Abstract
Traumatic brain injury (TBI) occurs when a blow or jolt to the head or a penetrating injury results in damage to the brain. It is the most frequent cause of hospitalization in young people with a higher prevalence in men. TBI is the leading cause of disability and mortality between the ages 1 and 45. TBI can be caused either by the direct result of trauma or due to a complication of the primary injury. The most common etiological factors for TBI are falls, road traffic accidents, violent physical assaults, and injuries associated with athletic activities. Following TBI, significant neurologic complications may occur which include seizures, dementia, Alzheimer's disease, and cranial nerve injuries. In addition, people may suffer from various psychiatric complications such as depression, posttraumatic stress disorder, generalized anxiety disorder, obsessive-compulsive disorder, and other cognitive and behavioral sequel that might significantly increase the comorbidity of the victims. Considering all of the above complications, TBI is one of the significant public health burdens. Literature has shown that only about 25% of people achieve long-term functional independence following TBI. In this paper, we focused not only on the epidemiology but also the etiology, complications following TBI and understanding their underlying pathogenesis. Further, we focused on analyzing the options to improve the treatment and rehabilitation following TBI in future.
Keywords: Neuropsychiatric, rehabilitation, traumatic brain injury
EPIDEMIOLOGY
Traumatic brain injury (TBI) primarily refers to the brain dysfunction caused by external trauma. There are many forms of traumatic injuries occurring around the globe, of which TBI is a major controversial health issue in today's society. To start with, children while playing sports at a younger age, a rising number of TBIs are taking place which can result in lifelong consequences. The U.S. emergency forces treat an estimated 135,000 sports and recreation-related TBIs per year, among children ages 5–18.[1] High school football players alone sustain 100,000 full-blown, diagnosed concussions per year while girls’ soccer accounts for nearly 12% of total team sports concussions compared to 6.6% for boys’ soccer.[2] However, TBIs can affect anyone at any age and may lead to severe complications and disabilities in the future. TBIs not only have an effect on the patients but also immensely affect families and friends. Risk factors that aggravate traumatic outcome are age, diseases, existing tumor, repeated trauma, and alcohol abuse.
Annually, 10 million people are affected by TBI all over the world, of which 5.3 million people are from the United States.[3,4] Every year around 52,000 people dies from TBI. In addition, every year 100,000 new disabilities emerge from TBI.[5] The total population suffering from long-term consequences of TBI is around 2.5 million to 6.5 million.[6] Falls are the most common reason for sustaining TBI in children aged 0–4 years and adults aged 75 years or older. According to the Centers for Disease Control and Prevention (CDC), falls contribute to 40.5% of the total TBI; other common causes are motor vehicle accidents 14.3%, struck by/against injuries 15.5%, assault 10.7%, and unknown 19%. According to the CDC 2001–2010, TBI rates were 29% higher in males compared to females in 2010. Alcohol use is a major factor leading to brain injury. Blood alcohol concentration was found to be positive in 56% of the victims.[7]
According to the CDC 2012, the economic cost of medical care of brain injury is staggeringly high: An estimate of lifetime (direct and indirect) costs of medical care and lost wages/productivity of patients with TBI is estimated to be $76.5 billion.[8] The financial burden is further enhanced when victims become vulnerable to neurological diseases such as seizures, epilepsy, dementia, and Alzheimer's disease.[9,10] In addition to the neurological complications of TBI, psychological, cognitive, behavioral, and social impairments result in a significant problem. Approximately, 75% of the patients suffer from mild injuries known as concussions and most of the patients with concussions never seek medical help. As a result, most of the injuries never get diagnosed.[11,12] Therefore, the true cost and impact of TBI may be much higher than the present estimated cost.
Male adolescents, young adults ages 15–24, children ages 5 and younger, and elderly ages 75 years and older are most at risk for TBIs.[13] Since most of the patients who suffer from TBI are at a younger age group, they may require prolonged rehabilitation due to a longer period of disability.
PATHOPHYSIOLOGY AND POTENTIAL COMPLICATIONS OF TRAUMATIC BRAIN INJURY
There are many different types of TBIs: concussions (short loss of consciousness in response to a head injury); penetrating injuries (foreign object enters the brain); closed head injuries (blow to the head, skull is closed); skull fractures (bone fractures or breaks); hematomas (bleeding in the brain); lacerations (tearing of blood vessels or tissue); anoxia (absence of oxygen supply to a tissue); contusions (bruising of brain tissue); and diffuse axonal injuries, which lead to a breakdown of neuronal connections.
