Abstract
Objective
To determine the impact of the day and time of admission and discharge from the intensive care unit on mortality.
Methods
Prospective observational study that included patients admitted to the intensive care unit of the Hospital Maciel in Montevideo between April and November 2014.
Results
We analyzed 325 patients with an average age of 55 (36 - 71) years and a SAPS II value of 43 (29 - 58) points. No differences were found in the mortality of patients in the intensive care unit when time of admission (35% on the weekend versus 31% on weekdays, p = ns) or the hour of entry (35% at night versus 31% in the daytime, p = ns) were compared. The time of discharge was associated with higher hospital mortality rates (57% for weekend discharges versus 14% for weekday discharges, p = 0.000). The factors independently associated with hospital mortality after discharge from the intensive care unit were age > 50 years (OR 2.4, 95%CI, 1.1 - 5.4) and weekend discharge (OR 7.7, 95%CI, 3.8-15.6).
Conclusion
This study identified the time of discharge from the intensive care unit as a factor that was independently associated with hospital mortality.
Keywords: Patient admission, Patient discharge, Prognosis, Mortality, Intensive care units
Abstract
Objetivo
Determinar el impacto en la mortalidad del día y horario de admisión y alta de la unidad de cuidados intensivos.
Métodos
Estudio prospectivo observacional, que incluyó pacientes admitidos entre abril y noviembre de 2014 en la unidad de cuidados intensivos del Hospital Maciel de Montevideo.
Resultados
Se analizaron 325 pacientes con una edad de 55 (36 - 71) años y un valor SAPS II de 43 (29 - 58) puntos. No se encontraron diferencias en la mortalidad en unidad de cuidados intensivos de los pacientes al comparar el momento de ingreso (35% el fin de semana versus 31% en los días laborales, p = ns) ni el horario de ingreso (nocturnos 35% versus diurnos 31%, p = ns). El momento de egreso se asoció a mayor mortalidad en el hospital (57% en egresos del fin de semana versus 14% en días laborales, p = 0,000). Los factores independientemente asociados a mortalidad hospitalaria luego del alta de unidad de cuidados intensivos fueron la edad mayor de 50 años (OR 2,4; IC95%, 1,1 - 5,4) y el egreso durante el fin de semana (OR 7,7; IC95%, 3,8 - 15,6).
Conclusión
Este estudio logró identificar al momento del alta de la unidad de cuidados intensivos como un factor independientemente asociado a mortalidad hospitalaria.
INTRODUCTION
Mortality in the intensive care unit (ICU) is closely linked to patients' clinical characteristics and severity. However, there are other factors, such as the time or day of admission to and discharge from the ICU, that impact the prognosis of critical patients.(1,2)
Bell et al.(2) conducted a study in Canada that included the records of millions of patients and found that the day and time at which ICU admission occurs has an impact on patients' hospital survival. This timing is related to access to various technological resources for diagnosis.(2-5)
However, other studies did not find differences in hospital stay or mortality between patients admitted during the week and those admitted on the weekend, nor were they able to find differences according to the time of admission.(6,7)
Although the results remain controversial, the time of ICU admission has been extensively studied. Conversely, although the ICU discharge time may also have a special prognostic impact, this has been much less frequently evaluated in the literature. The deterioration in the quality and quantity of care that occurs when a patient is discharged may play a role in hospital mortality, and the transfer of patients to an area with a reduced capacity for care, as may occur in the hospital room, is among the transitions that carries the greatest risk for patient care.(8) So-called "off-hour" discharges - those that occur on weekends or at night (after 19:00 or 20:00) - are associated with adverse patient outcomes, including increased readmission to the ICU and increased mortality.(9-11) Laupland et al., in their study that included 7,380 patients, showed that discharges to the ward at the beginning of the weekend (Friday in the afternoon) were associated with an increased risk of dying in the hospital.(12)
The prognostic impact of the time of admission to or discharge from the ICU has not been studied in our setting. Evaluating this fact and identifying the factors associated with a worse prognosis are critical to strengthening health care systems and generating patient safety strategies that improve patient outcomes.
