INTRODUCTION
Asthma is a chronic condition that affects more than 6 million children nationwide. Along with morbidity from the disease itself, asthma carries a strong social and economic impact and disproportionately affects underserved, poor children.[1] Further, urban and minority children who suffer from asthma are more likely to receive insufficient preventive care,[2–5] leading to preventable morbidity.
Previous studies have shown that children with asthma are more likely to be overweight/obese than non-asthmatic children[6, 7] and are less likely to be physically active.[7–9] Obesity is a growing epidemic in the United States affecting roughly 12.7 million children and adolescents ages 2–19 years.[10] Further, obesity is related to a number of health conditions including heart disease, stroke, and type 2 diabetes, many of which are preventable.[11] While overall national rates of childhood obesity are concerning, these rates are disproportionately high in low income and minority populations. The prevalence of obesity is greater among Hispanic (22.4%) and non-Hispanic Black children (20.2%) than among non-Hispanic White (14.1%) children.[10] Further, children from low-income households have more than 2 times higher odds of being obese than children from higher income households. [12]
While guidelines from the National Heart, Lung and Blood Institute (NHLBI)[13] encourage the maintenance of normal physical activity for asthmatic children, people with asthma in general and specifically urban children with asthma tend to be less physically active.[14] In fact, inactivity itself may exacerbate asthma symptoms.[15] Poor asthma control can then interfere with normal activity and lead to a sedentary lifestyle and subsequent overweight status.[15] Unfortunately, this may be particularly true for high-risk urban children with asthma, who have suboptimal medication adherence, ongoing asthma symptoms, and a higher risk for obesity.[5, 10, 12, 16, 17] However, there is limited research on the barriers to activity that asthmatic children from disadvantaged homes may face.
This study aims to 1) determine the prevalence of overweight/obesity among a sample of high-risk children with asthma, 2) assess physical activity, activity limitations, and barriers to activity by level of asthma control, and 3) evaluate whether physical activity is associated with weight status in this population. A better understanding of barriers and limitations these children face to physical activity may help to ultimately promote the optimization of asthma control and healthy weight.
METHODS
Study Population
Data were obtained from a larger study, the School-Based Telemedicine Enhanced Asthma Management (SB-TEAM) program in Rochester, NY.[5, 16, 17] Caregivers of children ages 3–10 years with asthma were interviewed to assess eligibility. Eligibility requirements for the study included the child having a physician diagnosis of asthma, poorly controlled symptoms at the time of screening based on NHLBI criteria,[18] ability to communicate in English, and not having other chronic conditions that could alter accurate reporting of asthma symptoms (including Cystic Fibrosis, heart disease, and Sickle Cell Disease). Caregivers provided informed written consent, and oral assent was obtained from children seven years and older. The study protocol was approved by the Institutional Review Board at the University of Rochester.
The SB-TEAM program intervention includes two main components: the delivery of prescribed preventive medication in schools under the supervision of the school nurse and telemedicine visits at the school to provide ongoing assessment and adjustment of therapy as needed. Data for this analysis were drawn from a total of 324 baseline assessments conducted over three years (2012–2014; 78% participation rate), obtained during in-home, interviewer administered surveys with primary caregivers.
Assessment of Asthma Symptoms and Severity
We obtained information about the child’s asthma symptoms from standardized interviewer administered questionnaires completed with the child’s primary caregiver (the caregiver who spends the most time with the child). Caregivers were asked to report how often in a 14-day period their child experienced daytime and nighttime symptoms and days requiring rescue medication use.[5] Since the majority of children included in this study (65%) were prescribed a preventive medication at the time of the screening assessment, we matched the caregiver’s report of symptom frequency to an assessment of asthma control (rather than a severity assessment) for this analysis. Level of asthma control was estimated based on NHLBI criteria,[13] with children classified as having either ‘not well controlled’ or ‘very poorly controlled’ asthma, depending on the frequency of symptoms reported. Children with well controlled symptoms were not included based on eligibility criteria for the SB-TEAM study.
