Abstract
Purpose
To assess efficacy of C-reactive protein levels as monitoring tools for patients with fascial space infections of odontogenic origin.
Material and Method
A randomized prospective study was conducted on 20 patients suffering from fascial space infection of odontogenic origin, in the department of Oral and Maxillofacial Surgery Bharati Vidyapeeth dental college and hospital, Pune, Patients between 18 and 60 years of age of both the sexes were selected. All patients were treated and observed by the same surgeon. Patient’s venous blood sample was collected pre-operatively and on 2nd and 5th post-operative days for evaluation of WBC count and C-reactive protein (CRP). All patients were encouraged for strict follow-up protocol.
Result
Where the results of WBC count and CRP when compared it was seen that the mean values of WBC were normal in 15 cases and abnormal in 5 cases on day 0, day 2 and day 5; whereas the mean values of CRP were abnormal on day 0 and day 2 and were within normal limit on day 5 in all cases.
Conclusion
The findings of this prospective analysis indicate that White blood cells and C-reactive protein are effective markers for determining severity of infection, efficacy of treatment regime for patients with fascial space infections of odontogenic origin. Thus the markers also help in making treatment of patients with fascial space infections of odontogenic origin more cost effective and they also help protecting patients from side effects of excess drugs usage. Thus we conclude that CRP should be incorporated as monitoring tools for managing patients with fascial space infections of odontogenic origin.
Keywords: Space infection, CRP vs WBC, Odontogenic infections, Ludwig’s angina
Introduction
Maxillofacial Infection is one of the life threatening conditions, despite greatly improved health services available in present era, severe odontogenic infections still remains leading cause of morbidity and mortality. Lethal complications like upper airway obstruction, descending mediastinitis, thrombosis of jugular vein, venous septic emboli, rupture of carotid artery, adult respiratory distress syndrome, pericarditis, septic shock and disseminated intravascular coagulopathy may become inevitable. Making vigilant scrutiny and monitoring of such patients is necessity. Although conventional measures to estimate infections such as WBC count and ESR values are valuable in determining state of patient at testing time, the predictability of these is worth limited [1].
The quest for a clinical crystal ball is not new. The desirability of serum derived surrogate predictor behavior and outcome cannot be under estimated, arousing interest in identifying substances which could function as prospective monitor of disease progression. Thus various inflammatory markers came into existance [1]. Advocates of inflammatory markers narrate numerous advantages for their usage. According to them, quantitative determination of serum markers can be used for determining therapeutic efficacy of different treatment regimes of infection, for monitoring post operative infections, for investigating various levels of infections, use of prophylactic antibiotics and duration of antibiotic usage become more appropriate [1, 2].
The advantage of having short half life makes CRP levels as sensitive indicators of infection [3–6]. So in the present prospective study, sincere attempt has been made to assess efficacy of CRP level compared to WBC count as monitoring tools for patients with fascial space infections of odontogenic origin.
Material and Method
A randomized prospective study was conducted on 20 patients suffering from fascial space infection of odontogenic origin visiting the Department of Oral and Maxillofacial Surgery, Bharati Vidyapeeth Dental College and Hospital, Pune. The Institutional Review Board approval and the informed written consent from all the patients was obtained.
Inclusion criteria consisted of:
Patients between 18 and 60 years of age.
Patients not receiving any antimicrobial medication prior to treatment
Fascial space infection of odontogenic origin only.
Exclusion criteria consisted of:
Immunocompromised patient and mentally challenged patients.
Patients with previously radiated maxillofacial region.
Patients having received antibiotics for recent systemic infection 6 weeks prior to surgery.
Pregnant female patients.
Patients unable to come for follow up visits.
Detailed clinical history of each patient was recorded. Patient’s venous blood sample was collected pre-operatively by applying tourniquet and puncturing anticubital vein using a vaccutainer. At every scheduled visit, 5 ml. of blood was withdrawn; out of which 4 ml each was used for estimation of WBC count (complete haemogram) and 1 ml was used for analysis of C Reactive Protein (CRP). Blood samples of patients with diagnosis of fascial space infections of odontogenic origin were taken three times for estimating serum levels of WBCs and CRP which was as follows:
D0-pre-operatively Before starting any treatment.
D2-post-operative day 2.
D5-post-operative day 5.
The sample reports of D0 visit was collected and used as reference for further treatment. Values of D2 and D5 were taken to confirm patient’s progress and continuous improvement towards normal values of WBC and CRP (i.e. D0).
