Introduction
Chemotherapy induced peripheral neuropathy (CIPN) is an under-addressed problem in oncology. Neurotoxic chemotherapy drugs are now used on the majority of persons who receive chemotherapy for cancer treatment in the United States (American Cancer Society, 2010). Numbness, muscle weakness, and loss of balance affecting the lower extremities are common manifestations of CIPN that lead to falls and other injuries (Hile, Fitzgerald, & Studenski, 2010; Tofthagen, Overcash, & Kip, 2011; Wampler et al., 2007). Primary treatment for CIPN includes dose reduction or discontinuation of the offending chemotherapeutic agent. Treatment of painful neuropathic symptoms with medications also has been a focus in clinical practice (Quasthoff & Hartung, 2002; Uceyler, Rogausch, Toyka, & Sommer, 2007). Medications often are useful for treating neuropathic pain, yet have not demonstrated any benefit for improving strength, gait, or balance (Kaley & Deangelis, 2009; Smith, Torrance, Bennett, & Lee, 2007; Smith, Cohen, Pett, & Beck, 2010). Little attention has been given to the deleterious effects of CIPN on physical performance in either research or clinical practice. With CIPN becoming a growing problem among both persons undergoing cancer treatment and cancer survivors, it is imperative that new methods of treating CIPN and its negative influence on physical performance are discovered (Visovsky, 2003; Visovsky, Collins, Abbott, Aschenbrenner, & Hart, 2007).
A conceptual model, developed by co-author, Constance Visovsky (Figure 1), illustrates the relationships between chemotherapy-induced peripheral neuropathy, exercise, including strength and balance training, and clinical outcomes. Neurotoxic chemotherapeutic agents induce sensory and motor neuropathy by activating mitochondrial and vascular dysfunction (Bennett, 2010; Flatters & Bennett, 2006; Siau, Xiao, & Bennett, 2006; Xiao & Bennett, 2007). These metabolic and vascular dysfunctions lead to sensory loss and reduced muscle strength, functions that depend upon cellular mitochondria to generate energy in the form of ATP (adenosine triphosphate). Thus, mitochondrial dysfunction results in the loss of energy-generating capability and vascular impairment deprives muscle and nerve cells of oxygen-rich nutrients, further impairing neuronal function. A limited number of human and animal studies have demonstrated that exercise stimulates endothelium-dependent vasodilation and vascular endothelial growth factor (VEGF) expression, increasing endoneurial blood flow and energy generating capacity through mitochondrial protein synthesis and glycolysis (Gustafsson, Puntschart, Kaijser, Jansson, & Sundberg, 1999; Ojala, Page, Moore, & Thompson, 2001). Exercises, including those designed to increase strength and balance, as well as aerobic exercise, may increase the supply of blood, oxygen, and glucose to mitochondria, allowing the mitochondria to produce energy in a more efficient manner. Increasing mitochondrial energy production and blood flow to peripheral nerves may result in fewer neuropathic symptoms, increased strength and balance, and better quality of life. Further studies designed to test this conceptual model are needed.
Figure 1.
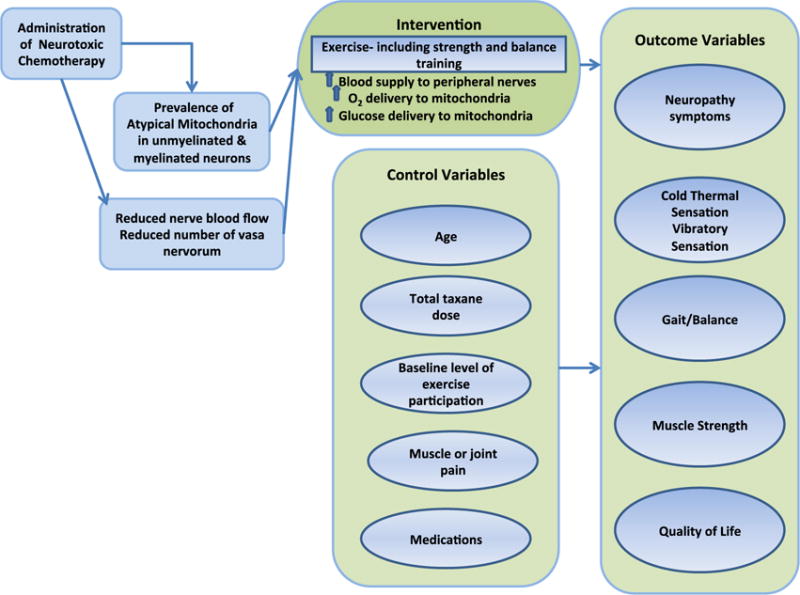
Conceptual Model
Although studies in cancer populations are lacking, there is a growing body of evidence to support specific muscle strengthening and balance training exercises in community dwelling older adults at risk for falls. While new studies of persons with CIPN are crucial, existing data suggest multiple benefits of strength and balance training that can be utilized in clinical oncology practice. A Cochrane Review published in 2009 analyzed the strength of evidence to support interventions for preventing falls in community dwelling older adults (Gillespie et al., 2009). Falls were defined as an unintentionally and sudden vertical decline to the floor or ground (Conroy et al., 2010). Fall risk measurement included measures of gait, balance, and performance status using measures such as the Timed Up and Go, which measures the time it takes to arise from a chair, walk 10 feet, turn around, walk back, and sit down and is highly sensitive and specific for fall prediction (Shumway-Cook, Brauer, & Woollacott, 2000). The meta-analysis included 31 randomized clinical trials of strength and balance training programs conducted from 1994–2008. The authors concluded that strength, balance, flexibility, and endurance training were effective in reducing falls and improving balance in community dwelling older adults, provided there was a combination of at least two of the four elements (strength, balance, flexibility, and endurance training). Although there is some conflicting evidence that such programs reduce fall risk, discrepancies are most likely related to methodological concerns (Gillespie et al., 2009).