Concussions are the most prevalent type of TBI. According to the CDC 2005, the number of children who visited the emergency room for treatment for concussion was twice more than the number in 1997. Concussions remain prevalent among athletes, who have an increased risk of repeated injury. Similarly, boxing may cause concussions from a blow to the head by a fist, causing the tear of bridging veins (subdural hematoma), microhemorrhages in the brain, and diffuse axonal injury.[14]
Pathological studies of coma patients with diffuse axonal injuries tested through CT scans showed widespread white matter axonal damage.[14] Diffuse axonal injuries result from severe acceleration or deceleration of the head. Patients who have sustained severe diffuse axonal injuries are typically unconscious from the moment of impact. They do not experience lucid interval; instead, patients remain unconscious or severely disabled until death. Even if patients survive diffuse axonal injuries, persistent neurologic deficits remain throughout their lives. Macroscopic appearance demonstrates focal lesion in the corpus callosum, which appears as clusters of petechial hemorrhages and could lead to intraventricular hemorrhage. TBIs also involve petechial hemorrhages in the brainstem. More severe damage results in hemorrhagic softening of the dorsal part of the midbrain. Long-term survivors of diffuse axonal injury typically show marked cerebral atrophy, dilatation of the lateral and third ventricle, and thinning of the corpus callosum. Microscopic appearance showed diffuse damage to axons in the corpus callosum, superior parasagittal cerebral white matter, brainstem, and various tracts.[15]
TBI patients should be stabilized to prevent further injury. Receiving proper oxygen supply, maintaining adequate blood flow, and controlling blood pressure are all crucial variables in the management of a traumatic injury. The Glasgow Coma Scale, which ranges from 0 to 15 is used to determine the patient's TBI severity. Range: 13–15 corresponds to mild TBI symptoms, 9–12 correlates to moderate disability, 3–8 corresponds to severe disability, and <3 correlates to a vegetative state and finally death.[16] About half of the injured patients require surgery to repair brain tissue and treat other injuries.[13]
The most common short-term complications associated with TBIs include cognitive impairment, difficulties with sensory processing and communication, immediate seizures, hydrocephalus, cerebrospinal fluid (CSF) leakage, vascular or cranial nerve injuries, tinnitus, organ failure, and polytrauma.[17] Polytrauma may include pulmonary, cardiovascular, gastrointestinal dysfunction, fluid and hormonal imbalances, deep vein thrombosis, excessive blood clotting, and nerve injuries. TBI patients tend to have increased metabolic rate, which leads to an excessive amount of heat produced within the body. Brain swelling occurs secondary to TBI and contributes to increased intracranial pressure as a result of cerebral vasodilatation and increased cerebral blood flow. Long-term complications associated with TBIs include Parkinson's disease, Alzheimer's disease, dementia pugilistica, and posttraumatic epilepsy.
Following TBI, there are acute changes in the neurotransmitters which lead to psychiatric manifestations by altering the levels of acetylcholine, norepinephrine, dopamine, and serotonin. Pharmacological drugs can be used to modify these neurotransmitters. Neuropsychiatric symptoms can arise after penetrating or focal trauma as well as nonpenetrating trauma. Penetrating trauma can produce psychiatric symptoms depending on the function served by that particular area (e.g. aggression and behavioral disinhibition in bifrontal contusion). Symptoms of nonpenetrating injuries can be explained by cytotoxic processes such as Ca+2 and Mg+2 dysregulation, neurotransmitter excitotoxicity, free radical-induced injury, and diffuse axonal injury.[18,19]
Catecholamines
Damage to the ascending monoaminergic projections may cause pathological functioning of the systems dependent on these pathways.[20] Several studies show that TBI in these areas leads to decrease in dopamine levels which have bad prognosis.[21,22,23] Drugs that increase dopaminergic transmission have shown improvement in cognitive functions (e.g., arousal, speed of processing, attention, and memory).
Serotonin
Serotonin pathways to the frontal cortex are interrupted by contusions as well as axonal injuries causing dysfunction in neurotransmitter system. These pathways can also be damaged by secondary mechanisms of neuronal damage such as excitotoxins and lipid peroxidation that mediate serotonin.[24] It has been seen that the levels of lumbar CSF 5-hydroxylindoleacetic acid (5-HIAA) is less than normal in conscious patients.[25] In unconscious patients, levels were found to be normal. 5-HIAA levels in the CSF vary with the size of lesions, for example, patients with frontotemporal contusions have shown a decrease in 5-HIAA level whereas increased levels are seen in diffuse contusions.[25]
Acetylcholine
Both acute and chronic changes are evident in cholinergic cortical transmission after TBI. Acutely, there is an increase in cholinergic transmission after TBI followed by chronic reductions in neurotransmitter function and cholinergic afferents. In the experimental studies, elevated acetylcholine levels are seen in interventricular catheters or lumbar puncture in the acute period after TBI.[26] Chronically following severe TBI, loss of cortical cholinergic afferents with concurrent preservation of postsynaptic muscarinic, and nicotinic receptors are recognized.[27,28]
PSYCHIATRIC COMPLICATIONS OF TRAUMATIC BRAIN INJURY
The rates of disorders in patients with TBI are 14%–77% for major depression, dysthymia 2%–14%, bipolar disorder 2%–17%, generalized anxiety disorder 3%–28%, panic disorder 4%–17%, phobic disorders 1%–10%, obsessive-compulsive disorder (OCD) 2%–15%, posttraumatic stress disorder (PTSD) 3%–27%, substance abuse or dependence 5%–28%, and schizophrenia 1%.[29] There are multiple factors that affect and determine the neuropsychiatric sequelae of TBI which includes severity and type of injury, past psychiatric diagnosis, sociopathy, premorbid behavioral problem (children), social support, substance abuse, preexisting neurological disorder, age, and apolipoprotein E status.
