Abstract
Background
The increasing burden of type 2 diabetes mellitus makes the continuous surveillance of its prevalence and incidence advisable. Electronic health records (EHRs) have great potential for research and surveillance purposes; however the quality of their data must first be evaluated for fitness for use. The aim of this study was to assess the validity of type 2 diabetes diagnosis in a primary care EHR database covering more than half a million inhabitants, 97% of the population in Navarra, Spain.
Methods
In the Navarra EPIC-InterAct study, the validity of the T90 code from the International Classification of Primary Care, Second Edition was studied in a primary care EHR database to identify incident cases of type 2 diabetes, using a multi-source approach as the gold standard. The sensitivity, specificity, positive predictive value, negative predictive value and the kappa index were calculated. Additionally, type 2 diabetes prevalence from the EHR database was compared with estimations from a health survey.
Results
The sensitivity, specificity, positive predictive value and negative predictive value of incident type 2 diabetes recorded in the EHRs were 98.2, 99.3, 92.2 and 99.8%, respectively, and the kappa index was 0.946. Overall prevalence of type 2 diabetes diagnosed in the EHRs among adults (35–84 years of age) was 7.2% (95% confidence interval [CI] 7.2–7.3) in men and 5.9% (95% CI 5.8–5.9) in women, which was similar to the prevalence estimated from the health survey: 8.5% (95% CI 7.1–9.8) and 5.5% (95% CI 4.4–6.6) in men and women, respectively.
Conclusions
The high sensitivity and specificity of type 2 diabetes diagnosis found in the primary care EHRs make this database a good source for population-based surveillance of incident and prevalent type 2 diabetes, as well as for monitoring quality of care and health outcomes in diabetic patients.
Keywords: Validity, Type 2 diabetes mellitus, Incidence, Electronic health records, Primary care
Background
According to the World Health Organization (WHO), type 2 diabetes mellitus is caused by the body’s ineffective use of insulin and is mainly the result of excess body weight and physical inactivity. In 2014 it was estimated that the prevalence of type 2 diabetes around the world was 9% among adults over 18 years old, and in 2012 diabetes was responsible for1.5 million deaths [1]. Observational studies have found that diabetes is associated with an increased risk of cardiovascular diseases and all-cause mortality [2–4].
The WHO recommends continuous surveillance of prevalence and incidence of the most common noncommunicable diseases: cardiovascular diseases, cancer, respiratory diseases and diabetes [5]. Several approaches have been used to monitor type 2 diabetes, including the use of mortality statistics, surveys with or without laboratory tests, diabetes registers, electronic health records (EHRs), diabetes medications prescriptions, claims, diabetes diagnosis in hospital discharge and laboratory tests. In recent years, some algorithms have been developed for ascertaining type 2 diabetes in adults and children using administrative and clinical databases, for example in Canada [6–10], the UK [11] and Spain [12–14], among others. The use of EHR data for surveillance does not require bespoke data collection or patient recruitment [15], provides data for large populations and could be cost-effective [16]. However, it is necessary to evaluate the validity of this data, obtained for clinical reasons, before using them for surveillance or research.
In Navarra, a region with 640,000 inhabitants, a single primary care EHR database covers >97% of the population. This database is administered by a software based in OMI-AP [17] and is structured around a list of episodes (problems in the bio-psycho-social sphere, reasons for consultation, etc.) coded according to the International Classification of Primary Care, Second Edition (ICPC-2) [18]. Coding gathered in this database distinguishes type 2 diabetes (T90) from type 1 diabetes (T89), impaired fasting glycemia (A91 descriptive term “impaired fasting glycemia”), glucose intolerance (T99 descriptive term “Glucose intolerance”) and gestational diabetes (W85).
The aim of this study was to assess the validity of the primary care EHR data for the surveillance of incidence and prevalence of type 2 diabetes in the Navarra population.