Numerous studies published since the 2009 Cochrane Review may provide additional information about the efficacy of these interventions. The purpose of this review article is to: 1) evaluate the evidence for strength and balance training programs in persons at high risk of falls; 2) discuss how results of existing studies might guide clinical practice; and 3) to discuss directions for further research.
Methods
A search of Pubmed and CINAHL databases was conducted in June of 2011 using the search terms strength, balance training, falls, elderly, and neuropathy. Only clinical trials conducted utilizing specific strength or balance training exercises that included community dwelling adults and examined falls, fall risk, balance, and/or strength as outcome measures were included in this review (Table 1). Studies of persons with peripheral neuropathy, or those at high risk for peripheral neuropathy also were included. Studies were excluded if the sample was focused on persons with non-cancer co-morbidities such as osteopenia, dementia, osteoporosis, stroke, or multiple sclerosis. Case studies, and studies comparing strength and balance training to another type of intervention, were also excluded. Because the previously mentioned Cochrane Review included research through October 2008, only studies published from October 2008 through June 2011 were reviewed. One matched case-control study and two randomized, controlled studies evaluating strength and balance training in persons with diabetes-related peripheral neuropathy were identified. Eleven studies evaluating strength and balance programs in community dwelling adults at high risk of fall were identified.
Table 1.
Table of Articles.
| Reference | Purpose | Design | Sample | Intervention | Measurement | Results | Comments |
|---|---|---|---|---|---|---|---|
| Morrison, Colberg, Mariano, Parson, & Vinik (2010) | Assess fall risk and efficacy of strength and balance training in diabetics | Interventional | 16 participants with neuropathy (group 1) and 21 age matched controls (group 2). | strength and balance program three times a week for 6 weeks | Physiologic Profile Assessment (PPA); Simple Reaction Time (SRT) | Group 1 demonstrated decreased fall risk | Intervention not fully described; Small sample; No long term follow up All participants had neuropathy; No random assignment; No blinding |
| Kruse, R. L., Lemaster, J. W., & Madsen, R. W. (2010). Ther. | Evaluate the efficacy of a home based exercise program in persons with diabetic neuropathy | RTC | Diabetics with neuropathy, >49 years old (control n=38, intervention n=41) | 2 parts: Months 1–3 Intervention group had 8 physical therapy sessions then 3 hour long sessions at home with therapist, development of an individualized walking program; months 4–12 intervention group received weekly phone calls encouraging exercise. | Berg Balance Test; Unipedal Stance Time;Timed UP and Go (TUG) Falls Efficacy Scale; Foot Function Disability Scale; Self-reported falls data | No significant differences between groups in falls or strength, one measure of balance better in the intervention group. | Home based program with low rates of compliance; Single blinded; No supervision of exercise after the first 2 months; Strength of the intervention may not have been enough to detect significant group differences; Outcome measures were evaluated at baseline,3, 6, and 12 months, although the 3 month data is not provided or included in the analyses |
| Allet, L., Armand, S., de Bie, R. A., Golay, A., Monnin, D., Aminian, K., & de Bruin, E. D. (2010). | Evaluate a 12 week strength and balance training program on gait, balance, and fear of falling | RCT | 71 patients with diabetic neuropathy (control n=36, intervention n=35) | 60 minute group exercise sessions with a physical therapist twice a week fir 12 weeks, the control group maintained their usual physical activities, which were unmonitored | Performance oriented mobility assessment (POMA);outdoor gait assessment using a Gyroscope device; dynamic balance test; static balance test using Biodex device | Walking speed, strength, and balance were significantly better in the intervention group, results sustained at 6 months | Demonstrate sustained results 3 months after the intervention ended; Falls were not an outcome measure |
| Clemson, L., Singh, M. F., Bundy, A., Cumming, R. G., Weissel, E., Munro, J., & Black, D. (2010). | Evaluate a program that embeds strength and balance exercises into daily activities | RCT | Intervention (n=18) control (n=16) adults> 70 years with 2 or more falls or a fall related injury over the past year | Intervention group received education on core balance and strength training principles taught in 5 home visits followed by 2 booster visits and 2 phone calls | Balance- Narrow base, half tandem. Tandem and unipedal stand times, timed tandem walk;dynamometer for hip, knee and ankle strength; falls-self reported | A reduced risk of recurrent falls was identified as well as improvement in dynamic balance and left knee strength | Low burden on participants; High attrition in the intervention group; Outcome measurements at baseline, 3, and 6 months; Results not sustained at 6 months |
