Abstract
Background:
Psychosocial dysfunctions in the various psychosocial areas in chronic schizophrenic patients predict the long-term course, outcome, and quality of life of these patients, which always varies with years of treatment.
Objective:
To know the influence and compare the level of psychosocial dysfunctions and severity of disability burden in chronic schizophrenic patients who are in remission with duration of 5 and 20 years.
Materials and Methods:
The sample was collected from the OPD of Mental Health Institute (COE), S.C.B. Medical College, Cuttack, Odisha, India. This study is a cross-sectional study. A total of 120 remitted schizophrenic patients (60 patients of each group with duration of 5 and 20 years), who fulfilled Nancy Andreasen criteria for Remission were selected for the study. Regional language of dysfunction analysis questionnaire (DAQ) was used to assess the level of psychosocial dysfunctions in personal, familial, social, vocational, and cognitive areas of each patient.
Results:
Qualitative data were analyzed using Chi-square and quantitative data were analyzed using t-test and correlation as a test of significance. Statistically significant differences (P < 0.05) were found in all five domains of DAQ between two groups. Statistically significant difference (P < 0.05) was found between the two groups with respect to severity of the disability.
Conclusion:
This study confirms that there are definite and substantial psychosocial dysfunctions in personal, familial, social, vocational, and cognitive spheres with the advancement of the duration of illness in chronic schizophrenic patients.
Keywords: Chronic schizophrenia, disability, dysfunction analysis questionnaire, National Classification of Occupation 2004, psychosocial dysfunction
INTRODUCTION
The term “psychosocial dysfunction” refers to a change in reference to a particular period, in the life of an individual with respect to age, sex, race, and culture. The functioning of an individual after an illness is always compared with one's own previous level of functioning.[1,2] Psychosocial dysfunction is the dysfunction in the various psychosocial areas such as personal, vocational/occupational, familial and social, which ultimately depends on the cognitive functioning of an individual. In fact, Schizophrenia is a disorder of the brain which affects one's thoughts, feelings, and acts and after a period of years leads to a marked change in personality, occupational disability, cognitive impairment, and poor health.
Dysfunctions in schizophrenic patients refer to lowering of functioning irrespective of whether an adjustment is made with the circumstances or not, whether it is of permanent nature or not and whether it can be corrected in the treatment or not. Hence, after remission of the disease, the different level of dysfunction is a psychological concept, which is concerned with the present functioning of the individual at a particular point of time in comparison to particular reference point in the person's life, without changing one with adjustment, without categorizing it as permanent or temporary and without creating a personal view on curability. Most of the studies in past have focused on the cognitive dysfunctions of schizophrenic patients. However, the other level of dysfunctions which is required for the maintenance of quality of life after reduction of unwanted symptoms are social, personal, vocational, and familial functions. Any disturbances in one or more areas have sufficient impact on the quality of life and daily living of the patients. As most of the patients are treated for a long period with medications, the mental health professionals most of the time neglect the social, personal, vocational, and familial dysfunctions and hence, the interventions accordingly. In the long run, while measuring the “Mental Disability” of these patients, professionals neglect the vocational and cognitive dimensions to a larger extent.
Persons with chronic schizophrenia experience problems in their living, working, social relationships, learning, and employment giving rise to the various level of dysfunctions in different areas according to different sociocultural backgrounds.[3] They have needs related to psychiatric treatment compliance, socialization, vocational training, interpersonal relationships, maintenance of interfamilial relationships, enhancing the skills of daily living, and meaningful employment. All the five areas of dysfunctions (i.e., social, personal, familial, vocational, and cognitive) are intrinsically correlated with each other to such an extent that a particular area cannot be advocated by excluding another area, but the cognitive dysfunction is the predominant area on which other functioning are mostly dependent.
