Abstract
Introduction
Hypermobility disorders of the Temporomandibular joint (TMJ) can be treated by both conservative and surgical approaches. Conservative approaches should be considered as first line treatment for such disorders. Prolotherapy with 25 % dextrose being injected into the posterior pericapsular tissues is one such treatment modality with favorable outcomes.
Aim
To study the efficacy of single injection of 25 % dextrose in pericapsular tissues in the management of hypermobility joint disorders of TMJ as first line treatment.
Patients and Methods
We have studied a total of 23 patients suffering from either chronic recurrent dislocation or subluxation of the TMJ who were treated with the single injection technique prolotherapy with 25 % dextrose into the pericapsular tissues along with auriculotemporal nerve block and found encouraging results.
Results
Overall success rate in our study was 91.3 % (21/23) with a minimum follow up period of 13.9 months. Number of successfully treated patients requiring one injection was 7 (30.4 %), two injections was 8 (34.7 %) and requiring three injections was 6 (26.1 %). There were no permanent complications.
Conclusion
Hence the use of 25 % dextrose as a proliferant to treat hypermobilty disorders of the TMJ is recommended by us as a first line treatment option as it is safe, economical and an easy procedure associated with minimal morbidity.
Keywords: Temporomandibular joint, Hypermobility disorders, Prolotherapy, Dextrose, Auriculotemporal nerve block
Introduction
Hypermobility disorders of the temporomandibular joint (TMJ) can be defined as hypertranslation of the mandibular condyle anterior and superior to the articular eminence during mouth opening [1]. Although no definite classification scheme exists yet it can be commonly classified as: subluxation, acute, chronic and recurrent dislocations of the TMJ [2]. Subluxation is defined as a self-reducing partial dislocation of the TMJ, during which the condyle passes anterior to the articular eminence [3]. In distinction, dislocation may be considered a long-lasting inability to close the mouth due to locking of the condyle anterior to the eminence that is maintained by muscle spasms [4].
Common etiologic factors of hypermobility include daily activities like yawning, wide biting, trauma, intubation with general anesthesia, dental extractions, forceful hyperextension, connective tissue disorders like Ehlers–Danlos syndrome and Marfan Syndrome, internal derangement, lost vertical dimension, occlusal discrepancies, psychogenic and drug induced such as Phenothiazine use [3]. These factors contribute by increasing capsule weakness and ligament laxity.
Treatment modalities available to treat chronic recurrent dislocations and troublesome subluxations are both conservative and surgical. Conservative methods include: restriction of mandibular movement, injection of botulinum toxin into the muscles of mastication, injection of sclerosing agents into the joint tissues, autologous blood transfer or a combination. Operations have also been tried including capsular plication, reduction or augmentation of the articular eminence, scarification of the temporalis tendon, lateral pterygoid myotomy, and condylectomy. Osteotomies like sagittal split and vertical ramus osteotomies have also been done utilizing the new joint position [5].
Proliferation treatment, or “prolotherapy,” is also known as regenerative injection therapy and “growth factor stimulation injection therapy”. First reported by Schultz in 1937, the technique has been reported to be effective in stabilising injured TMJ and relieving joint pain. Prolotherapy involves injecting a non-pharmacological irritant solution such as dextrose, glycerin etc. into the region of the tendons or ligaments, and it is hypothesized that it initiates a non-inflammatory or inflammatory process that results in a reparative process causing deposition of new additional fibres that will strengthen lax tendons or ligaments and possibly promote the release of local growth factors [6]. Prolotherapy is usually performed by injecting varying solutions of dextrose in multiple sites of a single joint [7], however as proposed by Zhou et al. [8] it can also be performed using a single site injection technique.
This study is undertaken to assess the therapeutic benefits of injecting 25 % dextrose in the pericapsular tissues of hypermobile TMJs’ via a single injection site in order to eliminate the episodes of dislocations/subluxations.
