ABSTRACT
Introduction
Dystrophinopathies are X‐linked muscle degenerative disorders that result in progressive muscle weakness complicated by bone loss. This study's goal was to evaluate feasibility and tolerability of whole‐body, low‐intensity vibration (WBLIV) and its potential effects on muscle and bone in patients with Duchenne or Becker muscular dystrophy.
Methods
This 12‐month pilot study included 5 patients (age 5.9–21.7 years) who used a low‐intensity Marodyne LivMD plate vibrating at 30–90 Hz for 10 min/day for the first 6 months. Timed motor function tests, myometry, and peripheral quantitative computed tomography were performed at baseline and at 6 and 12 months.
Results
Motor function and lower extremity muscle strength remained either unchanged or improved during the intervention phase, followed by deterioration after WBLIV discontinuation. Indices of bone density and geometry remained stable in the tibia.
Conclusions
WBLIV was well tolerated and appeared to have a stabilizing effect on lower extremity muscle function and bone measures. Muscle Nerve 55: 875–883, 2017
Keywords: Becker muscular dystrophy, Duchenne muscular dystrophy, myometry, pQCT, timed function test, vibration
Abbreviations
- 6MWT
6‐minute walk test
- BMC
bone mineral content
- BMD
Becker muscular dystrophy
- BSI
bone strength index
- CSA
cross‐sectional area
- DMD
Duchenne muscular dystrophy
- ISO
International Standards Organization
- pQCT
peripheral quantitative computer tomography
- TFT
timed function test
- vBMD
volumetric bone mineral density
- WBLIV
whole‐body, low‐intensity vibration
Dystrophinopathy (OMIM #310200) is a muscular dystrophy with a recessive X‐linked inheritance mode, caused by loss‐of‐function mutations in the gene encoding dystrophin.1 The clinical presentation ranges from more severe manifestations in Duchenne muscular dystrophy (DMD) to a milder allelic Becker muscular dystrophy (BMD).2, 3 Dystrophin is critical for structural stability of myofibers in skeletal, diaphragm, and cardiac muscles.4 In dystrophinopathy, its deficiency compromises functional integrity of muscle fibers and leads to progressive weakness manifesting as difficulty running and walking, rising from the floor, and taking stairs. Eventually, loss of ambulation, respiratory insufficiency, and cardiomyopathy ensue and lead to death due to cardiorespiratory compromise. During the ambulatory stage of the disease, boys with dystrophinopathies walk less and at a much slower pace, are significantly less active than healthy peers, and are at risk of frequent falls.
A progressive decline in muscle function with age is accompanied by a decline in bone mineral density and bone quality, leading to increased bone fragility and long‐bone and vertebral fractures.5, 6, 7, 8 In many cases, a bone fracture an inciting event that ends the ambulatory stage in these patients. Bone loss in dystrophinopathies is multifactorial due to reduced physical activity, immobility, long‐term glucocorticoid treatment, hypogonadism, low vitamin D levels, inflammatory changes, and other metabolic abnormalities related to the disease process.9, 10
The primary goal in treating boys with dystrophinopathies is to provide supportive measures through multidisciplinary care. The only accepted pharmacologic treatment thus far that slows disease progression is the use of glucocorticoids.11 Unfortunately, long‐term use of glucocorticoids is associated with significant multisystem side effects, including bone loss.12 Physical and occupational therapy play a major role, including stretching exercises to prevent contractures, and assistive devices to prolong ambulation and maintain independence,13 but these interventions do little to help preserve bone health.
Mechanical vibration has gained considerable interest as a way to improve muscle function and serve as a bone‐sparing strategy in children with disabling conditions, such as cerebral palsy,14, 15, 16 osteogenesis imperfecta, or spinal dysraphism.17 However, clinicians have been hesitant to use mechanical vibration in patients with dystrophinopathies due to concern about possible further damage to the diseased muscle.18, 19, 20, 21, 22 A number of whole‐body vibration platforms are currently available, which vary in terms of vibration intensity (expressed in g‐force, or “g”)23 and mode of vibration transmission (synchronous, meaning applied to both feet at the same time, or side‐alternating). Low‐intensity vibration devices deliver a force <1g (1g is earth's gravitational field), whereas high‐intensity vibration devices deliver acceleration intensity >1g (as high as 16.3g). In some cases, this exceeds the safety threshold limit values established by the International Standards Organization (ISO‐2631), depending on the vibration frequency and duration of exposure.23, 24
In recent years, 3 pilot studies have been published that examine the safety of whole‐body vibration in patients with DMD using high‐intensity, side‐alternating vibration platforms (Galileo training) for 4 weeks to 3 months, with varied target vibration frequencies of 15–24 Hz.25, 26, 27 These studies concluded that whole‐body vibration treatment was safe and tolerated by these patients, although its effect on bone and muscle was inconclusive.
None of the published studies addressed the effects of a low‐intensity vibrating platform in patients with DMD or BMD. Novotny et al. first investigated this approach in a preclinical study using the mdx mouse model for DMD.28 The mdx mice were subjected to low‐magnitude, whole‐body vibration at a frequency of 30–90 Hz, based on our previous work that identified 45 Hz as most effective at increasing the expression of osteogenic genes.29 There was no evidence of loss of force generation or any other parameter of muscle contractility measured during 8 weeks of vibration training, which supported the notion that whole‐body, low‐magnitude vibration (WBLIV) is not deleterious to dystrophic muscles30 and has the potential to improve muscle contractility.
