Abstract
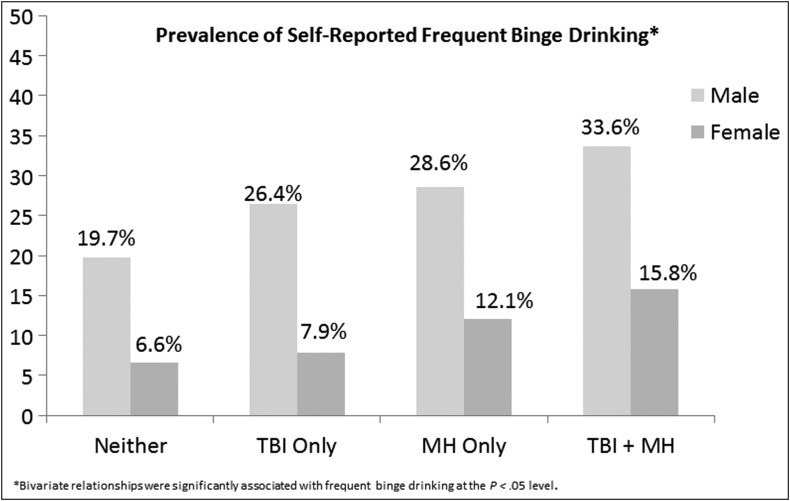
This study examines whether the relationship between traumatic brain injury (TBI) and post-deployment binge drinking is independent of screening positive for mental health problems among male and female service members. Data are from the Substance Use and Psychological Injury Combat Study of Army members returning from deployment to Afghanistan or Iraq in fiscal years 2008–2011. The sample consists of 240,694 male and 26,406 female active duty members who completed initial and follow-up questionnaires. The initial questionnaire, completed at the end of deployment, included screens for TBI and mental health problems (post-traumatic stress disorder, depression, harmful thoughts). The dependent variable, frequent binge drinking (six or more drinks on one occasion, at least monthly), was assessed on the follow-up questionnaire on average 3–9 months post-deployment. More than 21% of males and 7% of females reported frequent binge drinking. Male members were more likely to screen positive for TBI, compared with females (7.5% vs. 4.4%). Females with both TBI and mental health positive screens had more than double the risk of frequent binge drinking, compared with those without either problem (15.8% vs. 6.6%), and males with both problems had almost double the risk, compared with males with neither problem (33.6% vs. 19.7%). In multivariable logistic regression models, having a TBI and a comorbid positive mental health screen was associated with increased odds of frequent binge drinking among both males and females (adjusted odds ratio [AOR] = 1.59, CI: 1.50-1.69, and AOR = 2.11, CI: 1.57-2.83, respectively), compared with those with neither condition. More research is needed on the interaction of gender and binge drinking, especially when TBI and mental health problems co-exist.
Keywords: : binge drinking, gender, post-deployment, traumatic brain injury
Introduction
Binge drinking, frequently defined as consuming five or more (5+) drinks on one occasion for males, and four or more (4+) drinks for females, has been common historically among military service members.1–4 With more than a decade of deployments supporting Operation Enduring Freedom in Afghanistan and Operation Iraqi Freedom (OEF/OIF), studies have found that those who have been on a combat deployment or have experienced combat are at increased risk for binge drinking and problem alcohol use.5–7 A study of more than 300,000 Army active duty members returning from OEF/OIF deployments in fiscal years (FYs) 2008–2011 found that 38% reported binge drinking, using a higher and non–gender specific definition of six or more (6+) drinks on one occasion for males and females, when completing a U.S. Department of Defense (DoD) questionnaire at the end of their deployment.7 Prevalence of binge drinking is higher when assessed on DoD anonymous surveys, with 54% of active duty members returning from a combat deployment in 2007–2008 reporting binge drinking.8 Binge drinking is associated with negative drinking-related consequences among military members, including drinking-related injuries and job-performance problems.9–12 Female members represent approximately 10% of OEF/OIF deployments.13 DoD population-based surveys show that females binge drink less frequently than males, yet these studies have not analyzed differences in binge drinking by gender with a post-deployment cohort.3,14
Understanding deployment-related risk factors for post-deployment binge drinking is important for targeted prevention strategies. Studies suggest that experiencing a traumatic brain injury (TBI) while deployed increases the risk for post-deployment frequent (at least monthly) binge drinking,8,15 alcohol misuse,16 and negative drinking-related consequences.9 It is well-established that a TBI of sufficient force will damage the frontal lobes, ventral medial prefrontal cortex, and orbital frontal cortex regardless of the location of head impact.17 Neural networks connecting these areas of the prefrontal cortex to the basal ganglia and midbrain constitute the so-called “reward circuit,” which is implicated in substance abuse.18,19 In particular, damage to the orbital frontal cortex has been associated with reduced ability to inhibit impulsive behavior,20 which may be a factor when self-regulating drinking levels. Further, there may be an interaction between neuroinflammation caused by a TBI and increased post-injury drinking.21
Both psychosocial and biological differences by gender have been observed after TBI, including differences in executive function.22–26 Even though females have been excluded from direct ground combat until recent DoD policy changes,27 they have not been shielded from combat exposures while deployed.28,29 We do not know what portion of Army females experienced a TBI during an OEF/OIF deployment and whether TBI is a risk factor for post-deployment binge drinking among females.
Further complicating the relationship between TBI and post-deployment binge drinking are common comorbidities, including post-traumatic stress disorder (PTSD), depression, and harmful thoughts.8,30–35 In particular, TBI and PTSD are commonly comorbid within this population,32,35–37 and PTSD is a known risk factor for unhealthy drinking.33,38,39 One study of active duty members examined whether experiencing a TBI on a deployment ending in 2007–2008 was associated with post-deployment binge drinking, independent of PTSD, and found that both TBI and PTSD had direct effects on binge drinking.8 Yet almost 70% of the total effect of TBI on binge drinking was from the direct effect, with only 30% represented through the indirect effect through PTSD. It is unknown if these relationships were impacted by gender.
