Abstract
Heart failure has mortality rates that parallel those of breast cancer. Current management strategies include neurohormonal blockade, rate control measures, natriuretic peptide preservation, implantation of mechanical assist devices, and heart transplantation. Despite these strategies, however, the failing myocardium remains energy depleted. New strategies to promote metabolic recovery are being developed to potentially augment current treatment guidelines. For example, an unexpected finding of our own studies showed that mechanical unloading with assist devices in advanced-stage heart failure restored metabolic flux. Unfortunately, at that point it is too late for myocardial recovery.
Traditional metabolic therapies addressing hyperglycemia have had limited long-term outcome benefit. Now, new therapeutic options are emerging based on increased understanding of the molecular mechanisms underlying energy depletion. Metabolic cardiac imaging combined with laboratory diagnostics could guide the design of individual therapeutic strategies. To date, agents that show benefit in select individuals include mimetics that stimulate glucagon-like peptide-1, inhibitors of sodium-glucose cotransporter receptors, drugs that limit fatty acid oxidation, and hormonal therapy in select individuals. This review will summarize mechanisms and investigations related to these metabolic approaches to heart failure.
Keywords: metabolic management, heart failure, energy recovery
Introduction
Heart failure (HF) mortality rates parallel those of breast and other common forms of cancer. The unadjusted 5-year fatality rate for HF is 59% compared to 58% for cancer-related deaths.1 Current therapeutic strategies, including neurohormonal and mineralo-corticoid blockade as well as mechanical interventions, have improved HF survival.2 Recent advances have expanded on this, such as the introduction of natriuretic peptide mimetics and vasopeptidase inhibitors, sinoatrial node inhibitors, and medications for hyperkalemia control. Also, a recombinant form of the hormone relaxin has shown efficacy via vasodilator mechanisms. Despite these developments, metabolic treatments to date have had limited success, and the failing myocardium remains energy deprived. In terms of prevention, intensive glucose control measures have had no demonstrable favorable impact on HF occurrence.3 Myocardial energy depletion has been demonstrated by a variety of techniques, most notably 31P-magnetic resonance spectroscopy (MRS).4 Oxidative metabolic flux transfers energy from carbon bonds to high-energy phosphate ATP and phosphocreatine (PCr). As heart failure progresses, the PCr/ATP energy ratio declines.
Our local HF investigations of paired left ventricular (LV) wall samples unexpectedly demonstrated reversal of the stalled metabolic flux related to energy transfer. The sample pairs from the same hearts were procured at the time of left ventricular assist device (LVAD) placement and again during transplantation.5 These samples of course were from advanced, end-stage heart failure. Metabolic reversal notwithstanding, hemodynamic recovery would be unlikely. However, this provides a rational for earlier interventions to maintain substrate oxidation and high-energy phosphate production with the goal of preventing or even recovering the myocardium. This update offers an overview of the rationale for and identification of emerging therapeutics for HF treatment. The emphasis in this review is on the emerging role of metabolic management with medical decision making based on the stage of heart failure and the presence of comorbidities such as obesity, insulin resistance, and diabetes. These variables impact myocardial substrate selection and utilization and their response to specific therapeutic options. For example, early stage heart failure is characterized by fatty acid oxidation. A shift to enhanced glucose utilization occurs as the stress of heart failure progresses or becomes more severe.6 However, in individuals with obesity, insulin resistance, and/or type 2 diabetes, this shift is hindered. Relative fatty acid utilization then increases.7
Current Therapeutic Practices
