Abstract
Aim:
The study aimed to assess the efficacy of providing brief intervention (BI) for women tobacco users in a community-based setting.
Methods:
In this open-labeled randomized study, a representative sample of women (n = 100) from a community in East Delhi were screened using Alcohol, Smoking and Substance Involvement Screening Test. Eligible women were randomized to BI or simple advice (SA) arms. At baseline, they were assessed for tobacco use characteristics and severity of nicotine dependence using Fagerstrom's test for nicotine dependence. Intervention in the form of a single session of BI or SA to quit tobacco was provided at baseline. All participants were assessed at 1 week and 3 months following intervention. The principal outcome was self-reported abstinence from tobacco use at 3 months follow-up.
Results:
The mean age of the sample was 43 years (standard deviation = 13). Most women were married (80%), housewives (69%), illiterate (61%), socioeconomically disadvantaged and were smokeless tobacco users (94%). The subjects in the BI group were twice more likely to stop tobacco use as compared to individuals in the SA group (odds ratio = 2.2, 95% confidence interval: 0.962–5.197, P = 0.06).
Conclusion:
The study results are suggestive of beneficial effect of BI. A larger study might provide more significant results.
Keywords: Brief intervention, smokeless tobacco, women
INTRODUCTION
Tobacco, alcohol, and illicit drugs are among the top twenty risk factors for ill-health identified by the World Health Organization (WHO). It is estimated that tobacco is responsible for 9% of all deaths and 4.1% of the global burden of all disease, and the vast majority of these deaths are projected to occur in developing countries.[1]
The magnitude of India's tobacco problem was shown most recently by Global Adult Tobacco Survey[2] conducted in India from 2009 to 10 which shows that the prevalence of tobacco use in India is very high, and more than one-third (35%) of adults in India use tobacco in some form or the other. The prevalence of overall tobacco use among males is 48%, and that among females is 20%.
The number of women tobacco users in the country is on the rise. According to the Global Adult Tobacco Survey 2009–2010, India, women using tobacco now make for 20.3% of tobacco users while the figure used to be 11.5% in 2005,[3] which represents an alarming increase in a duration of 5 years. Among females, chewing tobacco is more common than smoking, and only a small proportion of females smoke tobacco. Women tobacco users not only share the same health risks as men but are also faced with health consequences that are unique to women, including those connected to pregnancy and cervical cancer.[4]
Tobacco dependence is a chronic health condition that often requires multiple, discrete interventions by a team of clinicians.[5] Screening and brief interventions (BIs) aim to identify current or potential problems with substance use and motivate those at risk to change their substance use behavior.[6] It is recommended that screening is carried out systematically using a standardized, validated screening instrument such as the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST).[7] The ASSIST determines a risk score (“lower,” “moderate”, or “high”) for each substance report card which is used to give personalized feedback to clients by presenting them with the scores that they have obtained, and the associated health problems related to their level of risk. The aim of BI is to help the patient understand that their substance use is putting them at risk. ASSIST linked BI, developed by the WHO has been manualized and validated across diverse cultural settings, including India.[8] BIs can range from 5 min of brief advice to 15–30 min of brief counseling.[9]
There is strong evidence for the effectiveness of BIs in primary care and community settings for alcohol and tobacco. BIs are low in cost and are effective across all levels of hazardous and harmful substance use and so are ideally suited for the use as a method of health promotion and disease prevention. Published evidence and the 2000 Public Health Service guideline confirm that identifying smokers and providing them with brief advice and cessation assistance in clinical practice are both very effective and cost effective.[10]
Given, the increasing magnitude of the problem in women and associated morbidity and mortality urgent steps need to be taken to enhance low-cost community-based interventions for tobacco use in this vulnerable population. In addition, though BI is widely researched in smokers, not much is known regarding its efficacy in smokeless tobacco (ST) users. This study was planned as a community-based pilot trial aimed at testing the feasibility and effectiveness of providing screening and BI to women in an urban community.