Assessment of Weight Status
During the baseline assessment the child’s height and weight were measured using a stadiometer and standardized scale, respectively. Child age was also collected at the time of the baseline interview. BMI for the child was calculated using Centers for Disease Control and Prevention (CDC) standards for height and weight using the BMI-for-age growth chart based on gender.[19] Children’s BMI was categorized as normal weight (BMI <85th percentile), overweight (BMI ≥85th and <95th percentile) or obese (BMI ≥95th percentile).
Assessment of Physical Activity and Barriers to Activity
Physical activity was assessed at the baseline interview which occurred during the fall to early winter months. Caregivers were asked to report on their child’s physical activity, as well as barriers and limitations their child experienced to being physically active.
Caregivers were also asked to report the amount of physical activity their child participated in throughout the period of an average week. Questions included the number of minutes and days their child participated in physical activity. Minutes of physical activity were dichotomized based on national recommendations for ≥60 minutes per day.[20]
Caregivers reported their child’s physical activity limitations using questions from the Children’s Health Survey for Asthma (CHSA) scale, a standardized, five-point Likert scale ranging from 1 (totally limited) to 5 (not limited).[21] Caregivers were asked to rate how much their child was limited in the last two weeks from participating in activities because of their asthma. Activities included “sports or running outside”, “very strenuous activities such as running fast or playing hard”, and “mild activities, such as walking”. We dichotomized responses for ‘any limitation’ vs. ‘not limited’.
We assessed barriers to physical activity from questions regarding the social and built-environment in which the child lived. Items included whether the child walked to/from school, whether there was recess at the child’s school, if they lived within walking distance to an outdoor play area, and whether there was a safe place for the child to play outdoors. We also explored minutes of ‘screen time’ including television viewing and computer use, and dichotomized responses to >2 hours/day based on national recommendations for maximum daily screen time.[22]
We included several child and caregiver demographics, including child age (continuous, and dichotomized at <5 years vs. ≥6 years), gender, race (white, black, other), ethnicity (Hispanic vs. non-Hispanic), insurance type (Medicaid/Public insurance vs. Other), smoker in the home (yes vs. no), and prescribed a preventive medication (yes vs. no). We also included caregiver age (continuous) and education level (<high school vs. ≥high school).
Analyses
We performed analyses using SPSS version 22 (Statistical Product and Service Solutions 22.0; SPSS Inc, Chicago, IL). Frequency analyses were used to provide descriptive data on the population, and to determine the prevalence of overweight and obese children within the sample.
We used chi-square and t-tests to compare levels of asthma symptom control with demographics and overweight/obese status. Bivariate and multivariate analyses were conducted to compare physical activity, limitations, and barriers to activity of children with ‘not well controlled’ symptoms to children with ‘very poorly controlled’ symptoms. In multivariate analyses, we controlled for race, ethnicity, insurance, age and gender (determined a priori).
We also conducted a multivariate logistic regression analysis to explore the relationship between physical activity, limitations, and barriers, with overweight/obese status. Variables for physical activity limitations that had a p-value of <0.10 were considered for inclusion in this logistic regression, along with level of control, preventive medication use, and a priori demographic variables, to test for the independent association between limitation in physical activity with overweight status. Among the activity limitation items, the variable “limited during mild activities” (yes vs. no) (p-value <.001) was chosen for inclusion in the full logistic regression model under the assumption that children limited in even mild activity would also be limited in more strenuous activity.
RESULTS
The sample included 324 children (mean age 7.9 years); 60% were male, 59% were Black, 31% Hispanic, and 69% were primarily insured by Medicaid (Table 1). Primary caregivers had a mean age of approximately 35 years, and 19% did not complete high school. Almost half (46%) of the children had a BMI greater than the 85%ile (15% overweight; 31% obese). Further, almost half of the children (46%) had symptoms indicating very poorly controlled asthma. Baseline demographics and overweight status did not differ by level of asthma control, with the exception that children with ‘not well controlled’ symptoms were older than those with ‘very poorly controlled’ symptoms (8.1 vs 7.6, p=.02).
Table 1.
