Abstract
Background
We conducted research to determine the effect of the weight on left ventricular (LV) diastolic function in Asians, who are at greater risk of cardiovascular events compared to individuals from Western countries with similar body mass indices (BMIs).
Methods
We studied 543 participants with structurally normal hearts and normal ejection fractions. Participants were classified as normal-weight (BMI < 23.0 kg/m2), overweight (BMI 23.0–27.4 kg/m2), or obese (BMI ≥ 27.5 kg/m2). Peak E velocity, peak A velocity, and E′ velocity were measured and E/E′ was calculated.
Results
Overweight participants had lower E than normal-weight participants (p = 0.001). E′ velocities in overweight and obese participants were less than those in normal weight participants (both p < 0.001). The E/E′ ratio in obese participants was higher compared to the value in normal-weight participants (p < 0.001) and overweight participants (p = 0.025). BMI was associated with E (R = −0.108), A (R = 0.123), E′ (R = −0.229), and E/E′ ratio (R = 0.138) (all p < 0.05). In multivariate analyses, BMI was independently associated with higher A, lower E′, and higher E/E′. The risk of diastolic dysfunction was significantly higher among overweight [adjusted odds ratio: 2.088; 95% confidence interval (CI): 1.348–3.235; p = 0.001] and obese participants (adjusted odds ratio: 5.910; 95% CI: 2.871–12.162; p < 0.001) compared to normal-weight participants.
Conclusion
Obesity and overweight independently predicted diastolic dysfunction. An optimal body weight lower than the universal cut-off is reasonable for preventing LV heart failure in Asians.
Keywords: Body weight, Obese, Diastole, Body mass index, Asian
Introduction
Obesity and overweight are major determinants of left ventricular (LV) diastolic function.1) Several mechanisms may contribute to the pathogenesis of LV dysfunction in obese patients. In the obese, cardiac preload and afterload are increased, leading to elevated levels of peripheral resistance.2),3) Increased proinflammatory cytokines originating from adipose tissue are suggested to be especially important contributors.4) Furthermore, recent experimental investigations have found that lipotoxicity in the heart results in cardiac steatosis and lipoapoptosis. 5),6) In obesity, diastolic function is correlated with fat mass, serum leptin levels, waist-to-hip ratio, LV mass, and LV end-diastolic volume.7) Increased body mass index (BMI) has also been associated with worse LV diastolic function.1)
However, it is uncertain whether similar relationships exist in Asian populations, because Asians generally have a lower BMI and a higher percentage of body fat at a given BMI compared to individuals from Western countries. Furthermore, Asians have a higher risk of cardiovascular events than individuals in Western populations at a similar BMI. Thus, the World Health Organization (WHO) expert consultation has proposed a new definition for obesity with a focus on the Asia-Pacific region.8) In Asians, the cut-off values for overweight (≥ 23.0 kg/m2) and obesity (≥ 27.5 kg/m2) are lower than those of the standard WHO criteria. The purpose of this study was to identify the effect of weight on the diastolic function of LV in Asians according to BMI criteria for Asian populations.
Methods
Study population
We enrolled 543 participants who visited the health promotion center of a tertiary hospital in Busan, South Korea, for health screening from March to December 2012 and performed transthoracic echocardiography. All patients had a medical record filled, including height, weight, heart rate, and blood pressure. We excluded participants with significant valvular heart disease, confirmed regional wall motion abnormalities, decreased LV ejection fraction (< 50%), atrial fibrillation, or congenital heart disease. Demographic data were obtained through a detailed medical history and physical examination. Hypertension was defined as systolic blood pressure of 140 mm Hg or higher, diastolic blood pressure of 90 mm Hg or higher or past history of hypertension. When there is more than 126 mg/dL of fasting plasma glucose or past history of diabetes mellitus, it was defined as diabetes mellitus. Dyslipidemia was defined as having total serum cholesterol level of 240 mg/dL or higher or past history of dyslipidemia. BMI was calculated as weight (kg) divided by height-squared (m2). The study participants were divided into three weight groups according to the criteria suggested by the WHO expert consultation: normal weight (BMI < 23.0 kg/m2), overweight (BMI 23.0–27.4 kg/m2), and obese (BMI ≥ 27.5 kg/m2).8) The study conformed to the principles of the Declaration of Helsinki and was approved by our Institutional Review Board. The need to obtain written informed consent was waived by the Institutional Review Board.
