The Maternal, Infant, and Early Childhood Home Visiting Program (MIECHV) under the Affordable Care Act has significantly expanded evidence-based home visiting services for pregnant women and new mothers at risk for child maltreatment (Health Resources and Services Administration, 2015). Home visiting (HV) is the most widely used child maltreatment prevention strategy across the country, and typical models provide high-risk parents with education about child development and effective parenting, as well as linkages to childcare, medical, and early intervention services (Azzi-Lessing, 2013). In line with their primary goal of child maltreatment prevention, most HV programs target pregnant women and new mothers with significant behavioral health risks known to be associated with impaired parenting such as substance use and mental health problems. However, the HV workforce is comprised of a wide range of professional and educational backgrounds, with many programs staffed largely by paraprofessionals who lack the necessary clinical training and skills to address challenging behavioral health risks (Paulsell, Del Grosso, & Supplee, 2014). While this discrepancy between client need and workforce qualification has long been recognized, the MIECHV legislation provided new impetus for action to address this mismatch by requiring state HV systems to demonstrate improvement on benchmark outcomes related specifically to maternal mental health (U.S. Department of Health and Human Services, 2014). Consequently, initiatives to bolster HV capacity to address maternal behavioral health have begun to emerge within HV networks.
Much of the work to date in this area has focused on maternal depression (MD), and has included mandated depression screening within HV, providing mental health consultation to home visitors, and integrating mental health treatment into home visits (Ammerman, Putnam, Teeters, & van Ginkel, 2014; Le, Perry, Mendelson, Tandon, & Munoz, 2015; Price, Gray, & Thacker, 2015; Rowan, Duckett, & Wang, 2015; Segre, O'Hara, Brock, & Taylor, 2012; Segre, Stasik, O'Hara, & Arndt, 2010; Tandon, Leis, Mendelson, Perry, & Kemp, 2014; Yonkers et al., 2009). In contrast, maternal substance use (SU) has received comparatively little attention within HV behavioral health initiatives, and is often an exclusion criterion from studies examining the impact of depression interventions (e.g., (Ammerman et al., 2011; Segre et al., 2010)). Maternal SU is a significant risk factor for child maltreatment (Dubowitz et al., 2011), is often co-morbid with depression (Connelly, Hazen, Baker-Ericzen, Landsverk, & McCue Horwitz, 2013), and is prevalent among pregnant and parenting women (Substance Abuse and Mental Health Services Administration, 2014), the population served by HV programs. Expansion of existing behavioral health initiatives within HV to include SU is sorely needed. In order to inform the development of an enhancement to HV aimed at addressing both SU and MD, the current study presents the results of a survey that asked home visitors to report on their current practices, knowledge and perceived self-efficacy, perceived barriers, and training needs regarding SU and MD in their clients. This research emanates from one state network's interest in advancing its practice in addressing maternal behavioral health within HV, and is aligned with the national HV research priorities of supporting the development of a competent workforce and strengthening HV effectiveness (Home Visiting Research Network, 2013).
Importance of Expanding HV Capacity to Address Maternal Substance Use
Expanding HV capacity to address maternal SU in addition to depression is important for several reasons. First, SU is prevalent among mothers served by HV programs and is associated with increased risk for negative outcomes. According to the latest report from the MIECHV national evaluation, nearly 40% of HV clients reported binge drinking or using illegal drugs in the three months prior to program entry (Michalopoulos et al., 2015). Maternal SU during pregnancy and in the early childhood years is associated with increased risk for child maltreatment as well as a host of negative child developmental outcomes (Dubowitz et al., 2011; Institute of Medicine & National Research Council, 2014). Moreover, substance using mothers are at high risk for losing their children to the child protective system (Berger, Slack, Waldfogel, & Bruch, 2010). Home visitors are present in the home during the critical early months, and, with proper training and support, have the potential to identify and address SU and associated problems early, prior to negative impacts on parenting and child outcomes. Second, the presence of client behavioral health risks such as SU has been associated with more difficult engagement in HV and attenuated program impacts (Azzi-Lessing, 2013; Green, Tarte, Harrison, Nygren, & Sanders, 2014). Equipping home visitors with strategies to enhance engagement for high-risk substance using families as well as to assist them in accessing needed treatment could improve outcomes for these families.
Finally, the few studies that have directly assessed home visitor perceptions of their ability to manage client behavioral health risks have found that home visitors feel that they are lacking in important training and practical skills in this area. For example, one study found that home visitors' ability to recognize mental health and SU problems in their clients was generally below 50%, based on a comparison of home visitor records with positive screen data (Duggan et al., 2004). Rates of referral for services were similarly low (Duggan et al., 2007; Jones-Harden, Denmark, & Saul, 2010; Tandon, Parillo, Jenkins, & Duggan, 2005), with one study finding no service linkages for SU, and a linkage rate of only 2% for mental health (Duggan et al., 2004). In a study asking home visitors to report on difficult situations encountered in HV, inability to connect families with needed mental health services and addressing SU were rated as among the most difficult (LeCroy & Whitaker, 2005). Across studies, home visitors reported feeling generally ill-equipped to effectively address these issues with clients (Eddy et al., 2008; Jones-Harden et al., 2010; LeCroy & Whitaker, 2005; Tandon et al., 2005), and required more training and supervision targeted specifically at addressing client behavioral health risks (Tandon, Mercer, Saylor, & Duggan, 2008; Zeanah, Larrieu, Boris, & Nagle, 2006).
Beginning to Address the Need: Existing Behavioral Health Initiatives within HV
It has been suggested for more than a decade that HV programs shift their focus to more directly target maternal behavioral health risk factors for child maltreatment (Chaffin, 2004; Duggan et al., 2004), and there is a growing body of literature documenting attempts to do so (Ammerman et al., 2011; Boris et al., 2006; Chamberlain, 2008; Eddy et al., 2008; Gray & Price, 2014; Segre et al., 2010; Tandon et al., 2014). Nearly all of the attempts to date have focused on MD, and have included teaming paraprofessional home visitors with mental health consultants (Boris et al., 2006), integrating evidence-based mental health interventions, such as cognitive behavioral therapy and interpersonal therapy, into home visits (Ammerman et al., 2014; Gray & Price, 2014; Tandon et al., 2014), and training home visitors to implement brief behavioral health interventions (Segre et al., 2010). Accumulating results from these initiatives have been largely positive, suggesting that enhancing HV with research-supported mental health interventions can be effective in reducing client symptoms of depression (Ammerman et al., 2013; Segre, Brock, & O'Hara, 2015; Tandon et al., 2014). It is yet unknown whether similar impacts could be achieved by integrating interventions targeted at SU into HV programs.
To inform efforts to develop interventions targeting SU within HV, more systematic and comprehensive data are needed on the degree to which paraprofessional home visitors currently address SU in their clients that includes knowledge, current practices, training, and barriers to fully addressing client SU concerns. While several studies have surveyed home visitors on their perceived ability to address client behavioral health risks (e.g.,(Duggan et al., 2004; LeCroy & Whitaker, 2005; Tandon et al., 2008; Tandon et al., 2005)), these studies have generally not focused on SU specifically as distinct from mental health. With a couple of notable exceptions (Duggan et al., 2004; Tandon et al., 2005), studies conducted to date have grouped mental health and SU together into a single category of risk factors for child maltreatment. Additionally, these studies were all conducted prior to the MIECHV legislation and its accompanying emphasis on addressing maternal behavioral health, particularly depression, within HV. Finally, these studies did not assess barriers at both the system-level and client-level that may prevent home visitors from being able to adequately address behavioral health concerns in their clients. Potential systemic barriers that have been shown to prevent access to treatment among pregnant and parenting women include lack of available treatment options, long waiting lists, lack of transportation and childcare, and insurance or other payment difficulties (Green, Rockhill, & Furrer, 2006; Rosen, Tolman, & Warner, 2004). Barriers at the client-level may include stigma, fear of losing custody of their children, fear of confidentiality violation, and prior negative experiences with treatment (Abrams, Dornig, & Curran, 2009; Leis, Mendelson, Perry, & Tandon, 2011; O'Mahen & Flynn, 2008). The current study provides more recent data from home visitors in a single state who reported on their current practices regarding addressing SU and MD in their clients, including screening, referral for treatment, and assisting clients in overcoming common barriers to treatment attendance. Home visitors also reported on their knowledge, perceived self-efficacy, training, and barriers at both the system and client levels regarding addressing client SU and MD. Examination of potential differences in the extent to which home visitors address SU compared to MD across these distinct domains, as well as what may predict these differences, can help inform the development of strategies for supporting HV programs to better address client SU.