METHODS
Clearance from ethical perspective for the study was obtained from the Institutional Ethics Committee of AIIMS, New Delhi. The community sample of 100 women tobacco users was recruited from Sundarnagari, Delhi an urban resettlement colony plus jhuggi cluster (shanty dwelling) with approximately one lakh population. The community is inhabited largely by people from the lower socioeconomic strata. A prior available sampling frame was utilized for this study, and the sample was selected through systematic random sampling for this open-label randomized study. After the selection of required number of women, simple randomization procedure (by the Excel functionality of RAND) was used to allocate individuals in the respective arm-BI or simple advice (SA). Women reporting current tobacco use, coming in moderate risk scores as classified by ASSIST and willing to participate were recruited in the study. Written informed consent was taken from each participant in the study. Women reporting the current use of any other drug of abuse besides tobacco were excluded from the study. Instruments used were WHO-ASSIST for screening,[11] a semi-structured pro forma to assess key tobacco-related parameters, Fagerstrom's test for nicotine dependence (FTND)[12], and FTND-ST[13] were used to determine the severity of dependence. Readiness to change questionnaire[14] was used to assess the stage of change.
Screening and BI were delivered by two social workers who were trained in these procedures. Baseline assessment procedures took about half an hour. Intervention in the form of BI or SA to quit tobacco was provided at baseline. BI was delivered in a single session of 30 min duration using FRAMES model.[15,16,17] The acronym FRAMES here stands for personalized feedback about ASSIST scores, client has responsibility for their choices, giving SA about how to reduce risk associated with substance use, menu of alternative strategies to promote personal choice, goals, and control, showing empathy which is a potent determinant of client motivation and change and self-efficacy to instill optimism. SA was given using a patient education brochure focusing of risk and consequences of tobacco use. A locator sheet with address and contact number was filled out at baseline. All participants were traced using the locator sheet and assessed at 1 week and 3 months following the intervention.
Outcome measures included self-reported point prevalence abstinence from tobacco at 3 months, ASSIST, and FTND scores.
RESULTS
Fifty women tobacco users each were allocated to BI and SA protocols, respectively.
Sociodemographic and tobacco use profile
As shown in Table 1, the mean (standard deviation [SD]) age of the sample was found to be 43 (13) years. Most of the women tobacco users were married (79.0%), housewives (69%), illiterate (61%), and belonged to nuclear family (60%). The median family size in the study was six.
Table 1.
Socio demographic profile
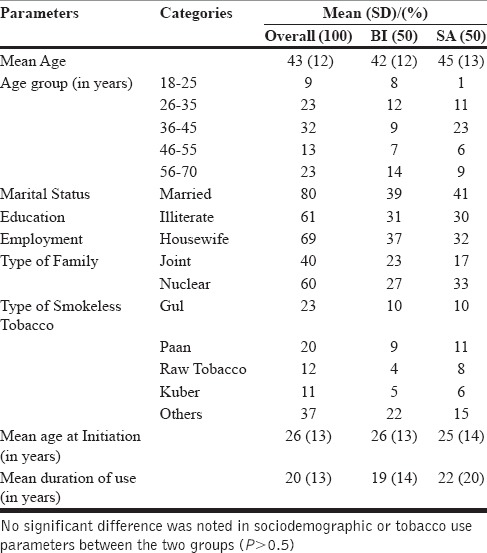
The predominant tobacco use among women was in the form of ST (94%), with gul (pyrolyzed tobacco) and betel quid with tobacco (20% each) being the most common forms used. The mean age of initiation of tobacco products was 26 (13) years, and most women were chronic users with a mean duration of use for 20 (13) years. The most commonly reported reason for the consumption of tobacco products was dental problems followed by peer pressure.
Interest in quitting and quit attempts
Although a majority of women (75%) reported that they were very interested in quitting tobacco use, 46% of women had never previously attempted to quit tobacco use, and the mean number of quit attempts among those who tried to quit was very low 1.3 (0.8). A quarter of women reported concerns about health as a reason for quit attempt, followed by family pressure to quit. Most women tried to quit using self-help alone. Only 6% sought medical help for quitting tobacco. The mean number of quit attempts was low (1.3 ± 0.7). Most commonly the duration of abstinence lasted for about a week. Dental problems were the most common reason reported for relapse to tobacco use.
Awareness of harms and perceived importance of intervention
Most women (81%) were aware that tobacco use is harmful, and a substantial proportion (40%) reported cancer as one the major harms of tobacco use. However, awareness of other harms was very low. Self-help alone (57%) and advice and guidance only (52%) were perceived as adequate interventions to quit tobacco use among these women.
Self-reported point prevalence abstinence
As shown in Table 2, at 3 months follow-up postintervention, the self-reported point prevalence abstinence rates were higher in the BI arm. Z-test for test of significance to assess the significant difference between two sample proportions and the result was statistically significant.
