Zometa®-Femara® Adjuvant Synergy Trials (Z-FAST, N =602; ZO-FAST, N=1065; E-ZO-FAST, N=527) compare the efficacy of zoledronate (4 mg IV q6mo) given in conjunction with AI therapy (immediate group), or after a BMD decrease to a T-score <–2.0 at any side or a non-traumatic fracture (delayed group) [69], [81], [83]. The final 61-month update from Z-FAST showed that delaying zoledronate resulted in losses in BMD at lumbar spine (LS) and total hip (TH) (–2.42% and –4.12%, respectively; P≤0.0003 for both vs. baseline) [101]. However, patients who immediately initiated zoledronate continued to gain BMD at the lumbar spine (LS) and total hip (TH) (6.19% and 2.57%, respectively; P≤0.0003 for both vs. baseline). Similar results for the 60-month analyses of the ZO-FAST studies confirmed that immediate zoledronate not only prevented bone loss, but patients continued to gain BMD during the 5 years of therapy (Table 2) [69], [83], [102]. Women receiving immediate zoledronate gained BMD at LS and TH (4.39% and 1.6%, respectively; P<0.0001 vs. delayed group for both), versus BMD losses at both sites in the delayed zoledronate group (–5.4% and –4.2%, respectively; P<0.0001 vs. baseline for both). Similar BMD gains and losses were observed in E-ZO-FAST at 36 months’ follow-up [83].
Another trial examined the efficacy of zoledronate (4 mg IV q6mo) for preventing AIBL in postmenopausal women with endocrine-responsive breast cancer who started adjuvant letrozole after completing ≤6 years of tamoxifen treatment [82]. Similar to the BMD increases seen in the Z-FAST, ZO-FAST, and E-ZO-FAST studies, women in the N03CC (ALLIANCE) trial who received immediate zoledronate had significantly increased mean BMD at LS (3.66% at 12 months and 4.94% at 24 months) and TH (1.02% at 12 months and 1.22% at 24 months) compared with baseline (P<0.001 for all comparisons) [82]. At the 12- and 24-month post-baseline assessments, women in the delayed zoledronate group lost BMD at the LS (–1.66% and –2.28%, respectively) and TH (–1.41% and –3.34%, respectively).
None of these studies (Z-FAST, ZO-FAST, and E-ZO-FAST and NO3CC Study) were designed to show a significant difference in fracture incidence between the treatment arms [103]. Despite the absence of fracture data, the BMD data from these 4 well-designed RCTs demonstrates that zoledronate (4 mg q6mo) at initiation of AI therapy can effectively prevent AIBL in postmenopausal women.
Zoledronate given on a 6 monthly schedule appears to be very well tolerated. The most common adverse events are transient infusion-site reactions and mild flu-like symptoms with rare renal adverse events and exceptionally osteonecrosis of the jaw (ONJ). [69], [81], [82], [83].
4.3. Oral bisphosphonates
4.3.1. Level of evidence: II-III
Several randomized clinical trials have investigated the efficacy of oral bisphosphonates for preventing AIBL (Table 2) [85], [86], [87], [88], [89], [90], [104], [105]. Because of the complex trial designs of some of these studies, the numbers of patients randomized to AI therapy alone versus AI therapy plus bisphosphonate is much smaller than the overall number of patients enrolled. Therefore, the evidence for oral bisphosphonates is less robust compared to IV zoledronate.
The Study of Anastrozole with the Bisphosphonate Risedronate (SABRE) compared the efficacy of risedronate (35 mg/wk oral) versus placebo for 2 years in postmenopausal women with hormone receptor-positive early breast cancer receiving adjuvant anastrozole who also had a moderate risk of fragility fracture (n=154) [85]. At 24 months, oral risedronate significantly increased LS BMD by 2.2% and TH BMD by 1.8% versus baseline (P<0.0001 for each vs. placebo). A similar trial in postmenopausal women with breast cancer receiving AI therapy demonstrated that oral risedronate (35 mg/wk) initially improved BMD versus baseline, but only modestly increased LS BMD (0.4%) and TH BMD (0.9%) at 24 months [86]. Among women enrolled in the International Breast Cancer Intervention Study (IBIS-II) bone substudy (n=613), women with osteopenia (n =59) receiving anastrozole plus risedronate (35 mg/wk) had better LS (0.32%) and TH (0.67%) BMD compared with women receiving anastrozole alone after 36 months of follow up [88]. The 3-year results showed that risedronate could prevent bone loss over the three years at the spine although the treatment was less effective at the hip [106]. These observations are consistent with the outcome of the Arimidex Bone Mass Index Oral Bisphosphonate (ARBI) trial in which 35 mg oral risedronate weekly was added to anastrozole in osteopenic patients which led to a significant increase of lumbar spine BMD over 2 yrs of 6.6% (n=93) [106]. The most recent RCT including risedronate vs. placebo was reported by Greenspan in which, after 24 months of follow up, BMD increased more in the active treatment group compared to placebo with an adjusted difference at 24 months of 3.9% at the spine and 3.2% at the hip (both p<0.05). Additionally, the adjusted differences in bone turnover markers between the active treatment and placebo groups were 0.09±0.04 nmol/LBCE for CTX and 23.3±4.8 μg/mL for P1NP (both p<0.05). Women with greater 12-month decreases in CTX and P1NP in the active treatment group had a greater 24-month increase in spinal BMD (p<0.05) [107].
In the 60-month analysis of the Arimidex®-Bondronat® (ARIBON) study, monthly oral ibandronate (150 mg) prevented bone loss in osteopenic women (n=25) compared with placebo (n=25) and in a small number of patients with pre-existing osteoporosis (n=13) Oral ibandronate increased LS BMD by 5.01% and TH BMD by 1.19% [89], [108].
In the BATMAN study, all 303 postmenopausal women with early breast cancer (EBC) received anastrozole (1 mg daily), calcium and vitamin D weekly [109]. All osteoporotic patients received weekly alendronate (70 mg) while osteopenic patients received alendronate or placebo in accordance to a given algorithm. At three years, lumbar spine mean BMD increased (15.6%, p<0.01) in the osteoporotic group. BMD in the osteopenic group with early intervention increased at three years (6.3%, p=0.02). No significant change was seen in the late intervention group. No change was observed in those with osteopenia without alendronate. There was a significant drop in lumbar spine (−5.4%) and hip (−4.5%) mean BMD, in the normal BMD group, none of whom received alendronate [110] A second short term RCT randomly assigned patients to 5 mg of alendronate and 0.5 μg of calcitriol or placebo. After 24-week of treatment, between group differences is lumbar spine BMD was 3.0% (p<0.005). The increase in C-telopeptide after 24 weeks was significantly less in the treatment group compared with that in the placebo group (35.2±17.5% vs. 109.8±28.6%, p<0.05) [109]. In all of the studies of oral bisphosphonates, patients who did not receive a bisphosphonate experienced substantial BMD loss during AI therapy [111].
Oral bisphosphonates were generally well tolerated in these trials. However, the rigid dosing requirements for oral bisphosphonates (fasting before and after dosing, the need to remain upright after dosing, etc) have been associated with some inconvenience for patients (Table 4). Moreover, patients’ compliance and persistence with oral therapies is suboptimal, even with potentially life-saving interventions such as adjuvant endocrine therapy [112], [113]. In the case of supportive treatments such as antiresorptives, insights from the osteoporosis setting show very low long-term adherence to treatment [114]. In one study, less than 20% of patients receiving daily bisphosphonate achieved clinically relevant persistence levels over 1 year, compared with approximately 30% of patients receiving weekly bisphosphonate [115]. In this setting, non-persistence has been associated with increased fracture rates (ie, poor clinical outcomes) [116], [117]. Trends toward better compliance with less-frequent dose schedules have been reported in multiple studies in women with postmenopausal osteoporosis [118], [119], [120]. Because of the strong association between compliance and clinical outcome [119], strategies to improve patients’ compliance and persistence with oral bisphosphonate therapy are necessary to ensure benefit from these agents in the AIBL setting.