Study Goals and Hypotheses
The study goals were (1) to compare the self-reported current practices of home visitors regarding SU and MD in their clients, and (2) to examine the degree to which differences in home visitor current practices regarding SU and MD can be explained by home visitor education, years of experience, prior training, self-reported knowledge of and perceived self-efficacy with the risk area, and home visitor perceptions of barriers at both the system and client levels. Given the recent national focus on enhancing HV to address MD, we hypothesized that home visitors would report more extensive management of MD compared to SU, as defined by their current practices. We also hypothesized that home visitor current practices in both risk areas would be predicted by more education, experience, and training, greater knowledge and perceived self-efficacy with the risk area, and lower perceived system-level and client-level barriers.
Method
This study was reviewed by the governing Institutional Review Board (IRB) and was determined to be exempt from IRB oversight, as it reports on anonymous survey data.
Participants
Study participants included 159 home visitors from the Healthy Families America (HFA; N = 104) or Parents as Teachers (PAT; N = 54) programs in a single northeastern state. Both HFA and PAT are included in the MIECHV list of evidence-based HV models (U.S. Department of Health and Human Services, 2014), and are widely implemented across the country (Donelan-McCall, Eckenrode, & Olds, 2009; Harding, Galano, Martin, Huntington, & Schellenbach, 2007; Zigler, Pfannenstiel, & Seitz, 2008). Home visitors were recruited for participation in an anonymous survey at a mandatory state-wide HV networking meeting (October, 2013) hosted by the umbrella agency responsible for providing training and technical assistance to the state's HV programs. Survey participation was offered to all home visitors attending the meeting and 159 home visitors completed the survey on paper at the networking meeting, representing approximately 85% of the total number of HFA and PAT home visitors in the state at that time.
The study sample was 96% female, 20% White, 22% African American, 50% Latino/a, 3% Multiracial, and 4% of other racial/ethnic background. Education level of home visitors included high school or GED (12%), some college (33%), college graduate (42%), some post-college education (6%) or graduate degree (8%). Home visitors were 36 years old on average (SD = 11.9; Range 20 to 76 years), with an average of 4.25 years of experience as home visitors (SD = 4.30), and 3.25 years working for their current program (SD = 3.58).
Study Measure: Home Visitor Survey
Adaptation of home visitor survey. The survey used in this study is an adapted version of a survey developed in a prior study to assess the management of maternal depression among primary care physicians (Leiferman, Dauber, Heisler, & Paulson, 2008; Leiferman, Dauber, Scott, Heisler, & Paulson, 2010). The conceptual model underlying the physician survey, grounded in the Health Belief and Social Ecological models, posited that the likelihood that physicians will address MD in their practice is impacted by their prior knowledge and training, level of self-efficacy (including confidence and comfort level with the topic), and barriers at the individual and system levels. The physician survey was administered to 217 primary care physicians and exploratory factor analysis was conducted, trimming items until adequate fit was achieved. The final structural model for the physician survey, described in Leiferman and colleagues (Leiferman et al., 2010), demonstrated good fit: (χ2 (71) = 122.006, CFI = .959, TLI = .941, RMSEA = .058). Though the individual and system-level barriers scales were not retained in the final model for the physician survey due to lack of statistical significance in predicting physician practice, we felt it was important to include them in the current study analyses given the different service context being assessed (home visiting vs. primary care) and the importance of examining barriers for informing the design of interventions to address service gaps in the home visiting context.
The process of adapting the physician survey for the home visiting context included the following steps. First, we developed an initial draft of proposed adaptations based on a review of relevant literature, focus groups with home visitors, and discussions with HV program administrators. Second, the adapted item set was reviewed for content validity and accuracy by a panel of researchers, HV supervisors, and HV administrators. Finally, the item set was narrowed based on panel feedback. The majority of items on the final home visitor survey were identical to those on the original physician survey, with the following adaptations made. First, we extended the survey to evaluate SU as well as MD, using parallel items for both constructs. Second, the original physician survey assessed barriers via dichotomous check-boxes, and we converted these to Likert-scale items in the home visitor survey, a modification that was expected to improve the measure's psychometric properties. Third, we adapted the language of several of the barriers items to ensure we were assessing barriers relevant to the home visiting context (e.g., “Clients are afraid that they will lose custody of their children if they admit to feeling depressed/using substances”). Finally, we adapted the training items from the original survey to assess home visitors' training needs to inform intervention design.
The final home visitor survey consisted of 9 demographic items, 35 items on MD, and 36 items on SU1. With one exception, the survey contained parallel items for MD and SU to facilitate comparisons across the two risk domains. Survey respondents were asked to rate the extent of their agreement with a series of statements assessing their knowledge of each risk area, perceived self-efficacy addressing each risk area with clients, and perceived system- and client-level barriers to addressing risk with clients. Each of these items was rated on a 6-point Likert scale ranging from Strongly Disagree to Strongly Agree. Examination of item distributions revealed that most items had few scores at the most extreme ends of the scale. Therefore, prior to conducting factor analysis, the original 6-point response scale was recoded into a 4-point scale, collapsing the two agreement anchors (Strongly Agree and Agree) as well as the two disagreement anchors (Strongly Disagree and Disagree) in order to create more favorable distribution properties for analysis (Nunnally & Bernstein, 1994). The final response scale was: 1=Disagree; 2=Somewhat Disagree; 3=Somewhat Agree; 4=Agree. Eight additional items per risk area assessed home visitors' current practices regarding the frequency with which they assess, screen, refer, follow up, and help clients overcome barriers to treatment for MD and SU. These items were rated on a 5-point Likert scale ranging from Always to Never.