Table 2.
Important assessments in BI vs SA at baseline and follow up
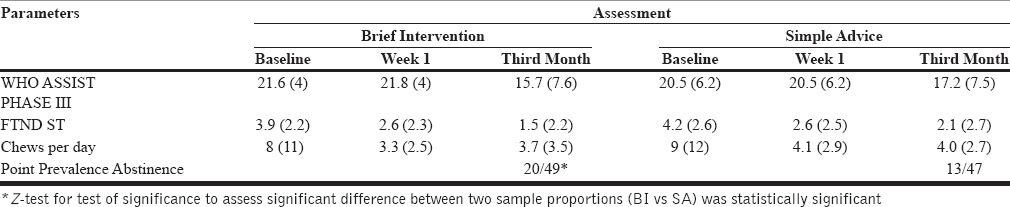
The subjects in the BI were twice more likely to stop tobacco use as compared to individuals in the SA group. The relative risk of stopping tobacco use among subjects in the BI was 2.24 (95% confidence interval [CI]: 0.96–5.20), and this result was marginally significant (P = 0.06).
Proportion of users who reduced tobacco at month-3 follow-up
The proportion of individuals showing reduction categorized in 3 levels as <50%, 51.75% >75% was found to be comparable across two groups (P value for Chi-square test = 0.523). Overall association between two groups was not statistically significant.
World Health Organization Alcohol, Smoking and Substance Involvement Screening Test and Fagerstrom's test for nicotine dependence smokeless tobacco scores
The general linear model with repeated measure revealed statistically significant difference in two other outcome parameters, namely, WHO ASSIST scores (F[1,98] =16.7 [P < 0.001]) and FTND-ST (F[1,98] =39.5 [P < 0.001]) scores at baseline, week 1, and month 3. Tobacco quantity used per day (F[1,98] =46 [P < 0.001]) and the number of chews per day (F[1,98] =52 [P < 0.001]) also showed statistically significant difference at baseline, week 1, and month 3. However, these findings were comparable across the two groups (BI vs. SA) at all-time points.
Subgroup analysis
On subgroup analysis, the distribution of socio-demographic parameters, types of tobacco used, age of initiation, duration of use, ASSIST and FTND-ST scores at baseline, and baseline chews per day were found to be comparable across subjects who were abstinent from tobacco use at follow-up versus those subjects who continued tobacco use.
DISCUSSION
In this open-label randomized community-based intervention study for tobacco cessation, most women were housewives (69%), illiterate (61%), socioeconomically disadvantaged, and ST users (94%). India is known to have a huge problem of widespread ST use among women, more so among disadvantaged women and differentials in the prevalence of tobacco use across socioeconomic groups are much more acute in women compared with men.[4] The mean age of the sample was 43 years (SD = 12.8). In general, tobacco use decreases in higher age groups[18] and India; also middle-aged adult males have a higher prevalence of tobacco use). However, a significant proportion (23%) of women in this study were above 55 years of age. This finding is not surprising as national data also indicates that the prevalence of all forms of tobacco increases linearly with age among females with elderly and middle-aged females having significantly higher odds of consuming every type of tobacco.[19] Hence, women across all age groups need to be targeted when planning interventions for tobacco control.
Hundred women tobacco users were randomized into two arms-BI and SA. BI was delivered by trained social workers. At 3 months follow-up postintervention, the self-reported point prevalence abstinence rates were higher in the BI arm. The subjects in the BI were twice more likely to stop tobacco use as compared to individuals in the SA group.