Baseline Demographics and Other Characteristics
| Variable, N (%) | Overall N=324 | Not Well Controlled Symptoms N=173 | Very Poorly Controlled Symptoms N=151 | p-value |
|---|---|---|---|---|
| Child gender (Male) | 195 (60%) | 99 (58%) | 96 (64%) | 0.305 |
| Child age, mean (SD) | 7.9 (1.7) | 8.1 (1.6) | 7.6 (1.8) | 0.020 |
| Race (Black) | 191 (59%) | 101 (58%) | 90 (60%) | 0.945 |
| Ethnicity (Hispanic) | 101 (31%) | 57 (33%) | 44 (29%) | 0.473 |
| Medicaid insurance | 224 (69%) | 117 (68%) | 107 (71%) | 0.549 |
| Overweight (≥85th percentile) | 142 (46%) | 76 (46%) | 66 (46%) | 0.909 |
| Overweight (≥85-95th percentile) | 46 (15%) | 21 (13%) | 25 (18%) | 0.425 |
| Obese (≥95th percentile) | 96 (31%) | 55 (33%) | 41 (29%) | |
| Caregiver education <High school | 63 (19%) | 35 (20%) | 28 (18%) | 0.779 |
| Parent age, mean (SD) | 35.0 (8.4) | 34.7 (8.4) | 34.8 (8.4) | 0.874 |
| Smokers in Home (Yes) | 156 (48%) | 82 (47%) | 74 (49%) | 0.824 |
| Preventive Medication Prescribed (Yes) | 211 (65%) | 109 (63%) | 102 (68%) | 0.415 |
According to caregivers, fewer than half of children participated in the recommended ≥1 hour of physical activity per day (39%), and on average children only participated in physical activity 4.9 days per week (Table 2).
Table 2.
Activity Level, Limitations and Barriers Among Urban Children with Persistent Asthma
| Variable, N (%) | Overall N=324 | Not Well Controlled Symptoms N=173 | Very Poorly Controlled Symptoms N=151 | Adjusted P-value |
|---|---|---|---|---|
| Physical Activity Levels | ||||
|
| ||||
| Total minutes of activity (≥1 hour) | 121 (39%) | 71 (42%) | 50 (34%) | 0.125 |
| Does not participate in gym | 22 (7%) | 8 (5%) | 14 (9%) | 0.152 |
| Number of days of activity/week, mean (SD) | 4.9 (2.0) | 4.9 (2.0) | 4.8 (2.1) | 0.397 |
|
| ||||
| Limitation of Physical Activity | ||||
|
| ||||
| Limited during gym activities | 161 (50%) | 75 (43%) | 86 (58%) | 0.013 |
| Limited during sports activities | 196 (61%) | 89 (52%) | 107 (71%) | 0.001 |
| Limited during strenuous activities | 218 (67%) | 102 (59%) | 116 (77%) | 0.001 |
| Limited during mild activities | 68 (21%) | 25 (14%) | 43 (28%) | 0.004 |
| Does not run a lot at recess | 86 (44%) | 35 (34%) | 51 (55%) | 0.003 |
|
| ||||
| Physical Activity Barriers | ||||
|
| ||||
| Do not walk to/from school | 266 (85%) | 141 (84%) | 125 (86%) | 0.700 |
| Do not have recess at school | 119 (38%) | 65 (39%) | 54 (37%) | 0.820 |
| No safe place to exercise | 113 (35%) | 61 (35%) | 52 (34%) | 0.943 |
| Do not live within walking distance to outdoor play area | 51 (16%) | 30 (17%) | 21 (14%) | 0.334 |
| Does not go to outdoor play area 1x per week | 155 (57%) | 86 (61%) | 69 (53%) | 0.237 |
| Screen time ≥2 hours | 110 (34%) | 64 (37%) | 46 (31%) | 0.259 |
Adjusted for race, ethnicity, insurance, age and gender
Across all measures of physical limitations, more caregivers of children with ‘very poorly controlled’ asthma symptoms reported limitations in physical activity, compared to caregivers of children with ‘not well controlled’ symptoms, even when controlling for demographics. In our adjusted models, significantly more children with ‘very poorly controlled’ asthma experienced limitation in gym class (58% v. 43%, p = .013), during sports activities (71% v. 52%, p = .001), during strenuous activities (77% v. 59%, p = .001), and even during mild activities such as walking (28% v. 14%, p<.004). Further, more caregivers of children with ‘very poorly controlled’ asthma reported their child did not run a lot during recess (55% v. 34%, p = .003) compared to caregivers of children with milder symptoms.
