Abstract
In this paper we demonstrate that the cells which initiate replication of Epstein-Barr virus (EBV) in the tonsils of healthy carriers are plasma cells (CD38hi, CD10−, CD19+, CD20lo, surface immunoglobulin negative, and cytoplasmic immunoglobulin positive). We further conclude that differentiation into plasma cells, and not the signals that induce differentiation, initiates viral replication. This was confirmed by in vitro studies showing that the promoter for BZLF1, the gene that begins viral replication, becomes active only after memory cells differentiate into plasma cells and is also active in plasma cell lines. This differs from the reactivation of BZLF1 in vitro, which occurs acutely and is associated with apoptosis and not with differentiation. We suggest that differentiation and acute stress represent two distinct pathways of EBV reactivation in vivo. The fraction of cells replicating the virus decreases as the cells progress through the lytic cycle such that only a tiny fraction actually release infectious virus. This may reflect abortive replication or elimination of cells by the cellular immune response. Consistent with the later conclusion, the cells did not down regulate major histocompatibility complex class I molecules, suggesting that this is not an immune evasion tactic used by EBV and that the cells remain vulnerable to cytotoxic-T-lymphocyte attack.
Epstein-Barr virus (EBV) is a human herpesvirus that infects over 90% of the world's adult population. Although EBV infection is usually benign, it is associated with several neoplasias (reviewed in references 39 and 43) and is the causative agent of acute infectious mononucleosis (AIM) (17). As with other herpesviruses, primary infection by EBV is followed by lifelong persistence. EBV persists in resting, recirculating memory B lymphocytes (4, 20, 33). We have previously presented evidence (5) in support of a model (44-46) whereby EBV gains access to memory B cells by using different transcription programs to first activate latently infected cells and then allow them to differentiate into resting memory B cells.
One major unresolved issue with EBV in vivo is the nature of the cells responsible for replicating the virus and the signals necessary to drive a latently infected cell into viral replication. Lytic replication of EBV occurs regularly in healthy carriers, since virus particles are found in their saliva (14). It is assumed that the latently infected memory B cells circulating in the body return periodically to Waldeyer's ring (tonsils and adenoids) (24), where they undergo periodic reactivation to produce infectious virus to be shed into saliva. The signal that initiates viral replication in vivo is unknown; however, we assume that it is not provided by the virus, since viral proteins are not expressed in the latently infected memory cells (18). The process of activating normal memory cells in lymph nodes usually causes them to differentiate into antibody-producing plasma cells (25). These cells are essentially biochemical factories, so they would be ideal for the efficient production of virions. Also, they are located in the tonsil epithelium (8, 26), which would allow them to shed virus into the saliva.
The first suggestion that EBV replication may be associated with terminal differentiation came from an early study that detected expression of a poorly characterized, plasma cell-associated surface marker (PC1) on cells replicating the virus in tissue culture cell lines (11). It has also been reported (2, 35) that very rare cells, in tonsils from AIM patients, express proteins from the viral lytic cycle. The cells were detected by immunohistochemistry and resembled plasma cells morphologically. These results need to be interpreted with care, however, since immunohistochemical studies are prone to artifacts, especially when detecting rare positive cells for which no independent verification of infection status or cell phenotype is established. These concerns are highlighted because those authors also observed rare infected cells bearing T-cell markers. Since infection of T cells is not normally associated with EBV, this raises concerns that the rare cells replicating EBV in AIM tonsils are artifacts or aberrations of the very high levels of infection found in AIM. It was also unresolved whether plasma cell differentiation is the signal for reactivation or whether reactivation results in plasma cell differentiation.
EBV reactivation has been extensively studied in vitro with latently infected cell lines. Lytic replication begins through expression of the immediate-early transcription factor BZLF1 (15). BZLF1 then initiates a cascade of gene expression beginning with the early genes, some of which are involved in viral DNA replication, and late genes, which are expressed after viral DNA synthesis and include components of the virion. Various signals have been shown to trigger rapid induction of the promoter for BZLF1 (41) and to induce viral replication in culture (13, 50). Although these in vitro systems employ potential differentiation signals (12, 28) to initiate viral replication, terminal differentiation of cells replicating the virus into plasma cells is not observed. Thus, the in vitro studies stand in contrast to the histochemical studies, and it is unclear what, if any, relationship exists between plasma cell differentiation and induction of viral replication.
In this paper we address the question of which cell type initiates viral replication in the tonsils of healthy carriers by separating subsets of tonsil cells and identifying which ones express the BZLF1 gene. We identify the plasma cell as the cell type in which EBV undergoes reactivation in vivo in human tonsils and provide evidence that the terminal differentiation of B cells into plasma cells may provide the signal that triggers the switch from latency into the lytic cycle.
MATERIALS AND METHODS
Cell culture and tissue preparation.
BJAB is an EBV-negative B-cell lymphoma cell line that was used as a negative control for all experiments. B95-8 is an EBV-positive marmoset cell line, and Akata is an EBV-positive Burkitt lymphoma cell line. Both were used as positive controls for lytic gene reverse transcription-PCR (RT-PCR). U266, RPMI 8226, MM.1S, and MM.1R are human plasma cell lines derived from multiple myelomas (kind gifts of K. Anderson).
To induce lytic gene expression in Akata cells, they were split to 106 cells per ml 1 day prior to treatment. The following day, the cells were spun down and resuspended in fresh medium to which anti-human immunoglobulin G (IgG) (Sigma) was added at a concentration of 100 μg/ml. The cells were harvested 24 h later.
Tonsils were obtained from Massachusetts General Hospital, and lymphocyte suspensions were prepared as described previously (5).
Lymphocyte fractionation.
IgD− CD20+, IgD− CD20−, and IgD+ CD20+ B cells were separated with magnetic cell separation (MACS; Miltenyi Biotec) columns as described previously (4). Resting memory B cells for in vitro culture with CD40 ligand were also isolated by using MACS. Tonsil buffy coat cells were stained with a phycoerythrin (PE)-coupled anti-CD38 antibody (0.5 U/ml; PharMingen) to separate plasma cells, germinal center cells, and activated memory cells; with a PE-coupled anti-CD3 antibody (0.5 U/ml; PharMingen) to label T cells; and with a PE-coupled anti-IgD antibody (0.06 μg/ml; Southern Biotechnology) to label naive B cells. The positively stained cells were then removed by positive selection with anti-PE microbeads. The negatively selected fraction of cells collected from the column consisted of resting memory B cells. All separations and manipulations were performed at 4°C.
The CD10− CD20+, CD10+ CD20+, CD38hi CD3−, CD38+ CD3−, and CD38− CD3− subsets of tonsil cells were isolated by fluorescence-activated cell sorting (FACS). Tonsil buffy coat cells were stained with both fluorescein isothiocyanate (FITC)-coupled anti-CD20 (1 μg/ml; DAKO) and CyChrome-coupled anti-CD10 (0.5 U/ml; PharMingen) or with PE-coupled anti-CD38 (0.5 U/ml; PharMingen) and FITC-coupled anti-CD3 (1 U/ml; Becton Dickinson). The appropriate B-cell subsets were sorted on a Mo-Flo (Dako Corp.). All operations were performed at 4°C.
FACS analysis.
The purity of all isolated populations was analyzed by flow cytometry with a Becton Dickinson FACScaliber with CellQuest software. B-cell populations always were 90% pure and usually were 95% pure when isolated by MACS (see the appropriate figures for representative FACS analysis). FACS-separated cell populations were 90 to 95% pure for the defining markers, with <5% contamination by any undesired B-cell subset.
In vitro cell differentiation.