After long years of research on Schizophrenia, it is now universally accepted that psychosocial interventions are an integral part of the comprehensive management of schizophrenia. The previous concept of schizophrenia management, which mostly focused on pharmacotherapy, has now been shifted to psychosocial rehabilitation, because of long-term research in different sociocultural settings.[3,4] While under treatment with pharmacotherapy at a tertiary care setting, the psychosocial rehabilitation is not a reality concept in Indian settings. To maintain the quality of life of these schizophrenic patients, it is highly essential after a period of intervals to assess the different level of psychosocial dysfunctions for proper planning of schizophrenia management schedule in the long-term management.[5,6]
In the Indian context, a cost-effective model of psychosocial rehabilitation has a paramount importance. Because family plays a greater role as a psychosocial rehabilitation center than anything else and no rehabilitation programs are standardized in the Indian context, hence the assessment of the influence of different level of functioning is a most essential component of management.[4] The psychosocial rehabilitation depends mostly on the level of dysfunction at a different level and different years of progression of the disease. For daily living and maintain a good quality of life, the influence of level of dysfunction in different areas will decide how a skilled-based cost-effective training by Mental Health Professionals and Paraprofessionals will be constructed by taking into account the following factors of the patients such as personal hygiene, activities of daily living, interpersonal skills, self-control skills, family relations, money management, job seeking, and job adjustment skills.[3,7]
In recent times, the World Health Organization estimated that schizophrenia is the 5th leading worldwide cause of global disease burden in 2004 among males and 6th among females with 2.8 percent of total years lived with the disease in males and 2.6 percent in females.[8]
In recent years by searching the database, such as Medline, Embase, Cochrane Library, and Google Scholar in new dimensions of schizophrenia, i.e., “Humanistic Dimension” was more popularly used to define the difference in the level of dysfunctions.[9] Experts suggested focusing on the quality of life, depression, treatment side effects, caregiver burden, cognitive functioning, social impairment, suicide, homelessness, stigmatization, morbidity, mortality, lifestyle, physical performance, violence, and abortion/pregnancy of these chronic schizophrenic patients in their humanistic dimension. Most of the dimensions are overlapping, and all are interlinked. For example, impaired cognitive functioning can lead to stigma and lack of empowerment, which may lead to depression causing physical, emotional, and economic distress that is likely to negatively affect a patient's quality of life and ultimately to provoke suicide in some cases.
In this study, we emphasized the above mentioned five dimensions which are most important components of quality of life. This study was conducted to assess the level of dysfunctions in all these areas of patients.
OBJECTIVE OF THE STUDY
To compare the level of psychosocial dysfunctions between remitted schizophrenic patients with duration of 5 years and 20 years
To assess the influence of disability burden between these two groups of remitted schizophrenic patients.
MATERIALS AND METHODS
Type of research design
The study was a cross-sectional descriptive study design.
Procedure
This study was conducted in the OPD of Mental Health Institute (COE), S.C.B. Medical College, Cuttack, Odisha, India. It is one of the largest tertiary care hospitals of eastern India providing service to populations of Eastern parts of the country. A total of 120 samples (60 patients in each group with 5 years and 20 years duration) were selected on the purposively basis by following the inclusion and exclusion criteria. The patients who already have been diagnosed as Schizophrenia as per International Classification of Diseases (ICD-10) criteria at the institute, having a duration of at least 5 years, were screened out from OPD of Mental Health Institute by using Nancy Andreasen criteria of Schizophrenia in remission. In consecutive two visits of these patients at 3 months interval, who earned a cutoff score of remission were finally selected for the study. The study was conducted from July 2015 to March 2016. The information was collected from the patients as well as from the caregivers. Those who had interested in taking part in this study were included in this study. Through semi-structured interview, all information were recorded in a scientifically designed structured pro forma, i.e., sociodemographic data sheet. Then dysfunction analysis questionnaire (DAQ)-Odia version transliteration was administered to each patient to find out the level of psychosocial dysfunctions in various spheres of the day to day life. The consent was taken from the patients and the caregivers to take part in the study.
Sample design
Purposive sampling method was used for selecting the patients for the study. A total of 120 patients (60 patients in each group) were taken for the study.
Inclusion criteria
Patients who are diagnosed as Schizophrenia as per ICD-10 criteria
Those who are in between age range of 20–55 years
Patients with duration of illness of 5 years and 20 years are included
Those who are fulfilled Nancy Andreasen criteria for schizophrenia in remission
Key relative/caregiver is defined as a family member living with the patient for minimum 1 year and present during onset of abnormal behavior and actively involved in patient care
Those who are willing to provide informed consent to participate in the study.
Exclusion criteria
Persons with other comorbid psychiatric conditions and organic mental conditions
Persons with comorbid substance use
Persons with other comorbid physical illness.
Tools used
Sociodemographic data sheet: A structured pro forma was developed and used in this study to collect information about various sociodemographic variables, i.e., age, sex, education, religion, occupation, marital status, monthly income, socioeconomic status, etc.