Similarly, the studies in western samples have found that brief advice to quit smoking is better than no advice, increasing 12-month quit rates by 1–3% over the unassisted quit rate of unassisted quit rate of 2–3%.[20,21,22,23] The US Preventive Services Task Force recommends screening and providing BIs for tobacco use as part of standard routine health care.[24] Brief advice is a low-cost intervention which can be delivered to large numbers by trained health workers.[20]
The effectiveness of brief advice for smoking cessation has not been evaluated extensively in low- or middle-income countries. A few available studies suggest that community-based counseling is a practical and cost-effective approach in the South Asian region.[25] In India, in a randomized controlled intervention for smoking cessation in rural Kerala, which comprised four counseling sessions in the active arm, self-reported point prevalence abstinence at 12-month follow-up in the intervention, and control areas were 14.7% and 6.8%, respectively. The control group received information and educational leaflets about risks of tobacco use. The quit status reported at 6 months interim period was higher in the intervention area (16%) compared to control area (5.7%) (P < 0.001) and rate of quitting at 12-month was 1.8 times more in the intervention group compared to the control group (adjusted risk ratio: 1.85, 95% CI: 1.05–3.25).[26] In a cluster randomized study conducted in Tamil Nadu, counseling sessions were given to 400 men using any form of tobacco. A physician offered two sessions of health education 5 weeks apart along with self-help material on tobacco cessation to the intervention group. The control group received only self-help material. Self-reported point prevalence abstinence of 12.5% in the intervention group was significantly higher than the 6.0% in the control group at 2 months.[27]
The general linear model with repeated measures in this study revealed statistically significant difference in two other outcome parameters, namely, WHO ASSIST scores (F, P value) and FTND-ST scores at baseline, week 1, and month 3. Tobacco quantity used per day and the number of chews per day also showed statistically significant difference at baseline, week 1, and month 3. However, these findings were comparable across the two groups (BI vs. SA) at all-time points. Comparable findings in the control groups have been previously reported in BIs studies and the possible postulated reasons for this may be that in screening and BI procedures, screening in and of itself may have some therapeutic.[28] Further, significant reductions in substance use and related harms are also seen in control groups as some elements such as information handouts as in this study are given to control groups making detection of a BI effect more difficult.[28]
The findings of this study may be generalizable to other urban resettlement colonies which represent economically disadvantaged localities in urban areas and also to other sections of illiterate and disadvantaged women. Hence, the findings of this study are important as they represent that low-cost efficacious interventions for tobacco use may be possible to implement in a resource-constrained country like India. The previous studies have also highlighted that the agenda to improve health outcomes among the poor in India must include effective interventions to control tobacco use.[29]
The strengths of the study are that it demonstrates the effectiveness of BI in women who were predominantly ST users in a randomized design. A major limitation of the study was the absence of biochemical validation of self-reported abstinence. There may be logistic issues in carrying out urine screening in community-based studies.
CONCLUSION
This study demonstrated that it is possible to carry out screening and BI in the natural community setting in women tobacco users. The empirical results are suggestive of beneficial effect of BI. A larger study may be conducted to further establish the efficacy of BI in this population and as such low-cost efficacious interventions such as BIs are of particular importance to a developing nation like India and may assume even more importance while dealing with a vulnerable population such as women.
Financial support and sponsorship
Indian Council of Medical Research.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organisation. The World Health Report: Reducing Risks, Promoting Healthy Life. Geneva: WHO; 2002. [Last accessed on 2015 Dec 21]. Available from: http://www.who.int/whr/2002 . [Google Scholar]
- 2.International Institute for Population Sciences (IIPS), Mumbai and Ministry of Health and Family Welfare. Government of India. Global Adult Tobacco Survey: India (GATS-INDIA); 2009-2010. [Last accessed on 2015 Dec 20]. Available from: http://mohfw.nic.in/WriteReadData/l892s/1455618937GATS%20India.pdf .
- 3.International Institute for Population Sciences (IIPS) and Macro International. 2005-2006. National Family Health Survey (NFHS-3. I. India, Mumbai: IIPS; 2007. [Last accessed on 2015 Dec 18]. Available from: http://www.rchiips.org/nfhs/nfhs3s.html . [Google Scholar]
- 4.Reddy KS, Gupta PC. Report on Tobacco Control in India. New Delhi: Ministry of Health and Family Welfare, Government of India; 2004. [Last accessed on 2015 Dec 18]. http://www.mohfw.nic.in/WriteReadData/l892s/4898484716Report%20on%20Tobacco%20Control%20in%20India.pdf . [Google Scholar]
- 5.Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating Tobacco Use and Dependence: 2008 Update. Quick Reference Guide for Clinicians Rockville, MD: US Department of Health and Human Services Public Health Service. 2009. [Last accessed on 2015 Dec 18]. Available from: http://www.healthquality.va.gov/tuc/phs_2008_quickguide.pdf .
- 6.Babor TF, Higgins-Biddle JC. Brief Intervention for Hazardous and Harmful Drinking: A Manual for Use in Primary Care. Document No. WHO/MSD/MSB/01.6b. World Health Organisation. 2001. [Last accessed on 2015 Dec 18]. Available from: http://www.whqlibdoc.who.int/hq/2001/who_msd_msb_01.6b.pdf .