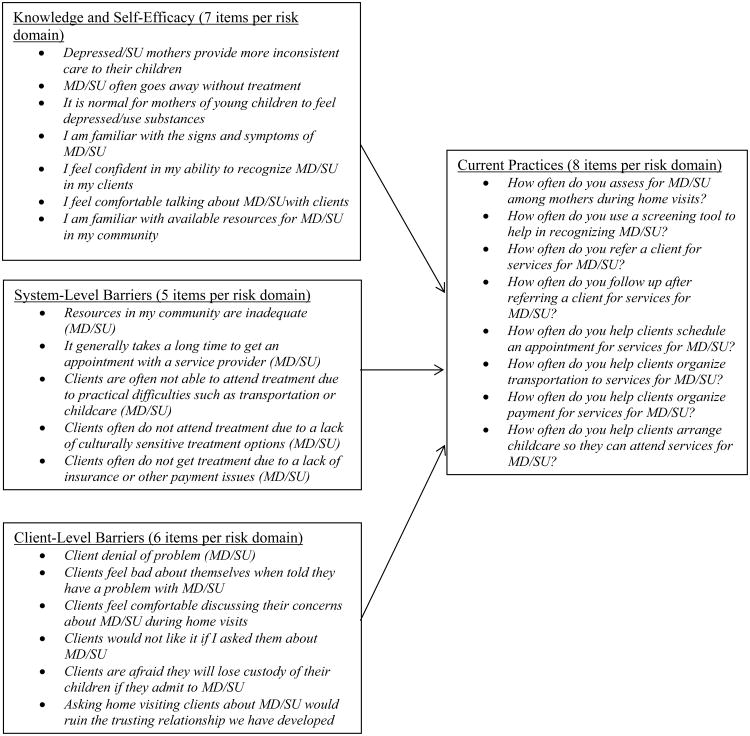
Several additional survey items assessed home visitors' prior training and perceived need for future training in the areas of MD and SU. These items were not included in the Confirmatory Factor Analysis because only a single item assessing prior training was used in the predictive models; thus, there was no need to create a latent factor for training. The items on perceived need for future training are presented to provide additional descriptive information for intervention planning; these were not included in formal analyses. For each risk area, home visitors indicated whether they had ever received any of five types of formal training, including formal coursework, workshops, conferences, seminars, and web-based training. Training was operationalized as the number of types of formal training received for each risk domain (range 0-5). Finally, home visitors rated the extent of their agreement with three statements per risk area regarding their desire for more formal training, desire for standardized procedures for addressing MD and SU within home visiting, and willingness to implement standardized screening for each risk area. These items were rated on a 6-point Likert scale from Strongly Agree to Strongly Disagree. The hypothesized factor structure underlying the survey items is depicted in Figure 1. Based on prior work with the physician survey (Leiferman et al., 2010), we expected that survey items would cluster into four latent scales per risk domain: knowledge and self-efficacy, client-level barriers, system-level barriers, and current practices.
Figure 1.
Hypothesized factor structure underlying the home visitor survey. MD = Maternal Depression; SU = Substance Use.
Confirmatory factor analysis
Confirmatory factor analysis (CFA) was conducted to confirm the hypothesized four-factor structure of the home visitor survey for the purpose of creating valid scales for analysis. Because we were able to construct a viable theoretical factor structure based on the results of the exploratory factor analysis (EFA) conducted on the physician survey (Leiferman et al., 2010), we did not conduct an additional EFA on the home visitor survey. Due to power concerns, all analyses were conducted separately for MD and SU risk domains. CFA proceeded according to the following steps. First, we examined intercorrelations among all items expected to load on each hypothesized latent factor (see Figure 1 for the items expected to load on each factor). On several occasions, there were two items within the same proposed latent factor subscale that were highly correlated with one another. For example, within the proposed knowledge and self-efficacy scale, the item, “I feel confident in my ability to recognize MD/SU in my clients” was highly correlated with “I am familiar with the signs and symptoms of MD/SU” (MD: r = 0.52, p < 0.01; SU: r =0.71, p < 0.01) as well as with “I feel comfortable talking about MD/SU with clients” (MD: r = 0.44, p < 0.01; SU: r = 0.49, p < 0.01). In these instances, the item that was highly correlated with other items was excluded from further analyses. Second, a series of preliminary CFA models was conducted to determine whether the items corresponding to each latent factor adequately loaded on that factor. Poor performing items were trimmed as needed to achieve adequate fit for each model, with adequate fit defined as RMSEA values of .08 and below and CFI values of .90 and above (Browne & Cudeck, 1993). Once adequate fitting models were established for each latent factor, final measurement models were fit for the MD and SU risk domains respectively.
The final CFA measurement models are depicted in Tables 1 (MD) and 2 (SU). For MD, the initial full measurement model did not converge. To achieve model convergence, we freed the first factor loadings on each latent factor and fixed all factor variances to 1 (Nunnally & Bernstein, 1994). The final MD measurement model demonstrated adequate fit: χ2 (146) = 203.81, p < 0.01, CFI = 0.92, RMSEA = 0.05. For SU, the initial full measurement model converged with good fit: χ2 (113) = 220.34, p < 0.001, CFI = 0.96, RMSEA = 0.08.
Table 1. Maternal Depression final CFA measurement model: Item factor loadings and scale internal consistency.
| Estimate | S.E. | Estimate/S.E. | p-value | Cronbach's Alpha | |
|---|---|---|---|---|---|
| Factor 1: Knowledge and Self-Efficacy | 0.05 | ||||
| Depressed mothers provide more inconsistent care to their children. | -0.18 | 0.09 | -1.91 | 0.06 | |
| Maternal depression often goes away without treatment. | -0.24 | 0.10 | -2.45 | 0.01 | |
| It is normal for mothers of young children to feel depressed. | -0.10 | 0.10 | -1.05 | 0.30 | |
| I am familiar with the signs and symptoms of depression. | 0.26 | 0.10 | 2.58 | 0.01 | |
| I feel comfortable talking about depression with clients. | 0.44 | 0.14 | 3.19 | 0.001 | |
| I am familiar with available mental health resources in my community. | 0.20 | 0.11 | 1.79 | 0.07 | |
| Factor 2: Systems-Level Barriers | 0.50 | ||||
| It generally takes a long time to get an appointment with a mental health professional. | 0.36 | 0.10 | 3.63 | 0.000 | |
| Clients are often not able to attend treatment for maternal depression due to practical difficulties such as transportation or childcare. | 0.72 | 0.11 | 6.67 | 0.000 | |
| Clients often do not attend treatment for maternal depression due to a lack of culturally sensitive treatment options | 0.70 | 0.09 | 7.76 | 0.000 | |
| Clients often do not get treatment for maternal depression due to a lack of insurance or other payment issues. | 0.65 | 0.11 | 6.03 | 0.00 | |
| Factor 3: Client-Level Barriers | 0.66 | ||||
| Clients often deny feeling depressed. | 0.66 | 0.08 | 8.65 | 0.000 | |
| Clients feel bad about themselves when told they have depression. | 0.58 | 0.08 | 7.74 | 0.000 | |
| Clients would not like it if I asked them about depression symptoms. | 0.65 | 0.07 | 9.22 | 0.000 | |
| Clients are afraid that they will lose custody of their children if they admit to feeling depressed. | 0.60 | 0.08 | 7.90 | 0.000 | |
| Asking clients about depression would ruin the trusting relationship we have developed. | 0.58 | 0.10 | 5.63 | 0.000 | |
| Factor 4: Current Practices | 0.84 | ||||
| Refer clients for treatment of maternal depression. | 0.72 | 0.05 | 15.82 | 0.000 | |
| Follow up after referring a client for treatment of maternal depression. | 0.71 | 0.06 | 12.67 | 0.000 | |
| Help clients schedule appointments for treatment for maternal depression. | 0.90 | 0.03 | 27.23 | 0.000 | |
| Help clients overcome barriers to treatment for maternal depression (e.g., transportation, payment, childcare). | 0.81 | 0.05 | 16.85 | 0.000 |
Note. χ2 (146) = 203.81, p < 0.01; RMSEA = 0.05 (90% CI: 0.03, 0.07), p = 0.49; CFI = 0.92; TLI = 0.90.
Factor variances fixed at one.