Echocardiographic analysis
Transthoracic echocardiography was performed using commercially available systems (iE33, Philips, Andover, MA, USA; Vivid 7, GE, Horten, Norway) by trained sonographers. LV diameter was measured in the parasternal short-axis view as recommended by the American Society of Echocardiography.9) The LV mass was calculated using simple geometric cube formula 10) and indexed by both for body surface area (BSA) and height. The LV ejection fraction was calculated by the biplane modified Simpson's method.
LV diastolic function was evaluated using mitral inflow velocity and mitral annular velocity. Peak E and A velocity of the mitral inflow were measured from an apical 4 chamber view, and then E/A ratio was calculated. The mean value of E′ velocities measured by tissue Doppler imaging from septal and lateral annulus was calculated and E/E′ ratio was used as an indicator of LV filling pressure. Definition of diastolic dysfunction was as follows:
E/A < 0.8: impaired relaxation (grade I)
0.8 ≤ E/A ≤ 1.5, E′ < 8 cm/s, and 9 ≤ mean E/E′ ≤ 12: pseudo-normalized pattern (grade II)
E/A > 2, E′ < 8 cm/s, and mean E/E′ ≥ 13: restrictive patter n (grade III)
Elevated LV filling pressure was defined as when E/E′ ratio exceeded 15.11)
Statistical analysis
Continuous variables and categorical variables were expressed as mean ± SD and proportions, respectively. One-way analysis and Bonferroni correction were used to assess differences between groups and analyze post hoc multiple comparisons. Fisher's exact test was used to assess the difference of categorical variables. Independent association between BMI and parameters of diastolic function was evaluated with multiple linear regression. We used multiple logistic model to assess the risk of the LV diastolic dysfunction related to the indicator of body size. SPSS software version 17.0 (SPSS Inc., Chicago, IL, USA) was used and two tailed p < 0.05 was considered as statistically significant.
Results
Study population and LV mass
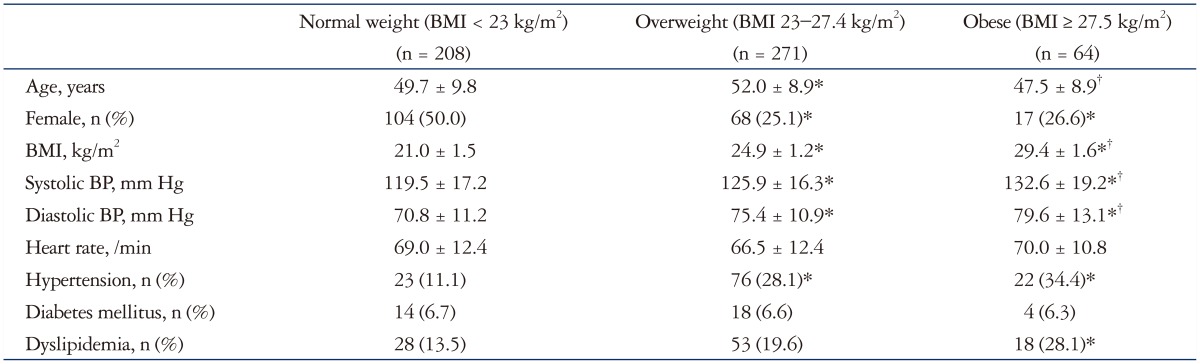
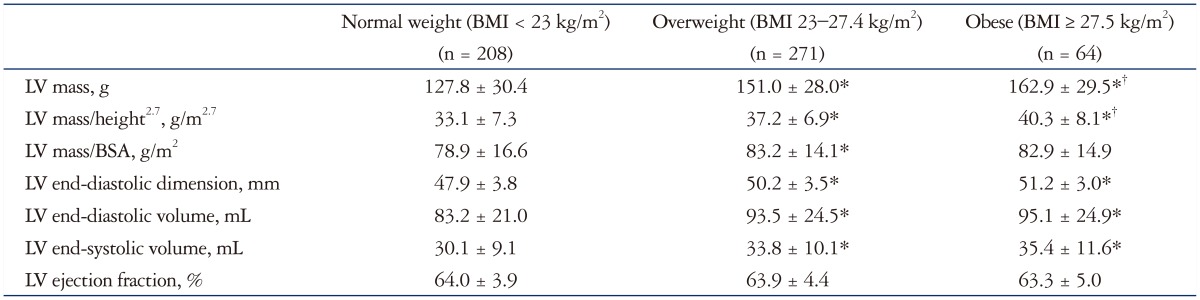
