ABSTRACT
Background:
Diabetes Education by Peer Coaching is a strategy which helps the patients with diabetes in the field of behavioral and emotional problems. However, the results of studies in this field in other countries could not be generalized in our context. So, the current study aimed to examine the effectiveness of Diabetes Education by Peer Coaching on Diabetes Management.
Methods:
Outcome variables for patients and peer coaches are measured at baseline and in3,6 and 12 months. The primary outcome consisted of Fasting Blood Sugar (FBS) and HbA1c. Secondary outcomes included Blood Pressure (BP), Body Mass Index (BMI,) Waist-Hip Ratio (WHR), Lipid Profile, diabetes self-care activities, diabetes-related quality of life, depression, and Social Capital levels.Initial analyses compared the frequency of baseline levels of outcome and other variables using a simple Chi-square test, t-test and the Mann-Whitney- U test. Sequential measurements in each group were evaluated by two-way analysis of variance. If significant differences in baseline characteristics were found, analyses were repeated adjusting for these differences using ANOVA and logistic regression for multivariate analyses. Additional analyses were conducted to look for the evidence of effect modification by pre-specified subgroups.
Conclusion:
The fact is that self-control and self-efficacy in diabetes management and treatment of diabetes could be important components. It seems that this research in this special setting with cultural differences would provide more evidence about peer-coaching model. It seems that if the peer-coaching model improves learning situations between patients with diabetes by offering one-on-one Diabetes Self Management Education, it could be an interactive approach to diabetic education.
Trial Registration Number: IRCT201501128175N3
KEYWORDS: Diabetes mellitus, Education, Peer group, Hemoglobin A, Glycosylated
INTRODUCTION
On the basis of WHO report, 171 million people in the world had diabetes in 2000.1 The most recent estimates of the International Diabetes Federation (IDF) show that 8.3% of adults, i.e. 382 million people, suffer from diabetes, and the number of people with diabetes is set to rise beyond 592 million in less than 25 years.2 The current evidence shows the effect of diabetes and diabetic complications on the patients’ lives and the health system of societies.3 Additionally, the complications due to diabetes are a major cause of disability, reduced quality of life, and death. It is noteworthy that unhealthy behaviors including lack of sufficient phyشsical activity, consumption of high calorie foods, unsuitable control of blood sugar level and taking medications incorrectly are among the major causes of increasing the risk of diabetic complications.4 It should be mentioned that, in addition to the blood sugar, cholesterol and blood pressure-lowering medications, lifestyle changes to increase physical activity and a healthy diet can significantly reduce the risk of diabetes complications.5 The evidence suggests that diabetes education has played a significant role in the diabetes control and promoting quality of life.6 In this regard, the documents of Iranian studies indicated that electronic education to the patient with diabetes and health care providers affect the diabetes control, as well.7,8
Therefore, one of the strategies to optimize metabolic control, prevent diabetes complications, and improve the quality of life of diabetic patients is Diabetes Self Management Education (DSME) which focuses on diabetics self care training.9,10 DSME is not only known as a valuable resource for patients to be actively involved in the diabetes management,11,12 but also it has been noted in some diabetes clinical guidelines.3 Moreover, the results of numerous studies demonstrate DSME interventions as an effective strategy in improving knowledge, management and metabolic control of diabetic patients. 13-18
Different groups are involved in diabetic patients’ education, including physicians and nurse educators. Studies indicated that short-term diabetes self management education carried out by health care professionals improve clinical outcomes and quality of life of diabetic patients.11,13,18-22 On the other hand, there is evidence showing that diabetic patient education programs could not be effective for long-term because this training alone does not maintain diabetic patients’ healthy behaviors during life time unless a combination of behavioral and affective mechanisms are involved together23-26 and support the patients to maintain behavioral changes induced during the training process.11,27-29
In this regard, Diabetes Education by Peer Coaching is a strategy which helps diabetic patients in the field of behavioral and emotional problems and provides ongoing support for DSME interventions.30
Education by Peer Coaching is a complex issue and it has been mentioned in several studies in different forms. The main functions of Education by Peer Coaching are training and ongoing support from a group of similar patients. In this approach, patient education provided by people in the same age, sex, race, cultural and social status with a common problem in a particular issue (such as a chronic disease).31,32
Available evidence suggests that Education by Peer Coaching is more effective than education by members of health care professionals since peer coac hes have a better understanding of their target group and, therefore, regularly interact with them.33 Over the past decade, numerous studies have evaluated the feasibility, acceptability and impact of self-care education to diabetic patients by Peer Coaches,34-45 and flexibility, cost effectiveness and effective communication with patients have been mentioned as the advantages of this method.