The purpose of this study was to first establish the prevalence of TBI positive screens and post-deployment binge drinking among Army female service members, compared with male members, returning from OEF/OIF deployments in FYs 2008–2011. Second, we examined if the relationship between TBI and post-deployment binge drinking differed between male and female members. Third, we investigated if the relationship between TBI and post-deployment binge drinking was independent of screening positive for mental health problems, by gender. Research that informs our understanding of risk factors for post-deployment binge drinking by gender will provide the DoD with gender-specific information to improve prevention efforts and responsiveness to unhealthy post-deployment drinking.
Methods
Study design and data sources
This study used data from the Substance Use and Psychological Injury Combat Study, a longitudinal, observational study of post-deployment substance use and mental health problems and outcomes. Rationale, methods, and a description of the main cohort are described elsewhere.13 We analyze data from a subsample of Army active duty members who completed both an initial and follow-up questionnaire as part of the DoD's post-deployment heath surveillance program.40 Initial questionnaires, known as the Post-Deployment Health Assessment (PDHA; Form DD 2796), were completed within 60 days before or after the return from deployment, and follow-up questionnaires, referred to as the Post-Deployment Health Re-Assessment (Form DD 2900), were completed on average within 3–9 months post-deployment.41 Questionnaires include a section where a clinical provider reviews items, asks additional questions, and can refer members for care. Members’ self-reported post-deployment behavioral health problems and deployment exposures, including TBI, were drawn from the initial questionnaire, and the dependent variable, frequent binge drinking, was assessed on the follow-up questionnaire. This study used the updated 2008 versions of the questionnaires. Additional data sources included deployment information from the Contingency Tracking System, DoD occupation specialty from the Defense Manpower Data Center, and demographic and military characteristics from the Defense Enrollment Eligibility Reporting System.13
From the main cohort of Army active duty members with an index (first) deployment ending in FY 2008–2011 (N = 434,986), we selected a subsample who had an initial questionnaire matched to a deployment (n = 333,803) using an algorithm described elsewhere.13 From this sample, we selected members who completed the follow-up questionnaire, resulting in analysis samples of 240,694 males and 26,406 females. We included follow-up questionnaires that were completed within 30–300 days of the end date of deployment: more than 90% occurred within 3–9 months post-deployment (data not shown).
Measures
Binge drinking was identified on the follow-up questionnaire when members were asked to report, “how often do you have 6+ drinks on one occasion.” This definition is non-gender specific and less conservative than the definition endorsed by the National Institute on Alcohol Abuse and Alcoholism, which defines binge drinking as five or more drinks for males and four or more drinks for females.42 The dependent variable, frequent binge drinking, captured members who reported binge drinking at least monthly. We constructed a measure of any binge drinking, which included members with any report of binge drinking.
A TBI positive screen was based on self-reported items of at least one injury event during the index deployment (blast or explosion; vehicular accident/crash; fragment wound or bullet wound above the shoulders; fall; other event), accompanied by either an alteration or loss of consciousness (lost consciousness or got knocked out; felt dazed, confused or saw stars; didn't remember the event). This is consistent with the American Congress of Rehabilitation Medicine's definition.43
Mental health problems
We constructed the variable any mental health positive screen as an indicator of a positive screen for PTSD, depression, and/or harmful thoughts. A positive screen for PTSD was assessed with the Primary Care-PTSD (PC-PTSD), a four-item screen that measures symptoms of re-experiencing, avoidance, hyperarousal, and numbing in the past 30 days. Endorsement of three or more symptoms was considered positive.44–46 The two-item Patient Health Questionnaire (PHQ-2) screened for depression by assessing how emotional problems impacted members’ functioning in the past month; a score of 3 or more was considered positive.47 A positive screen for harmful thoughts was met when members reported “yes” or “unsure” to either of two items that providers directly administered: if they had been bothered by thoughts of being “better off dead or hurting yourself in some way” or “thoughts or concerns that you might hurt or lose control with someone” in the past month.
For analysis, we combined the TBI and any mental health problems variables to make four mutually exclusive and exhaustive categories: 1) neither, 2) TBI positive screen only, 3) mental health positive screen only (a positive screen to PTSD, depression and/or harmful thoughts), and 4) both TBI and mental health positive screens.
Demographic variables, measured at the beginning of the index deployment, consisted of: rank (junior enlisted, senior enlisted, officer), gender, race/ethnicity (White, Black, Asian/Pacific Islander, American Indian/Alaskan Native, Hispanic, and other/unknown), marital status (married, divorced, other, never married), if members had child dependent(s) eligible for Military Health System benefits (a proxy for being a parent), and DoD occupational specialties (combat specialist; healthcare; functional support, services and supply; mechanical, electrical, engineering; other). Deployment events were based on self-report about the index deployment and included being wounded, injured, assaulted, or hurt; and combat exposure score (0–3; encountered dead bodies or saw people/killed wounded, engaged in direct combat/discharged a weapon, felt in great danger of being killed). We included length of index deployment (1–11, 12, > 12 months), any prior deployment to the index deployment, and fiscal year end date of the index deployment.
Statistical analysis
Chi-square tests of independence were used to test for associations between gender and member characteristics. Multivariable logistic regression was used to model the association between TBI, mental health, and binge drinking with adjustment for demographic and deployment characteristics, and the number of months between completion of the initial and follow-up questionnaires. Regression diagnostics including multi-collinearity diagnostics were performed. We report adjusted odds ratios (AORs) and 95% confidence intervals (CIs). The p values were two-sided.
Analyses were stratified by gender because the distributions of demographic and deployment characteristics varied by gender in this sample, and because we hypothesized that the factors associated with binge drinking may differ by gender. Finally, the threshold used to define binge drinking on the follow-up questionnaire (6+) was not gender-specific; thus, findings for males and females may not be exactly comparable. We conducted a sensitivity analysis in the female sample using the any binge drinking measure as the dependent variable to determine whether the association between TBI and binge drinking depended on how binge drinking was defined.
All calculations were performed using SAS/Base and SAS/STAT software (version 9.2; SAS Institute Inc., Cary, NC). Brandeis University's Committee for Protection of Human Subjects and the Human Research Protection Program at the Office of the Assistant Secretary of Defense for Health Affairs/Defense Health Agency conducted the human subjects review. The Defense Health Agency's Privacy and Civil Liberties Office executed the data use agreements.
