ABSRTACT
Background:
Coronary artery diseases and therapies such as coronary angioplasty would lead to changes in the quality of life in patients. The aim of this study was to determine the effects of collaborative care model on the quality of life in patients after coronary angioplasty.
Methods:
This randomized controlled clinical trial was conducted in Isfahan, Iran during 2015. In this study, 50 samples were selected by simple sampling and randomly allocated into two equal groups of intervention and control. Collaborative care model was performed in the intervention group for 3 months. Data were collected using quality of life (SF-36) questionnaire which includes 36 questions on physical and psychological dimensions and was completed before and one month after the intervention in both groups.
Data were analyzed using descriptive and analytical statistics and by independent t- test, paired t test, Chi square and Mann-Whitney tests through SPSS 18.
Results:
After the intervention, the mean score of quality of life in the intervention group was significantly higher than the control group (P<0.05). The results of independent t-test showed a significant difference between both groups regarding the mean of changes in the score of quality of life and its dimensions in patients undergoing coronary angioplasty 3 months after the intervention (P<0.001).
Conclusion:
Results revealed that patients who had been cared based on collaborative care model had better scores of quality of life in all the physical, mental and social dimensions than the control group. Therefore, using this model for taking care of patients after coronary angioplasty is recommended.
Trial Registration Number: IRCT2015120120912N4
KEYWORDS: Collaboration, Care, Coronary angioplasty, Quality of life
INTRODUCTION
Cardiovascular diseases are one of the main global problems of health systems and the most common and life threatening problem in different countries.1 Nowadays 17.3 million deaths annually around the world are caused by cardiovascular diseases and its prevalence is increasing. Thus, in 2030 the rate of deaths by cardiovascular diseases would be increased by 20.5%.2 In Iran also the mortality rate due to this disease is increasing.3 According to the statistics and demographics of National Organization for Civil Registration of Iran, 58% of recorded deaths in 2012 were caused by cardiovascular diseases.4 The most common and important vascular disease is coronary artery disease that, as a global epidemic, is the main reason of mortality in the world.5-8
For treatment of coronary artery diseases, different approaches including pharmacotherapy, interventional therapy and surgery are taken.7,8 One of the ways of opening coronary arteries is coronary angioplasty.6,7 This method is less risky than coronary artery bypass surgery and it is also less costly. Therefore, because of its low risk and high success rate, nowadays in the United States alone 400,000 angioplasties are performed every day.9 This method along with modification and improvement of patient’s condition could cause changes in the patient’s quality of life.5,10 During the first 5 years after discharge from the hospital, patients should pay regular visits to the health center for follow-up.11 Different studies have shown that cardiovascular diseases would cause various physical symptoms like activity intolerance and also changes in all the aspect of patient’s life including physical, mental and social aspects.12
Considering the high prevalence of using coronary artery angioplasty, lifestyle modification and long-term dieting seems necessary and changing or not changing the lifestyle has an important role in determination of the quality of life in patients after coronary artery angioplasty.12 Since improvement in the quality of life is one of the goals of educating the patient, nurses and the health care team could change the wrong attitudes of people toward diet therapy, health and lifestyle using their knowledge and professional skills.13
In a retrospective study, patients treated through three medical, surgical and angioplasty methods were followed up for 10 years. Results showed that physical and mental aspects of the quality of life in all patients were improved, but the angioplasty group had a lower quality of life than the medical and surgical groups. 14 In another study that followed up the patients after treatment with PTCA and CABG, in the first year and third year follow-up, it was shown that the quality of life in patients was improved in mental aspect, but it decreased in its physical aspect. 15
Since patients who had coronary angioplasty should be under the control and supervision of the health team for the rest of their lives, participation of the patient in treatment programs on one side and decision making and participation of the health team, from the other side, could be effective in providing better healthcare services. 12 One of the main goals of patient’s cooperation with the medical team is improvement of patient’s quality of life.16 Therefore, for improvement and making a more effective communication, the concept and approach of participation could be used. Working according to cooperation of the patient and the medical team could contribute to evaluating patient’s condition; creating a useful and meaningful communication between patients, nurses and physicians; determining healthcare goals; improving the quality of healthcare; and guiding and clarifying the activities. 17
