Abstract
With the marked increase of the Latino population in the United States during the past 20 years, there has been growing interest in the social, cultural, and structural factors that may impede breast cancer screening among Latino women, especially among those subgroups that have been understudied. Acculturation and fatalism are central cultural constructs in these growing fields of research. However, there is great debate on the extent to which acculturation and fatalism affect breast cancer screening among Latinas relative to other social or structural factors or logistical barriers. Moreover, little theoretical work specifies or tests pathways between social, structural, and cultural determinants of screening. This study tests a theoretical model of social and structural (socioeconomic status and access to health care) and cultural factors (acculturation and fatalism) as correlates of mammography screening among Dominican Latinas, a group that has been understudied. The study expands prior work by examining other factors identified as potential impediments to mammography screening, specifically psychosocial (e.g., embarrassment, pain) and logistical (e.g., not knowing how to get a mammogram, cost) barriers. Interview-administered surveys were conducted with 318 Latinas from the Dominican Republic aged 40 years or older. Fatalistic beliefs were not associated with mammogram screening. Greater acculturation assessed as language use was associated with decreased screening. The strongest predictor of decreased screening was perceived barriers. Results highlight the importance of assessing various self-reported psychosocial and logistical barriers to screening. Possible avenues for screening interventions include intensifying public health campaigns and use of personalized messages to address barriers to screening. Results add to a limited body of research on Dominicans, who constitute the fifth largest Latino group in the United States.
Keywords: acculturation, breast cancer screening, fatalism, Latinos, mammography
As the number of Latinos in the United States grows, there is increasing recognition of heterogeneity in this population and the varying sociodemographic and health profiles among different groups (Shelton, Jandorf, Thelemaque, King, & Erwin, 2012; Zsembik & Fennell, 2005). Many studies on breast cancer screening among Latinas aggregate participants originating from multiple Latin American countries, which may result in null findings or mask heterogeneity between groups. In fact, there is heterogeneity in cancer screening practices between Latinas from different countries of origin (Shelton et al., 2012), as well as differences when compared to non-Latino White women. To ultimately inform efforts to reduce disparities in screening, the Institute of Medicine has called for more research on Latino subgroups or subanalyses to better understand variation in health care by both race and ethnicity (Smedley, Stith, & Nelson, 2003).
The current study responds to this call by focusing on Dominican women. With some exceptions (Garbers, Jessop, Foti, Uribelarrea, & Chiasson, 2003; Lawsin, Erwin, Bursac, & Jandorf, 2011; Magai, Consedine, Conway, Neugut, & Culver, 2004; Shelton et al., 2012), little is known about the practices and determinants of breast cancer screening in this understudied population. Numbering approximately 1.5 million, Dominicans comprise the fifth largest Hispanic population in the United States (Brown & Patten, 2013). Almost half (48%) of all Dominicans in the United States reside in New York. Although there are few studies of recent mammography screening among Dominicans, there are differences between groups: Dominicans report slightly higher rates of recent screening (75.3%) than Puerto Ricans (70.5%), and Mexican Americans report the lowest rates (47.7%; Shelton et al., 2012). However, an older study found that Dominicans had the lowest rates compared with other Latino groups (O’Malley, Kerner, Johnson, & Mandelblatt, 1999). In addition, Dominicans have unique demographic characteristics. Relative to Hispanics in general, a greater proportion of Dominicans are foreign born (37% vs. 55%), a smaller proportion have English-language proficiency (65% vs. 55%), and a slightly higher proportion are living in poverty (26% vs. 28%; Brown & Patten, 2013). In light of the heterogeneity among Latinos and the scarcity of research on Dominicans in the United States, documenting the cultural and other factors that promote or present barriers to cancer screening among this population will provide more in-depth and targeted information to better address the needs of specific Latino groups.
Sociocultural Factors and Fatalism
Social and structural factors, such as socioeconomic status (SES) and access to health care, affect screening among Latinas (Schueler, Chu, & Smith-Bindman, 2008; Wells & Roetzheim, 2007). For example, lack of health insurance or a usual health care provider and inadequate or poor-quality health care constitute key determinants of nonadherence to breast cancer screening among Latinas (Echeverría & Carrasquillo, 2006; Gonzalez & Borrayo, 2011; Nuno, Castle, Harris, Estrada, & García, 2011).
Although social and structural factors, such as SES and access to health care, are associated with screening, cultural factors may also play an important role. Cultural explanations center on Latino norms, values, or customs (Abraído-Lanza, Chao, & Gates, 2005). Although definitions vary (Chun, Organista, & Marín, 2003; Clark & Hofsess, 1998; LaFromboise et al., 1993), acculturation broadly refers to the process of adopting the attitudes, values, customs, beliefs, and behavior of another culture (Abraído-Lanza, Armbrister, Flórez, & Aguirre, 2006). However, evidence is mixed on the association between acculturation and breast cancer screening (Schueler et al., 2008). After controlling for SES and structural factors (e.g., access to health care), some studies report that lower acculturation is associated with lower odds of receiving screening (O’Malley et al., 1999; Peragallo, Fox, & Alba, 1998), but other studies do not find these effects (Billmeier & Dallo, 2011; Lim, 2010; Buki, Jamison, Anderson, & Cuadra, 2007; Martinez-Donate et al., 2013; Pérez-Stable, Marín, & Marín, 1994; Ramirez, Suarez, Laufman, Barrosa, & Chalela, 2000; Ruiz, Marks, & Richardson, 1992). In yet others, various indices of acculturation differentially predict screening (Abraído-Lanza et al., 2005; Hiatt et al., 2001; Rosales & Gonzalez, 2013; Suarez, 1994; Wu, Black, & Markides, 2001; Zambrana, Breen, Fox, & Gutierrez-Mohamed, 1999). Given these mixed findings, there is growing interest in understanding the relationship between acculturation and screening.