Tonsil resting memory B cells were differentiated into plasma cells in vitro by the method described by Arpin et al. (3). A total of 1.5 × 107 to 2 × 107 purified resting tonsil memory B cells were isolated as described above and then cultured for 3 days in 20 ml of Iscove medium supplemented with 5% fetal calf serum in the presence of 20 ng of interleukin-2 (IL-2) (Endogen) per ml, 20 ng of IL-10 (Endogen) per ml, and CD40L-transfected NIH 3T3 cells (a gift from Gordon Freeman) (B-cell/fibroblast ratio, 5:1) which were irradiated with 1,400 rads. Cells were then harvested, washed, and recultured with 2 μg of anti-CD40L-blocking antibody (PharMingen) per ml, 20 ng of IL-2 (Endogen) per ml, 20 ng of IL-10 (Endogen) per ml, and NIH 3T3 cells (B-cell/fibroblast ratio, 5:1) which were irradiated with 1,400 rads. B cells were harvested at various time points for analysis.
RT-PCR.
RNA isolation, cDNA synthesis, and PCR were performed as described previously (7), except that all samples were treated with DNase (Invitrogen) prior to cDNA synthesis, according to the manufacturer's instructions. PCR was performed on the synthesized cDNA for the immediate-early gene BZLF1, the early gene BHRF1, and the late capsid component BcLF1. The reaction was carried out in a final volume of 50 μl of a reaction mixture which consisted of 50 mM KCl, 20 mM Tris (pH 8.4), 2.5 mM MgCl2, 0.2 mM deoxynucleoside triphosphates, and a 20 pM concentration of each of the amplimers. The exceptions were BHRF1, for which 3.0 mM MgCl2 was used, and BcLF1, for which 3.5 mM MgCl2 was used. The amplimers used were as follows: BZLF1, 5′-TTCCACAGCCTGCACCAGTG-3′ and 5′-GGCAGCAGCCACCTCACGGT-3′ (47); BHRF1, 5′-GTCAAGGTTTCGTCTGTGTG-3′ and 5′-TTCTCTTGCTGCTAGCTCCA-3′ (16); and BcLF1, 5′-TATGCCCAATCCCAAGTACACG-3′ and 5′-TGGACGGGTGGAGGAAGTCTTC-3′ (37).
Twenty microliters of the cDNA preparation was used for each PCR. Given that the cDNA synthesis reaction was in 100 μl, it was possible to perform RT-PCR for all of the genes described above from one cDNA preparation. Reaction mixtures were incubated at 95°C for 5 min, and 1 U of Taq DNA polymerase (Perkin-Elmer) was added to each tube. The tubes were loaded in a Geneamp 9600 thermocycler, and the following conditions were used for PCR: 40 cycles of 95°C for 15 s, x°C for 30 s, and 72°C for 30 s, where x was 59°C for BZLF1 and 63°C for BHRF1 and BcLF1. All PCRs were concluded with a 5-min incubation at 72°C to complete the extension of all synthesized products. PCR products were visualized by Southern blotting as described previously (34). Blots were probed with PCR products derived from the B95-8 cell line.
Limiting-dilution DNA PCR.
To determine the absolute number of infected cells in a population, a limiting-dilution DNA PCR analysis was performed as described previously (22). Isolated populations were serially diluted, and replicates (six to eight of each cell dilution) were aliquoted at the desired number into a 96-well V-bottom microtiter plate (Immulon) for PCR. Serial dilutions were never performed on cell extracts or isolated DNA. The DNA PCR can detect the presence of a single viral genome in as many as 106 uninfected cells. Poisson statistics were used to calculate the frequency of EBV-infected cells. To determine the absolute number of cells expressing a viral gene, a limiting-dilution analysis was also performed, except the replicates were aliquoted at the desired number into Eppendorf tubes and resuspended in 1 ml of Trizol (Gibco) for RT-PCR. The RT-PCR can detect transcripts from one lytic cell equivalent (see Fig. 3).
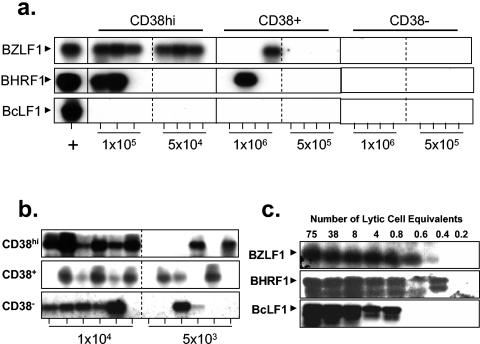
FIG. 3.
EBV replicates in the CD38hi subsets of tonsil B cells. CD38hi, CD38+, and CD38− B cells were separated by FACS from a single tonsil, subjected to limiting-dilution analyses, and analyzed for the presence of viral RNA and DNA. (a) The cell populations were tested by RT-PCR for expression of an immediate-early (BZLF1), an early (BHRF1), and a late (BcLF1) replicative gene. Due to the relatively low yields of pure CD38hi plasma cells, 10-fold higher numbers of cells could be tested for the CD38+ and CD38− subsets. (b) The cell populations were also tested for the presence of the virus by DNA PCR. PCR products were identified by Southern blotting with a gene-specific probe. Tonsil 1 from Table 1 was used in this experiment. (c) Sensitivity of the RT-PCR assays for EBV replicative genes. Akata cells were induced into the lytic cycle by cross-linking of the surface immunoglobulin. cDNA was then prepared, and serial dilutions were tested by RT-PCR analysis for detection of the immediate-early (BZLF1), early (BHRF1), and late (BcLF1) replicative genes. The fraction of cells replicating the virus in the cultures was estimated by immunofluorescence staining for the BZLF1 protein.
Immunofluorescence.
To stain B cells for cytoplasmic and membrane Ig, cells (5 × 106) isolated by FACS were fixed in 1 ml of 1% paraformaldehyde in phosphate-buffered saline (PBS) at room temperature for 3 min and permeabilized in 0.01% Triton X-100 at room temperature for 10 min. The cells were resuspended in PBSA, followed by treatment with 1 μl of FITC-coupled anti-Ig for 30 min at 4°C. They were then washed twice in PBSA (1× PBS plus 0.5% BSA) and resuspended in 300 nm DAPI (4′,6′-diamidino-2-phenylindole) (Molecular Probes) for 30 min at 4°C to stain the nuclei. Following two further washes in PBSA, the cells were mounted onto microscope slides, mounting buffer was added, and coverslips were applied.
Plasmids.
The BZLF1 promoter (Zp) sequence was excised from plasmid p294:Zp-BZLF1 (a kind gift of P. J. Farrell) and cloned into the multiple cloning site of pBS II SK (Promega) between the XhoI and BamHI sites. Zp was then cut with XhoI and SacI and cloned upstream of the luciferase reporter gene in the pGL2 plasmid (Promega) to create pGL2:Zp-luc. The pEBB-GFP plasmid was a kind gift of Ananda Roy.
Transfection and luciferase assays.
Cells (107) were washed twice and resuspended in 500 μl of Opti-Mem (Sigma). Ten micrograms of both the pGL2:Zp-luc and green fluorescent protein (GFP) plasmids was added to the cells, and the mixture was incubated at room temperature for 10 min. The cells were transferred to a 0.4-mm-gap-width cuvette (Eppendorf) and electroporated with a Bio-Rad Gene Pulser under the following conditions: 300 V and 500 mF for RPMI 8226 cells and 270V and 960 mF for MM.1S cells. The cells were placed on ice for 10 min and then added to flasks containing 5 ml of RPMI and 5 ml of cell line-conditioned medium. Transfection of primary cells was performed with the human B-cell Nucleofector kit (Amaxa Biosystems) according to the manufacturer's instructions.
