Abstract
Introduction:
Alzhiemers disease and Frontotemporal dementia are common neurodegenerative dementias with a wide prevalence. Falls are a common cause of morbidity in these patients. Identifying subclinical involvement of these parameters might serve as a tool in differential analysis of these distinct parameters involved in these conditions and also help in planning preventive strategies to prevent falls.
Patients and Methods:
Eight patients in age and gender matched patients in each group were compared with normal controls. Standardizes methods of gait and balance aseesment were done in all persons.
Results:
Results revealed subclinical involvement of gait and balancesin all groups specially during divided attention. The parameters were significantly more affected in patients. Patients with AD and FTD had involement of over all ambulation index balance more affected in AD patients FTD patients showed step cycle, stride length abnormalities.
Discussion:
There is balance and gait involvement in normal ageing as well as patients with AD and FTD. The pattern of involvement in AD correlates with WHERE pathway involvement and FTD with frontal subcortical circuits involvement.
Conclusion:
Identification the differential patterns of involvement in subclinical stage might help to differentiate normal ageing and the different types of cortical dementias. This could serve as an additional biomarker and also assist in initiating appropriate training methods to prevent future falls.
Keywords: Alzheimer disease, balance impairment, frontotemporal dementia, gait impairment, posturography
INTRODUCTION
Alzheimer disease (AD) is a neurodegenerative disorder characterized by progressive loss of recent and episodic memory and other cognitive functions, affects 35 million people worldwide.[1] Early diagnosis is important to initiate early treatment strategies to improve disability adjusted life years and reduce caregiver burden. The other type of cortical dementia is frontotemporal dementia (FTD) which manifests little more early and manifests often with neuropsychiatric manifestations. These two conditions are often misdiagnosed as each other or as purely psychiatric illness which delays the diagnosis. Morbidity and mortality are often due to secondary factors than the disease itself. Cortical structures are wired to subcortex by various functional circuits and therefore there is a possibility that subcortical signs which are easier to measure may be involved subclinically and if any differential pattern is observed it might help as an additional biomarker in early specific diagnosis as AD or FTD and also initiate appropriate treatments to delay progression to serious disability.
Gait and balance are the product of successful integration of various posture control mechanisms and locomotion. Neurological disorders at any level can compromise the biomechanics of the same as it involves several complex mechanisms. Posture control needs maintaining the center of mass over the BOS all through the gait cycle. Dynamic balance needs cerebellum, vestibular system, and unconscious reactive reflexes such as long loop reflexes. Standing balance needs sensory information with reference to environment generated by vision, proprioception, and vestibular system. Because of the frontal-subcortical circuits breaking down in FTD and WHERE dorsal pathway dysfunction in Ad, both these disorders are likely to have gait and balance-related problems.
Older persons with cognitive dysfunction are especially vulnerable for gait and balance problems resulting in repeated falls because of the associated multiaxial “dysfunction involving not only cognition but also, joints, ligaments, tendons, vision, and hearing”[2] Patients with attention and cognitive disorders are at risk of disequilibrium in this automatic, unconscious act of walking due to inability to concentrate in dual tasking.[3,4,5,6,7,8,9,10,11,12,13,14] There is evidence for abnormal equilibrium in Ad and motor dysfunction in FTD.[15,16,17] This can increase morbidity significantly in these patients.[18,19,20,21,22] The changes are expected to be subclinical in the early phase, and hence quantitative measurements will be of great help in understanding the pattern which apart from probably serving as a easily accessible biomarker, might also serve in initiating rehabilitatory tools early in the course of disease.
PATIENTS AND METHODS
Twenty-four male subjects with 50–70 years of age, 8 in each group of probable bvFTD diagnosed by revised consensus criteria,[23] probable AD, diagnosed by ADs association criteria,[24] and healthy volunteers as controls. The FTD and AD groups were recruited from Outpatient Department of Neurology and Geriatric Clinic, controls from the community. Informed consent was obtained from all and ethical clearance received from the Institute Ethical Committee. Subjects with orthopedic, visual deficit, other neurological conditions, and cardiovascular ailments were excluded. All demographic factors including age, gender, and height, weight are recorded.