Since diet therapy is one of the most important care and support needs of patients after coronary angioplasty,18 by not following their medical plan they would suffer severe consequences including relapse of the disease and progressive disability; hence, they would need immediate treatment and hospitalization. 19 Therefore, collaborative care model through medical team’s trainings for the patient could control the symptoms and demonstrations of the disease and would consequently lead to more compatibility with the disease and compliance with diet therapy, 20-22 improvement of patient’s participation in healthcare programs and patient’s more independence in performing daily activities. 23 Considering the important effect of trainings about diet, medication and activity programs on the recovery process of cardiovascular patients, it includes a significant and effective part of the patients’ educational programs. Based on their supportive, educational and collaboration role, nurses could provide appropriate condition for compliance to the diet, especially after discharge from hospital. 24
According to the results of different studies, healthcare providers, by sharing their expertise and experiences through inter-professional collaboration, could take an effective step toward getting positive results from patient’s treatments. 25 One of the effective measures in collaboration care model after angioplasty is training on exercise and physical activities, change in eating habits and compliance to the medication. 8 Results of a study on collaboration care intervention showed that, by involving the patient in the treatment process and patient’s cooperation with the medical team, the symptoms would relieve and lead to more compatibility with chronic heart failure. 26
Despite all the results about the effect of collaboration care model on modification of nutritional behaviors in diabetes patients,17 quality of life in patients with heart failure,16 depression and anxiety in patients with heart failure,27 and quality of life in patients with artery diseases,28 other studies have shown that this model has no effect on the quality of life of older patients 29 and patients with chronic obstructive pulmonary disease (COPD).30
Considering the importance of patient’s participation in development of programs and making an agreement in treatment programs for patients after coronary angioplasty, and lack of collaboration and inter-professional approach in taking care of these patients and also considering the low number of studies conducted in this regard, it seems necessary to conduct a study about the effect of collaboration care model on the patients’ quality of life. This study was conducted to determine the effects of collaboration care model on patients’ quality of life after angioplasty.
PATIENTS AND METHODS
The present study was a randomized controlled clinical trial on two groups in two stages that was conducted from February to August 2015 to determine the effects of collaboration care model on the patients’ quality of life that referred to specialized and internal surgery wards of Shahid Chamran hospital (a specialized cardiac hospital( in Isfahan, Iran and underwent surgical coronary angioplasty. For this study, the samples were selected by simple sampling from patients who referred to cardiac wards and underwent coronary angioplasty and also had the inclusion criteria. Then, using the table of random numbers and by moving along the table as many odd and even numbers and the number of participants, they were randomly allocated into two groups of intervention and control. The patients were blind about their group allocation.
The inclusion criteria were being 18 to 70 years old, having had coronary angiography during the past year, being conscious, having the ability to communicate, being aware of their disease, being willing to participate in the study, being able to read and write and having appropriate clinical condition according to physician’s diagnosis. Patients with acute cardiovascular diseases, diabetes, hormone disorders, renal and mental diseases and those who had any constraints for performing the interventions were excluded from the study. Also, if a patient from the intervention group missed more than 2 educational sessions, died or encountered any problem that would make them unable to continue the study, they were excluded.
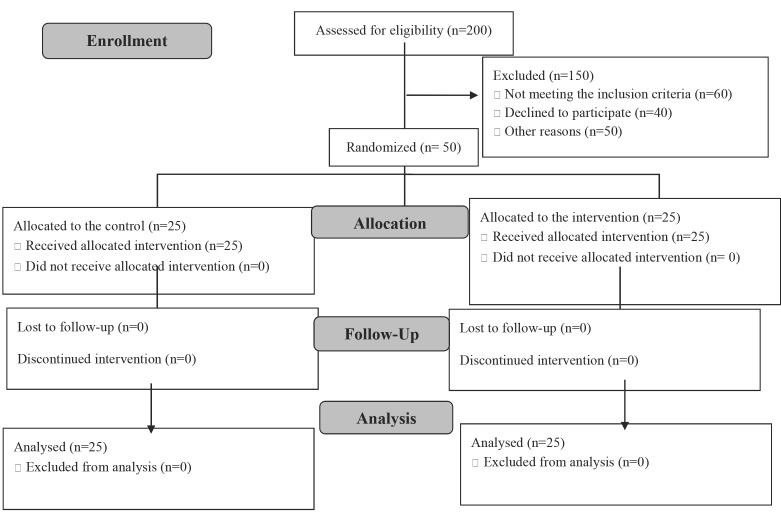
Based on previous research,31 the number of samples for this study with a 95% confidence interval and 80% statistical power was calculated to be 25 for each of the intervention and control groups. The study design and protocol of the study is shown in figure 1.