One-tenth of the transfected cells were analyzed for GFP content as a measure of transfection efficiency after 24 h, using a Becton Dickinson FACScaliber with CellQuest software. Transfection efficiencies ranged from 7 to 30% for the cell lines and were ∼10% for the primary cells. The remaining cells were collected by centrifugation, washed in PBS, and then lysed in 65 μl of reporter lysis buffer (Promega) for 15 min at room temperature. Debris was removed by centrifugation for 2 min at 11,000 rpm in a microcentrifuge (Biofuge A; Baxter Scientific). A 1-μl sample of supernatant was assayed for total protein with the Bio-Rad protein assay according the manufacturer's instructions. A 25-μl sample of supernatant was assayed for 20 s on a Tropix luminometer with 100 μl of luciferase assay buffer (Promega). Luciferase values were normalized both for transfection efficiency by using the percentage of GFP-positive cells and for cell number by using total protein values.
RESULTS
Detection of BZLF1 expression in tonsils.
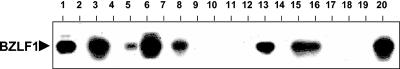
We wished to identify the subset of tonsil B cells in which EBV replication was initiated by screening isolated subsets for expression of BZLF1. BZLF1 is the first gene expressed in the lytic cycle (15, 41) and initiates a cascade of gene expression that ultimately leads to the production of virions. To identify which tonsils would be most fruitful for this analysis, we screened unfractionated lymphocytes, from a panel of frozen samples, by RT-PCR for BZLF1 expression. BZLF1 expression was observed in approximately half of the tonsils tested (Fig. 1). There was a trend towards finding BZLF1 in tonsils with higher levels of infected cells; however, the correlation was weak, suggesting that the number of cells reactivating EBV is not simply dependent on the total number of infected cells. The tonsils in which BZLF1 expression was detected were used in subsequent experiments.
FIG. 1.
Screen of tonsils for replication of EBV. RNA was extracted from the unfractionated tonsil lymphocytes of healthy EBV carriers. RT-PCR was then performed for expression of BZLF1, the first gene expressed in the lytic cycle, which initiates the gene expression cascade leading to production of infectious virus. PCR products were identified by Southern blotting with a BZLF1-specific probe.
EBV preferentially replicates in plasma cells in the tonsil.
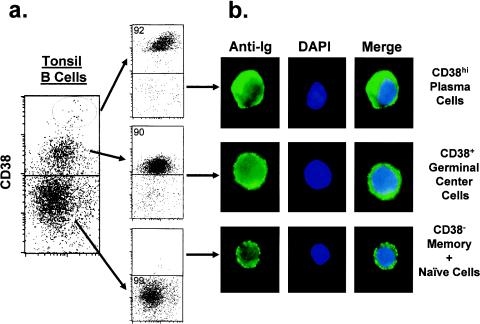
CD38 is used as a marker to identify and fractionate B-cell subsets from the tonsil (25). In particular, CD38hi is the defining phenotype for plasma cells (27, 31). Figure 2a demonstrates FACS analysis of tonsil lymphocytes stained for CD38 expression, after exclusion of T cells. A typical pattern of staining (33) was observed. Three clearly demarcated subsets were seen and separated by FACS. These include the CD38hi (plasma cells), CD38+ (germinal center B cells [25, 27] and possibly activated memory B cells [10]), and CD38− (naive and memory B cells) subsets. These three subsets of cells were then subjected to limiting-dilution RT-PCR for the detection of the BZLF1 immediate-early lytic gene, the early antigen BHRF1, and the late antigen BcLF1 (Fig. 3a). In a parallel analysis, the absolute frequency of virus-infected cells in each population was measured by using a limiting-dilution DNA PCR technique (Fig. 3b) (22). Combining the results of the two assays, we estimated the percentage of infected cells in each population undergoing viral replication based on expression of the three markers. The results of this analysis are shown in Table 1 for two separate tonsils.
FIG. 2.
Flow cytometric fractionation of tonsil B lymphocytes based on expression of CD38. (a) Tonsil lymphocytes were depleted of T cells by using MACS beads and the CD3 monoclonal antibody. The remaining B cells were stained with CD38. Three discrete populations were observed and separated with a Mo-Flo (Dako): CD38hi (plasma cells), CD38+ (germinal center cells), and CD38− (naive and memory cells). (b) The CD38hi B cells are plasma cells. The sorted cells from panel a were stained for immunoglobulin expression (green), and the nucleus was identified by DAPI staining (blue). Only the CD38hi subset consisted of plasma cells, based on high-level expression of cytoplasmic immunoglobulin, lack of membrane immunoglobulin, a large cytoplasm-to-nucleus ratio, and a displaced nucleus.
TABLE 1.
Percentage of EBV-infected cells replicating the virus in different B-cell subsets separated on the basis of CD38 expression
| Cellsa | Subset | % of cells expressing:
|
||
|---|---|---|---|---|
| Immediate-early gene | Early gene | Late gene | ||
| Tonsil 1 | CD38hi | 25 | 12 | <3 |
| CD38+ | 0.1b | 0.1b | <0.1 | |
| CD38− | <0.1 | <0.1 | <0.1 | |
| Tonsil 2 | CD38hi | 10 | 1.7b | 1b |
| CD38+ | 0.2 | 0.1b | 0.2b | |
| CD38− | <0.1 | <0.1 | <0.1 | |
| B95-8 | 0.3 | 0.3 | 0.2 | |
| Processed B95-8 | 0.2 | 0.3 | 0.3 | |
B95-8 is a B-cell line with a constitutive low level of cells replicating the virus. The cells were tested directly after removal from culture. Processed B95-8 cells are B95-8 cells that had been subjected to mock purification with the same methods as applied to the tonsil cells.
Value is approximate since it is based on detecting a single positive signal in the limiting dilution.
Several conclusions can be drawn from this study. First, lytic gene expression, including that of BZLF1, is almost exclusively limited to the CD38hi plasma cell population, indicating that viral replication initiates in plasma cells. Testing of 10-fold-higher numbers of cells produced only a single positive signal in the CD38+ population and none in the CD38− population. Second, 10 to 20% of the plasma cells carrying EBV are undergoing lytic replication. Taken together, these two conclusions strongly suggest that the cells first become plasma cells and then initiate viral replication, consistent with terminal differentiation being the signal to initiate lytic replication. Third, the levels of cells expressing lytic antigens decreases as the assays move from immediate-early (BZLF1) to early (BHRF1) to late (BcLF1), antigens to the point where BcLF1 expression was seen in only two of four tonsil samples tested and in each case only a single signal was seen in the limiting-dilution analysis. This is not an artifact of differential sensitivity of the RT-PCR assays used, since in control experiments (Fig. 3c) all three were able to detect a single cell expressing the transcript. An alternative explanation is that the relative recovery of cells at each stage represents the relative amount of time that the cells spend at each stage of the cycle; i.e., the immediate-early stage is longer than the early stage, which in turn is longer than the late stage. However, this does not appear to be the case, since a control experiment performed with a cell line showed no such bias towards cells expressing the immediate-early products. (B95-8 in Table 1). Another possibility is that the cells become increasingly frail as they proceed through the lytic cycle and are preferentially lost during the isolation procedure. Again this does not appear to be the case, since processing a cell line through a mock version of the same purification procedure (processed B95-8 in Table 1) did not result in preferential retention of cells expressing the immediate-early genes. We conclude, therefore, that the cells that initiate viral replication in the tonsils are CD38hi plasma cells and that most do not complete the cycle.
Phenotyping of BZLF1-positive cells in the tonsil.