There are more than 12 therapeutic classes of drugs for glucose control, and several drugs within each class are approved for use in individuals with diabetes and normal ventricular function. These include both oral and injectable agents. Three of the classes include injectables: insulin, incretin mimetics, and amylin analogues. Oral agents include sulfonylureas, biguanides (metformin), thiazolidinediones (TZD), alpha-glucosidase inhibitors, meglitinides, dipeptidyl peptidase-4 inhibitors (DPP-4), and more recently, the glycosuric sodium-glucose cotransporter 2 (SGLT-2) inhibitors. Bile acid sequestrates and dopamine agonists are less commonly used, especially in this population. The cardiovascular disease benefit of these agents, either alone or in combination, remains incomplete.8 Several of these drugs have warnings and restrictions with regard to their use in HF patients, the TZDs in particular. Recently there have been seemingly conflicting study results related to the DPP-4 agents,9 with initial studies to the contrary yielding to more nuanced analyses that indicate cardiovascular safety.10
Metabolic Impact of Mechanical Unloading
Continuous-flow LVAD placement has saved and prolonged the lives of those with advanced HF and is progressively replacing heart transplantation as long-term therapy. It has been documented to have hemodynamic and cellular effects on the failing heart.11 An additional and unanticipated consequence of unloading, which we were able to document in collaboration with the Houston Methodist Hospital HF and cardiothoracic surgery teams, was the LVAD's metabolic impact. We initially reported the presence of a subpopulation of mitochondria capable of coupled oxidative phosphorylation, contrary to convention at the time.12 We then completed paired pre- and post-LVAD LV wall sample metabolomic, transcriptomic, and protein analyses. The results demonstrated reversal of metabolic alterations and gene expression changes in HF that was unexpected and promising.5 This and earlier studies such as that by Thohan et al.11 would indicate possible recovery. Of course, early implantation of the LVAD for recovery alone would not be taken lightly; however, these findings open the door to early medical metabolic interventions for recovery of the failing ventricle.
Identifying the Metabolic Phenotype
As metabolic therapeutic agents become available, there will be an increased need for diagnostic interventions to identify the phenotype of the individual with heart risk or established disease. In addition to identifying traditional demographics, body type, and comorbidities, these diagnostics should be able to assess specific metabolic characteristics—for example, identifying the presence or absence of whole body and organ-specific cardiac insulin resistance—and answer questions such as: Is the myocardium predominately oxidizing fat or is it primarily utilizing glucose? Are amino acids and ketone bodies used as fuels? These features would form the basis for personalized metabolic treatment, and the identification of these parameters with reassessment longitudinally could guide current and upcoming therapeutics. Clinical methods to do this are already partially available, including laboratory and imaging diagnostics. Going forward, the development of cardiac metabolic imaging either with single-photon emission computed tomography (SPECT) or positron emission tomography (PET)/CT could individualize therapeutics to enhance outcomes.13 A comparative PET study using fluorodeoxyglucose (FDG) to assess glucose uptake and a palmitate isotope for fatty acid oxidation could guide the decision to enhance glucose and limit fatty acid utilization for cardiac energy production.14 As our understanding of metabolic management therapeutics advances, this concept could be expanded by incorporating positron-emitting isotopes into ketone bodies and/or amino acids.
Emerging and Future Therapeutics
The current classes of medication that show promise for HF include agents that impact various metabolic and energy transfer pathways, such as those that stimulate glucagon-like peptide-1 (GLP-1) or inhibit SGLT-2 receptors (Table 1). Both are FDA approved and have widespread clinical use treating individuals with type 2 diabetes. GLP-1 mimetics have potential benefits that go beyond glucose control alone.15,16 The positive impact of GLP-1 on myocardial glucose metabolism has recently been reviewed17 and shown to increase myocardial glucose uptake in a nondiabetic dog model with dilated cardiomyopathy.18 GLP-1 mimetics improve myocardial glucose utilization and show positive cardiovascular effects, including improved ejection fraction, endothelial function, and perfusion, although these effects could be indirect. These injectable drugs often promote weight reduction with reduced blood pressure and blood glucose. The GLP-1 agonists would potentially be beneficial to the myocardium that is locked into oxidizing fatty acids, as in obesity and diabetes, although the heart failure is continuing to progress.19
Table 1.
Overview of therapeutic agents for metabolic management of the failing heart.