The balance was measured by Biodex Balance Master Incorp., USA, using dynamic posturography, in single and dual tasks and gait with Biodex Gait Trainer.
The equipment has a posturography-based force platform which provides objective balance measurements in two situations, i.e., (1) dynamic balance and (2) limits of stability (LOS). It has a circular platform and a display monitor kept in front of the subject to see and get the feedback about their status of standing. The platform becomes unstable and the subject's experience wobbling. The change in the center of pressure due to this will be displayed in the monitor as a biofeedback as the cursor moves from the epicenter of the grid.
Each subjects “base of support” requirement for the perturbed stand is tested, and subjects are asked to adjust their BOS making the tilted platform to the neutral and stable position. They can utilize the feedback about their stand position from the display monitor and instructed to target at the innermost circle or epicenter of the grid. At the end, BOS is recorded including measurement of the angle of foot deviations and during the process.
Dynamic balance - Single task
Three trials each of 20 s duration are done. The amount of deviation from original BOS and direction of deviation were recorded without using handrail support. The test results contain overall balance index (OBI), anteroposterior index (API), i.e., amount of front to back sway, mediolateral index (MLI), i.e., side to side sway. Higher the score indicates poorer the balance.
Limits of stability - Single task
In the second part of balance test, the subjects ability to come back to the original BOS after a self-initiated sway in eight different direction, namely, (1) forward (F), (2) backward, (3) right, (4) left, (5) forward right, (6) forward left, (7) backward right, and (8) backward left was tested. The maximum overall score, individual direction score was 100 with the maximum time of 300 s. Higher the score and shorter the time taken indicates better the balance.
Procedure
The platform becomes unstable, and the subject sees a square box in the display monitor, the subjects has to shift the body weight toward the direction of the box so that the cursor moves and get inside the box and hold for 2 s. Then move to the direction where the next box appears. The display of the boxes appears in such a way that the subject needs to come back to the first box after completing the individual box in a different direction. The maximum time to complete the task is 300 s. The result generated consists of overall balance, forward, backward, forward right, forward left, backward right, backward left, and time take to complete the test.
Dual task
In dual task, the subject performs dynamic balance, LOS task along with cognitive task and repeated after a rest period for 2 min from the single task. The cognitive task includes digital subtraction of 3, 2, from 100 in dynamic balance, LOS tasks, respectively.[25,26] The patients are expected to utilize the visual feedback to obtain balance. A safety harness protects the subject from falling.
Gait assessment
The subjects gait was measured by Biodex Gait Trainer USA Incorp. The persons recruited had to walk for 2 min in a sensor-based treadmill at a comfortable speed. A safety harness was provided to protect the person from falling. Kinematic data includes gait speed, stride and step length, coefficient variation of the steps (CV) were gathered. After a rest period of about 2 min, the test was administered for the second time for a dual task where the subject counted backward from 100 as a cognitive task[27] while walking on a treadmill. The result contains total walking distance, average walking speed, average step cycle, average step length, CV of the right and left leg. Higher the score in gait parameter indicates better gait stability, however, increased coefficient variation of steps indicate poor gait stability.
RESULTS
The Shapiro–Wilkins test was conducted to test the normality of the parameters. Descriptive analysis was done for age, body mass index, education in years. Within group analysis of single versus dual task was analyzed with paired t-test. One-way ANOVA was conducted to reveal the difference between groups, followed by post hoc test with Bonferroni correction.
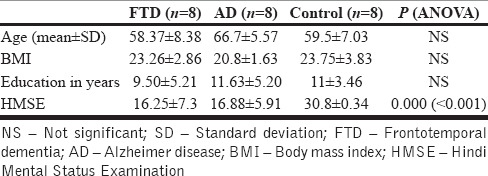
The mean age of FTD group = 58.37 ± 8.38; AD group = 66.7 ± 5.5; Control group = 59.5 ± 7.03, all the subjects were male (8 in each group), the Hindi Mental Status Examination score of FTD and AD group were significantly lower than the controls [Table 1].