Methods
The ability of EHR to accurately identify incident cases of diagnosed type 2 diabetes was investigated in a cohort from Navarra that had been included in a large prospective type 2 diabetes case-cohort study nested within the European Prospective Investigation into Cancer and Nutrition (EPIC-InterAct study) [19]. This is a large multi-center study to investigate how genetic and lifestyle behavioral factors, particularly diet and physical activity, interact in their influence on the risk of developing type 2 diabetes. The Navarra EPIC cohort included 8084 participants (3908 men and 4176 women) aged 45–65 years at the time of enrollment (1992–1995). Most of the participants were blood donors (75%), and the rest were civil servants and general population. More detailed information about the EPIC study methods have been described elsewhere [20, 21]. A sensitive approach was used with the aim of identifying all potential incident diabetes cases between the recruitment and December 2007 using multiple sources: self-reported diabetes or use of diabetes medication in a follow-up survey carried out 3 years after recruitment, diabetes diagnosis in the hospital discharge databases, type 2 diabetes (T90), type 1 diabetes (T89) and T99 (descriptive term “glucose intolerance”) diagnosis in primary care EHRs, prescription of antidiabetic drugs and cause-of-death register. A team of trained health professionals reviewed the clinical data to verify if the cases fulfilled the criteria proposed by the American Diabetes Association (ADA) in 2003: 1) Symptoms of diabetes (e.g.: polyuria, polydipsia, and unexplained weight loss) plus casual plasma glucose concentration ≥200 mg/dL (11.1 mmol/L). Or 2) Fasting plasma glucose (FPG) ≥126 mg/dL (7.0 mmol/L). Or 3) 2-h PG ≥200 mg/dL (11.1 mmol/L) during an oral glucose tolerance test (OGTT). In the absence of unequivocal hyperglycemia with acute metabolic decompensation, these criteria should be confirmed by repeat testing on a different day [22]. We excluded from the analysis 262 prevalent type 2 diabetes cases at recruitment, 5 participants who died before 2003 when EHR use was universalized in Navarra and 130 without primary care EHRs, resulting in a final sample of 7687 (3654 men and 4033 women).
The completeness of prevalence type 2 diabetes data recorded in EHRs was studied using “comparison of rates” [11, 23] methodology. To this end, type 2 diabetes prevalence in primary care EHR database in 2005 was compared with the estimations obtained from a health survey carried out in a census sample from the Navarra adult population in 2003 [24]. With the exception of <3% of the population (which was covered by private health insurance), the EHR database encompassed the entire Navarra population’s use of primary care centers.
Briefly, the aim of this survey was to estimate the prevalence of several cardiovascular risk factors including diabetes. After a response rate of 71%, self-reported diabetes prevalence was estimated in 4354 participants between 35 and 84 years of age. Data from surviving registered patients diagnosed with type 2 diabetes (ICPC-2, code T90) in June 2005 (n = 22,313) served to estimate type 2 diabetes prevalence in the EHR database that was compared with the health survey estimations to assess completeness and determine the level of under-reporting or over-reporting.
Statistical analyses
After the multi-source search and verification against medical records, EPIC cohort participants were categorized as having or not having an incident type 2 diabetes diagnosis. We compared T90-coded data in the EHRs against this gold standard to calculate sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) with their 95% confidence intervals (CI). The kappa index was also calculated. This validation method has been used successfully by other authors [12, 14, 25, 26]. The sensitivity was defined as the proportion of cases with T90 codes in the EHR database among those who were true incident type 2 diabetes cases according to the gold standard. The specificity was defined as the proportion of cases without T90 codes in the EHRs among those who were not type 2 diabetes cases according to the gold standard. The PPV was defined as the probability that a patient with a T90 code in the EHRs would be considered a true type 2 diabetes case according to the gold standard, and the NPV was defined as the probability that a patient without type 2 diabetes code would not meet the criteria to be considered a type 2 diabetes case according to the gold standard.
Additionally, we estimated the accuracy of the date of diagnosis registered in the EHRs via comparison with the real date of diagnosis in those patients who had been diagnosed between 2003 and 2006.
To evaluate the completeness of the type 2 diabetes diagnosis reported in the EHR database, the population was divided into five age groups as follows: 35–44 years, 45–54 years, 55–64 years, 65–74 years and 75–84 years. The prevalence of type 2 diabetes and its 95% CI in each sex-age group was compared with the prevalence of self-reported type 2 diabetes in the health survey. Age-adjusted prevalence in men and women 35–84 years of age was estimated using the age distribution of the Navarra population as a reference.
All statistical analyses were performed with the statistical software STATA/SE (version 12.0).