Figure1.
CONSORT flow diagram of the participants
In this study, data were gathered using a two-part questionnaire. The first part included demographic characteristics and disease condition including age, Body Mass Index (BMI), educational level, employment status, income, history of angioplasty, smoking cigarettes and consuming narcotics and alcohol. The second part was the quality of life questionnaire (SF-36) which was presented by John Ware in 1992 and contains 36 questions.32 This questionnaire has two aspects of physical components summary (PCS) and mental component summary (MCS) and each aspect contains 4 subfields; physical health contains physical performance, physical limitation, physical pain and general health and mental health contains social performance, mental problems, mental health and exhilaration. Physical performance has 10 questions to evaluate limitations in physical activities after the health problem. Limitations in playing the role due to physical health condition are evaluated by 4 questions. Limitations in playing the role due to emotional problems have 3 questions. Tiredness or exhilaration has 4 questions to evaluate the feeling of being powerful and energetic versus the feeling of tiredness. Emotional health is evaluated through 5 questions and social performance with 2 questions (to evaluate the limitations in social activities due to physical and mental problems). The subfield of pain has 2 questions to evaluate the intensity of pain and the limitations in daily activities caused by it. General health has 5 questions to assess the individuals’ evaluation of their current health condition and general understanding of health is evaluated by 1 question to study the changes in health condition during past year.1,32
Reliability and validity of this questionnaire were studied by Eskodua et al. in 2010 who found a Chronbach’s α of 0.88 for physical aspects of the questionnaire and 0.90 for its mental aspects.1 In addition, Montazeri et al. in 1995 calculated its Chronbach’s α to be 0.77-0.9.32
Demographic characteristics questionnaire and SF-36 questionnaire were completed by all the patients or one of their family members before the intervention. Samples of the intervention group, for creating a more dynamic group, were divided into two groups with 9 samples and one group with 7 samples and collaboration group sessions were coordinated with them. Also, to remind them, a phone call was made to each participant the day before the session.
In the intervention group, collaboration care model program was conducted in 5 sessions in a way that 3 educational collaboration care sessions were conducted weekly, and 2 collaboration care follow-up sessions were conducted every other week. Each session lasted 45 to 60 minutes. At first, the educational content was prepared by the nurse researcher based on authentic texts and original sources and then in a collaboration session with the presence of the expert physician and the participants, the educational content was represented by the researcher and the collaboration care model program was finalized after the participant’s agreement. In this educational collaboration model, we applied lecture, question and answer and group and individual discussion methods during the sessions. After conducting the collaboration program, follow-up was conducted by calling the participants and addressing their questions and problems.
In the first session, the patients’ current disease and its threats and complications and then appropriate diet, physical activity and the right method of drug consumption for patients with coronary artery disease were explained to them by an expert physician and a nurse.
In the second session, the educational content was discussed between the physician, the nurse researcher and participants and an agreement was reached about the appropriate diet and physical activities; then, the final program was performed by patients’ opinion.
The collaboration care follow-up sessions were conducted for continuity of the care program and involvement of the patients. Sessions were held every other week for two weeks. After the collaboration follow-up sessions, the patients were followed up for 12 weeks through phone calls and by addressing their questions and problems.
For the control group, two sessions were conducted to discuss the importance of medication, diet and exercise. Sessions were held weekly, each lasting 60 minutes.
It must be noted that after finishing the intervention, the educational booklet was given to the participants of the control group, too.
Three months after the collaboration care program, SF-36 questionnaire was completed by the participants of the intervention and control groups again.
This study was approved by ethics committee of Isfahan University of Medical Sciences under approval code IR.mui.rec.1394.3.174. Before the study started, the researcher explained the goals of the study to all the participants and obtained their written informed consent. The participants were ensured that all their information would remain confidential. Also, all of the participants were free to withdraw from the study at any time and any stage they wanted to.
The gathered data were analyzed through SPSS version 18, using independent t-test, paired t-test, Chi-square test and Mann-Whitney.
RESULT
Results of Mann-Whitney and Chi-square tests showed no significant difference between the intervention and control groups regarding their age (P=0.44), BMI (P=0.88), educational level (P=0.29), employment status (P=0.53), income (P=0.38), history of angioplasty (P=0.79), smoking cigarettes and consuming narcotics and alcohol (P=0.35). The mean age of the intervention group was 54.2 (8.1) years and that of the control group was 55.9 (7.6) years (Table 1).