| Conroy, S., Kendrick, D., Harwood, R., Gladman, J., Coupland, C., Sach, T., & Masud, T. (2010). | To determine the efficacy of a falls prevention program for older adults at high risk of fall dwelling in the community | RCT | Intervention (n=183) Control (n=181) Adults age>70 with a previous fall or two fall risk factors | 12 months of strength and balance training tailored to the needs and abilities of the individual, along with occupational therapy, home safety assessment and medical care | Monthly falls diaries | There was a definite trend toward reduction in falls but it was not statistically significant | Large sample;Targeted persons at high risk; High attrition rate; Few details provided about strength and balance aspects of the intervention; Control group members may have participated in a similar program available in the community;No measures of strength or balance included |
| Iwamoto, J., Suzuki, H., Tanaka, K., Kumakubo, T., Hirabayashi, H., Miyazaki, Y., & Matsumoto, H. (2009). | To evaluate an exercise program, including strength and balance training) for prevention of falls among older adults. | RTC | (N=68) persons>50 years old | 30 minutes, 3 times a week, for 5 months with strength, balance. And power training, and walking | Balance-Indices of flexibility, tandem standing time, tandem gait step number, unipedal standing time Muscle power –TUG, chair rising time, 10 m walk time | The intervention group had better balance, muscle power, and falls than the control group at the end of the intervention. | Intervention led by general practitioners rather than physical therapists; All of the intervention group completed 100% of the program; Small sample; No longitudinal data |
| Beling, J., & Roller, M. (2009). | To evaluate a small group balance program | RTC | N=23 adults >64 years | 30 minutes, three times a week for 12 weeks group in a small group balance program called Matter of Balance | Strength-Manual muscle testing Gait-cadence stride length, step length, velocity, base width, double support, swing, and stance using GAITRite system Balance-dynamic posturography with Smart Equitest, Motor Control Test, Adaptation Test, Berg Balance Scale | Measures of strength, balance, and falls were significantly better in the intervention group. | No objective measures of strength; small sample; Lack of inter-rater reliability for MMT |
| Comans, T. A., Brauer, S. G., & Haines, T. P. (2010). | To compare home based to center based delivery of a falls prevention program | RTC | N=107 >60 years old at increased risk of falls | Both groups received weekly supervised balance training for 8 weeks and were asked to perform 3 balance exercises twice a day for 10 minutes on other days. | Falls information collected monthly by telephone | Fall incidencelower in the center based group than in the home based group | Center based intervention also contained a home exercise component |
| Arampatzis, A., Peper, A., & Bierbaum, S. (2011). | To determine mechanisms responsible for dynamic stability | RTC | Healthy older adults age 65–75 (n=55) | 3 group study (two intervention and a control); balance exercises only, balance and strength exercises, no exercise. Intervention groups exercised for 1.5 hours twice a week for 14 weeks | Forward fall simulation for balance, dynamometer for muscle strength | Both control groups showed improvements in ability to regain balance group. | 38 completed the study;Interventions briefly described. |
| Hagedorn, D. K., & Holm, E. (2010). | To compare standard balance training with computer assisted balance training | RTC | Frail elderly, aged 69–95 (n=35) | Both groups exercised for 1.5 hours twice a week for 12 weeks | Muscle force testing using spring gauge; sit to stand test, Arm flexion, TUG, 6 minute walk test, MCTSIB Unipedal stance time, Tandem test, Berg Balance Scale, Dynamic Gait Index, Falls Efficacy Scale-International. | Both groups demonstrated significant improvements in strength and balance | 27 completed the study; computer assisted group also had improved endurance. |
| Hartmann, A., Murer, K., de Bie, R. A., & de Bruin, E. D. (2009). | Compare a standard exercise program with a similar program that also included gymnastic exercises of the feet. | RTC | Community dwelling adults > 64 years (n=56) | 3 groups- group 1 did 25 minutes of aerobic and resistance exercises twice a week for 12 weeks (n=28), group 2 did 4 additional minutes of foot gymnastics (n=28), and group 3 did no exercise. | Falls Efficacy Scale – International (ankle ROM, Expanded Timed Get-up-and-Go test (ETGUG), gait analysis and muscle power measurement | Both exercise groups exhibited improvement in strength, power, and performance. The addition of foot gymnastics made no significant difference. | No balance specific exercises were included;45 participants completed the study;control group data (n=14) came from a previous study. |