Table 4.
Comparison of antiresorptive agents.
| Agent | Advantages | Limitations | Long-term safety |
|---|---|---|---|
| Oral bisphosphonates |
|
|
|
| IV bisphosphonates (Zoledronate) |
|
|
|
| Denosumab |
|
|
|
Abbreviations: AIBL, aromatase inhibitor-associated bone loss; IV, intravenous; sc, subcutaneous.
5. Treatment and follow-up recommendations for patients receiving aromatase inhibitors
5.1. Fracture prevention
5.1.1. Level of evidence: I
5.1.1.1. Grade of recommendation: A
Our guidance for antiresorptive therapy to treat or prevent AIBL in women with early breast cancer is derived from well-designed randomized controlled studies, and is based on validated risk factors with or without BMD measurements (Evidence level 1A) (Fig. 1). All patients beginning AI therapy should be advised to exercise moderately (resistance and weight-bearing exercise). Whereas weight-bearing exercise has beneficial effects on BMD [121] (Evidence level 1A), fracture risk reduction has not been demonstrated [122], [123] (Evidence level 1A). With regard to calcium and vitamin D, the International Osteoporosis Foundation recommends a daily intake of 1200 mg calcium and 800–1000 IU vitamin D for postmenopausal women (guidelines available at www.iofbonehealth.org). Elderly women, or those with reduced physical activity and sunlight exposure, may need higher levels of these nutrients. For these high-risk for fracture individuals, the measurement of 25-OH Vitamin D levels is recommended and high dose vitamin D supplementation given if deficient [124]. For other postmenopausal women receiving AI therapy, a dose of at least 800 (and up to 2000) IU of vitamin D every day is recommended to maintain replete levels. It is important to note, that a recent meta-analysis has underlined that the use of Vitamin D+/-calcium supplementation alone has been shown to be ineffective for fracture risk prevention in women with breast cancer (Evidence level 1 A) [125].
Fig. 1.
Recommended algorithm for managing bone health in women receiving aromatase inhibitor (AI) therapy for breast cancer. *If patients experience an annual decrease in bone mineral density (BMD) of ≥10% (using the same DXA absorptiometry machine), secondary causes of bone loss such as vitamin D deficiency should be evaluated and antiresorptive therapy initiated. Use lowest T-score from 3 sites. Abbreviations: AI, aromatase inhibitor; BMD, bone mineral density; BMI, body mass index.
Adapted from Hadji et al. [5].
For patients initiating an AI treatment not receiving bisphosphonate for recurrence prevention, a BMD measurement is advised. Patients with a T-score >−2.0 and no other fracture risk factor, BMD and risk status should be reassessed after 12 months. If no adjuvant antiresorptive therapy is initiated an annual BMD decrease of ≥5–10% should trigger investigation for secondary causes of bone loss such as vitamin D deficiency etc. and an antiresorptive treatment for fracture prevention initiated. All patients initiating or receiving AI therapy with any 2 of the following risk factors should receive antiresorptive therapy: T-score <–1.5, age >65 years, low BMI (<20 kg/m2), family history of hip fracture, personal history of fragility fracture after age 50, oral corticosteroid use of >6 months, and current or history of smoking. Any patient initiating or receiving AI therapy with a T-score <–2.0 should receive antiresorptive therapy irrespective of the presence of other risk factors. Based on current evidence, subcutaneous denosumab (60 mg twice yearly) and intravenous zoledronate (4 mg q6mo) are the preferred agents for prevention and treatment of AIBL. The advantages and limitations of the different antiresorptive therapies investigated in the AIBL setting are summarized in Table 4.
For oral bisphosphonates, 35 mg risedronate/week is the bisphosphonate with the strongest evidence for prevention of AIBL. In all patients receiving oral bisphosphonate therapy, BMD should be monitored and compliance assessed every 1–2 years. Periodic assessment of bone resorption markers may offer a convenient, noninvasive measure of compliance with therapy [5], [126]. In case of poor compliance or unsatisfactory BMD changes after 1–2 years, a switch to denosumab or intravenous bisphosphonate is recommended. For patients receiving denosumab, intravenous bisphosphonates or other agents, BMD monitoring during therapy should be performed on an individualized basis and in accordance to local guidelines.
Patients receiving AIs are at elevated risk for fracture for at least the duration of AI treatment [26]. As a result, we recommend continuing antiresorptive therapy for as long as the patient is receiving an AI (up to 5–10 years). Currently, denosumab and zoledronate are the only antiresorptive agent with proven efficacy and safety in large prospective RCTs over a long duration [81], [101]. Consequently, side-effect profiles and management should be taken into account when selecting an antiresorptive agent to prevent or treat AIBL.
5.2. Disease recurrence prevention – adjuvant bisphosphonate
5.2.1. Level of evidence: I
5.2.1.1. Grade of recommendation: A
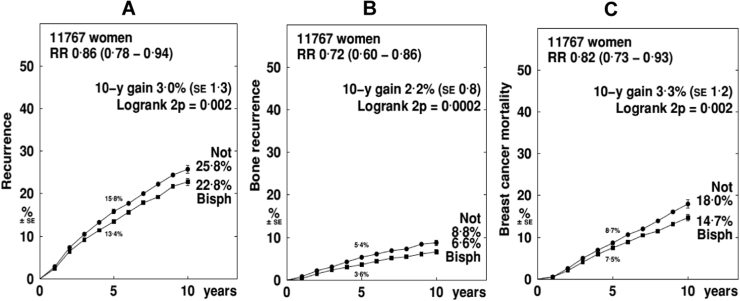
Important evidence was provided by the recent Early Breast Cancer Trialists Collaborative Group (EBCTCG) meta-analysis of data of >18,000 patients from postmenopausal breast cancer patients showing that adjuvant bisphosphonates (i.v. zoledronate, oral clodronate and oral ibandronate) reduce recurrences in bone and prolong survival in postmenopausal women [71]. Overall, despite a reduction in bone metastases, BPs had no significant effect on breast cancer recurrence (rate ratio 0.94) and the effect on breast cancer mortality, though significant, was small (RR=0.91). However, in postmenopausal women or those receiving ovarian surpression with goserelin, clinically important benefits were seen with improvements in overall breast cancer recurrence (RR=0.86), distant recurrence at any site (RR=0.82), bone recurrence (RR=0.72) and breast cancer-specific mortality (RR=0.82) (Fig. 2) (Evidence level 1A) [71]. In spite of the outstanding evidence and its magnitude it must be noted that bisphosphonates do not currently have regulatory approval for the prevention of breast cancer recurrence which currently limits the ability to prescribe these agents unless the patient fulfills the AIBL criteria for intervention.
Fig. 2.
Effects of adjuvant bisphosphonates on disease recurrence (A), bone recurrence (B) and breast cancer mortality (C) in postmenopausal women. Data from the EBCTCG meta-analysis of randomized clinical trials [72].