The primary aim of this pilot study was to test the feasibility and tolerability of low‐intensity vibration as a therapeutic approach for patients with dystrophinopathies using a portable Marodyne LivMD plate that delivers WBLIV with an oscillating frequency of 30–90 Hz, at a maximum g‐force of 0.4g, which is well within the ISO threshold limit values.23, 24 We hypothesized that this type of intervention would be feasible and well tolerated without adverse effects on the function of the lower extremity muscles with the greatest exposure to vibration. The secondary aim was to examine the effects of WBLIV on bone density, geometry, and strength of the tibia and radius. Because that transmissibility of vibrations is the highest to tissues closer to the source,31 the hypothesis was that the intervention would stabilize bone measures of the tibia but not the radius during the vibration intervention phase of the study.
METHODS
Participants
Participants were male patients (5.9–21.7 years old) with DMD or BMD confirmed through clinical examination and genetic testing, ambulatory (able to walk ≥ 75 meters unassisted), and not dependent on daytime ventilatory support. Exclusion criteria were treatment with human growth hormone or bisphosphonates, fracture within the last 4 weeks, or inability to stand for 10 minutes on flat feet. The participants were recruited from the Muscular Dystrophy Clinic at the University of Minnesota. Females who were manifesting carriers were not included due to minimal clinical manifestations. The study protocol was approved by the institutional review board at the University of Minnesota and was consistent with the requirements of the Declaration of Helsinki.
Study Procedures
The study design included 2 baseline evaluations 2 weeks apart, followed by a 6‐month intervention period and a subsequent 6‐month follow‐up period. At the initial visit, each patient underwent a physical examination with anthropometry and Tanner staging of pubertal development based on testicular volume (by orchidometer) and pubic hair, with the higher of the 2 values being recorded. Baseline, 6‐month, and 12‐month evaluations included timed motor function tests, quantitative myometry, and peripheral quantitative computed tomography (pQCT) of the tibia and non‐dominant radius.
Intervention
Each participant was given a portable Marodyne LivMD plate adjusted for lower weight (Marodyne Medical, Inc., Lakeland, Florida) to be used at home while free standing for 10 consecutive minutes per day,32 7 days per week for 6 months. The Marodyne LivMD plate is designed to deliver low‐magnitude (0.4g), high‐frequency vibration with an oscillating frequency of 30–90 Hz. Both participants and their caregivers were trained in the proper use of the vibratory plate. The first treatment was completed in the clinic after all baseline measurements were taken to demonstrate proper use of the plate. The second treatment took place at the subject's home the next day. The study coordinator called the participants every 2 weeks to ensure compliance. Information about other interventions, including night‐time splints, stretching, glucocorticoids, and novel drugs, is presented in Table 1.
Table 1.
Patients’ characteristics at baseline
| Patient 1 | Patient 2 | Patient 3 | Patient 4a | Patient 5 | Patient 6 | |
|---|---|---|---|---|---|---|
| Age (years) | 5.9 | 7.5 | 12.4 | 9.8 | 21.7 | 16.4 |
| Tanner stage | 1 | 2 | 2 | 1 | 5 | 5 |
| Height (Z‐score) | –2.2 | –2.0 | –3.6 | –0.1 | 0.3 | –0.7 |
| BMI (kg/m2) | 14.8 | 18.2 | 21.0 | 14.7 | 29.2 | 23.7 |
| BMI (Z‐score) | −0.5 | 1.2 | 1.0 | −1.2 | 1.7 | 0.9 |
| Diagnosis | DMD | DMD | DMD | DMD | BMD | BMD |
| Gene mutation | Dup exon 49, OOF | Del 55, OOF | Exon 32, c.4414T, p.Q1472X, OOF | Dup exon 2, OOF | Del exon 3–7, IF | Del exon 3–7, IF |
| Interventions in addition to WBLIV | DFZ, NTS, stretching | DFZ, NTS, stretching | DFZ, NTS, staluren, stretching | Pred, NTS, stretching | Stretching | Stretching |
BMD, Becker muscular dystrophy; DFZ, deflazacort; DMD, Duchenne muscular dystrophy; Del, deletion; Dup, duplication; IF, in‐frame; OOF, out‐of‐frame; WBLIV, whole‐body, low‐intensity vibration; NTS, night‐time splint; Pred, prednisone.
Dropped out of the study after 2 weeks due to worsening headaches.
Functional Assessment
The 6‐minute walk test (6MWT) was originally designed for adults, and for this reason it has been modified to fit the needs of children with muscular dystrophy.33 This version has been shown to be a reliable and valid measure of ambulation as well as safe and easy to perform in patients with dystrophinopathies without severe cognitive or behavioral problems. It is a submaximal exercise test, and because most activities of daily living are performed at a submaximal level, 6MWT reflects function. Briefly, the 6MWT was assessed using a 25‐meter taped line with 1‐meter marked intervals and cones at each end of the tape to mark the ambulatory path. Arrows were placed at the end of the cones in a counterclockwise direction to define the direction of ambulation. Continuous moderate verbal encouragement was allowed throughout the testing period. In addition, a “safety chaser” followed the child throughout the test to keep him on the correct path, to be in close proximity in case of a fall to help him to a standing position, or to tend to him quickly if an injury occurred. The following timed function tests (TFTs) were also performed: the time‐to‐run/walk test, measuring the time (in seconds) to walk or run, if possible, a distance of 10 meters; the time‐to‐climb‐4‐stairs test, measuring the time (in seconds) to ascend 4 standard stairs; and the supine‐to‐stand test, measuring the time (in seconds) for the child to assume a standing position from a supine starting position.34, 35
Quantitative Myometry
Strength testing included quantitative myometry using a handheld dynamometer (PowerTrack II Commander; JTech Medical, Midvale, Utah) to measure the maximum voluntary isometric force during muscle contraction of ankle plantar flexion, ankle dorsiflexion, hip flexion, knee flexion/extension, and elbow flexion/extension.36 Values were recorded as Newtons of force. Participants were asked to perform each test bilaterally, and the average of the 2 forces produced was used in analyses.
