Abstract
Fetal intraabdominal umbilical vein varix (FIUV) is focal dilatation of the intrabdominalumbilical vein of thefetus. It appears as a round or fusiform cystic structure in thefetal abdomen, which shows continuity with the umbilical vein ongrayscale andcolor Dopplerimaging. The diagnostic criteria include the FIUV varix diameter at least 50% wider than the diameter of the intrahepatic umbilical veinand an intraabdominal umbilical vein diameter exceeding 9 mm orgreater than twostandard deviations above the mean for gestational age. We report three cases, two cases with isolated FIUV and favorable outcome and the third case with FIUV and atrioventricular septal defect, where trisomy 21 (Down syndrome) was diagnosed.
Keywords: Antenatal ultrasound, fetal anomalies, trisomy 21, umbilical vein varix
Introduction
Fetalintraabdominal umbilical vein varix (FIUV) is an uncommon but easily detectable ultrasonographic finding.[1,2] Counselling for outcome is a challenge becauseoutcomes are variable. Though the outcome may be satisfactory, cases with fetal structural anomalies, chromosomal anomalies, orfetal hydrops with adverse pregnancy outcomes have been reported.
We report our experience with three cases of FIUV varix and review the available literature.
Case Report
Three cases of umbilical vein varix were identified at our referral centre from 2012 to 2015. The first patient was a 32-year-old, fifth gravida, with 32-week pregnancy who presented with intrauterine growth restriction; she reported three previous intrauterine deaths in late third trimester (cause unknown). FIUV was identified with a diameter of 14.2 mm (normal diameter of umbilical vein: 7–8 mm). ColorDoppler analysis showed turbulent flow in the varicose segment. There were no other structural abnormalities in the fetus. The umbilical artery Doppler was normal. Weekly serial sonographic and Doppler monitoring of pregnancy was performed. Patient delivered a healthy female at 37 weeks by elective caesarean section. The child is now 2 years old and is developmentally normal [Table 1; Figure 1].
Table 1.
Ultrasonographicfindings and neonatal outcome in fetuses with FIUV
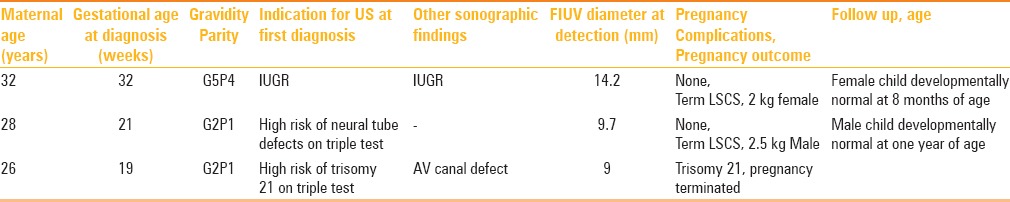
Figure 1.
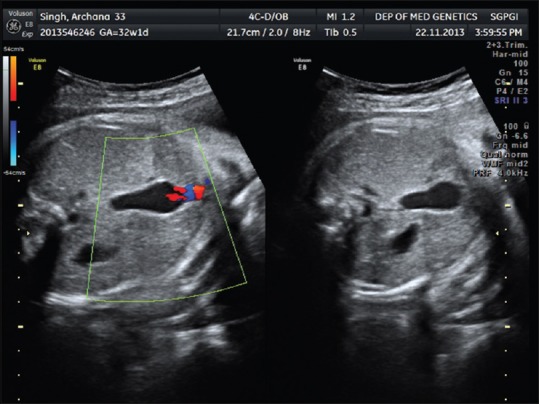
FIUV measuring 14.2 mm and showing normal color flow on Doppler
The second patient was a 28-year-old, 21-week pregnant, second gravida who referred with triple test showing high risk for neural tube defects (>1:50 on triple test, AFP of more than 2.5 MoM). On ultrasonography, isolated FIUV varix measuring 9.7 mm was identified with no other abnormalities. Patient did not opt for invasive testing. Follow-up ultrasound at 31 weeks showed varix size of 9.8 mm with normal Doppler study. She delivered a healthy male after elective caesarean section at term. The child is now 8 months of age and is developmentally normal.