The normal weight, overweight, and obese groups consisted of 208, 271, and 64 participants, respectively. The clinical characteristics and echocardiographic features of the three groups are shown in Tables 1 and 2. Overweight participants were older than normal weight and obese participants. The proportion of women was lower and the proportion of hypertension was higher in the overweight and obese groups. The proportion of patients with dyslipidemia was higher in the obese group than in the normal weight group and overweight group. Obese and overweight participants had higher height-indexed LV mass and BSA-indexed LV mass.
Table 1. Clinical characteristics of populations.
*p < 0.05 versus normal weight, †p < 0.05 versus overweight. BMI: body mass index, BP: blood pressure
Table 2. LV geometry and systolic function assessed by echocardiography.
*p < 0.05 versus normal weight, †p < 0.05 versus overweight. BMI: body mass index, LV: left ventricle, BSA: body surface area
Age and higher BMI were moderately associated with higher height-indexed LV mass (R = 0.355, p < 0.001 and R = 0.371, p < 0.001, respectively). The multivariate analysis indicated that a higher BMI may independently predict increased height-indexed LV mass (β = 0.375, p < 0.001). Age (β = 0.343, p < 0.001) and heart rate (β = -0.180, p < 0.001) were also independent predictors. Hypertension and diabetes were not predictors of increased LV mass in multivariate analysis. Similar relationship were shown between BMI and BSA-indexed LV mass (β = 0.151, p < 0.001).
BMI and diastolic function parameters
Higher BMI was associated with higher peak A wave velocity (R = 0.123; p = 0.004), higher E/E′ ratio (R = 0.138; p = 0.001), lower peak E wave velocity (R = -0.108; p = 0.012), and lower E′ velocity (R = -0.229; p < 0.001).
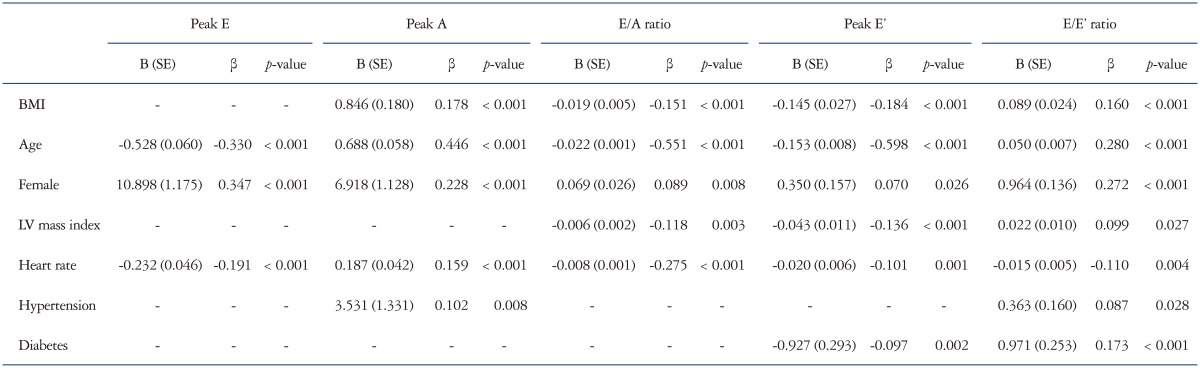
Table 3 shows the correlations of BMI and other clinical variables with parameters of LV diastolic function in multivariate analysis. BMI had positive association with peak A velocity (R2 = 0.032; p < 0.001) and E/E′ ratio (R2 = 0.026; p < 0.001). In contrast, BMI was negatively associated with E/A ratio (R2 = 0.023; p < 0.001) and E′ velocity (R2 = 0.034; p < 0.001). BMI was not correlated with E wave velocity after multivariate analysis.