Results
A total of 1285 charts of potential diabetes cases were reviewed and 598 cases of type 2 diabetes were confirmed in the EPIC-InterAct cohort. The T90 code for type 2 diabetes in the EHR database had a high sensitivity (98.2%), specificity (99.3%), PPV (92.2%) and NPV (99.8%) (Tables 1 and 2). The degree of global agreement measured with the kappa index was very high: ƙ = 0.946 (p <0.001).
Table 1.
Measures of validity of type 2 diabetes code (ICPC-2, T90) in a primary care EHR database. Navarra EPIC-InterAct cohort
| Gold standard (diagnosis from multiple sources) | Total | ||
|---|---|---|---|
| Information of EHR | T2DM yes | T2DM no | |
| Code T90 yes | (A) TP True cases correctly identified in EHR |
(B) FP Non-cases wrongly coded in EHR |
(A + B) |
| 587 | 50 | 637 | |
| Code T90 no | (C) FN True cases not identified in EHR |
(D) TN True non-cases correctly identified in EHR |
(C + D) |
| 11 | 7039 | 7050 | |
| Total | (A + C) | (B + D) | (A + B + C + D) |
| 598 | 7089 | 7687 | |
Sensitivity: A/(A + C); specificity: D/(B + D); positive predictive value: A/(A + B); negative predictive value: D/(C + D)
Table 2.
Validity of type 2 diabetes code (ICPC-2, T90) in a primary care EHR database. Navarra EPIC-InterAct cohort
| Sensitivity % (95% CI) |
Specificity % (95% CI) |
PPV % (95% CI) |
NPV % (95% CI) |
Kappa index (95% CI) |
|---|---|---|---|---|
| 98.2 (96.7–99.1) |
99.3 (99.1–99.5) |
92.2 (89.8–94.1) |
99.8 (99.7–99.9) |
0.946 (0.933–0.960) |
Abbreviations: ICPC-2, International Classification of Primary Care, Second Edition, PPV positive predictive value, NPV negative predictive value
The difference between the date of diagnosis reported in the EHRs (date of the T90 code) and the date of diagnosis according to the gold standard was less than 12 months in 3 out of 4 patients (Table 3).
Table 3.
Time lag of T90 code date in comparison with diagnosis date. Navarra EPIC-InterAct cohort (cases of type 2 diabetes diagnosed between 2003 and 2006)
| Time lag (months) | N | % |
|---|---|---|
| <12 | 154 | 75.5 |
| 12–23 | 31 | 15.2 |
| 24–35 | 13 | 6.4 |
| ≥36 | 6 | 2.9 |
| Total | 204 | 100.0 |
Type 2 diabetes prevalence estimates based on EHR data were comparable to those obtained from the health survey in all age groups. Overall prevalence of type 2 diabetes diagnosed in the EHRs among adults (35–84 years) was 7.2% (95% CI 7.2–7.3) and 5.9% (95% CI 5.8–5.9) in men and women, respectively, very similar to the prevalence estimated from the health survey: 8.5% (95% CI 7.1–9.8) in men and 5.5% (95% CI 4.4–6.6) in women (Table 4 and Fig. 1).
Table 4.
Comparison between type 2 diabetes prevalence registered in the primary care EHR database and self-reported prevalence from a health survey
| Diabetes prevalence in 2003 (health survey) | Population in primary care EHR database in 2005 | Expected cases in 2005 according to the health survey prevalence | Registered cases in primary care EHR (code T90) in June 2005 | Ratio between registered and expected cases | ||
|---|---|---|---|---|---|---|
| % | n | n | n | % | % | |
| Men | ||||||
| 35–44 years | 1.5 | 48,244 | 723 | 525 | 1.1 | 72.6 |
| 45–54 years | 4.7 | 38,169 | 1803 | 1568 | 4.1 | 87.0 |
| 55–64 years | 11.1 | 30,974 | 3442 | 3226 | 10.4 | 93.7 |
| 65–74 years | 17.7 | 23,003 | 4064 | 3643 | 15.8 | 89.7 |
| 75–84 years | 20.3 | 15,567 | 3166 | 2311 | 14.8 | 73.0 |
| 35–84 years | 155,957 | 13,198 | 11,273 | 85.4 | ||
| Age-adjusted prevalence (95% CI%) |
8.5 | 7.2 | ||||
| (7.1–9.8) | (7.2–7.3) | |||||
| Women | ||||||
| 35–44 years | 0.6 | 44,431 | 269 | 290 | 0.7 | 107.7 |
| 45–54 years | 2.1 | 36,546 | 771 | 708 | 1.9 | 91.8 |
| 55–64 years | 4.2 | 30,832 | 1282 | 1970 | 6.4 | 153.7 |
| 65–74 years | 11.2 | 25,855 | 2904 | 3121 | 12.1 | 107.5 |
| 75–84 years | 16 | 22,261 | 3557 | 3288 | 14.8 | 92.5 |
| 35–84 years | 159,925 | 8783 | 9377 | 106.8 | ||
| Age-adjusted prevalence (95% CI) |
5.5 | 5.9 | ||||
| (4.4–6.6) | (5.8–5.9) | |||||
Abbreviations: EHR electronic health record
Fig. 1.