- 7.WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction. 2002;97:1183–94. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- 8.Humeniuk RE, Henry-Edwards S, Ali RL, Poznyak V, Monteiro M. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for use in Primary Care. Geneva: World Health Organization; 2010. [Last accessed on 2015 Dec 18]. Available from: http://www.whqlibdoc.who.int/publications/2010/9789241599382_eng.pdf . [Google Scholar]
- 9.Miller W, Rollnick S. Motivational Interviewing. 2nd ed. New York, London: Guilford Press; 2002. [Google Scholar]
- 10.Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating tobacco use and dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008. [Last accessed on 2015 Dec 18]. Available from: www.ahrq.gov/clinic/tobacco/treating_tobacco_use08.pdf . [Google Scholar]
- 11.Humeniuk R, Henry-Edwards S, Ali R. Self-Help Strategies for Cutting Down or Stopping Substance Use: A Guide. (Draft Version 11 for Field Testing. Geneva: World Health Organization; 2003. [Last accessed on 2015 Dec 15]. Available from: http://www.whqlibdoc.who.int/publications/2010/9789241599405_eng.pdf . [Google Scholar]
- 12.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 13.Ebbert JO, Patten CA, Schroeder DR. The Fagerström test for nicotine dependence-smokeless tobacco (FTND-ST) Addict Behav. 2006;31:1716–21. doi: 10.1016/j.addbeh.2005.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. Br J Addict. 1992;87:743–54. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- 15.Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: A review. Addiction. 1993;88:315–35. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- 16.Miller W, Sanchez V. Motivating young adults for treatment and lifestyle change. In: Howard G, editor. Issues in Alcohol Use and Misuse by Young Adults. Notre Dame, IN: University of Notre Dame Press; 1993. [Google Scholar]
- 17.Miller W, Zweben A, Di Clemente C, Rychtarik Motivational Enhancement Therapy Manual: A Clinical Resource Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. (Project MATCH Monograph Series) 1992 [Google Scholar]
- 18.Substance Abuse and Mental Health Services Administration. Results from the 2006 National Survey on Drug Use and Health: National Findings (Office of Applied Studies, NSDUH Series H-32, DHHS Publication No. SMA 07-4293) Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2007. [Google Scholar]
- 19.Singh A, Ladusingh L. Prevalence and determinants of tobacco use in India: Evidence from recent Global Adult Tobacco Survey data. PLoS One. 2014;9:e114073. doi: 10.1371/journal.pone.0114073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2008;2:CD000165. doi: 10.1002/14651858.CD000165.pub3. [DOI] [PubMed] [Google Scholar]
- 21.Lancaster T, Stead L. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2004;4:CD000165. doi: 10.1002/14651858.CD000165.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2005;2:CD001292. doi: 10.1002/14651858.CD001292.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev. 2005;2:CD001007. doi: 10.1002/14651858.CD001007.pub2. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Preventive Services Task Force. Counseling and interventions to prevent tobacco use and tobacco-caused disease in adults and pregnant women. U.S. Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2009;150:551–5. doi: 10.7326/0003-4819-150-8-200904210-00009. [DOI] [PubMed] [Google Scholar]
- 25.Murthy P, Murali MB, Hiremath SS. Helping People Quit Tobacco: A Manual for Doctors and Dentists. South East Asia Region: World Health Organization; 2011. [Google Scholar]
- 26.Jayakrishnan R, Uutela A, Mathew A, Auvinen A, Mathew PS, Sebastian P. Smoking cessation intervention in rural Kerala, India: Findings of a randomised controlled trial. Asian Pac J Cancer Prev. 2013;14:6797–802. doi: 10.7314/apjcp.2013.14.11.6797. [DOI] [PubMed] [Google Scholar]
- 27.Kumar MS, Sarma PS, Thankappan KR. Community-based group intervention for tobacco cessation in rural Tamil Nadu, India: A cluster randomized trial. J Subst Abuse Treat. 2012;43:53–60. doi: 10.1016/j.jsat.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 28.Harris SK, Louis-Jacques J, Knight JR. Screening and brief intervention for alcohol and other abuse. Adolesc Med State Art Rev. 2014;25:126–56. [PubMed] [Google Scholar]
- 29.Rani M, Bonu S, Jha P, Nguyen SN, Jamjoum L. Tobacco use in India: Prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tob Control. 2003;12:e4. doi: 10.1136/tc.12.4.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]