B.G. Prasad's socioeconomic status scale (As per consumer price index for Industrial Workers of November 2015): This scale was used to determine the socioeconomic of these patients
ICD-10 criteria for the diagnosis of Schizophrenia
Nancy Andreasen criteria for patients with schizophrenia in remission: Defined remission according to positive and negative syndrome scale (PANSS) operational criteria set up by the Remission in schizophrenia working group. The symptomatic criterion includes eight core PANSS items (delusion, unusual thought content, hallucinatory behavior, conceptual disorganization, mannerism/posturing, blunted affect, social withdrawal, lack of spontaneity) with a score ≤3. The duration criterion is symptomatic remission maintenance over 6 consecutive months[10]
PANSS: This is a 30 item, 7-point rating instrument that evaluates positive (7 items), negative (7 items), and general psychopathology symptoms (16 items) of an individual. It was published in 1987 by Kay et al.[11] The PANSS is a relatively brief interview, requiring 45–50 min to administer. Each item on the PANSS is accompanied by a complete definition as well as detailed anchoring criteria for all seven rating points, which represent increasing levels of psychopathology: 1 = absent, 2 = minimal, 3 = mild, 4 = moderate, 5 = moderate-severe, 6 = severe, and 7 = extreme.
-
Dysfunction analysis questionnaire (DAQ)
The original scale of Hindi version has been developed by Pershad et al.[12] This scale is used to assess various psychosocial dysfunctions of an individual. This scale has highly satisfied test-retest and split half reliabilities that ranged from 0.77 to 0.97. In this study, Odia version DAQ has been used. This scale consists of 50 items grouped into five areas, i.e., Social, Vocational, Personal, Familial, and Cognitive. Each item has five alternate answers and these are scored in accordance to the scoring system. Higher the score, greater is the dysfunction.
-
National Classification of Occupations 2004
It is used in this study to understand the role of occupations in schizophrenia. The National Classification of Occupations 2004 (NCO 2004) is an updated classification developed by the Government of India (Directorate General of Employment and Training) based on the International Labour Organisation classification of occupations. It has a hierarchical system which allows for the coding of all the occupations at multiple levels. In this study, only the first level of classification, i.e., division has been used. The occupations are divided into 10 mutually exclusive classes of which 9 are numbered from 1 to 9. The tenth group is classified as X division or undefined group, i.e., those occupations which cannot be listed in divisions 1–9 are classed to this division (1: Legislators, Senior officials, Managers; 2: Professionals; 3: Technicians and Associate Professionals; 4: Clerks; 5: Service Workers and Shop Market sales worker; 6: Skilled agricultural and fishery workers; 7: Craft and related trade workers; 8: Plant and machine operators and assemblers; and 9: Elementary occupations; X: Workers not classified [Class 0 in this study]). In this study, the X division has been coded as 0 division and was used to class students, homemakers, and those without any explicit employment. Another distinct advantage of the NCO 2004 is that the hierarchical classification has been done taking into account the educational status of the individual with respect to each of the occupations or trades. Thus, it automatically factors into itself the educational attainment of the person.[13]
Method of data analysis
All the qualitative data were analyzed using Chi-square and quantitative data were analyzed using t-test and correlation as test of significance. Data analysis was done by SPSS, Version 11.0 (SPSS Inc., Illinois, USA).
Ethical clearance
Institutional Ethics Committee clearance was obtained before the commencement of the study.
RESULTS
The study was designed to probe the DAQ scores in the individual patient in all five domains of DAQ. The study subjects were divided into two groups based on the duration of their disease; 5 years and 20 years. Each group had 60 patients each. Thus, in all 120 patients were recruited for this study.
The sociodemographic parameters of the study subjects were compared among the two groups. As shown in Table 1, there was no statistically significant difference between the study subjects in the two groups. The only exception was the age distribution of the study subjects in the two groups. The difference in the mean age of the patients in both the groups was found to be statistically significant (t = 4.38; df = 118; P < 0.05). This is accounted for by the fact that the patients in both the study groups had an inherent time lag of 15 years, i.e. the duration of the disease, which was the defining characteristic of the comparison groups. This time lag would inevitably lead to a difference in the study groups with respect to age, even though the study is cross-sectional in design.
Table 1.
