Abstract
Soft tissue ganglions are commonly encountered cystic lesions around the wrist presumed to arise from myxomatous degeneration of periarticular connective tissue. Lesions with similar pathology in subchondral location close to joints, and often simulating a geode, is the less common entity called intraosseous ganglion. Rarer still is a lesion produced by mucoid degeneration and cyst formation of the periostium of long bones, rightly called the periosteal ganglion. They are mostly found in the lower extremities at the region of pes anserinus, typically limited to the periosteum and outer cortex without any intramedullary component. We report the case of a 62 year-old male who presented with a tender swelling on the mid shaft of the left tibia, which radiologically suggested a juxtacortical lesion extending to the soft tissue or a soft tissue neoplasm eroding the bony cortex of tibia. It was later diagnosed definitively as a periosteal ganglion in an atypical location, on further radiologic work-up and histopathological correlation.
Keywords: Computed tomography, magnetic resonance imaging, myxomatous degeneration, periosteal ganglion, periosteal reaction
Introduction
Ganglions are cysts derived from the myxomatous degeneration of connective tissue[1] which arise usually from the tendon sheaths of the wrist or foot. Rarely, ganglions arise from the periosteum of long tubular bones, causing periosteal reaction and cortical erosion with extension into the overlying soft tissue,[2] thus mimicking more sinister pathology. However, accurate radiological and histopathological assessment clinches the diagnosis of this rare condition, with few cases reported in the literature so far. We report a clinical case of this lesser known ganglion in disguise, located atypically in the mid-tibial shaft, without ligamentous or joint connection, along with its radiological differentials.
Case History
A 62 year-old male presented with a 1-month history of swelling over the anteromedial aspect of his left leg associated with a dull aching pain. There was no history of trauma or fever and previous medical history was unremarkable. On palpation, the swelling was fluctuant, tender, and cystic in consistency, without fixity to the overlying skin. However, it was not mobile and appeared to be fixed to the underlying surface.
Plain radiograph revealed an irregular diaphyseal cortical lucency on the anteromedial aspect of the left tibia, with tapering superior margins [Figure 1A]. Lateral radiograph demonstrated thick smooth periosteal reaction associated with an overlying lobulated soft tissue mass [Figure 1B]. There was superficial erosion and scalloping of the underlying cortex without endosteal breach by the lesion. Based on these findings, possibility of a soft tissue tumor involving the bony cortex or a bone-surface lesion involving the periosteum was considered.
Figure 1 (A and B).
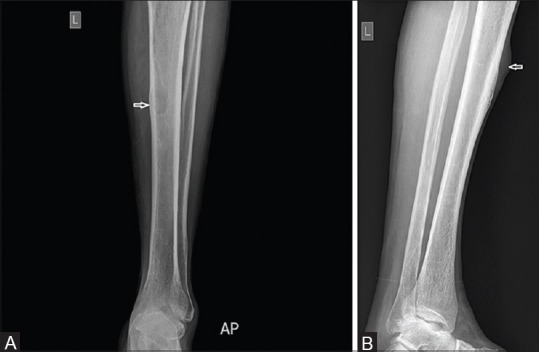
Plain radiograph (AP, lateral) of left tibia. An irregular cortical lucency is observed (arrow) over the medial aspect (A) with an overlying soft tissue mass on the anterior aspect of tibia (arrow) causing thick smooth periosteal reaction and cortical erosion (B)
Sonography of the swelling revealed a well-defined, lobulated, juxtacortical, anechoic lesion of approximate size 4 × 1.3 cm, made up of clear fluid-filled lobules with an internal septation and an irregular underlying bone surface [Figure 2]. Lesion showed no internal or peripheral vascularity on color Doppler examination. On computed tomography (CT), a sharply defined isodense mass relative to muscle, arising from the periosteum was observed, causing erosion and “scooping-out” of the external cortex [Figure 3A and B]. Endosteal surface remained intact.
Figure 2.

Ultrasound examination of the swelling on the left mid tibia. A well lobulated, anechoic lesion of approximate size 4 × 1.3 cm is noted in the juxtacortical location, possessing an internal septation (arrow) and causing irregularity of the bony surface beneath it
Figure 3 (A and B).