Incision and drainage with elimination of odontogenic focus of infection were done. Postoperative Blood sample was collected on 2nd and 5th for investigation of CRP and WBC count. CRP level was evaluated by quantitative turbidimetry method; WBC was evaluated by Complete blood count (automated hematology cell counter). All the personal information and reports of the patients included in the present study were kept strict confidential.
Results
This was a randomized prospective study conducted on 20 patients visiting Department of Oral and Maxillofacial Surgery, Bharati Vidyapeeth Dental College and hospital, Pune with diagnosis of fascial space infections of odontogenic origin. The patients were treated on in-patient and out-patient basis.
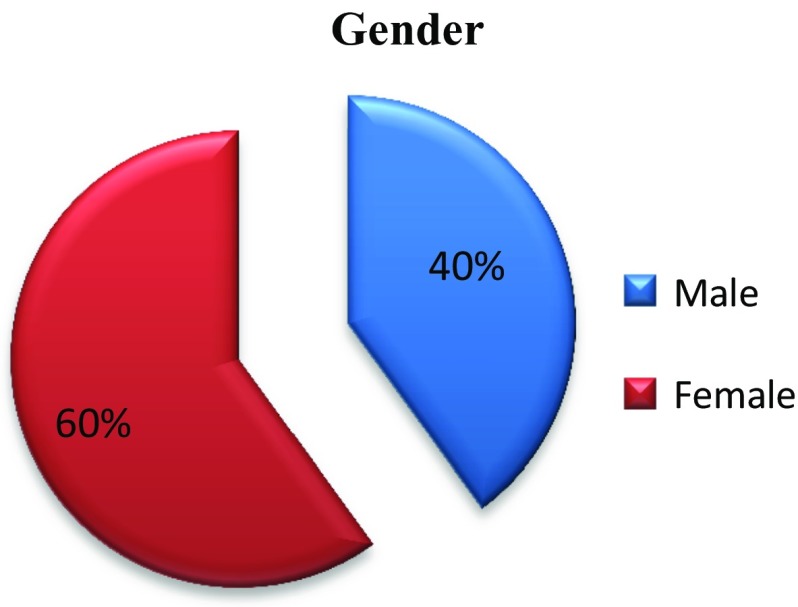
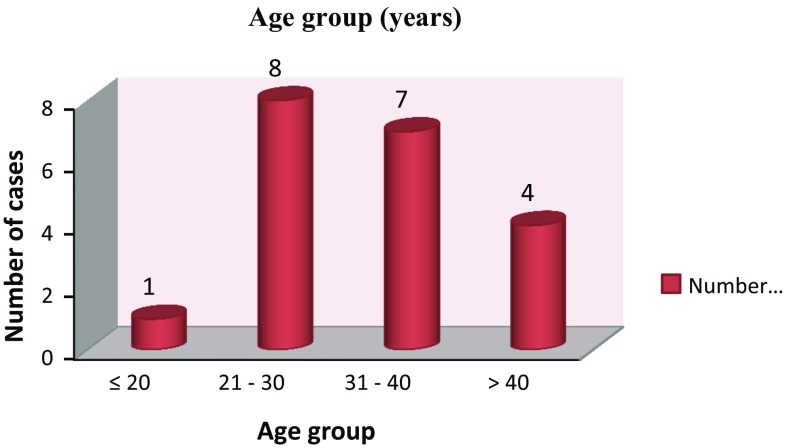
The patients were within age group of 18–60 years including 40 % males and 60 % females (Fig. 1) (Average = 33.7, Median = 31, SD = 10.91). The mean age of patients was <20 years in 5 %, 21–30 years in 40 % patients, 31–40 in 35 % and >40 years in 20 % patients (Fig. 2).
Fig. 1.
Gender wise distribution of patients
Fig. 2.
Distribution of patients with respect to age (years)
McNemar’s test and Paired t- test were used for statistical analysis. By using McNemar’s test (p value <0.05) it was seen that there was a significant difference at day 0 and at day 2 with respect to WBC count level. It was also noted thath there was significant difference (p value <0.05) at day 0 and at day 5 with respect to WBC count level. By using Paired t test (p value <0.05), it was seen that there was significant difference between mean CRP count at day 0 to day 2 and at day 0 to day 5.