Acculturation presumably leads to changes in beliefs, attitudes, or norms related to screening behavior; however, these assumptions are seldom tested. Therefore, to move the field forward, it would be useful to examine whether acculturation is associated with specific cultural belief systems that influence screening. One belief system, in particular, has attracted a great deal of research attention: fatalism. Defined as the belief that little can be done to change the course of one’s fate, fatalism is cited as a barrier to screening (Pérez-Stable, Sabogal, Otero-Sabogal, Hiatt, & McPhee, 1992). Fatalism is among the more controversial cultural-related constructs and has generated some debate (Abraído-Lanza et al., 2007; de los Monteros & Gallo, 2011) as to whether it acts as a deterrent to cancer screening. Greater acculturation among Latinos is associated with less fatalistic beliefs about cancer and cancer survival (Harmon, Castro, & Coe, 1996; Hubbell, Chavez, Mishra, & Valdez, 1996; Otero-Sabogal, Stewart, Sabogal, Brown, & Pérez-Stable, 2003; Pérez-Stable et al., 1992; Suarez, Nichols, Roche, & Simpson, 1997). However, evidence is mixed on the extent to which fatalism acts as a barrier to breast cancer screening, especially after controlling for potential confounders, such as SES (Magai et al., 2004; Otero-Sabogal et al., 2003; Ramirez et al., 2000).
A recent review of 11 studies concluded that “the majority of the studies reviewed reported a significant relationship between fatalism and cancer screening …” (de los Monteros & Gallo, 2011, p. 316). Our closer inspection of their findings revealed that slightly more than half of these studies assessed fatalism with questionable items. These included items measuring fear and other items unrelated to fate. The mixed evidence in this review underscores the importance of studying fatalism and other potential barriers to screening. In fact, barriers such as fear and pain can be deterrents of screening (Consedine, 2012; Garbers et al., 2003; Martínez-Donate et al., 2013; Tejada, Thompson, Coronado, & Martin, 2009), but they have not been explored simultaneously with fatalism as predictors of mammography. One of the main purposes of this study is to further explore these associations between fatalism and other barriers to screening.
Conceptual Framework
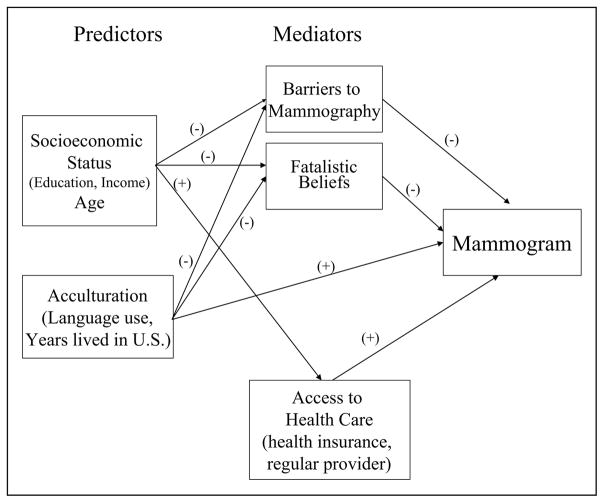
With some notable exceptions (e.g., Flynn, Betancourt, & Ormseth, 2011), relatively few theoretical frameworks guide research on acculturation, fatalism, and breast cancer screening among Latinas. Especially needed are studies that specify and test the mechanisms by which SES and acculturation affect screening. The aim of this study was to address these gaps by testing a theoretical model concerning the effects of social and demographic factors (SES), cultural variables (acculturation and fatalism), and structural (access to health care) determinants of mammography. The model, illustrated in Figure 1, outlines hypothesized paths between the predictor variables of SES, age, and acculturation; three mediators: perceived barriers to breast cancer screening, fatalistic beliefs about cancer, and access to health care; and receipt of a recent mammogram as an outcome. The model tests the extent to which fatalistic beliefs, other barriers, and access to health care mediate the effects of SES and acculturation on mammography screening.
Figure 1.
Hypothesized model showing paths between predictor variables of socioeconomic status, age, and acculturation; mediator variables: perceived barriers to breast cancer screening, fatalistic beliefs about cancer, and access to health care; and receipt of a recent mammogram.
Method
Participants and Procedures
Participants were recruited using several methods. A university-based research center provided recruitment assistance by referring eligible participants to the study. Flyers were posted in various locations throughout the medical center and surrounding neighborhood, and participants were asked to refer other eligible women living in the community. Women also were recruited from a general medicine clinic of a major hospital in the community. Approximately 60% of the sample was recruited via referrals and flyers, and 40% via the clinic. Eligibility criteria were the following: female aged 40 years or older, Dominican ethnicity, and no prior diagnosis of any form of cancer.
All respondents provided informed consent. The university’s medical center internal review board approved the study. A total of 318 Dominican women participated in the study.