Results
To assess for possible selection bias, we compared service members who completed the initial questionnaire to those who completed both questionnaires, by gender (Supplementary Table 1; see online supplementary material at www.liebertpub.com). There were no large differences among members in the analysis sample who completed both questionnaires (n = 276,100) and the larger sample of members that completed the initial questionnaire (n = 333,803) in terms of prevalence of TBI, mental health problems, demographics, or deployment characteristics (Supplementary Table 1). In the analysis sample, respondents were less likely to have an index deployment ending in FY 2011.
In the analysis sample of service members who completed both questionnaires, male and female members differed on many demographic and deployment characteristics (Supplementary Table 1). Compared with females, males were more likely to be White, married, have a child dependent eligible for Military Health System benefits, have an enlisted pay-grade, and have less than a college degree. Males were more likely to have had a deployment prior to the index deployment and higher combat exposure scores. Of note, both males and females had similar reports (almost 17%) of being wounded, injured, assaulted, or hurt. Male members were more likely to screen positive for TBI on their index deployment, compared with females (7.5% vs. 4.4%). Males had similar estimates of PTSD (5.3% vs. 5.7%) and harmful thoughts (1.5% vs. 1.8%) as females, and slightly lower estimates for depression (7.4% vs. 8.9%). The median number of days between the end date of deployment and completion of the follow-up questionnaire did not differ by gender: 129 days for males and 130 days for females (data not shown).
Males were more likely to report binge drinking than females on the follow-up questionnaire (Table 1). More than 52% of males and 26% of females reported any binge drinking, and 21.2% and 7.4%, respectively, reported frequent binge drinking (at least monthly). Figure 1 illustrates the relationship between the key independent variable of positive screens for TBI and/or mental health problems with post-deployment frequent binge drinking. Females with both TBI and mental health positive screens had more than double the risk of frequent binge drinking, compared with those without either problem (15.8% vs. 6.6%), and males with positive screens for both TBI and a mental health problem had almost double the risk, compared with males with neither problem (33.6% vs. 19.7%).
Table 1.
Prevalence of Self-Reported Binge Drinking on the Follow-Up Questionnaire among Male and Female Service Members Returning from OEF/OIF Deployments in FYs 2008–2011a
| Self-reported binge drinking total (% of total) | ||||
|---|---|---|---|---|
| Males | Females | |||
| n = 240,694 | n = 26,406 | |||
| n | % | n | % | |
| Frequency of binge drinkingb,* | ||||
| Not a current drinker | 38,970 | 16.2% | 6,343 | 24.0% |
| Drink, but never ‘binge’ | 75,759 | 31.5% | 13,117 | 49.7% |
| Less than monthly binging | 75,064 | 31.2% | 4,982 | 18.9% |
| Monthly binging | 30,420 | 12.6% | 1,296 | 4.9% |
| Weekly binging | 19,284 | 8.0% | 636 | 2.4% |
| Daily binging | 1,197 | 0.5% | 32 | 0.1% |
| Any occasion of binge drinking* | 125,965 | 52.3% | 6,964 | 26.3% |
| Frequent binge drinking (at least monthly)* | 50,901 | 21.2% | 1,964 | 7.4% |
The follow-up questionnaire was completed 30–300 days after the end of the index deployment.
Binge drinking is defined as drinking six or more drinks on an occasion.
Association between drinking and gender, chi-square test, p < 0.0001.
OEF/OIF, Operation Enduring Freedom in Afghanistan and Operation Iraqi Freedom; FY, fiscal year.
FIG. 1.
Frequent binge drinking among male and female service members on the follow-up questionnaire, by traumatic brain injury (TBI) and mental health positive screens.
Among all members, frequent binge drinking was more prevalent among those younger (ages 17–24), American Indian/Alaskan Native, never married, junior enlisted (E1-E4), and without a college degree (Table 2). Male and female members with a deployment longer than 12 months, or those who were wounded, injured, hurt, or assaulted were more at risk for frequent binge drinking. Males with a combat specialist occupation and females with a mechanical, electrical, or engineering occupation specialty were more likely to be frequent binge drinkers. As combat exposure score increased, the likelihood of frequent binge drinking increased in a dose–response relation for both males and females.
Table 2.
Prevalence of Male and Female Service Member Self-Reported Frequent Binge Drinking on Follow-Up Questionnaire, by Demographics and Deployment Characteristicsa
| Active duty sample (N = 267,100) | ||||
|---|---|---|---|---|
| Males | Females | |||
| n = 240,694, 90.1% | n = 26,406, 9.9% | |||
| Characteristicsb | Size of subgroup | Prevalence in subgroup | Size of subgroup | Prevalence in subgroup |
| Dependent variable | ||||
| Frequent binge drinking, n (%) | 50,901 | 21.2% | 1,964 | 7.4% |
| Demographic | ||||
| Age, n (%) | ||||
| 17–24 | 112,007 | 26.0% | 11,941 | 9.8% |
| 25–29 | 58,444 | 21.2% | 6,575 | 7.4% |
| 30–39 | 56,289 | 14.5% | 6,050 | 4.6% |
| 40+ | 13,954 | 9.3% | 1,840 | 2.0% |
| Race/ethnicity, n (%) | ||||
| White, non-Hispanic | 133,484 | 22.2% | 8,978 | 7.6% |
| Black, non-Hispanic | 37,698 | 16.6% | 9,090 | 6.7% |
| Asian/Pacific Islander | 37,237 | 21.3% | 3,965 | 8.1% |
| American Indian/Alaskan Native | 2,169 | 24.3% | 395 | 12.2% |
| Hispanic | 26,877 | 22.3% | 3,391 | 7.8% |