Peripheral Quantitative Computed Tomography
Measures of cortical and trabecular bone and estimated bone strength were obtained using peripheral quantitative computed tomography (pQCT; XCT‐3000; Stratec Medizintechnik GmbH, Pforzheim, Germany). Images were taken at the distal 3% and 33% of the non‐dominant radius with a scan speed of 20 mm/s. The distal 3% and 38% sites of the tibia were scanned at 25 mm/s. All scan sites had a section thickness of 2.4 mm and a voxel size of 0.4 mm. The reference line for both tibia and radius was placed at the proximal end of the distal growth plate using a scout view speed of 50 mm/s with a 1‐mm step width. Image processing and calculation of bone parameters were completed using the manufacturer's software (version 6.0). Phantom scanning was done daily for quality control.
Bone outcome measures37 at metaphyseal sites included trabecular volumetric bone mineral density (vBMD; mg/cm3), trabecular cross‐sectional area (CSA; mm2), and total bone strength index (BSI; mg2/mm4) using contour mode 3 with a threshold of 169 mg/cm3 and peel mode 4 threshold 650 mg/cm3 with 10% concentric peel at the tibia and 15% at the radius. At diaphyseal sites, the measures included cortical vBMD, cortical CSA, cortical bone mineral content (BMC; mg/mm), and cortical thickness (mm), using cort mode 2 with a threshold of 710 mg/cm3. Non‐weighted polar section modulus (mm3) and strength strain index (mm3) were measured at the 38% tibia site using cort mode 2 with a threshold of 480 mg/cm3.
Statistical Analysis
For each outcome measure, the statistical analysis included a mixed linear model to account for correlation of multiple visits within person, with random‐effect person and fixed‐effect visit. In the analysis, the 2 baseline evaluations were included as separate visits; changes from baseline to 6 or 12 months were estimated and tested as contrasts in the visit fixed effect, specifically as the 6‐month visit (or 12‐month visit) minus the average of the 2 baseline visits. A measure's percent change was calculated from 0 to 6 months, from 6 to 12 months, and from 0 to 12 months. No adjustments were made for multiple testing, because these results are preliminary and because the primary interest is in the broad pattern of results, not results for individual measures. All analyses were performed using JMP software (JMP version 12 Pro; SAS Institute, Inc., Cary, North Carolina).
RESULTS
Study Participation
Six patients were enrolled in the study. One patient (patient 4) with attention deficit hyperactivity disorder and a prior history of headaches had worsening headaches during the first 2 weeks of intervention. Although headaches were deemed unrelated to the study, he found the exercise routine an excessive burden and dropped out after 2 weeks. The remaining 5 patients completed the study and did not report any difficulty with using the platform, muscle pain, cramps, or any other adverse events. Table 1 shows characteristics of all 6 patients. None of the patients had fractures.
6‐Minute Walk Test
Overall, 6MWT results showed no significant change in distance walked over the course of this study. When analyzed for individual participants, the 6MWT results were consistent with the natural history reported previously38 and predicted by baseline distance, age, or genetic mutation (out‐of‐frame vs in‐frame). Patient 3 had an out‐of‐frame mutation and had a decline in the distance by 53 meters over the course of 12 months from 369 to 316 meters, which is consistent with the expected decline because of his baseline distance. Another participant (patient 2) showed a decline of 28 meters from 410.3 to 382 meters. The results for the remaining 3 participants were essentially unchanged.
Timed Function Tests
Motor function remained stable in all TFTs during the 6 months of intervention with WBLIV, followed by deterioration during the subsequent 6 months without WBLIV, which is consistent with the expected progressive deterioration in muscle function over time in dystrophinopathies. The time‐to‐climb‐4‐stairs test showed a 74.8% longer time at 12 months compared with 6 months. The time‐to‐stand test showed 70.9% longer time at 12 months compared with 6 months (Table 2 and Fig. 1). In both tests, 4 of 5 participants showed significant (>10%) increases in time after WBLIV was discontinued at 6 months. Only 1 patient with BMD, who had the best function in this group (patient 6), remained unchanged. The changes from baseline to 12 months were also significant. Although performance in the 10‐meter walk test did not change significantly during the intervention phase (0–6 months), the walking time was 23.6% longer at 12 months compared with baseline. In this test, only 3 patients showed an increase in time of >10%, and 2 remained unchanged.
Table 2.
Timed motor function tests before and after 6 months of vibration training and 6 months after discontinuation of vibration
| Time‐points | Estimated change ± SE and percent change | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 6 months | 12 months | 0–6 months | % | 6–12 months | % | 0–12 months | % | |
| 6‐min walk (m) | 412 | 395 | 396 | −16.8 ± 12.0 | −4.1 | 0.8 ± 13.9 | 0.2 | −16.0 ± 12.0 | −3.9 |
| 10‐m walk (s) | 5.6 | 6.0 | 7.0 | 0.4 ± 0.5 | 6.4 | 1.0 ± 0.6 | 16.2 | 1.3 ± 0.5 | 23.6a |
| Stair climb (s) | 4.0 | 3.9 | 6.8 | −0.1 ± 0.4 | −2.9 | 2.9 ± 0.5c | 74.8c | 2.8 ± 0.4c | 69.9c |
| Supine to stand (s) | 6.3 | 6.5 | 11.1 | 0.2 ± 1.6 | 3.9 | 4.6 ± 1.9a | 70.9a | 4.9 ± 1.6b | 77.6b |
Data are shown as adjusted means, estimated change ± standard error (SE), and percent change.
P < 0.05;
P < 0.01;
P < 0.001.
Figure 1.