Table 1.
Demographic characteristics of the patients after angioplasty in the intervention and control groups
| Group | Variable | Intervention Group | Control Group | Test | P value | ||
|---|---|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||||
| Educational level1* | Z=1.05 | 0.29 | |||||
| Elementary | 7 | 28 | 7 | 28 | |||
| Guidance | 2 | 8 | 6 | 48 | |||
| High school | 12 | 48 | 10 | 40 | |||
| University | 4 | 16 | 2 | 8 | |||
| Employment Status** | X2=17.3 | 0.53 | |||||
| Employee | 1 | 4 | 2 | 8 | |||
| Housewife | 1 | 4 | 0 | 0 | |||
| Retired | 10 | 40 | 7 | 28 | |||
| Laborer | 5 | 20 | 4 | 16 | |||
| Freelancer | 8 | 32 | 12 | 48 | |||
| Income level* | Z=0.86 | 0.38 | |||||
| Low | 8 | 32 | 11 | 44 | |||
| Average | 17 | 68 | 14 | 56 | |||
| History of Angioplasty** | X2=0.074 | 0.79 | |||||
| Yes | 4 | 19 | 4 | 16 | |||
| No | 17 | 81 | 21 | 84 | |||
| Substance abuse** | X2=2.84 | 0.35 | |||||
| Smoking cigarettes | 2 | 8 | 4 | 16 | |||
| Opioid | 1 | 4 | 0 | 0 | |||
| Alcohol consumption | 1 | 4 | 0 | 0 | |||
| BMI*** | 26.1±3.5 | 26±1.7 | T=0.14 | 0.88 | |||
Mann-Whitney test
Chi-Square test
Independent t-test
Independent t-test showed no significant difference between the intervention and control groups regarding their mean score of quality of life before the study (P=0.83). The difference between the total mean score of the quality of life and its aspects in both groups was significant three months after the study and the mean of changes in the total score of quality of life three months after the study showed a significant difference between both groups, using paired t-test (P<0.001) ().
In addition, comparing the mean of changes in total scores of quality of life and its aspects before and three months after the study, using independent t-test, showed a significant difference between both groups (P<0.001) (Table 2).
Table 2.
Comparison of the mean total score of the quality of life and its dimensions in the intervention and control groups
| Group | Variable | Before the study | Three month after the study | Paired t test | |||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | t | P value | ||
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | ||||
| Physical performance | 72.6±15.3 | 73.6±12.1 | 84±12.7 | 74.3±12.1 | 5.94 | <0.001 | |
| Role limitation due to physical problems | 43±31.9 | 39.6±28.8 | 89±21.7 | 41.6±28.4 | 7.01 | <0.001 | |
| Physical pain | 71.5±25.4 | 73.4±20.8 | 90.4±13.2 | 79.3±13.5 | 2.93 | <0.001 | |
| General health | 60±10.8 | 62±13.9 | 75±8.6 | 63±12 | 3.78 | <0.001 | |
| Exhilaration | 57±19 | 59.89±12.8 | 66.5±16.2 | 58±9.6 | 2.26 | <0.001 | |
| Social performance | 51.5±18.9 | 53.5±13 | 75±14 | 57.5±12.1 | 4.73 | <0.001 | |
| Role limitation due to emotional problems | 58.8±34.3 | 58.6±41.1 | 81.7±20.8 | 39.6±60 | 2.19 | <0.001 | |
| Mental health | 64±16 | 63.7±10.7 | 68.8±16 | 62.9±9.7 | 2.26 | <0.001 | |
| Quality of life | 60.4±13.9 | 61.4±13.5 | 80.1±12.3 | 63.1±12.8 | 4.81 | <0.001 | |
Paired t test
Although in the control group, the difference between the mean score of the quality of life and its aspects before and three months after the study was not significant, but this difference in the intervention group was significant (P<0.001).
Table 3.
