Abstract
Objective
Investigate cross-sectional and longitudinal associations of Diffuse Idiopathic Skeletal Hyperostosis (DISH) and thoracic kyphosis in older persons.
Methods
DISH and kyphosis were assessed in 1500 men from the Osteoporosis in Men (MrOS) study and 1267 women from the Study of Osteoporotic Fractures (SOF). DISH was assessed in baseline lateral spine radiographs, and Cobb angle of kyphosis was measured from baseline and follow-up radiographs, mean 4.6 years later in men, and 3.7 and 15 years later in women. Linear regression was used to analyze associations of DISH with baseline Cobb angle and with percent annualized change in Cobb angle. We tested for heterogeneity among studies.
Results
DISH was identified in 222 (15%) participants in MrOS and 156 (12%) participants in SOF. Participants with DISH in both cohorts had higher baseline Cobb (p<0.05), after adjusting for covariates. After approximately 4 years of follow-up, there was no significant difference in annualized percent change in Cobb among those with DISH compared to those without DISH (p>0.05) for men or women. Women with DISH had less progression of kyphosis over 15 years (0.25% less annualized change in Cobb) than those without DISH.
Conclusions
Prevalent DISH is associated with greater kyphosis in older men and women, and not significantly associated with change in kyphosis over 4–5 years. However, among women followed over 15 years, DISH was associated with less progression of kyphosis. These results suggest DISH influences kyphosis and may slow progression over long-term. Additional studies of DISH/kyphosis associations are warranted to understand functional implications.
Keywords: aging, gender, longitudinal studies, x-ray, spine
Diffuse idiopathic skeletal hyperostosis (DISH), characterized by ossifications of the anterior longitudinal ligament over at least 3 vertebral segments, and thoracic kyphosis are well-defined radiographic findings in the spines of older individuals. Both of these spinal conditions are known to impact physical function.1–5 DISH is a non-inflammatory disease, more common in men over the age of 60, with genetic, hormonal and mechanical factors that affect calcification and ossification in ligaments, tendons and bones.1 DISH can affect the anterior longitudinal ligament in the thoracic and thoracic-lumbar spine and is associated with loss of spinal mobility.6
Kyphosis, an anterior curvature in the thoracic spine, increases with age.7 Hyperkyphosis, commonly defined as a Cobb angle of kyphosis 40 degrees or more, has been associated with loss of spinal mobility in axial extension and rotation.8 Higher degrees of kyphosis are correlated with underlying bone, disc, and muscle pathology that impair upright spinal posture.9–12 Kyphosis progression among older women has been attributed to prevalent and incident vertebral fractures, low bone mineral density and concurrent bone density loss, low body weight, and concurrent weight loss.10 Higher kyphosis among older men is similarly influenced by incident vertebral fractures and low bone density, but in contrast to women, it also appears to be influenced by degenerative disc disease.13 Kyphosis progression in older men has not been previously reported. DISH could hasten the natural progression of kyphosis with age, but it is not known if DISH affects the progression of kyphosis in either sex.
DISH has recently been associated with greater Cobb angle of kyphosis in a cohort of older men and women from the Health Aging and Body Composition study, although that cohort was two sites in the eastern US, and subject recruitment focused on blacks, so it is not known whether that cohort is representative of older adults in the US.14 Both DISH and excessive kyphosis have been associated with worse physical function in older adults1–5 which supports the need to better understand their causal relationships. Additionally, we wanted to examine these associations in men and women in cross-sectional and longitudinal models because this has never been done and we thought this information would inform the medical community about these common, yet not well understood musculoskeletal problems of the aging population.
The aims of this study were to investigate the association of DISH with thoracic kyphosis in older men and women, and to describe the short-term change in kyphosis in older men from the Osteoporotic Fractures in Men (MrOS) Study and the short- and long-term changes in older women from the Study of Osteoporotic Fractures (SOF). In addition, given the higher prevalence of DISH in men, we sought to determine sex differences in the association of DISH with kyphosis cross-sectionally and over time.