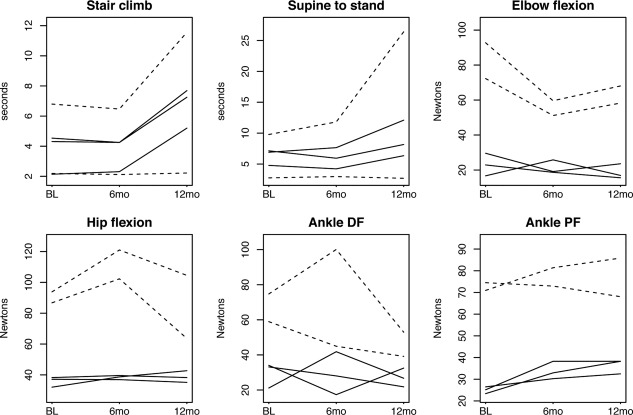
Plots of selected timed motor function tests and myometry for individual patients. Dashed lines: patients with Becker muscular dystrophy; solid lines: patients with Duchenne muscular dystrophy. DF, dorsiflexion; PF, plantar flexion.
Muscle Strength Testing
Muscle strength was measured by quantitative myometry. Elbow flexion strength decreased by 25.4% in the first 6 months compared with baseline and remained below baseline at 12 months (by 22.1%, Table 3) with changes more pronounced in patients with BMD (Fig. 1). There was no change in elbow extension strength (Table 3). Among lower extremity measures, ankle plantar flexion strength improved by 16% during the 6‐month intervention period and remained above baseline at 12 months (19%). All participants showed an increase in ankle plantar flexion strength, ranging from 8% to 48% when compared with baseline. Ankle dorsiflexion strength remained stable during the intervention phase and decreased by 25.4% after discontinuation of vibration training, although this change was not statistically significant. There was also a trend toward an increase in force in hip flexion during WBLIV (by 17.6%), followed by a 16% decrease toward baseline over the next 6 months (Table 3); these changes were also more apparent in patients with BMD. Overall, measures of upper extremity strength were either no different or worse over the 6‐month intervention period, whereas measures of lower extremity strength were either stable or showed increased force after the 6‐month intervention phase.
Table 3.
Myometry before and after 6 months of vibration training and 6 months after discontinuation of vibration
| Time‐points | Estimated change ± SE and percent | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 6 months | 12 months | 0–6 months | % | 6–12 months | % | 0–12 months | % | |
| Elbow flexion | 46.8 | 34.9 | 36.5 | −11.9 ± 4.7a | −25.4a | 1.6 ± 5.4 | 4.5 | −10.3 ± 4.7a | −22.1a |
| Elbow extension | 33.2 | 36.3 | 32.5 | 3.2 ± 2.8 | 9.5 | −3.8 ± 3.2 | −10.4 | −0.6 ± 2.8 | −1.9 |
| Hip flexion | 57.6 | 67.7 | 56.9 | 10.1 ± 5.0 | 17.6 | −10.8 ± 5.8 | −16.0 | −0.7 ± 5.0 | −1.2 |
| Knee flexion | 50.0 | 53.2 | 56.3 | 3.2 ± 4.0 | 6.4 | 3.0 ± 4.6 | 5.7 | 6.3 ± 4.0 | 12.5 |
| Knee extension | 60.0 | 59.6 | 63.2 | −0.4 ± 5.5 | −0.7 | 3.6 ± 6.4 | 6.0 | 3.2 ± 5.5 | 5.2 |
| Ankle dorsiflexion | 44.4 | 46.4 | 34.6 | 2.0 ± 5.7 | 4.5 | −11.8 ± 6.5 | −25.4 | −9.8 ± 5.7 | −22.0 |
| Ankle plantar flexion | 44.0 | 51.1 | 52.4 | 7.0 ± 3.2a | 16.0a | 1.3 ± 3.7 | 2.6 | 8.4 ± 3.2a | 19.0a |
Data are shown as adjusted mean (expressed in Newtons of force), estimated change ± standard error (SE), and percent change.
P < 0.05.
Bone Measures with Peripheral Quantitative Computed Tomography
Measures of bone density and geometry of the radius are shown in Table 4. Downward trends were noted in most measures, with statistically significant decreases in the cortical CSA, cortical BMC, cortical thickness, and BSI during the first 6 months followed by no significant changes during months 6–12.
Table 4.
pQCT bone measures for the radius before and after 6 months of vibration training and 6 months after discontinuation of vibration
| Time‐points | Estimated change ± SE and percent change | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 6 months | 12 months | 0–6 months | % | 6–12 months | % | 0–12 months | % | |
| Trabecular vBMD | 224.1 | 211.0 | 203.0 | –13 ± 12.9 | −5.8 | −7.6 ± 13.6 | −3.6 | −20.6 ± 21.1 | −9.2 |
| Trabecular CSA | 206.8 | 196.0 | 175.0 | −10.5 ± 42.7 | −5.1 | −21.1 ± 45.0 | −10.8 | −31.7 ± 69.9 | −15.3 |
| Cortical vBMD | 1,143.5 | 1,146.0 | 1,151.0 | 2.4 ± 23.7 | 0.2 | 4.7 ± 24.7 | 0.4 | 7.1 ± 37.3 | 0.6 |
| Cortical CSA | 68.5 | 64.0 | 65.0 | −4.7 ± 1.5a | −6.8a | 0.9 ± 1.6 | 1.3 | −3.8 ± 2.4 | −5.6 |
| Cortical BMC | 79.1 | 73.8 | 74.8 | −5.3 ± 1.8a | −6.7a | 1.1 ± 1.9 | 1.4 | −4.2 ± 2.9 | −5.4 |
| CT | 2.92 | 2.78 | 2.80 | −0.14 ± 0.05a | −4.8a | 0.02 ± 0.05 | 0.7 | −0.12 ± 0.08 | −4.1 |
| BSI | 31.8 | 27.0 | 26.0 | −4.3 ± 1.9a | −13.6a | −1.2 ± 1.9 | −4.2 | −5.5 ± 3.1 | −17.2 |
| Zp | 186.7 | 179.0 | 180.0 | −7.3 ± 5.6 | −3.9 | 0.2 ± 5.9 | 0.1 | −7.1 ± 8.8 | −3.8 |
| SSI | 154.7 | 154.0 | 156.0 | −0.2 ± 5.2 | −0.1 | 1.9 ± 5.8 | 1.2 | 1.6 ± 8.2 | 1.0 |
Data are shown as adjusted means for the radius length, estimated change ± standard error (SE), and percent change. BMC, bone mineral content (mg/mm); BSI, bone strength index (mg2/mm4); CT, cortical thickness (mm); CSA, cross‐sectional area (mm2); vBMD, volumetric bone mineral density (mg/cm3); Zp, polar section modulus (mm3); SSI, strength strain index (mm3).