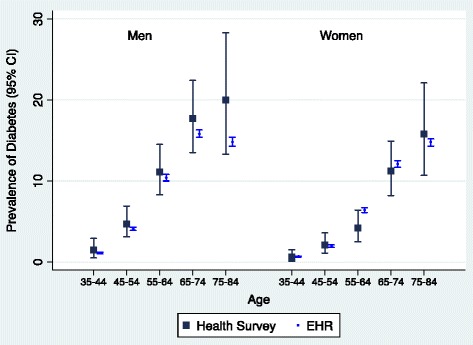
Comparison of type 2 diabetes prevalence estimated by the health survey and prevalence registered in primary EHR database by sex and age
Discussion
Most of the type 2 diabetes diagnoses in the primary care EHRs were well recorded when compared against the “gold standard,” showing a high sensitivity, specificity, PPV and NPV, and also a very high agreement. Moreover, this study showed that the information obtained from the EHRs provides a good estimation of type 2 diabetes prevalence in population with 35–84 years of age.
The incidence study in the EPIC-InterAct cohort showed that code T90 has a high sensitivity (98.2%), higher than that published in the outpatient records from a large health system, 79% [25]. The percentage of false negative cases in our study was 1.8%, and they corresponded mainly to cases that were coded as type 1 diabetes, impaired fasting glycemia or glucose intolerance. Similar sensitivity, 99.5%, was found in one study published in Spain using an internal validation method [14]. Another study conducted in Spain by Gil-Montalban et al. [12] using a similar approach as ours found a sensitivity of 83.5%. The sensitivity of administrative data ranged from 46 to 97% (median 81.5%) in a systematic review conducted by Saydah et al. [26].
In our study, we found a high specificity for the diagnosis of type 2 diabetes: 99.3%. The percentage of false positive cases was only 0.7% and most of them corresponded to patients that had impaired fasting glycemia, patients with adverse effects to some medications that cause hyperglycemia and type 1 diabetes cases. Other studies conducted in Spain have also reported specificities over 98% for the primary care EHRs [12, 14]. The review of studies based on administrative data carried out by Saydah et al. [26] found that the specificity was consistently high and ranged from 95 to 100% (median 99%).
The PPV and NPV that we found in our study were 92.2 and 99.8%, respectively. These were higher than the values observed by Gil-Montalban et al. [12] at 78.5 and 98.7%, and very similar to those found by Burgos-Lunar et al. [14] at 91.2 and 99.9% for PPV and NPV, respectively. Additionally the review of Saydah et al. [26] found that the PPV ranged from 60 to 98% (median 92%). Finally, the agreement found between the T90 codes in the EHRs and the gold standard was high at ƙ = 0.94 (p >0.001), as in other studies conducted in Spain, 0.99 and 0.79 (14,12). Additionally, Saydah et al. [26] found that the kappa index of the studies included in their review ranged from 67 to 96% (median 83%).
The prevalence of type 2 diabetes that we found in Navarra (7.2 and 5.9% in men and women ≥35 years, respectively) were quite similar to those found in adults over 30 years of age from Madrid, Spain (8.5 and 5.9% in men and women, respectively) registered in the primary care EHR database [12]. Additionally, the standardized prevalence of diabetes estimated with data from Spain’s 2006/2007 National Health Survey (NHS) [27] was 6.6% (CI95% 6.1–7.2) among men and 5.6% (CI95% 5.2–6.0) among women. The prevalence of the NHS was lower that the ones we found in our EHRs because they included adults above 16 years of age and our prevalence was calculated with older people (≥35 years), therefore our results are not fully comparable.