Patients and Methods
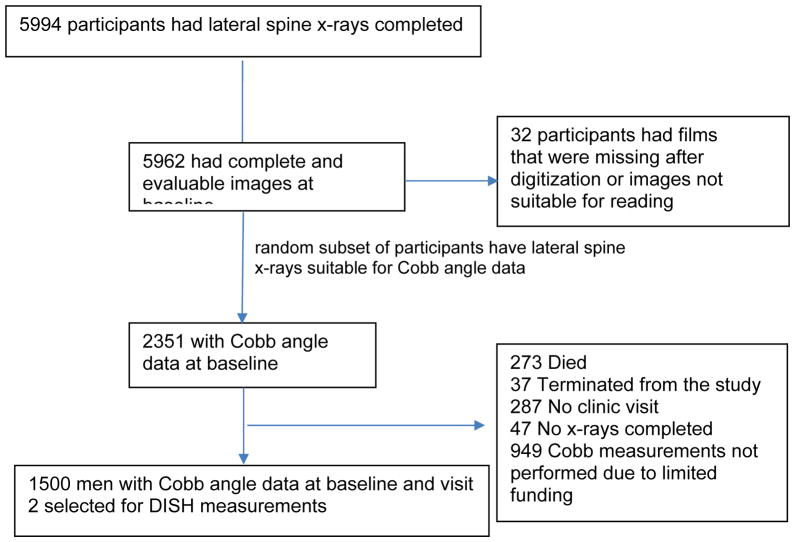
MrOS is a prospective cohort study of 5,994 community-dwelling older men who were 65 years and older when recruited in 2000–2002 from 6 academic medical centers in Birmingham AL; Minneapolis MN; Palo Alto CA; Pittsburgh PA; Portland OR; and San Diego CA.15,16 The study was initially designed to examine risk factors for fracture and osteoporosis in men. Of the 5,994 men enrolled in MrOS, 5229 men returned for a follow-up visit a mean 4.6 (SD=0.4) years later; 2351 of these men with lateral spine radiographs at both visits were randomly selected for kyphosis measurements. Our sample included a subset of 1500 men in the MrOS with lateral spine radiographs at both visits who had been previously randomly selected for kyphosis measurements (Figure 1). The subset of participants included in our sample compared to the overall MrOS cohort were healthier and reported less diabetes and fewer functional limitations.
Figure 1.
Flow chart of MrOS men selection for DISH measurements
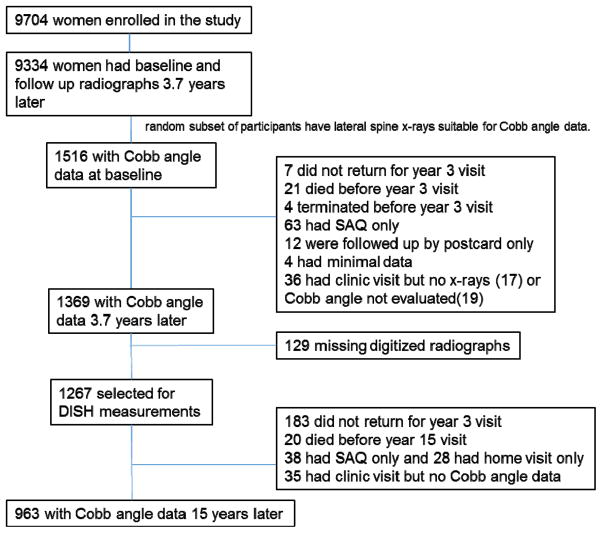
SOF is a prospective cohort study of 9,704 ambulatory white women aged 65 years or older when recruited in 1986 to 1988 from 4 academic medical centers in Baltimore MD; Minneapolis MN; Pittsburgh PA and Portland OR to study risk factors for fracture.17 Of the 9704 women enrolled in SOF, 9334 returned for a follow-up visit a mean 3.7 years later. We used data from 1267 women in the SOF randomly selected from the 9334 cohort who had baseline and follow-up measurements of kyphosis from radiographs of the thoracic spine at both visits (Figure 2). Among these women, 963 had follow-up radiographs and Cobb angle measurements 15 years later and were assessed for long term change in Cobb angle. DISH measurements were not calculated for 2 women due to poor image quality. Hence the total number of women used in the analysis was 1265 and 961 with Cobb angle measurements 3.7 years and 15 years later respectively. The subset of participants included in our sample compared to the overall SOF cohort were younger, heavier, had higher calcaneal BMD and fewer vertebral fractures.10
Figure 2.
Flow chart of SOF women selection for DISH measurements
Conduct of the MrOS and SOF studies was approved by the Institutional Review Board of each of the participating research centers. Written informed consent was obtained from all participants at each study visit.
Measurements
DISH
An experienced radiologist (ZM) read all baseline radiographs for the presence of DISH. A diagnosis of DISH was made according to the Resnick criteria that specifies 3 strict radiographic findings in the spine: flowing calcification and ossification along the anterolateral aspect of at least four contiguous vertebral bodies, relative preservation of the intervertebral disk height in the involved vertebral segment and the absence of extensive radiographic changes of degenerative disc disease, and the absence of apophyseal joint ankylosis and costovertebral joint fusion.18 All DISH participants had involvement of thoracic spine and 1 (0.08%) in SOF and 10 (0.67%) in MrOS had additional lumbar involvement. Thus DISH in both locations was combined into one DISH variable indicating presence or absence of DISH. Intra- and inter-rater agreement of this diagnosis was previously reported in another study of older adults at a kappa value of 0.9 (95% CI: 0.8, 0.9) and 0.6 (95% CI: 0.5, 0.7), respectively14.