| Other/unknown | 3,229 | 15.4% | 587 | 6.6% |
| Marital status, n (%) | ||||
| Never married | 89,016 | 25.8% | 11,106 | 8.8% |
| Married | 141,619 | 18.2% | 11,831 | 6.6% |
| Divorced | 9,400 | 21.0% | 3,248 | 5.7% |
| Other | 659 | 22.6% | 221 | 9.5% |
| Any child dependent eligible for Military Health System benefits, n (%) | ||||
| Has child dependent(s) | 109,172 | 17.2% | 10,098 | 5.8% |
| Does not have child dependent(s) | 131,522 | 24.4% | 16,308 | 8.5% |
| Rank, pay grade, n (%) | ||||
| Junior enlisted (E1-E4) | 135,030 | 24.4% | 14,155 | 9.6% |
| Senior enlisted (E5-E9) | 75,442 | 18.8% | 7,599 | 5.9% |
| Officers | 30,222 | 12.6% | 4,652 | 3.4% |
| Education, n (%) | ||||
| Less than college degree | 207,043 | 22.4% | 20,719 | 8.4% |
| College degree | 30,426 | 12.9% | 5,394 | 3.6% |
| Occupation specialty, n (%) | ||||
| Combat specialist | 83,891 | 23.7% | 969 | 6.2% |
| Healthcare | 13,765 | 16.9% | 4,285 | 6.5% |
| Functional support, service, and supply | 52,230 | 18.6% | 14,130 | 7.5% |
| Mechanical, electrical, engineering | 51,053 | 20.6% | 3,803 | 8.5% |
| Other | 39,076 | 21.5% | 3,165 | 7.4% |
| Deployment | ||||
| Length of index deployment (months), n (%) | ||||
| 1–11 | 82,432 | 18.8% | 9,703 | 6.1% |
| 12 | 81,040 | 21.6% | 8,557 | 7.8% |
| >12 | 77,222 | 23.2% | 8,146 | 8.7% |
| Any prior deployment to index, n (%) | ||||
| Has a prior deployment | 111,343 | 19.9% | 9,447 | 6.9% |
| Does not have a prior deployment | 129,351 | 22.3% | 16,959 | 7.7% |
| Combat Exposure Score, n (%) | ||||
| 0 | 138,088 | 18.9% | 18,813 | 7.0% |
| 1 | 52,436 | 22.1% | 5,612 | 8.0% |
| 2 | 30,498 | 24.8% | 1,786 | 9.8% |
| 3 | 19,672 | 28.7% | 195 | 14.4% |
| Wounded, injured, assaulted or hurt on most recent deployment, n (%) | ||||
| Was wounded, injured, assaulted, or hurt | 40,233 | 23.3% | 4,374 | 9.2% |
| Was not wounded, injured, assaulted, or hurt | 200,461 | 20.7% | 22,032 | 7.1% |
| TBI positive screen, n (%) | ||||
| Screened positive for TBI | 18,088 | 28.7% | 1,152 | 10.5% |
| Did not screen positive for TBI | 222,606 | 20.5% | 25,254 | 7.3% |
The follow-up questionnaire was completed 30–300 days after the end of the index deployment. All other variables were assessed on the initial questionnaire (completed within 60 days of the deployment end date).
All variables shown were significantly associated with frequent binge drinking at the p < .05 level with the exception of Hispanic ethnicity within the female sample.
TBI, traumatic brain injury.
Factors associated with frequent binge drinking among males and females
Table 3 presents the characteristics associated with the odds of post-deployment binge drinking among males and females. In Model 1, males who reported both TBI and mental health positive screens had increased odds of frequent binge drinking, compared with those without either condition, when controlling for demographics and deployment variables (AOR = 1.59, 95%; CI: 1.50-1.69). Similarly, males with a mental health problem only or with a TBI only, had increased odds of frequent binge drinking, compared with those without either condition, even though the AORs were smaller than among those with both TBI and mental health positive screens.
Table 3.
Characteristics Associated with the Odds of Post-Deployment Binge Drinking on the Follow-Up Questionnaire among Male and Female Service Members Returning from OEF/OIF Deployments in FYs 2008–2011a
| Multivariable logistic regression modelb,c | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| Frequent binge drinking among | Frequent binge drinking among | Any binge drinking among | ||||
| males | females | females | ||||
| Characteristics | AOR | CI | AOR | CI | AOR | CI |
| TBI and any mental health problemd | ||||||
| Neither (reference group) | 1.00 | 1.00 | 1.00 | |||
| TBI only | 1.19*** | 1.14, 1.24 | 1.03 | 0.78, 1.35 | 1.19* | 1.01, 1.40 |
| Mental health only | 1.49*** | 1.44, 1.53 | 1.73*** | 1.53, 1.97 | 1.39*** | 1.27, 1.51 |
| Both | 1.59*** | 1.50, 1.69 | 2.11*** | 1.57, 2.83 | 1.51*** | 1.21, 1.89 |
| DoD occupation specialty | ||||||
| Other occupation (reference group) | 1.00 | 1.00 | 1.00 | |||
| Combat specialist | 1.14*** | 1.11, 1.16 | 1.39* | 1.04, 1.85 | 1.40*** | 1.20, 1.64 |
| Functional support, services, and supply | 0.91*** | 0.89, 0.94 | 0.97 | 0.88, 1.07 | 0.80*** | 0.76, 0.85 |
| Length of index deployment (months) | ||||||
| 1–11 (reference group) | 1.00 | 1.00 | 1.00 | |||
| 12 | 1.19*** | 1.16, 1.22 | 1.28*** | 1.14, 1.44 | 1.24*** | 1.16, 1.33 |
| > 12 | 1.21*** | 1.18, 1.25 | 1.29*** | 1.13, 1.47 | 1.21*** | 1.12, 1.31 |
| Any prior deployment to index | ||||||
| Does not have a prior deployment (reference group) | 1.00 | 1.00 | 1.00 | |||
| Has a prior deployment | 1.14*** | 1.11, 1.16 | 1.16** | 1.04, 1.29 | 1.12*** | 1.05, 1.20 |
| Wounded, injured, assaulted, or hurt on most recent deployment | ||||||
| Was not wounded, injured, assaulted, or hurt (reference group) | 1.00 | 1.00 | 1.00 | |||
| Was Wounded, injured, assaulted, or hurt | 1.02 | 0.99, 1.05 | 1.16* | 1.03, 1.31 | 1.05 | 0.97, 1.14 |
| Combat Exposure Score | ||||||
| 0 (reference group) | 1.00 | 1.00 | 1.00 | |||
| 1 | 1.17*** | 1.14, 1.20 | 1.12 | 1.00, 1.26 | 1.12*** | 1.05, 1.21 |
| 2 | 1.25*** | 1.21, 1.29 | 1.29** | 1.08, 1.53 | 1.19** | 1.06, 1.33 |
| 3 | 1.35*** | 1.30, 1.40 | 1.65* | 1.09, 2.51 | 1.55** | 1.15, 2.08 |
The follow-up questionnaire was completed 30–300 days after the end of the index deployment. All other variables were assessed on the initial questionnaire (completed within 60 days of the deployment end date).