Barriers to being physically active were also measured by caregiver report. Overall, the majority of caregivers reported that their child did not walk to/from school (85%), 38% reported that their child did not have recess at school, and 35% of caregivers reported that there was no safe place for their child to exercise. Additionally, 16% of caregivers reported that their family does not live within walking distance to outdoor play areas, and 57% reported that their children did not go to an outdoor play area at least one time per week. In addition, 34% of caregivers reported that their child viewed 2 or more hours of screen time per day. There were no significant differences in reported barriers to physical activity by asthma control group.
In a logistic regression analysis (Table 3), we found that children who were limited in mild physical activity had 2 times greater odds of being overweight or obese compared to those children who were not limited in mild physical activity, even when adjusted for asthma symptoms (adjusted OR 2.1; 95% CI; 1.2,3.8). Child age was also associated with overweight/obese, with a greater odds of being overweight as the child gets older (adjusted OR 2.5; 95% CI; 1.1,6.0).
Table 3.
Factors Associated with Overweight Status in Multivariate Logistic Regression
| Variable | OR | 95% CI | P-value |
|---|---|---|---|
| Age | |||
| <5 years | 1.0 | - | - |
| ≥6 years | 2.5 | (1.0, 6.0) | 0.04 |
| Race | |||
| White | 1.0 | - | - |
| Black | 1.1 | (0.4, 2.9) | 0.80 |
| Other/Mixed | 1.2 | (0.4, 3.3) | 0.75 |
| Ethnicity | |||
| Hispanic | 0.8 | (0.3, 1.7) | 0.49 |
| Non-Hispanic | 1.0 | - | - |
| Insurance | |||
| Medicaid Insurance | 0.8 | (0.5, 1.4) | 0.47 |
| Non-Medicaid Insurance | 1.0 | - | - |
| Child gender | |||
| Female | 1.0 | - | - |
| Male | 1.1 | (0.7, 1.8) | 0.58 |
| Activity Limitation | |||
| Limited in mild activities | 2.1 | (1.2, 3.9) | 0.01 |
| Not limited in mild activities | 1.0 | - | - |
| Preventive Medication Use | |||
| Yes, medication use | 0.9 | (0.6, 1.6) | 0.93 |
| No, medication use | 1.0 | - | - |
| Symptom Control | |||
| Not Well Controlled | 1.0 | - | - |
| Very Poorly Controlled | 0.9 | (0.6, 1.5) | 0.74 |
CI, confidence interval; OR, odds ratio;
DISCUSSION
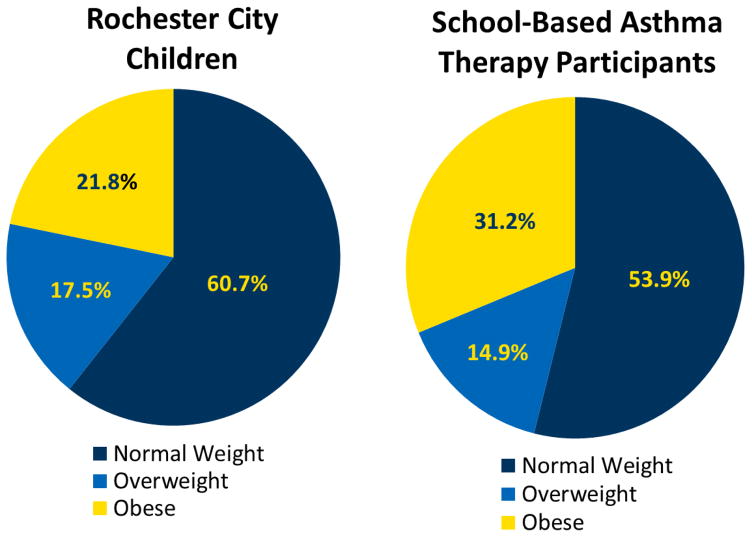
In this sample of urban children with asthma, we observed a very high prevalence of overweight and obesity (46%). In fact, the prevalence of overweight status in our study sample was even higher than in the general population of urban children aged 3–10 years in Rochester, NY (Figure 1).[23] We found that physical activity was significantly limited among this group of children. Overall, caregivers reported that fewer than half of children participated in the recommended 1 or more hours of physical activity per day, and on average only participated in any physical activity 4.9 days per week. This suggests that urban children who suffer from asthma are not achieving even the minimum recommended levels of physical activity, neither daily nor weekly.[13, 18] These findings are consistent with prior literature demonstrating a higher prevalence of obesity in children with asthma,[6, 24] as well as lower levels of activity per day among children with moderate or severe persistent symptoms relative to children without asthma.[14]
Figure 1.