Significant change, P < 0.05.
In the tibia, there was a trend toward an increase in trabecular CSA during the intervention phase (by 25% compared with baseline; Table 5). Other indices of bone geometry and strength did not change significantly.
Table 5.
pQCT bone measures for the tibia before and after 6 months of vibration training as well as 6 months after discontinuation of vibration
| Time‐points | Estimated change ± SE and percent change | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 6 months | 12 months | 0–6 months | % | 6–12 months | % | 0–12 months | % | |
| Trabecular vBMD | 201.2 | 207.0 | 199.0 | 6.2 ± 5.4 | 3.1 | −8.5 ± 6.2 | −4.1 | −2.2 ± 8.1 | −1.1 |
| Trabecular CSA | 544.0 | 680.0 | 627.0 | 136.1 ± 66.7 | 25.0 | −52.8 ± 75.8 | −7.8 | 83.3 ± 99.9 | 15.3 |
| Cortical vBMD | 1,111.6 | 1,129.0 | 1,134.0 | 17.0 ± 25.1 | 1.5 | 5.7 ± 28.3 | 0.5 | 22.7 ± 35.4 | 2.0 |
| Cortical CSA | 178.8 | 175.0 | 171.0 | −3.6 ± 7.2 | −2.0 | −4.0 ± 8.1 | −2.3 | −7.6 ± 10.2 | −4.2 |
| Cortical BMC | 202.2 | 198.5 | 195.8 | −3.7 ± 7.4 | −1.8 | −2.7 ± 8.4 | −1.4 | −6.4 ± 10.5 | −3.2 |
| CT | 3.99 | 4.01 | 3.97 | 0.03 ± 0.1 | 0.8 | −0.04 ± 0.11 | −1.0 | −0.02 ± 0.14 | −0.5 |
| BSI | 60.8 | 60.0 | 58.0 | −1.0 ± 1.5 | −1.6 | −1.6 ± 1.7 | −2.7 | −2.6 ± 2.2 | −4.3 |
| Zp | 1042.7 | 998.0 | 928.0 | −44.8 ± 46.9 | −4.3 | −70.1 ± 53.0 | −7.0 | −115.0 ± 66.3 | −11.0 |
| SSI | 928.1 | 886.0 | 834.0 | −41.6 ± 37.0 | −4.5 | −52.2 ± 41.9 | −5.9 | −93.8 ± 52.3 | −10.1 |
Data are shown as adjusted means for the tibia length, estimated change ± SE, and percent change. BMC, bone mineral content (mg/mm); BSI, bone strength index (mg2/mm4); CT, cortical thickness (in mm); CSA, cross‐sectional area (mm2); vBMD, volumetric bone mineral density (mg/cm3); Zp, polar section modulus (mm3); SSI, strength strain index (mm3).
DISCUSSION
In this pilot study of 5 patients with dystrophinopathies, we have shown that intervention with low‐intensity vibration using a portable Marodyne LivMD plate was well tolerated by ambulatory patients with DMD or BMD, without adverse effects on the function of the lower extremity muscles with the greatest exposure to vibration. The patients did not experience increased fatigue, muscle soreness, cramps, falls, or fractures. The portability and ease of use of a WBLIV plate made it suitable for use at home on a daily basis and without a therapist.
Motor capacity measured by TFTs remained stable during the 6 months of WBLIV intervention, followed by deterioration in the time‐to‐climb‐4 stairs test and the time‐to‐stand test after discontinuation of vibration training, suggesting that WBLIV does not have deleterious effects and may have a stabilizing effect on muscle function. Lack of appreciable change in the 6MWT may have been due to small sample size or variability in the natural history. Longitudinal studies have shown that boys <7 years of age with DMD typically have an increase in 6MWT over a year, whereas boys >7 years of age may have more of a plateau or decline in 6MWT performance.33, 38 There is little to no information about the changes expected in 6MWT over 6–12 months in patients with BMD.
Measures of muscle strength by quantitative myometry in the lower extremities were either stable or showed a trend for improvement during the 6‐month intervention phase, particularly in hip flexion and ankle plantar flexion strength. Although not statistically significant, an increase of 18% in hip flexion during the 6 months of the intervention is intriguing and suggests a positive trend. These results are corroborated by the time to climb 4 stairs, which showed an increase in 4 of 5 boys after discontinuation of intervention. Likewise, stabilization of ankle dorsiflexion after the intervention phase suggests a positive trend as compared with a 25% decrease in force after a 6‐month period without intervention. In contrast, no trends for improvement were observed in muscle strength of the upper extremities. WBLIV appeared to have a stabilizing effect on the pQCT measures of bone density and geometry of the tibia, and less so of the radius.