In addition, the symptoms of the injury are correlated with the type of damage sustained. Patients who suffer from direct axonal injury usually experience a problem with arousal, slow cognitive processing, and attention.[30] Age is a significant factor in the development of psychiatric symptoms, for example, older people suffering from TBI have a longer agitation period, greater cognitive impairment and a higher possibility to develop mass lesions and permanent disability as compared to younger victims.[31] Damage to the olfactory nerve located adjacent to the orbitofrontal cortex may cause posttraumatic anosmia. Impairment in olfactory functioning may often occur in patients with moderate to severe brain injury linked to frontal and temporal lobe damage [Figure 1].[32,33]
Figure 1.
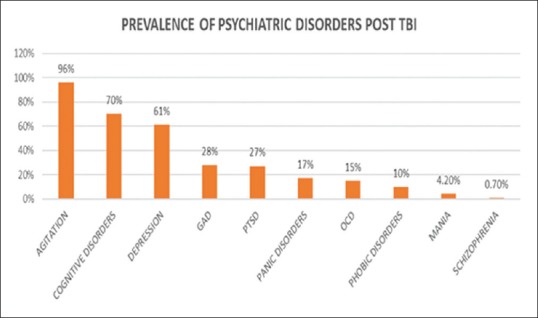
Prevalance of psychiatric disorders post TBI
Depression
Depression is a well-known symptom after TBI. Sadness is the most prevalent reaction after TBI as patients regret the loss of their past lives. We can evaluate depression by the Hamilton Rating Scale for Depression[34] or the Beck Depression Inventory.[35] Although these scales have been reported to evaluate depression after TBI, it is more important to evaluate the patients clinically. High scores on the Beck Depression Inventory represents hyperreactivity to post-TBI symptoms instead of depression. Patients with TBI may not encounter typical signs of depression such as somatic symptoms that are essential to diagnose depression. Mood liability is a frequent manifestation of depression after brain injury. The effect and liability of mood are also seen in temporal limbic and basal forebrain lesions[36] and are observed to be responsive to antidepressant medications. Other symptoms that manifest in brain injury are apathy, decreased motivation, schizoid behavior, impaired thought process, and cognitive dysfunction can resemble depression.[37]
Many studies report an increase in the risk of suicide after TBI. A study of 42 patients with severe TBI shows that after 1 year 10% of the patients had thought about suicide, and 2% attempted suicide.[38] After 5 years of the incident, 15 individuals attempted suicide. Many victims also express hopelessness and accept that life is not worth living.
Mania
Many patients suffer from bipolar disorder or manic episodes after TBI,[39] but the occurrence is lower as compared to depression.[40] Damage to the basal region of the right temporal lobe[41] and right orbitofrontal cortex[42] causes the development of manic symptoms post-TBI in patients with a positive family history of bipolar disorder.
Posttraumatic delirium
Patients present with delirium when they are regaining consciousness from the coma. The typical symptoms shown are restlessness, confusion, disorientation, hallucinations, agitation, and delusions. Delirium occurs by the effect of injury on brain tissue chemicals. However, there are other mechanisms that can cause posttraumatic delirium in TBI patients. For example, mechanical effects (acceleration or deceleration contusion), cerebral edema, hemorrhage, infection, subdural hematoma, seizure, hypoxia (cardiopulmonary or local ischemia), increased intracranial pressure, alcohol intoxication or withdrawal, Wernicke's encephalopathy, reduced hemoperfusion due to multiple trauma, fat embolism, alterations in pH, electrolyte imbalance, and medications (Steroids, opioids, barbiturates, and anticholinergics).