Table 3. Multivariate analysis for correlation of BMI and other clinical variables with parameters of LV diastolic function.
BMI: body mass index, LV: left ventricle, E: early transmitral velocity, A: late transmitral velocity, E′: early diastolic mitral annulus velocity
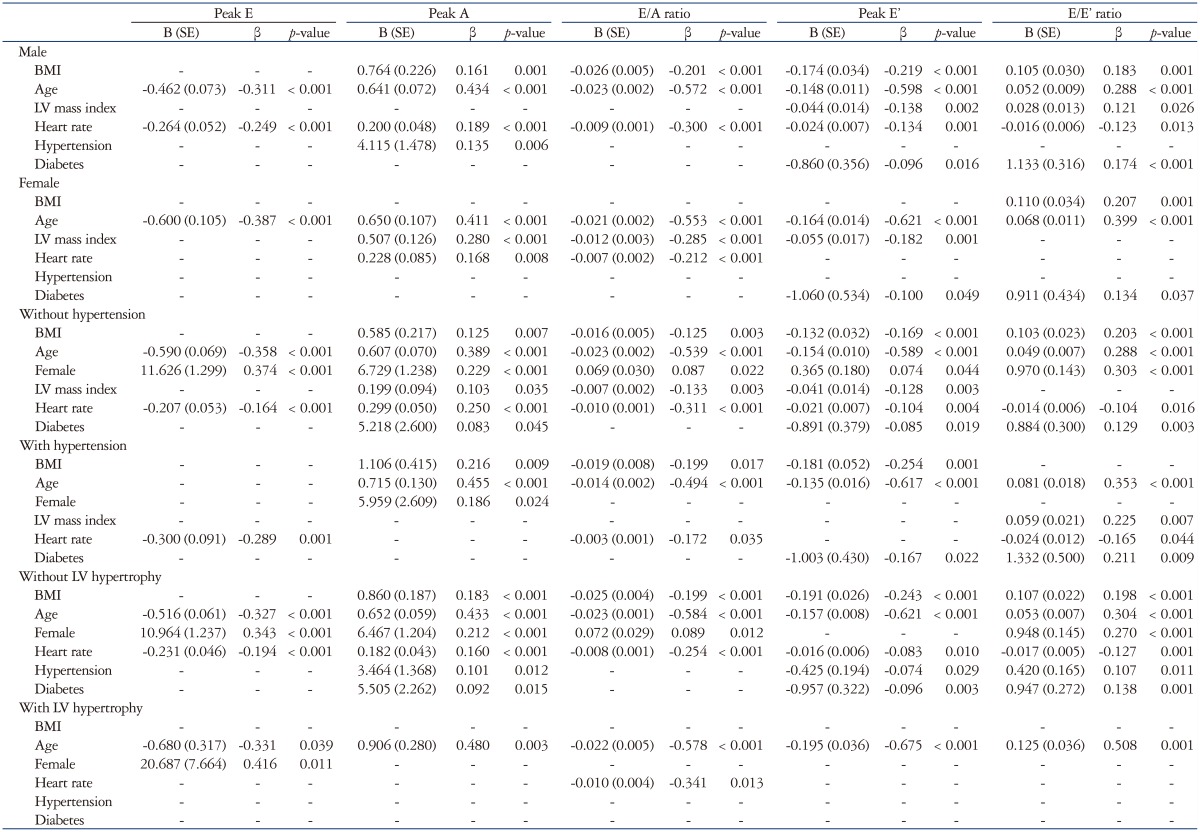
Age, gender, and heart rate were independently associated with all LV diastolic parameters (E, A, E/A ratio, E′ and E/E′ ratio). There were significant correlations between higher LV mass index and lower E/A ratio, lower E′ velocity, and higher E/E′ ratio. After dividing the study group according to gender, the results were similar for just men and the entire population (Table 4). However, in women, BMI was associated with E/E′ ratio only.