Comparison the mean changes in the total score of quality of life and its dimensions in the intervention and control groups
| Variable | Time | Intervention Group | Control Group | P value* |
|---|---|---|---|---|
| Mean±SD | Mean±SD | |||
| Physical performance | Before the intervention | 72.6±15.3 | 73.6±12.1 | 0.80 |
| After the intervention | 84±12.7 | 74.3±12.1 | 0.01 | |
| Difference | 11.4±1.9 | 0.7±0.6 | <0.001 | |
| Role limitation due to physical problems | Before the intervention | 43±31.9 | 39.6±28.8 | 0.69 |
| After the intervention | 89±21.7 | 41.6±28.4 | <0.001 | |
| Difference | 46±6.5 | 2±2 | <0.001 | |
| Physical pain | Before the intervention | 71.5±25.4 | 73.4±20.8 | 0.77 |
| After the intervention | 90.4±13.2 | 79.3±13.5 | <0.005 | |
| Difference | 19±3.6 | 6±3 | <0.001 | |
| General health | Before the intervention | 60±10.8 | 62±13.9 | 0.56 |
| After the intervention | 7±8.6 | 63±12 | <0.001 | |
| Difference | 15±1.9 | 1.7±1.9 | <0.001 | |
| Exhilaration | Before the intervention | 57±19 | 59.8±12.8 | 0.56 |
| After the intervention | 66.5±16.2 | 58±9.6 | 0.03 | |
| Difference | 9.5±2.7 | 1.8±1.6 | <0.001 | |
| Social performance | Before the intervention | 51.5±18.9 | 53.5±13 | 0.66 |
| After the intervention | 75±14 | 57.5±12.1 | <0.001 | |
| Difference | 23.5±3 | 4±1.2 | <0.001 | |
| Role limitation due to emotional problems | Before the intervention | 58.8±34.3 | 58.6±41.1 | 0.98 |
| After the intervention | 81.7±29.8 | 60±39.6 | <0.003 | |
| Difference | 22.8±5.3 | 1.3±3.5 | <0.001 | |
| Mental health | Before the intervention | 64±16 | 63.7±10.7 | 0.96 |
| After the intervention | 68.8±16 | 62.9±9.7 | 0.03 | |
| Difference | 4.7±1.1 | 0.7±0.6 | <0.001 | |
| Quality of life | Before the intervention | 60.4±13.9 | 61.4±13.5 | 0.83 |
| After the intervention | 80.1±12.3 | 63.1±12.8 | <0.001 | |
| Difference | 19.5±8.1 | 1.6±4.1 | <0.001 |
Independent t test
DISCUSSION
Results of the present study showed that collaboration care model was effective on the quality of life in patients after coronary angioplasty so that the total mean score of the quality of life and its aspects was significantly better in the intervention group three months after the study. Similar to the results of this study, other studies have also reported the effects of collaboration care model on the quality of life in patients with heart failure,16 asthma,33 hemodialysis,34 and diabetes.35 Another study showed that applying this model has been effective on improvement and enhancement of sleep quality in patients who had undergone coronary artery bypass grafting.36 In another study, collaboration care model has reduced depression and improved self-management of chronic diseases in patients with physical and mental problems.37
Various studies have shown the effects of collaboration care model on reduction of symptoms and improvement of quality of life in different patients, but no similar study has been conducted on patients who underwent coronary angioplasty. What distinguishes this study from other similar studies is participation of and follow-up by one of the family members. As mentioned in the present study, the quality of life in patients was significantly increased by participating in educational programs based on collaboration care model and the condition of dieting, medication and exercising was improved in the intervention group. It seems that the three-month follow-up has been effective on the impact of collaboration care model.