Psychotic disorders
The patient can present with psychosis any time after brain injury, acutely or after several months of normal functioning.[43] Many of post-TBI disorders such as mania, depression, and epilepsy can lead to psychotic manifestations.[44] These symptoms can persist despite improvement in the cognitive deficits caused by trauma.[45,46] In a study on 2907, war veterans in Finland, who had a brain injury, 26% of these veterans had psychotic disorders. Out of these veterans, authors did a detailed evaluation of 100 veterans and found that 14% had paranoid schizophrenia.[46] Schizophrenia patients may have had a history of TBI in the past which is not detected unless the clinician asks specifically for the event of brain trauma. Researchers have found a correlation between TBI and genetic predisposition to schizophrenia. A comparison between schizophrenia and bipolar families was made to know the effect of TBI on the development of schizophrenia. The result concludes that members of schizophrenia pedigree, even those without a schizophrenia diagnosis, have a higher exposure to TBI as compared with bipolar disorder pedigrees.[47]
Anxiety disorders
Many anxiety disorders can develop after TBI.[48] From a study of 66 patients with TBI, 11% of the patients developed generalized anxiety disorder in addition to major depression.[49] In a study which evaluated 120 soldiers suffering from moderate to severe TBI, 9% developed a panic attack.[50] After 1 year of registration in the study of cognitive rehabilitation, 15% fulfill the criteria of generalized anxiety disorder. In another study conducted on patients with TBI, 18% developed PTSD, 14% developed an OCD, 11% developed panic disorder, 8% developed generalized anxiety disorder, and 6% developed phobic disorder.[51]
In TBI patients, PTSD is very common.[52] A 2-year study conducted on 79 patients who sustained mild TBI showed that acute stress disorder developed in 14% of the patients within 1 month of the trauma. After 2 years, 73% of the patients with acute stress disorder developed PTSD.[53] In 96 patients who encountered severe TBI, 26 (27.1%) developed PTSD.[54] The development of PTSD in a patient depends on the severity of TBI. PTSD patients who show signs of memory deficits have temporal lobe injury.[55] Imaging studies exhibit small hippocampal volumes in PTSD patients.
Substance abuse
TBI and substance abuse disorders often co-occur. Persons with histories of alcohol or other drug abuse are at higher risk of sustaining TBI, and individuals with TBI commonly misuse substances before and after injury. Risk-taking behavior can be a direct result of substance abuse disorders, and risky behaviors may lead to subsequent injury or continued use of substances. The complications of moderate to severe TBI are well described, but the long-term effects associated with mild TBI are unclear. Alcohol and drug uses are well recognized to increase the risk of TBI, but the reverse pattern is debatable. According to a research study,[56] there is an enhanced risk for alcohol addiction, nondependent abuse of drugs, and nicotine dependency during the first 30 days following mild TBI and risk for alcohol dependence for at least 6 months after injury. In addition, studies have also shown that TBI in childhood, adolescence, and early adulthood is associated with increased criminal behavior and substance abuse.[57] However, early substance abuse is also a mediating factor for those injured early in life. Furthermore, according to another study, frequent binge drinking was reported in deployed military personnel who had experienced combat-acquired TBI and even mild TBI with altered consciousness.[58] Therefore, it is highly likely that a very high proportion of individuals who have been hospitalized for TBI will be at risk of developing a substance abuse after the injury, either because they had one before or because of the vulnerabilities created by the injury itself.
Sleep disorder
Disturbance of sleep pattern is a common complaint in patients with TBI. Patients complain about disturbed sleep patterns, hypersomnia, and difficulty maintaining sleep.[59] A study was conducted in which, 91 patients who are admitted to a neuro-rehabilitation outpatient clinic were assessed. Mild brain injury and coexistence with depression (as evaluated by the score on the Beck Depression Inventory) showed a correlation with insomnia.[60] Another study[61] evaluated 184 patients with TBI and hypersomnia in which they used Multiple Sleep Latency Test to check abnormalities. The most common symptom seen was sleep-disordered breathing (59/184 patients). Lack of motivation and apathy are symptoms of depression, and it is crucial to differentiate it from hypersomnia. Pain can cause insomnia too, so it should also be ruled out.
Cognitive and behavioral sequel of traumatic brain injury
Attention and memory deficits are the most common cognitive difficulties reported by patients and their families after the TBI. This could be due to primary brain damage or due to secondary factors such as sleep disturbance. Executive functioning impairment is the next important under evaluated cognitive sequel of the TBI. The executive functioning is mainly controlled by the prefrontal cortex. Deficits in the executive functioning hamper the individual's ability to focus and organize to accomplish tasks. These functions are critically essential to have a good quality of life, job performance, social life, and perform other functions of daily living.
In behavioral domain, they mainly suffer from disturbances related to aggression and impulsivity which not only affects patients but also the family and friends. Patients who suffered TBI may have irritability, aggressive behavior, and agitation.[62] Aggression can range from irritability to outbursts that would result in the destruction of property or assaults on others. Irritability or bad temper is very common in patients after the acute phase of TBI. A study was conducted on TBI inpatients, which showed that there is a significant correlation of aggression with other conditions such as new-onset major depression and impaired psychosocial functioning.[63] The other important behavioral sequel of TBI is OCD, although it is rare.