| Persch, L. N., Ugrinowitsch, C., Pereira, G., & Rodacki, A. L. (2009). | To evaluate the effects of strength training on gait parameters and fall risk. | RTC | Community dwelling women>59 years (n=27) | progressive resistance exercises three times a week for 12 weeks. | Photography was used to measure muscle strength and range of motion. | Strength training improved both strength and balance. | Duration (in minutes/hrs) of exercise program not provided. |
| Miller, K. L., Magel, J. R., & Hayes, J. G. (2010). | Evaluate a 4-week standing exercise and balance training intervention | Quasi-experimental | Adults aged 71 to 85 receiving home health care | therapist led standing exercise and balance training program twice a day, five days a week for 4 weeks. | Falls Efficacy Scale; one-leg stance test; Performance Oriented Mobility Assessment. | Balance, balance confidence and gait improved significantly from pre-test to post-test. | Home exercise program, led by therapist trained caregivers; 100% compliance; standardized protocol; objective and subjective measures; No control group; small sample, non-blinded. |
Effects of Strength and Balance Training in Peripheral Neuropathy
Symptoms of neuropathy are similar, regardless of the underlying cause, therefore in the absence of studies evaluating strength and balance training for CIPN, data from persons with diabetic neuropathy provide the best support for recommending strength and balance training to patients with neuropathy. Compared to healthy controls, persons with neuropathy secondary to diabetes have reduced proprioception, lower extremity sensation, and reduced ankle strength predisposing them to falls. Following participation in a strength and balance training intervention, significantly fewer falls occurred (Morrison, Colberg, Mariano, Parson, & Vinik, 2010).
Two randomized, controlled trials provide preliminary evidence to support the efficacy of strength and balance training for neuropathy. Allet and colleagues (2010) reported significantly improved balance and strength, increased walking speed, and decreased fear of falling in participants a 60 minute, twice a week for 12 weeks, strength, balance, and functional training program. The results were sustained for a period of six months. Furthermore, the training program was feasible and safe for persons with peripheral neuropathy.
Kruse, Lemaster, and Madsen (2010) assessed the effects of weight bearing exercise on lower extremity strength, balance, and falls. Although few differences in balance, muscle strength, fall or fear of falling, were identified, the intervention was determined to be safe and well tolerated in diabetic persons with peripheral neuropathy. This conclusion is of great importance because as the authors explained, exercise has not been encouraged in persons with diabetic neuropathy because of concerns of increased foot ulceration and fall (Kruse et al., 2010).
Improved Gait and Postural Control
Steady gait requires strength and coordination of the larger muscles of the lower extremities, which are diminished in persons with neuropathy. Progressive resistance training is considered to be the most effective intervention for building muscle strength in older adults (Ferri et al., 2003; Paterson, Jones, & Rice, 2007; Symons, Vandervoort, Rice, Overend, & Marsh, 2005). Strengthening of muscles around the knee joint is related to stride length and cadence changes and can influence reduction in falls in the elderly. Strength training is an intervention that can also improve gait pattern (Persch, Ugrinowitsch, Pereira, & Rodacki, 2009). Other interventions that improve standing balance or increase foot strength and ankle range of motion (ROM) also show promise in reducing falls and improving physical performance (Miller, Magel, & Hayes, 2010). Interventions specifically targeted toward improving muscle strength, balance or ROM have been efficacious in improving gait parameters and reducing falls (Hartmann, Murer, De Bie and De Bruin, 2009, Miller et al., 2010). Significant improvements in knee extension, ankle dorsiflexion, sitting to standing, the 6-minute walk test, and balance with eyes closed have been demonstrated even among frail older adults who displayed increased physical endurance and static balance after participating in both standard balance training and computer assisted balance training (Hagedorn & Holm, 2010). Interventions to improve balance and stability may also be important in assisting older persons to adapt to changes in terrain or gait speed and regain balance after forward falls (Arampatzis, Peper, & Bierbaum, 2011).