METHODS
This report describes a prospective, non-interventional, observational cohort study. We analyzed a cohort of patients older than 18 years consecutively admitted between April 1 and November 1, 2014, to the multipurpose ICU of a tertiary public hospital with 250 beds.
This intensive care unit has 24 beds divided into 19 intensive care beds and 5 moderate care beds.
The work model followed in the ICU includes 4 intensive care physicians in charge of 6 patients 24 hours a day, every day of the week. Three additional staff doctors attend for 8 hours a day, participating in patient care in the mornings and attending clinical meetings in the afternoon. These meetings involve the doctors and nurses of the service and focus on making decisions related to the care and discharge of the patients on the unit. In the ICU, there is a university nurse for every 6 patients and a nursing assistant for every 2 patients.
In the internment floor, the medical staff performs their activities from 8:00 to 14:00 from Monday to Friday. Outside of those hours, the care of patients on that floor shifts to 2 on-call doctors who confer for patient evaluations as required by the nursing staff. On the floor, each nurse is in charge of 8 patients, and each nursing assistant cares for 8 to 12 patients.
Patients are considered discharged from the unit upon their admission to the internment floor. Discharges are determined at the UCI clinical meeting that takes place in the afternoon; consequently, most discharges occur in the afternoon. As a consequence, the room staff has no contact with the patient until the following morning.
All patients younger than 18 years were excluded, as were those admitted to preoperative elective surgery whose stay was presumed to be less than 48 hours. These patients were excluded due to their low severity scores and their relatively short stay in the ICU and in the hospital.(13)
Data were collected using a standardized questionnaire and a pre-designed checklist. The data collected from all patients included sociodemographic and hospitalization information at the time of admission (age, sex, source, type of admission, comorbidities, severity score - Simplified Acute Physiology Score II (SAPS II) - in the first 24 hours, time and day of admission to the ICU, diagnosis and treatments performed at admission); ICU discharge data (day of discharge, indication of limits for therapeutic effort, and status at discharge); and finally, hospital evolution.
The following operating variables were defined: weekdays were from Monday at 8 AM to Friday at 7:59 AM; weekends were from Friday at 8 AM until Monday at 7:59 AM.
Daytime admissions occurred between 8:00 AM and 7:59 PM. Night admissions occurred between 8 PM and 7:59 AM. Off-hours discharges occurred after 8:00 PM.
This study was approved by the Ethics Committee of the Hospital Maciel, and the included patients gave prior informed consent.
Statistical analysis
The analysis was performed using the statistical package IBM SPSS version 21. The data are expressed as percentage or as median (quartiles 25% - 75%) for continuous variables. Categorical variables were compared using the chi square test or Fisher's exact test (with Yates correction when indicated). Continuous variables were compared with the Student t test or the rank-sum Mann-Whitney U test, according to the distribution of the variable. Statistical significance was set at p < 0.05. Variables associated with hospital mortality with p < 0.10 were included in a multivariate logistic regression model.
