Abstract
Osteomas of paranasal sinuses are common benign tumors and are diagnosed incidentally. However, osteomas complicated by pneumocephalus with air fluid level presenting with progressive hemiparesis is rare. Here, we present a case report of a 22-year-old male who presented with left-sided progressive hemiparesis with history of generalized headache since 2 years.
Keywords: MRI, osteoma, paranasal sinus, pneumocephalus
Introduction
Osteoma of the paranasal sinuses is a common benign tumor, usually found incidentally. They are most frequently diagnosed in middle age (2nd to 5th decade) with a male predilection. Osteomas of the paranasal sinuses mainly involve the frontal and ethmoid sinuses.[1] Osteomas are usually asymptomatic or may remain silent and grow slowly without causing neurological deficit.
Pneumocephalus is an uncommon complication of long standing osteomas; however, hemiparesis secondary to such pneumocephalus is a very rare complication.[2] This rarity justifies the follow up of paranasal sinus osteomas for possible intracranial complications.
Case History
A 22-year-old male presented with generalized headache since 2 years. He was taking symptomatic treatment for the same, but did not undergo any investigation. He started developing progressive left-sided hemiparesis since one month. There was no history of craniofacial trauma or surgery. Neurological examination revealed decreased power in left upper and lower limbs with signs of upper motor neuron involvement.
Plain radiograph skull posteroanterior and lateral view [Figure 1A and B] revealed well-defined, homogeneous lobulated radio-opaque lesion within the right frontal sinus. Moreover, air fluid level was seen in right frontal region in parasagittal location.
Figure 1 (A and B).

Plain radiograph skull anteroposterior (A) and lateral view (B) revealed well-defined, rounded, homogeneous radiopaque lesion within right frontal sinus with air fluid level overlying frontal bone on the right side
Non-enhanced computed tomography [Figure 2A and B] of the head revealed well-defined lobulated, homogeneous bone density mass lesion (approximate 2.4 × 2.6 × 3.2 cm in size), with no discernible medullary cavity within the right frontal sinus. The lesion was arising from the posterosuperior wall of the right frontal sinus [Figure 3A and B]. There were erosions noted in the wall of the frontal sinus with intracranial extradural extension of the lesion in the right frontal region. A large extra-axial pocket of air with fluid level was noted in the right frontal region adjacent to the lesion. There was subcortical white matter hypodensity suggestive of edema in the right frontal and high parietal lobe.
Figure 2 (A and B).
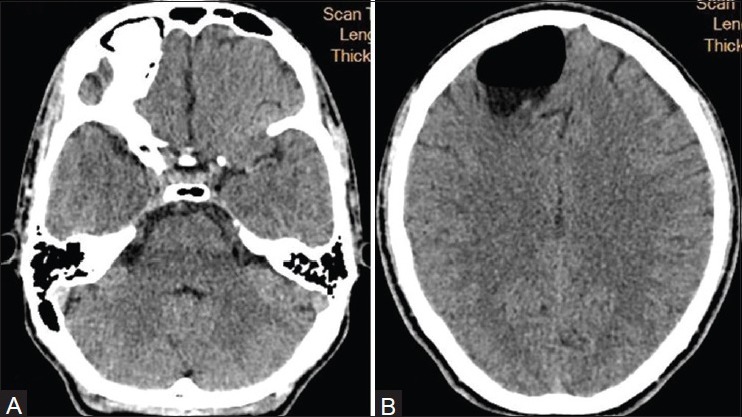
Non-enhanced computed tomography of the head (ICT 256 SLICE PHILIPS BRILLIANCE) soft tissue window revealed homogeneous bony mass within right frontal sinus (A) with associated extra axial pneumocephalus with air fluid level (B)
Figure 3 (A and B).
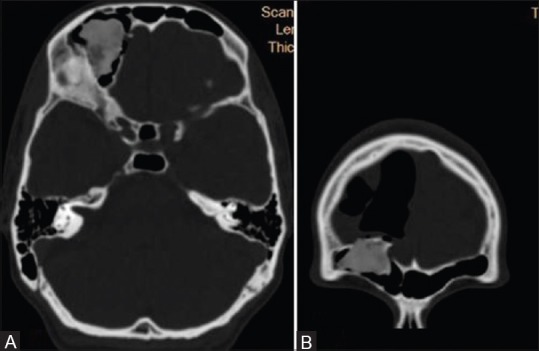
Non-enhanced computed tomography of the head (ICT 256 SLICE PHILIPS BRILLIANCE) (Bone window) axial (A) and coronal (B) images revealed homogeneous bony mass within right frontal sinus with intracranial extradural extension and associated pneumocephalus
Magnetic resonance imaging (MRI) brain was done for further evaluation [Figures 4 and 5], which revealed lesion arising from the posterior wall of the right frontal sinus which appeared hypointense on T1 weighted and isointense on T2 weighted imaging. There was blooming on fast field echo sequences [Figure 4B]. The lesion did not show any post-contrast enhancement. There was large extra-axial pocket of air with fluid level within. There was buckling of the right frontal cortex with subcortical white matter edema in the right frontal and high parietal lobe. The extra-axial air containing cavity did not show peripheral enhancement; the fluid within the cavity did not show restricted diffusion on diffusion weighted images, thus ruling out abscess as the differential diagnosis. Rest of the brain parenchyma appeared normal without any abnormal signal intensity.