Reducing Falls
Falls and fall related injuries are a major concern in persons with CIPN (Tofthagen, Overcash, & Kip, 2011). Several recent studies have demonstrated reductions in falls or fall risk in older adults participating in strength and balance training programs. Persons at greatest fall risk, who are the most likely to benefit from a falls prevention program, may also have the greatest difficulty participating (Conroy et al., 2010). Researchers in Australia identified the need for a strength and balance training program that imbedded strength and balance training exercises into daily activities. They evaluated a home based program called Lifestyle Approach to Reducing Falls Through Exercise (LiFE) The group receiving the LiFE intervention experienced fewer falls, improvements in dynamic balance, and fall related self-efficacy (Clemson et al., 2010). Interventions that include muscle power building exercises and walking in addition to strength and balance training also have resulted in improved balance, walking ability, and fall incidence (Iwamoto et al., 2009).
There is no clear indication from the literature as to whether home based or institution based falls prevention programs are better. Home based programs have demonstrated similar efficacy in improving physical function but institution based programs may offer greater benefits in terms of reducing falls. Data suggests that while institutional based programs may be more effective, participation and adherence may increase when a home based program is offered (Comans, Brauer, & Haines, 2010).
Discussion
The findings from the studies we reviewed provide substantial evidence to support the use of strength and balance training for older adults at risk for falls and beginning evidence to support strength and balance training for individuals with peripheral neuropathy. The studies we reviewed of strength and balance training programs for diabetics with peripheral neuropathy indicate that persons with neuropathy can safely participate in and may receive benefit from strength and balance training (Allet et al., 2010; Kruse et al., 2010; Morrison et al., 2010). Several studies have described risk for postural instability, falls, and fall related injury in persons with chemotherapy-induced peripheral neuropathy and recommended physical therapy as a treatment option but no studies were identified that evaluate strength and balance training for treatment of chemotherapy-induced peripheral neuropathy (Hile et al., 2010; Tofthagen, 2010; Tofthagen et al., 2011; Wampler et al., 2007). While more studies are needed to evaluate efficacy, data from the studies we reviewed support strength and balance training as a safe intervention for patients with chemotherapy-induced peripheral neuropathy. Strength and balance training should be recommended when patients are experiencing loss of balance associated with chemotherapy induced peripheral neuropathy since it is a source of significant disability with few evidence-based treatment strategies available (Visovsky et al., 2007).
Implications for Practice
Numerous studies, primarily in the physical therapy and geriatric literature, support the use of strength and balance training exercises among community dwelling adults with postural instability or high risk for falls (Allet et al., 2010; Arampatzis et al., 2011; Beling & Roller, 2009; Clemson et al., 2010; Comans et al., 2010; Conroy et al., 2010; Hagedorn & Holm, 2010; Iwamoto et al., 2009; Kruse et al., 2010; Miller et al., 2010; Morrison et al., 2010; Persch et al., 2009). These studies have direct application to oncology practice and research because many patients, particularly during chemotherapy or radiation therapy, or in advanced stages of disease, experience generalized weakness, muscle weakness, unsteadiness, or problems maintaining balance. Cancer-related fatigue from disease and treatment effects often induces patients to rest, inducing muscle weakness and atrophy that then can contribute to fall and injury risk. As the incidence of cancer increases exponentially with age, co-morbid conditions and age- related physiologic changes additionally contribute to muscle weakness, loss of balance, and increase the likelihood of falls and fall related injuries. A growing amount of data in non-cancer populations demonstrates that neuropathy, which is caused by many of the treatments used in the fight against cancer and also can occur as a result of the cancer itself, is a risk factor for falls and fall related injuries (Allet et al., 2010; Kruse et al., 2010; Morrison et al., 2010). A holistic and multi-disciplinary approach to cancer treatment includes attention to treating both the cancer and the symptoms that arise from the cancer and/or its treatment, as well as addressing issues that negatively affect quality of life.