Kyphosis
Cobb angle of kyphosis was measured from supine lateral thoracic spine radiographs according to published guidelines at a distance of 40 inches (102 cm) with a vertical beam centered on T7.19 Digital images were acquired in MrOS and conventional film was used in SOF. A trained technologist calculated the Cobb angle by placing digitized points to permit an automated computer reading. The technologist identified and placed digitized points marking the upper endplate inner and outer corners of T4, and lower endplate inner and outer corners of T12. The computerized program used these 4 points to erect straight lines and determine the angle of intersection. If for any reason either the upper end of T4 or lower end of T12 were not well visualized, the adjacent above and below vertebrae were used as alternative upper or lower vertebral bodies to define the angle of curvature.19 The Cobb angle intraclass correlation coefficients (ICC) have previously been reported in SOF at 0.99 for repeated observers from the same radiograph and 0.82 for single measurements from repeated radiographs.19,20
Prevalent and Incident Radiographic Vertebral Fractures
In MrOS, prevalent radiographic vertebral fractures were defined as a grade 2 or grade 3 fracture using the Genant semi-quantitative method, and incident vertebral fractures were defined as increase in SQ grade of ≥ 1.21 In SOF, prevalent radiographic vertebral fractures were defined using a full quantitative morphometric method (the modified Melton/Eastell criteria) fully described in prior publications.22 Incident radiographic vertebral fractures in SOF were defined as a >20% and >4 mm decrease in anterior, middle, or posterior vertebral height compared to the baseline radiograph.23
Physical and anthropometric measures
All physical and anthropometric measures were obtained at initial enrollment. Measurements of height and weight were obtained by Harpenden stadiometers and balance beam or digital scales. BMI was calculated as weight (kg) divided by height2 (m2). Bone mineral density (BMD) was measured at the proximal femur and spine using dual energy X-ray absorptiometry (QDR 4500; Hologic, Inc., Waltham, MA) in MrOS. Calcaneal bone mineral density collected at enrollment using single-photon absorptiometry (OsteoAnalyzer, Siemens-Osteon, Wahiawa, Hawaii) was used for BMD measurements in SOF.17 From a subsequent visit 2 years later, hip BMD with a Hologic QDR 1000 scanner15,24 was used in a sensitivity analysis.
Questionnaires
Information about age, demographic factors and medical history, including self-reported diabetes (reported insulin dependence or fasting glucose >126), functional limitations in instrumental activities of daily living (IADL) and physical disability, and use of osteoporosis medications, were obtained by self-administered questionnaires at the enrollments visits. Functional limitation was determined as being unable to perform one of the following IADL(shopping, meals or housework) and one of the following (walk 2–3 blocks or climb 10 steps). Race was self-reported at enrollment in MrOS, and was categorized as white versus non-white.
Statistical Methods
Baseline characteristics between those with DISH and without DISH were assessed using t-test for continuous or Wilcoxon nonparametric tests for non-normally distributed data and Chi square tests for categorical variables.
We ran separate models for each cohort. We first constructed a multivariate base model adjusted for age, race (for MrOS men), enrollment site and BMI and then added covariates that were selected a priori, one covariate at a time, to determine its impact on the association between DISH and Cobb angle. Additional covariates included 1) total hip BMD for men and calcaneal BMD for women, and 2) prevalent vertebral fractures. We expected that the association between DISH and Cobb angle would be reduced after adjusting for these factors if they were in the causal pathway. To obtain final multivariate estimates for the association between DISH and Cobb angle, we included age, race (for MrOS men), enrollment site, BMI, BMD and prevalent vertebral fractures in the models. For longitudinal analyses, we added incident vertebral fractures as a covariate.
Cross-sectional models
The association between DISH and Cobb angle was analyzed using linear regression, and least square means and 95% confidence intervals (CI) were calculated. The percent difference in the baseline Cobb angle in those with DISH compared to those without DISH was calculated as follows: Percent difference = (least square means/mean Cobb angle in those without DISH)*100. Models were adjusted as described above.
Longitudinal models
In this analysis, we were concerned that assessing longitudinal change by adjusting for the baseline Cobb angle as a covariate would produce invalid estimates of change because of the association of DISH and baseline level of Cobb angle.25 Therefore, we used annualized percent change as our primary outcome. Change in Cobb angle was measured by calculating the annualized percent change in Cobb angle from baseline to the follow up. Short term annualized percent change was calculated as change from baseline to visit 2 (4.6 years in MrOS) and visit 3 (3.7 years in SOF), while long term annualized percent change was only available for the SOF cohort and was calculated as annualized percent change from baseline to visit 8 (15 years from enrollment). Annualized percent change was calculated as the percent change in Cobb angle from baseline divided by number of years of follow-up to the next visit to provide a measure of percent change per year.
Multivariate linear regression models as outlined above were conducted to determine the association of short-term and long-term annualized percent changes in participants with DISH compared to those without DISH.