RESULTS
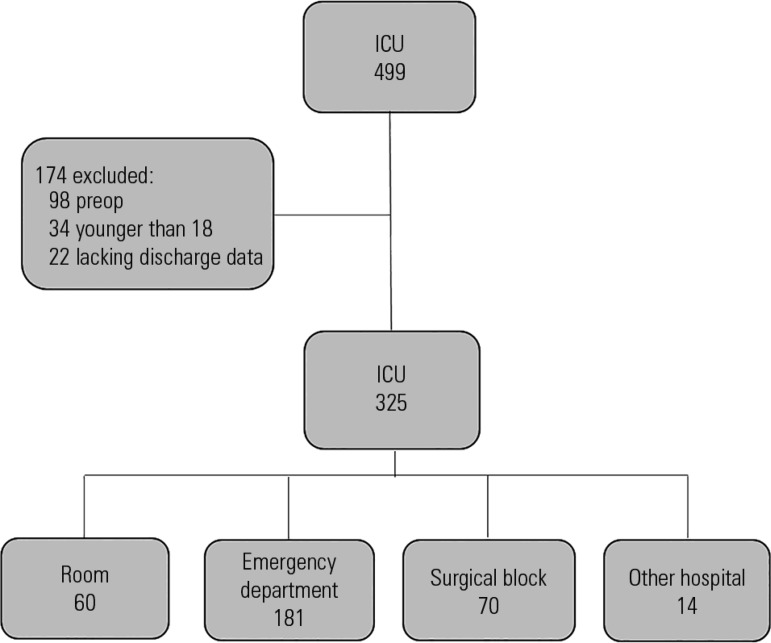
During the study period, 499 admissions to the ICU were recorded. A total of 174 patients were excluded (Figure 1). The 325 patients included in the study were predominantly male (61.8%), with a median age of 55 years (36 - 71) and a SAPS II value of 43 (29 - 58). The average ICU stay was 9 (4 - 16) days. The main comorbidities were heart disease (28%) and chronic obstructive disease (23%). The ICU admissions came mainly from the emergency department (ED; n = 181; 56%). Half of the admissions (163) occurred at night (8:00 PM - 07:59 AM), and 39% (127) occurred during the weekend (Friday 8:00 AM to Monday 7:59 AM). We identified 23 (7%) patients who were readmitted to the ICU. The remaining characteristics are presented in table 1.
Figure 1.
Structure for patient selection.
ICU - intensive care unit.
Table 1.
Characteristics of the population and comparisons based on the day and time of admission
| Characteristics | Total | Weekdays (N = 198) |
Weekend (N = 127) |
p value | Daytime admission (N = 163) |
Nighttime admission (N = 162) |
p value |
|---|---|---|---|---|---|---|---|
| N | 325 | 198 | 127 | 163 | 162 | ||
| Age | 55 (36 - 71) | 52 (35 - 71) | 59 (39 - 71) | ns | 58 (38 - 72) | 53 (32 - 70) | ns |
| Female | 124 (38%) | 72 (36) | 52 (41) | ns | 65 (40) | 59 (36) | ns |
| SAPS II | 43 (29 - 58) | 42 (28 - 54) | 46 (30 - 64) | ns | 45 (32 - 56) | 42 (26 - 61) | ns |
| Days before ICU admission | 0 (0 - 1) | 0 (0 - 1) | 0 (0 - 1) | ns | 0 (0 - 1) | 0 (0 - 1) | ns |
| Days in ICU | 9 (4 - 16) | 8,5 (4 - 16) | 10 (4 - 15) | ns | 10 (4 - 17) | 8 (4 - 15) | ns |
| Origin | ns | ns | |||||
| Room | 60 (19) | 40 (20) | 20 (16) | 33 (20) | 27 (17) | ||
| Surgical block | 70 (22) | 43 (22) | 27 (21) | 32 (20) | 38 (23) | ||
| Emergency | 181 (56) | 105 (53) | 76 (60) | 95 (58) | 86 (54) | ||
| Another hospital | 14 (4) | 10 (5) | 4 (3) | 4 (2) | 10 (6) | ||
| IMV | 270 (83) | 163 (82) | 107 (84) | ns | 136 (83) | 134 (83) | ns |
| Vasoactive drugs | 232 (71) | 139 (70) | 93 (73) | ns | 123 (75) | 109 (67) | ns |
| RRT | 12 (4) | 8 (4) | 8 (3) | ns | 9 (5) | 3 (2) | ns |
| Central venous access | 321 (99) | 196 (99) | 125 (98) | ns | 159 (97) | 162 (100) | ns |
| Arterial access | 262 (81) | 158 (80) | 104 (81) | ns | 131 (80) | 131 (81) | ns |
| Comorbidities | ns | ns | |||||
| EPOC | 75 (23) | 48 (24) | 27 (21%) | 43 (26) | 32 (20) | ||
| Cardiopathy | 90 (28) | 55 (28) | 35 (28) | 50 (31) | 40 (25) | ||
| Cancer | 16 (5) | 11 (6) | 5 (4) | 7 (4) | 9 (6) | ||
| CKD | 25 (8) | 17 (8) | 8 (6) | 17 (10) | 8 (5) | ||
| HIV | 10 (3) | 5 (2) | 5 (4) | 6 (4) | 4 (2) | ||
| Hospital stay | 20 (11 - 29) | 19 (10 - 29) | 21 (14 - 31) | ns | 20 (12 - 29) | 19,5 (10 - 30) | ns |
| Mortality in ICU | 107 (33) | 62 (31) | 45 (35) | ns | 51 (31) | 56 (35) | ns |
ns - non-significant; SAPS II - Simplified Acute Physiology Score II; ICU - intensive care unit; IMV - invasive mechanical ventilation; RRT - renal replacement therapy; COPD - chronic obstructive pulmonary disease; CKD - chronic kidney disease; HIV - human immunodeficiency virus; LTE - limitation of therapeutic effort. The results are expressed as number and percentage or median (25% - 75%).