Data were collected between 2006 and 2009 using a structured, in-person interview conducted in the respondent’s site of choice (e.g., home or clinic). Interviews were conducted in Spanish. Our previous pilot work and other research with this population and age-group indicated that women overwhelmingly preferred to be interviewed in Spanish. Interviews lasted an average of 40 minutes. Respondents were paid $25 for their participation.
Measures
We created Spanish versions of all scales using a back-translation technique with two iterations and four independent translators except for the acculturation measure, for which an established Spanish version already existed. All translators had extensive prior experience translating scales for research projects and were formally trained in public health, psychology, or both.
Sociodemographic Variables: Age and SES
Age was coded in years as a continuous variable. SES was assessed with two indicators: education, coded in years as the highest grade completed; and annual household income, ranging from 1 (<$10,000/year) to 8 (≥$70,000/year).
Acculturation
We used the Brief 12-item short form of the Acculturation Rating Scale for Mexican Americans (Brief ARSMA; Cuéllar, Bastida, & Braccio, 2004), which assesses English- and Spanish-language ability and preferences; and embeddedness with Anglo-American friends, rated on a 5-point scale ranging from never to always. The ARSMA is one of the most widely used measures of acculturation and can be adapted for use with other Latino populations (Chun et al., 2003). The scale developers suggest creating a linear measure by subtracting the English from the Spanish sub-scales. Because this method yields positive and negative scores, for ease of interpretation, we reverse-scored the Spanish-language items to create a summed score, such that higher scores reflected greater acculturation. The scale’s reliability, assessed with Cronbach’s alpha, was α = .69. We also assessed length of time living in the United States, measured in years, as a proxy of acculturation.
Fatalism
We used a modified version of the Powe Fatalism Inventory (Powe, 1995). Because it originally was developed to study beliefs about colorectal cancer, we eliminated questions on food, and five items that performed poorly during the pilot-testing phase of our study. We modified the resulting seven-item scale to refer specifically to breast cancer (e.g., “If a woman gets breast cancer, it was meant to be” and “If a woman gets breast cancer, that’s the way she was meant to die”) with a 4-point scale response scale ranging from strongly disagree to strongly agree. We calculated scores by averaging across all items, with higher scores reflecting greater fatalistic beliefs. The scale showed good reliability (α = .81).
Barriers to Breast Cancer Screening
We assessed a variety of self-reported barriers to screening identified in prior studies of Dominican and other Latina women (e.g., Garbers et al., 2003): embarrassment, pain, cost, and logistical barriers (e.g., not knowing how to obtain a mammography). Given the lack of existing measures of these various barriers, we used items from three scales to derive an 11-item measure. Sample items were the following: “Having a mammogram is too embarrassing” (6 items; Rawls, Champion, & Menon, 2000); “Having a mammogram costs too much money” (3 items; Champion & Scott, 1997), and “I’m too busy to get a mammogram” (2 items; Friedman et al., 1995). The reliability of the scale was α = .65.
Access to Health Care
We operationalized access to care as having a regular source of health care and health insurance, frequently used indicators of access (Schueler et al., 2008). We used an item commonly found in national surveys to measure access to a regular source of health care, “Is there a particular clinic, health center, doctor’s office, or other place that you usually go to if you are sick or need advice about your health?” coded dichotomously (1 = yes, 0 = no).
Health Insurance
Health insurance was assessed as having any coverage, coded as 0 = no health insurance, 1 = any type of health insurance (including private insurance or any form of public insurance, e.g., Medicaid, Medicare).
Main Dependent Variable: Recent Mammography
Mammography was described as “an X ray of the breasts taken by a machine that presses the breast against a plate,” and then women were asked, “Have you ever had a mammography?” Those who answered “yes” were then asked, “How long has it been since your last mammography?” On the basis of responses to these questions, we coded mammography screening as: 0 = never had, 1 = over 3 years ago, 2 = 1 to 3 years ago, and 3 = within past year, with higher scores representing more recent screening, following American Cancer Society guidelines that women aged 40 years or older be screened annually. Although in 2009, during the year that some of the data for this study were collected, the U.S. Preventive Services Task Force changed recommendations for screening, the American Cancer Society did not modify its guidelines.
Statistical Analyses
We tested the model depicted in Figure 1 with path analysis using reduced form equations, a procedure involving a series of multiple regression equations in which each variable is entered in order of causal priority (Cohen & Cohen, 1983). Mediating effects are tested by examining indirect effects, calculated as the difference in a variable’s coefficient before and after the mediator enters the equation.
We first entered as a set in these equations sociodemographic characteristics (age, education, income) and acculturation (ARSMA and number of years lived in the United States). In the second step, we entered the hypothesized mediators as a set: fatalism, barriers, and access to health care variables (health insurance and regular source of health care). This method of entering mediators as a set, rather than individually, is consistent with our theoretical model—that is, no particular mediator is hypothesized to be most important in the causal path (Cohen & Cohen, 1983).
These equations yield path coefficients from predictor (sociodemographic characteristics, acculturation) and mediating variables (fatalism, barriers, access to health care) to the criterion variable of screening. To complete the model, paths from predictor to mediating variables were calculated (see Baron & Kenny, 1986).
Results
Descriptive Statistics
The descriptive data in Table 1 show that all respondents were born in the Dominican Republic, except for one who was born in the United States of Dominican parents. Notably, although the sample was predominantly of low SES, 79.6% of women had a mammogram in the past year, and a large proportion had health insurance (95.9%) and a regular health care provider (95.6%).