But the chronic and progressive nature of diabetes stresses that there is a need to consistent and supportive interventions on diabetes self-management.46 In this regard, more research is needed to define the framework for the delivery of interventions by peer coaches to have lifelong support.47,48 Another interesting point in this area is that most of the research conducted on Diabetes Education by Peer Coaching do not clarify the behavioral strategies used to support diabetes self-management.30 Due to the differences in lifestyle behaviors, including Physical Activity and Diet in addition to therapeutic regiment compliance, the results of other studies in this field in other countries could not be generalized in our context. 49
Thus, the current study aimed to examine the effectiveness of Diabetes Education by Peer Coaching on Diabetes Control and Management. This study is an attempt to answer the question “Does Diabetes Education by Peer Coaching within 6 months lead to a better outcome for patients with type II diabetes, including HbA1c, FBS, Lipid Profile, WHR, BMI, BP, physical activity Levels, food intake, Self-care activities, Quality of Life, Depression and Social Capital levels?”
Objectives
This study aimed to determine if Diabetes Education by Peer Coaching within 6 months leads to a better outcome for patients with type II diabetes. Our primary outcome was measuring HbA1c and secondary outcomes consisted of measuring FBS, and Lipid Profile including High Density Lipoprotein (HDL), Low Density Llipoprotein (LDL), Triglyceride (TG), Cholesterol, BMI, WHR, BP, Levels of physical activity, food intake, Self-care activities, Quality of Life, Depression and Social Capital levels at baseline, 3, 6 and 12 months after the education period in the group receiving peer education and the routine care group. In addition, the mentioned outcomes were examined in peer coaches who also had type II diabetes. 30
The following objectives were considered in the study:
The main objective:
To determine the effectiveness of the peer education approach on diabetes control and management in the two groups which received education through peer coaches and routine care (including attending small group class on diabetes or education through national media).
Subsidiary Objectives
To determine and compare the HbA1c and FBS in patients suffering from type II diabetes who had received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A: diabetic patients who received education through peer coaches) (Group B: diabetic patients who received routine care including attending small group discussion on diabetes or education through national media) and in the peer coaches group who suffered from type II diabetes and received oral medications or insulin. 49
To determine and compare the Lipid Profile including LD, HD, TG, Cholesterol in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To determine and compare the BMI in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To determine and compare the WHR in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To determine and compare the BP in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To determine and compare the levels of physical activity in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To determine and compare the Food intake in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To determine and compare the Self-care activities including blood-sugar control, foods and physical activity) in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To determine and compare the Quality of Life in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To determine and compare the Depression level in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To determine and compare the Social Capital levels in patients suffering from type II diabetes who received oral medications or insulin before (at baseline) and after (at 3, 6, 12 months) training in both groups (Group A and B) and in the peer coaches group.
To describe the experiences of peer coaches around the patients’ education by qualitative study.
Practical Purposes
To promote self-care, social support and quality of life of diabetic patients.
MATERIALS AND METHODS
Study Design
An unblinded randomized clinical trial in which women with type 2 diabetes were divided into one of the two following categories:
Group A: diabetic patients who received education through peer coaches.
Group B: diabetic patients who received routine care including attending small group discussions on diabetes or education through national media)
Study Population
The study population included all women with type 2 diabetes who received diabetes care at one of the following health centers in Tehran:
All Primary Health Centers in 22 different regions of Tehran in which diabetics were admitted, trained and followed up.
Diabetes clinics (1 & 2) as two referral diabetes clinics in Tehran affiliated to EMRI.
Inclusion Criteria
Peer Coaches Group
The peers in the study were women with type 2 diabetes who had HbA1c ≤ 9%. It seems that diabetic patients who better control diabetes could be good educators.They should be capable to have glycemic control and interact with other people as well. According to the above definition, and the following criteria, the research team requested the health center staff to offer the diabetic patients as peer coaches:
Ability to speak in Persian
Age between 20 and 60 years old
Control of blood sugar and HbA1c≤9% during the study
Ability to attend a 20-hour training course
Ability to educate, engage and follow up the patients for at least six months
Participation in monthly meetings held by the research team and supervisors (including physicians and nurses).
A basic knowledge of self-care and communication skills without any judgment about patients. staying with patients for 6 months and no intention to leave the location.