Table 2. Substance use final CFA measurement model: Item factor loadings and scale internal consistency.
| Estimate | S.E. | Estimate/S.E. | p-value | Cronbach's Alpha | |
|---|---|---|---|---|---|
| Factor 1: Knowledge and Self-Efficacy | 0.47 | ||||
| Some amount of getting high is normal in mothers of young children and does not interfere with parenting. | 0.21 | 0.13 | 1.59 | 0.11 | |
| I am familiar with the signs and symptoms of substance use problems. | 0.59 | 0.10 | 6.02 | 0.000 | |
| I feel comfortable talking about substance use with clients. | 0.39 | 0.10 | 3.90 | 0.000 | |
| I am familiar with available substance use treatment resources in my community. | 0.84 | 0.09 | 8.93 | 0.000 | |
| Factor 2: Systems-Level Barriers | 0.68 | ||||
| It generally takes a long time to get an appointment at a substance use treatment program | 0.41 | 0.09 | 4.80 | 0.000 | |
| Clients are often not able to attend treatment for substance use due to practical difficulties such as transportation or childcare. | 0.80 | 0.05 | 15.11 | 0.000 | |
| Clients often do not attend treatment for substance use due to a lack of culturally sensitive treatment options | 0.76 | 0.05 | 14.11 | 0.000 | |
| Clients often do not get treatment for substance use due to a lack of insurance or other payment issues. | 0.77 | 0.06 | 12.07 | 0.000 | |
| Factor 3: Client-Level Barriers | 0.52 | ||||
| Clients often deny that their substance use is a problem. | 0.45 | 0.11 | 4.22 | 0.000 | |
| Clients feel bad about themselves when told they have a substance use problem. | 0.36 | 0.11 | 3.39 | 0.001 | |
| Clients would not like it if I asked them about their substance use. | 0.78 | 0.08 | 9.40 | 0.000 | |
| Clients are afraid that they will lose custody of their children if they admit to using substances. | 0.43 | 0.10 | 4.34 | 0.000 | |
| Asking clients about substance use would ruin the trusting relationship we have developed. | 0.70 | 0.08 | 8.85 | 0.000 | |
| Factor 4: Current Practices | 0.91 | ||||
| Refer clients for treatment of substance use. | 0.90 | 0.02 | 49.35 | 0.000 | |
| Follow up after referring a client for treatment of substance use. | 0.85 | 0.03 | 29.82 | 0.000 | |
| Help clients schedule appointments for treatment for substance use. | 0.94 | 0.01 | 65.10 | 0.000 | |
| Help clients overcome barriers to treatment for substance use (e.g., transportation, payment, childcare). | 0.94 | 0.02 | 41.68 | 0.000 |
Note. χ2 (113) = 220.34, p < 0.01; RMSEA = 0.08 (90% CI: 0.06, 0.09), p < 0.01; CFI = 0.96; TLI = 0.95.
For both MD and SU, the final models included the following four factors: Knowledge and Self-Efficacy, System-Level Barriers, Client-Level Barriers, and Current Practices. The Knowledge and Self-Efficacy scale included 6 items for MD and 4 items for SU. For MD, factor loadings were below 0.40 for all items except for one (“I feel comfortable talking about depression with clients”), and Cronbach's alpha for the scale was very low (α = 0.05). For the SU Knowledge and Comfort scale, two items had factor loadings above 0.40, and Cronbach's alpha for the scale was 0.47. Despite low evidence of internal consistency for both MD and SU, this scale was retained for three main reasons. First, this scale demonstrated good fit in the preliminary CFA models for both MD (χ2 (9) = 8.91, p = 0.45, CFI = 1.00, RMSEA = 0.00; 90% CI: 0.00 – 0.09) and SU (χ2 (2) = 0.34, p = 0.85, CFI = 1.00, RMSEA = 0.00; 90% CI: 0.00 – 0.09). Second, despite the modest factor loadings in the final measurement models, inclusion of these scales did not detract from the overall good fit of the full measurement model for both MD and SU. Finally, knowledge and self-efficacy were important constructs in the conceptual model underlying the survey, and assessing the contribution of home visitor knowledge and self-efficacy to their current practices in order to inform intervention development was an important study goal, so the scales were retained on substantive grounds.
System-Level Barriers included 4 items each for MD and SU. For MD, factor loadings were at or above 0.65 for all items except one (“It generally takes a long time to get an appointment with a mental health professional”), and alpha was adequate at 0.50. For SU, all items had factor loadings above 0.40, with three out of the four items loading above 0.75. This scale showed good internal consistency for SU (α = 0.68). Client-Level Barriers included 5 items each for MD and SU. For MD, factor loadings ranged from 0.58 for “Clients feel bad about themselves when told they have depression,” and “Asking clients about depression would ruin the trusting relationship we have developed,” to 0.66 for “Clients often deny feeling depressed.” Factor loadings were somewhat lower for SU, however all but one item had loadings above 0.40 (“Clients feel bad about themselves when told they have a substance use problem”), and two items had loadings above 0.70. Internal consistency for the Client-Level Barriers scale was good for MD (α = 0.66) and adequate for SU (α = 0.52).
The final scale, Current Practices, included four items each for MD and SU. The three items in the original scale that measured specific ways home visitors helped clients overcome barriers to treatment (“How often do you help clients organize transportation”; “How often do you help clients organize payment”; “How often do you help clients arrange childcare”) were combined into a single item by averaging the scores on the three items in the original scale. This was done due to high levels of collinearity among these three items that was contributing to poor fit in the CFA. All items on the final Current Practices scale for MD and SU had factor loadings above 0.70, and internal consistency was very high for both MD (α = 0.84) and SU (α = 0.91).
Scale scores for each latent factor were calculated by averaging the scores for all items loading on the corresponding factor. The resulting scale scores for Current Practices, Knowledge and Self-Efficacy, System-Level Barriers, and Client-Level Barriers were then used as the independent and dependent variables in study analyses.
Data Analysis Plan
First, paired samples t-tests were conducted on the four survey subscales (Current Practices, Knowledge and Self-Efficacy, System-Level Barriers, and Client-Level Barriers) to examine differences between SU and MD. Next, predictors of home visitors' Current Practices were assessed via two linear regression models, one for SU and one for MD. Full models were conducted including all potential predictors (education, training, experience, Knowledge and Self-Efficacy, System-Level Barriers, and Client-Level Barriers). Finally, descriptive statistics on home visitors' desire for additional formal training, desire for standardized procedures within home visiting, and willingness to implement standardized screening for the two risk areas are presented to inform the extent to which home visitors are open to training and practice enhancement in these areas.
Results
Preliminary Descriptive Statistics
Descriptive statistics on all study variables are contained in Table 3. As shown in the table, approximately half of the sample had graduated from college (55.3%), and about a third had more than five years of experience in HV, another third had between two and five years of experience, and 35% had less than one year of experience in HV. Home visitors reported receiving an average of about one type of formal training in MD or SU. Average scores on the Knowledge and Self-Efficacy scale were 3.03 (SD = 0.35) for MD and 2.84 (SD = 0.47) for SU, out of a possible range of 1 to 4, with higher scores representing greater knowledge and comfort. Regarding MD, average scores for System-Level Barriers (M = 3.34, SD = 0.57) were higher than those for Client-Level Barriers (M = 2.64, SD = 0.59). For SU, home visitors reported about the same level of System-Level Barriers (M = 3.05, SD = 0.72) and Client-Level Barriers (M = 3.19, SD = 0.44). For both barriers scales, possible scores ranged from 1 to 4, with higher scores representing more perceived barriers. The average score on MD Current Practices was 3.11 (SD = 1.00), which corresponds to “sometimes” on the response scale, and the average score on SU Current Practices was 2.37 (SD = 1.18), corresponding to “rarely” on the response scale.