The Laboratory value of WBC was evaluated using complete haemogram by automated hematology cell counter and CRP was evaluated using quantitative turbidimetry method. Lab Investigations were done on preoperatively i.e. Day 0, post-operative day 2 i.e. D2 and post-operative day 5 i.e. D5. The standard value of WBC in complete haemogram is 4000–11,000/cu mm and C-reactive protein is 0–6 mg/dl. The value of WBCs on Day 2 and Day 5 were compared to values on Day 0.
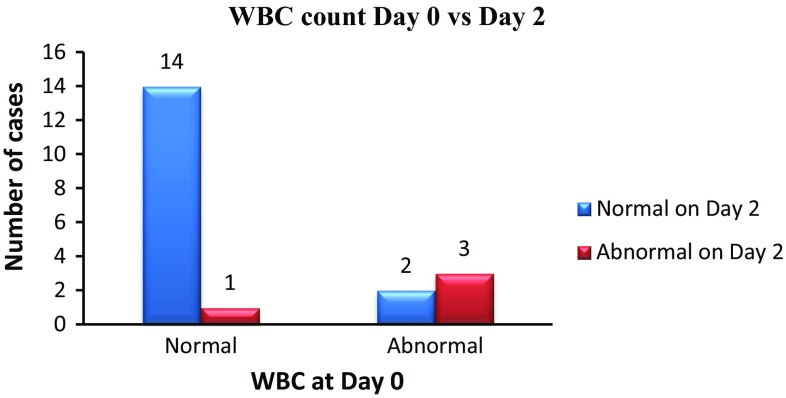
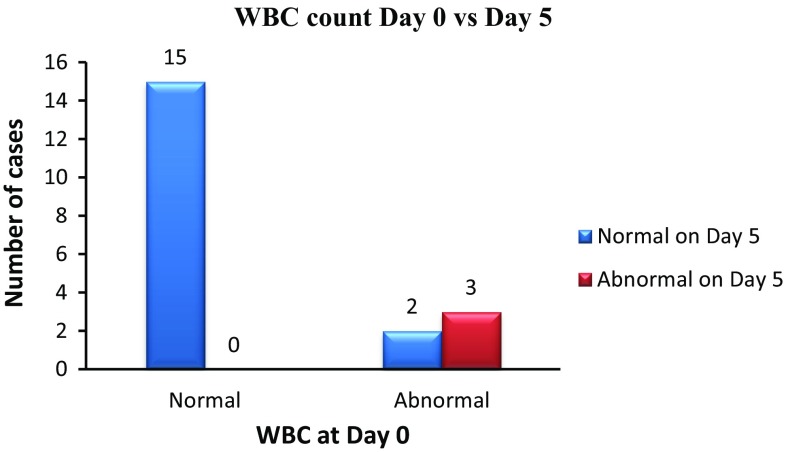
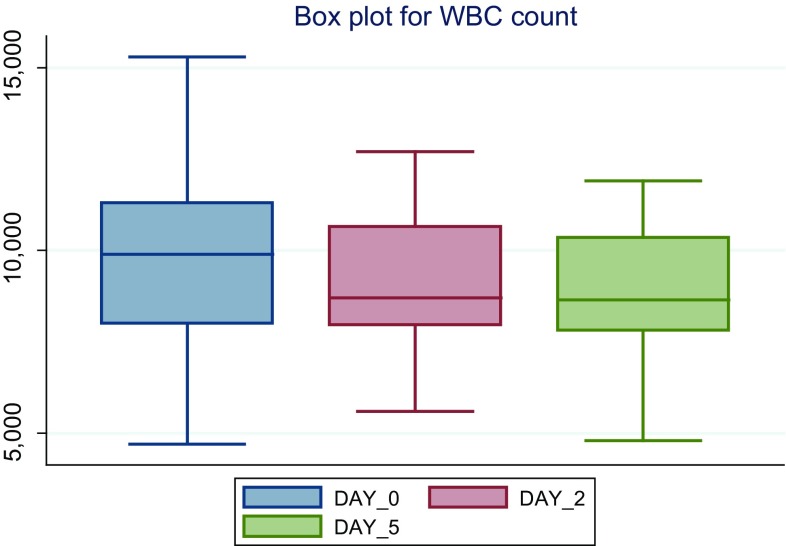
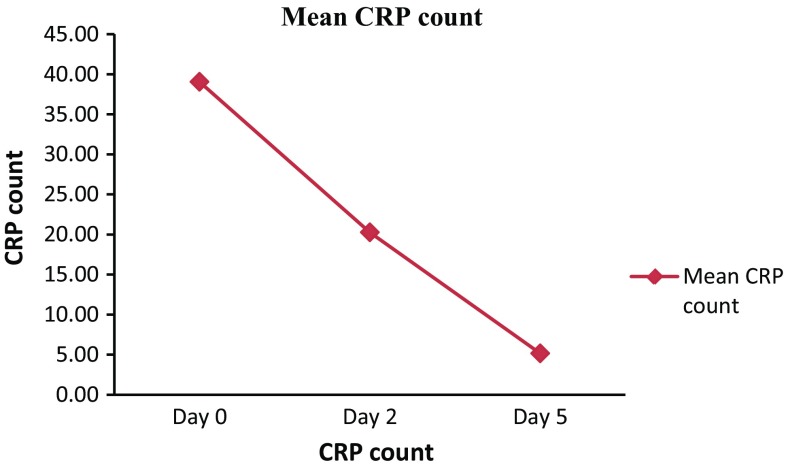
From the obtained data, we notice that distribution of cases with respect to WBC level at day 0 and Day 2 WBC count was normal in 15 cases and abnormal in 5 cases (Fig. 3) of cases with respect to WBC level at day 0 and Day 5 WBC count was normal in 15 cases and abnormal in 5 cases (Figs. 4, 5). By using McNemar’s test p value <0.05 therefore there is significant difference at day 0 and at day 2 and day 0 and day 5 with respect to WBC count level. Similarly, we noticed that CRP was also a significant predictor of fascial Space Infections of odontogenic origin and in Comparison of mean CRP count at day 0 and at day 2, Day 0 and Day 5. The mean of CRP count on day 0 was 39.05 mg/dl, on day 2 it was 20.25 mg/dl (p value <0.001) and on day 5 it was 5.15 mg/dl (p value <0.001) for all 20 cases. By using paired t test p value <0.05 therefore there is significant difference between mean CRP cont at day 0 to day 2 and at day 0 to day 5 (Fig. 6).
Fig. 3.
Distribution of cases with respect to WBC level at day 0 and Day 2
Fig. 4.
Distribution of cases with respect to WBC level at day 0 and Day 5
Fig. 5.
Mean WBC count
Fig. 6.
Mean CRP count
When these results of WBC count and CRP when compared it was seen that the mean values of WBC were normal in 15 cases and abnormal in 5 cases on day 0, day 2 and day5; whereas the mean values of CRP were abnormal on day 0 and day 2 and were within normal limit on day 5 in all cases.
Discussion