There were no differences in the population characteristics according to the day or time of admission. Mortality did not differ according to the day or time of admission (31% weekday admission versus 35% weekend admission; p = ns; 31% daytime admission versus 35% nighttime admission; p = ns) (Table 1).
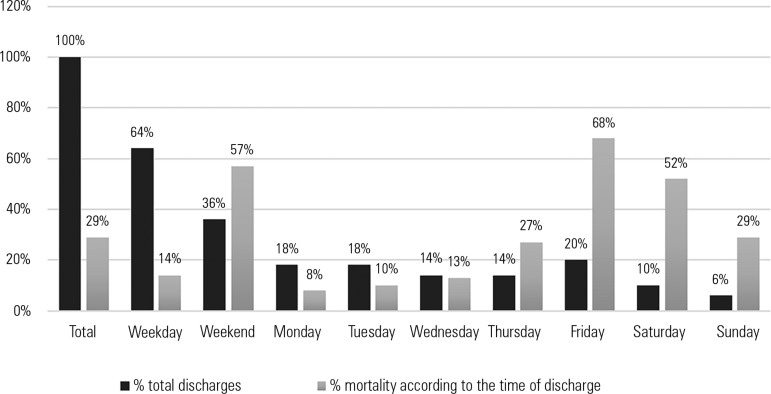
Of the patients discharged from the ICU (218), 30% (64) died in the hospital after ICU discharge. The ICU discharges were distributed as follows: 139 patients (64%) left the ICU on weekdays, and 79 (36%) left during the weekend (Figure 2). Patients discharged on the weekend had a significantly higher mortality (57% versus 14%; p = 0.000) (Table 2).
Figure 2.
Mortality according to the time of discharge from the intensive care unit.
Table 2.
Characteristics and mortality of patients based on the day of discharge from the intensive care unit
| Characteristics | Weekday discharge (N = 138) |
Weekend discharge (N = 79) |
p value |
|---|---|---|---|
| Female | 43 (31) | 29 (37) | ns |
| SAPS II | 37 (26 - 46) | 36 (23 - 43) | ns |
| Days in ICU | 10 (6 - 18) | 10 (5 - 22) | ns |
| Origin | ns | ||
| Room | 22 (16) | 15 (19) | |
| Surgical block | 33 (24) | 20 (25) | |
| Emergency | 78 (56) | 41 (52) | |
| Another hospital | 6 (4) | 3 (4) | |
| IMV | 103 (75) | 61 (79) | ns |
| Vasoactive drugs | 63 (46) | 30 (39) | ns |
| RRT | 8 (6) | 6 (8) | ns |
| Central venous access | 133 (97) | 73 (95) | ns |
| Arterial access | 81 (58) | 42 (55) | ns |
| Comorbidities | ns | ||
| EPOC | 25 (18) | 23 (29) | |
| Cardiopathy | 29 (21) | 22 (28) | |
| Cancer | 2 (1,5) | 4 (5) | |
| CKD | 7 (5) | 4 (5) | |
| HIV | 5 (3,5) | 1 (1,5) | |
| Tracheostomy | 33 (24) | 27 (35) | ns |
| Hospital stay | 21(12 - 29,5) | 16 (9,75 - 29) | ns |
| LTE | 7 (5) | 5 (6) | ns |
| Died in the hospital | 19 (14) | 45 (57) | 0,000 |
ns - non-significant; SAPS II - Simplified Acute Physiology Score II; ICU - intensive care unit; IMV - invasive mechanical ventilation; RRT - renal replacement therapy; COPD - chronic obstructive pulmonary disease; CKD - chronic kidney disease; HIV - human immunodeficiency virus; LTE - limitation of therapeutic effort. The results are expressed as percentage or median (25% - 75%).