Sociodemographic characteristics of the study subjects
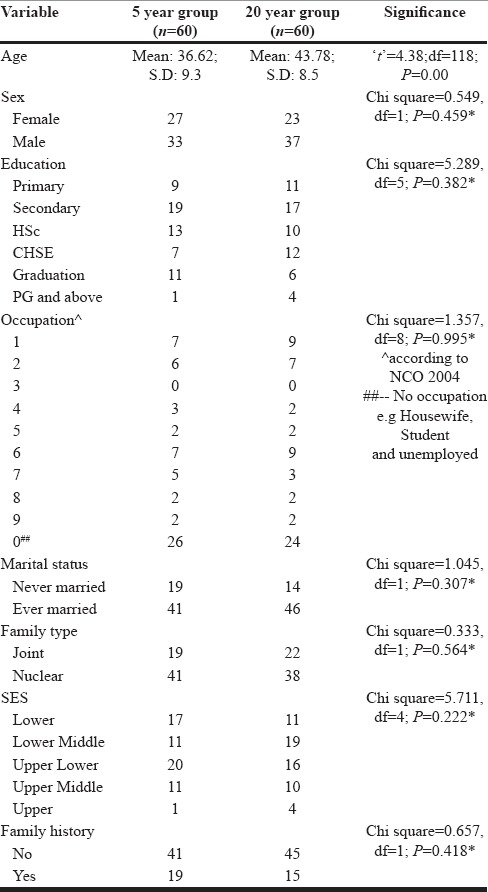
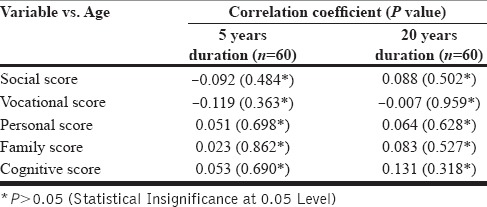
To see the effect of age on DAQ scores, a test of correlation was done for the ages of the individual patients and their respective DAQ scores in the five domains for each individual patient in both the study groups. No statistically significant correlation (P > 0.05) was noted in any of the DAQ domains indicating that there was no association between age and scores in the individual patient [Table 2].
Table 2.
Correlation between patients’age and score in the two study groups
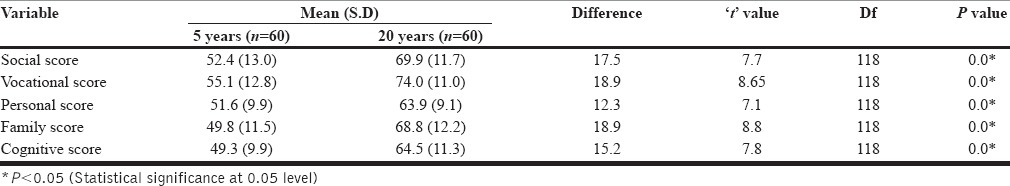
The DAQ scores were calculated in five different domains for each patient, namely, Social score, Vocational score, Personal score, Family score, and Cognitive score. The scores in all five domains are found to be higher for patients with 20 years disease compared to patients with 5 years disease. This difference was found to be statistically significant (social domain: t = 7.7, df = 118, P < 0.05; vocational domain: t = 8.65, df = 118, P < 0.05; personal domain: t = 7.1, df = 118, P < 0.05; family domain: t = 8.8, df = 118, P < 0.05; cognitive domain: t = 7.8, df = 118, P < 0.05) [Table 3].
Table 3.
Scores in the different domains in the study groups
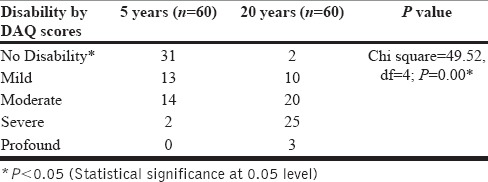
The mean scores were averaged in each domain for all the patients in both the study groups. For each patient a further average score was calculated by computing the arithmetic mean for all five domains. This was then used categorize the level of disability for each patient as normal (no disability), mild, moderate, severe, and profound. Higher DAQ scores indicate greater dysfunction or disability. The comparison of the level of disability for each of the study groups is shown in Table 4. The table shows increasing severity of disability in patients with 20 years disease compared to patients with 5 years disease. This difference was found to be statistically significant (Chi-square = 49.52, df = 4; P < 0.05).
Table 4.
Disability in the study groups according to DAQ scores
DISCUSSION
This research has been constantly emphasized on the different level of functioning in patients at different years of interval. Most of the research studies have been focused on cognitive dysfunctions of schizophrenia as the priority area than other level of dysfunction. The present study has given importance to all the five areas of functioning, (i.e., personal, vocational, familial, social, and cognitive) to maintain quality of life and daily living which ultimately is the criteria for deciding the management plan including pharmacotherapy, family therapy, and psychosocial intervention.