Strength and balance training exercises can easily be provided by a physical therapist and there is a great deal of data that supports physical therapist led exercise interventions that include specific exercises to strengthen the lower extremities and improve balance (Allet et al., 2010; Arampatzis et al., 2011; Beling & Roller, 2009; Clemson et al., 2010; Comans et al., 2010; Conroy et al., 2010; Hagedorn & Holm, 2010; Iwamoto et al., 2009; Kruse et al., 2010; Miller et al., 2010; Morrison et al., 2010; Persch et al., 2009). Participation in exercise programs focused on improving lower extremity strength and balance has been repeatedly demonstrated as safe, even among people with a very high risk of falls (Clemson et al., 2010; Comans et al., 2010; Conroy et al., 2010).
Directions for Future Research
There is a great need for additional research exploring the benefits and limitations of strength and balance training in oncology populations. The studies in our review indicate that while patients may be more likely to adhere to a home based strength and balance training program, institution based programs may offer better results, probably because of the inherent challenges of monitoring adherence in a home setting (Comans et al., 2010). Interventions that focus on strength and balance have not been adequately tested in an oncology population, and have not examined falls or related injury as the primary outcome. As the population ages and cancer survival rates increase, interventions aimed at improving strength and balance and ultimately physical functioning, become important in assisting elders in maintaining independence.
The best time to offer strength and balance training should be explored. Patients receiving chemotherapy and radiation therapy, who have multiple appointments for cancer therapy, blood draws, injections, physician and nursing visits, may benefit but making a commitment to attend or participate may prove challenging due to multiple demands on their time. Symptoms including fatigue, weakness, and insomnia also can interfere with patients’ ability to participate.
The amount of exercise (dose) needed to achieve the desired improvements in strength and balance and reduction in falls has not been determined and may vary from one population to the next. In the studies we reviewed, the time that participants engaged in exercise ranged from 10 minutes to 1 hour at a time, from once a week to twice a day, and from 4 weeks to 12 months. Therefore, even though strength and balance training exercises can be recommended, the frequency and duration with which they should be prescribed are as yet indeterminate.
Exercise in general is known to decrease fatigue among persons with cancer but it is unknown how strength and balance training might affect cancer related symptoms like fatigue, sleep disturbance, or depression. Exercise programs that include strength and balance training may increase physical performance, increase independence and have positive effects on role function or other elements of health related quality of life. Future studies involving oncology populations should include these as secondary outcomes. In addition to improving strength and balance, researchers should examine whether strength and balance training can decrease pain or numbness associated with chemotherapy induced peripheral neuropathy.
Conclusions
The evidence demonstrates that strength and balance training is safe and effective at reducing falls and improving lower extremity strength and balance in adults over 50 years of age, who are at high risk for falls, including persons with diabetic peripheral neuropathy. Future studies should evaluate the effects of strength and balance training in persons with cancer, particularly individuals with chemotherapy induced peripheral neuropathy. Important goals for future studies include identifying the most effective dose and method of delivery, and evaluating the effects on cancer related symptoms and quality of life.
References
- American Cancer Society. Cancer facts and figures 2010. 2010 Retrieved from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-026238.pdf.