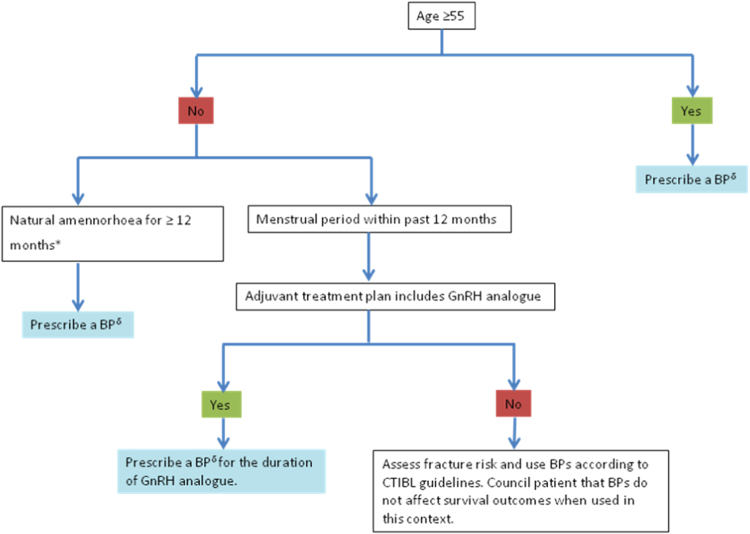
Recently, an international expert panel of oncologists and bone experts has published a consensus statement recommending the routine use of adjuvant bisphosphonates in women with BC at intermediate or significant risk for disease recurrence due to adverse clinical or biological characteristics such as node positive disease, a T2 or above, grade II/III breast tumor or disease found to be ER negative or HER-2 positive (Fig. 3) [72]. This include where available, that women with breast cancer may be recommended to receive bisphosphonates irrespective of fracture risk. In this setting, BMD monitoring may not be necessary.
Fig. 3.
*If not clinically assessable i.e. hysterectomy/IUD then ensure serum FSH is in postmenopausal range. Ensure patient is not receiving concurrent therapies that can affect the HPG axis. δInclude vitamin D 1000-2000IU and calcium 1000 mg/day.
Selection of patients suitable for adjuvant bisphosphonates to prevent metastases Adapted by Hadji et al. [72].
5.3. Disease recurrence prevention – Denosumab
5.3.1. Level of evidence: III
5.3.1.1. Grade of recommendation: C
Early disease free survival (DFS) results from the ABCSG-18 study suggest a benefit on disease recurrence with an absolute decrease in events of 2.1% at five years compared to placebo. Hereby, disease free survival was significantly improved in patients on denosumab vs. placebo HR 0.87 (CI 0.66–0.99; p<0.041) in the sensitivity analysis but not in the ITT (HR 0.816, CI 0.66–1.00; p<0.051) analysis [93]. The follow-up was too short to see effects on mortality. Further reports as of the D-CARE study results are anticipated in the next 12–18 months and will help to define the role of denosumab as a disease modifying agent.
6. Conclusions and future directions
It is evident that, in addition to BMD, clinical risk factors can greatly influence fracture risk. In addition to morbidity and mortality, fractures are associated with high healthcare costs and increased healthcare utilization for several months after fracture incidence [127], [128], [129]. In the European Union the economic burden of incident and prior fragility fractures was estimated at € 37 billion in 2010. Acute hip fracture costs in Europe were € 13,800 but varied widely from approximately €2000 in Bulgaria to about €25,000 in Denmark [130]. Additionally, vertebral and especially hip fractures are likely to result in prolonged disability and loss of independence, thereby leading to increased indirect costs. Improvements in assessing fracture risk can help identify patients who need pharmacologic intervention to improve bone health, thereby reducing fracture incidence. We have presented an evidence-based algorithm for assessing bone health in women with breast cancer and initiating antiresorptive therapy in postmenopausal women initiating AI therapy for early stage breast cancer as well as in other postmenopausal women not being considered for an AI treatment and in those receiving ovarian suppression therapies. Based on current evidence, six monthly denosumab or zoledronate for the duration of AI therapy is recommended for the prevention of AIBL in postmenopausal women receiving adjuvant AI therapy with zoledronate recommended when effects on disease recurrence are the priority and denosumab when fracture risk is the dominant concern. Long-term efficacy and safety data for other agents continue to mature, and should be taken into consideration as they become available.
In addition to the established risk factors used in our bone health algorithm, other potential fracture risk factors in women with breast cancer include chemotherapy, radiotherapy, low weight, and family history of hip fractures. Further studies examining the role of these factors are warranted. Furthermore, periodic (annual) assessment of breast cancer patients with these potential risk factors may be prudent.
Overall, data from the AIBL setting as well as long-term use in the treatment of postmenopausal osteoporosis indicate that denosumab and bisphosphonates are safe and effective agents for preserving bone health during adjuvant endocrine therapy for breast cancer. In addition, emerging anticancer benefits from bisphosphonates provide additional reasons to proactively use these agents during adjuvant AI treatment. Ongoing trials and the recent Oxford-meta analysis underlined the potential of oral and intravenous bisphosphonates and perhaps of denosumab to prevent breast cancer bone recurrence and to increase breast cancer survival. Therefore, the role of antiresorptive agents in early breast cancer has significantly been extended.
Conflicts of interest
Dr. Hadji has received honoraria, unrestricted educational grants, and research funding from the following companies: Amgen, AstraZeneca, Eli Lilly, MSD, Novartis, Pfizer and Roche.
Dr. Aapro has conducted studies and is a consultant on bone-modifying agents for Amgen, Bayer-Schering, Novartis, and Roche.
Dr. Body has received consultancy and speaker fees from Amgen.
Dr. Gnant has received institutional research support from AstraZeneca, Roche, Novartis, and Pfizer, and has received lecture fees and honoraria for participation on advisory boards from Roche, AstraZeneca, Celgene, Novartis, OBI-Pharma, and Amgen. He has served as a consultant for Accelsiors, and an immediate family member is employed by Sandoz.
Dr. Brandi served as consultant and has received grants recipient from Alexion, Abiogen, Amgen, Eli Lilly and Shire.
Dr. Reginster received consulting fees or paid advisory boards: SERVIER, IBSA-GENEVRIER, UCB, ASAHI, RADIUS HEALTH, MEDA, PIERRE FABRE. Lecture fees when speaking at the invitation of sponsor: MERCK SHARP AND DOHME, IBSA-GENEVRIER, SERVIER, DANONE, PHARMEVO, CNIEL, MEDA, DAIRY RESEARCH COUNCIL (DRC). Grant Support from Industry (All through Institution): MERCK SHARP & DOHME, AMGEN, LILLY, SERVIER, PFIZER, DANONE, MEDA, CNIEL, IBSA-GENEVRIER.
Dr. De Villiers has received honoraria, unrestricted educational grants or served as a speaker for: Adcock Ingram, Abbott, Amgen, Aspen, Bayer, MSD, Novartis and Pfizer.
Dr. Nasser Al-Daghri has no conflict of interest.
Dr. Baber has received honoraria and consultancy fees from Pfizer, Abbott and Besins.
Dr. Kanis reports grants from Amgen, grants from Lilly, non-financial support from Medimaps, grants from Unigene, non-financial support from Asahi, grants from Radius Health, other from AgNovos, outside the submitted work; and Dr. Kanis is the architect of FRAX but has no financial interest.
Dr. Zillikens has received fees for lectures and participation in advisory boards from Amgen, Eli Lilly and MSD.
Dr. Glüer on the speaker bureau for Amgen and received honoraria for lectures.
Dr. Langdahl has received fees for lectures and participation in advisory boards from Amgen, Merck, UCB, and Eli Lilly and research funding to her institution from Eli Lilly, Novo Nordisk and Amgen.
Dr. Roodman has received research funding to his institution from Novartis and Amgen.
Dr Eriksen has received fees for speaker engagement and consultancy from Eli Lilly, Novartis, Merck, Amgen, IDS and EffRx.