Table 1.
Sample Characteristics and Descriptive Statistics (N = 318).
| Age in years, (M, SD) | 57.3 | 11.1 |
| Socioeconomic status variables (M, SD) | ||
| Education in years | 9.3 | 4.3 |
| Household income (N, %), $ | ||
| <10,000 | 185 | 58.2 |
| 10,000–19,999 | 70 | 22.0 |
| >20,000 | 41 | 12.8 |
| Acculturation variables (M, SD) | ||
| Acculturation (Acculturation Rating Scale for Mexican Americans) | 20.4 | 6.1 |
| Years residing in the United States | 24.1 | 11.6 |
| Fatalism (M, SD) | 2.1 | 0.8 |
| Access to health care variables (N, %) | ||
| Health insurance | ||
| No | 13 | 4.1 |
| Yes | 304 | 95.9 |
| Regular health care provider | ||
| No | 14 | 4.4 |
| Yes | 304 | 95.6 |
| Mammography barriers (M, SD) | 1.4 | 0.4 |
| Recent mammogram (N, %) | ||
| Never had mammogram | 14 | 4.1 |
| >3 years | 10 | 3.1 |
| 1–3 years | 40 | 12.6 |
| <1 year | 253 | 79.6 |
Tests of Model and Main Hypotheses
Table 2 presents the bivariate correlations of all model variables. Of particular note, higher acculturation (assessed with the Brief ARSMA) was associated with greater years in the United States, lower fatalism, and less recent mammography. Barriers were positively correlated with fatalism and negatively associated with receipt of a recent mammogram.
Table 2.
Intercorrelation Matrix for Model Variables With Pearson Correlations and p Values (N = 318).
| Variable name | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Recent mammogram | |||||||||
| 2. Age | .19*** | ||||||||
| 3. Education | −.09 | −.44*** | |||||||
| 4. Income | −.07 | −.23*** | .26*** | ||||||
| 5. Acculturation | −.15** | −.16** | .32*** | .22*** | |||||
| 6. Years in United States | .11* | .38*** | −.12* | .01 | .24*** | ||||
| 7. Health insurance | .08 | .17** | −.17** | −.01 | −.03 | .24*** | |||
| 8. Regular health care provider | .14* | .14* | −.08 | −.01 | .03 | .11 | .34*** | ||
| 9. Mammography barriers | −.18*** | .10 | −.14** | −.10 | −.05 | .06 | −.03 | −.07 | |
| 10. Fatalism | .06 | .22*** | −.29*** | −.12* | −.20*** | −.06 | .06 | .04 | .26*** |
p ≤ .05.
p ≤ .01.
p ≤ .001.
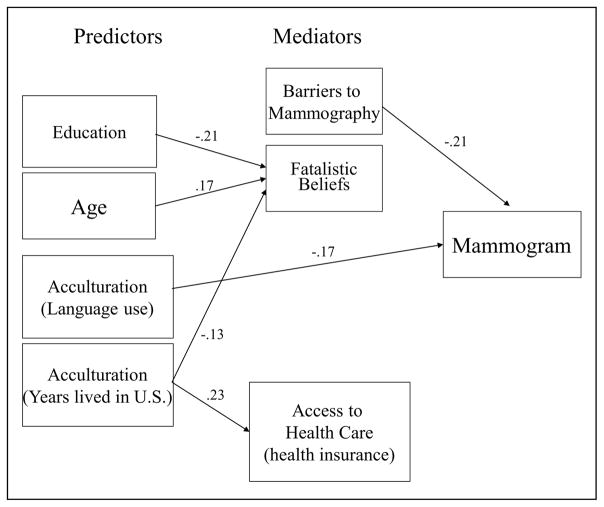
Table 3 shows the results of the regression equation predicting mammography. Analyses predicting fatalism, barriers, and access to health care variables are not shown but are available from the authors. Figure 2 illustrates direct paths obtained from the final steps in these models. Only significant paths are shown to simplify the diagram.
Table 3.
Regression Analysis of Sociodemographic Characteristics, Acculturation, Access to Health Care Variables, and Fatalism as Predictors of Mammography.
| Step and variable entered | Beta
|
R2 | R2 change | F change | Model F | |
|---|---|---|---|---|---|---|
| Step 1 | Step 2 | |||||
| Step 1 | .06 | 3.62** | ||||
| Age | .14* | .12 | ||||
| Years of Education | .04 | .03 | ||||
| Income | −.01 | −.02 | ||||
| Acculturation | −.17* | −.17* | ||||
| Years lived in the United States | .11 | .12 | ||||
| Step 2 | .12 | .06 | 4.36** | 4.04*** | ||
| Health insurance | −.01 | |||||
| Regular health care provider | .10 | |||||
| Barriers to mammography | −.22*** | |||||
| Fatalism | −.07 | |||||
Note. The final step contains coefficients for direct effects (illustrated in Figure 2). Indirect effects via mediators (access to health care variables, barriers, and fatalism) are calculated by subtracting the coefficient of a particular predictor from its coefficient at the previous step.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Figure 2.
Results of regression analyses.
Note. To simplify the diagram, only significant paths are shown.