To determine if sex modified the association of DISH and Cobb angle in men (MrOS) and women (SOF), we conducted a meta-analysis using the least square means and 95% confidence intervals from each of the linear regression models performed for the association of DISH and Cobb angle in each of the cohorts. We reported the p-value from the test of significance of heterogeneity between the two cohorts for each regression model.
Data collected from the study was analyzed using the SAS software (version 9.2, Cary, NC).
Results
At baseline, DISH was identified in 222 (15%) men and 156 (12%) women. The mean Cobb angle overall was 39 (SD=11) degrees in men and 45 (SD=12) degrees in women. Participants with DISH compared to those without DISH had greater Cobb angle in both cohorts (Table 1). The men with DISH were slightly older, and had higher BMI, hip and spine BMD than those without DISH, but no difference in morphometric fractures or functional limitation. Women with DISH had higher BMI, hip, calcaneal and spine BMD, and fewer morphometric vertebral fractures than those without DISH. Women with DISH reported more functional limitation.
Table 1.
Characteristics at baseline in MrOS (men) and SOF (women) by presence of DISH
| Characteristics at baseline | Men | Women | ||||
|---|---|---|---|---|---|---|
| No Dish (N= 1278) | Dish (N= 222) | P-value | No Dish (N= 1109) | Dish (N= 156) | P-value | |
| Age (years) | 73 ± 5 | 73 ± 6 | 0.02 | 69.6 ± 4.2 | 69.5 ± 3.9 | 0.73 |
| White | 1157 (90.5) | 207 (93.2) | 0.19 | N/A | N/A | N/A |
| Cobb angle (degrees) | 38 ± 11 | 41 ± 11 | <.001 | 45 ± 12 | 47 ± 13 | 0.02 |
| Baseline Cobb angle <40, n (%) | 78(58.5) | 106 (47.8) | 0.003 | 424 (38.2) | 53 (34.0) | 0.30 |
| BMI (kg/m2) | 27 ± 4 | 29 ± 4 | <.001 | 26 ± 4 | 29 ± 5 | <.001 |
| Total hip BMD (g/m2) | 0.96 ± 0.13 | 1.01 ± 0.14 | <.001 | 0.77 ±0.12 | 0.80 ± 0.10 | 0.02 |
| Spine BMD (g/m2) | 1.05 ± 0.17 | 1.15 ± 0.20 | <.001 | 0.86 ± 0.15 | 0.90 ± 0.20 | 0.01 |
| Prevalent vertebral fracture, yes (%) | 83 (6.5) | 20 (9.0) | 0.17 | 201 (18.1) | 13 (8.3) | <.001 |
| Self-reported diabetes (insulin dependence or fasting glucose >126) (%) | 149 (12.4) | 33 (16.4) | 0.11 | 41 (3.71) | 15 (9.62) | <0.001 |
| Osteoporosis drugs, yes (%) | 24 (2.0) | 3 (1.4) | 0.59 | N/A | N/A | N/A |
| Functional limitation, yes (%) | 63 (4.93) | 12 (5.41) | 0.76 | 81 (7.3) | 22 (14.1) | 0.004 |
| Absolute short-term change in Cobb angle (degrees) | 1.4 ± 5.6 | 0.9 ± 4.8 | 0.12 | 2.5 ± 5.1 | 2.1 ± 4.3 | 0.36 |
| Annualized short-term percent change in Cobb angle (%) | 1.1 ± 4.2 | 0.7 ± 3.0 | 0.14 | 1.7 ± 3.6 | 1.3 ± 2.8 | 0.13 |
Cross-sectional associations
In men, there was a 7.9% (95% CI: 3.7, 12.2) greater Cobb angle among those with DISH compared to those without DISH in models adjusted for age, race, clinic site and BMI, p<0.001 (Table 2). When adjusted for all covariates, this increased to 8.6% (95% CI: 4.3, 12.8) greater Cobb angle. In women, there was a 5.8% (95% CI: 1.2, 10.4) greater Cobb angle among those with DISH compared to those without DISH when adjusted for age, clinic site and BMI, p<0.01. When adjusted for all covariates, this increased to 8.0% (95% CI: 3.5, 12.4) greater Cobb angle. The test for heterogeneity among men and women in base model was not significant, p=0.76.
Table 2.
Percent difference (95% CI) in Cobb angle at baseline among those with DISH compared to those without DISH, by sex
| Men (N=1500) | Women (N=1265) | |||
|---|---|---|---|---|
| Percent difference (95%CI) | P-value | Percent difference (95%CI) | P-value | |
| Base model1 | 7.92 (3.68–12.15) | <0.001 | 5.81 (1.19 to 10.43) | 0.01 |
| Base + total hip BMD | 8.98 (4.75 to 13.22) | <.001 | 6.57 (2.03 to 11.1) | 0.005 |
| Base + prevalent and incident vertebral fracture | 8.55 (4.31 to 12.8) | <.001 | 7.63 (3.2 to 12.07) | <0.001 |
| Full multivariate model (MV) 2 | 8.55 (4.31 to 12.8) | <.001 | 7.99 (3.54 to 12.44) | <0.001 |
Base model adjusted for age, race (in MrOS only), clinic site and BMI
MV model is adjusted for age, race (in MrOS only), clinic site, BMI, total hip BMD (calcaneal BMD in SOF), prevalent and incident vertebral fractures and self-reported diabetes.