Focal brain lesions and diffuse damage to the central nervous system show explosive and violent behavior.[64] It is very vital to distinguish aggressive behavior from mood liability based on characteristic behavioral features that are present in patients having aggressive behavior.[62] Typically, aggressive behavior presents as a reactive type of violence is seen (triggered by simple stimuli). It is always nonreflective and prior planning of the actions is absent. Nonpurposeful aggression does not have any sense of long-term aims or goals. The violence is periodic, whereby there are brief episodes of aggression and rage followed by long periods of calm behavior. It is egodystonic; the patient is often embarrassed or upset after the scenario. Finally, it is usually explosive and sudden, occurring without any buildup.
DISCUSSION
Falls and Motor Vehicle accidents are major causes of TBI which can be prevented by appropriate primary prevention methods. Further after the occurrence of TBI, prompt treatment intervention is equally important. Rapid identification and stabilization of patients with severe TBI are essential for the effective initial management of focal injuries, conditions that contribute to secondary brain injury and also prevent the unwanted sequel. However, the outcome from severe head injury is dependent on a different range of factors including baseline patient characteristics, preexisting medical conditions (diabetes, heart disease), the severity of TBI, occurrence of medical complications, and secondary brain insults following the injury. Apart from all these, the heterogeneity of severe head injury makes it difficult to apply the clinical decision-making in individual patients. Recent studies have focused on the potentiality of biomarkers, such as the levels of S-100 β protein, neuron-specific enolase, and α-synuclein in the blood and/or CSF, to predict the neurological outcome. Further extensive research is needed to understand if these biomarkers can be targeted specifically to modify the treatment intervention and also affect prognosis following TBI.
Appropriate measures should be taken to expand knowledge about evidence-based interventions to prevent secondary injury associated with TBI to maximize neurocognitive recovery and increase functional independence. Healthcare providers have to be necessarily trained to promote prevention, early intervention, appropriate use of assessment scales, and effectively implement acute and rehabilitation therapies. An intensive team approach is needed to collaborate with the expertise of psychiatrists, neurologists, and psychologists for the efficient management of the patients. A careful assessment is required to get an accurate description of patient's functional and neurobehavioral status after the injury. Patients experiencing suicidal thoughts need aggressive psychological rehabilitation and care. In addition, caregivers have to be trained specially to take care of such patients. Future studies are to be focused on understanding if there are improved outcomes in the patients who are under the care of such trained caregivers. Such studies proved with evidence can help us focus on improving the quality of life for both the patients and also the caregivers. In conclusion, collaborative efforts are needed to continue and support research in this field in future, for accommodating better treatment and rehabilitative options to the patients who suffer TBI.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Halstead ME, Walter KD. Council on Sports Medicine and Fitness. American Academy of Pediatrics. Clinical report – Sport-related concussion in children and adolescents. Pediatrics. 2010;126:597–615. doi: 10.1542/peds.2010-2005. [DOI] [PubMed] [Google Scholar]
- 2.DeKosky ST, Ikonomovic MD, Gandy S. Traumatic brain injury – Football, warfare, and long-term effects. N Engl J Med. 2010;363:1293–6. doi: 10.1056/NEJMp1007051. [DOI] [PubMed] [Google Scholar]
- 3.Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States. Atlanta, GA: National Center for injury Prevention and Control, Centers for disease Control and Prevention; 2010. [Google Scholar]
- 4.Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: A global perspective. NeuroRehabilitation. 2007;22:341–53. [PubMed] [Google Scholar]