Patients and Methods
A total of 23 patients were included in our study and they reported to our OPD of Department of maxillofacial surgery between September 2014 and June 2016. The most common presenting complaints were history of locking episodes during yawning in the morning which in some cases were self reducible and in others required professional assistance and also loud sounds during opening and closing of the mouth. Pain was also a feature in some cases. The diagnosis of subluxation or chronic recurrent dislocation was made on the basis of history and clinical examination. Orthopantograms were ordered to aid in the diagnosis. Pre-operative mouth opening was recorded for all patients in millimeters at the beginning of the study and again post-operatively after a minimum of 6 months follow up time. Inclusion criteria for our study was occurrence of more than three locking episodes in the last 6 months time and for cases of subluxation, the diagnosis was criteria enough for inclusion into the study.
The technique followed was the single injection technique also called modified prolotherapy wherein a point 10 mm anterior to tragus on the Holmlund–Hellsing line and 10 mm below was marked (Fig. 1). This marking was used first to provide the auriculotemporal nerve block using 2 ml of 2 % lidocaine followed by an interval of 10 min after which the proliferant was injected. 25 % dextrose was the proliferant agent used in this study and using the same mark as previously described, the needle was first advanced 25 mm deep in an antero-medial direction staying behind the neck of the condyle and then injecting 1 ml of solution into the posterior periarticular tissues, and then the remaining 1 ml of solution was injected slowly while retracting the needle superficially (Fig. 2).
Fig. 1.

Marking of the Holmlund–Hellsing line and the point of needle insertion
Fig. 2.

Illustration of the direction of needle insertion for the auriculotemporal nerve block and 25 % dextrose solution
Post-operatively the patients were advised to eat soft food and to avoid wide opening of the mouth, and during activities like yawning to apply counter pressure in the chin region. Non-steroidal anti-inflammatory drugs were avoided in the postoperative period and were prescribed as ‘sos’ drugs as these class of analgesics are thought to interfere with the therapeutic action of the proliferants [6]. Patients were recalled at 2 weeks, 1 month, 3 months and 6 months, thereafter telephonic conversations were also done to follow up with the patients up to a maximum of 15 months. They were assessed for hypermobility of the joints, in the form of recurrence of dislocations or the persistence of loud sounds during opening and closing. Reinjection up to a maximum of three times was given in the follow-ups if required, the second injection usually been given at 2 week follow up to mount the response of the first injection and the third injection if required, between 1 and 2 months of follow up in case of recurrence or if the patient felt that there was a sensation of ‘looseness’ in the joints. Successful treatment outcome was defined as absence of any episodes of dislocation or subluxation for a minimum of 6 months after last injection.
Results were tabulated and derived. Statistical analysis was done where required using the fisher’s exact test and students t test.
Results
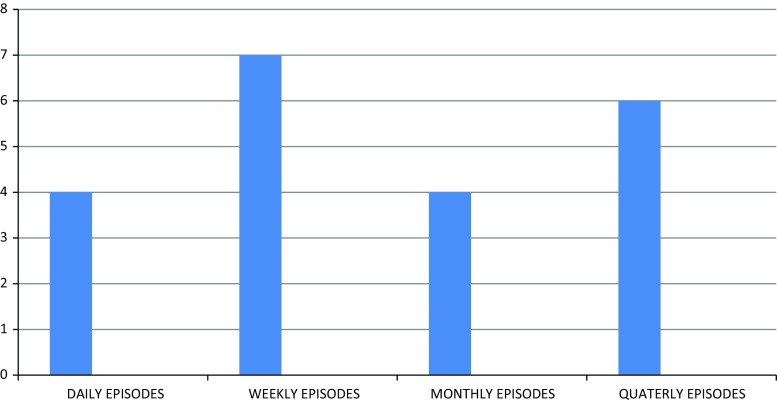
Out of the 23 patients, 14 patients (60.9 %) were female and 9 (39.1 % %) male. Age group ranged between 15 and 55 years (mean = 27 years). 21(91.3 %) cases were diagnosed as acute recurrent dislocation and 2 (8.7 %) as subluxation. 14 (60.8 %) cases had bilateral hypermobility disorders and 9 (39.1 %) had unilateral hypermobility disorders. Of the patients who were suffering from the unilateral hypermobility disorders, the left joint was more commonly involved (5/9 = 55.5 %) with the right joint being less commonly involved (4/9 = 44.5 %). The frequency of episodes of dislocations ranged between daily episodes to once in few months (Fig. 3). The mouth opening was more than three finger breadths in all cases.