Peer coaches were trained during one week (face to face education) according to the diabetes educational material which was prepared in the Education Department of EMRI. All diabetics in the peer coach group were assessed and after passing the exam, they could be a diabetes educator in this study.
Patients Group
Individuals eligible for participation in the study were women with type 2 diabetes who had HbA1c≤9% in the previous 6 months. Patients were asked not to migrate out of Tehran during the period of study so that the research team could easily be in contact with them. Additionally, the following criteria were essential:
Ability to speak in Persian
Age between 20 and 60 years old
Having HbA1c≤9% in the last 6 months
Non-pregnant
Patients with a life expectancy of less than a year and those who had a serious illness and disease with reduced cognitive capacity approved by the health center staff were recruited.
Exclusion Criteria
Peer Coaches Group
having HbA1c equal and above 9% during the study
Patients Group
having HbA1c equal and above 9% during the study
Becoming pregnant during the study (because the needs of pregnant women with diabetes differ from other diabetics.)
Sampling and Sample Size
In the presnt study, theparticipants were recruited using multistage sampling method from five geographical regions (north, south, east, west, and center) of Tehran city. In each geographical region, one municipal district was selected randomly. The unit of randomization was the municipal districts in the geographical region instead of the patient. In each municipal district, four neighborhoods were selected and assigned randomly to the intervention and control groups (two neighborhoods in each group). In each neighborhood, eligible participants were selected from the list of diabetes health homes. In each neighborhood in the intervention groups, eligible peers were selected.
Sample size was estimated according to the American Diabetes Association protocol (54), using two means comparison formula. In this formula, by considering the mean difference of 0.5% in HbA1c levels between the groups and standard deviation of 1.5 ( in each group), type I error of 0.05, type II error of 0.2 and attrition rate of 10%, 300 patients and 42 peer coaches were recruited for this study.
Accordingly 150 patients were selected in the intervention group who took oral medication and patients injecting insulin. In the control group, 150 patients were selected in oral medication and patients injecting insulin as well. In peer coaches, one group of the participants took oral medication and the other one injected insulin. It was noted that in the allocation of individuals in each group, the percentage of those taking insulin or oral medications was considered in the reference population.
Prior to patient enrollment, the study team created a randomization system to ensure unbiased sorting of patients to each study arm: to receive peer coaching vs. to receive usual care.
Actually, selection of intervention and control groupswas hidden both from the patients and from the evaluator in this study. The participants, investigators, and study personnel were unblind and the laboratory personnel and data entry operator were blind about the study.
Outcome Measures
Outcome variables for patients and peer coaches were measured at baseline and 3,6 and 12 months. The primary outcome consisted of FBS and HbA1c. Secondary outcomes included systolic blood pressure, BMI, Lipid Profile including LD, HD, TG, and Cholesterol, diabetes self-care activities, diabetes-related quality of life, depression and Social Capital levels.
So, the height, weight, HbA1c, BP, BMI, Lipid Profile, WHR, Food intake, physical activity, self-care activities, quality of life, depression and social capital levels were measured. Subgroup analysis was done based on receiving insulin or oral medication, age, education level.
Approximately, 10 cc of blood was drawn from the patient and peer coaches. Participants should have been fasting for 8 to 12 hours before the laboratory tests. Biochemical tests, including lipid and glucose were done with Autoanalyzer which was calibrated every 6 month by the manufacturing company and obtained the calibration certificate. All laboratory tests were done under the supervision of the Iranian Ministry of Health and under the control of the quality management system in accordance with national standards. Other devices used to measure blood pressure and weight had been sent to the company to be recalibrated after calibration of measurement devices.
Measurement and Scale
The questionnaires used in this study included the following parts (Table 1).
Table 1.
The Validity and Reliability of the questionnaires used in the study
| NO | Questionaire | Validity & Reliability | Number of questions |
|---|---|---|---|
| 1 | IPAQ50 | Cronbach’s Alpha coefficient (0.7) | 12 |
| Spearman Brown correlation coefficient (0.9) | |||
| 2 | SDSCA51 | Cronbach’s Alpha coefficient (0.71) and Pearson’s correlation coefficient: r=0.78 | 22 |
| 3 | DQOL52 | Cronbach’s Alpha coefficient : (0.77) and Pearson’s correlation coefficient: r=0.72 | 15 |
| 4 | Beck53 | The BDI-II-Persian had high internal consistency (Cronbach’s α=0.87) and acceptable test-retest reliability (r=0.74). | 13 |
| 5 | SC_IQ54 | The Intra Class Correlation Coefficient (ICC) range: (0.75-0.89). | 36 |
| Values of Cronbach’s alpha were 0.86, 0.82, and 0.69 for the ‘trust’, ‘empowerment and political actions’, and ‘social cohesion’ dimensions respectively, and 0.67 for the ‘cooperation’ dimension, which might be a result of the paucity of questions in this dimension (three questions). |
Demographic Questionnaire
Lab test checklist including Lipid Profile including FBS and HbA1c, LD, HD, TG, Cholesterol. Checklist of data related to the WHR, BMI, BP.