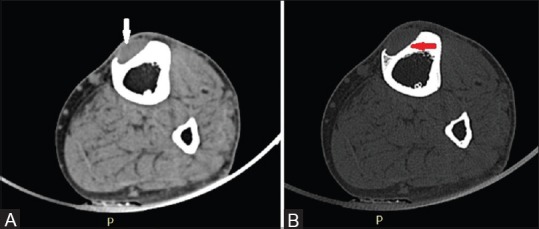
Axial CT view of the left tibia. An isodense soft tissue mass (arrow), arising from the anterior tibial periostium is perceived on soft tissue window (A). Underlying scalloping (arrow) of external cortex without endosteal breach is demonstrated on bone window (B)
In order to localize the lesion and identify its relation to the adjacent structures, a magnetic resonance imaging (MRI) scan was obtained. MRI revealed an isolated lobulated cyst-like mass which was isointense to muscle on T1-weighted imaging [Figure 4A] and homogenously hyperintense on T2-weighted images [Figure 4B], possessing an internal hypointense septation and scalloping the underlying bony cortex. All these radiological findings are classical findings of a subperiosteal ganglion, thus clinching the diagnosis.
Figure 4 (A and B).
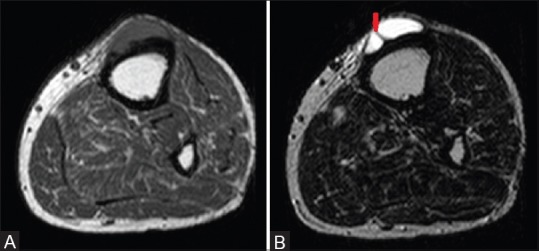
Magnetic resonance imaging of the left tibia. T1-weighted axial image (A) of the left mid tibia reveals eroded cortex with adjacent soft tissue mass, which is isointense to the muscle and converts to high-intensity signal on axial T2 (B), with a hypointense septation within (arrow)
On surgical excision, a lobulated, well-corticated cystic mass was found attached to the mid portion of the left tibia, arising from beneath the periosteum [Figure 5]. The floor of the cyst was slightly roughened cortical bone, which was curetted. There was no tract or connection to the knee joint nor endosteal breach of cortex.
Figure 5.
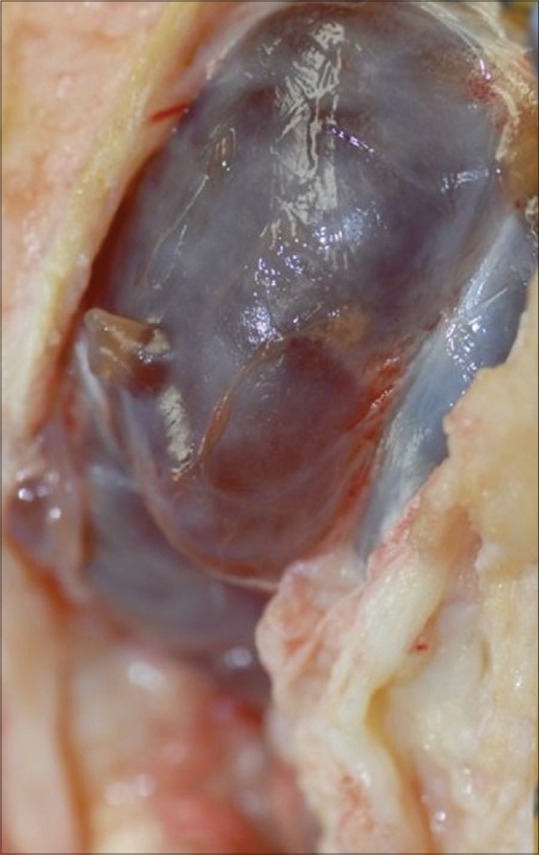
Peroperative appearance of lesion. Finding of a lobulated cystic lesion arising from the periostium of left tibia conformed to the diagnosis of a periosteal ganglion made on imaging studies
Histologically, tissue overlying the lesion was in continuity with the adjacent normal periosteum of tibia and had focal areas of myxomatous degeneration within. It possessed an inner lining of pseudosynovial cells and fibrous tissue covering outside [Figure 6], consistent with the diagnosis of a benign ganglion cyst arising from periosteum. When the patient was seen again after 4 months, there was no evidence of recurrence.
Figure 6.