- 5.Silver JM, McAllister TW, Yudofsky SC. Textbook of traumatic brain injury. American Psychiatric Pub. 2011 [Google Scholar]
- 6.National Institutes of Health Consensus Development Panel. National Institutes of Health Consensus Development Conference statement: Adjuvant therapy for breast cancer, November 1-3, 2000. J Natl Cancer Inst. 2001;93:979–89. doi: 10.1093/jnci/93.13.979. [DOI] [PubMed] [Google Scholar]
- 7.Kraus JF, Morgenstern H, Fife D, Conroy C, Nourjah P. Blood alcohol tests, prevalence of involvement, and outcomes following brain injury. Am J Public Health. 1989;79:294–9. doi: 10.2105/ajph.79.3.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pearson WS, Sugerman DE, McGuire LC, Coronado VG. Emergency department visits for traumatic brain injury in older adults in the United States: 2006-08. West J Emerg Med. 2012;13:289–93. doi: 10.5811/westjem.2012.3.11559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shlosberg D, Benifla M, Kaufer D, Friedman A. Blood-brain barrier breakdown as a therapeutic target in traumatic brain injury. Nat Rev Neurol. 2010;6:393–403. doi: 10.1038/nrneurol.2010.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sivanandam TM, Thakur MK. Traumatic brain injury: A risk factor for Alzheimer's disease. Neurosci Biobehav Rev. 2012;36:1376–81. doi: 10.1016/j.neubiorev.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Gean AD, Fischbein NJ. Head trauma. Neuroimaging Clin N Am. 2010;20:527–56. doi: 10.1016/j.nic.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Saatman KE, Duhaime AC, Bullock R, Maas AI, Valadka A, Manley GT. Workshop Scientific Team and Advisory Panel Members. Classification of traumatic brain injury for targeted therapies. J Neurotrauma. 2008;25:719–38. doi: 10.1089/neu.2008.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeffrey ME, Robin DA, Lindgren SD, Smith WL, Sato Y, Mattheis PJ, et al. Traumatic brain injury in children and adolescents: Psychiatric disorders at two years. J the American Academy of Child & Adolescent Psychiatry. 1997;36:1278–85. doi: 10.1097/00004583-199709000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Love S, Louis D, Ellison DW. Greenfield's Neuropathology. 2-Volume Set. 8th ed. USA: CRC Press; 2008. [Google Scholar]
- 15.Lunetta P, Modell JH. Forensic Pathology Reviews. USA: Humana Press; 2005. Macroscopical, microscopical, and laboratory findings in drowning victims; pp. 3–77. [Google Scholar]
- 16.Grubaugh JG. Comparing Levels of Supervision Across Occupational Therapy Intake and Discharge for Individuals Receiving Post-Acute Traumatic Brain Injury Rehabilitation. 2014 [Google Scholar]
- 17.Center for Disease Control and Prevention. Heads up: Concussion in youth sports. [Last updated on 2015 Feb 16, Last accessed on 2016 Oct 16]. Available from: http://www.cdc.gov/headsup/basics/concussion_symptoms.html .
- 18.Halliday A. Pathophysiology in traumatic brain injury. In: Marion D, editor. Traumatic Brain Injury. New York: Thieme Medical Publishers, Inc; 1999. pp. 29–38. [Google Scholar]
- 19.Mcintosh TK, Juhler M, Raghupathi R, Saatman KE, Smith DH. Secondary brain injury: Neurochemical and cellular mediators. Traumatic brain injury. New York: Thieme; 1999. pp. 39–54. [Google Scholar]
- 20.Morrison JH, Molliver ME, Grzanna R. Noradrenergic innervation of cerebral cortex: Widespread effects of local cortical lesions. Science. 1979;205:313–6. doi: 10.1126/science.451605. [DOI] [PubMed] [Google Scholar]
- 21.Donnemiller E, Brenneis C, Wissel J, Scherfler C, Poewe W, Riccabona G, et al. Impaired dopaminergic neurotransmission in patients with traumatic brain injury: A SPECT study using 123I-beta-CIT and 123I-IBZM. Eur J Nucl Med. 2000;27:1410–4. doi: 10.1007/s002590000308. [DOI] [PubMed] [Google Scholar]
- 22.Hamill RW, Woolf PD, McDonald JV, Lee LA, Kelly M. Catecholamines predict outcome in traumatic brain injury. Ann Neurol. 1987;21:438–43. doi: 10.1002/ana.410210504. [DOI] [PubMed] [Google Scholar]
- 23.Woolf PD, Hamill RW, Lee LA, Cox C, McDonald JV. The predictive value of catecholamines in assessing outcome in traumatic brain injury. J Neurosurg. 1987;66:875–82. doi: 10.3171/jns.1987.66.6.0875. [DOI] [PubMed] [Google Scholar]
- 24.Pasaoglu H, Inci Karaküçük E, Kurtsoy A, Pasaoglu A. Endogenous neuropeptides in patients with acute traumatic head injury, I: Cerebrospinal fluid beta-endorphin levels are increased within 24 hours following the trauma. Neuropeptides. 1996;30:47–51. doi: 10.1016/s0143-4179(96)90054-2. [DOI] [PubMed] [Google Scholar]