3 day recall questionnaire for determining the Food intake
International Physical Activity Questionnaire (IPAQ) to determine the Levels of physical activity
Summary of Diabetes Self-Care Activities - SDSCA to determine the Self-care activities
Diabetes Quality of Life (DQOL) to determine the quality of life
Beck Depression Inventory questionnaire (Beck) to determine the depression.
Social Capital Questionnaire - (SC-IQ) to measure social capital.
A log book to record the information obtained from peers
Intervention
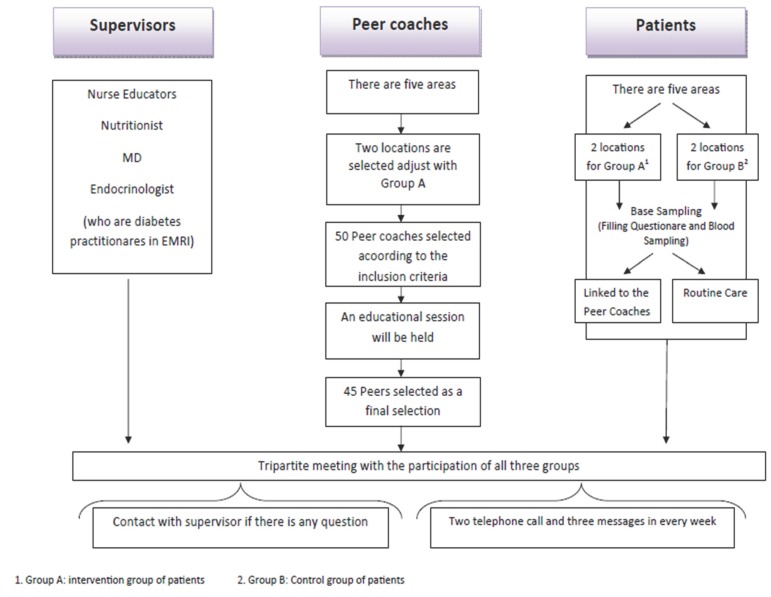
An unblinded randomized clinical trial in which women with type 2 diabetes were divided into one of the two following categories (Figure 1):
Figure1.
An unblinded randomized clinical trial diagram.
Control group: diabetic patients who received routine care including attendance in small group discussions on diabetes class or education through national media
Intervention group: diabetic patients who received education through peer coaches. Research population consisted of all women with type 2 diabetes who referred to the municipality clinics in Tehran and (Two clinics affiliated to endocrinology and metabolism research center and health centers in 22 districts of Tehran) for receiving primary care of diabetics (management and education). Intervention: all patients according to the type of received drugs in contact with a peer for 6 months. Essential information was obtained at the beginning of the project (pre-intervention) and 3, 6 and 12 months after the intervention. Intervention was continued for 6 months. All patients in the intervention group had two telephone calls with peers, two times face to face meetings and received three SMS (during one month). If essential, they also had two face-to-face meetings. If necessary, they had a clinic visit. Meetings, phone calls or SMS were arranged based on the patient and peer agreement. All peers recorded every meeting or call history including contact time, contact type, contact duration, and the subject of talk. Patients jointed the peers, based on their gender. The first meeting took place by telephone and introduction session between the peer and patient was held. Then, specific clinical goals including HbA1c, FBS, lipid profile (LDL, HDL, TG, Cholesterol) and high blood pressure; self-care skills such as using a glucometer and proper strategies during hypoglycemia; taking drugs; changing lifestyle; healthy eating; physical activity; and stress were discussed. Peers and patients talked about family, job or hobbies on holidays. There was not any educational intervention between patients and peers at 6 month to 12 month of the intervention. They just continued their relationship by telephone calls. All theinformation was recorded and measured at 12 month.