Among the patients discharged from the ICU, factors associated with hospital mortality in the univariate analysis were SAPS II score > 35 (36% versus 21%; p = 0.017), weekend discharge (57% versus 14%, p = 0.000), the presence of chronic obstructive pulmonary disease (43% versus 26%, p = 0.031), history of heart disease (46% versus 25%, p = 0.005), and tracheostomy during the ICU stay (42% versus 25%, p = 0.019) (Table 3). Table 3 shows that the bivariable analysis found that age > 50 years was a factor associated with post-ICU mortality (43% versus 16%; p = 0.000).
Table 3.
Bivariate analysis of factors associated with hospital mortality
| Characteristics | Died in the hospital (with the characteristics) |
Died in the hospital (without the characteristics) |
p value |
|---|---|---|---|
| Age > 50 years | 46/108 43 | 18/109 16 | 0.000 |
| SAPS II > 35 | 43/118 36 | 21/99 21 | 0.017 |
| Comorbidities | |||
| CKD | 4/11 36 | 60/206 29 | 0.7 |
| EPOC | 20/47 43 | 44/170 26 | 0.031 |
| Cardiopathy | 23/50 46 | 41/167 25 | 0.005 |
| Cancer | 4/6 67 | 60/211 28 | 0.06 |
| HIV | 2/6 33 | 62/211 29 | 1 |
| MV | 51/166 31 | 13/51 25 | 0.5 |
| Vasopressors | 27/92 29 | 37/121 31 | 0.8 |
| Hemodialysis | 7/14 50 | 57/198 29 | 0.13 |
| Tracheostomy | 25/59 42 | 39/154 25 | 0.019 |
| Weekend discharge | 45/79 57 | 19/138 14 | 0.000 |
SAPS II - Simplified Acute Physiology Score II; CKD - chronic kidney disease; COPD - chronic obstructive pulmonary disease; HIV - human immunodeficiency virus; MV - mechanical ventilation. The results are expressed as specific value, total and percentage.
Using multivariate logistic regression analysis, the factors associated with hospital mortality after discharge from the ICU were discharge during the weekend (odds ratio [OR] 7.7; 95% confidence interval - 95% CI 3.8 - 15.6; p = 0.000) and age > 50 years (OR 2.4, 95% CI 1.1 - 5.4, p = 0.02) (Table 4).
Table 4.
Multivariate analysis of factors associated with hospital mortality
| OR | 95%CI | p value | |
|---|---|---|---|
| Age > 50 years | 2.4 | 1.1 - 5.4 | 0.02 |
| SAPS II> 35 points | 1.5 | 0.7 - 3.3 | ns |
| EPOC | 1.02 | 0.4 - 2.5 | ns |
| Cardiopathy | 1.6 | 0.7 - 3.9 | ns |
| Neoplasia | 3.3 | 0.4 - 23.9 | ns |
| Tracheostomy | 1.6 | 0.7 - 3.5 | ns |
| Weekend ICU discharge | 7.7 | 3.8 - 15.6 | 0.000 |
OR - odds ratio; CI - confidence interval; SAPS II - Simplified Acute Physiology Score II; COPD - chronic obstructive pulmonary disease; ICU - intensive care unit; ns - not significant.