One limitation of the present study is the fact that the survey conducted in 2003 did not register the specific type of diabetes (1 or 2). However, the prevalence of type 1 diabetes represents only around 4% of total diabetes cases in Spain [28]. The strengths of the study are the exhaustive examination of clinical data in each case of potential type 2 diabetes identified in multiples source, the use of the whole population of Navarra for the prevalence study validation and the large number of participants included for the incidence validation study.
To the best of our knowledge, this is the first study that validates diabetes diagnosis in primary care EHRs using a multi-source approach including self-reported diabetes, hospital discharge diagnoses, drug prescription records, cause-of-death registers and several diabetes-related codes from the EHRs. Moreover, all potential diabetes cases were reviewed to confirm their fulfillment of the criteria proposed by the ADA in 2003. Implementation of algorithms that include other variables from the EHRs, especially prescription of antidiabetic drugs, would identify cases that need review to improve the accuracy of estimation as has been shown in a recent study from Spain [28].
The validation methodology used in this study might also be useful for validating EHR diagnosis of those diseases that need continuous surveillance of prevalence and incidence such as: cardiovascular diseases, cancer and respiratory diseases.
Conclusions
With the results of this validation study, we can conclude that the accuracy and completeness of type 2 diabetes diagnoses in the primary care EHR database proved it to be a valid source for epidemiological surveillance and quality care monitoring in our population.
Acknowledgments
We would like to acknowledge María Jesús Guembe of the Government Department of Health for her contribution to the study.
Funding
Partially funded by the European Union, Integrated Project LSHM-CT-2006-037197 in Framework Programme 6 of the European Community (EPIC-Interact study) and the Research Network for Health Services in Chronic Diseases (REDISSEC, grant RD12/0001 from the Carlos III Health Institute, Spanish Ministry of Health, co-financed by the European Regional Development Fund).
Availability of data and materials
The datasets used and/or analyzed during this study are available from the corresponding author upon reasonable request.
Authors’ contributions
CM-I designed the research. CM-I and MG conducted the research. CM-I, JD, and CS-O analyzed the data. CM-I, MG and CS-O wrote the article. All authors revised the manuscript for important intellectual content and read and approved the final manuscript. CM-I and MG are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Competing interests
No potential conflicts of interest relevant to this article were reported.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All participants gave their informed consent, and the Medical Ethical Review Board of Bellvitge Hospital of Barcelona, Spain granted approval to the project.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ADA
American Diabetes Association
- CI
Confidence intervals
- EHR
Electronic health record
- EPIC
European Prospective Investigation into Cancer and Nutrition
- ICPC-2
International Classification of Primary Care, Second Edition
- NPV
Negative predictive value
- PPV
Positive predictive value
- WHO
World Health Organization
Contributor Information
Conchi Moreno-Iribas, Phone: +34 848 423470, Email: mmorenoi@cfnavarra.es.
Carmen Sayon-Orea, Email: msayon@alumni.unav.es.
Josu Delfrade, Email: D800782@navarra.es.
Eva Ardanaz, Email: me.ardanaz.aicua@cfnavarra.es.
Javier Gorricho, Email: javier.gorricho.mendivil@cfnavarra.es.
Rosana Burgui, Email: rosana.burgui.perez@navarra.es.
Marian Nuin, Email: ma.nuin.villanueva@cfnavarra.es.
Marcela Guevara, Email: mp.guevara.eslava@navarra.es.
References
- 1.World Health Organization: Global status report on noncommunicable diseases 2014. http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1 Accessed 7 Nov 2016
- 2.Emerging Risk Factors Collaboration. Seshasai SR, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, Whincup PH, Mukamal KJ, Gillum RF, Holme I, Njølstad I, Fletcher A, Nilsson P, Lewington S, Collins R, Gudnason V, Thompson SG, Sattar N, Selvin E, Hu FB, Danesh J. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364:829–841. doi: 10.1056/NEJMoa1008862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baena-Díez JM, Peñafiel J, Subirana I, Ramos R, Elosua R, Marín-Ibañez A, Guembe MJ, Rigo F, Tormo-Díaz MJ, Moreno-Iribas C, Cabré JJ, Segura A, García-Lareo M, Gómez De La Cámara A, Lapetra J, Quesada M, Marrugat J, Medrano MJ, Berjón J, Frontera G, Gavrila D, Barricarte A, Basora J, García JM, Pavone NC, Lora-Pablos D, Mayoral E, Franch J, Mata M, Castell C, Frances A, Grau M, FRESCO Investigators Diabetes Care. 2016;39:1987–1995. doi: 10.2337/dc16-0614. [DOI] [PubMed] [Google Scholar]
- 4.Emerging Risk Factors Collaboration. Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, Stehouwer CD, Lewington S, Pennells L, Thompson A, Sattar N, White IR, Ray KK, Danesh J. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UN General Assembly. Political declaration of the high-level meeting of the general assembly on the prevention and control of non-communicable diseases. A/66/L.1. Sept 16, 2011. http://www.un.org/ga/search/view_doc.asp?symbol=A/66/L.1. (Accessed 6 Apr 2017).