Table 1.
Age, body mass index, HMSE score, education of patients with FTD and AD
Within group comparison of single versus dual
Dynamic balance
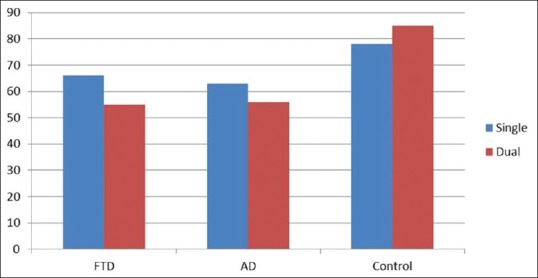
The OBI and API of the dynamic balance of FTD group and control group significantly differed between single versus dual task. However, AD group had significant difference in mediolateral (MLI) stability index only [Table 2 and MLI score in Figure 1].
Table 2.
Within group single task versus dual task-balance measurement
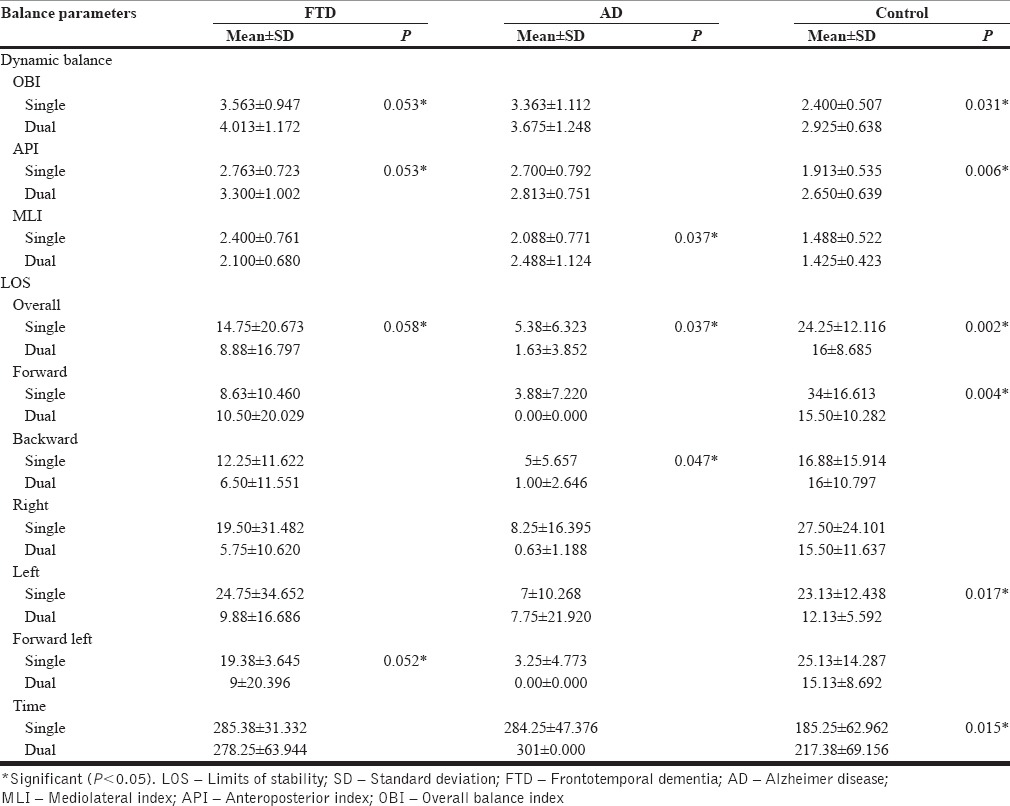
Figure 1.