Dr. Nogues has received consultancy fees and speaker fees from Lilly, and Amgen.
Dr. Palacios has received honoraria or consultation fees: Pfizer, Servier, Amgen, MSD, Preglem, Gynea, Sandoz, Procare Health, Bayer, MSD, Serelys and Shiono and participated in company sponsored speaker's bureau of Servier, Pfizer, GSK, Abbott, Ferrer, Bioiberica, Shionogi, Amgen, Novo Nordisk, Teva, Bayer Healthcare, Serelys and Gedeon Richter.
Dr. Brandi has received consultancy fees and grants from Alexion, Abiogen, Amgen, Eli Lilly and Shire.
Dr. Coleman has received research funding to his institution from Bayer and Amgen.
All other authors have no conflict of interest to declaire.
References
- 1.Ginsburg O., Bray F., Coleman M.P. The global burden of women's cancers: a grand challenge in global health. Lancet. 2016 doi: 10.1016/S0140-6736(16)31392-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guise T.A. Bone loss and fracture risk associated with cancer therapy. Oncologist. 2006;11:1121–1131. doi: 10.1634/theoncologist.11-10-1121. [DOI] [PubMed] [Google Scholar]
- 3.Kim H.J., Yoon T.I., Chae H.D. Concurrent gonadotropin-releasing hormone agonist administration with chemotherapy improves neoadjuvant chemotherapy responses in young premenopausal breast cancer patients. J. Breast Cancer. 2015;18:365–370. doi: 10.4048/jbc.2015.18.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicks K.M., Fowler T.W., Akel N.S. Bone turnover across the menopause transition: the role of gonadal inhibins. Ann. N.Y. Acad. Sci. 2010;1192:153–160. doi: 10.1111/j.1749-6632.2009.05349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hadji P., Body J.J., Aapro M.S. Practical guidance for the management of aromatase inhibitor-associated bone loss. Ann. Oncol. 2008;19:1407–1416. doi: 10.1093/annonc/mdn164. [DOI] [PubMed] [Google Scholar]
- 6.Goldhirsch A., Ingle J.N., Gelber R.D. Thresholds for therapies: highlights of the St Gallen International expert consensus on the primary therapy of early breast cancer 2009. Ann. Oncol. 2009;20:1319–1329. doi: 10.1093/annonc/mdp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Winer E.P., Hudis C., Burstein H.J. American society of clinical oncology technology assessment on the use of aromatase inhibitors as adjuvant therapy for postmenopausal women with hormone receptor-positive breast cancer: status report 2004. J. Clin. Oncol. 2005;23:619–629. doi: 10.1200/JCO.2005.09.121. [DOI] [PubMed] [Google Scholar]
- 8.Bjarnason N.H., Hitz M., Jorgensen N.R., Vestergaard P. Adverse bone effects during pharmacological breast cancer therapy. Acta Oncol. 2008;47:747–754. doi: 10.1080/02841860802001467. [DOI] [PubMed] [Google Scholar]
- 9.Vestergaard P., Rejnmark L., Mosekilde L. Effect of tamoxifen and aromatase inhibitors on the risk of fractures in women with breast cancer. Calcif. Tissue Int. 2008;82:334–340. doi: 10.1007/s00223-008-9132-7. [DOI] [PubMed] [Google Scholar]
- 10.Early Breast Cancer Trialists' Collaborative G., Dowsett M., Forbes J.F. Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet. 2015;386:1341–1352. doi: 10.1016/S0140-6736(15)61074-1. [DOI] [PubMed] [Google Scholar]
- 11.Coleman R., Body J.J., Aapro M. Bone health in cancer patients: ESMO clinical practice guidelines. Ann. Oncol. 2014;25(Suppl 3):iii124–iii137. doi: 10.1093/annonc/mdu103. [DOI] [PubMed] [Google Scholar]
- 12.Hadji P. Aromatase inhibitor-associated bone loss in breast cancer patients is distinct from postmenopausal osteoporosis. Crit. Rev. Oncol. Hematol. 2009;69:73–82. doi: 10.1016/j.critrevonc.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Hadji P. Cancer treatment-induced bone loss in women with breast cancer. Bonekey Rep. 2015;4:692. doi: 10.1038/bonekey.2015.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hadji P., Asmar L., van Nes J.G. The effect of exemestane and tamoxifen on bone health within the Tamoxifen Exemestane adjuvant multinational (team) trial: a meta-analysis of the US, German, Netherlands, and Belgium sub-studies. J. Cancer Res. Clin. Oncol. 2011;137:1015–1025. doi: 10.1007/s00432-010-0964-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee S.J., Kim K.M., Brown J.K. Negative impact of aromatase inhibitors on proximal femoral bone mass and geometry in postmenopausal women with breast cancer. Calcif. Tissue Int. 2015;97:551–559. doi: 10.1007/s00223-015-0046-x. [DOI] [PubMed] [Google Scholar]
- 16.Colzani E., Clements M., Johansson A.L. Risk of hospitalisation and death due to bone fractures after breast cancer: a registry-based cohort study. Br. J. Cancer. 2016;115:1400–1407. doi: 10.1038/bjc.2016.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim W., Chung Y., Kim S.H. Increased sclerostin levels after further ablation of remnant estrogen by aromatase inhibitors. Endocrinol. Metab. (Seoul) 2015;30:58–64. doi: 10.3803/EnM.2015.30.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hadji P., Ziller M., Kieback D.G. Effects of exemestane and tamoxifen on bone health within the tamoxifen exemestane Adjuvant Multicentre (TEAM) trial: results of a German, 12-month, prospective, randomised substudy. Ann. Oncol. 2009;20:1203–1209. doi: 10.1093/annonc/mdn762. [DOI] [PubMed] [Google Scholar]
- 19.Kyvernitakis I., Rachner T.D., Urbschat A. Effect of aromatase inhibition on serum levels of sclerostin and dickkopf-1, bone turnover markers and bone mineral density in women with breast cancer. J. Cancer Res. Clin. Oncol. 2014;140:1671–1680. doi: 10.1007/s00432-014-1726-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kyvernitakis I., Knoll D., Struck M. Impact of BMI on serum estradiol and bone turnover markers in postmenopausal women with hormone-sensitive early breast cancer treated with anastrozole. J. Cancer Res. Clin. Oncol. 2014;140:159–166. doi: 10.1007/s00432-013-1557-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howell A. Adjuvant aromatase inhibitors for breast cancer. Lancet. 2005;366:431–433. doi: 10.1016/S0140-6736(05)67036-5. [DOI] [PubMed] [Google Scholar]