Weight Status among Urban Children with Asthma Compared to Rochester City Children
We also found that, relative to children with more mild asthma symptoms, those with very poorly controlled symptoms experienced more limitation in gym class, during sports and strenuous activities, and even during mild activities. While we do not know if participation in gym was restricted by school officials because the child had asthma, or by the child or caregiver due to concerns about the child’s asthma symptoms, clearly more work is needed to promote school-based physical activity for these children. Appropriate education for families and for all school personnel can help to avoid misconceptions around asthma and physical activity. Furthermore, ensuring that children with asthma have rescue medications available at school, and optimizing asthma control with guideline-based preventive measures is an important first step toward reducing physical activity limitations among this population of children.[16]
We also found more than a third of these young school children did not have any recess at school, despite evidence that school-based physical activity has documented benefits for overall overweight/obesity prevention as well as improved health of children with asthma.[13, 25] Interestingly, while the majority of caregivers reported living within walking distance of a playground or park, more than 1/3 reported that there is no safe place to exercise near their home and few children frequented outdoor play areas. Thus, in addition to activity limitation there are also environmental barriers to attaining physical activity. This highlights the need for further research about these barriers and what steps can be taken to overcome them. Understandably, safety is a concern in urban environments, and harsh weather conditions may also impact outdoor play in some locations particularly in the fall and winter months. Advocating for clean, well-lit and patrolled playgrounds as well as indoor play areas, and empowering parent volunteers and neighborhood watch organizations to supervise parks may help to address safe play areas in urban environments.[26, 27] Further, these environmental barriers further highlight the need for schools to ensure daily safe play for young urban school children, as this may be their only opportunity for physical activity.
The relationship between asthma and obesity is bi-directional,[6–8, 10]and both can impact participation in physical activity.[7–9, 14, 15] Our data show that asthmatic children with limitation in physical activity had a 2 times greater odds of being overweight or obese compared to asthmatic children with no limitation in physical activity. These findings contribute to current literature which shows that limitation in physical activity is related to obesity in asthmatic children.[6, 7]
There are some potential limitations to this study. First, the study population only includes children with poorly controlled asthma and therefore we are unable to make comparisons of activity level and weight status with children with less significant symptoms and children without asthma. Since the majority of children were prescribed a preventive medication at the time of enrollment, we were not able to assess the underlying severity of their disease, but rather focused on a symptom-based assessment of control. Importantly, though, only 65% of the children enrolled in this study were prescribed a preventive asthma medication, which represents clear under treatment for large numbers of children.[15] There is a potential for over-diagnosing asthma among patients with obesity,[28–30] which could have influenced our study sample. Further, findings from this study can only be generalized to similar populations and school districts, however we would argue that this population is the most at-risk, relative to non-asthmatic, higher income children, and in need of action around the area of focus. The cross-sectional nature of this study precludes us from making a causal association between the physical activity levels of children with persistent asthma and weight status. Further, we did not have an objective measure of physical activity and instead relied on caregiver report. While data collection was strengthened by structured interviewer-led methods, there was a potential for caregivers to be subjected to social desirability bias and under report physical activity limitations.
This study was strengthened by the large sample of more than 300 subjects and a high participation rate from the parent study. Additionally, we used an objective measure of height and weight to calculate BMI. Finally, the parent study used a community-based recruitment strategy, thus the population represents a broad group of children with asthma from an urban, inner-city setting.