In Step 1 of the model, greater age predicted higher screening (β = .14), and greater acculturation (assessed by the ARSMA) was associated with lower screening (β = −.17). In Step 2, when the hypothesized mediators entered the equation, age became nonsignificant, but the inverse association held between acculturation and screening. The strongest predictor of decreased screening was greater barriers (β = −.21). No other variables were significant predictors of mammography in the final model (see Figure 2). Because the effect of acculturation on mammography was not attenuated with the addition of the hypothesized mediator variables, results indicate that acculturation had a direct effect on screening. The final regression model predicted 12% of the variance in mammography screening, R2 = .12, F(9, 283) = 4.04, p ≦ .0001.
With regard to the equations predicting the mediators in the model (see Figure 2), greater age predicted increased fatalism (β = .17), and greater education (β = −.21) and years lived in the United States (β = −.13) were associated with decreased fatalism. Income and acculturation assessed as language were not associated with fatalism. These variables predicted 12% of the variance in fatalism, R2 = .12, F(5, 283) = 7.63, p ≦ .0001. None of the variables in the model significantly predicted barriers, R2 = .03, F(5, 283) = 1.47, p = .20. Only years lived in the United States predicted having health insurance (β = 0.23), R2 = .08, F(5, 283) = 5.00, p ≦ .0001, and there were no significant predictors of having a regular health care provider, R2 = .03, F(5, 283) = 1.49, p = .20.
Discussion
Despite growing interest and debate on the associations between acculturation, fatalism, and breast cancer screening among Latinas, to date, little is known about the mechanisms that mediate the effect of acculturation on screening. This study’s main purpose was to address these gaps in the literature by testing a model of social, cultural, and structural factors as correlates of mammography screening among Dominican Latinas.
Our results contribute to the growing debate on the extent to which fatalism predicts screening. One of the major findings in this study was that fatalism was not associated with mammography screening. Although fatalism (fatalismo) is often cited as a dominant cultural belief that deters Latinos from being screened (Pérez-Stable et al., 1992), evidence of this effect is inconclusive and mixed (Bundek, Marks, & Richardson, 1993; Dettenborn, DuHamel, Butts, Thompson, & Jandorf, 2004; Otero-Sabogal et al., 2003; Ramirez et al., 2000). We could not locate any published study that investigated the extent to which acculturation is associated with fatalistic beliefs about breast cancer among Latinas, and whether these beliefs, in turn, prevent women from being screened. Our results indicate that greater years lived in the United States (a proxy of “exposure”) was associated with less fatalism; however, acculturation assessed as language did not predict fatalism. Instead, greater acculturation as measured by language use (the ARSMA) had a direct effect in predicting decreased mammogram screening.
The observed direct, negative effect of acculturation on screening contradicts other reports that language acculturation is associated with recent receipt of mammography in a large sample of Latinas that included 308 Dominicans (O’Malley et al., 1999). Overall, evidence is mixed on the association between acculturation and screening (Abraído-Lanza et al., 2005; Rosales & Gonzalez, 2013; Suarez, 1994; Zambrana et al., 1999). Nevertheless, our results replicate at least two other recent studies reporting that lower acculturation (assessed as Spanish-language use) predicts greater mammography screening (Mack, Pavao, Tabnak, Knutson, & Kimerling, 2009; Rosales & Gonzalez, 2013). These findings led to speculations that outreach programs geared toward low–English-proficient populations are having an impact on screening (Rosales & Gonzalez, 2013).
A key finding in our study was that the strongest predictor of mammography was perceived psychosocial and logistical barriers to screening. This illustrates the importance of considering other barriers to screening simultaneously with fatalism. Our findings are consistent with prior research that Dominican women in New York City cite personal and psychosocial barriers (e.g., fear) as the most common deterrents to cancer screening (Garbers et al., 2003) and that barriers such as embarrassment and logistical issues are significantly associated with decreased mammography screening (Magai et al., 2004). Our findings warrant continued support of health education campaigns and other public health approaches (e.g., use of personalized messages) to assess and eliminate psychosocial and logistical barriers to screening. This would ultimately assist in identifying early-stage breast cancer, and enhancing timely and effective treatment.
Another key finding was the high rate of mammography screening: Almost 80% of women had a mammogram in the past year. There are only a handful of studies on the cancer screening practices of women from the Dominican Republic, and they have yielded mixed findings (Consedine, Magai, & Neugut, 2004; Lawsin et al., 2011; Magai et al., 2004; Mandelblatt et al., 1999). Our observed high rate of screening is consistent with other population-based data from the New York City Community Health Surveys, which indicate that 80% of all women (not limited to Dominicans) living in the upper Manhattan communities from which our sample was drawn had received a mammogram within the past 2 years (Olson, Van Wye, Kerker, Thorpe, & Frieden, 2006). Moreover, consistent with prior research among Dominican women (Shelton et al., 2012), the relatively high rate of screening among our sample is not too surprising considering that the majority of women in our sample had lived in the United States for many years, had insurance and a usual source of care, and, therefore, had a provider who might recommend mammography screening. Nevertheless, given the relatively high rate of screening that we observed, our results point to a public health success.