- 25.van Woerkom TC, Teelken AW, Minderhous JM. Difference in neurotransmitter metabolism in frontotemporal-lobe contusion and diffuse cerebral contusion. Lancet. 1977;1:812–3. doi: 10.1016/s0140-6736(77)93008-2. [DOI] [PubMed] [Google Scholar]
- 26.Grossman R, Beyer C, Kelly P, Haber B. “Acetylcholine and related enzymes in human ventricular and subarachnoid fluids following brain injury.” vol. 76. In Proceedings of the 5th Annual Meeting for Neuroscience. 1975:506. [Google Scholar]
- 27.Dewar D, Graham DI. Depletion of choline acetyltransferase activity but preservation of M1 and M2 muscarinic receptor binding sites in temporal cortex following head injury: A preliminary human postmortem study. J Neurotrauma. 1996;13:181–7. doi: 10.1089/neu.1996.13.181. [DOI] [PubMed] [Google Scholar]
- 28.Murdoch I, Perry EK, Court JA, Graham DI, Dewar D. Cortical cholinergic dysfunction after human head injury. J Neurotrauma. 1998;15:295–305. doi: 10.1089/neu.1998.15.295. [DOI] [PubMed] [Google Scholar]
- 29.Deb S, Lyons I, Koutzoukis C, Ali I, McCarthy G. Rate of psychiatric illness 1 year after traumatic brain injury. Am J Psychiatry. 1999;156:374–8. doi: 10.1176/ajp.156.3.374. [DOI] [PubMed] [Google Scholar]
- 30.Lovell MR, Iverson GL, Collins MW, McKeag D, Maroon JC. Does loss of consciousness predict neuropsychological decrements after concussion? Clin J Sport Med. 1999;9:193–8. doi: 10.1097/00042752-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Kim E. Elderly. In: Silver JM, McAllister TW, Yudofsky SC, editors. Textbook of Traumatic Brain Injury. Arlington: American Psychiatric Publishing, Inc; 2005. pp. 495–508. [Google Scholar]
- 32.Levin HS, High WM, Eisenberg HM. Impairment of olfactory recognition after closed head injury. Brain. 1985;108(Pt 3):579–91. doi: 10.1093/brain/108.3.579. [DOI] [PubMed] [Google Scholar]
- 33.Dilley M, Avent C. Long-term neuropsychiatric disorders after traumatic brain injury. Psychiatric Disorders-Worldwide Advances. 2011:301–27. [Google Scholar]
- 34.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 36.Ross ED, Stewart RS. Pathological display of affect in patients with depression and right frontal brain damage. An alternative mechanism. J Nerv Ment Dis. 1987;175:165–72. doi: 10.1097/00005053-198703000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Marin RS, Wilkosz PA. Disorders of diminished motivation. J Head Trauma Rehabil. 2005;20:377–88. doi: 10.1097/00001199-200507000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Tate R, Simpson G, Flanagan S, Coffey M. Completed suicide after traumatic brain injury. J Head Trauma Rehabil. 1997;12:16–28. [Google Scholar]
- 39.Burstein A. Bipolar and pure mania disorders precipitated by head trauma. Psychosomatics. 1993;34:194–5. doi: 10.1016/S0033-3182(93)71920-9. [DOI] [PubMed] [Google Scholar]
- 40.Bakchine S, Lacomblez L, Benoit N, Parisot D, Chain F, Lhermitte F. Manic-like state after bilateral orbitofrontal and right temporoparietal injury: Efficacy of clonidine. Neurology. 1989;39:777–81. doi: 10.1212/wnl.39.6.777. [DOI] [PubMed] [Google Scholar]
- 41.Starkstein SE, Mayberg HS, Berthier ML, Fedoroff P, Price TR, Dannals RF, et al. Mania after brain injury: Neuroradiological and metabolic findings. Ann Neurol. 1990;27:652–9. doi: 10.1002/ana.410270612. [DOI] [PubMed] [Google Scholar]
- 42.Starkstein SE, Boston JD, Robinson RG. Mechanisms of mania after brain injury 12 case reports and review of the literature. J Nerv Ment Dis. 1988;176:87–100. doi: 10.1097/00005053-198802000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Corcoran C, McAllister TW, Malaspina D. Psychotic disorders. In: Silver JM, McAllister TW, Yudofsky S C, editors. Textbook of traumatic brain injury. Arlington, VA: American Psychiatric Publishing, Inc; 2005. pp. 213–29. [Google Scholar]
- 44.McAllister TW. Traumatic brain injury and psychosis: What is the connection? Semin Clin Neuropsychiatry. 1998;3:211–23. [PubMed] [Google Scholar]
- 45.Nasrallah HA, Fowler RC, Judd LL. Schizophrenia-like illness following head injury. Psychosomatics. 1981;22:359–61. doi: 10.1016/S0033-3182(81)73526-6. [DOI] [PubMed] [Google Scholar]
- 46.Achté K, Jarho L, Kyykkä T, Vesterinen E. Paranoid disorders following war brain damage. Preliminary report. Psychopathology. 1991;24:309–15. doi: 10.1159/000284731. [DOI] [PubMed] [Google Scholar]