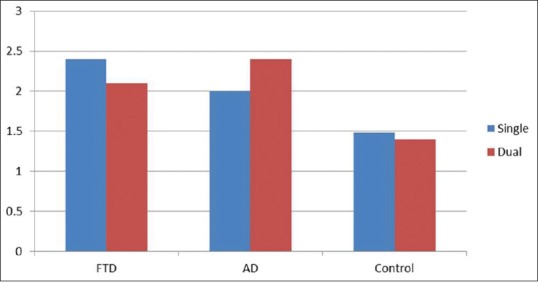
Dynamic balance showing significant mediolateral instability in Alzheimer diseases. FTD – Frontotemporal dementia; AD – Alzheimer disease
Limits of stability
All the three group had significant difference in overall LOS score between single vs. dual task however the sub-component of LOS revealed FTD patients had problem balancing on forward lateral direction and control group had problem in forward, left direction whereas the AD group had significant difficulty in backward direction [Table 2 and overall LOS score in Figure 2].
Figure 2.
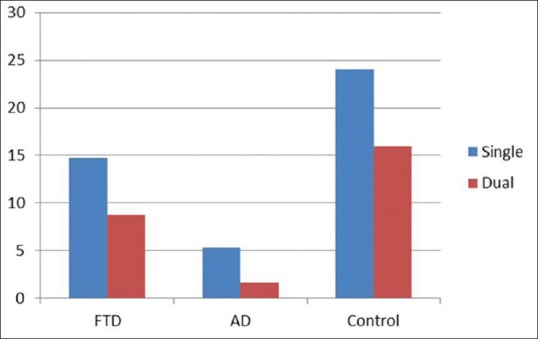
Overall limits of stability performance between single vs dual among frontotemporal dementia, AD and Controls. All the three group performed poorly in dual task. FTD – Frontotemporal dementia; AD – Alzheimer disease
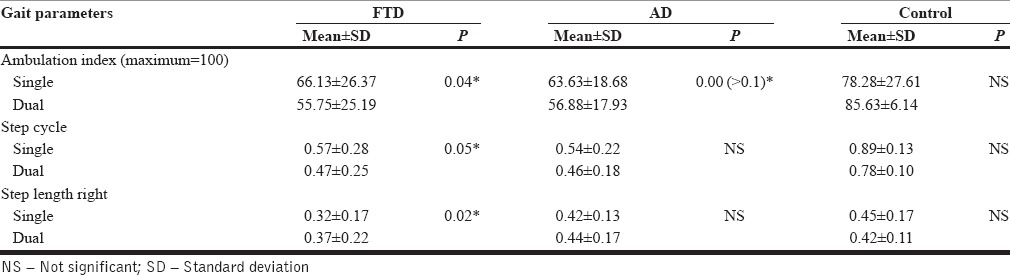
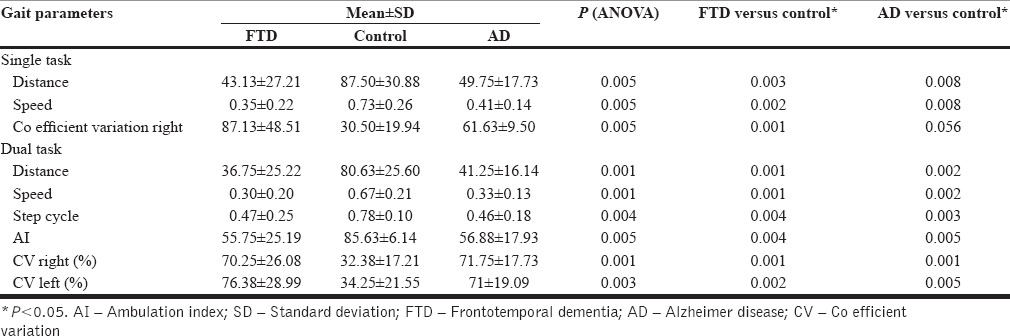
Gait analysis
FTD, AD group, performed poorly in dual task gait analysis while the control group showed no significant worsening of gait. Ambulation index (AI) is a cumulative score of overall gait performance which is found to be low on dual task for both dementias [Figure 3]. In addition, FTD group had significant reduction of step cycle, step length especially on the right side [Table 3].