Table 4. Multivariate analysis for association between BMI and parameters of LV diastolic function in subgroups with and without risk factors.
BMI: body mass index, LV: left ventricle, E: early transmitral velocity, A: late transmitral velocity, E′: early diastolic mitral annulus velocity
In subgroup analysis of participants without hypertension (n = 422), BMI was still associated with peak A, E/A ratio, E′ velocity, and E/E′ ratio (Table 4). However, the correlation between BMI and E/E′ ratio was not significant in this subgroup. In the subgroup with LV hypertrophy, BMI was not correlated with any parameters of LV diastolic function. There were significant corrections between BMI and the parameters of LV diastolic function in the non-LV hypertrophy subgroup (Table 4).
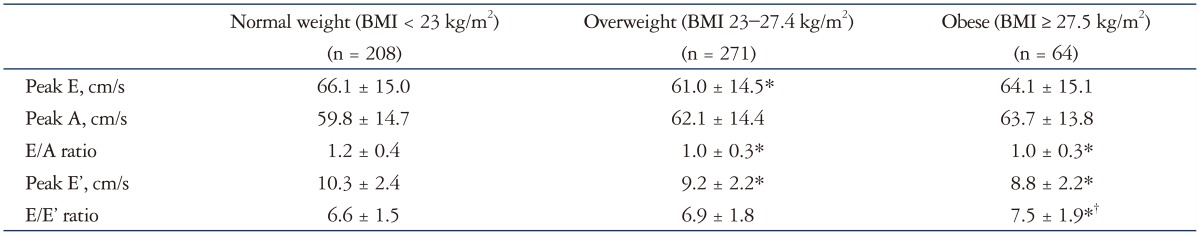
LV diastolic function in abnormal body weight
E velocity was significantly lower in overweight participants than in normal-weight participants (p = 0.001). Peak A velocity was not different between the three groups. The E/A ratio was significantly lower in the overweight and obese groups compared to the normal-weight group (p < 0.001 and p = 0.026, respectively). E′ wave was significantly lower in the overweight and obese groups than in the normal-weight group (both p < 0.001). The E/E′ ratio was significantly higher in obese participants only compared with normal-weight participants (p = 0.001) (Table 5).
Table 5. Comparisons of diastolic parameters between three groups.
*p < 0.05 versus normal weight, †p < 0.05 versus overweight. BMI: body mass index, E: early transmitral velocity, A: late transmitral velocity, E′: early diastolic mitral annulus velocity
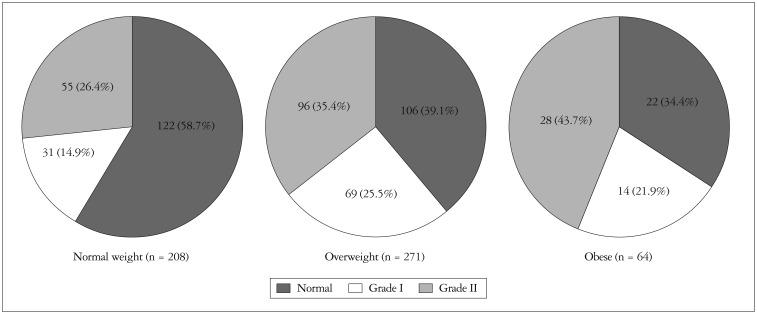
Among all participants, the prevalence of LV diastolic dysfunction was 54% (n = 293). Diastolic dysfunction was more common in the overweight (60.9%) and obese (65.6%) groups than in the normal-weight group (41.3%) (p < 0.001). The prevalence of pseudo-normalized diastolic pattern was 26.4, 35.4, and 43.7% in normal weight, overweight and obese, respectively (p = 0.017) (Fig. 1).