Treatment and taking care of patients in health system, especially chronic and long-term patients, requires existence and participation of a medical team and cooperation of all the caregivers. In this study, the presence of a cardiologist, a nurse and a family member with the angioplasty patient and providing some notes about the disease, dieting, physical activities and drug consumption improved physical, mental and social status of the patients. In this regard, a study showed that collaboration care intervention with the presence of a nurse, a psychologist and experts by palliative and psychosocial care model improved the symptoms and quality of life in patients with heart failure.26 Also, another study showed that constant educational programs could be effective on improvement of quality of life in patients with heart failure.14 Another study that aimed to determine the role of multidisciplinary and team work on improvement of recovery time after being discharged from hospital indicated that the multidisciplinary approach for managing heart transplant patients had a significant effect on the quality of services received by the patient.38 In the same line, another research showed that multidisciplinary management program for heart failure during the patient’s hospitalization would lead to improvement of therapeutic condition and enhancement of results after discharge from hospital in Japanese patients with heart failure. 39
In the present study, conducting regular collaboration care sessions for educating the patients led to more participation of the patients in their own care and consequently more acceptance of their disease, finding more strategies to adapt with their disease, and also increasing their quality of life. “Lakdizaji et al. (2013) showed that comprehensive disease management programs, including patient’s educating and self-care strategies by multidisciplinary medical team would significantly improve the quality of life in patients with heart failure. Furthermore, among all the conducted interventions, multidisciplinary educational interventions by nurses, pharmacists and nutritionists were mostly effective on reduction of the risk of primary results”.11
Unlike the results of the present study, a study showed that collaboration care model did not reduce the mortality rate among patients with chronic obstructive pulmonary disease.30 Also, another study showed that collaboration care model has not been effective on the response of older patients with anxiety disorders to treatment.29 The difference between the results of the present study and these two studies could be due to the difference between the sample sizes, the cultural and social differences between studied populations, the differences between the method of collaboration care model, method of nurses’ follow-ups, educational sessions and phone calls to the participants and also participation of one of the patient’s family members.
What distinguishes this study from other similar studies is the agreement between the physician, the nurse and the patient on the diet therapy (nutritional diet, medicinal diet and physical activities), three-month follow-up of the patients, and also participation of one of the patient’s family members in the study for continuity of the effect of collaboration care model on the patient’s quality of life.
Involvement of patients in their own care services through collaboration and educational programs like collaboration care model is important because, along with improvement of educational and care programs, it has a significant effect on patient’s quality of life, too. Therefore, it is recommended that this collaboration care model, which involves the patients and medical team in the treatment process, should be used for other patients, as well. The sample size of this study and the period of follow-up that was just 3 months were the most important limitations of this study. Also, due to lack of random access, the sampling method had to be convenience sampling based on the inclusion criteria and this was another limitation of this study, but the selected sample were randomly allocated into two groups of intervention and control. Therefore, it is recommended that further studies with bigger sample sizes and longer periods of follow-up should be conducted.
CONCLUSION
Results of this study showed that participation of the patient and their family members in the treatment process as a collaboration care model could have a significant effect on acceptance and execution of measures and consequently on the patient’s quality of life. Also, patient follow-up for monitoring the execution of agreed matters and evaluating the continuity of collaboration care model’s effect could be effective on the patient’s commitment to and application of care programs. Therefore, it is recommended that patient’s family should participate in developing collaboration care programs with an inter-professional approach.
ACKNOWLEDGEMENT