- 22.Coleman R.E., Banks L.M., Girgis S.I. Skeletal effects of exemestane on bone-mineral density, bone biomarkers, and fracture incidence in postmenopausal women with early breast cancer participating in the Intergroup exemestane Study (IES): a randomised controlled Study. Lancet Oncol. 2007;8:119–127. doi: 10.1016/S1470-2045(07)70003-7. [DOI] [PubMed] [Google Scholar]
- 23.Goss P.E., Ingle J.N., Martino S. Randomized trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17. J. Natl. Cancer Inst. 2005;97:1262–1271. doi: 10.1093/jnci/dji250. [DOI] [PubMed] [Google Scholar]
- 24.Coates A.S., Keshaviah A., Thurlimann B. Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1-98. J. Clin. Oncol. 2007;25:486–492. doi: 10.1200/JCO.2006.08.8617. [DOI] [PubMed] [Google Scholar]
- 25.Coleman R.E., Banks L.M., Girgis S.I. Skeletal effects of exemestane on bone-mineral density, bone biomarkers, and fracture incidence in postmenopausal women with early breast cancer participating in the Intergroup exemestane Study (IES): a randomised controlled Study. Lancet Oncol. 2007;8:119–127. doi: 10.1016/S1470-2045(07)70003-7. [DOI] [PubMed] [Google Scholar]
- 26.Forbes J.F., Cuzick J., Buzdar A. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the ATAC trial. Lancet Oncol. 2008;9:45–53. doi: 10.1016/S1470-2045(07)70385-6. [DOI] [PubMed] [Google Scholar]
- 27.Rabaglio M., Sun Z., Price K.N. Bone fractures among postmenopausal patients with endocrine-responsive early breast cancer treated with 5 years of letrozole or tamoxifen in the BIG 1-98 trial. Ann. Oncol. 2009;20:1489–1498. doi: 10.1093/annonc/mdp033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amir E., Seruga B., Niraula S. Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: a systematic review and meta-analysis. J. Natl. Cancer Inst. 2011;103:1299–1309. doi: 10.1093/jnci/djr242. [DOI] [PubMed] [Google Scholar]
- 29.Bliuc D., Nguyen N.D., Milch V.E. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301:513–521. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 30.Edwards B.J., Gradishar W.J., Smith M.E. Elevated incidence of fractures in women with invasive breast cancer. Osteoporos. Int. 2016;27:499–507. doi: 10.1007/s00198-015-3246-3. [DOI] [PubMed] [Google Scholar]
- 31.Gnant M. Denosumab and fracture risk in women with breast cancer – author's reply. Lancet. 2015;386:2057–2058. doi: 10.1016/S0140-6736(15)00975-7. (all A-i.) [DOI] [PubMed] [Google Scholar]
- 32.Edwards B.J., Raisch D.W., Shankaran V. Cancer therapy associated bone loss: implications for hip fractures in mid-life women with breast cancer. Clin. Cancer Res. 2011;17:560–568. doi: 10.1158/1078-0432.CCR-10-1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Melton L.J., 3rd, Hartmann L.C., Achenbach S.J. Fracture risk in women with breast cancer: a population-based study. J. Bone Min. Res. 2012;27:1196–1205. doi: 10.1002/jbmr.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bouvard B., Legrand E. The dilemmas of breast cancer treatment and increased fracture risk' by Malik. Ann. Oncol. 2014;25:1664–1665. doi: 10.1093/annonc/mdu222. [DOI] [PubMed] [Google Scholar]
- 35.Schimdt N., Jacob L., Coleman R. The impact of treatment compliance on fracture risk in women with breast cancer treated with aromatase inhibitors in the United Kingdom. Breast Cancer Res. Treat. 2016;155:151–157. doi: 10.1007/s10549-015-3661-3. [DOI] [PubMed] [Google Scholar]
- 36.Villa P., Lassandro A.P., Amar I.D. Impact of aromatase inhibitor treatment on vertebral morphology and bone mineral density in postmenopausal women with breast cancer. Menopause. 2016;23:33–39. doi: 10.1097/GME.0000000000000515. [DOI] [PubMed] [Google Scholar]
- 37.Chang C.H., Chen S.J., Liu C.Y. Fracture risk and adjuvant therapies in young breast cancer patients: a population-based study. PLoS One. 2015;10:e0130725. doi: 10.1371/journal.pone.0130725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brufsky A.M., Bosserman L.D., Caradonna R.R. Zoledronic acid effectively prevents aromatase inhibitor-associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: Z-FAST study 36-month follow-up results. Clin. Breast Cancer. 2009;9:77–85. doi: 10.3816/CBC.2009.n.015. [DOI] [PubMed] [Google Scholar]
- 39.Goss P.E., Ingle J.N., Pritchard K.I. Extending aromatase-inhibitor adjuvant therapy to 10 years. N. Engl. J. Med. 2016;375:209–219. doi: 10.1056/NEJMoa1604700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.V.C. VHI Tjan-Heijnen, P.G. Peer, A.C. Swinkels, C.H. Smorenburg, M. Van der Sangen, J.R. Kroep, H. De Graaf, A.H. Honkoop, F. Erdkamp, F.W. Van den Berkmortel, J.J. Kitzen, M. De Boer, W.K. De Roos, S.C. Linn, A.L. Imholz, C. Seynaeve, First results from the multicenter phase III DATA study comparing 3 versus 6 years of anastrozole after 2-3 years of tamoxifen in postmenopausal women with hormone receptor-positive early breast cancer. In Presented as an oral presentation at the SABCS on Wednesday, December 7th 2016 (S1-03), 2016.
- 41.EJvdVC Blok, E.M. Meershoek-Klein Kranenbarg, H. Putter, J. van den Bosch, E. Maartense, A.E. van Leeuwen-Stok, G.-.J. Liefers, J.W.R. Nortier, E.J.T. Rutgers, J.R. Kroep, Optimal duration of extended letrozole treatment after 5 years of adjuvant endocrine therapy; results of the randomized phase III. IDEAL trial (BOOG 2006-05). In Presented as an oral presentation at the SABCS on Wednesday, December 7th, 2016 (S1-04), 2016.
- 42.EPBH Mamounas, B.C. Lembersky, C.E. Geyer, L. Fehrenbacher, M.L. Graham, S.L. Chia, A.M. Brufsky, B.T. Hennessy, G.S. Soori, S.R. Dakil, T.E. Seay, J.L. Wade, E.C. McCarron, S. Paik, S.M. Swain, D.L. Wickerham, N. Wolmark, A randomized, double-blinded, placebo-controlled clinical trial to evaluate extended adjuvant endocrine therapy (5 years of letrozole) in postmenopausal women with hormone-receptor positive breast cancer who have completed previous adjuvant endocrine therapy: Initial results of NRG oncology/NSABP B-42. In Presented as an oral presentation at the SABCS on Wednesday, December 7th, 2016 (S1-05), 2016.