Fig. 1. Proportion of diastolic dysfunction in each weight group.
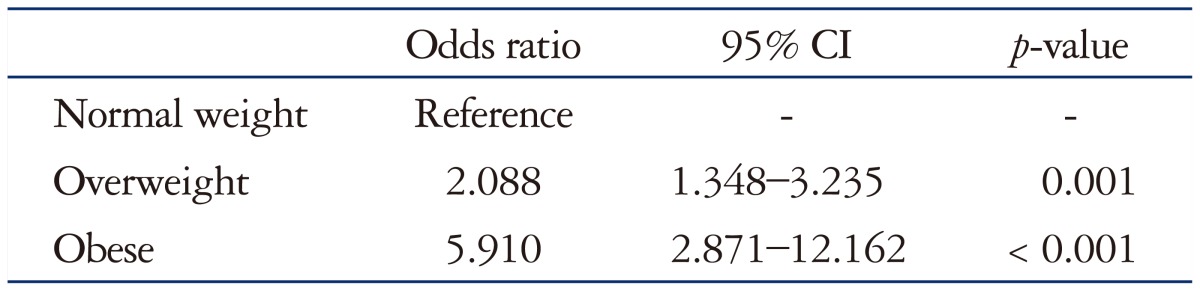
Risk of LV diastolic dysfunction was assessed using a multivariate logistic model (Table 6). Overweight [odds ratio (OR): 2.088; 95% confidence interval (CI): 1.348–3.235; p = 0.001] and obese (OR: 5.910; 95% CI: 2.871–12.162; p < 0.001) were independent risk factor of diastolic dysfunction. Numerical BMI was also an independent risk factor of diastolic dysfunction (adjusted: 1.163; 95% CI: 1.077–1.257; p < 0.001).
Table 6. Risk of diastolic dysfunction associated with overweight and obesity (multivariate analysis).
CI: confidence interval
Discussion
We analyzed the relationships between LV diastolic function and overweight and obesity as classified by the WHO expert consultation definition for Asians. Our data suggest that BMI has independent correlation with parameters of LV diastolic function and overweight and obese status according to the WHO expert consultation criteria are independent risk factors for LV diastolic dysfunction in Asians. In our study population, the overweight and obese groups had more impaired diastolic function compared with the normal-weight group, and both of these weight groups were independent predictors of LV diastolic dysfunction. It is notable that there was no significant difference in diastolic parameters between obese and overweight participants. Although gender, hypertension, diabetes, and LV hypertrophy also negatively affect LV diastolic function, the relationship between BMI and LV diastolic function maintained after adjusting for these variables. In subgroup analysis of male participants, participants without LV hypertrophy, and participants without hypertension, a significantly negative association between BMI and LV diastolic function was also detected. We found no such significant relationships in women or participants with LV hypertrophy. However, the numbers of women and participants with LV hypertrophy included in the study were small, so the results of the subgroup analysis of these participants should be considered with caution.