Figure 3.
Ambulation index score of frontotemporal dementia, Alzheimer disease and controls. Both frontotemporal dementia and Alzheimer disease had poor score in dual task. FTD – Frontotemporal dementia; AD – Alzheimer disease
Table 3.
Comparison of parameters in patients with FTD and AD during single and dual tasking
Between group comparisons
Dynamic balance - Single task
FTD group had a significant worsening of balance in comparison with control group in all subcomponent of dynamic balance, i.e., OBI, API, and MLI. The Alzheimer's group had worsening of balance in OBI, API only. There was no significant difference between FTD and AD group on all parameters of dynamic balance. This denotes that both FTD and AD have a deficit in dynamic balance than control group [Table 4].
Table 4.
Between group comparison of balance-single task
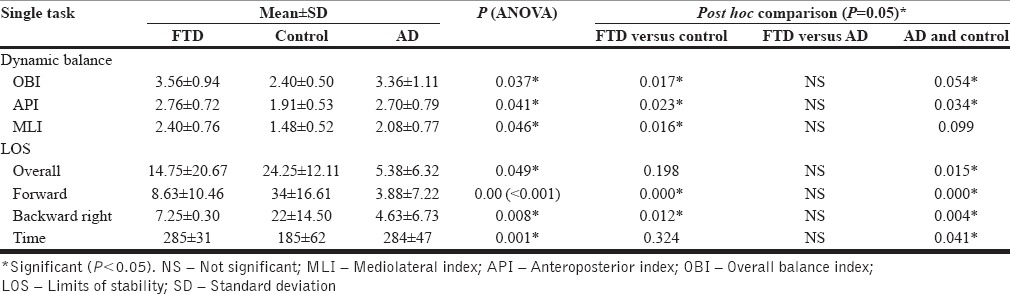
Limits of stability - Single task
Alzheimer group had a significant deficit in overall LOS score in comparison with controls. FTD group had no deficit in overall LOS score except few directions wise deficit than controls. FTD group showed deficit in forward, backward right direction (BR) than controls whereas AD group had deficit in overall, forward (F), backward (B), forward right (FR), forward left (FL), and backward right (BR) direction. Both FTD and AD groups consumed more time to complete the task than the controls [Table 4 and Figure 4].
Figure 4.
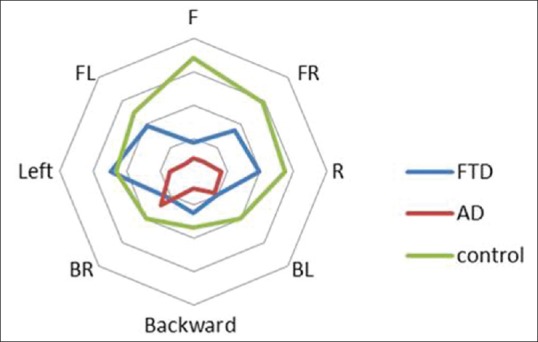
Between group single task analysis of limits of stability. Alzheimer diseases performed worst in various direction. LOS – Limits of stability; FR – Forward right; R – Right; L: Left; BL – Backward left; FL – Forward left; F – Forward; B – Backward; BR – Backward right
Dynamic balance - Dual task
The OBI was significantly affected between FTD and control group. Mediolateral stability index (MLI) was significantly affected between AD and controls [Table 5].
Table 5.