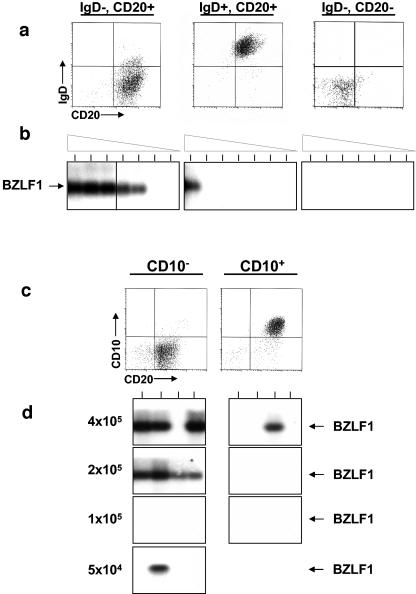
Use of the CD38 marker allowed the cells that initiate viral replication to be identified as plasma cells. To confirm and extend this observation, we performed a more extensive phenotypic analysis. T-cell-depleted tonsil lymphocytes were fractionated on the basis of IgD, CD10, and CD20 expression and then analyzed for the expression of immediate-early lytic genes. The results are presented in Fig. 4. Figure 4a and b show the analysis of the cells after fractionation by using surface IgD expression and the pan-B-cell marker CD20. Three populations were identified and separated by FACS: the IgD+ CD20+ population, which contains predominantly naive B cells; IgD− CD20+ cells, which contain predominantly memory and germinal center B cells; and the IgD− CD20− population, which should contain contaminating non-B cells and plasma cells (Fig. 4a), based on the generally held view that plasma cells do not express the B-cell lineage marker CD20 (25). Figure 4b shows the result of performing RT-PCR analysis for the immediate-early gene BZLF1 on serial twofold dilutions of these three populations. The results clearly demonstrate that the cells expressing BZLF1 reside almost exclusively in the IgD− CD20+ population. Similarly, cells were fractionated based on the expression of CD10, which specifically identifies germinal center cells. As seen in Fig. 4c and d, the cells expressing BZLF1 reside almost exclusively in the CD10− CD20+ population. This analysis is more informative than the IgD study, because CD38+ and CD10+ are known to be coexpressed markers for germinal center cells (see Fig. 5 for an example). The failure to find significant numbers of BZLF1+ cells in the CD10+ fraction provides further support for our conclusion that the signals seen in the CD38+ fraction in Fig. 3a probably arise from cross contamination with CD38hi cells and not from bona fide infected CD38+ cells.
FIG. 4.
EBV replicates in the IgD− CD10− CD20+ subset of tonsil B cells. (a) T-cell-depleted tonsil lymphocytes (CD3−) were fractionated by MACS into IgD+ and IgD− fractions. The IgD− subset was further fractionated by MACS into CD20+ and CD20− fractions. The purified cells were analyzed by flow cytometry for purity (top panels). (The T-cell depletion was less efficient for this experiment than for the one shown in Fig. 2.) The CD20− fraction probably consists of contaminating T cells and macrophages but could also include plasma cells that had lost their lineage markers. (b) Cells (106) of each fraction were subjected to serial twofold dilutions, and the dilutions were tested by RT-PCR for expression of the immediate-early gene BZLF1. PCR products were identified by Southern blotting with a gene-specific probe. Tonsil 1 from Table 1 was used in this experiment. (c) CD10+ CD20+ and CD10− CD20+ tonsil lymphocytes were separated by FACS sorting. (d) The samples were serially diluted, and then multiple replicates were made for each dilution. Each sample was analyzed by RT-PCR (upper panels) for expression of the immediate-early BZLF1 gene. PCR products were identified by Southern blotting with a gene-specific probe. Tonsil 2 from Table 1 was used in this experiment.
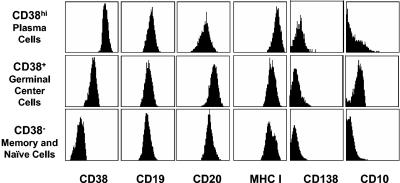
FIG. 5.
Cell surface phenotyping of the three populations separated on the basis of CD38 expression. CD38hi, CD38+, and CD38− B cells were analyzed by flow cytometry for expression of CD38, the pan-B-cell markers CD19 and CD20, CD138 (Syndecan), MHC class I, and the germinal center-specific marker CD10. Isotype-matched antibodies were used for the negative controls. The plasma cells are CD38hi B cells that express reduced levels of CD20 and are CD138 (Syndecan) negative.
Plasma cells in the tonsil express B-cell lineage markers.
The phenotype for cells replicating EBV in the tonsil, described in the previous sections (CD38hi, CD10−, IgD−, and CD20+) eliminates naive B cells (CD38−, CD10−, IgD+, and CD20+), memory cells (CD38−, CD10−, IgD−, and CD20+), and germinal center cells (CD38+, CD10+, IgD−, and CD20+) as the population in which the virus replicates (36). The CD38hi CD10− IgD− phenotype is consistent with plasma cells; however, there is a discrepancy in the phenotype, since the cells are also CD20+. General reviews state that plasma cells from the tonsil do not express the pan-B-cell marker CD20 (25), while earlier published data suggest that they do (31). Therefore, there are two possible explanations for our observations. Either the cells replicating EBV are not typical plasma cells, or tonsil plasma cells do express CD20. To distinguish these possibilities and confirm the identity of the CD38hi population, T-cell-depleted tonsil lymphocytes were stained for CD38 expression and then separated into the three populations shown in Fig. 2. The separated cells fixed on slides were then subjected to immunofluorescence staining with FITC-coupled anti-Ig to demonstrate the distribution of Ig within the cells and with DAPI to stain the nuclei (Fig. 2b). The CD38hi cell population has been characterized extensively before and has been shown to consist of highly purified plasma cells (31). Confirming this, we found that the Ig staining of these cells was diffuse, cytoplasmic, and not on the membrane and that the cells had a large cytoplasm-to-nucleus ratio with the nucleus positioned off to one side of the cell, characteristic of plasma cells; >90% of the CD38hi population had these morphological characteristics of plasma cells. By comparison, CD38+ and CD38− populations had only membrane Ig staining with low cytoplasm-to-nucleus ratios. Further confirmation of the plasma cell nature of the CD38hi cells was obtained by Wright-Giemsa staining, which indicated that the cells had a characteristic plasmacytoid morphology (data not shown). Having confirmed that the CD38hi population was comprised of plasma cells, we proceeded to characterize the surface phenotype. The three populations of non-T cells separated on the basis of CD38 expression were stained for the B-cell lineage markers CD19 and CD20 and for MHC Class I which is widespread in its expression. As shown in Fig. 5, the CD38hi population, which we have shown morphologically and immunologically to be comprised of plasma cells, is positive for both B lineage markers and major histocompatibility complex (MHC) class I. However, expression of CD20 is significantly lower on the plasma cells than on the other B-cell subsets and Syndecan, as expected (30), is not expressed at all. In these respects tonsil plasma cells are different from bone marrow plasma cells, which are CD20 negative but Syndecan (CD138) positive (30, 42). We can conclude, therefore, that the cellular phenotype we have described is fully consistent with plasma cells being the cell type responsible for replicating EBV in the tonsil, with the addendum that they should be referred to as CD20lo.
The BZLF1 promoter is activated in plasma cells.