The acute phase response is a complex set of systemic and metabolic reactions elicited by infections or other causes of injury. Besides other physiological, metabolic and biochemical changes, the acute phase response is characterized by alterations in the hepatic synthesis and serum levels of some proteins. Thus, while the levels of positive acute phase proteins like CRP, complement 3, serum Amyloid A, alpha-1 and glycoprotein etc. increase due to stimulation of hepatic synthesis, depression of hepatic production of visceral transport proteins (negative acute phase proteins) like albumin, transferring, thyroxin binding prealbumin (TBPA) and retinol binding proteins (RBP) etc. occurs [7]. Several reports have indicated that visceral transport proteins, mainly those with a low turnover rate, like TBPA, RBP are useful to evaluate protein and protein energy under nutrition as well as to monitor nutritional recovery during nutrient repletion. However the presence of infection results in depression of their hepatic production as well as in increased passage to the extra vascular space, consequently diminishing their serum levels making them markers for acute phase conditions [7]. Similarly CRP, which is present in only small amounts in healthy individuals, is involved in several processes of the unspecific immunologic defense. In severe infections or inflammatory reactions a striking rise in the serum concentration is often seen. This suggests the possibility that rise of CRP is sufficiently rapid and specific to serve as a definitive aid in the early diagnosis of septicemia [5]. Thus based on these properties of the markers attempt has been made to use them in patients with fascial space infections [2].
In the past, the complete blood count (CBC) has been chiefly a tool of the physician. Standard normal values for the various CBC components have been available for nearly 40 years, and in the last two decades clinicians are utilizing CBC results for making diagnostic, Prognostic, and therapeutic recommendations. But the use of the CBC by dentists is limited; most CBC examinations are ordered as part of routine laboratory examinations upon admission to the hospital for operative procedure in Oral surgery. CBC examinations are requested for treatment of patients with facial cellulitis of dental origin to monitor the course of the infection and the efficacy of therapy. The various indices of the CBC are found to be sensitive indicators for physiologic and pathologic state of the individual. These count and the differential WBC counts have been used for the past 75 years to help evaluate infectious and non-infectious diseases [8].