Table 3. Descriptive statistics on all study variables.
| Mean (SD) or N (%) | |
|---|---|
| College graduate (N, %) | 88 (55.3%) |
| Up to one year experience in home visiting (N, %) | 56 (35.2%) |
| Two to five years of experience in home visiting (N, %) | 48 (30.2%) |
| More than five years of experience in home visiting (N, %) | 50 (31.4) |
| Number of types of formal depression training received (M, SD) | 1.30 (1.03) |
| Number of types of formal substance use training received (M, SD) | 1.11 (1.11) |
| Maternal Depression knowledge and self-efficacy (M, SD) | 3.03 (0.35) |
| Substance Use knowledge and self-efficacy (M, SD) | 2.84 (0.47) |
| Maternal Depression system level barriers (M, SD) | 3.34 (0.57) |
| Substance Use system level barriers (M, SD) | 3.05 (0.72) |
| Maternal Depression client level barriers (M, SD) | 2.64 (0.59) |
| Substance Use client level barriers (M, SD) | 3.19 (0.44) |
| Maternal Depression current practices (M, SD) | 3.11 (1.00) |
| Substance Use current practices (M, SD) | 2.37 (1.18) |
Bivariate correlations among all potential predictor variables were examined to assess for multicollinearity prior to conducting regression analyses. Being a college graduate was significantly correlated with having less than one year of HV experience (r = 0.45, p<0.01), and with less Knowledge and Self-Efficacy with SU (r = -0.26, p < 0.01). Having more than five years of experience in HV was associated with having more formal training in both MD (r = -0.20, p < 0.05) and SU (r = -0.24, p < 0.01). More training in SU was associated with greater Knowledge and Self-Efficacy regarding SU (r = 0.29, p < 0.01); however, this was not the case for MD. For MD, greater perceived Client-Level Barriers was associated with less Knowledge and Self-Efficacy (r = -0.23, p < 0.01) and more System-Level Barriers (r = 0.21, p < 0.01). For SU, greater perceived Client-Level Barriers was associated with fewer perceived System-Level Barriers (r = -0.25, p < 0.01). All significant correlations were in the low to moderate range, and thus did not pose issues of multicollinearity for the regression analyses.
Comparison of MD and SU on Survey Subscales
Paired samples t-tests were conducted to compare home visitor scores on Current Practices, Knowledge and Self-Efficacy, System-Level Barriers, and Client-Level Barriers across the two risk domains (MD and SU). Significant differences between the two risk domains were found for Current Practices (t (155) = 10.94, p < 0.001, d = 0.89), Knowledge and Self-Efficacy (t (158) = 4.30, p < 0.001, d = 0.35), System-Level Barriers (t (158) = 5.30, p < 0.001, d = 0.43), and Client-Level Barriers (t (158) = -13.23, p < 0.001, d = 1.08). Means and standard deviations for each subscale by risk domain are presented in Table 3. Scores on Current Practices, Knowledge and Self-Efficacy, and System-Level Barriers were significantly higher for MD compared to SU, and Client-Level Barriers were higher for SU compared to MD. Following the guidelines established by Cohen for the interpretation of effect size magnitude (Cohen, 1988), effect sizes were large for Current Practices and Client-Level Barriers and small to moderate for Knowledge and Self-Efficacy and System-Level Barriers.
Potential Predictors of Home Visitor Current Practices in MD and SU
Linear regressions were conducted to examine potential predictors of home visitor Current Practices in managing MD and SU (see Table 4). A separate regression was conducted for each risk domain. Potential predictors included: college graduate (yes vs. no); up to one year experience in home visiting (vs. more than five years); two to five years of experience in home visiting (vs. more than five years); number of types of formal training received in MD or SU (range 0 to 5); Knowledge and Self-Efficacy scale score; System-Level Barriers scale score; and Client-Level Barriers scale score.
Table 4. Predictors of home visitor current practices in managing depression and substance use.
| Maternal Depressiona | Substance Useb | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| B (SE) | B | t | B (SE) | B | t | |
|
|
||||||
| College graduate | -0.14 (1.01) | -0.07 | -0.78 | 0.21 (0.22) | 0.09 | 0.96 |
| Training | 0.26 (0.08) | 0.27 | 3.30*** | 0.17 (0.09) | 0.16 | 1.84ψ |
| Up to one year experience | -0.14 (0.22) | -0.07 | -0.61 | -0.48 (0.26) | -0.19 | -1.82 ψ |
| 2-5 years experience | 0.18 (0.20) | 0.09 | 0.93 | -0.14 (0.23) | -0.06 | -0.60 |
| Knowledge and self-efficacy | 0.55 (0.24) | 0.19 | 2.32* | 0.56 (0.21) | 0.22 | 2.62** |
| System-level barriers | 0.06 (0.14) | 0.03 | 0.42 | 0.13 (0.13) | 0.08 | 1.00 |
| Client-level barriers | 0.02 (0.14) | 0.01 | 0.13 | -0.18 (0.22) | -0.07 | -0.82 |
Note.
R2 = 0.16, Adjusted R2 = 0.12.
R2 = 0.14, Adjusted R2 = 0.10.
p<0.10,
p<0.05,
p<0.01
For MD, higher scores on the Current Practices scale were predicted by more types of formal depression training (B (SE) = 0.26 (0.08), p < 0.01, β = 0.27) and higher scores on the Knowledge and Self-Efficacy subscale (B (SE) = 0.55 (0.24), p < 0.05, β = 0.19). For SU, higher scores on the Current Practices scale were significantly predicted only by higher scores on the Knowledge and Self-Efficacy scale (B (SE) = 0.56 (0.21), p < 0.05, β = 0.22). Both training and experience predicted SU Current Practices at a trend-level, with more training (B (SE) = 0.17 (0.09), p = 0.07, β = 0.16) and more than five years of experience (compared to less than one year) (B (SE) = -0.48 (0.26), p = 0.07, β = -0.19) associated with higher scores on SU Current Practices.
Home Visitor Openness to Practice Enhancements Focused on MD and SU within HV
Home visitors reported on their desire for additional formal training, desire for standardized procedures within HV to address SU and MD, and willingness to use a standardized screening tool with their clients. These data are presented here descriptively to further inform intervention planning in this area. The vast majority of home visitors reported a desire for more formal training in MD (80.4%) and SU (84.6%). Additionally, more than 70% either agreed or strongly agreed with the statement “I wish there were standard procedures for dealing with MD/SU within HV” (71.4% for MD, 77.4% for SU). Finally, more than 80% expressed willingness to use a standardized screening tool to help them recognize MD (84.8%) or SU (83.3%) in HV clients.
Discussion
This study presents results of a survey of home visitors within a single state who self-reported on their practices in managing (identifying and addressing) client SU and MD within the context of two widely used and empirically supported HV models. As expected given the current emphasis on MD under MIECHV, home visitors reported managing MD more extensively than SU. However, the extent to which home visitors reported currently managing both risk areas corresponded to approximately “rarely” or “sometimes” on the survey response scale. Thus, the degree to which home visitors currently identify and address both SU and MD in their clients is relatively low, by their own report. This finding is consistent with prior studies that found that paraprofessional home visitors infrequently identified and responded to behavioral health risks in their clients (Duggan et al., 2004; Tandon et al., 2005).
Home visitors reported greater knowledge and perceived self-efficacy regarding MD compared to SU. Additionally, they perceived system-level barriers such as long waiting lists, insurance, and lack of transportation and childcare to be greater for MD compared to SU and client-level barriers, including client reluctance to discuss the problem and client fears related to child custody, to be greater for SU compared to MD. The past decade has seen increased recognition of the prevalence of depression among pregnant and postpartum women and the consequent risk posed to family functioning and child development (Goodman et al., 2011; Paulson, Dauber, & Leiferman, 2006). As a result, early childhood intervention systems, including HV programs, have begun to institute policies regarding screening and referral to treatment for MD (Horowitz, Murphy, Gregory, & Wojcik, 2009; Price & Masho, 2014; Rowan et al., 2015; Segre et al., 2012). Thus, home visitors may have had more training and more experience with MD compared to SU, increasing their perceived self-efficacy and decreasing their perception of client-level barriers such as stigma and fear of custody loss. It is possible that increased experience with the mental health treatment system due to the new focus on depression in HV heightened their awareness of systemic barriers to accessing treatment. However, further inquiry is needed to confirm these explanations.