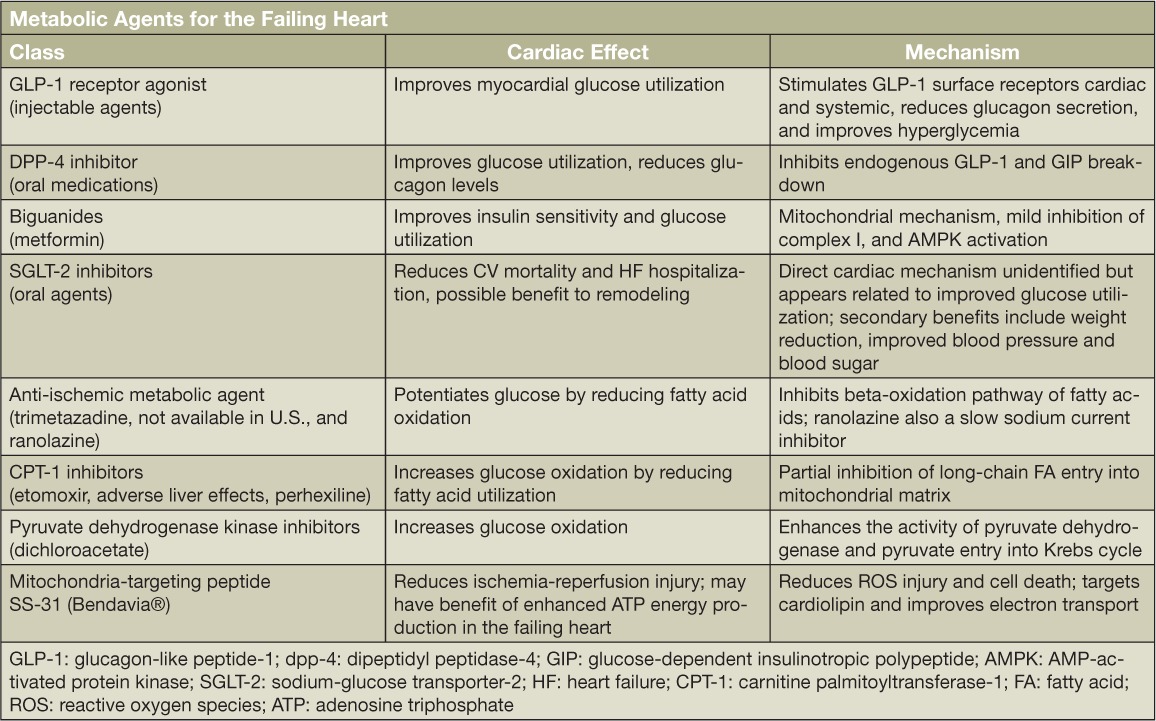
Whether by direct, indirect, or combined effects, these agents appear to have positive cardiac metabolic effects. The recently published LEADER trial reports improvement in cardiovascular outcomes including mortality, nonfatal stroke, and myocardial infarction in individuals with type 2 diabetes taking liraglutide. It was not a heart failure trial.20 If one were to use cardiac metabolic imaging to demonstrate a relative decline in cardiac 18F-FDG uptake by PET/CT relative to fatty acid such as 11C-palmitate, then targeted measures to enhance glucose utilization through use of metformin and GLP-1 mimetics might prove to be beneficial. At this stage of investigation, however, the reports on GLP-1 action on myocardial substrate metabolism are incomplete and need further evaluation.
The SGLT-2 class has had favorable cardiovascular outcomes in individuals with type 2 diabetes. These drugs result in glycosuria by inhibiting glucose reabsorption through SGLT-2 transporters in the proximal renal tubule. The result is urinary loss of glucose and reduction of blood glucose concentrations. SGLT receptors are also expressed in the heart, with SGLT-1 as the dominate isoform. However, SGLT-2 receptors have also been identified. Activation rather than inhibition of the SGLT-1 isoform has been reported to have a role in optimizing cardiac energy metabolism, at least during acute ischemia-reperfusion injury.21 This would raise concern if SGLT-1 were coinhibited by SGLT-2 agents, but the SGLT-2 inhibitors are isoform specific. Specific agents as reviewed by Kurosaki et al. have varying selectivity for the SGLT-2 and -1 receptors.22 The recently published Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG OUTCOME) reported a 14% reduction in adverse cardiac events, including a 38% relative risk reduction in cardiovascular mortality in subjects taking the inhibitor. They also reported a 35% reduction in hospitalization for HF,23 although the mechanisms have yet to be identified.24 A phase-IV randomized, double-blind, placebo-controlled trial was begun in March 2015 and designed to assess the effects of SGLT-2 inhibition on LV remodeling.25 There are reports of a shift to glucose oxidation in heart and kidney metabolism associated with these agents that might account for the benefits.26 Additionally, noncardiac treatment effects including improved glycemic control, reduced blood pressure, and weight reduction might be factors. Use with metformin appears to have an additive effect.