There is a suggestion of a differential effect of WBLIV on upper vs. lower extremity muscle strength and bone indices with a trend for improvement in both muscle and bone measures in the lower extremities. This may have been due to a positive effect of WBLIV on skeletal muscle tissue and bone in close proximity to the vibrating platform. This finding is consistent with other studies showing that skeletal regions closest to the source of vibration have more robust responses39 compared with distal sites, where transmission is diminished.31 The decrease in biceps strength during the first 6 months of intervention was likely due to natural disease progression. In fact, the purpose of assessing the upper extremities in this study was to have an “internal” control for disease progression. This change is less likely to represent a deleterious effect of vibration because of its distance from the vibrating platform. However, this finding should be explored further in future studies.
In this investigation we have examined the effects of a low‐intensity synchronous vibrating platform. Three previous studies performed on boys with DMD used a high‐intensity, side‐alternating vibration platform.25, 26, 27 These 3 studies aimed primarily to examine safety and tolerability of vibration training, and all found whole‐body vibration to be feasible and safe, similar to our study and consistent with our preclinical observations.28 Besides using a different platform, the earlier studies used a shorter duration of vibration training and a lower frequency of vibration.
In the first study, from Sweden,26 6 ambulatory patients with DMD used whole‐body vibration (at 16–24 Hz) for up to 6 minutes, 2 or 3 times weekly for 3 months. No changes in trabecular or cortical density of the tibia, muscle strength, motor function, or bone turnover markers were observed, except for a trend toward an increase in a bone‐specific alkaline phosphatase level and muscle density (by pQCT). The lack of a noticeable positive effect of vibration training on muscle and bone was thought to be due to small sample size, low vibration frequency, or short duration of training.
The second study, from Canada,27 involved 4 ambulatory patients with DMD who participated in vibration therapy sessions (target frequency 20 Hz), each consisting of vibration 2 minutes on, 60 seconds off, 2 minutes on, 3 times per week during a 4‐week training period, without any resultant major changes in functional mobility. The third study, from Germany,25 included 14 ambulatory boys with DMD and 8 with spinal muscular atrophy. Galileo training (target frequency 15–18 Hz) was performed for 9 minutes, twice a day for 5 days per week for 8 weeks. Although no clear statistically significant effect of whole‐body vibration training was observed on muscle strength, function, or flexibility, some positive trends were noted. For example, patients with DMD had small improvements in 6MWT, stair‐climb test, muscle strength of the legs (knee myometry and ankle dorsiflexion), and angular degree of ankle dorsiflexion. These trends suggest that a longer training period may be needed to see a greater impact of vibration training. Overall, the effect of whole‐body vibration on bone and muscle using a side‐alternating vibration platform for 4–18 min/day, 2–5 times weekly for 4 weeks to 3 months, with target vibration frequencies of 15–24 Hz, was considered indeterminate.
We chose a 10‐minute duration of low‐intensity vibration training based on previous reports that low‐magnitude, high‐frequency, whole‐body vibration treatment for 10 min/day resulted in increases in both bone and muscle mass in young women with low bone mineral density.32 The vibration frequency delivered by the Marodyne LivMD plate, 30–90 Hz, is similar to the frequency found to be safe and without deleterious effects on diseased muscle in an mdx mouse model of DMD.28 Recent data show that, although high‐intensity training induces muscle damage in mdx mice, low‐intensity training reduces the level of protein carbonylation, a marker of oxidative damage, and rescues the mdx phenotype.40 The duration of daily vibration therapy in our study was 6 months, which is the longest intervention so far and which could explain some of the promising positive effects on muscle function and strength. Our data further suggest that this intervention may need to continue long term to maintain the improvements observed.
Other forms of physical training have also shown promise in delaying functional deterioration in patients with dystrophinopathies. For example, in a randomized, controlled trial in 30 boys with DMD that involved assisted bicycle training for 24 weeks, the motor function measure score remained stable in the intervention group, yet it decreased significantly in the control group.41 In the control group, 3 boys lost the ability to walk 10 meters, and 2 boys lost the ability to rise from the floor. In the intervention group, none of the boys lost the ability to walk 10 meters, and only 1 boy lost the ability to rise from the floor during the training period. Range of motion remained relatively stable in the intervention group during the training period. Likewise, resistance training of upper and lower extremity muscles can increase muscle strength in muscular dystrophies, as shown by Sveen et al.,42 who assessed 2 patients with BMD and 6 with limb‐girdle muscular dystrophy. They found that elbow flexion and knee extension improved significantly after 6 months of low‐intensity resistance training.
The limitations of this and other studies include a small sample size, heterogeneous patient populations, and absence of matched controls. The analyses were necessarily exploratory and did not adjust for multiple comparisons. Although our study demonstrated the feasibility and tolerability of this approach in patients with dystrophinopathies, any observable positive effects on muscle and bone, albeit encouraging, should be considered preliminary. The findings lay the groundwork for a larger, controlled trial to establish effective vibration parameters for a given type of platform, taking cost and portability into account. Because any biological effect of vibration is likely to decrease with increasing distance from the synchronous vibrating platform, a supplemental device that can be placed on the elbows16 or supplemental upper extremity exercise training may be needed.43 Vry et al.25 showed that at least a portion of the clinically significant increase in joint flexibility could be attributed to mechanical stretching due to vibration. Thus, consideration should be given to supplementing traditional physiotherapy with whole‐body vibration as future rehabilitative approaches.
The authors thank Dr. Jamie Marsh, who performed assessments of muscle function and strength; Rebecca Hollister and Alise Thone for technical assistance with pQCT scanning; and the patients and their families for participation in the study.
This study was supported by grants from the Maslowski Foundation (to P.K.), the Muscular Dystrophy Association (114071 to D.L.), and the National Center for Advancing Translational Sciences of the National Institutes of Health (UL1TR000114).