Overall, few predictors of the extensiveness of home visitor management of SU and MD were found in the current study. Greater home visitor reported knowledge and self-efficacy with MD and SU predicted more extensive management of each risk domain respectively, and is consistent with other studies that have found that home visitors' personal comfort level discussing difficult topics impacts whether and how they address them with clients (Rollans, Schmied, Kemp, & Meade, 2013). Additionally, more training was associated with more extensive management of both risk domains, though this was significant only for MD. Surprisingly, home visitor reported system- and client-level barriers did not predict current practices in either of the risk domains in this study. It is possible that factors that were not measured in this study may explain home visitors' practices regarding managing client behavioral health risks. For example, other studies have found that home visitor psychological characteristics, as well as characteristics of the home visitor-client relationship, are important predictors of home visitor behaviors in their work with high-risk families (Jones-Harden et al., 2010). Specifically, home visitor self-reported anxiety has been shown to be associated with the likelihood of addressing sensitive topics with clients, with highly anxious home visitors less likely to address poor mental health in clients (McFarlane et al., 2010). Home visitors may also experience burnout and secondary traumatic stress that often occurs in providers serving high-risk families and may detract from their ability to adequately address clients' needs (Gill, Greenberg, Moon, & Margraf, 2007; Jones-Harden et al., 2010). While these variables were not measured in the current study, they will clearly be important to look at in future studies.
Prior studies have suggested that home visitors lack adequate training to address client behavioral health risks (Duggan et al., 2004; LeCroy & Whitaker, 2005; Tandon et al., 2008). Our findings lend some support to this point, as home visitors with less training reported less extensive management of both MD and SU. However, more than 75% of home visitors in the study sample reported receiving at least one type of formal training in both risk domains, though the quality and intensity of training is not known. Home visitors in the current sample also reported high levels of confidence and perceived self-efficacy addressing both risk domains. Despite this, the majority of home visitors also reported a desire for additional training and for standardized procedures for addressing SU and MD with HV clients. Taken together, study findings largely support the need for interventions to enhance home visitor capacity to address SU and MD in their clients that would include enhanced training coupled with specific practice-based strategies targeted at client behavioral health.
Limitations
This study has several limitations that must be considered in interpreting the findings. First, the study sample was selective, including home visitors representing only two of the myriad HV program models as implemented in a single state, thus generalizability of findings is limited. Second, as indicated above, potential important predictive variables, such as home visitor psychological characteristics, were not measured in this study. Third, although the survey instrument used in this study was not a standardized validated tool, the constructed scales were based on a sound conceptual model used in a prior study (Leiferman et al., 2010) and demonstrated good fit in confirmatory factor analysis. However, further psychometric evaluation would be needed to fully validate the survey as a measurement tool. Finally, all data were self-reported by home visitors and thus present only a single perspective on very complex issues. Recent qualitative research suggests that HV clients' views of their own depressive symptoms and their preferred way of receiving help differs from their home visitors' perceptions (Price & Cohen-Filipic, 2013). Complementary surveys assessing client perspectives as well as perspectives of treatment providers, program supervisors and administrators, and other stakeholders would provide a more complete picture, particularly of the potential barriers to home visitor management of client behavioral health risks and client access to needed services. A larger-scale survey of home visitors, administrators, and clients that includes a larger sample, multiple perspectives on management of behavioral health risks within HV, and a larger spectrum of potential predictive variables is currently underway as part of the MIECHV-funded research program, and will provide further information to guide HV programs in addressing client behavioral health risks.
Implications and Future Directions
Study findings lend further support to several areas of need that have been increasingly stated by HV researchers and other stakeholders. First, HV programs must do more to support home visitors in identifying behavioral health risks such as SU and MD in their clients and promoting access to treatment (Green et al., 2014; Paulsell et al., 2014). MIECHV legislation has already resulted in many local HV programs placing increased emphasis on maternal behavioral health risks (Michalopoulos et al., 2015). In the recently released first report from the national HV evaluation, MIHOPE, more than 90% of HFA home visitors believed it was their responsibility to recognize and address mental health and SU in their clients (Michalopoulos et al., 2015). However, about a quarter of home visitors felt that their programs did not provide them with adequate strategies and tools for addressing these issues and about 30% felt that they were not adequately trained in these areas. In the MIHOPE sample, many local programs reported having formal policies for screening clients for behavioral health needs, however only 20% had systematic protocols for how to respond to positive screens (Michalopoulos et al., 2015). It is being increasingly recognized that home visitors are not routinely equipped with the requisite skills and tools to engage high-risk families, identify specific risk factors, and navigate complex systems to assist families in accessing needed services (Azzi-Lessing, 2013). Second, HV researchers have suggested the need for more intensive and reflective supervision to provide essential support to home visitors in intervening with the highest risk families (Azzi-Lessing, 2013; Jones-Harden et al., 2010). Qualitative studies of home visitor experiences suggest that the day-to-day of working with high-risk families takes an emotional toll, and adequate supervisory support as well as peer support is necessary to prevent burnout (Dmytryshyn, Jack, Ballantyne, Wahoush, & MacMillan, 2015; Gill et al., 2007). Third, systematic consultation with service providers is a high priority, as formal collaborations with mental health and substance use providers are required to adequately meet the needs of high-risk families (Jones-Harden et al., 2010). Because HV alone is not sufficient to adequately address the complex needs of vulnerable families, it must be viewed as one part of a larger, coordinated system of care that includes both child and adult services (Azzi-Lessing, 2013).
As described in the Introduction, there have been several attempts to systematically integrate assessment and treatment for MD into HV programs. Results of these studies support the potential of integrating mental health interventions into HV for reducing client symptoms of depression. Whether or not similar approaches could work for SU is still an open question. Additionally, the approach of delivering behavioral health treatment directly in the home is costly and requires the availability of licensed mental health counselors, resources that are lacking in most statewide HV systems. A potential alternative is the integration of standardized behavioral health screening implemented by home visitors followed by brief intervention aimed at linking clients to needed services. This approach is based on the Screening Brief Intervention and Referral to Treatment (SBIRT) model that is widely used for SU problems in primary care settings (Substance Abuse and Mental Health Services Administration, 2013), and has demonstrated notable success in improving access to treatment and reducing SU for adult substance users, though results are not definitive (Agerwala & McCance-Katz, 2012; Babor et al., 2007). SBIRT has not been systematically attempted and evaluated within HV to date, however, arguably, this approach has potential as a way to address SU and mental health in the HV context. While SBIRT approaches may be more cost-effective than home-based treatment, they would rely on the skill of the home visitor to identify client risks, motivate the client to engage in treatment, and coordinate with service providers to eliminate barriers to treatment access. Additionally, the success of SBIRT is dependent on the availability and accessibility of quality community-based treatment services for home visitors to make referrals to (Babor et al., 2007). To be effective within HV, such an approach must include behavior- and skills-based training for home visitors, collaborative partnerships with behavioral health providers, minimal additional burden, and adequate supervisory practical and emotional support for home visitors (Azzi-Lessing, 2013; Dmytryshyn et al., 2015; Home Visiting Research Network, 2013; Jones-Harden et al., 2010; Tandon et al., 2008). The survey results presented in the current study were used to inform the development of a protocol to integrate standardized screening for SU, as well as for MD and domestic violence, into HV, followed by a brief intervention targeted at motivation and engagement of clients into needed services. A pilot feasibility test of this protocol is currently underway and results will be forthcoming.
Surveys such as the one used in the current study can be helpful in revealing service gaps and the particular barriers at play to inform the development of model enhancements and interventions to increase HV program capacity to address client behavioral health risks. However, additional research is needed that includes the perspectives of clients, administrators, and other stakeholders in addition to home visitors, to elucidate the individual, organizational, and systemic factors that determine how and to what extent maternal behavioral health risks are addressed within HV programs. Such research is being conducted as part of the ongoing national MIECHV-funded HV evaluation, and will be instrumental in informing the development of targeted strategies to expand HV program capacity to better meet the needs of the highest risk families while simultaneously supporting the practical and emotional needs of the HV workforce.