Dual task balance analysis
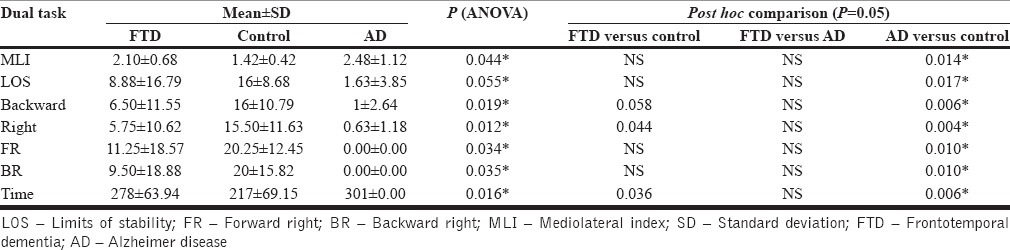
Limits of stability - Dual task
Overall LOS, forward, backward, right, forward right (FR), backward right (BR), was significantly reduced, consumed more time to complete the task in AD group compare to controls. FTD found to have issues only in backward, right directions and consumed more time complete the task than the controls [Table 5 and Figure 5].
Figure 5.
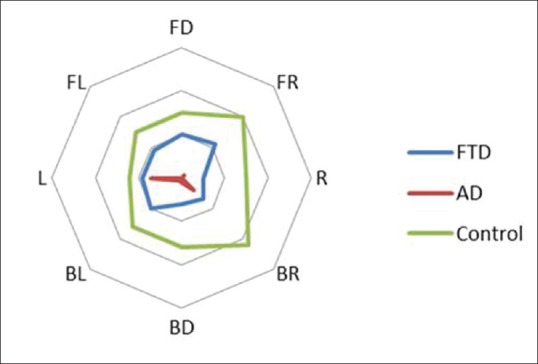
Between group dual task analysis of limits of stability. Alzheimer diseases performed worst in various direction (P = 0.05). Lower the value indicates poorer the balance. LOS – Limits of stability; FR – Forward right; BR – Backward right; MLI – Mediolateral index; FTD – Frontotemporal dementia; AD – Alzheimer disease; R – Right; L – Left; FD – Forword; – BL – Backward left; FL – Forward left
Gait analysis
The gait parameters such as distance walked, speed, step cycle, CV of steps in the right, left leg, and AI were affected in FTD and AD from controls in single, dual task gait [Table 6].
Table 6.
Gait parameters in patients with FTD vs controls and AD vs controls
DISCUSSION
Even though AD and FTDs are predominantly concerned with cognitive functions balance and gait are significantly affected subclinically in both groups compared to controls. Controls also had problems during dual tasking in all parameters indicating the role of divided attention in gait and balance in even healthy aging. However, patients with FTD had significant dynamic balance component abnormalities evidenced by higher value in OBI and API sparing MLI, patients with AD, had poor scores during dual task score in MLI only, sparing OBI and MLI.
LOS analysis, the individual direction wise analysis, persons with FTD revealed poor score in Forward left direction and AD had poor score in backward direction. The overall LOS score did not show any differentiation as the entire three group had poor score in the dual task.
Single versus dual task gait performance
Patients with FTD showed a reduction of step cycle, and step length and overall gait score, i.e., AI. The AD subjects AI score too significantly reduced in dual task though there was no specific gait parameters affected.
The between group
Both FTD and AD patients have balance and gait difficulties than controls in single as well as dual task but AD seems to be having deficit more on balance especially LOS component of balance.