AOR, adjusted odds ratio; CI, 95% confidence interval.
Models also control for the time between the two questionnaires, rank, race/ethnicity, marital status, any child dependent eligible for Military Health System benefits, and FY end date of index deployment.
Any positive mental health is defined as a positive screen for post-traumatic stress disorder, depression, and/or harmful thoughts.
p < 0.05 level, **p < 0.01 level, ***p < 0.001 level.
OEF/OIF, Operation Enduring Freedom in Afghanistan and Operation Iraqi Freedom; TBI, traumatic brain injury.
Model 2 revealed that among female members, having a TBI in combination with a mental health problem (AOR = 2.11; 95% CI: 157-2.83) or a positive mental health screen only was significantly associated with frequent binge drinking (AOR = 1.73; 95% CI: 153-1.97). Yet, having a TBI only did not increase the odds of frequent binge drinking for females.
Model 3 depicts a sensitively analysis for females with any binge drinking as the dependent variable, a less conservative measure of binge drinking. Females who reported both TBI and mental health positive screens had increased odds of binge drinking, compared with those without either condition (AOR = 1.51; 95% CI: 121-1.89). Similarly, females with only a mental health positive screen or with only a TBI positive screen had increased odds of binge drinking, compared with those with neither condition, even though the AORs were smaller than among those with both TBI and a mental health problem.
In all multivariable models, having a higher combat score, being a combat specialist, having a longer index deployment, and having had a prior deployment were significantly associated with increased odds of binge drinking.
Discussion
Binge drinking post-deployment can lead to reintegration problems, especially when members drink to reduce symptoms associated with psychological problems or injuries.9,11 Prior to this study, prevalence estimates of binge drinking stratified by gender were largely unavailable for those returning from OEF/OIF. This study found that among Army active duty members returning from OEF/OIF deployments in FYs 2008-2011, 21.2% of males and 7.4% of females reported frequent (at least monthly) binge drinking. These estimates are much lower than the 53.7% of active duty members, males and females combined, from all service branches with a past year combat deployment who reported at least monthly binge drinking (defined as five or more drinks for males and four or more drinks for females) on an anonymous DoD survey.8 It is unclear how much of this difference is attributable to the slightly different cut-offs used to define binge drinking, or due to the non-anonymous nature of the DoD's post-deployment health surveillance program.
Over 52% of males and 26% of females reported any occasion of binge drinking on the follow-up questionnaire. When combining males and females, the combined prevalence of 49.8% was higher than the 37.6% of members who reported any binge drinking on the initial questionnaire in a prior study utilizing a similar sample of Army active duty members and both studies using the six or more non-gender specific binge drinking definition.7 This increase suggests that either the prevalence of binge drinking among members increases in the initial months post-deployment or that members are less willing to report binge drinking on the initial questionnaire.
This study is one of the first to examine the prevalence of OEF/OIF-related TBIs among females. We found that 7.5% of males and 4.4% of females had a TBI positive screen on their index deployment. These estimates, even among males, are lower than reported in studies that elicited a history of TBI from all previous deployments35,48 or those that relied on smaller, non-representative samples.32,35,36,49,50 In addition, some studies were conducted anonymously,15,32,35,50 as opposed to the current study, which used DoD post-deployment health surveillance data that can be shared with commanders. Similar to binge drinking, reports of TBIs that occurred during a deployment may be higher when assessed further after the end date of deployment. A study of one National Guard brigade combat team in 2007 found that when members were surveyed 1 month before leaving Iraq, and again 1 year later, self-reported rates of TBI were 9.2% while still deployed and 22.0% post-deployment.36 This suggests that members may be hesitant to report TBIs near the end of a deployment, or that members may feel more comfortable reporting health concerns once back at home.36 Hence, our study may underestimate of the prevalence of TBI because history of TBI was assessed around the end of deployment.
This longitudinal study uniquely examined the interaction between TBI and any positive mental health screen (PTSD, depression, or harmful thoughts) and found that male and female members who screened positive for both TBI and any mental health problem had the highest odds of binge drinking, compared with those with neither problem. The odds of post-deployment binge drinking more than doubled for females with positive TBI and mental health screens, compared with females with neither condition, and was 59% higher for males with positive TBI and mental health screens, compared with those with neither problem. This study also suggests that having experienced a TBI on an OEF/OIF deployment, with or without a comorbid mental health problem, is a risk factor for post-deployment binge drinking among both males and females. These findings are consistent with results from other studies that found TBI had an independent association with increased post-deployment binge drinking, after controlling for mental health problems including PTSD.8,15 To our knowledge, this was the first study to examine these relationships by gender.
Our findings are consistent with previous reports that almost twice as many males binge drink, compared with females.51 When comparing Models 1 and 2, even though confidence intervals for males and females often overlapped, females showed a somewhat greater risk of frequent binge drinking if they had longer deployments; were exposed to more combat; were wounded, injured, assaulted, or hurt; or had either a mental health problem alone or in combination with a TBI. However, if female members experienced only a TBI, they were not significantly more likely to report frequent binge drinking. Risk factors related to gender were essentially equivalent when frequent binge drinking for males was compared with any binge drinking among females (Model 3). The greater risk for binge drinking observed in our study is likely multi-factorial. Regardless the cause, alcohol screening results may require gender-specific interpretation when used to initiate preventive strategies.42
The differential prevalence of occupation specialty and combat exposure score by gender is not surprising given differences in combat roles among males and females deployed during the study window. Further studies are needed to examine how DoD occupation specialty and combat exposure are related to prevalence of TBI and post-deployment binge drinking when some females achieve assignment to direct combat occupations.27
As with most military studies,15,32 the occurrence of TBI was operationalized based on retrospective self-report. The limitations of self-report as elicited by the PDHA include potential over-identification due to mistaking a stress response to the events surrounding an injury with the alteration of consciousness due to the physical effect on the brain. The PDHA elicitation procedure also risks under-identification due to a bias toward minimization of problems when the assessment is completed. Both sources of bias increase error associated with the TBI variable, which in turn attenuates observable effects. We also were unable to explore the possible connection between frontal lobe deficits associated with a TBI, or to draw conclusions about such deficits and binge drinking after a TBI. The relationship between TBI experienced during combat deployment and post-deployment alcohol misuse will require replication via other methodologies in order to characterize its full nature and extent.