The finding of the present study investigation reveals that the schizophrenic patients of duration of 20 years have substantial level of dysfunctions in personal, vocational, familial, social, and cognitive areas than the schizophrenia patients of duration of 5 years which indicates that with advancement of years of duration of disease in spite of pharmacotherapy the level of psychosocial dysfunction in all the major areas increase with time which needs a definitive psychosocial rehabilitation in Indian context.[14,15] Hence, with increase in duration of disease, the schizophrenic patients have global disability burden which has focused on a comprehensive and cost effective mental health management plan in a particular sociocultural setting. This finding is consistent with the results of disabilities in patients of schizophrenia, done by Siddiqui et al.[16] in Indian context and by Goreishizadeh et al.[17] and Li et al.[18] in other cultural settings after assessment of psychosocial disabilities of schizophrenic patients.
Despite 50 years of pharmacological and psychosocial interventions, schizophrenia remains one of the leading causes of disability. The inability to function in everyday settings includes deficits in performance of social, occupational, and independent living activities. Dysfunctional lifestyles including sedentary behavior and lack of physical activity prevail while treatment with adipogenic psychotropic medication interacts with poor performance in screening, monitoring, and intervention that result in shortening of life expectancies by 25–30 years. Disability interferes with self-care and medical care, further worsening physical health to produce a vicious cycle of disability.[19]
Schizophrenia is a chronic mental disorder that leads to disability in several aspects of the individual's personal, social, and occupational functioning.[20,21,22] A study conducted by Akinsulore et al. found out that the patients with chronic schizophrenia reported greater disability in an individual's personal, social, and occupational life.[23] In this study, disability burden in patients with chronic schizophrenia having duration of more than 20 years is much more than schizophrenia patients having duration of 5 years.
Here, the age effect has been found to be no role to play in causing disability and dysfunction in all spheres. Patients with longer duration of disease who are in the higher age group having increased level of psychosocial dysfunctions are direct effect of the disease duration rather than the effect of their chronological age. In Indian context to maintain a family, the money management, job seeking, job adjustment skills, and adherence to job for maintenance of family plays a major role in the long run to maintain the familial and social relationships.
Although in the past most attention was paid to psychopathology, these days outcome parameters such as cognitive and occupational performance, emotional stability, quality of life, and psychosocial functioning are being recognized as important determinants of treatment success. Instead of only reducing the symptoms, therapy with antipsychotics must attain higher goals such as remission and recovery today.[24]
CONCLUSION
There are definite dysfunctions in personal, familial, social, vocational, and cognitive spheres with advancement of years of illness in chronic schizophrenic patients
The global disability burden because of schizophrenia in terms of personal and familial is more in the long term illness than short term illness
The occupational inefficiency is manifested in all levels of skilled and nonskilled workers with advancement of years because of dysfunctions in all spheres with advancement of illness
Although the psychosocial dysfunction and disability is a burden for chronic schizophrenic patients in spite of treatment, in addition with advancement of years. The age effect which has a definitive role in cognition and other areas also contributing for increasing the disability burden
Hence, a cost-effective comprehensive Indian model of psychosocial rehabilitation of chronic schizophrenia patients is a future perspective for these chronic schizophrenic patients.
Limitations
The sample was collected/taken from a tertiary care hospital which cannot represent the community as a whole
This study was a cross-sectional study due to limited time period which can be extended for a longitudinal follow-up to measure the level of dysfunctions
As chronic stable patients were included in this study, data from patients with more severe illness are missing.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chadda RK. Social support and psychosocial dysfunction in depression. Indian J Psychiatry. 1995;37:119–23. [PMC free article] [PubMed] [Google Scholar]
- 2.Verma SK, Pershad D. Measurement of change in psychosocial functioning following illness and therapeutic intervention. Indian J Clin Psychol. 1989;16:64–7. [Google Scholar]