The failing myocardium utilizes noncarbohydrate substrates such as fatty acids and ketone bodies. An approach to reduce long-chain fatty acid oxidation in combination with the agents noted above could potentially replenish depleted energy stores. Trimetazidine, while not available in the United States, has been one the most studied fatty acid oxidation inhibitors.27 Agents that inhibit carnitine palmitoyltransferase-1 (CPT-1) would limit entry of long-chain fatty acid moieties into the mitochondria for beta-oxidation. These agents include etomoxir, which in clinical trials increased liver enzymes in patients with HF, and perhexiline, which was developed as an antianginal agent. Perhexiline inhibits the cardiac CPT-1 isoform and reduces fatty-acid oxidation.28 Ranolazine, also available as an antianginal agent, has been shown to have mitochondrial effects.29 Intracellular malonyl-coenzyme-A inhibits and regulates CPT-1; agents that then would inhibit its synthesis are under development. Likewise, inhibiting phosphoinositide-dependent protein kinase, which inhibits pyruvate dehydrogenase activity and pyruvate entry into the Krebs cycle, would enhance glucose oxidation and help reenergize the failing myocardium. Finally, mitochondrial-targeted agents such as SS-31 (Bendavia®) that may stabilize cardiolipin structure and reduce oxidative damage are under investigation and in clinical trials.30,31
Conclusions and Clinical Implications
Heart failure progresses even in the setting of current evidenced-based therapies, with many patients ultimately requiring mechanical support and/or heart transplantation for survival. Therapies that complement current treatments and promote metabolic recovery are desperately needed. As our awareness and understanding of the molecular mechanisms underlying energy depletion increases, so too does the opportunity for metabolic therapy. Noninvasive cardiac imaging modalities such as SPECT and PET/CT offer the opportunity to identify the mechanisms that are unique to a specific etiology or stage of disease. Treatments targeted to specific metabolic phenotypes at different stages of heart failure are emerging. Agents that have so far shown benefit in select patients include mimetics that stimulate glucagon-like peptide-1, inhibitors of sodium-glucose cotransporter receptors, drugs that limit fatty acid oxidation, and hormonal therapy. In addition, new classes of medications that impact various metabolic and energy transfer pathways are being evaluated. The above review offers a rationale for earlier interventions to maintain substrate oxidation and high-energy phosphate production with the goal of reversing the outcomes associated with heart failure.
Key Points
The failing myocardium is energy depleted.
Adaptive and possible maladaptive metabolic changes in substrate selection characterize different etiologies and stages of heart failure.
The emerging technological advances in cardiac metabolic imaging allow identification of patterns of substrate utilization.
With knowledge of the metabolic phenotype, therapeutic interventions could be individualized using established and emerging agents.
Conflict of Interest Discloser
Extramural funding from the American Heart Association and NIH have provided support to the faculty of the Center for Bioenergetic and Metabolomic Research. Dr. Hamilton has received funding for related research from the Houston Methodist Foundation supporters including Patrick Studdert, Stedman-West Foundation, Jerold B. Katz Foundation, Charif Souki, Elaine and Marvy Finger, and George and Angelina Kostas Research Center Funding.