Short-term associations
The absolute overall short-term change in Cobb angle of kyphosis was 1.3 degrees (SD = 5.5) over 4.6 years in men and 2.4 (SD = 5.0) degrees over 3.7 years in women. There was no association of DISH and short-term absolute or annualized percent change in Cobb angle in any model in either cohort (p≥0.19) (Table 3). The test for heterogeneity in the base model was not significant, p=0.94.
Table 3.
Annualized percent change in Cobb angle over an average of 4.6 years in men and 3.7 years in women with DISH and without DISH
| Men (N=1500) | *Women (N=1265) | |||||
|---|---|---|---|---|---|---|
| Adjusted means of annualized percent change in Cobb angle (95%CI) | P for trend | Adjusted means of annualized percent change in Cobb angle (95%CI) | P for trend | |||
|
| ||||||
| DISH | No DISH | DISH | No DISH | |||
| Base model1 | 0.72 (0.18, 1.25) | 1.06 (0.84, 1.28) | 0.25 | 1.34 (0.79, 1.89) | 1.71 (1.51, 1.91) | 0.22 |
| Base + total hip BMD | 0.77 (0.23, 1.31) | 1.05 (0.83, 1.27) | 0.36 | 1.32 (0.77, 1.87) | 1.71 (1.51, 1.91) | 0.19 |
| Base + prevalent and incident vertebral fracture | 0.73 (0.19, 1.27) | 1.05 (0.83, 1.27) | 0.28 | 1.33 (0.78, 1.88) | 1.71 (1.51,1.91) | 0.21 |
| Full multivariate models (MV)2 | 0.73 (0.19, 1.27) | 1.05 (0.83, 1.27) | 0.28 | 1.34 (0.79, 1.89) | 1.72 (1.51, 1.92) | 0.22 |
Base model adjusted for age, race (in MrOS only), clinic site and BMI
MV model is adjusted for age, race (in MrOS only), clinic site, BMI, total hip BMD (calcaneal BMD in SOF), prevalent and incident vertebral fractures and self-reported diabetes.
One woman had Cobb angle measured but no clinic visit. Annualized percent change was calculated using follow up time from enrollment to the midpoint of the overall year 3 visit.
Long-term associations
There were 961 women in SOF who returned for long-term follow-up 15 years after enrollment with DISH measurements completed. Of these, 111 (12%) had DISH at the time of enrollment. Among women with DISH, the absolute change in Cobb angle over 15 years was significantly lower than in those without DISH, mean change (SD): 5.1 (SD = 6.0) versus 6.9 (SD = 7.6) degrees respectively, p=0.002. Women with DISH had less annualized percent change in Cobb angle, −0.25% (95% CI: −0.48, −0.01), p=0.03, than those without DISH, in models adjusted for age, clinic site and BMI (Table 4). This association of DISH with Cobb angle was slightly attenuated in the fully adjusted model additionally adjusted for calcaneal BMD, prevalent and incident vertebral fractures and self-reported diabetes, p=0.04.
Table 4.
Long-term change in Cobb angle over an average of 15 years in 961 women with DISH and without DISH
| Model | Adjusted means of annualized percent change in Cobb angle (95%CI) | P for trend | |
|---|---|---|---|
|
| |||
| DISH | No DISH | ||
| Base model1 | 0.82 (0.59, 1.05) | 1.08 (1.0, 1.17) | 0.03 |
| Base + total hip BMD | 0.83 (0.6, 1.05) | 1.08 (1.0, 1.16) | 0.04 |
| Base +prevalent and incident vertebral fracture | 0.83 (0.61, 1.05) | 1.08 (1.0, 1.16) | 0.04 |
| Full multivariate model (MV)2 | 0.83 (0.6, 1.06) | 1.08 (1.0, 1.16) | 0.04 |
Base model adjusted for age, race (in MrOS only), clinic site and BMI
MV model is adjusted for age, race (in MrOS only), clinic site, BMI, total hip BMD (calcaneal prevalent and incident vertebral fractures and self-reported diabetes.
Discussion
We found that both men and women with DISH had significantly greater Cobb angle at baseline than those without DISH, yet the presence of DISH did not significantly affect change in kyphosis over 4–5 years. However, among women who were followed over 15 years, DISH was associated with less progression of kyphosis.