Data Analysis
Normal distribution of continuous variables was checked using Kolmogrov-smirnov test. Continuous variables with or without normal distribution are presented as mean (standard deviation) and median (interquartile range), respectively. Categorical variables were reported as percentage. Continuous variables with or without normal distribution between groups (intervention and non- intervention group) were compared using independent T-test, and Mann-Whitney- U test, respectively. Frequency of categorical variables between groups was compared using Chi-square test.
Two way repeated measure ANOVA (RMANOVA) test was used to compare repeated measurements of continuos outcomes between groups. Cochran’s Q test was used to compare repeated measurements of binary outcomes between groups.
If the patient changed the drug during the study or if the patient was excluded from the study with any reason, his/her basic information was compared with those who remained in the study and had the intention to be treated and per protocol analysis was used.
Sensitivity analyses for primary outcomes (HBA1c and FBS) were performed to estimate the effects of missing data using different assumptions.
Missing data were imputed by Amila package in R. Sensitivity analysis was used to estimate the effect size with or without missing data. Subgroup analysis was performed to analyze the effect of intervention according to the type of intervention.
Qualitative Evaluation
The peer coaches voluntarily participated in a focus group, semi-structured interviews, or both, to assess how they experienced the training and coaching process. The focus group was designed to reveal the coaches’ general attitudes and facilitate the development of the interview guide. Semi-structured interviews were conducted in Persian. Peers were prompted to discuss their efficacy as coaches, the training experience, the impact of coaching on their management of their own diabetes, and their role in the health care team. The focus group and interviews were audio-recorded and transcribed. Analyses were encoded and organized to identify, develop and analyze the themes.
Ethics and Dissemination
The trial registration number was IRCT201501128175N3. The related project was approved (code: EC-00378) by the ethics committee of Endocrinology and Metabolism Research Institute of Tehran University of Medical Sciences (TUMS) in accordance with Helsinki Declaration and the guideline of Iranian Ministry of Health and Medical Education. In this regard, it should be noted that all patients were informed that they might be placed in the intervention or control group. Moreover, written informed consent was obtained. The anonymity of participants in the study for analysts and other peers was maintained. Additionally, blood samples were taken just as much as tests needed and samples were kept anonymous the private information which was shared between patient and peer coaches was protected. Another point to mention is that there was the possibility of withdrawal at any time at the request of the patient. Last but not least is that considering the Iranian cultural context and moral considerations, the women with diabetes type 2 were just included in the study. It should be noted that the participants could leave this trial, at any time, with no penalty or loss of benefits.
It should be noted that the trial management was performed by all authors and trial steaming was done by the corresponding author who advised on development of the study intervention and trial procedures. The analysis strategy group chaired by the fifth author and data Monitoring Committee included the Fourth and Fifth authors. Observer of the study was Dr Shohre Naderimagham as an independent member.
DISCUSSION
The fact is that self-control and self-efficacy in diabetes management and treatment of diabetes could be important components. It seems that this research in this special setting with cultural differences would provide more evidence about peer-coaching model.
Since this is a community-based program and the needs of different groups in the society should be considered. Especially in our country we do not have community health nurses, and healthcare workers (who are known as Behvarz) have successful experiences in the disease education and control.
Due to the fact that information about diabetes could be obtained from sources other than peer education, randomization was used in sampling to control it. There was the possibility of loss of patients and changing the group of patients during the study, which was controlled by sensitivity test and intention to treat and per protocol analysis. Moreover, only women with diabetes type 2 were included in the study; it was related to the cultural context and ethical considerations to reduce the conflicts.
Health care providers do not have enough time to provide training and ongoing support of diabetic patients. Also, training the diabetic peer coach not only makes the patients with diabetes hopeful in self-care but also supports other diabetic patients.
These people can help as the training arm of the health care system in our country in the long run, especially in rural areas and small towns. After conducting this study and according to the results of this project in Tehran, it could be implemented in other rural areas.
There are several ethnic groups in our country. Training peers with the same dialect, language, nutritional habits and lifestyle causes can influence and change the behavior of different groups. Educational content from peers can be evaluated as a curriculum and widely used in peer training.
It seems that participation of the women with diabetes type 2 in this study could be a weakness because the findings will only reflect the women’s self-control behaviors.
On the other hand, one of the strengths of this study was the participants who were selected randomly from all five geographical regions of Tehran city. In this way, the the impact of certain economic, social and cultural conditions will be reduced.
CONCLUSION
Patients who suffer from diabetes especially those with type 2 diabetes mostly grapple with a chronic illness; however, they are generally not considered as resources to provide and improve DSME. Actually, if the peer-coaching model improves learning situations between patients with diabetes by offering one-on-one DSME, it could be an interactive approach to diabetic education.