- 6.Guttmann A, Nakhla M, Henderson M, To T, Daneman D, Cauch-Dudek K, Wang X, Lam K, Hux J. Validation of a health administrative data algorithm for assessing the epidemiology of diabetes in Canadian children. Pediatr Diabetes. 2010;11:122–128. doi: 10.1111/j.1399-5448.2009.00539.x. [DOI] [PubMed] [Google Scholar]
- 7.Amed S, Vanderloo SE, Metzger D, Collet JP, Reimer K, McCrea P, Johnson JA. Validation of diabetes case definitions using administrative claims data. Diabet Med. 2011;28:424–427. doi: 10.1111/j.1464-5491.2011.03238.x. [DOI] [PubMed] [Google Scholar]
- 8.Chen G, Khan N, Walker R, Quan H. Validating ICD coding algorithms for diabetes mellitus from administrative data. Diabetes Res Clin Pract. 2010;89:189–195. doi: 10.1016/j.diabres.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 9.Hux JE, Ivis F, Flintoft V, Bica A. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;3:512–516. doi: 10.2337/diacare.25.3.512. [DOI] [PubMed] [Google Scholar]
- 10.Dart AB, Martens PJ, Sellers E, Brownell MD, Rigatto C, Dean HJ. Validation of a Pediatric Diabetes Case Definition Using Administrative Health Data in Manitoba, Canada. Diabetes Care. 2011;34:898–903. doi: 10.2337/dc10-1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract. 2010;60:128–36. [DOI] [PMC free article] [PubMed]
- 12.Gil Montalbán E, Ortiz Marrín H, López-Gay Lucio-Villegas D, Zorrilla Torres B, Arrieta Blanco F, Nogales Aguado P. Validity and concordance of electronic health records in primary care (AP-Madrid) for surveillance of diabetes mellitus. PREDIMERC study. Gac Sanit. 2014;28:393–396. doi: 10.1016/j.gaceta.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Ramos R, Balló E, Marrugat J, Elosua R, Sala J, Grau M, Vila J, Bolíbar B, García-Gil M, Martí R, Fina F, Hermosilla E, Rosell M, Muñoz MA, Prieto-Alhambra D, Quesada M. Validity for use in research on vascular diseases of the SIDIAP (Information System for the Development of Research in Primary Care): the EMMA study. Rev Esp Cardiol. 2012;65:29–37. doi: 10.1016/j.recesp.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 14.De Burgos-Lunar C, Salinero-Fort MA, Cárdenas-Valladolid J, Soto-Díaz S, Fuentes-Rodríguez CY, Abánades-Herranz JC, del Cura-González I. Validation of diabetes mellitus and hypertension diagnosis in computerized medical records in primary health care. BMC Med Res Methodol. 2011;11:146. doi: 10.1186/1471-2288-11-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weiskopf NG, Weng C. Methods and dimensions of electronic health record data quality assessment: enabling reuse for clinical research. J Am Med Inform Assoc. 2013;20:144–151. doi: 10.1136/amiajnl-2011-000681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woodward M. Use of national data sources in diabetes epidemiology. Lancet Diabetes Endocrinol. 2015;3:92–93. doi: 10.1016/S2213-8587(14)70237-2. [DOI] [PubMed] [Google Scholar]
- 17.Stacks consulting e ingeniería en software. OMI-AP Módulo Historia Clínica. 2006.