Lack of anonymity may contribute to underreporting on these self-report measures, which may lead to our results being an underestimate of problems. Also, we did not know lifetime history of TBI, which may complicate recovery from the recent TBI or use of substances,52–55 nor did we know history of drinking prior to the deployment.56 Additionally, we excluded members who completed the older version of the initial questionnaire (before 2008) and those respondents with date fields on the deployment record and initial questionnaire that were a poor match (i.e., outside a 60-day window), which reduced inclusion of many 2008 cohort members. Yet, respondents in the analysis sample did not differ from those in the larger sample that completed the initial questionnaire on key characteristics (Supplementary Table 1).
Our findings confirm that post-deployment binge drinking is common. Results suggest that post-deployment screening and preventive interventions should incorporate risk due to combat exposure, length of deployment, injury while deployed, having incurred a TBI, or experiencing mental health concerns. However, mild TBI may not require or result in the initiation of a treatment episode; thus, population-based prevention messages and programs to reduce binge drinking may be more effective. More research is needed on the interaction of gender with risks for binge drinking, especially when TBI and mental health issues co-exist. Further study of how TBI influences binge drinking is also needed. Does TBI increase stress and thus drive unhealthy coping strategies, or does poor impulse control affect the decision to initiate or continue drinking? A better understanding of the relationship between these conditions would help inform preventive strategies. Finally, this study once again underscores the prevalence of binge drinking among male and female military members and the need to better understand intra-personal and interpersonal drivers of the behavior, as well as cultural influences that maintain it.
Supplementary Material
Acknowledgments
This study was funded by National Institute of Drug Abuse (NIDA) grant R01DA030150. We acknowledge Kennell and Associates, Inc. for compiling the data files used in these analyses, as well as Dr. Thomas V. Williams, the Defense Health Agency's (DHA) DoD data sponsor. The DHA's Privacy and Civil Liberties Office, and the U.S. Army Medical Department's Patient Administration Systems and Biostatistics Activity of the U.S. DoD provided access to these data.
Author Disclosure Statement
The opinions and assertions herein are those of the authors and do not necessarily reflect the official views of the DoD, NIDA, or the National Institutes of Health. No competing financial interests exist.
References
- 1.Bray R.M., Pemberton M. R., Lane M. E., Hourani L. L., Mattiko M. J., and Babeu L. A. (2010). Substance use and mental health trends among U.S. military active duty personnel: key findings from the 2008 DoD health behavior survey. Mil. Med. 175, 390–399 [DOI] [PubMed] [Google Scholar]
- 2.Larson M.J., Wooten N. R., Adams R.S., and Merrick E. L. (2012). Military combat deployments and substance use: review and future directions. J. Soc. Work Pract. Addict. 12, 6–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barlas F.M., Higgins W. B., Pflieger J. C., and Diecker K. (2013). 2011 Department of Defense Health Related Behaviors Survey of Active Duty Military Personnel. Available at: www.ecu.edu/cs-dhs/rehb/upload/DoD-Health-related-Behaviors-Survey-of-Active-Duty-2011.pdf Accessed October21, 2016
- 4.O'Brien C.P., Oster M., and Morden E., (eds); Committee on Prevention, Diagnosis, Treatment and Management of Substance Use Disorders in the U.S. Armed Forces; Board on the Health of Select Populations; Institute of Medicine. (2013). Substance Use Disorders in the U.S. Armed Forces. Available at: www.nap.edu/catalog.php?record_id=13441 Accessed October21, 2016
- 5.Bray R.M., Brown J. M., and Williams J. (2013). Trends in binge and heavy drinking, alcohol-related problems, and combat exposure in the U.S. military. Subst. Use Misuse 48, 799–810 [DOI] [PubMed] [Google Scholar]
- 6.Spera C., Thomas R., Barlas F., Szoc R., and Cambridge M. (2010). Relationship of military deployment recency, frequency, duration, and combat exposure to alcohol use in the Air Force. J. Stud. Alcohol. Drugs 72, 5–14 [DOI] [PubMed] [Google Scholar]
- 7.Larson M.J., Mohr B. A., Adams R. S., Wooten N. R., and Williams T. V. (2014). Missed opportunity for alcohol problem prevention among army active duty service members postdeployment. Am. J. Public Health 104, 1402–1412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adams R.S., Larson M.J., Corrigan J.D., Ritter G.A., Horgan C.M., Bray R.M., and Williams T.V. (2016). Combat-acquired traumatic brain injury, posttraumatic stress disorder, and their relative associations with postdeployment binge drinking. J. Head Trauma Rehabil. 31, 13–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adams R.S., Larson M.J., Corrigan J.D., Ritter G.A., and Williams T.V. (2013). Traumatic brain injury among US active duty military personnel and negative drinking-related consequences. Subst. Use Misuse 48, 821–836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mattiko M.J., Olmsted K. L. R., Brown J. M., and Bray R. M. (2011). Alcohol use and negative consequences among active duty military personnel. Addict. Behav. 36, 608–614 [DOI] [PubMed] [Google Scholar]
- 11.Santiago P.N., Wilk J. E., Milliken C. S., Castro C. A., Engel C. C., and Hoge C. W. (2010). Screening for alcohol misuse and alcohol-related behaviors among combat veterans. Psychiatr. Serv. 61, 575–581 [DOI] [PubMed] [Google Scholar]