- Allet L, Armand S, de Bie RA, Golay A, Monnin D, Aminian K, de Bruin ED. The gait and balance of patients with diabetes can be improved: a randomised controlled trial. Diabetologia. 2010;53(3):458–466. doi: 10.1007/s00125-009-1592-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arampatzis A, Peper A, Bierbaum S. Exercise of mechanisms for dynamic stability control increases stability performance in the elderly. Journal of Biomechanics. 2011;44(1):52–58. doi: 10.1016/j.jbiomech.2010.08.023. doi: S0021-9290(10)00457-4 [pii] 10.1016/j.jbiomech.2010.08.023. [DOI] [PubMed] [Google Scholar]
- Beling J, Roller M. Multifactorial intervention with balance training as a core component among fall-prone older adults. Journal of Geriatric Physical Therapy. 2009;32(3):125–133. doi: 10.1519/00139143-200932030-00008. [DOI] [PubMed] [Google Scholar]
- Bennett GJ. Pathophysiology and animal models of cancer-related painful peripheral neuropathy. The Oncologist. 2010;2010(15 Suppl 2):9–12. doi: 10.1634/theoncologist.2009-S503. [DOI] [PubMed] [Google Scholar]
- Clemson L, Singh MF, Bundy A, Cumming RG, Weissel E, Munro J, Black D. LiFE Pilot Study: A randomised trial of balance and strength training embedded in daily life activity to reduce falls in older adults. Australian Occupational Therapy Journal. 2010;57(1):42–50. doi: 10.1111/j.1440-1630.2009.00848.x. doi: AOT848 [pii]10.1111/j.1440-1630.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- Comans TA, Brauer SG, Haines TP. Randomized trial of domiciliary versus center-based rehabilitation: which is more effective in reducing falls and improving quality of life in older fallers? Journals of Gerontology Series A Biological Sciences and Medical Sciences. 2010;65(6):672–679. doi: 10.1093/gerona/glq054. doi: glq054 [pii] 10.1093/gerona/glq054. [DOI] [PubMed] [Google Scholar]
- Conroy S, Kendrick D, Harwood R, Gladman J, Coupland C, Sach T, Masud T. A multicentre randomised controlled trial of day hospital-based falls prevention programme for a screened population of community-dwelling older people at high risk of falls. Age and Ageing. 2010;39(6):704–710. doi: 10.1093/ageing/afq096. doi: afq096 [pii] 10.1093/ageing/afq096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferri A, Scaglioni G, Pousson M, Capodaglio P, Van Hoecke J, Narici MV. Strength and power changes of the human plantar flexors and knee extensors in response to resistance training in old age. Acta Physiologica Scandinavica. 2003;177(1):69–78. doi: 10.1046/j.1365-201X.2003.01050.x. doi: 1050 [pii] [DOI] [PubMed] [Google Scholar]
- Flatters SJ, Bennett GJ. Studies of peripheral sensory nerves in paclitaxel-induced painful peripheral neuropathy: evidence for mitochondrial dysfunction. Pain. 2006;122(3):245–257. doi: 10.1016/j.pain.2006.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, Rowe BH. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. 2009;(2):CD007146. doi: 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- Gustafsson T, Puntschart A, Kaijser L, Jansson E, Sundberg C. Exercise-induced expression of angiogenesis-related transcription and growth factors in human skeletal muscle. American Journal of Physiology. 1999;276:H679–H685. doi: 10.1152/ajpheart.1999.276.2.H679. [DOI] [PubMed] [Google Scholar]
- Hagedorn DK, Holm E. Effects of traditional physical training and visual computer feedback training in frail elderly patients. A randomized intervention study. European Journal of Physical Rehabilitation Medicine. 2010;46(2):159–168. doi: R33102227 [pii] [PubMed] [Google Scholar]
- Hile ES, Fitzgerald GK, Studenski SA. Persistent mobility disability after neurotoxic chemotherapy. Physical Therapy. 2010;90(11):1649–1657. doi: 10.2522/ptj.20090405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwamoto J, Suzuki H, Tanaka K, Kumakubo T, Hirabayashi H, Miyazaki Y, Matsumoto H. Preventative effect of exercise against falls in the elderly: a randomized controlled trial. Osteoporosis International. 2009;20(7):1233–1240. doi: 10.1007/s00198-008-0794-9. [DOI] [PubMed] [Google Scholar]
- Kaley TJ, Deangelis LM. Therapy of chemotherapy-induced peripheral neuropathy. British Journal of Haematology. 2009;145(1):3–14. doi: 10.1111/j.1365-2141.2008.07558.x. [DOI] [PubMed] [Google Scholar]
- Kruse RL, Lemaster JW, Madsen RW. Fall and balance outcomes after an intervention to promote leg strength, balance, and walking in people with diabetic peripheral neuropathy: “Feet First” randomized controlled trial. Physical Therapy. 2010;90(11):1568–79. doi: 10.2522/ptj.20090362. [DOI] [PubMed] [Google Scholar]