References
- 1. Stewart S, Ekman I, Ekman T, Oden A, Rosengren A.. Population impact of heart failure and the most common forms of cancer: a study of 1 162 309 hospital cases in Sweden (1988 to 2004). Circ Cardiovasc Qual Outcomes. 2010. November; 3( 6): 573– 80. [DOI] [PubMed] [Google Scholar]
- 2. Jhund PS, Macintyre K, Simpson CR, . et al. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: a population study of 5.1 million people. Circulation. 2009. February 3; 119( 4): 515– 23. [DOI] [PubMed] [Google Scholar]
- 3. Castagno D, Baird-Gunning J, Jhund PS, . et al. Intensive glycemic control has no impact on the risk of heart failure in type 2 diabetic patients: evidence from a 37,229 patient meta-analysis. Am Heart J. 2011. November; 162( 5): 938– 48. e2. [DOI] [PubMed] [Google Scholar]
- 4. Neubauer S. High-energy phosphate metabolism in normal, hypertrophied and failing human myocardium. Heart Fail Rev. 1999. October; 4( 3): 269– 80. [Google Scholar]
- 5. Gupte AA, Hamilton DJ, Cordero-Reyes AM, . et al. Mechanical unloading promotes myocardial energy recovery in human heart failure. Circ Cardiovasc Genet. 2014. June; 7( 3): 266– 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bedi KC Jr, Snyder NW, Brandimarto J, . et al. Evidence for Intramyocardial Disruption of Lipid Metabolism and Increased Myocardial Ketone Utilization in Advanced Human Heart Failure. Circulation. 2016. February 23; 133( 8): 706– 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Riggs K, Ali H, Taegtmeyer H, Gutierrez AD.. The Use of SGLT-2 Inhibitors in Type 2 Diabetes and Heart Failure. Metab Syndr Relat Disord. 2015. September; 13( 7): 292– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ferrannini E, DeFronzo RA. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J. 2015. September 7; 36( 34): 2288– 96. [DOI] [PubMed] [Google Scholar]
- 9. Filion KB, Suissa S. DPP-4 Inhibitors and Heart Failure: Some Reassurance, Some Uncertainty. Diabetes Care. 2016. May; 39( 5): 735– 7. [DOI] [PubMed] [Google Scholar]
- 10. Ou HT, Chang KC, Li CY, Wu JS.. Risks of cardiovascular diseases associated with dipeptidyl peptidase-4 inhibitors and other antidiabetic drugs in patients with type 2 diabetes: a nation-wide longitudinal study. Cardiovasc Diabetol. 2016. March 1; 15: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thohan V, Stetson SJ, Nagueh SF, . et al. Cellular and hemodynamics responses of failing myocardium to continuous flow mechanical circulatory support using the DeBakey-Noon left ventricular assist device: a comparative analysis with pulsatile-type devices. J Heart Lung Transplant. 2005. May; 24( 5): 566– 75. [DOI] [PubMed] [Google Scholar]
- 12. Cordero-Reyes AM, Gupte AA, Youker KA, . et al. Freshly isolated mitochondria from failing human hearts exhibit preserved respiratory function. J Mol Cell Cardiol. 2014. March; 68: 98– 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hamirani YS, Kundu BK, Zhong M, . et al. Noninvasive Detection of Early Metabolic Left Ventricular Remodeling in Systemic Hypertension. Cardiology. 2016; 133( 3): 157– 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gupte AA, Hamilton DJ. Molecular Imaging and Precision Medicine. Cardiology. 2016; 133( 3): 178– 80. [DOI] [PubMed] [Google Scholar]
- 15. Grieve DJ, Cassidy RS, Green BD.. Emerging cardiovascular actions of the incretin hormone glucagon-like peptide-1: potential therapeutic benefits beyond glycaemic control? Br J Pharmacol. 2009. August; 157( 8): 1340– 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ban K, Noyan-Ashraf MH, Hoefer J, Bolz SS, Drucker DJ, Husain M.. Cardioprotective and vasodilatory actions of glucagon-like peptide 1 receptor are mediated through both glucagon-like peptide 1 receptor-dependent and -independent pathways. Circulation. 2008; 117( 18): 2340– 50. [DOI] [PubMed] [Google Scholar]