- 12.Stahre M.A., Brewer R. D., Fonseca V. P., and Naimi T. S. (2009). Binge drinking Among US active-duty military personnel. Am. J. Prev. Med. 36, 208–217 [DOI] [PubMed] [Google Scholar]
- 13.Larson M.J., Adams R. S., Mohr B. A., Harris A. H. S., Merrick E. L., Funk W., Hoffman K., Wooten N. R., Jeffery D. D., and Williams T. V. (2013). Rationale and methods of the substance use and psychological injury combat study (SUPIC): A longitudinal study of Army service members returning from deployment in FY2008–2011. Subst. Use Misuse 48, 863–879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bray R.M., Pemberton M. R., Hourani L. L., Witt M., Olmsted K. L. R., Brown J. M., Weimer B., Lane M. E., Marsden M. E., Scheffler S., Vandermaas-Peeler R., Aspinwall K. R., Anderson E., Spagnola K., Close K., Gratton J. L., Calvin S., and Bradshaw M. (2009). Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel. http://www.documentcloud.org/documents/684941-2008-department-of-defense-survey-of-health.html (last accessed July11, 2016)
- 15.Adams R.S., Larson M.J., Corrigan J.D., Horgan C.M., and Williams T.V. (2012). Frequent binge drinking after combat-acquired traumatic brain injury among active duty military personnel with a past year combat deployment. J. Head. Trauma. Rehabil. 27, 349–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rona R.J., Jones M., Fear N. T., Hull L., Murphy D., Machell L., Coker B., Iversen A. C., Jones N., David A. S., Greenberg N., Hotopf M., and Wessely S. (2012). Mild traumatic brain injury in UK military personnel returning from Afghanistan and Iraq: cohort and cross-sectional analyses. J. Head Trauma Rehabil. 27, 33–44 [DOI] [PubMed] [Google Scholar]
- 17.Bigler E.D., and Maxwell W. L. (2012). Neuropathology of mild traumatic brain injury: relationship to neuroimaging findings. Brain Imaging Behav. 6, 108–136 [DOI] [PubMed] [Google Scholar]
- 18.Casement M.D., Shaw D. S., Sitnick S. L., Musselman S. C., and Forbes E. E. (2015). Life stress in adolescence predicts early adult reward-related brain function and alcohol dependence. Soc. Cogn. Affect. Neurosci. 10, 416–423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Forbes E.E., Rodriguez E. E., Musselman S., and Narendran R. (2014). Prefrontal response and frontostriatal functional connectivity to monetary reward in abstinent alcohol-dependent young adults. PLoS One 9, e94640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sellitto M., Ciaramelli E., and di Pellegrino G. (2010). Myopic discounting of future rewards after medial orbitofrontal damage in humans. J. Neurosci. 30, 16429–16436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weil Z.M., Corrigan J. D., and Karelina K. (2016). Alcohol abuse after traumatic brain injury: experimental and clinical evidence. Neurosci. Biobehav. Rev. 62, 89–99 [DOI] [PubMed] [Google Scholar]
- 22.Chase S., Ratcliff G., Vernich L., Al-Sukhni E., Yasseen B., and Colantonio A. (2012). Preventive health practices and behavioral risk factors in women surviving traumatic brain injury. Health Care Women Int. 33, 631–645 [DOI] [PubMed] [Google Scholar]
- 23.Preiss-Farzanegan S.J., Chapman B., Wong T. M., Wu J., and Bazarian J. J. (2009). The relationship between gender and postconcussion symptoms after sport-related mild traumatic brain injury. PM R 1, 245–253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wunderle K., Hoeger K. M., Wasserman E., and Bazarian J. J. (2014). Menstrual phase as predictor of outcome after mild traumatic brain injury in women. J. Head Trauma Rehabil. 29, E1–E8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Slewa-Younan S., van den Berg S., Baguley I. J., Nott M., and Cameron I. D. (2008). Towards an understanding of sex differences in functional outcome following moderate to severe traumatic brain injury: a systematic review. J. Neurol. Neurosurg. Psychiatry 79, 1197–201 [DOI] [PubMed] [Google Scholar]
- 26.Niemeier J.P., Marwitz J. H., Lesher K., Walker W. C., and Bushnik T. (2007). Gender differences in executive functions following traumatic brain injury. Neuropsychol. Rehabil. 17, 293–313 [DOI] [PubMed] [Google Scholar]
- 27.US Department of Defense. US Department of Defense and Joint Chiefs of Staff policy memorandum. (2013). Elimination of the 1994 direct ground combat definition and assignment rule. Available at: www.defense.gov/news/WISRJointMemo.pdf Accessed October21, 2016,
- 28.Conard P.L., and Sauls D. J. (2014). Deployment and PTSD in the female combat veteran: a systematic review. Nurs. Forum 49, 1–10 [DOI] [PubMed] [Google Scholar]
- 29.Maguen S., Luxton D. D., Skopp N. A., and Madden E. (2012). Gender differences in traumatic experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. J. Psychiatr. Res. 46, 311–316 [DOI] [PubMed] [Google Scholar]
- 30.Pietrzak R.H., Whealin J. M., Stotzer R. L., Goldstein M. B., and Southwick S. M. (2011). An examination of the relation between combat experiences and combat-related posttraumatic stress disorder in a sample of Connecticut OEF-OIF Veterans. J. Psychiatr. Res. 45, 1579–1584 [DOI] [PubMed] [Google Scholar]
- 31.Bryant R.A. (2008). Disentangling mild traumatic brain injury and stress reactions. N. Engl. J. Med. 358, 525–527 [DOI] [PubMed] [Google Scholar]
- 32.Hoge C.W., McGurk D., Thomas J. L., Cox A. L., Engel C. C., Castro C. A. (2008). Mild traumatic brain Injury in U.S. soldiers returning from Iraq. N. Engl. J. Med. 358, 453–463 [DOI] [PubMed] [Google Scholar]
- 33.Institute of Medicine. (2012). Treatment for posttraumatic stress disorder in military and veteran populations: Initial assessment. Available at: www.nap.edu/catalog.php?record_id=13364 Accessed October21, 2016 [PubMed]
- 34.Kennedy J., Jaffee M., Leskin G., Stokes J., Leal F., and Fitzpatrick P. (2007). Posttraumatic stress disorder and posttraumatic stress disorder-like symptoms and mild traumatic brain injury. J. Rehabil. Res. Dev. 44, 895–920 [DOI] [PubMed] [Google Scholar]