Some of the limitations of the study include its correlational design, which limits causal inferences concerning direction of effects. Moreover, all variables were based on self-report, introducing the possibility of bias. However, it is important to note that this potential bias is widespread in research on mammography screening—the vast majority of which relies on self-reports. In addition, there was low variability in some of the constructs in the study (e.g., family income and health insurance). The study did not employ population-based sampling; therefore, it is subject to the limitations of its convenience sampling methods. Finally, the study’s focus on women from the Dominican Republic living in New York City potentially limits generalizability. As discussed below, however, the findings add to a limited body of work on a large and growing subgroup of Latinos in the United States.
Despite these limitations, some strengths of this study are notable. First, this study contributes to a limited understanding of factors that are associated with screening among an understudied population: Dominican women. Moreover, the size of the Dominican sample (N = 318) is among the largest in studies published to date. Currently, the vast majority of research on acculturation and breast cancer screening among Latinas relies predominantly on samples of Mexican American women, who constitute the largest Latino group in the United States. With some exceptions (e.g., Flórez et al., 2009; Magai et al., 2004), the focus on Mexican samples is true also of research on fatalism and cancer screening among Latinos (see review by de los Monteros & Gallo, 2011). Studies of Dominican women, the fifth largest group of Latinos in the United States, are particularly important, given Institute of Medicine recommendations to study Latinos by country of origin, rather than as a homogenous group (Smedley et al., 2003).
A further strength is the study’s test of a theoretical model that includes structural and cultural factors and potential mediating mechanisms. The study contributes to the literature on breast cancer screening among Latinas by testing a model that specifies how acculturation and SES are related to fatalism, other barriers to screening, and health care factors, and whether these variables, in turn, predict mammography screening. Importantly, fatalism was not associated with screening. Instead, the strongest predictor of mammography was perceived barriers to screening. Although the model does not capture all factors that may influence screening, results provide a unique contribution to the existing literature, grounded in prior research on Latinas, from which more expansive models can be developed in future research.
Acknowledgments
The authors thank Alejandra Aguirre, Amarilis Céspedes, and Ana Alicia De La Cruz for their research assistance.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Susan Komen Foundation (Grant No. POP0402832); the National Institutes of Health (Grants R21CA134247, R25GM062454, and UL1TR000040); and a grant to Rachel C. Shelton from the American Cancer Society (124793-MRSG-13-152-01-CPPB).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abraído-Lanza AF, Armbrister AN, Flórez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. American Journal of Public Health. 2006;96:1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza AF, Chao MT, Gates CY. Acculturation and cancer screening among Latinas: Results from the National Health Interview Survey. Annals of Behavioral Medicine. 2005;29:22–28. doi: 10.1207/s15324796abm2901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza AF, Viladrich A, Flórez KR, Céspedes A, Aguirre AN, De La Cruz AA. Fatalismo reconsidered: A cautionary note for health-related research and practice with Latino populations. Ethnicity & Disease. 2007;17:153–158. [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Billmeier TM, Dallo FJ. Nativity status and mammography use: Results from the 2005 National Health Interview Survey. Journal of Immigrant Minority Health. 2011;13:883–890. doi: 10.1007/s10903-010-9334-8. [DOI] [PubMed] [Google Scholar]
- Brown A, Patten E. Hispanics of Dominican origin in the United States, 2011. Washington, DC: Pew Hispanic Center; 2013. Retrieved from http://www.pewhispanic.org/files/2013/06/DominicanFactsheet.pdf. [Google Scholar]
- Buki LP, Jamison J, Anderson CJ, Cuadra AM. Differences in predictors of cervical and breast cancer screening by screening need in uninsured Latina women. Cancer. 2007;110:1578–1585. doi: 10.1002/cncr.22929. [DOI] [PubMed] [Google Scholar]
- Bundek NI, Marks G, Richardson JL. Role of health locus of control beliefs in cancer screening of elderly Hispanic women. Health Psychology. 1993;12:193–199. doi: 10.1037//0278-6133.12.3.193. [DOI] [PubMed] [Google Scholar]
- Champion VL, Scott CR. Reliability and validity of breast cancer screening belief scales in African American women. Nursing Research. 1997;46:331–337. doi: 10.1097/00006199-199711000-00006. [DOI] [PubMed] [Google Scholar]
- Chun KM, Organista BP, Marín G, editors. Acculturation: Advances in theory, measurement and applied research. Washington, DC: American Psychological Association; 2003. [Google Scholar]
- Clark L, Hofsess L. Acculturation. In: Loue S, editor. Handbook of immigrant health. New York, NY: Plenum Press; 1998. pp. 37–59. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression and correlation analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum; 1983. [Google Scholar]
- Consedine NS. The demographic, system, and psychosocial origins of mammographic screening disparities: Prediction of initiation versus maintenance screening among immigrant and non-immigrant women. Journal of Immigrant and Minority Health. 2012;14:570–582. doi: 10.1007/s10903-011-9524-z. [DOI] [PubMed] [Google Scholar]