DISCUSSION
The prognostic impact of the time of admission to and discharge from the ICU has been evaluated in different studies. The factors that have most often been associated with an increase in mortality for off-hours discharges are difficulty accessing diagnostic or therapeutic procedures, greater severity of patients who arrive on weekends and at night, and a lack of 24-hours access to intensive care doctors.(1-4,14-16)
When we analyzed our population, we did not find differences in patient according to the day or time of admission. In this context, there were no differences in patient mortality linked to the day or time of admission to the ICU. It should be noted that the analyzed hospital has intensive care doctors available in the ICU 24 hours per day every day of the year and similar access to diagnostic techniques at different times and days of the week. These factors may explain the lack of an effect on mortality by the time of ICU admission at this hospital.
The time at which the patient is discharged had a special prognostic implication in our study. Discharges to the floor during the weekend and mainly on Fridays were associated with higher hospital mortality rates. Several European authors have found similar results linked to off-hours discharges.(1,7,9,11,17-21) An evaluation of the causes associated with this lower survival is beyond the scope of this study, which was not designed for that purpose. Nevertheless, the increase in absenteeism on weekends combined with the treatment changes that result from transfer to the hospital room can explain this increase in mortality.(22,23) When evaluating the mortality rate for the 3 days of the weekend, we observed that the highest mortality occurred on Friday. Discharges on Sunday were associated with better prognoses. Like the results of the study that Laupland conducted in France, this finding raises the hypothesis that patients who are exposed to greater risk associated with reduced human resources or probable inconsistencies in care face a worse prognosis in the hospital.(12)
The fact that Fridays are associated with a worse prognosis can be explained by the greater amount of time patients admitted on Fridays are exposed to the weekend effect. It is likely that the high mortality of our patients on the hospital floor was the results of a clinical deterioration that went unnoticed during the transition of care on the weekend.
This problem will be challenging to resolve. Not allowing weekend discharges and prolonging patients' stays does not seem a reasonable solution, nor is increasing the number of beds feasible in the short-term. However, promoting a culture of safety and integrating it into the hospital's strategy can help resolve this conflict. In this scenario, strategies for improving the perception of risks, the safety of patients outside the ICU and the management of clinical deterioration may have a beneficial effect on mortality.(24-26) Early detection, follow-up at discharge, active screening for at-risk patients, and the activation of resources when alarming signs and symptoms appear reduces the risk of inadvertent clinical deterioration.(27-29) Expanding intensive care services outside the unit walls and developing critical care transition programs with the activation of rapid response teams, ICU extension teams, or ICU nursing liaison programs has proven to effectively reduce the weekend effect and increase patient safety.(30-33)
This study has limitations that must be considered when interpreting its results. It was conducted in a single center, so it only demonstrates the situation in that center over a specific period, and its results cannot be generalized to other settings. Additionally, the definitions of weekend and off-hour admission were arbitrarily established. Different studies have used different definitions.(18) Finally, our study focused on the ICU setting and evaluated data from patients' stay in the unit; therefore, it lacks detailed data on the aftercare provided in the rooms. Consequently, we can only generate hypotheses regarding the increase in mortality during the weekends.
CONCLUSION
This study shows that factors in addition to those related to the severity of the critical patient are associated with patient prognosis. Both the structure and the process of care impact the final outcome. In this sense, the time of discharge is independently associated with hospital mortality.
ACKNOWLEDGEMENTS
To Dr. Estrellita Echavarría for her ongoing support and to members of the Statistics Department of Hospital Maciel for their support.
Footnotes
Conflicts of interest: None.