Disclaimer: The content of this study is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1. Wein N, Alfano L, Flanigan KM. Genetics and emerging treatments for Duchenne and Becker muscular dystrophy. Pediatr Clin N Am 2015;62:723–742. [DOI] [PubMed] [Google Scholar]
- 2. Punnoose AR, Burke AE, Golub RM. JAMA patient page. Muscular dystrophy. JAMA 2011;306:2526. [DOI] [PubMed] [Google Scholar]
- 3. Flanigan KM. Duchenne and Becker muscular dystrophies. Neurol Clin 2014;32:671–688. [DOI] [PubMed] [Google Scholar]
- 4. Deconinck N, Dan B. Pathophysiology of Duchenne muscular dystrophy: current hypotheses. Pediatr Neurol 2007;36:1–7. [DOI] [PubMed] [Google Scholar]
- 5. Sbrocchi AM, Rauch F, Jacob P, McCormick A, McMillan HJ, Matzinger M, et al The use of intravenous bisphosphonate therapy to treat vertebral fractures due to osteoporosis among boys with Duchenne muscular dystrophy. Osteoporos Int 2012;23:2703–2711. [DOI] [PubMed] [Google Scholar]
- 6. Larson CM, Henderson RC. Bone mineral density and fractures in boys with Duchenne muscular dystrophy. J Pediatr Orthop 2000;20:71–74. [PubMed] [Google Scholar]
- 7. Houston C, Mathews K, Shibli‐Rahhal A. Bone density and alendronate effects in Duchenne muscular dystrophy patients. Muscle Nerve 2014;49:506–511. [DOI] [PubMed] [Google Scholar]
- 8. McDonald DG, Kinali M, Gallagher AC, Mercuri E, Muntoni F, Roper H, et al Fracture prevalence in Duchenne muscular dystrophy. Dev Med Child Neurol 2002;44:695–698. [DOI] [PubMed] [Google Scholar]
- 9. Bianchi ML, Mazzanti A, Galbiati E, Saraifoger S, Dubini A, Cornelio F, et al Bone mineral density and bone metabolism in Duchenne muscular dystrophy. Osteoporos Int 2003;14:761–767. [DOI] [PubMed] [Google Scholar]
- 10. Aparicio LF, Jurkovic M, DeLullo J. Decreased bone density in ambulatory patients with Duchenne muscular dystrophy. J Pediatr Orthop 2002;22:179–181. [PubMed] [Google Scholar]
- 11. Yilmaz O, Karaduman A, Topaloglu H. Prednisolone therapy in Duchenne muscular dystrophy prolongs ambulation and prevents scoliosis. Eur J Neurol 2004;11:541–544. [DOI] [PubMed] [Google Scholar]
- 12. King WM, Ruttencutter R, Nagaraja HN, Matkovic V, Landoll J, Hoyle C, et al Orthopedic outcomes of long‐term daily corticosteroid treatment in Duchenne muscular dystrophy. Neurology 2007;68:1607–1613. [DOI] [PubMed] [Google Scholar]
- 13. Ciafaloni E, Moxley RT. Treatment options for Duchenne muscular dystrophy. Curr Treat Options Neurol 2008;10:86–93. [DOI] [PubMed] [Google Scholar]
- 14. Ruck J, Chabot G, Rauch F. Vibration treatment in cerebral palsy: a randomized controlled pilot study. J Musculoskelet Neuronal Interact 2010;10:77–83. [PubMed] [Google Scholar]
- 15. Ward K, Alsop C, Caulton J, Rubin C, Adams J, Mughal Z. Low magnitude mechanical loading is osteogenic in children with disabling conditions. J Bone Miner Res 2004;19:360–369. [DOI] [PubMed] [Google Scholar]
- 16. Reyes ML, Hernandez M, Holmgren LJ, Sanhueza E, Escobar RG. High‐frequency, low‐intensity vibrations increase bone mass and muscle strength in upper limbs, improving autonomy in disabled children. J Bone Miner Res 2011;26:1759–1766. [DOI] [PubMed] [Google Scholar]
- 17. Semler O, Fricke O, Vezyroglou K, Stark C, Schoenau E. Preliminary results on the mobility after whole body vibration in immobilized children and adolescents. J Musculoskelet Neuronal Interact 2007;7:77–81. [PubMed] [Google Scholar]
- 18. Moens P, Baatsen PH, Marechal G. Increased susceptibility of EDL muscles from mdx mice to damage induced by contractions with stretch. J Muscle Res Cell Motil 1993;14:446–451. [DOI] [PubMed] [Google Scholar]
- 19. Petrof BJ, Shrager JB, Stedman HH, Kelly AM, Sweeney HL. Dystrophin protects the sarcolemma from stresses developed during muscle contraction. Proc Natl Acad Sci USA 1993;90:3710–3714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Necking LE, Lundstrom R, Dahlin LB, Lundborg G, Thornell LE, Friden J. Tissue displacement is a causative factor in vibration‐induced muscle injury. J Hand Surg Br 1996;21:753–757. [DOI] [PubMed] [Google Scholar]
- 21. Murfee WL, Hammett LA, Evans C, Xie L, Squire M, Rubin C, et al High‐frequency, low‐magnitude vibrations suppress the number of blood vessels per muscle fiber in mouse soleus muscle. J Appl Physiol (1985) 2005;98:2376–2380. [DOI] [PubMed] [Google Scholar]
- 22. Necking LE, Lundstrom R, Lundborg G, Thornell LE, Friden J. Skeletal muscle changes after short term vibration. Scand J Plast Reconstr Surg Hand Surg 1996;30:99–103. [DOI] [PubMed] [Google Scholar]
- 23. Muir J, Kiel DP, Rubin CT. Safety and severity of accelerations delivered from whole body vibration exercise devices to standing adults. J Sci Med Sport 2013;16:526–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Evaluation of Human Exposure to Whole Body Vibration. Geneva: International Standards Organization; 1997. Available from: International Standards Organization. Specific to ISO‐2631.