- Consedine NS, Magai C, Neugut AI. The contribution of emotional characteristics to breast cancer screening among women from six ethnic groups. Preventive Medicine. 2004;38:64–77. doi: 10.1016/j.ypmed.2003.09.030. [DOI] [PubMed] [Google Scholar]
- Cuéllar I, Bastida E, Braccio SM. Residency in the United States, subjective well-being, and depression in an older Mexican-origin sample. Journal of Aging and Health. 2004;16:447–466. doi: 10.1177/0898264304265764. [DOI] [PubMed] [Google Scholar]
- de los Monteros KE, Gallo LC. The relevance of fatalism in the study of Latinas’ cancer screening behavior: A systematic review of the literature. International Journal of Behavioral Medicine. 2011;18:310–318. doi: 10.1007/s12529-010-9119-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dettenborn L, DuHamel K, Butts G, Thompson H, Jandorf L. Cancer fatalism and its demographic correlates among African American and Hispanic women: Effects on adherence to cancer screening. Journal of Psychosocial Oncology. 2004;22(4):47–60. [Google Scholar]
- Echeverría SE, Carrasquillo O. The roles of citizenship status, acculturation, and health insurance in breast and cervical cancer screening among immigrant women. Medical Care. 2006;44:788–792. doi: 10.1097/01.mlr.0000215863.24214.41. [DOI] [PubMed] [Google Scholar]
- Flórez KR, Aguirre AN, Viladrich A, Céspedes A, De La Cruz AA, Abraído-Lanza AF. Fatalism or destiny?: A qualitative study and interpretative framework on Dominican women’s breast cancer beliefs. Journal of Immigrant and Minority Health. 2009;11:291–301. doi: 10.1007/s10903-008-9118-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn PM, Betancourt H, Ormseth SR. Culture, emotion, and cancer screening: An integrative framework for investigating health behavior. Annals of Behavioral Medicine. 2011;42:79–90. doi: 10.1007/s12160-011-9267-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman LC, Woodruff A, Lane M, Weinberg AD, Cooper HP, Webb JA. Breast cancer screening behaviors and intentions among asymptomatic women 50 years of age and older. American Journal of Preventive Medicine. 1995;11:218–223. [PubMed] [Google Scholar]
- Garbers S, Jessop DJ, Foti H, Uribelarrea M, Chiasson MA. Barriers to breast cancer screening for low-income Mexican and Dominican women in New York City. Journal of Urban Health. 2003;80(1):81–91. doi: 10.1007/PL00022327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez P, Borrayo EA. The role of physician involvement in Latinas’ mammgraphy screening adherence. Women’s Health Issues. 2011;21:165–170. doi: 10.1016/j.whi.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon MP, Castro FG, Coe K. Acculturation and cervical cancer: Knowledge, beliefs, and behaviors of Hispanic women. Women & Health. 1996;24(3):37–57. doi: 10.1300/j013v24n03_03. [DOI] [PubMed] [Google Scholar]
- Hiatt RA, Pasick RJ, Stewart S, Bloom J, Davis P, Gardiner P, … Stroud F. Community-based cancer screening for underserved women: Design and baseline findings from the Breast and Cervical Cancer Intervention Study. Preventive Medicine. 2001;33:190–203. doi: 10.1006/pmed.2001.0871. [DOI] [PubMed] [Google Scholar]
- Hubbell FA, Chavez LR, Mishra SI, Valdez RB. Differing beliefs about breast cancer among Latinas and Anglo women. Western Journal of Medicine. 1996;164:405–409. [PMC free article] [PubMed] [Google Scholar]
- LaFromboise T, Coleman HLK, Gerton J. Psychological impact of biculturalism: Evidence and theory. Psychological Bulletin. 1993;114:395–412. doi: 10.1037/0033-2909.114.3.395. [DOI] [PubMed] [Google Scholar]
- Lawsin C, Erwin D, Bursac Z, Jandorf L. Heterogeneity in breast and cervical cancer screening practices among female Hispanic immigrants in the United States. Journal of Immigrant and Minority Health. 2011;13:834–841. doi: 10.1007/s10903-010-9378-9. [DOI] [PubMed] [Google Scholar]
- Lim J. Linguistic and ethnic disparities in breast and cervical cancer screening and health risk behaviors among Latina and Asian American women. Journal of Women’s Health. 2010;19:1097–1107. doi: 10.1089/jwh.2009.1614. [DOI] [PubMed] [Google Scholar]
- Mack KP, Pavao J, Tabnak F, Knutson K, Kimerling R. Adherence to recent screening mammography among Latinas: Findings from the California Women’s Health Survey. Journal of Women’s Health. 2009;18:347–354. doi: 10.1089/jwh.2008.0793. [DOI] [PubMed] [Google Scholar]
- Magai C, Consedine N, Conway F, Neugut A, Culver C. Diversity matters: Unique populations of women and breast cancer screening. Cancer. 2004;100:2300–2307. doi: 10.1002/cncr.20278. [DOI] [PubMed] [Google Scholar]
- Mandelblatt JS, Gold K, O’Malley AS, Taylor K, Cagney K, Hopkins JS, Kerner J. Breast and cervix cancer screening among multiethnic women: Role of age, health, and source of care. Preventive Medicine. 1999;28:418–425. doi: 10.1006/pmed.1998.0446. [DOI] [PubMed] [Google Scholar]
- Martinez-Donate AP, Vera-Cala LM, Zhang X, Vedro R, Angulo R, Atkinson T. Prevalence and correlates of breast and cervical cancer screening among a Midwest community sample of low-acculturated Latinas. Journal of Health Care for the Poor and Underserved. 2013;24:1717–1738. doi: 10.1353/hpu.2013.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuno T, Castle PE, Harris R, Estrada A, García F. Breast and cervical cancer screening utilization among Hispanic women living near the United States-Mexico Border. Journal of Women’s Health. 2011;20:685–693. doi: 10.1089/jwh.2010.2205. [DOI] [PubMed] [Google Scholar]
- Olson EC, Van Wye G, Kerker B, Thorpe L, Frieden TR. Take care Inwood and Washington Heights. (2) 2006 Retrieved from http://www.nyc.gov/html/doh/downloads/pdf/data/2006chp-301.pdf.