Fig. 3.
This chart shows the number of patients having daily, weekly, monthly and quarterly episodes of dislocations respectively
All patients tolerated the technique well and complained of no or minimal pain on injection. Transient facial palsy seen in all cases resolved 2 h post-operatively as the effect of lidocaine subsided. The minimum period of follow up was 6 months and ranged between 12 and 21 months (mean = 13.9 months). Seven patients were given single injection (30.4 %),of which all had successful outcome. Remaining sixteen patients were treated with second injection on the second week. Of these, 9 (39.1 %) were successfully treated for their hypermobilty disorder, six (26.1 %) patients received a third injection in the second month due to either episode(s) of dislocation, recurrence of sounds in the TMJ or a sensation of ‘looseness’ of the TMJ in the corresponding time period, following which their symptoms got resolved. Two (8.7 %) patients experienced episodes of dislocation even after second injection and refused the third injection.
Hence by the end of our study, the overall success rate was 91.3 % (21/23). Of the successfully treated cases, seven were treated by single injection alone (30.4 %), eight (34.7 %) by two injections and six (26.1 %) by three injections (Table 1). Those patients who received either two or three injections mostly had bilateral disorders (12/16 = 75 %) and the association between requirement of multiple injections and bilateral disorders was highly significant (p = 0.006).
Table 1.
Evaluation of success rate at different follow up periods and after giving additional injections until a maximum of 3 where required
| Time of follow up | Number of patients who received single injection | Number of patients who received two injections | Number of patients who received three injections | Success rate % |
|---|---|---|---|---|
| 2 weeks | 23 | – | – | 7/23 = 30.4 % |
| 4 weeks | 7 | 16 | – | (7/23 + 9/23) = 69.5 % |
| 3 months | 7 | 10 | 6 | (7/23 + 10/23 + 6/23) = 100 % |
| 6 months | 7 | 10 | 6 | (7/23 + 8/23 + 6/23) = 91.3 %a |
aFailure in two cases after 4 months
The mean difference between pre-operative and 6 month postoperative mouth openings was 3.83 mm which was a statistically significant difference (p value = 0.001), however no patient complained of any interference with functional activities (Table 2).
Table 2.
Pre-operative and post-operative changes in mouth opening
| Pre-operative mean (mm) | Pre-operative SD | Post-operative mean (mm) | Post-operative SD | p value | |
|---|---|---|---|---|---|
| Mouth opening | 43.65 | 3.71 | 39.83 | 3.68 | 0.001 |
Discussion
Various methods have been described in literature to treat hypermobility disorders of the TMJ. Conservative methods include injecting autologous blood intra-articularly (ABI) and in pericapsular tissues [9, 10]; sclerosing agents like tetracycline, cyclophosphamide and OK-32 [11]; injecting botulinum toxin A into the lateral pterygoid muscle [12], prolotherapy [7] or combination treatments like Inter-Maxillary Fixation with ABI [13]. Surgical methods used were capsulorrhaphy, ligation of capsule with fascia lata, augmentation of the eminence, eminectomy, myotomy and down fracturing of the zygomatic arch [14].
We have used the method of prolotherapy as it avoids the use of surgery as the first line of treatment and also overcomes the complications associated with direct intra-articular injections of ABI and sclerosing agents, as prolotherapy is done in pericapsular tissues.
Since 1937 the technique of prolotherapy has been reported to be effective in stabilising injured TMJ and relieving joint pain [15]. Proliferants used for prolotherapy are substances injected into a ligament which lead to new collagen formation. They do so by causing local inflammation. Once the inflammation has begun and granulocytes and macrophages have been attracted to the injection site, fibroblasts follow and deposit new collagen. The new collagen that is produced at the injection site undergoes contraction and pulls the ligament tighter hence reducing the laxity. There are three classes of proliferants: irritants, osmotics and chemoattractants. Dextrose is an osmotic proliferant which acts by dehydrating the cells at the injection sites which leads to release of cellular fragments that act as chemoattractants and start the inflammatory cascade which ultimately leads to deposition of collagen. Another mechanism is by glycosylating tissues making them appear foreign to the immune system hence starting an inflammatory reaction. Whatever the initiating mechanism, the subsequent inflammatory reaction and the consequent wound healing cascade lead to fibroplasia in due time [6]. Unlike repair after an injury, disruption of the architecture of the tissue does not occur from injury, and new cells and matrix can be deposited in an organized fashion, with maturation of new tissue from 6 to 8 weeks [6]. Photomicrographs of histologically prepared samples taken from injection sites confirm that granulation occurs at the prolotherapy injection site [16].