- 35.Schneiderman A.I., Braver E. R., and Kang H. K. (2008). Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: persistent postconcussive symptoms and posttraumatic stress disorder. Am. J. Epidemiol. 167, 1446–1452 [DOI] [PubMed] [Google Scholar]
- 36.Polusny M.A., Kehle S. M., Nelson N. W., Erbes C. R., Arbisi P. A., and Thuras P. (2011). Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in national guard soldiers deployed to Iraq. Arch. Gen. Psychiatry 68, 79–89 [DOI] [PubMed] [Google Scholar]
- 37.Stein M.B., Ursano R. J., Campbell-Sills L., Colpe L. J., Fullerton C. S., Heeringa S. G., Nock M. K., Sampson N. A., Schoenbaum M., Sun X., Jain S., and Kessler R. C. (2016). Prognostic indicators of persistent post-concussive symptoms after deployment-related mild traumatic brain injury: a prospective longitudinal study in U.S. Army soldiers. J. Neurotrauma 2016. April 8; Epub ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ramchand R., Miles J., Schell T., Jaycox L., Marshall G. N., and Tanielian T. (2011). Prevalence and correlates of drinking behaviors among previously deployed military and matched civilian populations. Mil. Psychol. 23, 6–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jakupcak M., Tull M. T., McDermott M. J., Kaysen D., Hunt S., and Simpson T. (2010). PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addict Behav. 35, 840–843 [DOI] [PubMed] [Google Scholar]
- 40.Bliese P.D., Wright K. M., Adler A. B., Hoge C.W., and Prayner R. (2005). Post-Deployment Psychological Screening: Interpreting and Scoring DD Form 2900, in Using the PDHRA 1 of 14, Research Report #2005-003. Available at: http://usamrd-w.amedd.army.mil/assets/docs/publications/bliese_et_al_2005_report_2005-003_interpreting_and_scoring_dd_form_2900.pdf Accessed October21, 2016
- 41.Bliese P.D., Wright K. M., and Hoge C. W., (2011), Preventive mental health screening in the military, in: Deployment Psychology: Evidence-Based Strategies to Promote Mental Health in the Military. Adler A.B., Bliese P.D., and Castro C.A., (eds). American Psychological Association: Washington, D.C, pp. 175–193 [Google Scholar]
- 42.National Institute on Alcohol Abuse and Alcoholism. (2005). Helping Patients Who Drink Too Much: A Clinician's Guide. Available at: http://pubs.niaaa.nih.gov/publications/practitioner/CliniciansGuide2005/guide.pdf Accessed October21, 2016
- 43.Kay T., Harrington D. E., Adams R., Anderson T., Berrol S., Cicerone K., Dahlberg C., Gerber D., Goka R., Harley P., Hilt J., Horn L., Lehmkuhl D., and Malec J. (1993). Definition of mild traumatic brain injury. J. Head Trauma Rehabil. 8, 86–87 [Google Scholar]
- 44.Prins A., Ouimette P., Kimerling R., Cameron R.P, Hugelshofer D.S., Shaw-Hegwer J., Thraikill A., Gusman F.D., and Sheikh J.I. (2003). The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry 9, 151–151 [Google Scholar]
- 45.Bliese P.D., Wright K.M., Adler A.B., Cabrera O., Castro C.A., and Hoge C.W. (2008). Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. J. Consult. Clin. Psychol. 76, 272–281 [DOI] [PubMed] [Google Scholar]
- 46.Calhoun P.S., McDonald S. D., Guerra V. S., Eggleston A. M., Beckham J. C., and Straits-Troster K. (2010). Clinical utility of the primary care—PTSD screen among U.S. veterans who served since September 11, 2001. Psychiatry Res. 178, 330–335 [DOI] [PubMed] [Google Scholar]
- 47.Kroenke K., Spitzer R. L., and Williams J. B. W. (2003). The Patient Health Questionnaire-2 - validity of a two-item depression screener. Med. Care 41, 1284–1292 [DOI] [PubMed] [Google Scholar]
- 48.Tanielian T., and Jaycox L. H. (eds). (2008). Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. RAND Corporation: Santa Monica, CA [Google Scholar]
- 49.Terrio H., Brenner L. A., Ivins B. J., Cho J. M., Helmick K., Schwab K., Scally K., Bretthauer R., andnWarden D. (2009). Traumatic brain injury screening: preliminary findings in a US Army brigade combat team. J. Head Trauma Rehabil. 24, 14–23 [DOI] [PubMed] [Google Scholar]
- 50.Wilk J.E., Thomas J. L., McGurk D. M., Riviere L. A., Castro C. A., and Hoge C. W. (2010). Mild traumatic brain injury (concussion) during combat: lack of association of blast mechanism with persistent postconcussive symptoms. J. Head Trauma Rehabil. 25, 9–14 [DOI] [PubMed] [Google Scholar]
- 51.Brown J.M., Bray R.M., and Hartzell M.C. (2010). A comparison of alcohol use and related problems among women and men in the military. Mil. Med. 175, 101–107 [DOI] [PubMed] [Google Scholar]
- 52.Corrigan J.D., Boger J., and Holloman C. (2012). Lifetime history of traumatic brain injury among persons with substance use disorders. Brain Inj. 26, 139–150 [DOI] [PubMed] [Google Scholar]
- 53.Kennedy C.H., Porter Evans J., Chee S., Moore J. L., Barth J. T., and Stuessi K. A. (2012). Return to combat duty after concussive blast injury. Arch. Clin. Neuropsychol. 27, 817–827 [DOI] [PubMed] [Google Scholar]
- 54.McKinlay A., Grace R. C., Horwood L. J., Fergusson D. M., and MacFarlane M. R. (2010). Long-term behavioural outcomes of pre-school mild traumatic brain injury. Child Care Health Dev. 36, 22–30 [DOI] [PubMed] [Google Scholar]
- 55.Corrigan J.D., Bogner J., Mellick D., Bushnik T., Dams-O'Connor K., Hammond F. M., Hart T., and Kolakowsky-Hayner S. (2013). Prior history of traumatic brain injury among persons in the Traumatic Brain Injury Model Systems National Database. Arch. Phys. Med. Rehabil. 94, 1940–1950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Golub A., and Bennett A. S. (2014). Substance use over the military–veteran life course: An analysis of a sample of OEF/OIF veterans returning to low-income predominately minority communities. Addict. Behav. 39, 449–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.