- 47.Malaspina D, Goetz RR, Friedman JH, Kaufmann CA, Faraone SV, Tsuang M, et al. Traumatic brain injury and schizophrenia in members of schizophrenia and bipolar disorder pedigrees. Am J Psychiatry. 2001;158:440–6. doi: 10.1176/appi.ajp.158.3.440. [DOI] [PubMed] [Google Scholar]
- 48.Warden DL, Labbate LA. Posttraumatic stress disorder and other anxiety disorders. In: Silver JM, McAllister TW, Yudofsky SC, editors. Textbook of traumatic brain injury. Arlington, VA: American Psychiatric Publishing, Inc; 2005. pp. 231–43. [Google Scholar]
- 49.Jorge RE, Robinson RG, Starkstein SE, Arndt SV. Depression and anxiety following traumatic brain injury. J Neuropsychiatry Clin Neurosci. 1993;5:369–74. doi: 10.1176/jnp.5.4.369. [DOI] [PubMed] [Google Scholar]
- 50.Salazar AM, Warden DL, Schwab K, Spector J, Braverman S, Walter J, et al. Cognitive rehabilitation for traumatic brain injury: A randomized trial. Defense and Veterans Head Injury Program (DVHIP) Study Group. JAMA. 2000;283:3075–81. doi: 10.1001/jama.283.23.3075. [DOI] [PubMed] [Google Scholar]
- 51.Hibbard MR, Uysal S, Kepler K, Bogdany J, Silver J. Axis I psychopathology in individuals with traumatic brain injury. J Head Trauma Rehabil. 1998;13:24–39. doi: 10.1097/00001199-199808000-00003. [DOI] [PubMed] [Google Scholar]
- 52.Silver JM, Rattok J, Anderson K. Post-traumatic stress disorder and traumatic brain injury. Neurocase. 1997;3:151–7. [Google Scholar]
- 53.Harvey AG, Bryant RA. Two-year prospective evaluation of the relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry. 2000;157:626–8. doi: 10.1176/appi.ajp.157.4.626. [DOI] [PubMed] [Google Scholar]
- 54.Bryant RA, Marosszeky JE, Crooks J, Gurka JA. Posttraumatic stress disorder after severe traumatic brain injury. Am J Psychiatry. 2000;157:629–31. doi: 10.1176/appi.ajp.157.4.629. [DOI] [PubMed] [Google Scholar]
- 55.Bremner JD, Scott TM, Delaney RC, Southwick SM, Mason JW, Johnson DR, et al. Deficits in short-term memory in posttraumatic stress disorder. Am J Psychiatry. 1993;150:1015–9. doi: 10.1176/ajp.150.7.1015. [DOI] [PubMed] [Google Scholar]
- 56.Olson-Madden JH, Brenner LA, Corrigan JD, Emrick CD, Britton PC. Substance use and mild traumatic brain injury risk reduction and prevention: A novel model for treatment. Rehabil Res Pract 2012. 2012:174579. doi: 10.1155/2012/174579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McKinlay A, Corrigan J, Horwood LJ, Fergusson DM. Substance abuse and criminal activities following traumatic brain injury in childhood, adolescence, and early adulthood. J Head Trauma Rehabil. 2014;29:498–506. doi: 10.1097/HTR.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 58.Miller SC, Baktash SH, Webb TS, Whitehead CR, Maynard C, Wells TS, et al. Risk for addiction-related disorders following mild traumatic brain injury in a large cohort of active-duty U.S. airmen. Am J Psychiatry. 2013;170:383–90. doi: 10.1176/appi.ajp.2012.12010126. [DOI] [PubMed] [Google Scholar]
- 59.Rao V, Rollings P, Spiro J. Fatigue and sleep problems. Textbook of Traumatic Brain Injury. Washington, DC: American Psychiatric Publishing, Inc; 2005. pp. 369–84. [Google Scholar]
- 60.Fichtenberg NL, Millis SR, Mann NR, Zafonte RD, Millard AE. Factors associated with insomnia among post-acute traumatic brain injury survivors. Brain Inj. 2000;14:659–67. doi: 10.1080/02699050050044015. [DOI] [PubMed] [Google Scholar]
- 61.Guilleminault C, Yuen KM, Gulevich MG, Karadeniz D, Leger D, Philip P. Hypersomnia after head-neck trauma: A medicolegal dilemma. Neurology. 2000;54:653–9. doi: 10.1212/wnl.54.3.653. [DOI] [PubMed] [Google Scholar]
- 62.Yudofsky SC, Silver JM, Hales RE. Pharmacologic management of aggression in the elderly. J Clin Psychiatry. 1990;51(Suppl):22–8. [PubMed] [Google Scholar]
- 63.Rao V, Rosenberg P, Bertrand M, Salehinia S, Spiro J, Vaishnavi S, et al. Aggression after traumatic brain injury: Prevalence and correlates. J Neuropsychiatry Clin Neurosci. 2009;21:420–9. doi: 10.1176/appi.neuropsych.21.4.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Anderson KE, Silver JM. Neurological and medical diseases and violence. In: Tardiff K, editor. Medical Management of the Violent Patient: Clinical Assessment and Therapy. New York: Marcel Dekker; 1999. pp. 87–124. [Google Scholar]