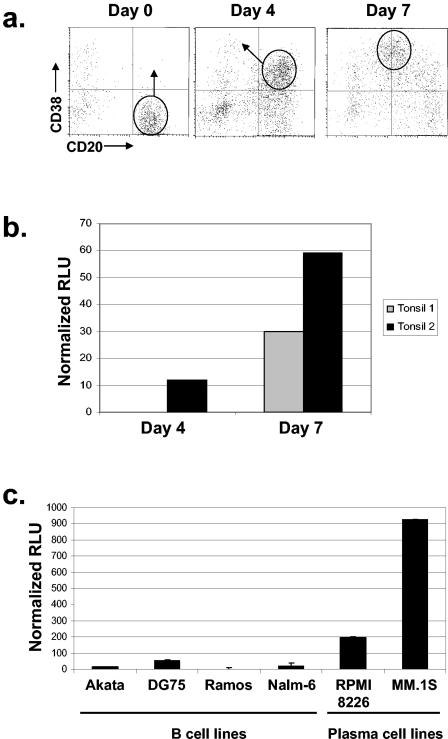
The promoter for the immediate-early gene BZLF1, which initiates viral replication, has been studied extensively (reviewed in reference 40). The experiments described above predict that this promoter should become activated when resting memory B cells differentiate into plasma cells. To test this in vitro, we took advantage of a system that drives the differentiation of resting memory B cells to plasma cells in culture (3). As shown previously, and reproduced in Fig. 6a (left panel), isolated resting memory B cells are CD38− CD20+. After 4 days of culture with CD40 ligand, IL-2, and IL-10 a population of cells that are CD38+ CD20+ emerges (Fig. 6a, middle panel), a phenotype characteristic of memory cells activated in vitro (10). After an additional 3 days of culture, the population shifts to CD38hi CD20lo (Fig. 6a, right panel), the characteristic phenotype of plasma cells (30, 31, 42). Constructs containing the BZLF1 promoter sequences upstream of a luciferase reporter gene were transfected into cells from day 4 and 7 cultures. The results are shown in Fig. 6b. Because the cell cultures produce a heterogeneous mixture of cells, the results have to be interpreted with care; however, two observations are clear. First, the promoter was not functional in the cell preparations containing the activated memory cells after 4 days in culture. Second, the promoter became active only when cells expressing the full plasma cell phenotype appeared after 7 days of culture. This experiment is an important control because it demonstrates directly that the BZLF1 promoter is activated in bona fide plasma cells. This eliminates the possibility that EBV up regulates CD38 expression in a non-plasma cell population, accounting for the results described above. It also provides support for our conclusion that the rare cells found expressing lytic genes in the CD38+ population are contaminating plasma cells, since CD38+ CD20+ cells do not support BZLF1 promoter activity. To confirm the in vitro findings, we also tested plasma cell lines for activity of the BZLF1 promoter. As seen in Fig. 6c, the promoter was active in the two plasma cell lines tested but not in a number of other cell lines, including other human B-cell lines and a murine plasma cell line (data not shown). These results are consistent with our in vivo studies. They support the idea that lytic replication is not initiated by the signals that cause plasma cell differentiation; rather, the cells have to differentiate into plasma cells before the BZLF1 promoter and the lytic cycle can be activated.
FIG. 6.
The BZLF1 promoter Zp functions in plasma cells but not activated memory cells. (a) Resting tonsil memory cells (CD38− CD20+) were isolated by negative selection and induced to differentiate by culturing with IL-2 and IL-10 together with NIH 3T3 fibroblasts expressing CD40 ligand as described previously (3). After 4 days of culture a subset of cells had adopted the phenotype of activated memory cells (CD38+ CD20+) (10), and after 7 days they had adopted that of plasma cells (CD38hi CD20lo). (b) Relative transcriptional activity of a BZLF1 promoter-luciferase reporter construct transfected into resting memory B cells after 4 or 7 days of culture as described for panel a. The results of two separate experiments are shown. (c) As for panel b, but with a collection of human B-cell lines, including two plasma cell lines. Error bars indicate standard deviations. RLU, Relative light units.
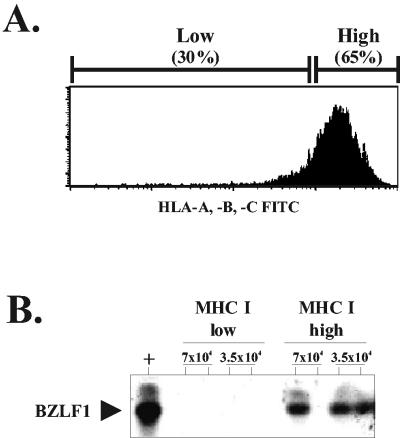
EBV-infected plasma cells do not down regulate MHC class I molecules when they undergo lytic replication.
Several herpesviruses, such as cytomegalovirus and herpes simplex virus (HSV), encode proteins that are expressed early in the lytic phase of infection and interfere with presentation of processed viral peptides for recognition by cytotoxic T cells (CTL) (reviewed in reference 48). It is believed that this is done in order to reduce the effectiveness of the immune response while infectious virus is being produced. A similar mechanism has been suggested for EBV, based on the claim that tissue culture cells down regulate MHC when they replicate the virus (21). To test whether this occurred in vivo, tonsil plasma cells were isolated based on CD38 expression and then fractionated into high and low expressers of MHC. Limiting-dilution RT-PCR was then performed for BZLF1 expression on the two populations (Fig. 7). Tonsil plasma cells expressing BZLF1 were all found in the population expressing average to high levels of MHC class I. None were detected in the fraction expressing low levels. We conclude that down regulation of MHC expression is not an immune evasion strategy used by EBV during viral replication in plasma cells in vivo.
FIG. 7.
MHC class I expression is not down regulated on plasma cells replicating EBV. Plasma cells were purified as described in the legend to Fig. 2. The cells were then stained for expression of MHC class I molecules and separated into low and high expressers as shown. The two populations were then subjected to RT-PCR to detect expression of the viral BZLF1 gene as described in the legend to Fig. 3.
DISCUSSION
In this paper we demonstrate that the cells that initiate EBV replication, i.e., express the immediate-early gene BZLF1, in the tonsils have the phenotype of plasma cells (CD38hi, CD10−, CD19+, CD20lo, IgD−, surface Ig−, and cytoplasmic Ig+). Unfortunately, cells expressing viral late proteins were extremely rare, and we have no way to test whether infectious virus is actually produced by this population. These technical difficulties make it difficult to conclude with certainty that plasma cells actually produce infectious virus, although they clearly initiate replication. The possibility that the replication is abortive cannot be excluded at this time. The main arguments against this conclusion are that we did detect single BcLF1-positive cells in some experiments, we showed that memory cells have to differentiate into plasma cells before the BZLF1 promoter is activated, and plasma cells were the only population where a significant fraction of the infected cells initiate replication based on BZLF1 expression. Therefore, if virus is being produced by any B-cell subset, it must be in the plasma cells.
Viral replication was not detected in naive (IgD+ CD38− CD20+) or germinal center (CD10+ CD38+ CD20+) cells. Rare cells expressing BZLF1 or early or late antigens were found in the CD38+ fraction, but these probably represent contamination by a small number of CD38hi cells. For example, ∼25% of the infected CD38hi cells were BZLF1 positive for tonsil 1 (Fig. 3a and Table 1), whereas only ∼0.1% of the infected CD38+ cells were BZLF1 positive. Since there are similar frequencies of virus-infected cells in both populations (Fig. 3b), it would take only a ∼0.5% contamination of CD38hi cells in the CD38+ population to account for this result. Most likely, therefore, the BZLF1 signals in the CD38+ population are caused by small numbers of contaminating CD38hi cells. Even if there was no contamination and the CD38+ signals were real, the ratio of CD38hi to CD38+ to CD38− B cells in the tonsil is 1:10:30 (Fig. 2) (31). Therefore, in absolute terms, 25 out of every 26 (∼95%) BZLF1-expressing cells reside in the CD38hi population for tonsil 1. Similarly, ∼85% can be estimated to reside in the CD38hi population for tonsil 2.
Plasma cells are not thought to be self-renewing, and therefore it is unlikely that they are in themselves a site of persistent infection. This is because the infected cells would be rapidly depleted when they die producing infectious virus. EBV could persist through chronic reinfection and replication in plasma cells; however, this is unlikely because they do not express a known viral receptor and there is no evidence that plasma cells can be directly infected. It is most likely that plasma cells replicating the virus are produced through terminal differentiation of a small number of cells from the pool of latently infected circulating resting memory cells that are generally believed to be the site of long-term persistent infection for EBV (44, 46). It follows that these cells must circulate back to Waldeyer's ring (24), where they occasionally undergo viral replication to release infectious virus into the saliva (4).