- 43.Consensus Development Conference: Diagnosis, Prophylaxis, and Treatment of Osteoporosis. Am. J. Med., vol. 94, 1993, pp. 646–650. [DOI] [PubMed]
- 44.Kanis J.A., Melton L.J., 3rd, Christiansen C. The diagnosis of osteoporosis. J. Bone Min. Res. 1994;9:1137–1141. doi: 10.1002/jbmr.5650090802. [DOI] [PubMed] [Google Scholar]
- 45.Marshall D., Johnell O., Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312:1254–1259. doi: 10.1136/bmj.312.7041.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aapro M., Abrahamsson P.A., Body J.J. Guidance on the use of bisphosphonates in solid tumours: recommendations of an international expert panel. Ann. Oncol. 2008;19:420–432. doi: 10.1093/annonc/mdm442. [DOI] [PubMed] [Google Scholar]
- 47.Body J.J., Bergmann P., Boonen S. Management of cancer treatment-induced bone loss in early breast and prostate cancer - a consensus paper of the Belgian bone Club. Osteoporos. Int. 2007;18:1439–1450. doi: 10.1007/s00198-007-0439-4. [DOI] [PubMed] [Google Scholar]
- 48.Hillner B.E., Ingle J.N., Chlebowski R.T. American Society of Clinical Oncology 2003 update on the role of bisphosphonates and bone health issues in women with breast cancer. J. Clin. Oncol. 2003;21:4042–4057. doi: 10.1200/JCO.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 49.Reid D.M., Doughty J., Eastell R. Guidance for the management of breast cancer treatment-induced bone loss: a consensus position statement from a UK Expert Group. Cancer Treat. Rev. 2008;34(Suppl 1) doi: 10.1016/j.ctrv.2008.03.007. (S3-18) [DOI] [PubMed] [Google Scholar]
- 50.Rochlitz C., Senn H.J., Betticher D. Recommendations of a swiss expert group on the use of bisphosphonates in patients with solid tumors. Swiss Med. Forum. 2010;10 (In press) [Google Scholar]
- 51.Body J.J., Terpos E., Tombal B. Bone health in the elderly cancer patient: a SIOG position paper. Cancer Treat. Rev. 2016;51:46–53. doi: 10.1016/j.ctrv.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 52.Rizzoli R., Body J.J., DeCensi A. Guidance for the prevention of bone loss and fractures in postmenopausal women treated with aromatase inhibitors for breast cancer: an ESCEO position paper. Osteoporos. Int. 2012;23:2567–2576. doi: 10.1007/s00198-011-1870-0. [DOI] [PubMed] [Google Scholar]
- 53.Van Poznak C.H., Temin S., Yee G.C. American Society of Clinical Oncology executive summary of the clinical practice guideline update on the role of bone-modifying agents in metastatic breast cancer. J. Clin. Oncol. 2011;29:1221–1227. doi: 10.1200/JCO.2010.32.5209. [DOI] [PubMed] [Google Scholar]
- 54.Leslie W.D., Rubin M.R., Schwartz A.V., Kanis J.A. Type 2 diabetes and bone. J. Bone Min. Res. 2012;27:2231–2237. doi: 10.1002/jbmr.1759. [DOI] [PubMed] [Google Scholar]
- 55.Hadji P., Ziller M., Albert U.S., Kalder M. Assessment of fracture risk in women with breast cancer using current vs emerging guidelines. Br. J. Cancer. 2010;102:645–650. doi: 10.1038/sj.bjc.6605548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Neuner J.M., Yen T.W., Sparapani R.A. Fracture risk and adjuvant hormonal therapy among a population-based cohort of older female breast cancer patients. Osteoporos. Int. 2011;22:2847–2855. doi: 10.1007/s00198-010-1493-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chlebowski R.T., Chen Z., Cauley J.A. Oral bisphosphonate use and breast cancer incidence in postmenopausal women. J. Clin. Oncol. 2010 doi: 10.1200/JCO.2010.28.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Newcomb P.A., Trentham-Dietz A., Hampton J.M. Bisphosphonates for osteoporosis treatment are associated with reduced breast cancer risk. Br. J. Cancer. 2010;102:799–802. doi: 10.1038/sj.bjc.6605555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rennert G., Pinchev M., Rennert H.S. Use of bisphosphonates and risk of postmenopausal breast cancer. J. Clin. Oncol. 2010 doi: 10.1200/JCO.2010.28.1113. [DOI] [PubMed] [Google Scholar]
- 60.Aft R., Naughton M., Trinkaus K. Effect of zoledronic acid on disseminated tumour cells in women with locally advanced breast cancer: an open label, randomised, phase 2 trial. Lancet Oncol. 2010;11:421–428. doi: 10.1016/S1470-2045(10)70054-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Greenberg S., Park J.W., Melisko M.E. Effect of adjuvant zoledronic acid (ZOL) on disseminated tumor cells (DTC) in the bone marrow (BM) of women with early stage breast cancer (ESBC): updated results. J. Clin. Oncol. 2010;28(suppl) (abstr 1002) [Google Scholar]
- 62.Rack B., Schindlbeck C., Strobl B. [Efficacy of zoledronate in treating persisting isolated tumor cells in bone marrow in patients with breast cancer. A phase II pilot study] Dtsch. Med. Wochenschr. 2008;133:285–289. doi: 10.1055/s-2008-1046707. [DOI] [PubMed] [Google Scholar]
- 63.Solomayer E.F., Gebauer G., Hirnle P. Influence of zoledronic acid on disseminated tumor cells (DTC) in primary breast cancer patients. Cancer Res. 2009;69:170s–171s. doi: 10.1093/annonc/mdr612. (Abstract 2048) [DOI] [PubMed] [Google Scholar]
- 64.Coleman R.E., Winter M.C., Cameron D. The effects of adding zoledronic acid to neoadjuvant chemotherapy on tumour response: exploratory evidence for direct anti-tumour activity in breast cancer. Br. J. Cancer. 2010;102:1099–1105. doi: 10.1038/sj.bjc.6605604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Diel I.J., Jaschke A., Solomayer E.F. Adjuvant oral clodronate improves the overall survival of primary breast cancer patients with micrometastases to the bone marrow—a long-term follow-up. Ann. Oncol. 2008;19:2007–2011. doi: 10.1093/annonc/mdn429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ha T.C., Li H. Meta-analysis of clodronate and breast cancer survival. Br. J. Cancer. 2007;96:1796–1801. doi: 10.1038/sj.bjc.6603661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Powles T., Paterson A., McCloskey E. Reduction in bone relapse and improved survival with oral clodronate for adjuvant treatment of operable breast cancer [ISRCTN83688026] Breast Cancer Res. 2006;8:R13. doi: 10.1186/bcr1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Saarto T., Vehmanen L., Virkkunen P., Blomqvist C. Ten-year follow-up of a randomized controlled trial of adjuvant clodronate treatment in node-positive breast cancer patients. Acta Oncol. 2004;43:650–656. doi: 10.1080/02841860410032885. [DOI] [PubMed] [Google Scholar]
- 69.Eidtmann H., de Boer R., Bundred N. Efficacy of zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: 36-month results of the ZO-FAST Study. Ann. Oncol. 2010 doi: 10.1093/annonc/mdq217. [DOI] [PubMed] [Google Scholar]
- 70.Gnant M., Mlineritsch B., Schippinger W. Endocrine therapy plus zoledronic acid in premenopausal breast cancer. N. Engl. J. Med. 2009;360:679–691. doi: 10.1056/NEJMoa0806285. [DOI] [PubMed] [Google Scholar]
- 71.Early Breast Cancer Trialists' Collaborative G., Coleman R., Powles T. Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomised trials. Lancet. 2015;386:1353–1361. doi: 10.1016/S0140-6736(15)60908-4. [DOI] [PubMed] [Google Scholar]
- 72.Hadji P., Coleman R.E., Wilson C. Adjuvant bisphosphonates in early breast cancer: consensus guidance for clinical practice from a European Panel. Ann. Oncol. 2016;27:379–390. doi: 10.1093/annonc/mdv617. [DOI] [PubMed] [Google Scholar]
- 73.De Laet C., Kanis J.A., Oden A. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos. Int. 2005;16:1330–1338. doi: 10.1007/s00198-005-1863-y. [DOI] [PubMed] [Google Scholar]
- 74.Kanis J.A., Johnell O., De Laet C. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375–382. doi: 10.1016/j.bone.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 75.Kanis J.A., Johansson H., Oden A. A family history of fracture and fracture risk: a meta-analysis. Bone. 2004;35:1029–1037. doi: 10.1016/j.bone.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 76.Kanis J.A., Johnell O., Oden A. Smoking and fracture risk: a meta-analysis. Osteoporos. Int. 2005;16:155–162. doi: 10.1007/s00198-004-1640-3. [DOI] [PubMed] [Google Scholar]
- 77.van Staa T.P., Leufkens H.G., Abenhaim L. Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology. 2000;39:1383–1389. doi: 10.1093/rheumatology/39.12.1383. [DOI] [PubMed] [Google Scholar]
- 78.Kanis J.A., Johansson H., Oden A. A meta-analysis of prior corticosteroid use and fracture risk. J. Bone Min. Res. 2004;19:893–899. doi: 10.1359/JBMR.040134. [DOI] [PubMed] [Google Scholar]
- 79.Kanis J.A., Johansson H., Johnell O. Alcohol intake as a risk factor for fracture. Osteoporos. Int. 2005;16:737–742. doi: 10.1007/s00198-004-1734-y. [DOI] [PubMed] [Google Scholar]
- 80.Waning D.L., Guise T.A. Cancer-associated muscle weakness: what's bone got to do with it? Bone. Rep. 2015;4:691. doi: 10.1038/bonekey.2015.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.A. Brufsky, W.G. Harker, J.T. Beck, et al. The effect of zoledronic acid on aromatase inhibitor-associated bone loss in premenopausal women with early breast cancer receiving adjuvant letrozole: the Z-FAST study 5-year final follow-up [poster]. Presented at in: Proceedings of the 32nd Annual San Antonio Breast Cancer Symposium, San Antonio, TX, 9–13 December 2009 (Abstr 4083). Available at: 〈http://www.posters2view.com/sabcs09/viewp.php?Nu=4083〉. (Accessed 4 February 2010), 2009.