It should be noted that due to the cultural, ethical and religious considerations, we will enroll the female patients with diabetes for the study. Thus, all the participants (patients and peers) were female.
Also, further researches aiming to consider peer support in diabetes management with more participants in the long term are recommended.
ACKNOWLEDGEMENT
This project was supported by Endocrinology and Metabolism Research Institute. We gratefully acknowledge the substantial contribution of all scientific and executive personnel of this institution. Moreover, we would like to thank the municipality of Tehran for its role in helping to access the diabetic patients. Last but not least, we would also like to extend our sincere thanks to all the diabetic patients who participated in this research project.
Conflict of Interest: None declared.
REFRENCES
- 1.Wild S, Roglic G, Green A, et al. Global prevalence of diabetes estimates for the year 2000 and projections for 2030. Diabetes care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.International Diabetes Federation (IDF) IDF diabetes atlas. 6th ed. Belgium: International Diabetes Federation; 2013. [Google Scholar]
- 3.American Diabetes Association: clinical practice recommendations 1999. Diabetes care. 1999;23:S1–S114. [PubMed] [Google Scholar]
- 4.International Diabetes Federation. Diabetes Atlas. 7th ed. Brussels, Belgium: International Diabetes Federation; 2015. [ Cited 12 October 2015] Available from: [http://www.diabetesatlas.org/ ]
- 5.Knowler WC, Barrett-Connor E, Fowler SE, et al. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thakurdesai PA, Kole PL, Pareek R. Evaluation of the quality and contents of diabetes mellitus patient education on Internet. Patient Education and Counseling. 2004;53:309–13. doi: 10.1016/j.pec.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Moattari M, Moosavinasab E, Dabbaghmanesh MH, ZarifSanaiey N. Validating a Web-based Diabetes Education Program in continuing nursing education: knowledge and competency change and user perceptions on usability and quality. Journal of Diabetes & Metabolic Disorders. 2014;13:12–70. doi: 10.1186/2251-6581-13-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moattari M, Hashemi M, Dabbaghmanesh MH. The impact of electronic education on metabolic control indicators in patients with diabetes who need insulin: a randomised clinical control trial. Journal of Clinical Nursing. 2013;22:32–8. doi: 10.1111/j.1365-2702.2012.04200.x. [DOI] [PubMed] [Google Scholar]
- 9.Mensing C, Boucher J, Cypress M, et al. National standards for diabetes self- management education. Diabetes Care. 2006;29:S78–85. [PubMed] [Google Scholar]
- 10.Gucciardi E. A systematic review of attrition from diabetes education services: strategies to improve attrition and retention research. Canadian Journal of Diabetes. 2008;32:53–65. [Google Scholar]
- 11.Norris SL, Engelgau MM, Narayan KV. Effectiveness of self-management training in type 2 diabetes a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–87. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 12.Clement S. Diabetes self-management education. Diabetes care. 1995;18:1204–14. doi: 10.2337/diacare.18.8.1204. [DOI] [PubMed] [Google Scholar]
- 13.Norris SL, Lau J, Smith SJ, et al. Self-Management education for adults with type 2 Diabetes A meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–71. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 14.Padgett D, Mumford E, Hynes M, et al. Meta-analysis of the effects of educational and psychosocial interventions on management of diabetes mellitus. Journal of Clinical Epidemiology. 1988;41:1007–30. doi: 10.1016/0895-4356(88)90040-6. [DOI] [PubMed] [Google Scholar]
- 15.Brown SA. Studies of educational interventions and outcomes in diabetic adults: a meta-analysis revisited. Patient Education and Counseling. 1990;16:189–215. doi: 10.1016/0738-3991(90)90070-2. [DOI] [PubMed] [Google Scholar]
- 16.Brown SA. Meta-analysis of diabetes patient education research: Variations in intervention effects across studies. Research in Nursing & Health. 1992;15:409–19. doi: 10.1002/nur.4770150603. [DOI] [PubMed] [Google Scholar]
- 17.Ellis SE, Speroff T, Dittus RS, et al. Diabetes patient education: a meta-analysis and meta-regression. Patient Education and Counseling. 2004;52:97–105. doi: 10.1016/s0738-3991(03)00016-8. [DOI] [PubMed] [Google Scholar]