- Miller KL, Magel JR, Hayes JG. The effects of a home-based exercise program on balance confidence, balance performance, and gait in debilitated, ambulatory community-dwelling older adults: a pilot study. Journal of Geriatric Physical Therapy. 2010;33(2):85–91. [PubMed] [Google Scholar]
- Morrison S, Colberg SR, Mariano M, Parson HK, Vinik AI. Balance training reduces falls risk in older individuals with type 2 diabetes. Diabetes Care. 2010;33(4):748–750. doi: 10.2337/dc09-1699. doi: dc09-1699[pii] 10.2337/dc09-1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojala B, Page L, Moore M, Thompson L. Effects of inactivity on glycolytic capacity of single skeletal muscle fibers in adult and aged rats. Biological Research for Nursing. 2001;3(2):86–95. doi: 10.1177/109980040200300204. [DOI] [PubMed] [Google Scholar]
- Paterson DH, Jones GR, Rice CL. Ageing and physical activity: evidence to develop exercise recommendations for older adults. Canadian Journal of Public Health. 2007;98(Suppl 2):S69–108. [PubMed] [Google Scholar]
- Persch LN, Ugrinowitsch C, Pereira G, Rodacki AL. Strength training improves fall-related gait kinematics in the elderly: a randomized controlled trial. Clinical Biomechanics (Bristol, Avon) 2009;24(10):819–825. doi: 10.1016/j.clinbiomech.2009.07.012. doi: S0268-0033(09)00173-9[pii] 10.1016/j.clinbiomech.2009.07.012. [DOI] [PubMed] [Google Scholar]
- Quasthoff S, Hartung HP. Chemotherapy-induced peripheral neuropathy. Journal of Neurology. 2002;249(1):9–17. doi: 10.1007/pl00007853. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community dwelling older adults using the Timed Up & Go Test. Physical Therapy. 2000;80(9):896–903. [PubMed] [Google Scholar]
- Siau C, Xiao W, Bennett GJ. Paclitaxel- and vincristine-evoked painful peripheral neuropathies: loss of epidermal innervation and activation of Langerhans cells. Experimental Neurology. 2006;201(2):507–514. doi: 10.1016/j.expneurol.2006.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BH, Torrance N, Bennett MI, Lee AJ. Health and quality of life associated with chronic pain of predominantly neuropathic origin in the community. Clinical Journal of Pain. 2007;23(2):143–149. doi: 10.1097/01.ajp.0000210956.31997.89. [DOI] [PubMed] [Google Scholar]
- Smith EM, Cohen JA, Pett MA, Beck SL. The reliability and validity of a modified total neuropathy score-reduced and neuropathic pain severity items when used to measure chemotherapy-induced peripheral neuropathy in patients receiving taxanes and platinums. Cancer Nursing. 2010;33(3):173–183. doi: 10.1097/NCC.0b013e3181c989a3. [DOI] [PubMed] [Google Scholar]
- Symons TB, Vandervoort AA, Rice CL, Overend TJ, Marsh GD. Effects of maximal isometric and isokinetic resistance training on strength and functional mobility in older adults. Journals of Gerontology Series A Biological Sciences and Medical Sciences. 2005;60(6):777–781. doi: 10.1093/gerona/60.6.777. doi: 60/6/777 [pii] [DOI] [PubMed] [Google Scholar]
- Tofthagen C. Patient perceptions associated with chemotherapy-induced peripheral neuropathy. Clinical Journal of Oncology Nursing. 2010;14(3):E22–28. doi: 10.1188/10.CJON.E22-E28. [DOI] [PubMed] [Google Scholar]
- Tofthagen C, Overcash J, Kip K. Falls in persons with chemotherapy-induced peripheral neuropathy. Supportive Care in Cancer. 2011 doi: 10.1007/s00520-011-1127-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uceyler N, Rogausch J, Toyka K, Sommer C. Differential expression of cytokines in painful and painless neuropathies. Neurology. 2007;69(1):42–49. doi: 10.1212/01.wnl.0000265062.92340.a5. [DOI] [PubMed] [Google Scholar]
- Visovsky C. Chemotherapy-induced peripheral neuropathy. Cancer Investigation. 2003;21(3):439–451. doi: 10.1081/cnv-120018236. [DOI] [PubMed] [Google Scholar]
- Visovsky C, Collins M, Abbott L, Aschenbrenner J, Hart C. Putting evidence into practice: evidence-based interventions for chemotherapy-induced peripheral neuropathy. Clinical Journal of Oncology Nursing. 2007;11(6):901–913. doi: 10.1188/07.CJON.901-913. [DOI] [PubMed] [Google Scholar]
- Wampler M, Topp K, Miaskowski C, Byl N, Rugo H, Hamel K. Quantitative and clinical description of postural instability in women with breast cancer treated with taxane chemotherapy. Archives of Physical Medicine and Rehabilitation. 2007;88:1002–1008. doi: 10.1016/j.apmr.2007.05.007. [DOI] [PubMed] [Google Scholar]
- Xiao WH, Bennett GJ. Chemotherapy-evoked neuropathic pain: Abnormal spontaneous discharge in A-fiber and C-fiber primary afferent neurons and its suppression by acetyl-l-carnitine. Pain. 2007;35(3):262–270. doi: 10.1016/j.pain.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