- 82.Hines S.L., Mincey B., Dentchev T. Immediate versus delayed zoledronic acid for prevention of bone loss in postmenopausal women with breast cancer starting letrozole after tamoxifen-N03CC. Breast Cancer Res. Treat. 2009;117:603–609. doi: 10.1007/s10549-009-0332-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.A. Llombart, A. Frassoldati, O. Paija, et al. Zoledronic acid prevents aromatase inhibitor-associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: E-ZO-FAST 36-month follow-up. Presented at: American Society of Clinical Oncology 2009 Breast Cancer Symposium; October 8-10; San Francisco, CA. Abstract 213, 2009.
- 84.Ellis G.K., Bone H.G., Chlebowski R. Randomized trial of denosumab in patients receiving adjuvant aromatase inhibitors for nonmetastatic breast cancer. J. Clin. Oncol. 2008;26:4875–4882. doi: 10.1200/JCO.2008.16.3832. [DOI] [PubMed] [Google Scholar]
- 85.Van Poznak C., Hannon R.A., Mackey J.R. Prevention of aromatase inhibitor-induced bone loss using risedronate: the SABRE trial. J. Clin. Oncol. 2010;28:967–975. doi: 10.1200/JCO.2009.24.5902. [DOI] [PubMed] [Google Scholar]
- 86.Greenspan S.L., Brufsky A., Lembersky B.C. Risedronate prevents bone loss in breast cancer survivors: a 2-year, randomized, double-blind, placebo-controlled clinical trial. J. Clin. Oncol. 2008;26:2644–2652. doi: 10.1200/JCO.2007.15.2967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Saarto T., Vehmanen L., Elomaa I. The effect of clodronate and antioestrogens on bone loss associated with oestrogen withdrawal in postmenopausal women with breast cancer. Br. J. Cancer. 2001;84:1047–1051. doi: 10.1054/bjoc.2001.1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Singh S., Cuzick J., Edwards R. Effect of anastrozole on bone mineral density after one year of treatment: results from bone sub-study of the International breast cancer intervention Study (IBIS-II) Breast Cancer Res. Treat. 2007;106(suppl 1):S9. (Abstract 28) [Google Scholar]
- 89.Lester J.E., Dodwell D., Purohit O.P. Prevention of anastrozole-induced bone loss with monthly oral ibandronate during adjuvant aromatase inhibitor therapy for breast cancer. Clin. Cancer Res. 2008;14:6336–6342. doi: 10.1158/1078-0432.CCR-07-5101. [DOI] [PubMed] [Google Scholar]
- 90.Confavreux C.B., Fontana A., Guastalla J.P. Estrogen-dependent increase in bone turnover and bone loss in postmenopausal women with breast cancer treated with anastrozole. Prevention with bisphosphonates. Bone. 2007;41:346–352. doi: 10.1016/j.bone.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 91.Miller P.D. Bone density and markers of bone turnover in predicting fracture risk and how changes in these measures predict fracture risk reduction. Curr. Osteoporos. Rep. 2005;3:103–110. doi: 10.1007/s11914-005-0018-6. [DOI] [PubMed] [Google Scholar]
- 92.Han M., Liang L., Liu L.R. Liver X receptor gene polymorphisms in tuberculosis: effect on susceptibility. PLoS One. 2014;9:e95954. doi: 10.1371/journal.pone.0095954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gnant M., Pfeiler G., Dubsky P.C. Adjuvant denosumab in breast cancer (ABCSG-18): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2015;386:433–443. doi: 10.1016/S0140-6736(15)60995-3. [DOI] [PubMed] [Google Scholar]
- 94.K. Fizazi, M.A. Carducci, M.R. Smith, et al. A randomized phase lll trial of denosumab versus zoledronic acid in patients with bone metastases from castration-resistant prostate cancer, in: Proceedings of the 46th Annual Meeting of the American Society of Clinical Oncology, Chicago, IL. Abstract LBA4507, June 4–8 2010.
- 95.D. Henry, R. von Moos, S. Vadhan-Raj, et al. A double-blind, randomized study of denosumab versus zoledronic acid for the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma, in: Proceedings of the Joint ECCO 15–34th ESMO Multidisciplinary Congress, Berlin, Germany. Abstract 20LBA, 20–24 September 2009.
- 96.A. Stopeck, J.J. Body, Y. Fujiwara, et al. Denosumab versus zoledronic acid for the treatment of breast cancer patients with bone metastases: results of a randomized phase 3 study, in: Proceedings of the Joint ECCO 15–34th ESMO Multidisciplinary Congress, Berlin, Germany. Abstract 2LBA, 20–24 September 2009.
- 97.Bone H.G., Bolognese M.A., Yuen C.K. Effects of denosumab treatment and discontinuation on bone mineral density and bone turnover markers in postmenopausal women with low bone mass. J. Clin. Endocrinol. Metab. 2011;96:972–980. doi: 10.1210/jc.2010-1502. [DOI] [PubMed] [Google Scholar]
- 98.Miller P.D., Wagman R.B., Peacock M. Effect of denosumab on bone mineral density and biochemical markers of bone turnover: six-year results of a phase 2 clinical trial. J. Clin. Endocrinol. Metab. 2011;96:394–402. doi: 10.1210/jc.2010-1805. [DOI] [PubMed] [Google Scholar]
- 99.Popp A.W., Zysset P.K., Lippuner K. Rebound-associated vertebral fractures after discontinuation of denosumab-from clinic and biomechanics. Osteoporos. Int. 2016;27:1917–1921. doi: 10.1007/s00198-015-3458-6. [DOI] [PubMed] [Google Scholar]
- 100.Anastasilakis A.D., Makras P. Multiple clinical vertebral fractures following denosumab discontinuation. Osteoporos. Int. 2016;27:1929–1930. doi: 10.1007/s00198-015-3459-5. [DOI] [PubMed] [Google Scholar]
- 101.R. Coleman, N. Bundred, R. de Boer, et al. Impact of zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: Z-FAST, ZO-FAST, and E-ZO-FAST, in: Proceedings of the 32nd Annual San Antonio Breast Cancer Symposium, San Antonio, TX [abstract 4082], December 9–13 2009.