Acknowledgments
Preparation of this article was supported by grant 1R21DA034108 from the National Institute on Drug Abuse. Additional support for this project was provided by the New Jersey Department of Children and Families, the New Jersey Department of Human Services: Division of Family Development, and the New Jersey Department of Health. The authors gratefully acknowledge Anne K. Duggan, ScD, for her guidance in preparing this manuscript.
Footnotes
Note that the original survey also included 30 items on domestic violence that were parallel to the maternal depression and substance use items. However, survey validation analyses did not support the use of the domestic violence scales, so these items are not included in study analyses.
Contributor Information
Sarah Dauber, The National Center on Addiction and Substance Abuse.
Frances Ferayorni, Stony Brook University.
Craig Henderson, Sam Houston State University.
Aaron Hogue, The National Center on Addiction and Substance Abuse.
Jessica Nugent, Prevent Child Abuse New Jersey.
Jeannette Alcantara, Prevent Child Abuse New Jersey.
References
- Abrams LS, Dornig K, Curran L. Barriers to service use for postpartum depression symptoms among low-income ethnic minority mothers in the United States. Qualitative Health Research. 2009;19:535–551. doi: 10.1177/1049732309332794. [DOI] [PubMed] [Google Scholar]
- Agerwala SM, McCance-Katz EF. Integrating Screening, Brief Intervention, and Referral to Treatment (SBIRT) into clinical practice settings: A brief review. Journal of Psychoactive Drugs. 2012;44(4):307–317. doi: 10.1080/02791072.2012.720169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FG, Altaye M, Teeters AR, Stevens J, Van Ginkel JB. Treatment of depressed mothers in home visiting: Impact on psychological distress and social functioning. Child Abuse and Neglect. 2013;37:544–554. doi: 10.1016/j.chiabu.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Stevens J, Bosse NR, Short JA, Bodley AL, Van Ginkel JB. An open trial of in-home CBT for depressed mothers in home visitation. Maternal and Child Health Journal. 2011;15(8):1333–1341. doi: 10.1007/s10995-010-0691-7. doi:0.1007/s10995-010-0691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Teeters AR, van Ginkel JB. Moving Beyond Depression: A collaborative approach to treating depressed mothers in home visiting programs. Zero to Three. 2014;34(5):20–27. [Google Scholar]
- Azzi-Lessing L. Serving highly vulnerable families in home visitation programs. Infant Mental Health Journal. 2013;34(5):376–390. doi: 10.1002/imjh.21399. [DOI] [Google Scholar]
- Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): Toward a public health approach to the management of substance abuse. Substance Abuse. 2007;28:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- Berger LM, Slack KS, Waldfogel J, Bruch SK. Caseworker-perceived caregiver substance abuse and child protective services outcomes. Child Maltreatment. 2010;15(3):199–210. doi: 10.1177/1077559510368305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boris NW, Larrieu JA, Zeanah PD, Nagle GA, Steier A, McNeill P. The process and promise of mental health augmentation of nurse home-visiting programs: Data from the Louisiana Nurse-Family Partnership. Infant Mental Health Journal. 2006;27(1):26–40. doi: 10.1002/imhj.20078. [DOI] [PubMed] [Google Scholar]
- Browne M, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, editors. Testing Structural Models. Newbury Park, CA: Sage Publications; 1993. [Google Scholar]
- Chaffin M. Is it time to rethink Healthy Start/Healthy Families? Child Abuse and Neglect. 2004;28:589–595. doi: 10.1016/j.chiabu.2004.04.004. [DOI] [PubMed] [Google Scholar]
- Chamberlain L. Ten lessons learned in Alaska: Home visitation and intimate partner violence. Journal of Emotional Abuse. 2008;8:205–216. doi: 10.1080/10926790801986130. [DOI] [Google Scholar]
- Cohen JB. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Connelly CD, Hazen A, Baker-Ericzen MJ, Landsverk J, McCue Horwitz S. Is screening for depression in the perinatal period enough? The co-occurrence of depression, substance abuse, and intimate partner violence in culturally diverse pregnant women. Journal of Women's Health. 2013;22(10):844–852. doi: 10.1089/jwh.2012.4121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dmytryshyn AL, Jack SM, Ballantyne M, Wahoush O, MacMillan HL. Long-term home visiting with vulnerable young mothers: An interpretive description of the impact on public health nurses. BMC Nursing. 2015;14:12. doi: 10.1186/s12912-015-0061-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donelan-McCall N, Eckenrode J, Olds D. Home visiting for the prevention of child maltreatment: Lessons learned during the past 20 years. Pediatric Clinics of North America. 2009;56:389–403. doi: 10.1016/j.pcl.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Dubowitz H, Kim J, Black MM, Weisbart C, Semiatin J, Magder LS. Identifying children at high risk for a child maltreatment report. Child Abuse and Neglect. 2011;35:96–104. doi: 10.1016/j.chiabu.2010.09.003. [DOI] [PubMed] [Google Scholar]
- Duggan AK, Caldera D, Rodriguez K, Burrell L, Rohde C, Crowne SS. Impact of a statewide home visiting program to prevent child abuse. Child Abuse and Neglect. 2007;31:801–827. doi: 10.1016/j.chiabu.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Duggan AK, Fuddy L, Burrell L, Higman SM, McFarlane E, Windham A, Sia C. Randomized trial of a statewide home visiting program to prevent child abuse: Impact in reducing parental risk factors. Child Abuse and Neglect. 2004;28:623–643. doi: 10.1016/j.chiabu.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Eddy T, Kilburn E, Chang C, Bullock L, Sharps P DOVE Research Team. Facilitators and barriers for implementing home visit interventions to address intimate partner violence: Town and Gown partnerships. Nursing Clinics of North America. 2008;43(3):419–435. doi: 10.1016/j.cnur.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill S, Greenberg MT, Moon C, Margraf P. Home visitor competence, burnout, support and client engagement. Journal of Human Behavior in the Social Environment. 2007;15(1):23–44. doi: 10.1300/J137v15n01-02. [DOI] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Robbins Broth M, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Gray LA, Price SK. Partnering for mental health promotion: Implementing evidence based mental health services within a maternal and child home health visiting program. Clinical Social Work Journal. 2014;42:70–80. doi: 10.1007/s10615-012-0426-x. [DOI] [Google Scholar]
- Green BL, Rockhill A, Furrer C. Understanding patterns of substance abuse treatment for women involved with child welfare: The influence of the Adoption and Safe Families Act (ASFA) The American Journal of Drug and Alcohol Abuse. 2006;32:149–176. doi: 10.1080/00952990500479282. [DOI] [PubMed] [Google Scholar]
- Green BL, Tarte JM, Harrison PM, Nygren M, Sanders MB. Results from a randomized trial of the Healthy Families Oregon accredited statewide program: Early program impacts on parenting. Children and Youth Services Review. 2014;44:288–298. doi: 10.1016/j.childyouth.2014.06.006. [DOI] [Google Scholar]
- Harding K, Galano J, Martin J, Huntington L, Schellenbach CJ. Healthy Families America effectiveness: A comprehensive review of outcomes. Journal of Prevention and Intervention in the Community. 2007;34:149–179. doi: 10.1300/J005v34n01_08. [DOI] [PubMed] [Google Scholar]
- Health Resources and Services Administration. The Maternal Infant, and Early Childhood Home Visiting Program: Partnering with Parents to Help Children Succeed. 2015 Retrieved 04/01/15, from mchb.hrsa.gov/programs/homevisiting/programbrief.pdf.
- Home Visiting Research Network. National Home Visiting Research Agenda. 2013 Retrieved 03_12_15, from http://hvrn.org/uploads/3/2/1/0/3210553/home_visiting_research_agenda_2013_10_20_final.pdf.