CONCLUSION
This study reveals balance and gait problems in normal elderly, as well as patients with AD and FTD during dual tasking indicating the role of divided attention. However, the abnormality is significantly more in patients with FTD and AD. Patients with FTD and AD have abnormalities in overall AI, but patients with FTD have significant abnormalities in stride length and step cycle which is unaffected in AD. With reference to balance, all parameters are uniformly affected in FTD, but mediolateral balance is most affected in AD. Patients with FTD have a tendency to tilt forward, but AD have tendency to tilt backward. This unique information indicates a differential pattern of balance and gait impairment subclinically in cortical dementias. Uniform but moderate involvement in FTD can be explained by the role of frontal-subcortical circuits as the cause of impairment in FTD and the sensory WHERE pathway involvement in patients with AD. These differences might serve as a marker to differentiate these two conditions in the early stages. Postural stability training early in patients with AD and gait training in patients with FTD might help in delaying future development of falls in these patients. However, the study needs to be repeated in a larger population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Borson S, Raskind MA. Clinical features and pharmacologic treatment of behavioral symptoms of Alzheimer's disease. Neurology. 1997;48(5 Suppl 6):S17–24. doi: 10.1212/wnl.48.5_suppl_6.17s. [DOI] [PubMed] [Google Scholar]
- 2.Sudarsky L. Geriatrics: Gait disorders in the elderly. N Engl J Med. 1990;322:1441–6. doi: 10.1056/NEJM199005173222007. [DOI] [PubMed] [Google Scholar]
- 3.Alexander NB, Mollo JM, Giordani B, Ashton-Miller JA, Schultz AB, Grunawalt JA, et al. Maintenance of balance, gait patterns, and obstacle clearance in Alzheimer's disease. Neurology. 1995;45:908–14. doi: 10.1212/wnl.45.5.908. [DOI] [PubMed] [Google Scholar]
- 4.Allali G, Assal F, Kressig RW, Dubost V, Herrmann FR, Beauchet O. Impact of impaired executive function on gait stability. Dement Geriatr Cogn Disord. 2008;26:364–9. doi: 10.1159/000162358. [DOI] [PubMed] [Google Scholar]
- 5.Allali G, Dubois B, Assal F, Lallart E, de Souza LC, Bertoux M, et al. Frontotemporal dementia: Pathology of gait? Mov Disord. 2010;25:731–7. doi: 10.1002/mds.22927. [DOI] [PubMed] [Google Scholar]
- 6.Allan LM, Ballard CG, Burn DJ, Kenny RA. Prevalence and severity of gait disorders in Alzheimer's and non-Alzheimer's dementias. J Am Geriatr Soc. 2005;53:1681–7. doi: 10.1111/j.1532-5415.2005.53552.x. [DOI] [PubMed] [Google Scholar]
- 7.Beauchet O, Annweiler C, Dubost V, Allali G, Kressig RW, Bridenbaugh S, et al. Stops walking when talking: A predictor of falls in older adults? Eur J Neurol. 2009;16:786–95. doi: 10.1111/j.1468-1331.2009.02612.x. [DOI] [PubMed] [Google Scholar]
- 8.Bridenbaugh SA, Kressig RW. Motor cognitive dual tasking: Early detection of gait impairment, fall risk and cognitive decline. Z Gerontol Geriatr. 2015;48:15–21. doi: 10.1007/s00391-014-0845-0. [DOI] [PubMed] [Google Scholar]
- 9.Cardoso F, Hodges J, Evans AH, Revesz T, Williams DR. Postural instability, frontotemporal dementia, and ophthalmoplegia: Clinicopathological case. Mov Disord. 2011;26:1808–13. doi: 10.1002/mds.23359. [DOI] [PubMed] [Google Scholar]
- 10.Cieslik B, Jaworska L, Szczepanska-Gierach J. Postural stability in the cognitively impaired elderly: A systematic review of the literature. Dementia (London) 2016 doi: 10.1177/1471301216663012. pii: 1471301216663012 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Coelho FG, Stella F, de Andrade LP, Barbieri FA, Santos-Galduróz RF, Gobbi S, et al. Gait and risk of falls associated with frontal cognitive functions at different stages of Alzheimer's disease. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2012;19:644–56. doi: 10.1080/13825585.2012.661398. [DOI] [PubMed] [Google Scholar]