Our cross-sectional results were consistent with previous findings that DISH is associated with greater Cobb angle in older adults.14 It appears that calcification and ossification of the anterior longitudinal ligament restricts the ability to straighten the spine, and limits flexibility in the anterior longitudinal ligament that is necessary for upright posture. Once ossification of the ligament occurs over several segments in DISH, kyphosis becomes exaggerated. In fact, a cadaver study reported that anterior longitudinal ligament transection at T3–T7 resulted in a 16 degree reduction in Cobb angle,26 further evidence of the effect of DISH on thoracic spine kyphosis.
We hypothesized that DISH would accelerate the progression of kyphosis, but we did not observe this in our study. While kyphosis did progress in the short-term in both men and women overall, the differences in absolute and annualized percent change among those with DISH were not significantly different than in those without DISH. Interestingly, DISH in women was associated with less long-term change in Cobb angle over 15 years compared to those without DISH. Among women with DISH, the absolute change in Cobb angle over 15 years was significantly lower than in those without DISH, mean change (SD): 5.1 (SD = 6.0) versus 6.9 (SD = 7.6) degrees respectively. Considering that a previous study in SOF reported a 7-degree progression of Cobb angle over 15 years, an absolute difference of 1.8 degrees represents an important clinical difference. While the difference in annualized percent change in Cobb angle in those with DISH compared to those without DISH was small, −0.25% (95%CI: −0.05, −0.01), it may have a cumulative impact over time.
We did not find evidence for sex differences in the associations between DISH and kyphosis. The tests for heterogeneity among studies were not significant in the cross-sectional and longitudinal analyses. However, the data in men and women were from separate cohorts recruited at separate times and various enrollment centers, and these inconsistencies may have impaired our ability to detect sex differences. Furthermore, we did not have long-term data in men, and were unable to test for sex differences in these associations over the long-term.
This is the first study that has investigated the progression of kyphosis in older men. Kado, et al,10 previously reported short- and long-term progression of kyphosis in the SOF in women, and our study contributes new information about kyphosis progression in men over the short-term. In men, spine radiographs were obtained only at two time points and therefore long-term change in Cobb angle in the MrOS cohort could not be studied.
Based on these findings, we posit that as the anterior longitudinal ligament ossifies in DISH, it limits the ability to stand erect and increases kyphosis; however it slows the long-term progression of kyphosis that normally occurs with aging. Ossification could theoretically extend to involve additional vertebral segments and expand over already ossified segments that may further affect the progression of Cobb angle over time. Further research is needed to determine if there is additional ossification of supporting structures in the spine once DISH has been established, and whether these changes affect kyphosis and its progression over time.
We reported lower prevalence estimates of DISH than has been previously reported in the literature.27,28 We were conservative in describing those cases where DISH was evolving, and this may have affected our results. To determine whether we under-classified DISH, we ran crosstabs for DISH classification using the Resnick criteria in our MrOS sample compared to Diederichs27 and Holton,28 MrOS samples that previously reported higher prevalence of DISH. There was 100% agreement in DISH classification among the 46 participants who were in both our sample and the Diederichs sample. We were unable to calculate agreement with the Holton sample because we had no participants without DISH common to both samples. However, the agreement in DISH classification between the Holton and Diederichs samples was high with kappa agreement (95%CI) = 0.82 (0.74–0.90). Thus, we have confidence that our prevalence estimates are valid.
Individuals of both sexes with DISH had higher BMI and BMD, characteristics that are usually protective against greater degree of kyphosis. Women with DISH had fewer morphometric vertebral fractures, even though DISH has been previously linked to greater prevalence of vertebral fracture.27 It is possible that these women decreased their physical activity due to reduced spinal flexibility from DISH, and limited their exposure to activities that otherwise could have resulted in fractures. In fact, women with DISH in the SOF cohort reported greater limitations in the performance of IADLs (shopping, meals or housework) and walking 2–3 blocks or climbing 10 steps at enrollment. We postulate that the combined effect of DISH and higher Cobb angle at baseline may contribute to the limitations in IADLs, and more physical disability among women. Further research is needed in this area to better understand the causal pathways.
Our findings may have clinical implications when treating excessive kyphosis. Recent studies report that spinal strengthening exercises may effectively reduce kyphosis among individuals with excessive kyphosis, particularly when the spinal extensor muscles are weak.29 It may be possible to reduce kyphosis as long as the spine is flexible, although once ossification is established in DISH; the spine may become fixed and probably will be less responsive to exercise training. However, preventing kyphosis from developing in someone with DISH may be achievable. Moreover, strengthening the spinal extensor muscles may have a modulating effect on the ossification that can develop in DISH and warrants further investigation.