The relationship between asthma and obesity is complex. Limitations in activity participation and barriers to physical activity among children with poorly controlled asthma present significant challenges for the prevention of unhealthy weight gain and promotion of optimal asthma control. Solutions will likely require a multifaceted approach with healthcare systems, schools, and communities working together to ensure delivery of guideline-based preventive asthma treatment, reduce misconceptions, and eliminate barriers in order to promote full participation in activity.
Acknowledgments
Funding Source: NIH/NHLBI 2R01HL079954
Abbreviations
- BMI
Body Mass Index
- SB-TEAM
School-Based Telemedicine Enhanced Asthma Management
- NHLBI
National Heart, Lung and Blood Institute
- CDC
Centers for Disease Control and Prevention
- CHSA
Children’s Health Survey for Asthma
Footnotes
Trial Registration: www.clinicaltrials.org reference #: NCT01650844
Author Contribution:
Conception and design of the study: All authors
Data generation: Ms. Holderness, Ms. Fagnano
Analysis and interpretation of the data: All authors
Preparation or critical revision of the manuscript: All authors
Conflicts of Interest: Dr. Halterman and Dr. Reznik declare that they have received research grant funding from the National Institutes of Health. The remaining authors declare that they have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Akinbami LJ, Moorman JE, Simon AE, Schoendorf KC. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001–2010. Journal of Allergy and Clinical Immunology. 2014;134(3):547–553. doi: 10.1016/j.jaci.2014.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cabana MD, Lara M, Shannon J. Racial and Ethnic Disparities in the Quality of Asthma Care. CHEST. 2007;132(5_suppl):810S–817S. doi: 10.1378/chest.07-1910. [DOI] [PubMed] [Google Scholar]
- 3.Akinbami LJ, LaFleur BJ, Schoendorf KC. Racial and income disparities in childhood asthma in the United States. Ambul Pediatr. 2002;2(5):382–387. doi: 10.1367/1539-4409(2002)002<0382:raidic>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 4.Lieu TA, Lozano P, Finkelstein JA, et al. Racial/ethnic variation in asthma status and management practices among children in managed medicaid. Pediatrics. 2002;109(5):857–865. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- 5.Halterman JS, Szilagyi PG, Fisher SG, et al. Randomized controlled trial to improve care for urban children with asthma: results of the School-Based Asthma Therapy trial. Arch Pediatr Adolesc Med. 2011;165(3):262–268. doi: 10.1001/archpediatrics.2011.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gennuso J, Epstein LH, Paluch RA, Cerny F. The relationship between asthma and obesity in urban minority children and adolescents. Arch Pediatr Adolesc Med. 1998;152(12):1197–1200. doi: 10.1001/archpedi.152.12.1197. [DOI] [PubMed] [Google Scholar]
- 7.Fedele DA, Janicke DM, Lim CS, Abu-Hasan M. An examination of comorbid asthma and obesity: assessing differences in physical activity, sleep duration, health-related quality of life and parental distress. J Asthma. 2014;51(3):275–281. doi: 10.3109/02770903.2013.873807. [DOI] [PubMed] [Google Scholar]
- 8.Glazebrook C, McPherson AC, Macdonald IA, et al. Asthma as a barrier to children's physical activity: implications for body mass index and mental health. Pediatrics. 2006;118(6):2443–2449. doi: 10.1542/peds.2006-1846. [DOI] [PubMed] [Google Scholar]
- 9.Brasholt M, Baty F, Bisgaard H. Physical activity in young children is reduced with increasing bronchial responsiveness. J Allergy Clin Immunol. 2010;125(5):1007–1012. doi: 10.1016/j.jaci.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108(3):712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 12.Food Research and Action Center. [Accessed September 13, 2016];Relationship Between Poverty and Obesity. http://frac.org/initiatives/hunger-and-obesity/are-low-income-people-at-greater-risk-for-overweight-or-obesity/