- 102.Coleman R., de Boer R., Eidtmann H. Zoledronic acid (zoledronate) for postmenopausal women with early breast cancer receiving adjuvant letrozole (ZO-FAST study): final 60-month results. Ann. Oncol. 2013;24:398–405. doi: 10.1093/annonc/mds277. [DOI] [PubMed] [Google Scholar]
- 104.Rennert G., Pinchev M., Gronich N. Oral bisphosphonates and improved survival of breast cancer. Clin. Cancer Res. 2016 doi: 10.1158/1078-0432.CCR-16-0547. [DOI] [PubMed] [Google Scholar]
- 103.Wagner-Johnston N.D., Sloan J.A., Liu H. 5-year follow-up of a randomized controlled trial of immediate versus delayed zoledronic acid for the prevention of bone loss in postmenopausal women with breast cancer starting letrozole after tamoxifen: N03CC (Alliance) trial. Cancer. 2015;121:2537–2543. doi: 10.1002/cncr.29327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Inoue H., Hirano A., Ogura K. The effect of anastrozole on bone mineral density during the first 5 years of adjuvant treatment in postmenopausal women with early breast cancer. Springerplus. 2015;4:303. doi: 10.1186/s40064-015-1096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sestak I., Singh S., Cuzick J. Changes in bone mineral density at 3 years in postmenopausal women receiving anastrozole and risedronate in the IBIS-II bone substudy: an international, double-blind, randomised, placebo-controlled trial. Lancet Oncol. 2014;15:1460–1468. doi: 10.1016/S1470-2045(14)71035-6. [DOI] [PubMed] [Google Scholar]
- 107.Greenspan S.L., Vujevich K.T., Brufsky A. Prevention of bone loss with risedronate in breast cancer survivors: a randomized, controlled clinical trial. Osteoporos. Int. 2015;26:1857–1864. doi: 10.1007/s00198-015-3100-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lester J.E., Dodwell D., Brown J.E. Prevention of anastrozole induced bone loss with monthly oral ibandronate: final 5 year results from the ARIBON trial. J. Bone Oncol. 2012;1:57–62. doi: 10.1016/j.jbo.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rhee Y., Song K., Park S. Efficacy of a combined alendronate and calcitriol agent (Maxmarvil(R)) in Korean postmenopausal women with early breast cancer receiving aromatase inhibitor: a double-blind, randomized, placebo-controlled study. Endocr. J. 2013;60:167–172. doi: 10.1507/endocrj.ej12-0283. [DOI] [PubMed] [Google Scholar]
- 110.Lomax A.J., Yee Yap S., White K. Prevention of aromatase inhibitor-induced bone loss with alendronate in postmenopausal women: the BATMAN Trial. J. Bone Oncol. 2013;2:145–153. doi: 10.1016/j.jbo.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rodriguez-Sanz M., Prieto-Alhambra D., Servitja S. AI-related BMD variation in actual practice conditions: a prospective cohort study. Endocr. Relat. Cancer. 2016;23:303–312. doi: 10.1530/ERC-16-0025. [DOI] [PubMed] [Google Scholar]
- 112.Hadji P. Improving compliance and persistence to adjuvant tamoxifen and aromatase inhibitor therapy. Crit. Rev. Oncol. Hematol. 2010;73:156–166. doi: 10.1016/j.critrevonc.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 113.Ziller V., Kalder M., Albert U.S. Adherence to adjuvant endocrine therapy in postmenopausal women with breast cancer. Ann. Oncol. 2009;20:431–436. doi: 10.1093/annonc/mdn646. [DOI] [PubMed] [Google Scholar]
- 114.Carbonell-Abella C., Pages-Castella A., Javaid M.K. Early (1-year) Discontinuation of Different Anti-osteoporosis Medications Compared: a Population-Based Cohort Study. Calcif. Tissue Int. 2015;97:535–541. doi: 10.1007/s00223-015-0040-3. [DOI] [PubMed] [Google Scholar]
- 115.Bartl R., Gotte S., Hadji P., Hammerschmidt T. [Adherence with daily and weekly administration of oral bisphosphonates for osteoporosis treatment] Dtsch. Med. Wochenschr. 2006;131:1257–1262. doi: 10.1055/s-2006-946559. [DOI] [PubMed] [Google Scholar]
- 116.Hadji P., Claus V., Kostev K. GRAND—The German retrospective cohort analysis on non-adherence in osteoporosis: analysis of persistence with intravenous bisphosphonates in women. Osteoporos. Int. 2010;21:S168–S169. doi: 10.1007/s00198-011-1535-z. (Abstr P422) [DOI] [PubMed] [Google Scholar]
- 117.Hoer A., Seidlitz C., Gothe H. Influence on persistence and adherence with oral bisphosphonates on fracture rates in osteoporosis. Patient Prefer Adherence. 2009;3:25–30. [PMC free article] [PubMed] [Google Scholar]
- 118.Bock O., Felsenberg D. Bisphosphonates in the management of postmenopausal osteoporosis—optimizing efficacy in clinical practice. Clin. Inter. Aging. 2008;3:279–297. doi: 10.2147/cia.s2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Reginster J.Y. Adherence and persistence: impact on outcomes and health care resources. Bone. 2006;38(Suppl. 2):S18–S21. doi: 10.1016/j.bone.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 120.Silverman S.L., Gold D.T. Compliance and persistence with osteoporosis therapies. Curr. Rheumatol. Rep. 2008;10:118–122. doi: 10.1007/s11926-008-0021-x. [DOI] [PubMed] [Google Scholar]
- 121.Howe T.E., Shea B., Dawson L.J. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst. Rev. 2011:CD000333. doi: 10.1002/14651858.CD000333.pub2. [DOI] [PubMed] [Google Scholar]
- 122.Kemmler W., Haberle L., von Stengel S. Effects of exercise on fracture reduction in older adults: a systematic review and meta-analysis. Osteoporos. Int. 2013;24:1937–1950. doi: 10.1007/s00198-012-2248-7. [DOI] [PubMed] [Google Scholar]
- 123.Knobf M.T., Jeon S., Smith B. Effect of a randomized controlled exercise trial on bone outcomes: influence of adjuvant endocrine therapy. Breast Cancer Res. Treat. 2016;155:491–500. doi: 10.1007/s10549-016-3693-3. [DOI] [PubMed] [Google Scholar]
- 124.Servitja S., Martos T., Rodriguez Sanz M. Skeletal adverse effects with aromatase inhibitors in early breast cancer: evidence to date and clinical guidance. Ther. Adv. Med. Oncol. 2015;7:291–296. doi: 10.1177/1758834015598536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Datta M., Schwartz G.G. Calcium and vitamin D supplementation and loss of bone mineral density in women undergoing breast cancer therapy. Crit. Rev. Oncol. Hematol. 2013;88:613–624. doi: 10.1016/j.critrevonc.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Diez-Perez A., Naylor K.E., Abrahamsen B. International osteoporosis foundation and european calcified tissue society working group. Recommendations for the screening of adherence to oral bisphosphonates. Osteoporos. Int. 2017;28:767–774. doi: 10.1007/s00198-017-3906-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Christensen L., Iqbal S., Macarios D. Cost of fractures commonly associated with osteoporosis in a managed-care population. J. Med. Econ. 2010;13:302–313. doi: 10.3111/13696998.2010.488969. [DOI] [PubMed] [Google Scholar]
- 128.Becker D.J., Yun H., Kilgore M.L. Health services utilization after fractures: evidence from medicare. J. Gerontol. A Biol. Sci. Med. Sci. 2010 doi: 10.1093/gerona/glq093. [DOI] [PubMed] [Google Scholar]
- 129.Shi N., Foley K., Lenhart G., Badamgarav E. Direct healthcare costs of hip, vertebral, and non-hip, non-vertebral fractures. Bone. 2009;45:1084–1090. doi: 10.1016/j.bone.2009.07.086. [DOI] [PubMed] [Google Scholar]
- 130.Hernlund E., Svedbom A., Ivergard M. osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International osteoporosis foundation (IOF) and the European Federation of pharmaceutical industry Associations (EFPIA) Arch. Osteoporos. 2013;8:136. doi: 10.1007/s11657-013-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]