The present article was adopted from the thesis that was written by Parastoo Rezapoor and financially supported by Isfahan University of Medical Sciences under grant No. 394174. The authors would like to acknowledge the Nursing & Midwifery Faculty of Isfahan University of Medical Sciences for supporting this work. We would like to thank all the patients who participated in this study and also the authorities and personnel of Shahid Chamran hospital.
Conflict of Interest:None declared.
REFRENSES
- 1.Skodova Z, Van Dijk JP, Nagyova I, et al. Psychosocial predictors of change in quality of life in patient after coronary interventions. HEART & LUNG. 2011;40:331–9. doi: 10.1016/j.hrtlng.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 2.Laslett LJ, Alagona P Jr, Clark BA, et al. The worldwide life environment of cardiovascular disease: Prevalence, diagnosis, therapy, and policy issues: a report from the American journal of cardiology. J Am Coll Cardiol. 2012;60:S1–49. doi: 10.1016/j.jacc.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Ezzatti N. Perceptions of patients with coronary artery disease about their therapeutic regimen. Iranian Journal of Nursing. 2010;23:26–34. [In Persian] [Google Scholar]
- 4.Daei MM, Zeighami R, Arjeini Z, Alipour Heidary M. The effect of continuous care model on quality of life of patients after coronary angioplasty in Bou Ali Sina hospital. Evidence Based Care Journal. 2014;4:61–70. [Google Scholar]
- 5.Tang L, Patao C, Chuang J, Wong ND. Cardiovascular risk factor control and adherence to recommended lifestyle and medical therapies in persons with coronary heart disease (From the national health and nutrition examination survey 2007-2010) Am J Cardiol. 2013;112:1126–32. doi: 10.1016/j.amjcard.2013.05.064. [DOI] [PubMed] [Google Scholar]
- 6.Long J, Luckraz H, Thekkudan J, et al. Heart team discussion in managing patients with coronary artery disease outcome and reproducibility. Interact Cardiovasc Thorac Surg. 2012;14:594–8. doi: 10.1093/icvts/ivr157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Windecker S, Stortecky S, Stefanini GG, et al. Revascularization versus medical treatment in patients with stable coronary artery disease: network meta-analysis. BMJ. 2014;348:g3859. doi: 10.1136/bmj.g3859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park LG, Howie-Esquivel J, Chung ML, Dracup K. A text messaging intervention to promote medication adherence for patient with coronary heart disease: A randomized controlled trial. Patient Educ Couns. 2014;94:261–8. doi: 10.1016/j.pec.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 9.Yousefnezhad K, Shabankhani B, Etemadinezhad S, et al. Analysis of survival in patients after angioplasty to help cardiovascular COX regression model. J Mazand Univ Med Sci. 2012;22:101–6. [In Persian] [Google Scholar]
- 10.Peterson JC, Allegrante JP, Piraglia PA, et al. Living with heart disease after angioplasty: A qualitative study of patient who have been successful or unsuccessful in multiple behavior chang. HEART & LUNG. 2010;39:105–15. doi: 10.1016/j.hrtlng.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lakdizaji S, Hassankhani H, Mohajjel Agdam A, et al. Effect of educational program on quality of life of patients with heart failure: A randomized clinical trial. J Caring Sci. 2013;2:11–8. doi: 10.5681/jcs.2013.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baljani E, Rahimi ZH, Heydari Sh, Azimpour A. The Effect of Self Management Interventions on Medication Adherence and Life Style in Cardiovascular Patients. Scientific Journal of Hamadan Nursing & Midwifery Faculty. 2012;20:58–68. [In Persian] [Google Scholar]
- 13.Sadeghzadeh V, Moshtagh Eshgh Z. The effect of cardiac rehabilitation on improving the quality of life in patients with myocardial infarction in Zanjan. Faculty of Nursing of Midwifery Quarterly. 2011;21:8–13. [In Persian] [Google Scholar]
- 14.De Oliveira, Carvallno AL, HuebW Gresh BJ, et al. Quality of life in patients with multivessel coronary artery disease Ten-year follow-up of a comparison of surgical, angioplasty or medical strategies MASS II trial. J Clinic Trials. 2014;4:2. [Google Scholar]
- 15.Tofighi SH, Ahmadkiadaliri A, Sadeghifar J, et al. Health-related quality of life among patients with coronary artery disease: A post-treatment follow-up study in Iran. Cardiology Research Practice. 2012;2012:973974. doi: 10.1155/2012/973974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borhani F, Khoshab H, Abbas Zadeh A, et al. Study of the effect of partnership care model on the quality of life in patient with heart failure. Iranian Journal of Critical Care Nursing. 2012;1:43–8. [Google Scholar]
- 17.Mamene M, Lakdizaji S, Rahmani A, Behshid M. The effect of teaching based collaborative care model on diet habits in diabetes type II: A clinical trial study. Scientific Journal of Hamadan Nursing & Midwifery Faculty. 2014;22:41–51. [In Persian] [Google Scholar]
- 18.Kim MJ, Jeon DS, Gwon HC, et al. Health-Related quality of life after percutaneous coronary intervention in patient with UA/NSTEMI and STEMI. J Korean Med Sci. 2013;28:848–54. doi: 10.3346/jkms.2013.28.6.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carter BL, Bosworth HB, Green BB. The hypertension team: The role of the pharmacist, nurse, and team work in hypertension therapy. J Clin Hypertens (Greenwich) 2012;14:51–65. doi: 10.1111/j.1751-7176.2011.00542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Modanloo Sh, Zolfaghari M, Dehghankar L, et al. Assessment the effect of small message service (SMS) follow up on selfefficacy in dialysis patients. Iranian Journal of Nursing Research. 2014;8:61–71. [In Persian] [Google Scholar]