Responsible editor: Jorge Ibrain Figueira Salluh
REFERENCES
- 1.Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117(3):151–157. doi: 10.1016/j.amjmed.2004.02.035. [DOI] [PubMed] [Google Scholar]
- 2.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345(9):663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 3.Cavallazzi R, Marik PE, Hirani A, Pachinburavan M, Vasu TS, Leiby BE. Association between time of admission to the ICU and mortality: a systematic review and metaanalysis. Chest. 2010;138(1):68–75. doi: 10.1378/chest.09-3018. [DOI] [PubMed] [Google Scholar]
- 4.Laupland KB, Shahpori R, Kirkpatrick AW, Stelfox HT. Hospital mortality among adults admitted to and discharged from intensive care on weekends and evenings. J Crit Care. 2008;23(3):317–324. doi: 10.1016/j.jcrc.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Wallace DA, Angus DC, Barnato AE, Kramer AA, Kahn JM. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012;366(22):2093–2101. doi: 10.1056/NEJMsa1201918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taira BR, Meng H, Goodman MS, Singer AJ. Does "off-hours" admission affect burn patient outcome. Burns. 2009;35(8):1092–1096. doi: 10.1016/j.burns.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 7.Morales IJ, Peters SG, Afessa B. Hospital mortality rate and length of stay in patients admitted at night to the intensive care unit. Crit Care Med. 2003;31(3):858–863. doi: 10.1097/01.CCM.0000055378.31408.26. [DOI] [PubMed] [Google Scholar]
- 8.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 9.Gantner D, Farley K, Bailey M, Huckson S, Hicks P, Pilcher D. Mortality related to after-hours discharge from intensive care in Australia and New Zealand, 2005-2012. Intensive Care Med. 2014;40(10):1528–1535. doi: 10.1007/s00134-014-3438-x. [DOI] [PubMed] [Google Scholar]
- 10.Goldfrad C, Rowan K. Consequences of discharges from intensive care at night. Lancet. 2000;355(9210):1138–1142. doi: 10.1016/S0140-6736(00)02062-6. [DOI] [PubMed] [Google Scholar]
- 11.Uusaro A, Kari A, Ruokonen E. The effects of ICU admission and discharge time on mortality in Finland. Intensive Care Med. 2003;29(12):2144–2148. doi: 10.1007/s00134-003-2035-1. [DOI] [PubMed] [Google Scholar]
- 12.Laupland KB, Misset B, Souweine B, Tabah A, Azoulay E, Goldgran-Toledano D, et al. Mortality associated with timing of admission to and discharge from ICU: a retrospective cohort study. BMC Health Serv Res. 2011;11:321–321. doi: 10.1186/1472-6963-11-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abella A, Hermosa C, Enciso V, Torrejón I, Molina R, Díaz M, et al. Efecto del momento de ingreso sobre el pronóstico de los pacientes en la Unidad de Cuidados Intensivo: on-hours vs. off-hours. Med Intensiva. 2016;40(1):26–32. doi: 10.1016/j.medin.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Bell CM, Redelmeier DA. Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004;117(3):175–181. doi: 10.1016/j.amjmed.2004.02.047. [DOI] [PubMed] [Google Scholar]
- 15.Selker HP, Beshansky JR, Pauker SG, Kassirer JP. The epidemiology of delays in a teaching hospital. The development and use of a tool that detects unnecessary hospital days. Med Care. 1989;27(2):112–129. doi: 10.1097/00005650-198902000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Kramer AA, Higgins TL, Zimmerman JE. The association between ICU readmission rate and patient outcomes. Crit Care Med. 2013;41(1):24–33. doi: 10.1097/CCM.0b013e3182657b8a. [DOI] [PubMed] [Google Scholar]
- 17.Obel N, Schierbeck J, Pedersen L, Storgaard M, Pedersen C, Sorensen HT, et al. Mortality after discharge from the intensive care unit during the early weekend period: a population-based cohort study in Denmark. Acta Anaesthesiol Scand. 2007;51(9):1225–1230. doi: 10.1111/j.1399-6576.2007.01431.x. [DOI] [PubMed] [Google Scholar]
- 18.Priestap FA, Martin CM. Impact of intensive care unit discharge time on patient outcome. Crit Care Med. 2006;34(12):2946–2951. doi: 10.1097/01.CCM.0000247721.97008.6F. [DOI] [PubMed] [Google Scholar]