The results achieved in our study showed a high success rate of 91.3 %. A dextrose concentration of more than 10 % works partly by inflammation [7] and we have used a stronger concentration of 25 % as it is expected to have a stronger inflammatory reaction and hence more fibroplasia. 25 % dextrose is also very easily available, it is cost effective and is very safe. Also the use of a single injection technique was used, as a single injection into pericapsular tissues is more beneficial as compared to additional injection into the articular space that disturbs the equilibrium of the articular surfaces especially the cartilage. Evidence of therapeutic fibrosis in the pericapsular tissues was evidenced in post-operative MRI’s taken at 1 year follow up (Fig. 4).
Fig. 4.
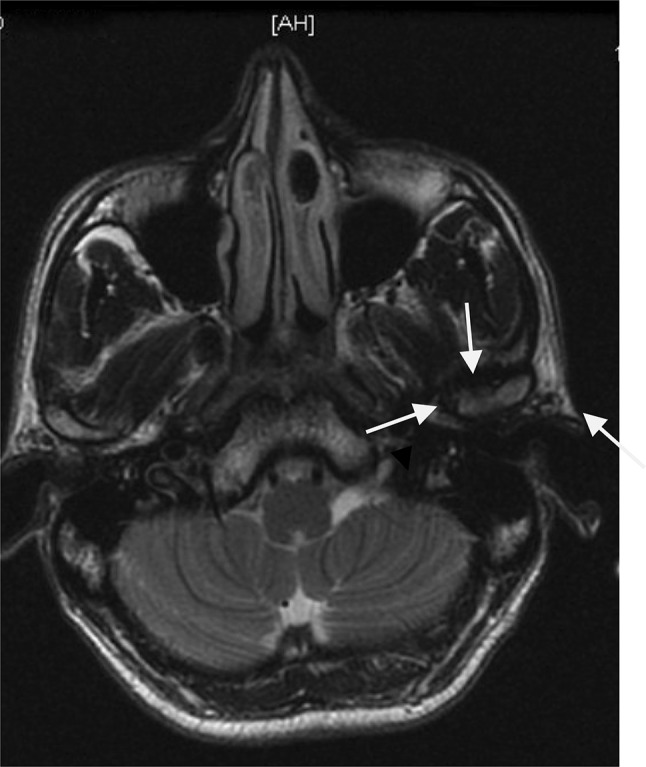
Arrows pointing at the fibrosis (reduced signal intensity) seen in the pericapsular tissues of the left TMJ as compared to the right TMJ in a patient who received two sessions of prolotherapy. The MRI was taken after 1 year from last injection
The pain associated with the injection could be efficiently reduced with the use of auriculotemporal nerve block prior to the dextrose injection. None of our patients complained of any severe pain although mild discomfort was reported by a few. Most of the patients required two injections in total for successful outcome (8/23 = 34.7 %). Those patients who received either two or three injections mostly had bilateral disorders (12/23 = 75 %) and as previously mentioned, this association was highly significant (p = 0.006). No patient had any permanent facial nerve damage. Although patients had a statistically significant decrease in mouth opening (p value = 0.001), it was not associated with any limitations in performing daily activities like mastication and speech and was hence not described as a complication or side effect.
Conclusion
Prolotherapy with 25 % dextrose as single injection technique either in single dose or multiple doses should be considered as first line treatment of chronic recurrent dislocations and subluxations of the mandible with surgical options kept in reserve for refractory cases or cases of recurrence. Although we followed up our patients for an average time period of 13.9 months, a longer follow up is needed to further substantiate this treatment modality.