There are two possible mechanisms by which EBV in a tonsil memory cell could be induced to replicate: (i) viral replication is initiated in memory cells that subsequently differentiate into plasma cells, or (ii) latently infected memory cells differentiate into plasma cells and then initiate viral replication. We favor the second mechanism. The observation that BZLF1 is predominantly expressed in the plasma cell fraction together with our quantitation showing that only about a quarter of the infected plasma cells express BZLF1 implies that infected memory cells differentiate into plasma cells while remaining latently infected and then initiate viral replication. This conclusion is supported by our in vitro studies demonstrating that the BZLF1 promoter functions in memory cells only after they have been driven in culture to become plasma cells. Since this process takes 7 days, it is apparent that lytic replication is induced by plasma cell differentiation and not by the acute signals that drive the differentiation. We may conclude further that plasma cell differentiation is the signal for initiating viral replication rather than that viral replication allows or drives cellular differentiation.
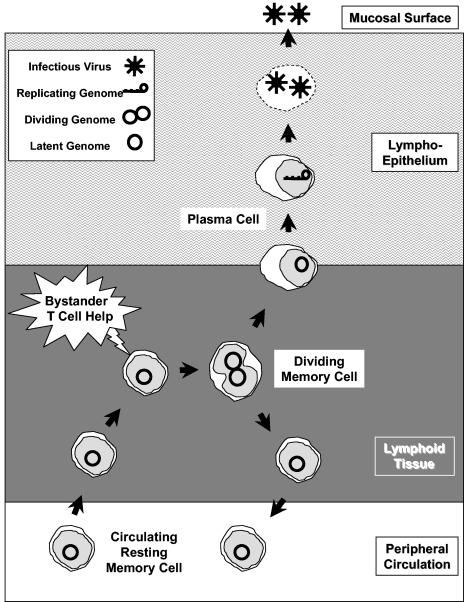
Since the circulating, latently infected memory cells express no viral proteins (18), the signal that causes them to undergo terminal differentiation in vivo is probably host derived. An explanation for how this could work is offered by elegant studies demonstrating that immunological B-cell memory does not require antigen but may be sustained by polyclonal stimuli provided by bystander T-cell help (7). This mechanism provides for continuous renewal of memory cells through sporadic division, which also produces plasma cells and antibody. The result is maintenance of the memory population while stable levels of antibody are produced over time in the absence of antigen. Applied to EBV (Fig. 8), this would explain how the population of latently infected memory cells can be maintained at stable levels for years (22) while, through the continuous generation of plasma cells, virus can also be continuously produced (49).
FIG. 8.
A model of how EBV may persist in the circulating memory B-cell compartment while being continuously shed into saliva, based on the work of Bernasconi et al (7). They have suggested that memory B cells exposed to bystander T-cell help become activated and divide, generating new memory cells and plasma cells. This process maintains the level of memory cells and antibody-secreting plasma cells in an antigen-independent way. If the memory B cell contained latent EBV, the process would produce another latently infected memory cell, maintaining the levels of latently infected cells in the peripheral circulation, while also producing a plasma cell, thus also ensuring the continuous release of infectious virus. Since this process occurs in the tonsils, the plasma cell would migrate into the lymphoepithelium and produce the virus. Whether this virus is released directly into saliva or is first amplified through lytic infection of epithelial cells is a controversial and, as yet, unresolved issue.
An alternate hypothesis is that plasma cell generation is stimulated by cognate antigen and T-cell help. This would mean that EBV becomes reactivated when the latently infected memory cell undergoes an antigen-specific secondary response. This hypothesis has the attractive feature that latency is established in antigen-specific memory cells in the tonsil. These cells would then enter the peripheral circulation, where they would maintain persistent infection. As these cells reenter secondary lymphoid tissue, the site where they would most likely reencounter cognate antigen would be the tonsil. This would provide a mechanism for preferential homing and reactivation of the latently infected memory cells in the tonsil compared to other lymph nodes. This hypothesis is made uncertain by the fact that EBV encodes latent proteins, LMP1 and LMP2, which, respectively, can mimic CD40 and antigen receptor-like signals (9, 23). This makes cells latently infected with EBV potentially independent of T-cell help and/or antigen. The situation is further complicated by the observation from in vitro studies that signaling through LMP1 and/or LMP2 can block reactivation initiated by antigen receptor signaling (1, 32), implying that the virus has encoded latent proteins with the specific intent of blocking antigen-driven activation. This means that a cell destined to replicate the virus cannot be expressing LMP1 and LMP2. This strongly implicates the circulating resting memory cell, the only latently infected cells type in which expression of these proteins is absent. Taken together, this information leads to a model whereby reception of host-derived signals by a resting latently infected memory cell in the tonsil leads to activation and then terminal differentiation of the cell into a plasma cell without turning on expression of the latent genes. Once the cell becomes a full-blown plasma cell, viral replication begins. This model predicts that the BZLF1 promoter should be highly and specifically responsive to a plasma cell-specific transcription factor(s).
In vitro studies with the Akata cell line appear at first glance to support the idea that antigen drives viral replication. Cross-linking of the antigen receptor (BCR) on these cells leads to their synchronous entry into the lytic cycle, and BCR signaling is known to be important in plasma cell differentiation (41). However, a number of properties of this system suggest that it may not be representative of in vivo replication. First and most striking is that activation of the BZLF1 promoter in Akata cells occurs within minutes of the antigen receptor signal, whereas differentiation into plasma cells takes days. The response in Akata cells is too acute to be the same as the in vivo mechanism, and not surprisingly, the Akata cells do not undergo plasma cell differentiation prior to viral replication. The Akata system may be more closely related to the spontaneous reactivation that occurs when latently infected peripheral memory cells are placed into culture (38). This is an acute reactivation, presumably in response to the stress induced upon being placed in culture, and also occurs too rapidly to be associated with terminal differentiation. It is also important to note that all of the signals that induce viral replication in vitro in cell lines, including surface Ig cross-linking of Akata cells, are associated with the induction of apoptosis in the cells (19). However, expression of lytic EBV genes protects these cells from apoptosis (19), suggesting that EBV has acquired specific genes to save a stressed cell from death while the virus replicates. This discussion raises the possibility that there may be two mechanisms for reactivating EBV in vivo. One may be an acute reactivation in resting memory cells in response to stress that allows the virus to escape quickly before the cell dies. The other allows replication of EBV in plasma cells located in the epithelium of the tonsil. This allows for high-level production of virions that may be shed directly into saliva.
For the tonsils that we fractionated and studied in detail, 10 to 20% of the infected plasma cells initiated viral replication. We measured the frequencies of virus-infected cells in the unfractionated tonsil lymphocytes and in the subsets isolated on the basis of CD38 expression. Since we also know the relative abundance of plasma cells based on CD38 staining, we can use this information to estimate that 0.1 to 0.5% of all of the infected cells in the tonsil are replicating the virus. Assuming approximately 1010 B lymphocytes in Waldeyer's ring and a range of infected cells from 1 to 1,000/107 (10), we may calculate that anywhere from 5 to 1,000 cells are replicating EBV in Waldeyer's ring at any one time. However, we found sequentially fewer cells expressing the immediate-early, early, and then late lytic antigens, such that it appears that only ∼10% of the cells (Table 1) complete the replicative cycle. This suggests that fewer than 100 cells are actually releasing virus in Waldeyer's ring at any given time. This may account for the relatively low titers of EBV observed in the saliva of most healthy carriers (49).