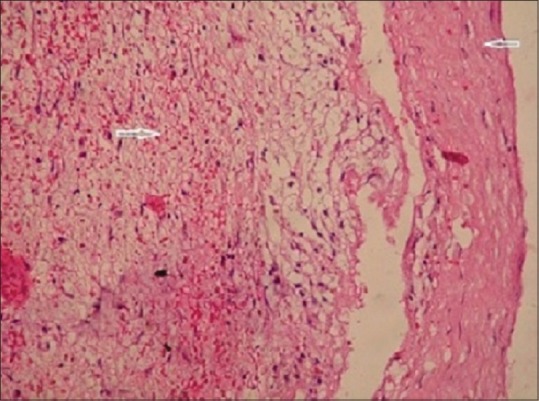
Specimen histopathology. Histological sample after excision of the swelling in the shaft of left mid-tibia on hematoxylin-eosin staining shows the presence of myxomatous material (arrow) within a lining of pseudosynovial cells and surrounding fibrous connective tissue capsule (arrow) on ×40 magnification
Discussion
Ganglions are cystic structures with gelatinous contents and surrounded by a dense fibrous tissue capsule. They are mostly visualized as cystic soft tissue swellings in the dorsum of hand or foot, where they are postulated to arise from the periarticular tendon, muscle, or semilunar cartilage.[3] Their next common location is within the bones, adjacent to the joint space. These intraosseous ganglions are seen as benign subchondral radiolucent lesions with sclerotic margins in a patient without degenerative arthritis. Common sites of their occurrence are medial malleolus, femoral head, and proximal tibia.[4] Very rarely they may arise from the ganglionic degeneration of the periostium of long bones, producing reactive periosteal new bone formation and underlying cortical scalloping, without any intraosseous component or discrete soft-tissue ganglion.[1] This entity called as periosteal ganglion or subperiosteal ganglion, was first described by Olliers (1864) and Poncet (1874) as a peculiar form of periostitis; “periostitis albuminosa” or “ganglion periostale.”[3] This peculiar cyst affects mainly the long tubular bones of lower extremity, majority being found in the region of pes anserinus, with connection to the adjacent knee joint. Other rare sites include distal ends of ulna, radius, femur, medial malleolus, and ilium.[3,5]
Etiology of periosteal ganglion is unknown; repetitive stress and trauma are the speculated causes. Pathogenesis relates to the mucoid degeneration of connective tissues of periosteum.[1] Fibroblasts within the periosteum produce intercellular mucin, which coalesces to form one or several cysts, and their proliferation and collagen formation results in an outer fibrous wall. The cells on the inner aspect of the wall become somewhat cuboidal giving it a pseudosynovial appearance.[6]
Periosteal ganglions have a male preponderance and are usually seen in adults in their fourth and fifth decades, although few cases have been reported in children as well.[5] They present with swelling and mild tenderness and occasional derangement of knees, if the joint is involved. Ganglions may be associated with major vessels in 10–20% cases, and may occasionally bleed into the ganglion spontaneously, in which case it becomes hot, red, and painful.[7] When adjacent nerves are compressed, MRI may reveal abnormalities in the corresponding muscle groups, including atrophy, fat infiltration, and increased signal intensity on T2-weighted imaging.[8]
Radiographically, most lesions are perceived as soft tissue masses associated with periosteal reaction and cortical bone destruction in the form of external scalloping. Often erosions are irregular and multifocal and periosteal new bone formation may be linear or spiculated, radiating from the scalloped area.[1]
Sonography is a helpful modality in assessing any juxtacortical soft tissue mass and demonstration of cystic nature of the lesion virtually excludes other diagnoses.[9] In addition to characterizing the nature and location of the lesion, ultrasound-guided aspiration may also be attempted. Periosteal ganglions are identified as anechoic collections with occasional septations.[8] Long standing lesions may demonstrate more complex cystic appearances, especially if complicated by hemorrhage or infection.
CT usually demonstrates a well-defined soft tissue mass which is hypo or isodense to muscle, adjacent to the bone cortex which shows partial saucerization and irregular erosion.[3] Endosteal surface of cortex is characteristically intact. Typically, contrast enhancement is absent, although slight enhancement of the wall of the ganglion cyst may be apparent.[8]
MRI shows multilobulated cyst-like mass which is hypo to isointense to muscle on T1-weighted imaging and occasionally hyperintense with high protein contents or hemorrhage. T2-weighted and short TI inversion recovery (STIR) imaging characteristically shows hyperintense signal. Rim enhancement maybe seen following gadolinium administration.[8] In the preoperative setting, the delayed arthrographic technique may also be used to rule out any suspected communication between the ganglion cyst and the adjacent joint.[8]
Though a rare entity, it is essential to differentiate periosteal ganglion from other common pretibial masses for proper choice of management. These include nodular pretibial myxedema, subcutaneous sarcoidosis, subperiosteal abscess or hematoma, parosteal lipoma, periosteal aneurysmal bone cyst, or chondroma.[5]