The third patient was a 26-year-old, 19-week pregnant, second gravida who referred with high risk of trisomy 21 on triple test (1:214). On ultrasonography, fetus was found to have a FIUV of diameter 9 mm. The FIUV showed turbulent flow on colour Doppler. An atrioventricular canal defect was also detected in the fetus. Amniocentesis was done and trisomy 21 was detected on fetal karyotyping. The pregnancy was terminated.
Discussion
Of the three cases with FIUV, two cases with isolated FIUV had a normal outcome. In the third patient with atrioventricularcanal defect and FIUV, fetal karyotyping showed trisomy 21 (Down syndrome). Umbilical vein varix corresponds to approximately 4% of the malformations of the umbilical cord. FIUV represents focal dilatation of the extrahepatic intraabdominal part of the fetal umbilical vein. It appears as a round or fusiform cystic structure in the fetal abdomen between the inferior part of the liver and the anterior abdominal wall. Among the intraabdominalumbilical vein varices, extrahepatic intraabdominal varices are more common than intrahepatic intraabdominal varices, probably due to lack of liversupport in the extrahepatic region. The diameter of the umbilical vein increases linearly from 3 mm at 15 weeks to 8 mm at term. The diameter of most umbilical veinvarices is between 6 and 12 standard deviations (SD) above the mean umbilical vein diameter for the patient's gestational age.[2,3] Extremely large varices of up to 85 mm have been reported.[4]
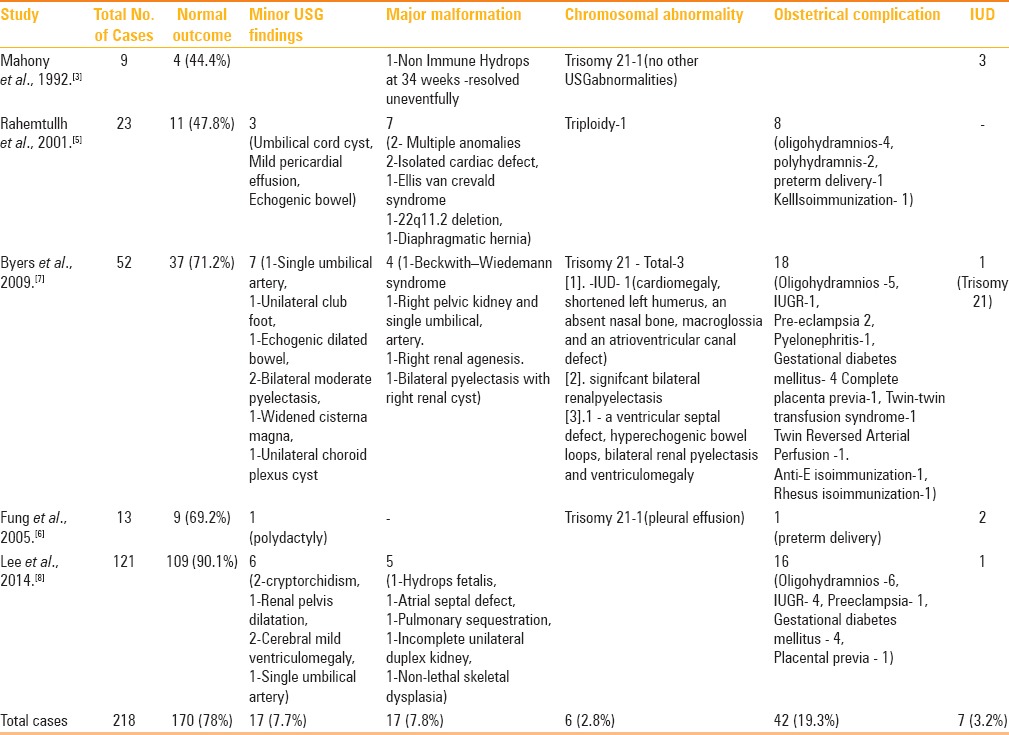
Till date more than 200 cases have been reported in the literature [Table 2].[5,6,7,8] The results of four large case series on FIUV by Rahemtullh et al., Byers et al., Fung et al., and Lee et al. are compiled in Table 2. Out of 218 FIUV cases, 170 had normal outcome (78%). Eighteen fetuses (8.3%) had major malformations. Five cases with FIUV had trisomy 21 and one had triploidy. Except one case, all fetuses with trisomy 21 had ultrasonographically detected major abnormalities, as was the situation in our case. Intrauterine deaths were reported in 7 cases, one of these was trisomy 21. Approximately18% of the pregnancies had obstetrical complications. Twin-to-twin transfusion and twin-reversed arterial perfusion (TRAP) and three cases of isoimmunizationneed special mention because FIUV may be the effect of hemodynamic manifestation of these causes.