The sequential diminution in the numbers of cells replicating the virus as they proceed through the cycle does not appear to be a technical artifact; therefore, some physiological process is impeding the progress of the cells. One possibility, as discussed above, is that replication in the majority of cells is abortive and simply never reaches completion. An alternative explanation for the diminution is that immunosurveillance by CTL kills the cells as they progress through the lytic cycle, leaving fewer and fewer cells as the cycle progresses. This is consistent with our finding that the cells expressing BZLF1, a major target of CTL, do not down regulate class I MHC and are therefore liable to CTL attack. It is possible that MHC down regulation could occur at later times, since we analyzed only immediate-early (i.e., BZLF1) expression; however, this presumably would be too late, since the CTL would already have detected the cells expressing the immediate-early genes. This distinguishes EBV from other herpesviruses, such as HSV, which encode immediate-early proteins that specifically blunt CTL responses by down regulating MHC class I (48). The failure of EBV to do so may reflect different strategies for these viruses. For HSV the strategy of the virus is to sporadically reactivate and produce infectious virus for a brief period of time before viral replication is shut down by the immune response. EBV, on the other hand, is chronically shed into the saliva, so transient delay of the immune response would not be useful. Rather, it appears that EBV is able to continue generating replicative cells, a few of which complete the cycle despite the cellular immune response. This suggests that EBV may have developed a mechanism to constitutively reduce the local effectiveness of the CTL response, perhaps through the production of viral IL-10 during the lytic cycle (6, 29).
In a previous study on viral replication, we used Gardella gels to detect the linear replicating form of viral DNA (4). In that study we failed to detect linear DNA in the IgD− fraction, which would appear to be inconsistent with the present results. However, the present study predicts that only very small numbers of plasma cells reach the late stages of replication, and it would not be possible to load sufficient cells on a Gardella gel to detect this very low level. Conversely, in that study we did detect linear viral DNA in the CD19− fraction. In follow-up studies we were unable to associate this linear DNA with a particular cell type. It is possible that it could be due to epithelial cells with replicating virus or cell debris-associated virion DNA from dead cells.
One confusion that resulted from this study was the observed surface phenotype (CD20lo) of tonsil plasma cells. This arose in part because plasma cells from the bone marrow are CD20− (30, 42) and in part because some reviews state that tonsil plasma cells are also CD20− (25). However, our study and several previous studies show clearly that tonsil plasma cells, unlike the bone marrow, continue to express CD20, albeit at a reduced level (30, 31, 42).
In conclusion, we have shown that differentiation to plasma cells is associated with induction of the EBV lytic cycle in vivo. It now remains to be discovered what the signals are that drive this differentiation.
Acknowledgments
We thank Allen Parmelee for flow cytometry, Cheryl Greene for supplying the tonsils, and Paul Farrell for supplying plasmids.
This work is supported by Public Health Service grants AI 18757 and CA 65883.
REFERENCES
- 1.Adler, B., E. Schaadt, B. Kempkes, U. Zimber-Strobl, B. Baier, and G. W. Bornkamm. 2002. Control of Epstein-Barr virus reactivation by activated CD40 and viral latent membrane protein 1. Proc. Natl. Acad. Sci. USA 99:437-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anagnostopoulos, I., M. Hummel, C. Kreschel, and H. Stein. 1995. Morphology, immunophenotype, and distribution of latently and/or productively Epstein-Barr virus-infected cells in acute infectious mononucleosis: implications for the interindividual infection route of Epstein-Barr virus. Blood 85:744-750. [PubMed] [Google Scholar]
- 3.Arpin, C., J. Banchereau, and Y. J. Liu. 1997. Memory B cells are biased towards terminal differentiation: a strategy that may prevent repertoire freezing. J. Exp. Med. 186:931-940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babcock, G. J., L. L. Decker, M. Volk, and D. A. Thorley-Lawson. 1998. EBV persistence in memory B cells in vivo. Immunity 9:395-404. [DOI] [PubMed] [Google Scholar]
- 5.Babcock, G. J., D. Hochberg, and A. D. Thorley-Lawson. 2000. The expression pattern of Epstein-Barr virus latent genes in vivo is dependent upon the differentiation stage of the infected B cell. Immunity 13:497-506. [DOI] [PubMed] [Google Scholar]
- 6.Bejarano, M. T., and M. G. Masucci. 1998. Interleukin-10 abrogates the inhibition of Epstein-Barr virus-induced B-cell transformation by memory T-cell responses. Blood 92:4256-4262. [PubMed] [Google Scholar]
- 7.Bernasconi, N. L., E. Traggiai, and A. Lanzavecchia. 2002. Maintenance of serological memory by polyclonal activation of human memory B cells. Science 298:2199-2202. [DOI] [PubMed] [Google Scholar]
- 8.Brandtzaeg, P., E. S. Baekkevold, I. N. Farstad, F. L. Jahnsen, F. E. Johansen, E. M. Nilsen, and T. Yamanaka. 1999. Regional specialization in the mucosal immune system: what happens in the microcompartments? Immunol. Today 20:141-151. [DOI] [PubMed] [Google Scholar]
- 9.Caldwell, R. G., J. B. Wilson, S. J. Anderson, and R. Longnecker. 1998. Epstein-Barr virus LMP2A drives B cell development and survival in the absence of normal B cell receptor signals. Immunity 9:405-411. [DOI] [PubMed] [Google Scholar]
- 10.Casamayor, P. M., M. Khan, and I. C. MacLennan. 1995. A subset of CD4+ memory T cells contains preformed CD40 ligand that is rapidly but transiently expressed on their surface after activation through the T cell receptor complex. J. Exp. Med. 181:1293-1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crawford, D. H., and I. Ando. 1986. EB virus induction is associated with B-cell maturation. Immunology 59:405-409. [PMC free article] [PubMed] [Google Scholar]
- 12.Defrance, T., B. Vanbervliet, F. Briere, I. Durand, F. Rousset, and J. Banchereau. 1992. Interleukin 10 and transforming growth factor beta cooperate to induce anti-CD40-activated naive human B cells to secrete immunoglobulin A. J. Exp. Med. 175:671-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fahmi, H., C. Cochet, Z. Hmama, P. Opolon, and I. Joab. 2000. Transforming growth factor beta 1 stimulates expression of the Epstein-Barr virus BZLF1 immediate-early gene product ZEBRA by an indirect mechanism which requires the MAPK kinase pathway. J. Virol. 74:5810-5818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Golden, H. D., R. S. Chang, W. Prescott, E. Simpson, and T. Y. Cooper. 1973. Leukocyte-transforming agent: prolonged excretion by patients with mononucleosis and excretion by normal individuals. J. Infect. Dis. 127:471-473. [DOI] [PubMed] [Google Scholar]