- 12.Manckoundia P, Pfitzenmeyer P, d’Athis P, Dubost V, Mourey F. Impact of cognitive task on the posture of elderly subjects with Alzheimer's disease compared to healthy elderly subjects. Mov Disord. 2006;21:236–41. doi: 10.1002/mds.20649. [DOI] [PubMed] [Google Scholar]
- 13.Ohsugi H, Ohgi S, Shigemori K, Schneider EB. Differences in dual-task performance and prefrontal cortex activation between younger and older adults. BMC Neurosci. 2013;14:10. doi: 10.1186/1471-2202-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suttanon P, Hill KD, Said CM, Logiudice D, Lautenschlager NT, Dodd KJ. Balance and mobility dysfunction and falls risk in older people with mild to moderate Alzheimer disease. Am J Phys Med Rehabil. 2012;91:12–23. doi: 10.1097/PHM.0b013e31823caeea. [DOI] [PubMed] [Google Scholar]
- 15.Burrell JR, Kiernan MC, Vucic S, Hodges JR. Motor neuron dysfunction in frontotemporal dementia. Brain. 2011;134(Pt 9):2582–94. doi: 10.1093/brain/awr195. [DOI] [PubMed] [Google Scholar]
- 16.Franssen EH, Souren LE, Torossian CL, Reisberg B. Equilibrium and limb coordination in mild cognitive impairment and mild Alzheimer's disease. J Am Geriatr Soc. 1999;47:463–9. doi: 10.1111/j.1532-5415.1999.tb07240.x. [DOI] [PubMed] [Google Scholar]
- 17.Issac TG, Chandra SR, Nagaraju BC. Transcranial magnetic stimulation in patients with early cortical dementia: A pilot study. Ann Indian Acad Neurol. 2013;16:619–22. doi: 10.4103/0972-2327.120493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Talerico KA, Evans LK. Responding to safety issues in frontotemporal dementias. Neurology. 2001;56(11 Suppl 4):S52–5. doi: 10.1212/wnl.56.suppl_4.s52. [DOI] [PubMed] [Google Scholar]
- 19.Cotter VT. The burden of dementia. Am J Manag Care. 2007;13(Suppl 8):S193–7. [PubMed] [Google Scholar]
- 20.Waite LM, Broe GA, Grayson DA, Creasey H. Motor function and disability in the dementias. Int J Geriatr Psychiatry. 2000;15:897–903. doi: 10.1002/1099-1166(200010)15:10<897::aid-gps215>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 21.Weller I, Schatzker J. Hip fractures and Alzheimer's disease in elderly institutionalized Canadians. Ann Epidemiol. 2004;14:319–24. doi: 10.1016/j.annepidem.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Imamura T, Hirono N, Hashimoto M, Kazui H, Tanimukai S, Hanihara T, et al. Fall-related injuries in dementia with Lewy bodies (DLB) and Alzheimer's disease. Eur J Neurol. 2000;7:77–9. doi: 10.1046/j.1468-1331.2000.00021.x. [DOI] [PubMed] [Google Scholar]
- 23.Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134(Pt 9):2456–77. doi: 10.1093/brain/awr179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer's disease: Recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:263–9. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lajoie Y, Gallagher SP. Predicting falls within the elderly community: Comparison of postural sway, reaction time, the berg balance scale and the activities-specific balance confidence (ABC) scale for comparing fallers and non-fallers. Arch Gerontol Geriatr. 2004;38:11–26. doi: 10.1016/s0167-4943(03)00082-7. [DOI] [PubMed] [Google Scholar]
- 26.Vaillant J, Martigné P, Vuillerme N, Caillat-Miousse JL, Parisot J, Juvin R, et al. Prediction of falls with performance on timed “up-and-go” and one-leg-balance tests and additional cognitive tasks. Ann Readapt Med Phys. 2006;49:1–7. doi: 10.1016/j.annrmp.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 27.Allali G, Kressig RW, Assal F, Herrmann FR, Dubost V, Beauchet O. Changes in gait while backward counting in demented older adults with frontal lobe dysfunction. Gait Posture. 2007;26:572–6. doi: 10.1016/j.gaitpost.2006.12.011. [DOI] [PubMed] [Google Scholar]