- Horowitz JA, Murphy CA, Gregory KE, Wojcik J. Community-based postpartum depression screening: Results from the CARE study. Psychiatric Services. 2009;60(11):1432–1434. doi: 10.1176/appi.ps.60.11.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine, & National Research Council. New Directions in Child Abuse and Neglect Research. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- Jones-Harden B, Denmark N, Saul D. Understanding the needs of staff in Head Start programs: The characteristics, perceptions, and experiences of home visitors. Children and Youth Services Review. 2010;32(3):371–379. doi: 10.1016/J.childyouth.2009.10.008. [DOI] [Google Scholar]
- Le H, Perry DF, Mendelson T, Tandon SD, Munoz RF. Preventing perinatal depression in high risk women: Moving the Mothers and Babies Course from clinical trials to community implementation. Maternal Child Health Journal. 2015;19:2102–2110. doi: 10.1007/s10995-015-1729-7. [DOI] [PubMed] [Google Scholar]
- LeCroy CW, Whitaker K. Improving the quality of home visitation: An exploratory study of difficult situations. Child Abuse and Neglect. 2005;29:1003–1013. doi: 10.1016/j.chiabu.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Leiferman JA, Dauber S, Heisler K, Paulson JF. Primary care physicians' beliefs and practices towards maternal depression. Journal of Women's Health. 2008;17(7):1–8. doi: 10.1089/jwh.2007.0543. [DOI] [PubMed] [Google Scholar]
- Leiferman JA, Dauber S, Scott K, Heisler K, Paulson JF. Predictors of maternal depression management among primary care physicians. Depression Research and Treatment. 2010 doi: 10.1155/2010/671279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leis JA, Mendelson T, Perry DF, Tandon SD. Perceptions of mental health services among low-income perinatal African-American women. Women's Health Issues. 2011;21(4):314–319. doi: 10.1016/j.whi.2011.03.005. [DOI] [PubMed] [Google Scholar]
- McFarlane E, Burrell L, Fuddy L, Tandon SD, Derauf DC, Leaf P, Duggan A. Association of home visitors' and mothers' attachment style with family engagement. Journal of Community Psychology. 2010;38(5):541–556. doi: 10.1002/jcop.20380. [DOI] [Google Scholar]
- Michalopoulos C, Lee H, Duggan A, Lundquist E, Tso A, Crowne S, et al. Knox V. The Mother and Infant Home Visiting Program Evaluation: Early Findings on the Maternal, Infant, and Early Childhood Home Visiting Program. Washington, DC: Office of Planning, Research, and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2015. [Google Scholar]
- Nunnally J, Bernstein L. Psychometric Theory. New York: McGraw Hill; 1994. [Google Scholar]
- O'Mahen HA, Flynn HA. Preferences and perceived barriers to treatment for depression during the perinatal period. Journal of Women's Health. 2008;17(8):1301–1309. doi: 10.1089/jwh.2007.0631. [DOI] [PubMed] [Google Scholar]
- Paulsell D, Del Grosso P, Supplee L. Supporting replication and scale-up of evidence-based home visiting programs: Assessing the implementation knowledge base. American Journal of Public Health. 2014;104(9):1624–1632. doi: 10.2105/AJPH.2014.301962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of maternal and paternal depression on parenting behavior. Pediatrics. 2006;118(2):659–668. doi: 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- Price SK, Cohen-Filipic K. Daily life or diagnosis? Dual perspectives on perinatal depression within maternal and child health home visiting. Social Work in Public Health. 2013;28(6):554–565. doi: 10.1080/19371918.2011.592087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price SK, Gray LA, Thacker LR. Enhanced Engagement: An intervention pilot for mental health promotion among low-income women in a community home visiting program. Best Practices in Mental Health. 2015;11(1):69–82. [Google Scholar]
- Price SK, Masho SW. What does it mean when we screen? A closer examination of perinatal depression and psychosocial risk screening within one MCH home visiting program. Maternal Child Health Journal. 2014;18:765–771. doi: 10.1007/s10995-013-1317-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollans M, Schmied V, Kemp L, Meade T. Negotiating policy in practice: Child and family health nurses' approach to the process of postnatal psychosocial assessment. BMC Health Services Research. 2013;13:133–145. doi: 10.1186/1472-6963-13-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen D, Tolman RM, Warner LA. Low-income women's use of substance abuse and mental health services. Journal of Health Care for the Poor and Underserved. 2004;15(2):206–219. doi: 10.1353/hpu.2004.0028. [DOI] [PubMed] [Google Scholar]
- Rowan PJ, Duckett SA, Wang JE. State mandates regarding postpartum depression. Psychiatric Services. 2015;66(3):324–328. doi: 10.1176/appi.ps.201300505. [DOI] [PubMed] [Google Scholar]
- Segre LS, Brock RL, O'Hara MW. Depression treatment for impoverished mothers by point-of-care providers: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2015;83(2):314–324. doi: 10.1037/a0038495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segre LS, O'Hara MW, Brock RL, Taylor D. Depression screening of perinatal women by the Des Moines Healthy Start project: Program description and evaluation. Psychiatric Services. 2012;63(3):250–255. doi: 10.1176/appi.ps.201100247. [DOI] [PubMed] [Google Scholar]
- Segre LS, Stasik SM, O'Hara MW, Arndt S. Listening Visits: An evaluation of the effectiveness and acceptability of a home-based depression treatment. Psychotherapy Research. 2010;20(6):712–721. doi: 10.1080/10503307.2010.518636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Systems-Level Implementation of Screening Brief Intervention, and Referral to Treatment. Rockville, MD: SAMHSA; 2013. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-48, HHS Publication No (SMA) 14-4863. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- Tandon SD, Leis JA, Mendelson T, Perry DF, Kemp K. Six-month outcomes from a randomized controlled trial to prevent perinatal depression in low-income home visiting clients. Maternal and Child Health Journal. 2014;18:873–881. doi: 10.1007/S10995-013-1313-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon SD, Mercer CD, Saylor EL, Duggan AK. Paraprofessional home visitors' perspectives on addressing poor mental health, substance abuse, and domestic violence: A qualitative study. Early Childhood Research Quarterly. 2008;23:419–428. doi: 10.1016/j.ecresq.2008.02.002. [DOI] [Google Scholar]
- Tandon SD, Parillo KM, Jenkins MA, Duggan AK. Formative evaluation of home visitors' role in addressing poor mental health, domestic violence, and substance abuse among low-income pregnant and parenting women. Maternal and Child Health Journal. 2005;9(3):273–283. doi: 10.1007/S10995-005-0012-8. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. The Maternal, Infant, and Early Childhood Home Visiting (MIECHV) Program: Summary of Benchmark Measures Selected by Grantees. 2014 Retrieved 04/01/15, from http://mchb.hrsa.gov/programs/homevisiting/ta/resources/summarybenchmarkmeasures.pdf.
- Yonkers KA, Smith MV, Lin H, Howell HB, Shao L, Rosenheck RA. Depression screening of perinatal women: An evaluation of the Healthy Start Depression Initiative. Psychiatric Services. 2009;60:322–328. doi: 10.1176/appi.ps.60.3.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah CH, Larrieu JA, Boris NW, Nagle GA. Nurse home visiting: Perspectives from nurses. Infant Mental Health Journal. 2006;27(1):41–54. doi: 10.1002/imhj.20079. [DOI] [PubMed] [Google Scholar]
- Zigler E, Pfannenstiel JC, Seitz V. The Parents as Teachers program and school success: A replication and extension. Journal of Primary Prevention. 2008;29:103–120. doi: 10.1007/s10935-008-0132-1. [DOI] [PubMed] [Google Scholar]