- 18.Gary TL, Genkinger JM, Guallar E, et al. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. The Diabetes Educator. 2003;29:488–501. doi: 10.1177/014572170302900313. [DOI] [PubMed] [Google Scholar]
- 19.Brown SA. Interventions to promote diabetes self-management: state of the science. The Diabetes Educator. 1999;25:52–61. doi: 10.1177/014572179902500623. [DOI] [PubMed] [Google Scholar]
- 20.Norris SL. Self-management education in type 2 diabetes. Practical Diabetology. 2003;22:7–13. [Google Scholar]
- 21.Renders CM, Valk GD, Griffin SJ, et al. Interventions to improve the management of diabetes in primary care, outpatient, and community settings a systematic review. Diabetes Care. 2001;24:1821–33. doi: 10.2337/diacare.24.10.1821. [DOI] [PubMed] [Google Scholar]
- 22.Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;18:CD003417. doi: 10.1002/14651858.CD003417.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Roter DL, Hall JA, Merisca R, et al. Effectiveness of interventions to improve patient compliance: a meta-analysis. Medical Care. 1998;36:1138–61. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Barlow J, Wright C, Sheasby J, et al. Self-management approaches for people with chronic conditions: a review. Patient Education and Counseling. 2002;48:177–87. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 25.Skinner TC, Cradock S, Arundel F, Graham W. Four theories and a philosophy: self-management education for individuals newly diagnosed with type 2 diabetes. Diabetes Spectrum. 2003;16:75–80. [Google Scholar]
- 26.Anderson RM, Funnell MM, Nwankwo R, et al. Evaluating a problem-based empowerment program for African Americans with diabetes: results of a randomized controlled trial. Ethnicity and Disease. 2005;15:671–8. [PubMed] [Google Scholar]
- 27.Polonsky WH, Earles J, Smith S, et al. Integrating Medical Management With Diabetes Self-Management Training A randomized control trial of the Diabetes Outpatient Intensive Treatment Program. Diabetes Care. 2003;26:3048–53. doi: 10.2337/diacare.26.11.3048. [DOI] [PubMed] [Google Scholar]
- 28.Brown SA, Blozis SA, Kouzekanani K, et al. Dosage Effects of Diabetes Self-Management Education for Mexican Americans The Starr County Border Health Initiative. Diabetes care. 2005;28:527–32. doi: 10.2337/diacare.28.3.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bodenheimer T, MacGregor K, Sharifi C. Helping patients manage their chronic conditions[Internet]. US: California HealthCare Foundation; 2005. [Cited 5 August 2014] . Available from: [http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/PDF%20H/PDF%20HelpingPatientsManageTheirChronicConditions.pdf. ]
- 30.Funnell MM. Peer-based behavioural strategies to improve chronic disease self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Family Practice. 2010;27:i17–i22. doi: 10.1093/fampra/cmp027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davis C, Leveille S, Favaro S, LoGerfo M. Benefits to volunteers in a community-based health promotion and chronic illness self-management program for the elderly. Journal of Gerontological Nursing. 1998;24:16–23. doi: 10.3928/0098-9134-19981001-06. [DOI] [PubMed] [Google Scholar]
- 32.Pakin S, McKeganey N. The rise and rise of peer education approaches. Drugs: Education, Prevention, and Policy. 2000;7:293–310. [Google Scholar]
- 33.Rogers EM. Diffusion of innovation. 3rd ed. New York: Free Press; [Google Scholar]
- 34.Baksi A, Al-Mrayat M, Hogan D, Whittingstall E. Peer advisers compared with specialist health professionals in delivering a training programme on self-management to people with diabetes: a randomized controlled trial. Diabetic Medicine. 2008;25:1076–82. doi: 10.1111/j.1464-5491.2008.02542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Batik O, Phelan EA, Walwick JA, et al. Peer Reviewed: Translating a Community-Based Motivational Support Program to Increase Physical Activity Among Older Adults With Diabetes at Community Clinics: A Pilot Study of Physical Activity for a Lifetime of Success (PALS) Preventing Chronic Disease. 2008;5:A18. [PMC free article] [PubMed] [Google Scholar]
- 36.Cade J, Kirk SF, Nelson P, et al. Can peer educators influence healthy eating in people with diabetes? Results of a randomized controlled trial. Diabetic Medicine. 2009;26:1048–54. doi: 10.1111/j.1464-5491.2009.02808.x. [DOI] [PubMed] [Google Scholar]