Many studies have demonstrated that overweight and obesity are important risk factors for the development of heart failure.1),12),13),14) Most studies use the most popular WHO BMI criteria of ≥ 25 kg/m2 for overweight and ≥ 30 kg/m2 for obesity, 15) which were both calculated based on Western populations. However, Asian populations have a lower mean BMI than Western populations, in addition to a higher percentage of body fat and a greater risk for cardiovascular disease at a given BMI.16),17) Many experts agree that population-spefv cific cut-off points for BMI are necessary. The WHO expert consultation group observed that the risk of obesity-related diseases among Asians increases from a BMI of 23 kg/m2, and suggested appropriate cut-off values for overweight (≥ 23 kg/m2) and obesity (≥ 27.5 kg/m2) in Asians that are lower than the standard WHO criteria.8) Although these criteria in Asian populations need further validation, we observed that Asians had impaired diastolic function with a BMI ≥ 23 kg/m2. There are several BMI criteria for Asians, but the consensus is that the definition of overweight is a BMI ≥ 23 kg/m2. The definition of obesity varies, but all criteria for Asians are lower than the universal WHO criteria.8),18) As mentioned above, Asians have a higher prevalence of heart failure and cardiovascular disease at a particular BMI than Westerners, and the present results suggest one mechanism to explain this important difference.
Early diastolic annular velocity is essential for the assessment of diastolic function. E′ is not affected by loading state or by physiologic changes like respiration.19) We adopted the values for diastolic dysfunction recommended by the American Society of Echocardiography11) and by accounting for the age of the studied population. Diastolic dysfunction was considered when septal E′ was < 8 cm/s.
Previous studies reported that BMI is correlated with impairment of LV diastolic function,1),12) which is in agreement with our findings. In the same Asia-Pacific region (Japan), Dote et al.20) showed that overweight was not an independent risk factor for LV diastolic dysfunction. However, they used the universal WHO criteria for overweight and a different definition of diastolic function. They emphasized the use of the deceleration time of early mitral flow and parameters of LV filling pressure. They also overlooked the pattern of annular velocity of the mitral valve and limited the role of E′ as the parameter of LV filling pressure. We hypothesize that the discrepancies between our results and those of previous studies may be related to the intrinsic differences in racial characteristics, the definitions of overweight and obesity, and the differences in the definitions of LV diastolic function used.
Our study had several limitations. First, obesity was determined using only BMI, and no measurements of body fat distribution were performed. A stronger correlation might have been found between abdominal obesity and echocardiographic alterations. Second, this study demonstrated impairment of LV diastolic function echocardiographically, without investigating long-term outcomes such as heart failure or major adverse cardiac events. Further studies addressing these issues are needed. Third, this study was monocentric, the studied population size was limited, and only Korean participants were included. Therefore, our results may not be generalizable to other ethnic groups in other Asian regions.
In conclusion, the results of the present study revealed that LV diastolic dysfunction is present in overweight subjects, and that lower BMI categories are appropriate for evaluating relationships among overweight, obese, and LV diastolic dysfunction in Asian populations. On this basis, lower BMI cut-off points to define overweight and obesity are warranted for daily practice and clinical trials in Asian populations. If we expand our goal to the promotion of policies for reducing the burdens of increasing obesity in Asia, a lower cut-off point may be useful for stimulating changes in prevention and intervention strategies.
Acknowledgements
This work was supported by a 2011 Inje University research grant.