Periosteal chondroma is usually associated with matrix calcification unlike periosteal ganglion and shows heterogeneous peripheral enhancement on gadolinium administration.[10] Subperiosteal hematoma often has a non-aggressive appearance and is centred in the subperiosteum. If they ossify, they can contain fatty marrow.[11] Parosteal lipoma appears as lobulated and well-marginated high signal intensity mass with thin low signal striations on T1 and T2 sequences. On fat-suppressed T2-weighted images, low signal intensity conversion of the lesion represents fat content, with intervening high signal thin striations.[12] Subperiosteal aneurysmal bone cyst appears as single, eccentric, trabeculated lesion which reaches the periosteum and has well-defined margins with onion-skin periosteal reaction. CT and MRI show heterogeneous fluid-fluid levels in loculation.[13] Hydatid cyst of bone appears as round or ovoid cystic lesion often with double arcuate calcification on CT, with parent cyst having signal intensity similar to muscle and secondary cyst to that of water in T1 sequences.[14]
Definitive diagnosis can be made by histopathology, which reveals a cyst in continuation with the periosteum, containing myxoid material, surrounded by fibrous tissue, and having an inner layer composed of flattened cells resembling synovium, termed pseudosynovial cells.[8]
Periosteal ganglions are benign cysts with good prognosis. Treatment options include excision with surrounding portion of bony cortex and aspiration, with or without injection of corticosteroids. When a communication between the ganglion cyst and the adjacent joint is present there may be a recurrence after excision, if this communication is left in place.[8] Further, the mucoid degenerative process may commence postoperatively in the connective tissues occupying the surgical defect, leading to recurrence.[6]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.McCarthy EF, Matz S, Steiner GC, Dorfman HD. Periosteal ganglion: A cause of cortical bone erosion. Skeletal Radiol. 1983;10:243–6. doi: 10.1007/BF00357897. [DOI] [PubMed] [Google Scholar]
- 2.Kobayashi H, Kotoura Y, Hosono M, Tsuboyama T, Sakahara H, Koinishi J. Periosteal ganglion of the tibia. Skeletal Radiol. 1996;25:381–3. doi: 10.1007/s002560050099. [DOI] [PubMed] [Google Scholar]
- 3.Valls R, Melloni P, Darnell A, Munoz J, Canalies J. Diagnostic imaging of tibial periosteal ganglion. Eur Radiol. 1997;7:70–2. doi: 10.1007/s003300050112. [DOI] [PubMed] [Google Scholar]
- 4.Schajowicz F, Clavel Sainz M, Slullitel JA. Juxta-articular bone cysts (intra-osseous ganglia): A clinicopathological study of eighty eight cases. J Bone Joint Surg. 1979;61-B:107–16. doi: 10.1302/0301-620X.61B1.422629. [DOI] [PubMed] [Google Scholar]
- 5.Ferguson NN, Asarch A, Tschetter AJ, Stone M. Periosteal ganglia presenting as subcutaneous nodules on the tibia. JAMA Dermatol. 2014;150:663–4. doi: 10.1001/jamadermatol.2013.6352. [DOI] [PubMed] [Google Scholar]
- 6.Paul D. Byers, Thomas G. Wadsworth. Periosteal Ganglion. J Bone Joint Surg. 1970;52-B:290-5. [PubMed] [Google Scholar]
- 7.Barry M1, Heyse-Moore GH. Acute Haemorrhage Into A Subperiosteal Ganglion. J Bone Joint Surg. 1990;72-B:519. doi: 10.1302/0301-620X.72B3.2341461. [DOI] [PubMed] [Google Scholar]
- 8.De Maeseneer M, De Boeck H, Shahabpour M, Hoorens A, Oosterlinck D, Van Tiggelen R. Subperiosteal ganglion cyst of the tibia: A communication with the knee demonstrated by delayed arthrography. J Bone Joint Surg. 1999;81-B:643–6. doi: 10.1302/0301-620x.81b4.9445. [DOI] [PubMed] [Google Scholar]
- 9.Choi YS, Kim BS, Kim DH, Chun TJ, Yang SO, Choi KH. Sonographic evaluation of a tibial periosteal ganglion with an intra-osseous component. J Ultrasound Med. 2006;25:1369–73. doi: 10.7863/jum.2006.25.10.1369. [DOI] [PubMed] [Google Scholar]
- 10.Zheng K, Yu X, Xu S, Xu M. Periosteal chondroma of the femur: A case report and review of the literature. Oncol Lett. 2015;9:1637–40. doi: 10.3892/ol.2015.2889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mhuircheartaigh JN, Lin YC, Wu JS. Bone tumour mimickers: A pictorial essay. Indian J Radiol Imaging. 2014;24:225–36. doi: 10.4103/0971-3026.137026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaudhary RJ, Dube V, Bhansali C, Gupta A, Balwantkar S. Parosteal lipoma of humerus—A rare case. Int J Surg Case Rep. 2013;4:1159–62. doi: 10.1016/j.ijscr.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meohas W, de Sá Lopes AC, da Silveira Möller JV, Barbosa LD, Oliveira MB. Parosteal aneurysmal bone cyst. Rev Bras Ortop. 2015;50:601–6. doi: 10.1016/j.rboe.2015.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song XH, Ding LW, Wen H. Bone hydatid disease. Postgrad Med J. 2007;83:536–42. doi: 10.1136/pgmj.2007.057166. [DOI] [PMC free article] [PubMed] [Google Scholar]