- 18.WONCA International Classification Committee . [ICPC-2. International Classification of Primary Care]. Second Edition. Barcelona: Masson; 1999. [Google Scholar]
- 19.InterAct Consortium. Langenberg C, Sharp S, Forouhi NG, Franks PW, Schulze MB, Kerrison N, Ekelund U, Barroso I, Panico S, Tormo MJ, Spranger J, Griffin S, van der Schouw YT, Amiano P, Ardanaz E, Arriola L, Balkau B, Barricarte A, Beulens JW, Boeing H, Bueno-De-Mesquita HB, Buijsse B, Chirlaque Lopez MD, Clavel-Chapelon F, Crowe FL, de Lauzon-Guillan B, Deloukas P, Dorronsoro M, Drogan D, Froguel P, Gonzalez C, Grioni S, Groop L, Groves C, Hainaut P, Halkjaer J, Hallmans G, Hansen T, Huerta Castaño JM, Kaaks R, Key TJ, Khaw KT, Koulman A, Mattiello A, Navarro C, Nilsson P, Norat T, Overvad K, Palla L, Palli D, Pedersen O, Peeters PH, Quirós JR, Ramachandran A, Rodriguez-Suarez L, Rolandsson O, Romaguera D, Romieu I, Sacerdote C, Sánchez MJ, Sandbaek A, Slimani N, Sluijs I, Spijkerman AM, Teucher B, Tjonneland A, Tumino R, van der A DL, Verschuren WM, Tuomilehto J, Feskens E, McCarthy M, Riboli E, Wareham NJ. Design and cohort description of the InterAct Project: an examination of the interaction of genetic and lifestyle factors on the incidence of type 2 diabetes in the EPIC Study. Diabetologia. 2011;54:2272–2282. doi: 10.1007/s00125-011-2182-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M, Charrondière UR, Hémon B, Casagrande C, Vignat J, Overvad K, Tjønneland A, Clavel-Chapelon F, Thiébaut A, Wahrendorf J, Boeing H, Trichopoulos D, Trichopoulou A, Vineis P, Palli D, Bueno-De-Mesquita HB, Peeters PH, Lund E, Engeset D, González CA, Barricarte A, Berglund G, Hallmans G, Day NE, Key TJ, Kaaks R, Saracci R. European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr. 2002;5:1113–1124. doi: 10.1079/PHN2002394. [DOI] [PubMed] [Google Scholar]
- 21.Riboli E, Kaaks R. The EPIC Project: rationale and study design. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol. 1997;26(Suppl 1):S6–S14. doi: 10.1093/ije/26.suppl_1.S6. [DOI] [PubMed] [Google Scholar]
- 22.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):5–20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 23.Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol. 2010;69:4–14. doi: 10.1111/j.1365-2125.2009.03537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Viñes JJ, Díez J, Guembe MJ, González P, Amézqueta C, Barba J, Sobejano I, Martínez-Vila E, Grijalba AM, Serrano M, Moreno C, Los-Arcos E, Guerrero D. Study of vascular risk in Navarre: objectives and design. Prevalence of metabolic syndrome and of vascular risk. An Sist Sanit Navar. 2007;30:113–124. [PubMed] [Google Scholar]
- 25.Zgibor JC, Orchard TJ, Saul M, Piatt G, Ruppert K, Stewart A, Siminerio LM. Developing and validating a diabetes database in a large health system. Diabetes Res Clin Pract. 2007;75:313–319. doi: 10.1016/j.diabres.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 26.Saydah SH, Geiss LS, Tierney E, Benjamin SM, Engelgau M, Brancati F. Review of the performance of methods to identify diabetes cases among vital statistics, administrative, and survey data. Ann Epidemiol. 2004;14:507–516. doi: 10.1016/j.annepidem.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 27.Basterra-Gortari FJ, Bes-Rastrollo M, Ruiz-Canela M, Gea A, Martinez-Gonzalez MA. Prevalence of obesity and diabetes in Spanish adults 1987–2012. Med Clin. 2017;148:250–256. doi: 10.1016/j.medcli.2016.11.022. [DOI] [PubMed] [Google Scholar]
- 28.Mata-Cases M, Mauricio D, Real J, Bolíbar B, Franch-Nadal J. Is diabetes mellitus correctly registered and classified in primary care? A population-based study in Catalonia, Spain. Endocrinol y Nutr. 2016;63:440–448. doi: 10.1016/j.endonu.2016.07.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during this study are available from the corresponding author upon reasonable request.