In the present study, we found that WBC and CRP had a high degree of correlation with severity of infection having p value <0.01 from Day 0 and Day 2 and Day 5. In the similar study conducted by Pinilla et al., where they found statistically significant correlation between prealbumin and CRP at 2nd day (r = 0.45, p < 0.01) and 5th day (r = 0.53, p < 0.01) in infection patients [8]. Similar study was conducted by Malve I on under nourished children with associated clinical infection. They found that mean serum levels of prealbumin was significantly decreased (p < 0.001) and levels of CRP was significantly increased (p < 0.01) when compared to healthy controls [7]. In one more study by Pinilla et al. [9], they conducted a study on 70 critically ill patients by measuring plasma levels of prealbumin and CRP, energy expenditure by indirect calorimeter and severity of multiple organ dysfunctions, his study demonstrated a strong correlation between severity of organ dysfunction and ratio of two hepatic proteins- CRP and prealbumin. They concluded that use of inflammatory markers prealbumin and CRP is an easy and inexpensive method of assessing severity of illness incritically ill patients. similarly Girish Nagarale, S. Ravindra, Srinath Thakur, and Swati Setty. In 2010 did study, A total of 45 Systemically healthy subjects were selected for the study. Subjects were divided into three groups: group A: healthy controls, group B: gingivitis, group C: periodontitis. Serum levels of CRP were determined by using a latex slide agglutination method with commercially available kit with lower detection limit of 6 mg/L. CRP was negative in all the 15 subjects in groups A and B at baseline, 7 and 30th day. CRP was positive only in 2 subjects in Group C at baseline and 7th day [10].
All assessments were made during index hospitalization and within 72 h of symptom onset. The patients were divided into two groups based on the presence or absence of periodontal diseases and were frequency matched for sex, body mass index, smoking and traditional risk factors of cardiovascular disease. Using t test, the results were compared between the two groups [11]. Ebersole in 1997 [12] did a comparative assessment of clinical characteristic in adult periodontitis patients and normal subjects. They found significant increased levels of CRP and hepatoglobin in patients with periodontitis. With this finding they concluded that localized infection resulted in increased inflammation eliciting systemic host changes manifested by increased CRP [13]. Manelli also conducted a retrospective review on 107 burn patients in 1998 to determine efficacy of prealbumin and CRP as markers of inflammation and tissue destruction. They found that values of prealbumin showed upward and CRP a downward slope in those patients in which the condition improved, whereas no change in values in patients who died. Thus they came to conclusion that both prealbumin and CRP are important markers of inflammation and tissue destruction [14]. Gunnel et al. and Haupt et al. [15] demonstrated the association between preoperative acute phase response and post operative complications. They found out that the serum concentration of IL-6, α-1 antitrypsin and CRP were raised [16, 17]. Flores et al. in 2001 prospectively studied 54 patients with blunt trauma over a 4 month period. Culture proven infections were collected and CRP was determined every day. The results showed that serum CRP was higher in severely infected patients. The study concluded that CRP levels higher than 11 mg per dl suggest an underlying infectious complication [18]. The present study goes well with the above mentioned studies in the way that CRP levels decline significantly when effective treatment was given to the patient. Thus in the present study, it is seen that WBC and CRP are significant predictors for severity of infection.
Conclusion
The findings of this prospective analysis indicate that White blood cells and C-reactive protein are effective markers for determining severity of infection, efficacy of treatment regime for patients with fascial space infections of odontogenic origin. Thus the markers also help in making treatment of patients with fascial space infections of odontogenic origin more cost effective and they also help protecting patients from side effects of excess antibiotic usage. Thus we conclude that CRP should be incorporated as monitoring tools for managing patients with fascial space infections of odontogenic origin. With CRP having an additional advantage of being a sensitive indicator than WBC count, and one of the good measuring tool in determining the control of infection in patients with fascial space infections of odontogenic origin.
Compliance with Ethical Standards
Conflict of interest
None.