- 13.National Heart, Lung, and Blood Institute. Full Report 2007. U.S. Department of Health and Human Services; 2007. National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. NIH publication 08–4051. [Google Scholar]
- 14.Lang DM, Butz AM, Duggan AK, Serwint JR. Physical activity in urban school-aged children with asthma. Pediatrics. 2004;113(4):e341–346. doi: 10.1542/peds.113.4.e341. [DOI] [PubMed] [Google Scholar]
- 15.Ritz T, Rosenfield D, Steptoe A. Physical activity, lung function, and shortness of breath in the daily life of individuals with asthma. CHEST. 2010;138(4):913–918. doi: 10.1378/chest.08-3073. [DOI] [PubMed] [Google Scholar]
- 16.Halterman JS, Borrelli B, Fisher S, Szilagyi P, Yoos L. Improving care for urban children with asthma: design and methods of the School-Based Asthma Therapy (SBAT) trial. J Asthma. 2008;45(4):279–286. doi: 10.1080/02770900701854908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Halterman JS, Fagnano M, Montes G, et al. The school-based preventive asthma care trial: results of a pilot study. J Pediatr. 2012;161(6):1109–1115. doi: 10.1016/j.jpeds.2012.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. Department of Health and Human Services. [Accessed September 14, 2016];2008 Physical Activity Guidelines for Americans. 2008 ODPHP Publication No. U0036. [ https://health.gov/paguidelines/pdf/paguide.pdf]
- 19.Centers for Disease Control and Prevention. [Accessed September 13, 2016];About Child & Teen BMI. http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html#HowIsBMICalculated.
- 20.Centers for Disease Control and Prevention. [Accessed September 14, 2016];Physical activity for everyone: Guidelines. http://www.cdc.gov/physicalactivity/everyone/guidelines/children.html.
- 21.Asmussen L, Olson LM, Grant EN, Fagan J, Weiss KB. Reliability and validity of the Children's Health Survey for Asthma. Pediatrics. 1999;104(6):e71. doi: 10.1542/peds.104.6.e71. [DOI] [PubMed] [Google Scholar]
- 22.American Academy of Pediatrics Committee on Public Education. Children, adolescents, and television. Pediatrics. 2001;107(2):423–426. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 23.Monroe County Department of Public Health. [Accessed September 13, 2016];Maternal/Child Health Report Card Update. 2011 Feb; https://www2.monroecounty.gov/files/health/DataReports/MCH%20Report%20Card,%202011%20FINAL.pdf.
- 24.von Kries R, Hermann M, Grunert VP, von Mutius E. Is obesity a risk factor for childhood asthma? Allergy. 2001;56(4):318–322. doi: 10.1034/j.1398-9995.2001.00727.x. [DOI] [PubMed] [Google Scholar]
- 25.Walker TJ, Reznik M. In-school asthma management and physical activity: children's perspectives. J Asthma. 2014;51(8):808–813. doi: 10.3109/02770903.2014.920875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakahara S, Nakamura Y, Ichikawa M, Wakai S. Relation between increased numbers of safe playing areas and decreased vehicle related child mortality rates in Japan from 1970 to 1985: a trend analysis. J of Epidemiology & Community Health. 2004;58(12):976–981. doi: 10.1136/jech.2003.018804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen DA, Han B, Isacoff J, et al. Impact of park renovations on park use and park-based physical activity. J of Physical Activity & Health. 2015;12(2):289–295. doi: 10.1123/jpah.2013-0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bibi H, Shoseyov D, Feigenbaum D, et al. The relationship between asthma and obesity in children: is it real or a case of over diagnosis? J Asthma. 2004;41(4):403–410. doi: 10.1081/jas-120026097. [DOI] [PubMed] [Google Scholar]
- 29.Sah PK, Gerald Teague W, Demuth KA, Whitlock DR, Brown SD, Fitzpatrick AM. Poor asthma control in obese children may be overestimated because of enhanced perception of dyspnea. The Journal of Allergy and Clinical Immunology In Practice. 2013;1(1):39–45. doi: 10.1016/j.jaip.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pakhale S, Doucette S, Vandemheen K, et al. A comparison of obese and nonobese people with asthma: exploring an asthma-obesity interaction. CHEST. 2010;137(6):1316–1323. doi: 10.1378/chest.09-2491. [DOI] [PubMed] [Google Scholar]