- 37.Comellas M, Walker EA, Movsas S, et al. Training community health promoters to implement diabetes self-management support programs for urban minority adults. The Diabetes Educator. 2010;36:141–51. doi: 10.1177/0145721709354606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dale J, Caramlau I, Sturt J, et al. Telephone peer-delivered intervention for diabetes motivation and support: the telecare exploratory RCT. Patient Education and Counseling. 2009;75:91–8. doi: 10.1016/j.pec.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 39.Heisler M, Piette JD. “I Help You, and You Help Me” Facilitated Telephone Peer Support Among Patients With Diabetes. The Diabetes Educator. 2005;31:869–79. doi: 10.1177/0145721705283247. [DOI] [PubMed] [Google Scholar]
- 40.Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Annals of Internal Medicine. 2010;153:507–15. doi: 10.7326/0003-4819-153-8-201010190-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Klug C, Toobert DJ, Fogerty M. Healthy Changes for Living With Diabetes An Evidence-Based Community Diabetes Self-management Program. The Diabetes Educator. 2008;34:1053–61. doi: 10.1177/0145721708325886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lorig K, Ritter PL, Villa F, Piette JD. Spanish Diabetes Self-Management With and Without Automated Telephone Reinforcement Two randomized trials. Diabetes Care. 2008;31:408–14. doi: 10.2337/dc07-1313. [DOI] [PubMed] [Google Scholar]
- 43.Lorig K, Ritter PL, Villa FJ, Armas J. Community-Based Peer-Led Diabetes Self-management A Randomized Trial. The Diabetes Educator. 2009;35641:51. doi: 10.1177/0145721709335006. [DOI] [PubMed] [Google Scholar]
- 44.Thompson JR, Horton C, Flores C. Advancing Diabetes Self-Management in the Mexican American Population: A Community Health Worker Model in a Primary Care Setting. The Diabetes Educator. 2007;33:159S–165S. doi: 10.1177/0145721707304077. [DOI] [PubMed] [Google Scholar]
- 45.Tudor-Locke C, Lauzon N, Myers AM, et al. Effectiveness of the First step Program delivered by professionals versus peers. Journal of Physical Activity & Health. 2009;6:456–62. doi: 10.1123/jpah.6.4.456. [DOI] [PubMed] [Google Scholar]
- 46.Fisher EB, Brownson CA, O’Toole ML, Anwuri VV. Ongoing follow-up and support for chronic disease management in the Robert Wood Johnson Foundation Diabetes Initiative. The Diabetes Educator. 2007;33:201S–7S. doi: 10.1177/0145721707304189. [DOI] [PubMed] [Google Scholar]
- 47.Fisher EB, Thorpe CT, Devellis BM, Devellis RF. Healthy Coping, Negative Emotions, and Diabetes Management A Systematic Review and Appraisal. The Diabetes Educator. 2007;103:1080–103. doi: 10.1177/0145721707309808. [DOI] [PubMed] [Google Scholar]
- 48.Hill-Briggs F, Gemmell L. Problem Solving in Diabetes Self-management and Control A Systematic Review of the Literature. The Diabetes Educator. 2007;33:1032–50. doi: 10.1177/0145721707308412. [DOI] [PubMed] [Google Scholar]
- 49.American Diabetes Association. Standards of Medical Care in Diabetes-2015 Abridged for Primary Care Providers. Clinical Diabete. 2015;33:97–111. doi: 10.2337/diaclin.33.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baghiani Moghaddam, MH Bakhtari, Aghdam F, Asghari Jafarabadi M, et al. The Iranian Version of International Physical Activity Questionnaire (IPAQ) in Iran: content and construct validity, factor structure, internal consistency and stability. World Appl Sci. 2012;18:1073–80. [Google Scholar]
- 51.Vosoghi Karkazloo, N Abootalebi, Daryasari Gh, Farahani B, et al. The study of self-care agency in patients with diabetes (Ardabil) Modern Care Journal. 2012;8:197–204. [Google Scholar]
- 52.Nasihatkon A, Pishva AR, Habibzade F, et al. Reliability and validity of the clinical summary of Diabetic Quality Of Life (DQOL) in Farsi. Diabetes and Lipid Disorders Journal of Iran. 2012;11:483–7. [In persian] [Google Scholar]
- 53.Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory-Second edition: BDI-II-PERSIAN. Depression and Anxiety. 2005;21:185–92. doi: 10.1002/da.20070. [DOI] [PubMed] [Google Scholar]
- 54.Nedjat S, Majdzadeh R, Kheiltash A, et al. Social capital in association with socioeconomic variables in Iran. Social indicators research. 2013;113:1153–70. [Google Scholar]