References
- 1.Russo C, Jin Z, Homma S, Rundek T, Elkind MS, Sacco RL, Di Tullio MR. Effect of obesity and overweight on left ventricular diastolic function: a community-based study in an elderly cohort. J Am Coll Cardiol. 2011;57:1368–1374. doi: 10.1016/j.jacc.2010.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alpert MA. Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci. 2001;321:225–236. doi: 10.1097/00000441-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Kasper EK, Hruban RH, Baughman KL. Cardiomyopathy of obesity: a clinicopathologic evaluation of 43 obese patients with heart failure. Am J Cardiol. 1992;70:921–924. doi: 10.1016/0002-9149(92)90739-l. [DOI] [PubMed] [Google Scholar]
- 4.Lyon CJ, Law RE, Hsueh WA. Minireview: adiposity, inflammation, and atherogenesis. Endocrinology. 2003;144:2195–2200. doi: 10.1210/en.2003-0285. [DOI] [PubMed] [Google Scholar]
- 5.Zhou YT, Grayburn P, Karim A, Shimabukuro M, Higa M, Baetens D, Orci L, Unger RH. Lipotoxic heart disease in obese rats: implications for human obesity. Proc Natl Acad Sci U S A. 2000;97:1784–1789. doi: 10.1073/pnas.97.4.1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chiu HC, Kovacs A, Ford DA, Hsu FF, Garcia R, Herrero P, Saffitz JE, Schaffer JE. A novel mouse model of lipotoxic cardiomyopathy. J Clin Invest. 2001;107:813–822. doi: 10.1172/JCI10947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rider OJ, Francis JM, Ali MK, Holloway C, Pegg T, Robson MD, Tyler D, Byrne J, Clarke K, Neubauer S. Effects of catecholamine stress on diastolic function and myocardial energetics in obesity. Circulation. 2012;125:1511–1519. doi: 10.1161/CIRCULATIONAHA.111.069518. [DOI] [PubMed] [Google Scholar]
- 8.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 9.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ Chamber Quantification Writing Group; American Society of Echocardiography's Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–458. doi: 10.1016/0002-9149(86)90771-x. [DOI] [PubMed] [Google Scholar]
- 11.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–133. doi: 10.1016/j.echo.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 12.Bae HK, Choi HS, Sohn S, Shin HJ, Nam JH, Hong YM. Cardiovascular screening in asymptomatic adolescents with metabolic syndrome. J Cardiovasc Ultrasound. 2015;23:10–19. doi: 10.4250/jcu.2015.23.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loehr LR, Rosamond WD, Poole C, McNeill AM, Chang PP, Folsom AR, Chambless LE, Heiss G. Association of multiple anthropometrics of overweight and obesity with incident heart failure: the Atherosclerosis Risk in Communities study. Circ Heart Fail. 2009;2:18–24. doi: 10.1161/CIRCHEARTFAILURE.108.813782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ávila-Vanzzini N, Machain Leyva CZ, Rodríguez Castellanos LE, Arias Godínez JA, Ruiz Esparza ME, Herrera Bello H. Excessive weight and obesity are associated to intra-ventricular asynchrony: pilot study. J Cardiovasc Ultrasound. 2015;23:86–90. doi: 10.4250/jcu.2015.23.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kossaify A, Nicolas N. Impact of overweight and obesity on left ventricular diastolic function and value of tissue Doppler echocardiography. Clin Med Insights Cardiol. 2013;7:43–50. doi: 10.4137/CMC.S11156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3:141–146. doi: 10.1046/j.1467-789x.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- 17.Chang CJ, Wu CH, Chang CS, Yao WJ, Yang YC, Wu JS, Lu FH. Low body mass index but high percent body fat in Taiwanese subjects: implications of obesity cutoffs. Int J Obes Relat Metab Disord. 2003;27:253–259. doi: 10.1038/sj.ijo.802197. [DOI] [PubMed] [Google Scholar]
- 18.Oh SW, Shin SA, Yun YH, Yoo T, Huh BY. Cut-off point of BMI and obesity-related comorbidities and mortality in middle-aged Koreans. Obes Res. 2004;12:2031–2040. doi: 10.1038/oby.2004.254. [DOI] [PubMed] [Google Scholar]
- 19.Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quiñones MA. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30:1527–1533. doi: 10.1016/s0735-1097(97)00344-6. [DOI] [PubMed] [Google Scholar]
- 20.Dote K, Miyasaka Y, Tsujimoto S, Motohiro M, Maeba H, Suwa Y, Iwasaka T. Obesity as an independent risk for left ventricular diastolic dysfunction in 692 Japanese patients. Obes Res Clin Pract. 2012;6:e175–e262. doi: 10.1016/j.orcp.2012.01.001. [DOI] [PubMed] [Google Scholar]