- 17. Hansen J, Brock B, Botker HE, Gjedde A, Rungby J, Gejl M.. Impact of glucagon-like peptide-1 on myocardial glucose metabolism revisited. Rev Endocr Metab Disord. 2014. September; 15( 3): 219– 31. [DOI] [PubMed] [Google Scholar]
- 18. Bhashyam S, Fields AV, Patterson B, . et al. Glucagon-like peptide-1 increases myocardial glucose uptake via p38alpha MAP kinase-mediated, nitric oxide-dependent mechanisms in conscious dogs with dilated cardiomyopathy. Circ Heart Fail. 2010. July; 3( 4): 512– 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Aravindhan K, Bao W, Harpel MR, Willette RN, Lepore JJ, Jucker BM.. Cardioprotection Resulting from Glucagon-Like Peptide-1 Administration Involves Shifting Metabolic Substrate Utilization to Increase Energy Efficiency in the Rat Heart. PLoS One. 2015. June 22; 10( 6): e0130894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Marso SP, Daniels GH, Brown-Frandsen K, . et al.; LEADER Steering Committee; LEADER Trial Investigators Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med. 2016. July 28; 375( 4): 311– 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kashiwagi Y, Nagoshi T, Yoshino T, . et al. Expression of SGLT1 in Human Hearts and Impairment of Cardiac Glucose Uptake by Phlorizin during Ischemia-Reperfusion Injury in Mice. PLoS One. 2015; 10( 6): e0130605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kurosaki E, Ogasawara H. Ipragliflozin and other sodium-glucose cotransporter-2 (SGLT2) inhibitors in the treatment of type 2 diabetes: preclinical and clinical data. Pharmacol Ther. 2013. July; 139( 1): 51– 9. [DOI] [PubMed] [Google Scholar]
- 23. Zinman B, Wanner C, Lachin JM, . et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015. November 26; 373( 22): 2117– 28. [DOI] [PubMed] [Google Scholar]
- 24. Abdul-Ghani M, Del Prato S, Chilton R, DeFronzo RA.. SGLT2 Inhibitors and Cardiovascular Risk: Lessons Learned From the EMPA-REG OUTCOME Study. Diabetes Care. 2016. May; 39( 5): 717– 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Singh JS, Fathi A, Vickneson K, . et al. Research into the effect of SGLT2 inhibition on left ventricular remodelling in patients with heart failure and diabetes mellitus (REFORM) trial rationale and design. Cardiovasc Diabetol. 2016; 15: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mudaliar S, Alloju S, Henry RR.. Can a Shift in Fuel Energetics Explain the Beneficial Cardiorenal Outcomes in the EMPA-REG OUTCOME Study? A Unifying Hypothesis. Diabetes Care. 2016. July; 39( 7): 1115– 22. [DOI] [PubMed] [Google Scholar]
- 27. Lopatin YM, Rosano GM, Fragasso G, . et al. Rationale and benefits of trimetazidine by acting on cardiac metabolism in heart failure. Int J Cardiol. 2016. January 15; 203: 909– 15. [DOI] [PubMed] [Google Scholar]
- 28. Lee L, Campbell R, Scheuermann-Freestone M, . et al. Metabolic modulation with perhexiline in chronic heart failure: a randomized, controlled trial of short-term use of a novel treatment. Circulation. 2005. November 22; 112( 21): 3280– 8. [DOI] [PubMed] [Google Scholar]
- 29. Aldakkak M, Camara AK, Heisner JS, Yang M, Stowe DF.. Ranolazine reduces Ca2+ overload and oxidative stress and improves mitochondrial integrity to protect against ischemia reperfusion injury in isolated hearts. Pharmacol Res. 2011. October; 64( 4): 381– 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Brown DA, Hale SL, Baines CP, . et al. Reduction of early reperfusion injury with the mitochondria-targeting peptide bendavia. J Cardiovasc Pharmacol Ther. 2014. January; 19( 1): 121– 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Birk AV, Chao WM, Bracken C, Warren JD, Szeto HH.. Targeting mitochondrial cardiolipin and the cytochrome c/cardiolipin complex to promote electron transport and optimize mitochondrial ATP synthesis. Br J Pharmacol. 2014. April; 171( 8): 2017– 28. [DOI] [PMC free article] [PubMed] [Google Scholar]