A strength of our study design is the use of data from 2 large longitudinal cohorts of older men and women with lateral spine radiographs at multiple time-points. This allowed us to assess DISH at baseline and the progression of kyphosis over time. However, there were several limitations. First, the covariates of hip BMD were not measured at the same time in both cohorts. We used baseline measurements of BMD that included hip BMD in MrOS and calcaneal BMD in SOF. However, when we performed a sensitivity analysis with hip BMD measured at a subsequent visit in SOF, the results were not appreciably different. Second, we restricted our SOF analysis to those women with Cobb angle measurements at baseline and 3.7 years later. Of these, we have Cobb angle measurements for 961 women who returned 15 years later. We may have underestimated Cobb angle progression over 15 years because those who were too physically impaired to return for follow-up or did not survive may have had greater Cobb angle progression that could have influenced our long-term results. Third, presumably DISH could progress over time; thus progression of DISH in relation to Cobb angle change is a topic that warrants future research. Finally, we do not have measurement of spine muscle strength or quality and consequently do not know if control for these measures would have altered our results. It is possible that spine muscle strength or quality could have metabolic effects on the anterior longitudinal ligament that impact ossification. Further work is needed to investigate how spine muscle strength and quality may be affected in DISH and whether individuals with DISH respond to spine strengthening exercises that target kyphosis.
We observed a phenotype of kyphosis among participants with DISH characterized by higher BMI and higher BMD, and among women only, fewer vertebral fractures. DISH presence at baseline was associated with greater baseline Cobb angle of kyphosis, yet the presence of DISH did not significantly influence change in kyphosis over the short-term in either sex. However, among women followed over 15 years, DISH was associated with less progression of kyphosis. These results suggest DISH may affect the etiology and progression of kyphosis. Additional studies are warranted to understand the functional implications of the associations between DISH and kyphosis.
Significance and Innovations.
Diffuse Idiopathic Skeletal Hyperostosis (DISH) is associated with greater Cobb angle of kyphosis cross-sectionally in older persons.
DISH did not affect change in kyphosis over 4–5 years in older men and women.
DISH was associated with less progression of kyphosis among women who were followed over 15 years.
Additional studies to understand functional implications of DISH/kyphosis associations are warranted.
Acknowledgments
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute on Aging (NIA), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Center for Advancing Translational Sciences (NCATS), and NIH Roadmap for Medical Research under the following grant numbers: U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, U01 AR066160, R01 AG024246, AR 060828 and UL1 TR000128. The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: R01 AG005407, R01 AR35582, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574, and R01 AG027576. NIAMS provides support under grant numbers R01 AR06828, R01 AR35582, R01 AR35583, R01 AR35584, K24 AR048841, R01 AR052000, P50 AR063043, P50 AR060752 and P60 AR05473101. Other grants supporting this research were P50 AR063043 and RO1 AG041921.
References
- 1.Mata S, Fortin PR, Fitzcharles MA, et al. A controlled study of diffuse idiopathic skeletal hyperostosis. Clinical features and functional status. Medicine (Baltimore) 1997;76(2):104–117. doi: 10.1097/00005792-199703000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Huang MHKW, Cummings SR, Kado DM. Hyperkyphosis and decline in functional status in older community dwelling women: The Study of Osteoporotic Fractures. Paper presented at: ASBMR; 2010. [Google Scholar]
- 3.Katzman W, Huang M-H, Lane N, Ensrud K, Kado D. Kyphosis and decline in physical function over 15years in older community-dwelling women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2013;68:976–983. doi: 10.1093/gerona/glt009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katzman WB, Vittinghoff E, Ensrud K, Black D, Kado D. Increasing Kyphosis Predicts Worsening Mobility Among Older Community-Dwelling Women: a Prospective Cohort Study. J Amer Geriatr Soc. 2011;59(1):96–100. doi: 10.1111/j.1532-5415.2010.03214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katzman WB, Harrison SL, Fink HA, et al. Physical Function in Older Men With Hyperkyphosis. J Gerontol A Biol Sci Med Sci. 2014 doi: 10.1093/gerona/glu213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mader R, Verlaan JJ, Buskila D. Diffuse idiopathic skeletal hyperostosis: clinical features and pathogenic mechanisms. Nat Rev Rheumatol. 2013;9(12):741–750. doi: 10.1038/nrrheum.2013.165. [DOI] [PubMed] [Google Scholar]
- 7.Ensrud KE, Black DM, Harris F, Ettinger B, Cummings SR. Correlates of kyphosis in older women. The Fracture Intervention Trial Research Group. J Am Geriatr Soc. 1997;45(6):682–687. doi: 10.1111/j.1532-5415.1997.tb01470.x. [DOI] [PubMed] [Google Scholar]