- 25. Vry J, Schubert IJ, Semler O, Haug V, Schonau E, Kirschner J. Whole‐body vibration training in children with Duchenne muscular dystrophy and spinal muscular atrophy. Eur J Paediatr Neurol 2014;18:140–149. [DOI] [PubMed] [Google Scholar]
- 26. Soderpalm AC, Kroksmark AK, Magnusson P, Karlsson J, Tulinius M, Swolin‐Eide D. Whole body vibration therapy in patients with Duchenne muscular dystrophy—a prospective observational study. J Musculoskelet Neuronal Interact 2013;13:13–18. [PubMed] [Google Scholar]
- 27. Myers KA, Ramage B, Khan A, Mah JK. Vibration therapy tolerated in children with Duchenne muscular dystrophy: a pilot study. Pediatr Neurol 2014;51:126–129. [DOI] [PubMed] [Google Scholar]
- 28. Novotny SA, Mader TL, Greising AG, Lin AS, Guldberg RE, Warren GL, et al Low intensity, high frequency vibration training to improve musculoskeletal function in a mouse model of Duchenne muscular dystrophy. PloS One 2014;9:e104339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Novotny SA, Eckhoff MD, Eby BC, Call JA, Nuckley D, Lowe DA. Musculoskeletal response of dystrophic mice to short term, low intensity, high frequency vibration. J Musculoskelet Neuronal Interact 2013;13:418–429. [PMC free article] [PubMed] [Google Scholar]
- 30. McKeehen JN, Novotny SA, Baltgalvis KA, Call JA, Nuckley DJ, Lowe DA. Adaptations of mouse skeletal muscle to low‐intensity vibration training. Med Sci Sports Exerc 2013;45:1051–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rubin C, Pope M, Fritton JC, Magnusson M, Hansson T, McLeod K. Transmissibility of 15‐hertz to 35‐hertz vibrations to the human hip and lumbar spine: determining the physiologic feasibility of delivering low‐level anabolic mechanical stimuli to skeletal regions at greatest risk of fracture because of osteoporosis. Spine 2003;28:2621–2627. [DOI] [PubMed] [Google Scholar]
- 32. Gilsanz V, Wren TA, Sanchez M, Dorey F, Judex S, Rubin C. Low‐level, high‐frequency mechanical signals enhance musculoskeletal development of young women with low BMD. J Bone Miner Res 2006;21:1464–1474. [DOI] [PubMed] [Google Scholar]
- 33. McDonald CM, Henricson EK, Han JJ, Abresch RT, Nicorici A, Elfring GL, et al The 6‐minute walk test as a new outcome measure in Duchenne muscular dystrophy. Muscle Nerve 2010;41:500–510. [DOI] [PubMed] [Google Scholar]
- 34. McDonald CM, Henricson EK, Abresch RT, Florence JM, Eagle M, Gappmaier E, et al The 6‐minute walk test and other endpoints in Duchenne muscular dystrophy: longitudinal natural history observations over 48 weeks from a multicenter study. Muscle Nerve 2013;48:343–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mazzone E, Martinelli D, Berardinelli A, Messina S, D'Amico A, Vasco G, et al North Star Ambulatory Assessment, 6‐minute walk test and timed items in ambulant boys with Duchenne muscular dystrophy. Neuromuscul Disord 2010;20:712–716. [DOI] [PubMed] [Google Scholar]
- 36. Hebert LJ, Maltais DB, Lepage C, Saulnier J, Crete M, Perron M. Isometric muscle strength in youth assessed by hand‐held dynamometry: a feasibility, reliability, and validity study. Pediatr Phys Ther 2011;23:289–299. [DOI] [PubMed] [Google Scholar]
- 37. Zemel B, Bass S, Binkley T, Ducher G, Macdonald H, McKay H, et al Peripheral quantitative computed tomography in children and adolescents: the 2007 ISCD Pediatric Official Positions. J Clin Densitom 2008;11:59–74. [DOI] [PubMed] [Google Scholar]
- 38. McDonald CM, Henricson EK, Abresch RT, Florence J, Eagle M, Gappmaier E, et al The 6‐minute walk test and other clinical endpoints in duchenne muscular dystrophy: reliability, concurrent validity, and minimal clinically important differences from a multicenter study. Muscle Nerve 2013;48:357–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Judex S, Lei X, Han D, Rubin C. Low‐magnitude mechanical signals that stimulate bone formation in the ovariectomized rat are dependent on the applied frequency but not on the strain magnitude. J Biomech 2007;40:1333–1339. [DOI] [PubMed] [Google Scholar]
- 40. Hyzewicz J, Tanihata J, Kuraoka M, Ito N, Miyagoe‐Suzuki Y, Takeda S. Low intensity training of mdx mice reduces carbonylation and increases expression levels of proteins involved in energy metabolism and muscle contraction. Free Radic Biol Med 2015;82:122–136. [DOI] [PubMed] [Google Scholar]
- 41. Jansen M, van Alfen N, Geurts AC, de Groot IJ. Assisted bicycle training delays functional deterioration in boys with Duchenne muscular dystrophy: the randomized controlled trial “no use is disuse.” Neurorehabil Neural Repair 2013;27:816–827. [DOI] [PubMed] [Google Scholar]
- 42. Sveen ML, Andersen SP, Ingelsrud LH, Blichter S, Olsen NE, Jonck S, et al Resistance training in patients with limb‐girdle and Becker muscular dystrophies. Muscle Nerve 2013;47:163–169. [DOI] [PubMed] [Google Scholar]
- 43. Alemdaroglu I, Karaduman A, Yilmaz OT, Topaloglu H. Different types of upper extremity exercise training in Duchenne muscular dystrophy: effects on functional performance, strength, endurance, and ambulation. Muscle Nerve 2015;51:697–705. [DOI] [PubMed] [Google Scholar]