- 21.Menchetti M, Sighinolfi C, Di Mihele V, et al. Effectiveness of collaborative care for depression in Italy. A randomized controlled trial. Gen Hosp Psychiatry. 2013;35:579–86. doi: 10.1016/j.genhosppsych.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 22.Tully PJ, Baumeister H. Collaborative care for the treatment of comorbid depression and coronary heart disease: A systematic review and meta-analysis protocol. Systematic Reviews. 2014;3:127. doi: 10.1186/2046-4053-3-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dehghani A, Orang M, Abdollahyfard S, et al. Barriers to patient education in clinical care; Viewpoints of nurse. Iranian Journal of Medical Education. 2014;14:332–41. [Google Scholar]
- 24.Mohammadi M, Meamari AM, Shaban M, et al. Effect of computer education and face-to-face on adherence to diet patients after myocardial infarction. Hayat. 2010;16:77–85. [In Persian] [Google Scholar]
- 25.Cheong LH, Armour CL, Pharm B, Bosnic-Anticevich SZ. Primary health care teams and the patient perspective: A social network analysis. Res Social Adm Pharm. 2013;9:741–57. doi: 10.1016/j.sapharm.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Bekelman DB, Hooker S, Nowels CT, et al. Feasibility and acceptability of a collaborative care intervention to improve symptom and quality of life in chronic heart failure: Mixed methods pilot trial. J Palliat Med. 2014;17:145–51. doi: 10.1089/jpm.2013.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khoshab H, Bagheryan B, Abbaszadeh A, et al. The effect of partenership care model on depression and anxiety in the patient with heart failure. Evidence Based Care Journal. 2012;2:37–45. [In Persian] [Google Scholar]
- 28.Azadi F, Mohammadi E. Effects of collaborative care model on quality of life in patient’s coronary artery disease. Iranian Journal of Nursing Research. 2006;1:23–9. [In Persian] [Google Scholar]
- 29.Wetherell JL, Petkus AJ, Thorp SR, et al. Age differences in treatment respone to a collaborative care intervention for anxiety disorders. The British Journal of Psychiatry. 2013;203:65–72. doi: 10.1192/bjp.bp.112.118547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gershon AS, Macdonald EM, Luo J, et al. Impact of early collaborative care after hospital admission or emergency department disease (COPD): A population study. Am J Respir care med. 2015;191:A1097 . [Google Scholar]
- 31.Khalife-Zade A, Dorri S, Shafiee S. The effect of cardiac rehabilitation on quality of life in patients with acute coronary syndrome. Iranian Journal of Nursing and Midwifery Rresearch. 2015;20:588–93. doi: 10.4103/1735-9066.164504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The short from health survey (SF-36) translation and validation of the Iranian version, quality of life researcher. Quality of Life Researcher. 2005;14:875–82. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 33.Daneshi F, Sabzevari S, Pooraboli B, Shojaei Shahrokhabadi B. The effect of collaborative care model on the quality of life of adults with asthma. Iran Journal of Nursing . 2014;27:1–10. [In Persian] [Google Scholar]
- 34.Ghavidel F, Mohammadzadeh S, Pirasteh H, Alavi Majd H. Effect assessment of applying the partnership care model in quality of life in hemodialysis patients referring to Be’sat Hospital of IRI Air Force. Journal of IRIAF Health Administration. 2009;2:22–8. [In Persian] [Google Scholar]
- 35.Mamene M, Lakdizaji S, Rahmani A, Behshid M. The effect of teaching based collaborative care model on diet habits in diabetes type II: A clinical trial study. Scientific Journal of Hamadan Nursing & Midwifery Faculty. 2014;22:41–51. [In Persian] [Google Scholar]
- 36.Alamdarloo A, Hosseini MA, Khankeh H, et al. The effect of collaborative care model on sleep quality of patients undergoing coronary artery bypass graft surgery. Iranian Journal of Rehabilitation Research in Nursing. 2015;1:49–59. [In Persian] [Google Scholar]
- 37.Coventry P, Lovell K, Dickens CH, et al. Integrated primary care for patients with mental and physical multi morbidity: cluster randomized controlled trial of collaborative care for patients with depression comorbid with diabetes or cardiovascular disease. BMJ. 2015;350:h638. doi: 10.1136/bmj.h638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roussel MG, Gorham N, Wilson L, Mangi AA. Improving recovery time following heart transplantation: the role of the multidisciplinary health care team. J Multidiscip Health care. 2013;6:293–302. doi: 10.2147/JMDH.S31457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kinugasa Y, Kato M, Sugihara S, et al. Multidisciplinary intensive education in the hospital and improves out comes for hospitalized heart failure patient in a Japanes rural setting. BMC Health Services Research. 2014;14:351. doi: 10.1186/1472-6963-14-351. [DOI] [PMC free article] [PubMed] [Google Scholar]