References
- 1.Ylyjoki S, Suuronen R, Somer HJ, Meurman JH, Lindqvist C. Differences between patients with or without the need for intensive care due to severe odontogenic infections. J Oral Maxillofac Surg. 2001;59:867–872. doi: 10.1053/joms.2001.25017. [DOI] [PubMed] [Google Scholar]
- 2.Ren YF, et al. Rapid quantitative determination of C-reactive protein at chair side in dental emergency patients. J Tripleo. 2007;104(1):49–55. doi: 10.1016/j.tripleo.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Sann L, et al. Evolution of serum prealbumin, C-reactive protein, and orosomucoid in neonates with bacterial infection. J Pediatr. 1984;105:977–981. doi: 10.1016/S0022-3476(84)80094-3. [DOI] [PubMed] [Google Scholar]
- 4.Sganga, et al. Hepatic protein repriosation after trauma and sepsis. J Surg. 1985;120:189–199. [Google Scholar]
- 5.Sabel KG, Wadsworth C. C-reactive protein in early diagnosis of neonatal septicemia. Acta Paediatr Scand. 1979;68:825–831. doi: 10.1111/j.1651-2227.1979.tb08219.x. [DOI] [PubMed] [Google Scholar]
- 6.Stahl WM. Acute phase protein response to tissue injury. Crit Care Medicine. 1987;15(6):545–550. doi: 10.1097/00003246-198706000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Manelli JC, Badetti C, Golstein MM, Bernard D. A refrence standard for plasma proteins is required for nutritional assessment of adult burn patients. Burns. 1998;24:337–345. doi: 10.1016/S0305-4179(98)00031-X. [DOI] [PubMed] [Google Scholar]
- 8.Ridker PM, et al. Prospective study of C- reactive protein and the risk of future cardiovascular events among apparently healthy women. Circulation. 1998;98:731–733. doi: 10.1161/01.CIR.98.8.731. [DOI] [PubMed] [Google Scholar]
- 9.Pinilla JC, et al. The C-reactive protein to prealbumin ratio correlates with the severity of multiple organ dysfunction. Surgery. 1998;124:799–806. doi: 10.1067/msy.1998.91365. [DOI] [PubMed] [Google Scholar]
- 10.Nagarale G, Ravindra S, Thakur S, Setty S (2010) Efficacy of a chairside diagnostic test kit for estimation of C-reactive protein levels in periodontal disease. J Indian Soc Periodontol 14(4):213–216 [DOI] [PMC free article] [PubMed]
- 11.Malve I. Serum levels of thyroxin binding prealbumin, C-reactive protein and IL-6 in protein- energy undernourished children and normal controls without or with associated clinical infections. J Trop Pediatr. 1998;44:256–262. doi: 10.1093/tropej/44.5.256. [DOI] [PubMed] [Google Scholar]
- 12.Ebersole JL. Systemic acute phase protein reactants, C-reactive protein and hepatoglobin in adult periodontitis. Clin Exp Immunol. 1997;107:347–352. doi: 10.1111/j.1365-2249.1997.270-ce1162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lagrand WL, et al. C-reactive protein as a cardiovascular risk factor. J Am Heart Assoc. 1999;100:96–102. doi: 10.1161/01.cir.100.1.96. [DOI] [PubMed] [Google Scholar]
- 14.Yeun JY, et al. C-reactive protein predicts all-cause and cardiovascular mortality in hemodialysis patients. Am J Kidney Dis. 2000;35(3):469–476. doi: 10.1016/S0272-6386(00)70200-9. [DOI] [PubMed] [Google Scholar]
- 15.Haupt W, et al. Association between preoperative acute phase response and postoperative complications. Eur J Surg. 1997;163:39–44. [PubMed] [Google Scholar]
- 16.Flores JM, et al. C reactive protein as a marker of infection among patients with severe closed trauma. Enferm Infecc Microbiol Clin. 2001;19(2):61–65. doi: 10.1016/S0213-005X(01)72562-1. [DOI] [PubMed] [Google Scholar]
- 17.Sullivan DH, Bopp MM, Roberson PK. Protein-energy undernutrition and life threatening complications among the hospitalized elderly. J Gen Intern Med. 2002;17(12):923–932. doi: 10.1046/j.1525-1497.2002.10930.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ortega O, et al. Significance of C- reactive protein levels in pre-dialysis patients. Nephrol Dial Trans. 2002;17:1105–1109. doi: 10.1093/ndt/17.6.1105. [DOI] [PubMed] [Google Scholar]