- 19.Azevedo LC, de Souza IA, Zygun DA, Stelfox HT, Bagshaw SM. Association between nighttime discharge from the intensive care unit and hospital mortality: a multi-center retrospective cohort study. BMC Health Serv Res. 2015;15:378–378. doi: 10.1186/s12913-015-1044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Araujo TG, Rieder MM, Kutchak FM, Franco JW., Filho Readmissões e óbitos após a alta da UTI - um desafio da terapia intensiva. Rev Bras Ter Intensiva. 2013;25(1):32–38. doi: 10.1590/S0103-507X2013000100007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vollam SA, Dutton SJ, Young D, Watkinson PJ. Out-of-hours discharge from intensive care, in-hospital mortality and intensive care readmission rates: a systematic review protocol. Syst Rev. 2015;4:93–93. doi: 10.1186/s13643-015-0081-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bell CM, Redelmeier DA. Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004;117(3):175–181. doi: 10.1016/j.amjmed.2004.02.047. [DOI] [PubMed] [Google Scholar]
- 23.Schilling PL, Campbell DA, Jr, Englesbe MJ, Davis MM. A comparison of in-hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza. Med Care. 2010;48(3):224–232. doi: 10.1097/MLR.0b013e3181c162c0. [DOI] [PubMed] [Google Scholar]
- 24.Abella Álvarez A, Torrejón Perez I, Enciso Calderón V, Hermosa Gelbard C, Sicilia Urbán JJ, Ruiz Grispan M, et al. Proyecto UCI sin paredes. Efecto de la detección precoz de los pacientes de riesgo. Med Intensiva. 2013;37(1):12–18. doi: 10.1016/j.medin.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 25.Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, et al. ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016;44(8):1553–1602. doi: 10.1097/CCM.0000000000001856. [DOI] [PubMed] [Google Scholar]
- 26.van Sluisveld N, Hesselink G, van der Hoeven JG, Westert G, Wollersheim H, Zegers M. Improving clinical handover between intensive care unit and general ward professionals at intensive care unit discharge. Intensive Care Med. 2015;41(4):589–604. doi: 10.1007/s00134-015-3666-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laupland KB, Ball CG, Kirkpatrick AW. Hospital mortality among major trauma victims admitted on weekends and evenings: a cohort study. J Trauma Manag Outcomes. 2009;3:8–8. doi: 10.1186/1752-2897-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abizanda Campos R. Atención especializada al paciente crítico. Una contribución a la perspectiva sobre la especialidad en medicina intensiva. Med Intensiva. 2003;27(8):541–543. [Google Scholar]
- 29.Albright KC, Raman R, Ernstrom K, Hallevi H, Martin-Schild S, Meyer BC, et al. Can comprehensive stroke centers erase the "weekend effect"? Cerebrovasc Dis. 2009;27(2):107–113. doi: 10.1159/000177916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Niven DJ, Bastos JF, Stelfox HT. Critical care transition programs and the risk of readmission or death after discharge from an ICU: a systematic review and meta-analysis. Crit Care Med. 2014;42(1):179–187. doi: 10.1097/CCM.0b013e3182a272c0. [DOI] [PubMed] [Google Scholar]
- 31.Stelfox HT, Bastos J, Niven DJ, Bagshaw SM, Turin TC, Gao S. Critical care transition programs and the risk of readmission or death after discharge from ICU. Intensive Care Med. 2016;42(3):401–410. doi: 10.1007/s00134-015-4173-7. [DOI] [PubMed] [Google Scholar]
- 32.Rosa RG, Maccari JG, Cremonese RV, Tonietto TF, Cremonese RV, Teixeira C. The impact of critical care transition programs on outcomes after intensive care unit (ICU) discharge: can we get there from here? J Thorac Dis. 2016;8(7):1374–1376. doi: 10.21037/jtd.2016.05.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brunsveld-Reinders AH, Ludikhuize J, Dijkgraaf MG, Arbous MS, de Jonge E, COMET study group Unexpected versus all-cause mortality as the endpoint for investigating the effects of a Rapid Response System in hospitalized patients. Crit Care. 2016;20(1):168–168. doi: 10.1186/s13054-016-1339-9. [DOI] [PMC free article] [PubMed] [Google Scholar]