Compliance with Ethical Standards
Conflict of interest
None.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Quinn PD. Osseous surgery of the temporomandibular joint. In: Quinn PD, editor. Color atlas of temporomandibular joint surgery. St. Louis: Mosby; 1998. pp. 102–111. [Google Scholar]
- 2.Adekeye EO, Shamia RI, Cove P. Inverted L-shaped ramus osteotomy for prolonged bilateral dislocation of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1976;41:568–577. doi: 10.1016/0030-4220(76)90308-X. [DOI] [PubMed] [Google Scholar]
- 3.August M, Troulis MJ, Kaban LB, et al. Hypomobility and hypermobility dis-orders of the temporomandibular joint. In: Miloro M, Ghali GE, Larsen PE, et al., editors. Peterson’s principles of oral and maxillofacial surgery. London: BC Decker; 2004. pp. 1033–1047. [Google Scholar]
- 4.Sato J, Segami N, Nishimura M, et al. Clinical evaluation of arthroscopic eminoplasty for habitual dislocation of the temporomandibular joint: comparative study with conventional open eminectomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2003;95:390. doi: 10.1067/moe.2003.128. [DOI] [PubMed] [Google Scholar]
- 5.Aaron L, Daniel P. Temporomanibular joint dislocation. Oral Maxillofacial Surg Clin Am. 2015;27:125–136. doi: 10.1016/j.coms.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Banks A. A rationale for prolotherapy. J Orthop Med J. 2003;116:1179. [Google Scholar]
- 7.Refai H, Altahhan O, Elsharkawy R. The efficacy of dextrose prolotherapy for temporomandibular joint hypermobility: a preliminary prospective, randomized, double-blind, placebo-controlled clinical trial. J Oral Maxillofac Surg. 2011;69(2962–70):9. doi: 10.1016/j.joms.2011.02.128. [DOI] [PubMed] [Google Scholar]
- 8.Zhou H, Hu K, Ding Y (2014) Modified dextrose prolotherapy for recurrent temporomandibular joint dislocation. Br J Oral Maxillofac Surg 52:62–66 [DOI] [PubMed]
- 9.Coser R, da Silveira H, Medeiros P, Ritto FG. Autologous blood injection for the treatment of recurrent mandibular dislocation. Int J Oral Maxillofac Surg. 2015;44:1034–1037. doi: 10.1016/j.ijom.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Brachmann F. Autologous blood injection for recurrent hypermobility of the temporomandibular joint. Dtsch Zahnarztl Z. 1964;15:97–102. [Google Scholar]
- 11.Matsushita K, Abe T, Fujiwara T. OK-432 (Picibanil) sclerotherapy for recurrent dislocation of the temporomandibular joint in elderly edentulous patients: case reports. Br J Oral Maxillofac Surg. 2007;45:511–513. doi: 10.1016/j.bjoms.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Fu K, Chen HM, Sun ZP, et al. Long term efficacy of botulinum toxin type A for the treatment of habitual dislocation of the temporomandibular joint. Br J Oral Maxillofac Surg. 2010;48:281–284. doi: 10.1016/j.bjoms.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Hegab AF. Treatment of chronic recurrent dislocation of the temporomandibular joint with injection of autologous blood alone, intermaxillary fixation alone, or both together: a prospective, randomised, controlled clinical trial. Br J Oral Maxillofac Surg. 2013;51:813–817. doi: 10.1016/j.bjoms.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 14.Bradley P. Injuries of the condylar and coronoid process. In: Rowe NL, Williams JL, editors. Maxillofacial injuries. Churchill Livingstone: Elsevier; 2009. pp. 354–355. [Google Scholar]
- 15.Schultz LW. A treatment of subluxation of the temporomandibular joint. JAMA. 1937;25:1035–1037. [Google Scholar]
- 16.Hackett GS, Henderson DG. Joint stabilization: an experimental, histologic study with comments on the clinical application in ligament proliferation. Am J Surg. 1955;80:968–973. doi: 10.1016/0002-9610(55)90568-7. [DOI] [PubMed] [Google Scholar]