- 8.Hinman MR. Comparison of thoracic kyphosis and postural stiffness in younger and older women. Spine J. 2004;4(4):413–417. doi: 10.1016/j.spinee.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Katzman W, Cawthon P, Hicks GE, et al. Association of Spinal Muscle Composition and Prevalence of Hyperkyphosis in Healthy Community-Dwelling Older Men and Women. J Gerontol A Biol Sci Med Sci. 2011 doi: 10.1093/gerona/glr160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kado DM, Huang MH, Karlamangla AS, et al. Factors associated with kyphosis progression in older women: 15 years' experience in the study of osteoporotic fractures. J Bone Miner Res. 2013;28(1):179–187. doi: 10.1002/jbmr.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schneider DL, von Muhlen D, Barrett-Connor E, Sartoris DJ. Kyphosis does not equal vertebral fractures: the Rancho Bernardo study. J Rheumatol. 2004;31(4):747–752. [PubMed] [Google Scholar]
- 12.Sinaki M, Itoi E, Rogers JW, Bergstralh EJ, Wahner HW. Correlation of back extensor strength with thoracic kyphosis and lumbar lordosis in estrogen-deficient women. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists. 1996;75(5):370–374. doi: 10.1097/00002060-199609000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Kado DM, Miller-Martinez D, Lui LY, et al. Hyperkyphosis, Kyphosis Progression, and Risk of Non-Spine Fractures in Older Community Dwelling Women: The Study of Osteoporotic Fractures (SOF) J Bone Miner Res. 2014 doi: 10.1002/jbmr.2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nardo L, Lane NE, Parimi N, et al. Diffuse Idiopathic Skeletal Hyperostosis Association With Thoracic Spine Kyphosis: A Cross-sectional Study for the Health Aging and Body Composition Study. Spine (Phila Pa 1976) 2014;39(24):E1418–1424. doi: 10.1097/BRS.0000000000000615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study--a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26(5):569–585. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 16.Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS) Contemp Clin Trials. 2005;26(5):557–568. doi: 10.1016/j.cct.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 17.Cummings SR, Black DM, Nevitt MC, et al. Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. JAMA. 1990;263(5):665–668. [PubMed] [Google Scholar]
- 18.Resnick D, Curd J, Shapiro RF, Wiesner KB. Radiographic abnormalities of rheumatoid arthritis in patients with diffuse idiopathic skeletal hyperostosis. Arthritis and rheumatism. 1978;21(1):1–5. doi: 10.1002/art.1780210101. [DOI] [PubMed] [Google Scholar]
- 19.Kado DM, Christianson RN, Palermo L, Smith-Bindman R, Cummings SR, Greendale G. Comparing a supine radiographic versus standing clinical measurement of kyphosis in older women: the fracture intervention trial. Spine. 2006;31(4):463–467. doi: 10.1097/01.brs.0000200131.01313.a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lundon KM, Li AM, Bibershtein S. Interrater and intrarater reliability in the measurement of kyphosis in postmenopausal women with osteoporosis. Spine. 1998;23(18):1978–1985. doi: 10.1097/00007632-199809150-00013. [DOI] [PubMed] [Google Scholar]
- 21.Cawthon PM, Haslam J, Fullman R, et al. Response to BONE-D-14–00884. Bone. 2015;75:246. doi: 10.1016/j.bone.2014.11.020. [DOI] [PubMed] [Google Scholar]
- 22.Black DM, Cummings SR, Stone K, Hudes E, Palermo L, Steiger P. A new approach to defining normal vertebral dimensions. J Bone Miner Res. 1991;6(8):883–892. doi: 10.1002/jbmr.5650060814. [DOI] [PubMed] [Google Scholar]
- 23.Black DM, Arden NK, Palermo L, Pearson J, Cummings SR. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999;14(5):821–828. doi: 10.1359/jbmr.1999.14.5.821. [DOI] [PubMed] [Google Scholar]
- 24.Cummings SR, Black DM, Nevitt MC, et al. Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group. Lancet. 1993;341(8837):72–75. doi: 10.1016/0140-6736(93)92555-8. [DOI] [PubMed] [Google Scholar]
- 25.Glymour MM, Weuve J, Berkman LF, Kawachi I, Robins JM. When is baseline adjustment useful in analyses of change? An example with education and cognitive change. Am J Epidemiol. 2005;162(3):267–278. doi: 10.1093/aje/kwi187. [DOI] [PubMed] [Google Scholar]
- 26.Birnbaum K, Siebert CH, Hinkelmann J, Prescher A, Niethard FU. Correction of kyphotic deformity before and after transection of the anterior longitudinal ligament--a cadaver study. Arch Orthop Trauma Surg. 2001;121(3):142–147. doi: 10.1007/s004020000193. [DOI] [PubMed] [Google Scholar]
- 27.Diederichs G, Engelken F, Marshall LM, et al. Diffuse idiopathic skeletal hyperostosis (DISH): relation to vertebral fractures and bone density. Osteoporos Int. 2011;22(6):1789–1797. doi: 10.1007/s00198-010-1409-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holton KF, Denard PJ, Yoo JU, et al. Diffuse idiopathic skeletal hyperostosis and its relation to back pain among older men: the MrOS Study. Seminars in arthritis and rheumatism. 2011;41(2):131–138. doi: 10.1016/j.semarthrit.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bansal S, Katzman WB, Giangregorio LM. Exercise for improving age-related hyperkyphotic posture: a systematic review. Arch Phys Med Rehabil. 2014;95(1):129–140. doi: 10.1016/j.apmr.2013.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]