- O’Malley AS, Kerner J, Johnson AE, Mandelblatt J. Acculturation and breast cancer screening among Hispanic women in New York City. American Journal of Public Health. 1999;89:219–227. doi: 10.2105/ajph.89.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otero-Sabogal R, Stewart R, Sabogal F, Brown BA, Pérez-Stable EJ. Access and attitudinal factors related to breast and cervical cancer screening: Why are Latinas still underscreened? Health Education & Behavior. 2003;30:337–359. doi: 10.1177/1090198103030003008. [DOI] [PubMed] [Google Scholar]
- Peragallo NP, Fox PG, Alba ML. Breast care among Latino immigrant women in the U.S. Health Care for Women International. 1998;19:165–172. doi: 10.1080/073993398246494. [DOI] [PubMed] [Google Scholar]
- Pérez-Stable EJ, Marín G, Marín BV. Behavioral risk factors: A comparison of Latinos and Non-Latino Whites in San Francisco. American Journal of Public Health. 1994;84:971–976. doi: 10.2105/ajph.84.6.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Stable EJ, Sabogal F, Otero-Sabogal R, Hiatt RA, McPhee SJ. Misconceptions about cancer among Latinos and Anglos. Journal of the American Medical Association. 1992;268:3219–3223. doi: 10.1001/jama.1992.03490220063029. [DOI] [PubMed] [Google Scholar]
- Powe BD. Cancer fatalism among elderly Caucasians and African Americans. Oncology Nursing Forum. 1995;22:1355–1359. [PubMed] [Google Scholar]
- Ramirez AG, Suarez L, Laufman L, Barrosa C, Chalela P. Hispanic women’s breast and cervical cancer knowledge, attitudes, and screening behavior. American Journal of Health Promotion. 2000;14:292–300. doi: 10.4278/0890-1171-14.5.292. [DOI] [PubMed] [Google Scholar]
- Rawls SM, Champion VL, Menon U. The impact of age and race on mammography practices. Health Care for Women International. 2000;21:583–597. doi: 10.1080/07399330050151833. [DOI] [PubMed] [Google Scholar]
- Rosales M, Gonzalez P. Mammography screening among Mexican, Central-American, and South-American women. Journal of Immigrant and Minority Health. 2013;15:225–233. doi: 10.1007/s10903-012-9731-2. [DOI] [PubMed] [Google Scholar]
- Ruiz MS, Marks G, Richardson JL. Language acculturation and screening practices of elderly Hispanic women: The role of exposure to health-related information from the media. Journal of Aging and Health. 1992;4:268–281. doi: 10.1177/089826439200400206. [DOI] [PubMed] [Google Scholar]
- Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: A systematic quantitative review of the literature. Journal of Women’s Health. 2008;17:1477–1498. doi: 10.1089/jwh.2007.0603. [DOI] [PubMed] [Google Scholar]
- Shelton RC, Jandorf L, Thelemaque L, King S, Erwin DO. Sociocultural determinants of breast and cervical cancer screening adherence: An examination of variation among immigrant Latinas by country of origin. Journal of Health Care for the Poor and Underserved. 2012;23:1268–1792. doi: 10.1353/hpu.2012.0191. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith A, Nelson A, editors. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Suarez L. Pap smear and mammogram screening in Mexican-American women: The effects of acculturation. American Journal of Public Health. 1994;84:742–746. doi: 10.2105/ajph.84.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suarez L, Roche RA, Nichols D, Simpson DM. Knowledge, behavior, and fears concerning breast and cervical cancer among older low-income Mexican American women. American Journal Preventive Medicine. 1997;13:137–142. [PubMed] [Google Scholar]
- Tejada S, Thompson B, Coronado GD, Martin DP. Barriers and facilitators related to mammography use among lower educated Mexican women in the USA. Social Science & Medicine. 2009;68:832–839. doi: 10.1016/j.socscimed.2008.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. Screening for breast cancer: U.S. preventive services task force recommendation statement. Annals of Internal Medicine. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- Wells KJ, Roetzheim R. Health disparities in receipt of screening mammography in Latinas: A critical review of recent literature. Cancer Control. 2007;14:369–379. doi: 10.1177/107327480701400407. [DOI] [PubMed] [Google Scholar]
- Wu ZH, Black SA, Markides KS. Prevalence and associated factors of cancer screening: Why are so many older Mexican American women never screened? Preventive Medicine. 2001;33:268–273. doi: 10.1006/pmed.2001.0880. [DOI] [PubMed] [Google Scholar]
- Zambrana RE, Breen N, Fox SA, Gutierrez-Mohamed ML. Use of cancer screening practices by Hispanic women: Analyses by subgroup. Preventive Medicine. 1999;29:466–477. doi: 10.1006/pmed.1999.0566. [DOI] [PubMed] [Google Scholar]
- Zsembik BA, Fennell D. Ethnic variation in health and the determinants of health among Latinos. Social Science & Medicine. 2005;61:53–63. doi: 10.1016/j.socscimed.2004.11.040. [DOI] [PubMed] [Google Scholar]