Table 2.
Larger case series of FIUV fetuses and their outcome
The complications of FIUV are rupture, thrombosis, compression of the umbilical artery and other veins, and cardiac failure due to vascular stealing by the varix and increased preload. Hence, close serial ultrasonography and Doppler monitoring is required.[9]
Conclusion
Detection of FIUV calls for careful screening of malformations by ultrasound. Monitoring for growth and wellbeing is required. The incidence of chromosomal abnormalities is approximately 2.8% in fetuses with FIUV.[3,5,6,7,8] In absence of malformations, usually the prognosis is favorable. Fetal karyotyping needs to be offered if there are other abnormalities observed on ultrasound. Isolated FIUV does not warrant fetal karyotyping.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nyberg DA, McGahan JP, Pretorius DH, Pilu G, editors. Varix of the umbilical vein. Diagnostic imaging of fetal anomalies. Philadelphia: Lippincott Williams and Wilkins; 2003. pp. 114–5. [Google Scholar]
- 2.Weissman A, Jakobi P, Bronshtein M, Goldstein I. Sonographic measurements of the umbilical cord and vessels during normal pregnancies. J Ultrasound Med. 1994;13:11–4. doi: 10.7863/jum.1994.13.1.11. [DOI] [PubMed] [Google Scholar]
- 3.Mahony BS, McGahan JP, Nyberg DA, Reisner DP. Varix of the fetal intra-abdominal umbilical vein: Comparison with normal. J Ultrasound Med. 1992;11:73–6. doi: 10.7863/jum.1992.11.2.73. [DOI] [PubMed] [Google Scholar]
- 4.Fuster JS, Benasco C, Saad I. Giant dilatation of the umbilical vein. J Clin Ultrasound. 1985;13:363–5. doi: 10.1002/jcu.1870130516. [DOI] [PubMed] [Google Scholar]
- 5.Rahemtullah A, Lieberman E, Benson C, Norton ME. Outcome of pregnancy after prenatal diagnosis of umbilical vein varix. J Ultrasound Med. 2001;20:135–9. doi: 10.7863/jum.2001.20.2.135. [DOI] [PubMed] [Google Scholar]
- 6.Fung TY, Leung TN, Leung TY, Lau TK. Fetal intra-abdominal vein varix: What is the clinical significance? Ultrasound Obstet Gynecol. 2005;25:149–54. doi: 10.1002/uog.1815. [DOI] [PubMed] [Google Scholar]
- 7.Byers BD, Goharkhay N, Mateus J, Ward KK, Munn MB, Wen TS. Pregnancy outcome after ultrasound diagnosis of fetalintra-abdominal umbilical vein varix. Ultrasound Obstet Gynecol. 2009;33:282–6. doi: 10.1002/uog.6233. [DOI] [PubMed] [Google Scholar]
- 8.Lee SW, Kim MY, Kim JE, Chung JH, Lee HJ, Yoon JY. Clinical characteristics and outcomes of antenatal fetal intra-abdominal umbilical vein varix detection. Obstet Gynecol Sci. 2014;57:181–6. doi: 10.5468/ogs.2014.57.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zalel Y, Lehavi O, Heifetz S, Aizenstein O, Dolitzki M, Lipitz S, et al. Varix of the fetal intra-abdominal umbilical vein: Prenatal sonographic diagnosis and suggested in utero management. Ultrasound Obstet Gynecol. 2000;16:476–8. doi: 10.1046/j.1469-0705.2000.00283.x. [DOI] [PubMed] [Google Scholar]