- 3.Chowdur R, Dharitri R, Kalyanasundaram S, Suryanarayana RN. Efficacy of psychosocial rehabilitation program: The RFS experience. Indian J Psychiatry. 2011;53:45–8. doi: 10.4103/0019-5545.75563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thara R. Cost of illness of schizophrenia – Perspective from an NGO. Indian J Psychiatry. 2005;47:205–17. doi: 10.4103/0019-5545.43054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brekke JS, Ansel M, Long J, Slade E, Weinstein M. Intensity and continuity of services and functional outcomes in the rehabilitation of persons with schizophrenia. Psychiatr Serv. 1999;50:248–56. doi: 10.1176/ps.50.2.248. [DOI] [PubMed] [Google Scholar]
- 6.Halford WK, Hayes R. Psychosocial rehabilitation of chronic schizophrenic patients: Recent findings on social skill training and family psychoeducation. Clin Psychol Rev. 1991;11:23–44. [Google Scholar]
- 7.Nagaswami V. Integration of psychosocial rehabilitation in national health care programmes. J Psychosoc Rehabil Ment Health. 1990;14:53–65. [Google Scholar]
- 8.Leucht S, Burkard T, Henderson J, Maj M, Sartorius N. Physical illness and schizophrenia: A review of the literature. Acta Psychiatr Scand. 2007;116:317–33. doi: 10.1111/j.1600-0447.2007.01095.x. [DOI] [PubMed] [Google Scholar]
- 9.Millier A, Schmidt U, Angermeyer MC, Chauhan D, Murthy V, Toumi M, et al. Humanistic burden in schizophrenia: A literature review. J Psychiatr Res. 2014;54:85–93. doi: 10.1016/j.jpsychires.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 10.Andreasen NC, Carpenter WT, Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: Proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162:441–9. doi: 10.1176/appi.ajp.162.3.441. [DOI] [PubMed] [Google Scholar]
- 11.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 12.Pershad D, Verma SK, Malhotra A, Malhotra S. Manual for Dysfuntion Analysis Questionnaire (DAQ) 2nd ed. Agra: National Psychological Corporation; 2004. [Google Scholar]
- 13.National Classification of Occupation. 2004. Available from: http://www.dget.nic.in/upload/uploadfiles/files/publication/Code%20Structure.pdf .
- 14.Thomas JK, Suresh Kumar PN, Verma AN, Sinha VK, Andrade C. Psychosocial dysfunction and family burden in schizophrenia and obsessive compulsive disorder. Indian J Psychiatry. 2004;46:238–43. [PMC free article] [PubMed] [Google Scholar]
- 15.Suresh Kumar PN. Impact of vocational rehabilitation on social functioning, cognitive functioning, and psychopathology in patients with chronic schizophrenia. Indian J Psychiatry. 2008;50:257–61. doi: 10.4103/0019-5545.44747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siddiqui RS, Verma SK, Pershad D. Cognitive and psychosocial dysfunction in chronic schizophrenia. Indian J Disabil Rehabil. 1992;6:1–6. [Google Scholar]
- 17.Goreishizadeh M, Mohagheghi A, Farhang S, Alizadeh L. Psychosocial disabilities in patients with schizophrenia. Iran J Public Health. 2012;41:116–21. [PMC free article] [PubMed] [Google Scholar]
- 18.Li XJ, Wu JH, Liu JB, Li KP, Wang F, Sun XH, et al. The influence of marital status on the social dysfunction of schizophrenia patients in community. Int J Nurs Sci. 2015;2:149–52. [Google Scholar]
- 19.Strassnig M, Harvey PD. Treatment of obesity and disability in schizophrenia. Innov Clin Neurosci. 2013;10:15–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Kiang M, Light GA, Prugh J, Coulson S, Braff DL, Kutas M. Cognitive, neurophysiological, and functional correlates of proverb interpretation abnormalities in schizophrenia. J Int Neuropsychol Soc. 2007;13:653–63. doi: 10.1017/S1355617707070816. [DOI] [PubMed] [Google Scholar]
- 21.Villalta-Gil V, Vilaplana M, Ochoa S, Haro JM, Dolz M, Usall J, et al. Neurocognitive performance and negative symptoms: Are they equal in explaining disability in schizophrenia outpatients? Schizophr Res. 2006;87:246–53. doi: 10.1016/j.schres.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 22.Schaub D, Brüne M, Jaspen E, Pajonk FG, Bierhoff HW, Juckel G. The illness and everyday living: Close interplay of psychopathological syndromes and psychosocial functioning in chronic schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2011;261:85–93. doi: 10.1007/s00406-010-0122-1. [DOI] [PubMed] [Google Scholar]
- 23.Akinsulore A, Mapayi BM, Aloba OO, Oloniniyi I, Fatoye FO, Makanjuola RO. Disability assessment as an outcome measure: A comparative study of Nigerian outpatients with schizophrenia and healthy control. Ann Gen Psychiatry. 2015;14:40. doi: 10.1186/s12991-015-0079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Juckel G, Morosini PL. The new approach: Psychosocial functioning as a necessary outcome criterion for therapeutic success in schizophrenia. Curr Opin Psychiatry. 2008;21:630–9. doi: 10.1097/YCO.0b013e328314e144. [DOI] [PubMed] [Google Scholar]