- 15.Grogan, E., H. Jenson, J. Countryman, L. Heston, L. Gradoville, and G. Miller. 1987. Transfection of a rearranged viral DNA fragment, WZhet, stably converts latent Epstein-Barr viral infection to productive infection in lymphoid cells. Proc. Natl. Acad. Sci. USA 84:1332-1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hayes, D. P., A. A. Brink, M. B. Vervoort, J. M. Middeldorp, C. J. Meijer, and A. J. van den Brule. 1999. Expression of Epstein-Barr virus (EBV) transcripts encoding homologues to important human proteins in diverse EBV associated diseases. Mol. Pathol. 52:97-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henle, G., W. Henle, and V. Diehl. 1968. Relation of Burkitt's tumor-associated herpes-type virus to infectious mononucleosis. Proc. Natl. Acad. Sci. USA 59:94-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hochberg, D., J. M. Middeldorp, M. Catalina, J. L. Sullivan, K. Luzuriaga, and D. A. Thorley-Lawson. 2003. Demonstration of the Burkitt's lymphoma Epstein-Barr virus phenotype in dividing latently infected memory cells in vivo. Proc. Natl. Acad. Sci. USA 101:239-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inman, G. J., U. K. Binne, G. A. Parker, P. J. Farrell, and M. J. Allday. 2001. Activators of the Epstein-Barr virus lytic program concomitantly induce apoptosis, but lytic gene expression protects from cell death. J. Virol. 75:2400-2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joseph, A. M., G. J. Babcock, and D. A. Thorley-Lawson. 2000. EBV persistence involves strict selection of latently infected B cells. J. Immunol. 165:2975-2981. [DOI] [PubMed] [Google Scholar]
- 21.Keating, S., S. Prince, M. Jones, and M. Rowe. 2002. The lytic cycle of Epstein-Barr virus is associated with decreased expression of cell surface major histocompatibility complex class I and class II molecules. J. Virol. 76:8179-8188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khan, G., E. M. Miyashita, B. Yang, G. J. Babcock, and D. A. Thorley-Lawson. 1996. Is EBV persistence in vivo a model for B cell homeostasis? Immunity 5:173-179. [DOI] [PubMed] [Google Scholar]
- 23.Kilger, E., A. Kieser, M. Baumann, and W. Hammerschmidt. 1998. Epstein-Barr virus-mediated B-cell proliferation is dependent upon latent membrane protein 1, which simulates an activated CD40 receptor. EMBO J. 17:1700-1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laichalk, L. L., D. Hochberg, G. J. Babcock, R. B. Freeman, and D. A. Thorley-Lawson. 2002. The dispersal of mucosal memory B cells: evidence from persistent EBV infection. Immunity 16:745-754. [DOI] [PubMed] [Google Scholar]
- 25.Liu, Y. J., and C. Arpin. 1997. Germinal center development. Immunol Rev. 156:111-126. [DOI] [PubMed] [Google Scholar]
- 26.Liu, Y. J., C. Barthelemy, O. de Bouteiller, C. Arpin, I. Durand, and J. Banchereau. 1995. Memory B cells from human tonsils colonize mucosal epithelium and directly present antigen to T cells by rapid up-regulation of B7-1 and B7-2. Immunity 2:239-248. [DOI] [PubMed] [Google Scholar]
- 27.MacLennan, I. C. 1994. Germinal centers. Annu. Rev. Immunol. 12:117-139. [DOI] [PubMed] [Google Scholar]
- 28.Massague, J., and Y. G. Chen. 2000. Controlling TGF-beta signaling. Genes Dev. 14:627-644. [PubMed] [Google Scholar]
- 29.Matsuda, M., F. Salazar, M. Petersson, G. Masucci, J. Hansson, P. Pisa, Q. J. Zhang, M. G. Masucci, and R. Kiessling. 1994. Interleukin 10 pretreatment protects target cells from tumor- and allo-specific cytotoxic T cells and downregulates HLA class I expression. J. Exp. Med. 180:2371-2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Medina, F., C. Segundo, A. Campos-Caro, I. Gonzalez-Garcia, and J. A. Brieva. 2002. The heterogeneity shown by human plasma cells from tonsil, blood, and bone marrow reveals graded stages of increasing maturity, but local profiles of adhesion molecule expression. Blood 99:2154-2161. [DOI] [PubMed] [Google Scholar]
- 31.Merville, P., J. Dechanet, A. Desmouliere, I. Durand, O. de Bouteiller, P. Garrone, J. Banchereau, and Y. J. Liu. 1996. Bcl-2+ tonsillar plasma cells are rescued from apoptosis by bone marrow fibroblasts. J. Exp. Med. 183:227-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller, C. L., A. L. Burkhardt, J. H. Lee, B. Stealey, R. Longnecker, J. B. Bolen, and E. Kieff. 1995. Integral membrane protein 2 of Epstein-Barr virus regulates reactivation from latency through dominant negative effects on protein-tyrosine kinases. Immunity 2:155-166. [DOI] [PubMed] [Google Scholar]
- 33.Miyashita, E. M., B. Yang, G. J. Babcock, and D. A. Thorley-Lawson. 1997. Identification of the site of Epstein-Barr virus persistence in vivo as a resting B cell. J. Virol. 71:4882-4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miyashita, E. M., B. Yang, K. M. Lam, D. H. Crawford, and D. A. Thorley-Lawson. 1995. A novel form of Epstein-Barr virus latency in normal B cells in vivo. Cell 80:593-601. [DOI] [PubMed] [Google Scholar]
- 35.Niedobitek, G., A. Agathanggelou, N. Steven, and L. S. Young. 2000. Epstein-Barr virus (EBV) in infectious mononucleosis: detection of the virus in tonsillar B lymphocytes but not in desquamated oropharyngeal epithelial cells. Mol. Pathol. 53:37-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pascual, V., Y. J. Liu, A. Magalski, O. de Bouteiller, J. Banchereau, and J. D. Capra. 1994. Analysis of somatic mutation in five B cell subsets of human tonsil. J. Exp. Med. 180:329-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prang, N. S., M. W. Hornef, M. Jager, H. J. Wagner, H. Wolf, and F. M. Schwarzmann. 1997. Lytic replication of Epstein-Barr virus in the peripheral blood: analysis of viral gene expression in B lymphocytes during infectious mononucleosis and in the normal carrier state. Blood 89:1665-1677. [PubMed] [Google Scholar]
- 38.Rickinson, A. B., S. Finerty, and M. A. Epstein. 1977. Mechanism of the establishment of Epstein-Barr virus genome-containing lymphoid cell lines from infectious mononucleosis patients: studies with phosphonoacetate. Int. J. Cancer 20:861-868. [DOI] [PubMed] [Google Scholar]
- 39.Rickinson, A. B., and E. Kieff. 2001. Epstein-Barr virus, p. 2575-2628. In D. M. Knipe and P. M. Howley (ed.), Virology, 4th ed., vol. 2. Lippincott Williams and Wilkins, New York, N.Y.
- 40.Speck, S. H., T. Chatila, and E. Flemington. 1997. Reactivation of Epstein-Barr virus: regulation and function of the BZLF1 gene. Trends Microbiol. 5:399-405. [DOI] [PubMed] [Google Scholar]
- 41.Takada, K., and Y. Ono. 1989. Synchronous and sequential activation of latently infected Epstein-Barr virus genomes. J. Virol. 63:445-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Terstappen, L. W., S. Johnsen, I. M. Segers-Nolten, and M. R. Loken. 1990. Identification and characterization of plasma cells in normal human bone marrow by high-resolution flow cytometry. Blood 76:1739-1747. [PubMed] [Google Scholar]
- 43.Thorley-Lawson, D. A. 2001. Epstein-Barr virus, p. 970-985. In K. F. Austen, M. M. Frank, J. P. Atkinson, and H. Cantor (ed.), Sampter's immunologic diseases, 6th ed., vol. 2. Williams and Wilkins, New York, N.Y.
- 44.Thorley-Lawson, D. A. 2001. Epstein-Barr virus: exploiting the immune system. Nat. Rev. Immunol. 1:75-82. [DOI] [PubMed] [Google Scholar]
- 45.Thorley-Lawson, D. A., and G. J. Babcock. 1999. A model for persistent infection with Epstein-Barr virus: the stealth virus of human B cells. Life Sci. 65:1433-1453. [DOI] [PubMed] [Google Scholar]
- 46.Thorley-Lawson, D. A., and A. Gross. 2004. Persistence of the Epstein-Barr virus and the origins of associated lymphomas. N. Engl. J. Med. 350:1328-1337. [DOI] [PubMed] [Google Scholar]
- 47.Tierney, R. J., N. Steven, L. S. Young, and A. B. Rickinson. 1994. Epstein-Barr virus latency in blood mononuclear cells: analysis of viral gene transcription during primary infection and in the carrier state. J. Virol. 68:7374-7385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tortorella, D., B. E. Gewurz, M. H. Furman, D. J. Schust, and H. L. Ploegh. 2000. Viral subversion of the immune system. Annu. Rev. Immunol. 18:861-926. [DOI] [PubMed] [Google Scholar]
- 49.Yao, Q. Y., A. B. Rickinson, and M. A. Epstein. 1985. A re-examination of the Epstein-Barr virus carrier state in healthy seropositive individuals. Int. J. Cancer 35:35-42. [DOI] [PubMed] [Google Scholar]
- 50.zur Hausen, H., F. J. O'Neill, U. K. Freese, and E. Hecker. 1978. Persisting oncogenic herpesvirus induced by the tumour promotor TPA. Nature 272:373-375. [DOI] [PubMed] [Google Scholar]