Figure 4 (A and B).
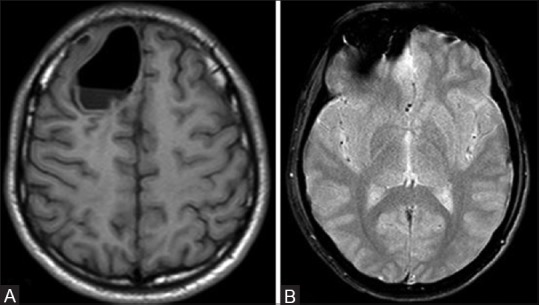
Magnetic resonance imaging of the brain (PHILIPS 1.5T) axial images reveals extra axial pneumocephalus with air fluid level appears hypointense on T1 weighted images (A), and osseous mass showing blooming on fast field echo (B)
Figure 5 (A and B).
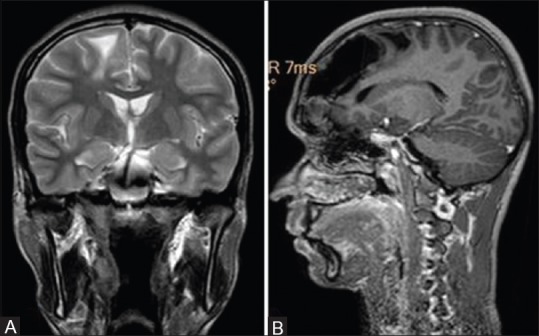
Magnetic resonance imaging of the brain T2 weighted coronal (A) demonstrating subcortical white matter edema in the right frontal lobe and sagittal T1 weighted post-contrast image (B) reveals isointense osseous lesion in right frontal sinus with associated pneumocephalus with air fluid level without any peripheral enhancement and mass effect on right frontal and high parietal lobe with surrounding edema
Considering bony lesion within frontal sinus with associated extra-axial air containing cavity and ruling out abscess by MRI brain, diagnosis of frontal sinus osteoma eroding the posterior wall with associated pneumocephalus with air fluid level was kept. The patient underwent surgical excision of the lesion and postoperative period was uneventful.
Discussion
Osteomas are relatively common, benign, and slow-growing tumors occurring mainly in the paranasal sinuses, more commonly involving the frontal sinus.[3] Osteomas are usually asymptomatic, however, sometimes cause complications such as headache, cerebrospinal fluid (CSF) fistula, meningitis, ptosis, diplopia, and pneumocephalus. Pneumocephalus is a rarely reported complication of frontal sinus osteomas,[3] and to best of our knowledge, have been mentioned in the literature in a few case reports. Pneumocephalus is commonly encountered after neurosurgical procedures but can also be the result of trauma or infrequent causes. In the context of nontraumatic pneumoencephalus, it is important to know the other possible secondary causes such as neoplastic, iatrogenic, and infectious.[4]
This patient presented with rare case of progressive hemiparesis secondary to intracranial pneumocephalus due to erosion by the frontal sinus osteoma. Usually, two hypotheses are related to development of nontraumatic pneumocephalus. These are the “ball valve” and “inverted bottle” mechanisms. In the ball valve mechanism, it is postulated that air enters through a fracture or foramens of the skull base bone adjacent to an air-containing space. The only requirement, then, is a force to push the air into the intracranial space. Once this has occurred, the air remains trapped and a seal is created by the arachnoid membrane, cerebral cortex, or ventricle. The second theory, the inverted bottle mechanism, hypothesizes that as CSF flows out of the skull, negative pressure is created within the intracranial space. This negative pressure does not allow the efflux of more CSF until air enters to take its place and equilibrates the pressure differential. The first theory is probably the cause of development of pneumocephalus in our patient.[5]
The patient underwent surgery and the postoperative period was uneventful with remission of his symptoms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cheng KJ, Wang SQ, Lin L. Giant osteomas of the ethmoid and frontal sinuses: Clinical characteristics and review of the literature. Oncol Lett. 2013;5:1724–30. doi: 10.3892/ol.2013.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kendre B, Deopujari C, Karmarkar V, Shah S. Frontal sinus osteoma with pneumocephalus and progressive hemiparesis. Neurol India. 2013;61:694–5. doi: 10.4103/0028-3886.125395. [DOI] [PubMed] [Google Scholar]
- 3.Kamide T, Nakada M, Hayashi Y, Hayashi Y, Uchiyama N, Hamada J. Intraparenchymal pneumocephalus caused by ethmoid sinus osteoma. J Clin Neurosci. 2009;16:1487–9. doi: 10.1016/j.jocn.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Choi YY, Hyun DK, Park HC, Park CO. Pneumocephalus in the absence of craniofacial skull base fracture. J Trauma Acute Care Surg. 2009;66:E24–7. doi: 10.1097/01.ta.0000229049.11274.96. [DOI] [PubMed] [Google Scholar]
- 5.Johnson D, Tan L. Intraparenchymal tension pneumatocele complicating frontal sinus osteoma: Case report. Neurosurgery. 2002;50:878–80. doi: 10.1097/00006123-200204000-00038. [DOI] [PubMed] [Google Scholar]


